Background:
Although assisted reproductive technology (ART) is extensively used in couples with fertility problems, the risk of birth defects among infants conceived with ART is still a concern. Therefore, to more accurately assess the risk of birth defects after ART treatment, we performed a meta-analysis of all available cohort studies relating to birth defects among infants conceived with ART.
Methods:
We used an established strategy to search the databases of PUBMED, EMBASE, COCHRANE, WEB OF SCIENCE, CNKI, CBM and VIP for studies published between 2008 and 2020. Subgroup analyses and sensitivity analyses were used to examine sources of heterogeneity. Pooled adjusted odds ratios (ORs) were calculated using a fixed effects model. RevMan5.3 was used to draw a forest plot, and Stata14.0 was used to test for publication bias.
Results:
We included 14 cohort studies from different countries. The infants conceived with ART had a 1.22-fold higher likelihood of birth defects than children born after natural pregnancy(OR = 1.22, 95% CI [1.17, 1.28], P < .05). The prevalence of birth defects after ART treatment was higher in singleton births than in multiple births. In a meta-analysis of data from 6 studies, we found associations between ART and birth defects related to specifics organs: cardiovascular defects, OR = 1.51, 95% CI [1.34–1.69], P < .05; musculoskeletal defects, OR = 1.09, 95% CI [1.03–1.15], P < .05; urogenital defects, OR = 1.24, 95% CI [1.11–1.38], P < .05; central nervous system defects, OR = 1.33, 95% CI [1.14–1.55], P < .05; and orofacial defects, OR = 1.45, 95% CI [1.15–1.83], P < .05.
Conclusions:
ART treatment does present an increased risk of birth defects. The prevalence of birth defects after ART treatment is lower in multiple births than in singleton births. Further research is required to examine the risks for birth defects after ART treatment.
Keywords: assisted reproductive technology, birth defects, meta-analysis, natural pregnancy
1. Introduction
Currently, the incidence of infertility caused by various factors is on the rise, and statistics from the World Health Organization show that infertility affects up to 15% of couples of reproductive age.[1] Since the birth of the first baby via in vitro fertilization (IVF) in 1978, assisted reproductive technology (ART) has been extensively used worldwide.[2] However, there are concerns about the use of ART, such as poor adverse perinatal outcomes. Some researchers[3] believe that the increased risk of adverse outcomes after in vitro fertilization and embryo transfer (IVF-ET) conception is mainly related to IVF-ET operating factors, such as the type of ovulatory drugs used in the early stage, the composition of the medium, the storage time in the medium, the freezing and thawing process of embryos, polyspermic fertilization, and the hormone levels in the body when implanting embryos. Thus, the reproductive medicine community has been paying great attention to whether the safety of offspring is affected by ART and whether there is any difference in long-term growth and development between infants conceived with ART and natural pregnancy (NP) offspring. Although the risk of birth defects after undergoing ART has been assessed in many retrospective cohort studies, current research on ART and birth defects lacks a strict follow-up of NP offspring or lacks sufficient sample sizes, which leads to biased results in current studies. Some studies suggest that there is no difference in the deformity rate between infants conceived with ART and NP offspring,[4] while other studies suggest that infants conceived with ART have higher deformity rates than NP offspring.[5,6] To date, there has been little agreement on whether infants conceived with ART have a higher rate of birth defects.
Birth defects, also known as congenital abnormalities, refer to the 4 types of developmental disorders that occur before the baby is born, including morphological and structural abnormalities, physiological and metabolic dysfunction, congenital mental retardation, and intrauterine growth retardation.[7] However, the diagnostic criteria for these defects are ambiguous and may change over time and place. The severity and continuity of defects also vary, such as for oral clefts or hypospadias. More important, however, are the general problems with ascertaining and reporting some categories of birth defects. These problems are likely to be reflected in the prevalences of birth defects reported by different studies. A particular concern would be bias due to the systematic underreporting of prenatal diagnoses.[8]
An extensive search was performed to identify studies comparing birth defects between infants conceived with ART and infants born after NP. We performed a meta-analysis of all available cohort studies relating to ART and birth defects. We examined the differences in birth defects between singleton and multiple births and studied 5 types of defects (cardiovascular defects, musculoskeletal defects, urogenital defects, central nervous system defects, and orofacial defects) to determine the impact of ART on these specific defects.
2. Methods
2.1. Search strategy
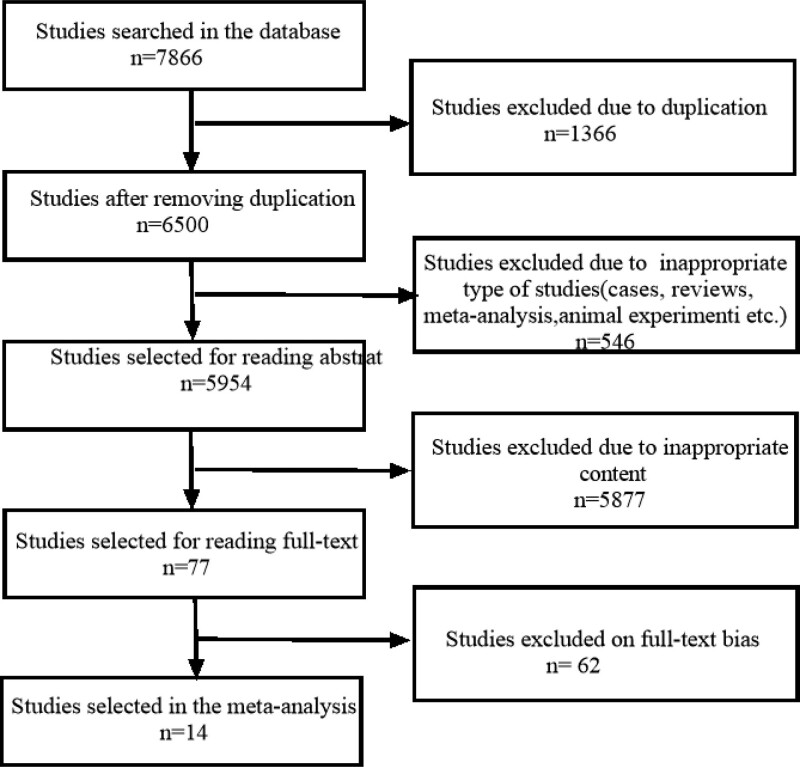
To obtain eligible studies, we searched the databases PUBMED, EMBASE, COCHRANE, WEB OF SCIENCE, CNKI, CBM and VIP. The search strategy involved various combinations of the following keywords: “assisted reproductive technology,” “microinjection,” “in vitro fertilization,” “reproduction techniques” and “birth defects,” “chromosomal abnormalities,” “pregnancy outcome,” “developmental disabilities,” “cardiovascular defects,” “musculoskeletal defects,” “hypospadias,” “neural tube defects,” “cleft lip,” and “palate.” All selected articles were published in English or Chinese. A recent large-scale meta-analysis of ART and birth defects was conducted by Hansen,[9] and their latest article from 2012 was included. To make our meta-analysis more convincing, we only analyzed articles published between Jan 01, 2008, and Jan 01, 2020. We specifically searched for papers that compared birth defects in ART infants with a non-ART comparison group (Fig. 1).The initial screening of our articles was conducted by 2 reviewers (Yue Lu and Lele Liu), and any disagreements were resolved by a panel discussion. This study was approved by the Ethics Committee of Hebei General Hospital. It is a retrospective Meta-analysis without any identifiers related with patients.
Figure 1.
Flow chart of selected studies.
2.2. Selection criteria of relevant studies
The inclusion criteria were as follows: cohort studies; studies that explicitly refer to birth defects in infants conceived with ART and naturally conceived offspring. Women in the control group were not restricted to be fertile or infertile; articles that report the odds ratio (OR) or the risk ratio (RR) of ART and NP and their 95% confidence intervals (CIs).
2.3. Data extraction and studies of quality evaluation
The data extraction of the studies was completed by 2 reviewers (Yue Lu and Lele Liu) independently, and any disagreements were resolved by a panel discussion. We used the Newcastle-Ottawa quality assessment scale [10] to evaluate the quality of the included studies (Tables 1–3). The total scores ranged from 0 (lowest quality) to 9 (highest quality); studies with scores above 6 were considered high-quality studies, while studies with scores below 6 were classified as low-quality studies.
Table 1.
Characteristics of selected studies of birth defects in infants from ART and NP pregnancies.
| Author | Publication date | Study period | Case/control | Conception method of case group | Conception method of the control group |
|---|---|---|---|---|---|
| Yang[5] | 2018 | 2006–2016 | 2484/109,559 | ART (IVF/ICSI) | NP |
| Henningsen[11] | 2018 | (2003–2007)a | 90,201/482,552 | ART | NP |
| (1998–2002)a | |||||
| (1998–2002) | |||||
| (1998–2002) | |||||
| Shechter-Maor[6] | 2018 | 2011–2013 | 71,050/11,791,730 | ART | NP |
| Bensdorp[12] | 2016 | 2000–2012 | 2437/3276 | ART | NP |
| Heisey[13] | 2015 | 1997–2005 | 1997/1,118,162 | ART | NP |
| Moses[4] | 2014 | 2007–2011 | 2071/342,496 | ART | NP |
| Farhi[14] | 2013 | 1997–2004 | 9042/213,288 | ART | NP |
| Farhangniya[15] | 2013 | 2008–2010 | 326/652 | ART | NP |
| Davies[16] | 2012 | 1986–2002 | 6163/302,811 | ART | NP |
| Halliday[17] | 2010 | 1991–2004 | 6946/20,838 | ART (IVF/ICSI) | NP |
| Vasario[18] | 2010 | 2004–2008 | 84/139 | ART | NP |
| Fujii[19] | 2010 | 1999–2003 | 1408/53,939 | ART | NP |
| El-Chaar[20] | 2009 | 2005 | 1399/60,170 | ART | NP |
| Apantaku[21] | 2008 | 1999–2004 | 88/88 | ART (IVF/ICSI) | NP |
ART = assisted reproductive technology, ICSI = intracytoplasmic sperm injection, IVF = in vitro fertilization, Multiple = included twins and higher order multiples, NP = natural pregnancy (none of the 14 articles selected indicate that the control cohort comprised of the general population was fertile women or infertile women who conceived without ART).
This article would use data 2003–2007 and 1998–2002.
Table 3.
Quality assessment of included studies.
| Author | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Causal relationship | Comparability | Assessment of outcome | Follow-up time | Follow-up quality | Quality scores |
|---|---|---|---|---|---|---|---|---|---|
| Yang[5] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| Henningsen[11] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| Shechter-Maor[6] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| Bensdorp[12] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| Heisey[13] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| Moses[4] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| Farhi[14] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| Farhangniya[15] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
| Davies[16] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| Halliday[17] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
| Vasario[18] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
| Fujii[19] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
| El-Chaar[20] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
| Apantaku[21] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
2.4. Statistical analysis
The analysis was performed using Review Manager 5.3 software provided by the Cochrane network for meta-analysis. The ORs for birth defects in the infants conceived with ART and NP offspring in the cohort studies were combined, and their 95% CIs were calculated. Since the prevalence of birth defects was 10% in all studies, we assumed that the adjusted OR was equal to the adjusted relative risk (RR: Heisey[13] 2015).[9,13] The chi-squared test was used to determine the heterogeneity of the included studies. If P > .1 and I2 < 50%, a study was considered to be homogeneous, and the fixed effects model (the Mantel–Haenszel method) was used for analysis. If P < .1 or I2 < 50%, a study was not considered homogeneous, and we used subgroup analysis or sensitivity analysis to determine the cause of heterogeneity. Finally, we also tested the included studies for publication bias. If the number of included articles was less than 10, Egger’s regression asymmetry test was used to evaluate publication bias. Otherwise, Begg’s funnel plot and Egger’s test for asymmetry were used to evaluate publication bias. Publication bias was assessed using Stata/SE14.0 for Windows (Stata Corp LP, College Station) and RevMan5.3.
3. Results
3.1. ART versus NP
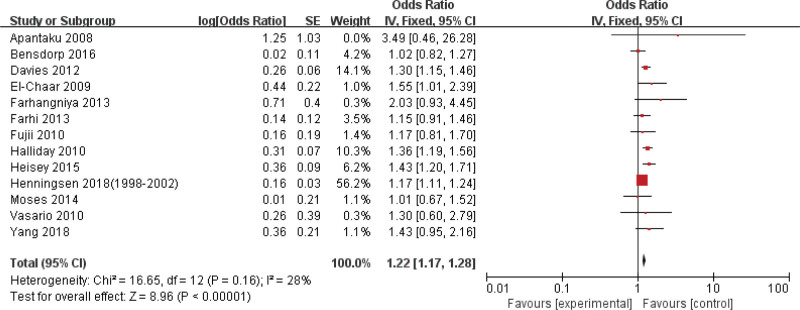
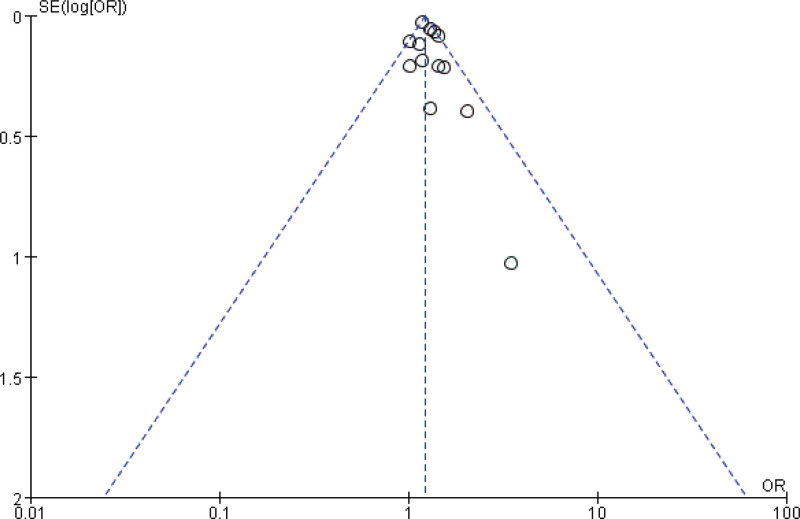
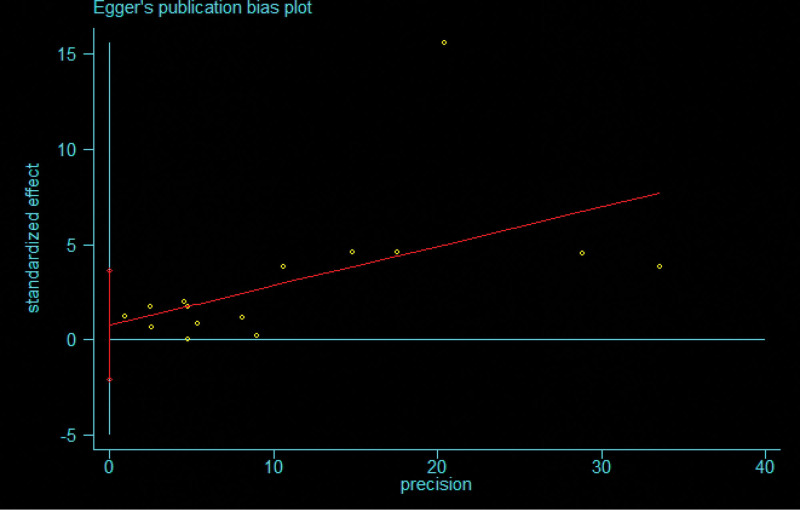
The meta-analysis of the risk of birth defects in infants conceived with ART versus NP offspring indicated that ART was weakly related to birth defects, OR = 1.22, 95% CI [1.17, 1.28], P < .05. A statistically significant amount of heterogeneity was observed among the 14 included studies, I2 = 90%, P < .1. We performed a sensitivity analysis to determine the cause of heterogeneity; to do so, we examined the effect of a single data set on the combined ORs by omitting 1 study at a time. We found that the study by Shechter-Maor[12] and Henningsen 2018 (2003–2007)[12] had the greatest impact on heterogeneity. After these studies were removed, the heterogeneity test results showed that the heterogeneity among the remaining 13 studies was significantly weakened (I2 = 28%, P = .16). We used a fixed effects model to combine the data from the 13 studies. The meta-analysis revealed that ART had a 1.22-fold higher risk for birth defects than NP (OR = 1.22, 95% CI [1.17, 1.28], P < .05) (Fig. 2). Then, Begg’s funnel plot and Egger’s test for asymmetry were used to evaluate publication bias. The shape of the funnel plot did not indicate any significant asymmetry (Fig. 3). Egger’s test was also used to provide statistical evidence of the symmetry of the funnel plot (Fig. 4).
Figure 2.
Forest plot for risk of birth defects in ART compared with NP. ART = assisted reproductive technology, NP = natural pregnancy.
Figure 3.
Funnel plot for the risk of birth defects in ART compared with NP. ART = assisted reproductive technology, NP = natural pregnancy.
Figure 4.
Egger publication bias plot for risk of birth defects in ART compared with NP. ART = assisted reproductive technology, NP = natural pregnancy.
3.2. Subgroup
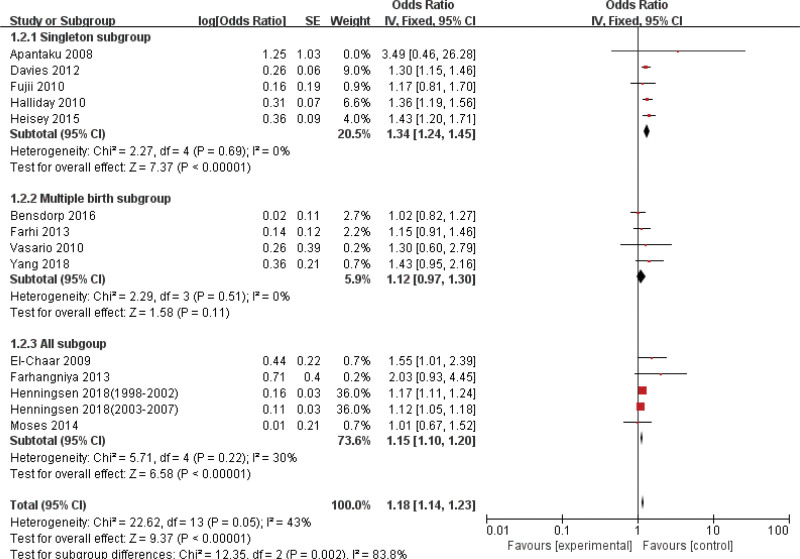
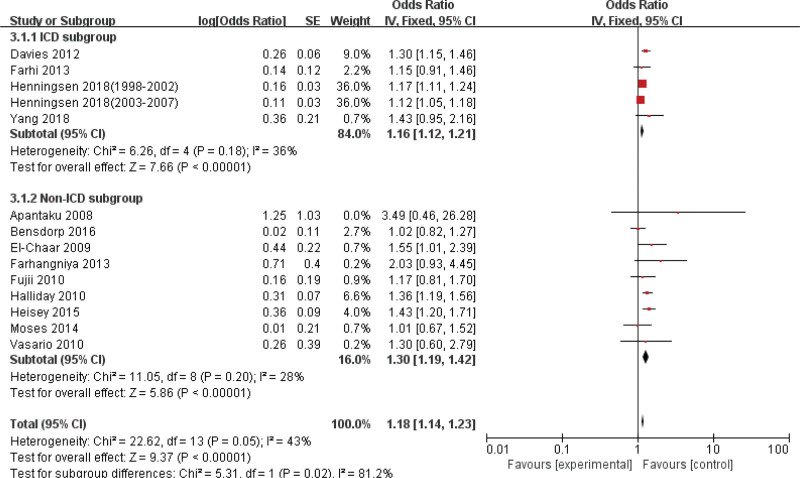
To study whether the risk of birth defects differs between singleton and multiple births and whether different defect classification methods have an impact on the outcome of defects, we performed subgroup analyses. The first subgroup analysis included the singleton subgroup, the multiple births subgroup and all subgroup (singleton and multiple births). The second subgroup analysis included the international classification of diseases (ICD) subgroup and the non-ICD subgroup. In addition, we also summarized the OR values of the specific defects (cardiovascular defects, musculoskeletal defects, urogenital defects, central nervous system defects, orofacial defects) in the 6 studies. We created forest plots to test for heterogeneity, and we used Egger’s test for each subgroup to examine publication bias (Table 4).
Table 4.
The outcomes of subgroup analyses.
| Subgroup | OR 95% CI | Heterogeneity test | Egger test |
|---|---|---|---|
| Singleton | 1.34 [1.24–1.45] | I2 = 0%, P = .69 | P = .493 |
| Multiple birth | 1.12 [0.97–1.30] | I2 = 0%, P = .51 | P = .302 |
| All | 1.15 [1.10–1.20] | I2 = 30%, P = .22a | P = .278 |
| ICD | 1.16 [1.12–1.21] | I2 = 36%, P = .18 | P = .292 |
| Non-ICD | 1.30 [1.19–1.42] | I2 = 21%, P = .26b | P = .771 |
| Cardiovascular | 1.51 [1.34–1.69] | I2 = 42%, P = .14c | P = .221 |
| Musculoskeletal | 1.09 [1.03–1.15] | I2 = 23%, P = .26 | P = .158 |
| Urogenital | 1.24 [1.11–1.38] | I2 = 0%, P = .77d | P = .221 |
| Central nervous | 1.33 [1.14–1.55] | I2 = 14%, P = .33 | P = .959 |
| Orofacial | 1.45 [1.15–1.83] | I2 = 0%, P = .86e | P = .371 |
ICD = international classification of diseases, OR = odds ratios.
The study by Shechter-Maor[7] removed after sensitivity analysis.
The study by Shechter-Maor[7] removed after sensitivity analysis.
The study by Henningsen[11] removed after sensitivity analysis.
The study by Henningsen[11] removed after sensitivity analysis.
3.3. Singleton versus Multiple birth versus All
In the singleton subgroup, the meta-analysis revealed that the risk of birth defects was slightly higher for ART than for NP (OR = 1.34, 95% CI [1.24–1.45], P < .05). In the multiple birth subgroup, the meta-analysis also revealed that the risk of birth defects was slightly higher for ART than for NP (OR = 1.12, 95% CI[0.97–1.30], P > .05). For all subgroup, the risk of birth defects was slightly higher for ART than for NP (OR = 1.15, 95% CI [1.10–1.20], P < .05). The heterogeneity was examined in all subgroups, and we found severe heterogeneity. Then, sensitivity analysis was used to determine the cause of heterogeneity. After the study by Shechter-Maor[12] was removed, the heterogeneity among the remaining 5 studies was significantly decreased. The combined ORs for the singleton subgroup were significantly higher than the combined ORs for the multiple birth subgroup (Fig. 5). The prevalence of birth defects after ART treatment was higher in the singleton subgroup than in the multiple birth subgroup.
Figure 5.
Forest plot of comparison: singleton subgroup versus Multiple birth subgroup versus all subgroup on birth defects.
3.4. ICD versus others
The definition of birth defects is still vague. Four of the 14 studies we included defined birth defects using the ICD. Six studies defined birth defects by questionnaires, organ classifications, and previously used classifications. The other 4 studies did not specify the definition of birth defects. Therefore, we classified these studies into an ICD subgroup and a non-ICD subgroup. There was a low level of heterogeneity among the studies in the ICD subgroup (I2 = 36%, P = .18). There was a high level of heterogeneity among the studies in the non-ICD subgroup (I2 = 86%, P < .05). When the study by Shechter-Maor[6] was removed, the combined ORs in the ICD subgroup decreased from 1.62 to 1.30 (95% CI 1.19–1.42). The heterogeneity among the studies also decreased (I2 = 21%, P = .26) (Fig. 6).
Figure 6.
Forest plot of comparison: ICD subgroup versus non-ICD subgroup. ICD = international classification of diseases.
3.5. Specific categories of defects
We decided to perform subgroup analyses of 5 specific subcategories of relatively common defects: cardiovascular defects, musculoskeletal defects, urogenital defects, central nervous system defects and orofacial defects. Data from the 6 studies are presented in Table 2. We performed heterogeneity tests and sensitivity analyses on these studies based on defect types. The results indicates that ART increased the risk of cardiovascular defects (OR = 1.51 95% CI [1.34–1.69], P < .05). ART also increased the risk of orofacial defects (OR = 1.45 95% CI [1.15–1.83], P < .05). There was a statistically significant amount of heterogeneity among the studies, I2 = 59%, P = .06. Sensitivity analysis was used to determine the source of the heterogeneity. We found that the study by Henningsen[11] had the greatest impact on the heterogeneity. Henningsen’s study examined orofacial defects, and the other studies examined cleft lip and/or cleft palate. After Henningsen’s study was removed, no heterogeneity was observed among the remaining studies (I2 = 0%, P = .86).
Table 2.
Characteristics of selected studies of specific categories of defects.
| Number of children in each category of birth defect | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Total number of birth defects | Cardiovascular | Musculoskeletal | Urogenital | Central nervous | Orofacial | ||||||
| ART | NP | ART | NP | ART | NP | ART | NP | ART | NP | ART | NP | |
| Yang[5](2018) | 77 | 1031 | 21 | 192 | 20 | 390 | 17 | 157 | 2 | 9 | 5c | 106c |
| Shechter-Maor[6] (2018) | 544 | 29,898 | 352 | 8499 | 22a | 4506a | 97b | 6094b | 16 | 3112 | 67c | 8229c |
| Henningsen[11] (2018) | 2100 | 10,223 | 732 | 3285 | 1200 | 5361 | 265 | 1116 | 164 | 606 | 122 | 656 |
| Farhi[14] (2013) | 221 | 3966 | 114 | 1659 | 26 | 710 | 9 | 188 | 15 | 274 | 9c | 171c |
| Davies[16] (2012) | 361 | 16,989 | 459 | 15,862 | 155 | 4878 | 145 | 5045 | 32 | 1146 | – | – |
| El-Chaar[20] (2009) | 790 | 43,462 | 798d | 16,516d | 213d | 16,516d | – | – | – | – | – | – |
ART = assisted reproductive technology, NP = natural pregnancy.
Musculoskeletal defects include omphalocele.
Urogenital defects include hypospadias.
Orofacial defects include cleft lip and/or cleft palate.
We calculated the figure.
3.6. Sensitivity analysis and publication bias
To prove the reliability of the available evidence, we performed a sensitivity analysis and bias test on all groups, and the results are presented in Table 4. We also removed studies with a large amount of heterogeneity. None of the groups showed publication bias, which proved that our selected studies were robust and reliable.
4. Discussion
Our meta-analysis addresses the question of whether ART leads to an increased risk of birth defects compared to that of NP and whether this risk is different between singleton and multiple births. We also investigated the effects of ART on cardiovascular defects, musculoskeletal defects, urogenital defects, central nervous system defects and orofacial defects. Our results suggest that infants conceived with ART had an increased risk of birth defects compared to NP offspring (OR = 1.22, 95% CI [1.17, 1.28], P < .05). When we performed subgroup analysis on singletons and multiple births, we found that the prevalence of birth defects after ART treatment was higher in singleton than multiple births. ART increased the risk of cardiovascular defects (OR = 1.51, 95% CI [1.34–1.69], P < .05).
We found that the risk of birth defects was higher in infants conceived with ART than in NP offspring (OR = 1.22, 95% CI [1.17,1.28], P < .05). Although this issue is still controversial, our results are consistent with a previously published meta-analysis.[9,22,23] The reasons why the risk of birth defects is higher among infants conceived with ART than among NP offspring are as follows. First, conventional ART operations may have a direct or potential impact on the occurrence of birth defects. Patients undergoing IVF-ET bypass the natural selection process for sperm during normal reproductive activities. The ART in vitro culture system includes semen treatment, sperm optimization, oocyte collection, egg selection and incubation, IVF, oocyte degranulation, fertilization observation, intracytoplasmic sperm injection, embryo culture and observation, embryo freezing and recovery, blastocyst culture, and blastocyst biopsy. The safety of the offspring may also be affected by the various consumables, reagents, instruments, equipment, embryo laboratory conditions, culture fluid, petri dishes, egg-holding needles, injection needles, micromanipulation systems, incubators, temperatures, humidities, and gases for culture; however, powerful and clear conclusions have not yet been reached.[24] The use of drugs that stimulate the simultaneous growth and maturation of multiple follicles may also cause birth defects. Ovarian overstimulation creates an unnatural uterine environment for the embryo.[25] However, Rimm et al[26] believe that some studies[27] may exaggerate the risk and may neglect to examine how ART can actually prevent defects. The research participants were not infertile people. For example, PGD and embryologists choose gametes and embryos, which may have a protective effect. It is too early to assert that ART itself increases the risk of birth defects. Second, the increased risk of birth defects observed in infants conceived with ART is partly attributable to parents’ basic fertility.[28–30] However, Jaques et al[31] believe that parental infertility is only weakly related to birth defects. Several previous studies have found that the increased risk of birth defects in infants conceived with ART is attributed to maternal characteristics related to infertility.[28,32–34] The risk of birth defects would increase among women with a history of infertility but no history of assisted reproductive technology.[29]
The risk of birth defects was higher in multiple births than in singleton births. However, the opposite results were obtained in the present study. The combined ORs for singletons were significantly greater than the combined ORs for multiple births. The combined effect of ART and twins on birth defects was lower than the sum of the individual effects of ART and twins.[5] This phenomenon can be explained as follows: twins conceived with ART are more likely to be dizygotic twins,[35,36] and dizygotic twins have a lower risk of birth defects than monozygotic twins.
To explore the underlying mechanism or association between antiretroviral therapy and specific deformities, a new classification system based on pathology or etiology rather than organ systems has been proposed.[37] In addition to an increased risk for all congenital malformations, increased risks for organ-specific malformations have been reported, such as cardiovascular defects,[6,11,14,16,38–40] musculoskeletal defects,[5,39] hypospadias,[41–43] central nervous system defects[14,16,40] and cleft lip and/or cleft palate.[6,14,44,45] Shechter-Maor et al[6] found that some birth defects have stronger correlations with ART than others.[6] In their study, in contrast to the NP group, for the ART group, the occurrence of cardiovascular defects was the highest risk congenital defect. Some studies,[46,47] including the present study, reported the same findings. Some studies have indicated that intracytoplasmic sperm injection causes the highest risk of hypospadias.[41,48] It is speculated that hypospadias is caused by heritable low levels of testosterone, which negatively affects the spermatogenesis of the testes.[49] Feng et al[50] found an increased Y-chromosome microdeletion rate in male children conceived by intracytoplasmic sperm injection or IVF, which may be associated with hypospadias. A Danish-based cohort study[43] used Cox regression analyses and found no associations between waiting time-to-pregnancy (TTP) and hypospadias among those who conceived naturally. They found that couples with TTP > 12 months who were pregnant after fertility treatment had a 71% higher risk of having a child with hypospadias than couples with TTP < 5 months (aHR = 1.71, 95% CI [1.24–3.36]). These findings suggest that the level of fertility treatment or infertility is related to hypospadias. For central nervous system defects, Wen et al[22] found that the probability of neural tube defects was significantly higher among infants conceived with ART (RR = 2.01 95% CI [1.27–3.20]). The present meta-analysis shows that ART and nervous system defects have a weak connection (OR = 1.33, 95% CI [1.14–1.55]). However, Shechter-Maor et al[6] did not find a link between this birth defect and ART. The protective effect of free folic acid supplementation for cerebral palsy, which began in China in 2009, will offset some of the nervous system’s defects, and early intervention through ultrasound detection (such as abortion of children with no brain or severe polymorphism) will also offset some of the nervous system defects.[5] For cleft lip and/or cleft palate, Reefhuis et al[27] suggested that ART increases the risk of orofacial clefts. Henningsen et al[11] suggested that ART does not increase the risk of cleft lip and/or cleft palate (OR = 0.94, 95% CI [0.76–1.16]); the present meta-analysis had the same results with Reefhuis et al[27] (OR = 1.45, 95% CI [1.15–1.83]).
Although the vast majority of babies born through assisted conception have no birth defects, ART is associated with an higher risk of birth defects than NP. The use of ART has increased dramatically in the past few decades, but birth defects among infants conceived with ART are still relatively rare. Most of the studies are insufficient to adequately examine the potential association between ART and birth defects. The difficulty of grouping birth defects creates a challenge for the study design and sample size. The different classification standards of birth defects used in different countries have also made research difficult. Our research can provide guidance for the use of ART. When using ART, women may choose to transfer 2 embryos because the combined risk of birth defects in ART-conceived twins is lower than the separate effects of ART and twins.[5] When studying ART-related birth defects, women may focus more on high-risk organs for birth defects, including cardiovascular defects, musculoskeletal defects, urogenital defects, urogenital defects, central nervous system defects, orofacial defects, gastrointestinal defects and respiratory system defects. Therefore, we recommend that ART staff and obstetricians pay more attention to the screening of high-risk fetuses to detect birth defects early and take appropriate interventions to reduce the incidence of birth defects.
This meta-analysis has some shortcomings. One study[15] examined major birth defects, which may have led to a slightly lower estimated incidence than the actual incidence. For the specific organ-based classification, due to the different classification methods used in various studies, the ORs of specific organs may be biased. The current main challenge is the lack of standardized ovulation induction and ART processes, unified diagnostic criteria for birth defects and classification criteria. Reproductive medicine experts, obstetricians, pediatricians, and geneticists should strengthen cooperation in the design of prospective, multicenter large-scale studies. With an increased amount of research in the future, we will have a deeper understanding of the relationship between ART and birth defects, which can better guide the use of ART.
Author contributions
Conceptualization: Yue Lu.
Investigation: Yue Lu, Lele Liu.
Supervision: Pingping Zhang, Yanmei Sun, Yali Li.
Software: Yue Lu, Cong Ma.
Writing – original draft: Yue Lu, Lele Liu.
Writing – review & editing: Pingping Zhang, Yali Li, Cong Ma.
Abbreviations:
- ART =
- assisted reproductive technology
- ICD =
- international classification of diseases
- IVF =
- in vitro fertilization
- IVF-ET =
- in vitro fertilization and embryo transfer
- NP =
- natural pregnancy
- OR =
- odds ratios
- RR =
- risk ratio
- TTP =
- time-to-pregnancy
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
How to cite this article: Lu Y, Liu L, Zhang P, Sun Y, Ma C, Li Y. Risk of birth defects in children conceived with assisted reproductive technology: A meta-analysis. Medicine 2022;101:52(e32405).
Contributor Information
Yue Lu, Email: 409367790@qq.com.
Lele Liu, Email: sophie814@163.com.
Pingping Zhang, Email: 396511819@qq.com.
Yanmei Sun, Email: sunyanmei1986@163.com.
Cong Ma, Email: 1617548331@qq.com.
References
- [1].Woldringh GH, Kremer JA, Braat DD, et al. Intracytoplasmic sperm injection: a review of risks and complications. BJU Int. 2005;96:749–53. [DOI] [PubMed] [Google Scholar]
- [2].Beltran Anzola A, Pauly V, Montjean D, et al. No difference in congenital anomalies prevalence irrespective of insemination methods and freezing procedure: cohort study over fourteen years of an ART population in the south of France. J Assist Reprod Genet. 2017;34:867–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Palomba S, Homburg R, Santagni S, et al. Risk of adverse pregnancy and perinatal outcomes after high technology infertility treatment: a comprehensive systematic review. Reprod Biol Endocrinol. 2016;14:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Moses XJ, Torres T, Rasmussen A, et al. Congenital anomalies identified at birth among infants born following assisted reproductive technology in Colorado. Birth Defects Res A Clin Mol Teratol. 2014;100:92–9. [DOI] [PubMed] [Google Scholar]
- [5].Yang M, Fan XB, Wu JN, et al. Association of assisted reproductive technology and multiple pregnancies with the risks of birth defects and stillbirth: a retrospective cohort study. Sci Rep. 2018;8:8296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Shechter-Maor G, Czuzoj-Shulman N, Spence AR, et al. The effect of assisted reproductive technology on the incidence of birth defects among livebirths. Arch Gynecol Obstet. 2018;297:1397–403. [DOI] [PubMed] [Google Scholar]
- [7].Bedard T, Lowry RB, Sibbald B. ICD-10 coding for congenital anomalies: a Canadian experience. J Registry Manag. 2012;39:4–7. [PubMed] [Google Scholar]
- [8].Lie RT, Anita L, Ørstavik KH, et al. Birth defects in children conceived by ICSI compared with children conceived by other IVF-methods; a meta-analysis. Int J Epidemiol. 2004:3. [DOI] [PubMed] [Google Scholar]
- [9].Michèle H, Kurinczuk JJ, Elizabeth M, et al. Assisted reproductive technology and birth defects: a systematic review and meta-analysis. Hum Reprod Update. 2013:4. [DOI] [PubMed] [Google Scholar]
- [10].Wells G, Shea B, O’Connell D, et al. The Newcastle–Ottawa scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. 2000.
- [11].Henningsen AA, Bergh C, Skjaerven R, et al. Trends over time in congenital malformations in live-born children conceived after assisted reproductive technology. Acta Obstet Gynecol Scand. 2018;97:816–23. [DOI] [PubMed] [Google Scholar]
- [12].Bensdorp AJ, Hukkelhoven CW, van der Veen F, et al. Dizygotic twin pregnancies after medically assisted reproduction and after natural conception: maternal and perinatal outcomes. Fertil Steril. 2016;106:371–377.e2. [DOI] [PubMed] [Google Scholar]
- [13].Heisey AS, Bell EM, Herdt-Losavio ML, et al. Surveillance of congenital malformations in infants conceived through assisted reproductive technology or other fertility treatments. Birth Defects Res A Clin Mol Teratol. 2015;103:119–26. [DOI] [PubMed] [Google Scholar]
- [14].Farhi A, Reichman B, Boyko V, et al. Congenital malformations in infants conceived following assisted reproductive technology in comparison with spontaneously conceived infants. J Matern-Fetal Neonatal Med. 2013;26:1171–9. [DOI] [PubMed] [Google Scholar]
- [15].Farhangniya M, Dortaj RE, Mozafari KR, et al. Comparison of congenital abnormalities of infants conceived by assisted reproductive techniques versus infants with natural conception in Tehran. Int J Fertil Steril. 2013;7:217–24. [PMC free article] [PubMed] [Google Scholar]
- [16].Davies MJ, Moore VM, Willson KJ, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012;366:1803–13. [DOI] [PubMed] [Google Scholar]
- [17].Halliday JL, Ukoumunne OC, Baker HWG, et al. Increased risk of blastogenesis birth defects, arising in the first 4 weeks of pregnancy, after assisted reproductive technologies. Hum Reprod. 2010;25:59–65. [DOI] [PubMed] [Google Scholar]
- [18].Vasario E, Borgarello V, Bossotti C, et al. IVF twins have similar obstetric and neonatal outcome as spontaneously conceived twins: a prospective follow-up study. Reprod Biomed Online. 2010;21:422–8. [DOI] [PubMed] [Google Scholar]
- [19].Fujii M, Matsuoka R, Bergel E, et al. Perinatal risk in singleton pregnancies after in vitro fertilization. Fertil Steril. 2010;94:2113–7. [DOI] [PubMed] [Google Scholar]
- [20].El-Chaar D, Yang Q, Gao J, et al. Risk of birth defects increased in pregnancies conceived by assisted human reproduction. Fertil Steril. 2009;92:1557–61. [DOI] [PubMed] [Google Scholar]
- [21].Apantaku O, Chandrasekaran I, Bentick B. Obstetric outcome of singleton pregnancies achieved with in vitro fertilisation and intracytoplasmic sperm injection: experience from a district general hospital. J Obstet Gynaecol. 2008;28:398–402. [DOI] [PubMed] [Google Scholar]
- [22].Wen J, Jie J, Chenyue D, et al. Birth defects in children conceived by in?. Vitro fertilization and intracytoplasmic sperm injection: a meta-analysis. Fertil Steril. 2012;97. [DOI] [PubMed] [Google Scholar]
- [23].Qin J, Sheng X, Wang H, et al. Assisted reproductive technology and risk of congenital malformations: a meta-analysis based on cohort studies. Arch Gynecol Obstet. 2015;292:777–98. [DOI] [PubMed] [Google Scholar]
- [24].Zhang Y. Human assisted reproductive technology offspring safety issues. J Shandong Uni (Medical Edition). 2019;57:52–9. [Google Scholar]
- [25].Seggers J, de Walle HEK, Bergman JEH, et al. Congenital anomalies in offspring of subfertile couples: a registry-based study in the northern Netherlands. Fertil Steril. 2015;103:1001–10. [DOI] [PubMed] [Google Scholar]
- [26].Rimm AA, Katayama AC, Paul KK. ART and major structural birth defects in the United States. Hum Reprod. 2009:7. [DOI] [PubMed] [Google Scholar]
- [27].Reefhuis J, Honein MA, Schieve LA, et al. Assisted reproductive technology and major structural birth defects in the United States. Hum Reprod. 2009;24:360–6. [DOI] [PubMed] [Google Scholar]
- [28].Pinborg A, Wennerholm UB, Romundstad LB, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome?. Systematic review and meta-analysis. Hum Reprod Update. 2012:2. [DOI] [PubMed] [Google Scholar]
- [29].Zhu JL, Basso O, Obel C, et al. Infertility, infertility treatment, and congenital malformations: Danish national birth cohort. BMJ. 2006;333:679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Mitchell AA. Infertility treatment--more risks and challenges. N Engl J Med. 2002;346:769–70. [DOI] [PubMed] [Google Scholar]
- [31].Jaques AM, Amor DJ, Baker HW, et al. Adverse obstetric and perinatal outcomes in subfertile women conceiving without assisted reproductive technologies. Fertil Steril. 2010;94:2674–9. [DOI] [PubMed] [Google Scholar]
- [32].Li HZ, Qiao J, Chi HB, et al. Comparison of the major malformation rate of children conceived from cryopreserved embryos and fresh embryos. Chin Med J (Engl). 2010;123:1893–7. [PubMed] [Google Scholar]
- [33].Huang B, Qian K, Li Z, et al. Neonatal outcomes after early rescue intracytoplasmic sperm injection: an analysis of a 5-year period. Fertil Steril. 2015;103:1432–7.e1. [DOI] [PubMed] [Google Scholar]
- [34].Metzger BE, Gabbe SG, Persson B, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Davies M, Norman R. Neurological sequelae in in-vitro fertilisation babies. Lancet. 2002,360:718–9, 719. [DOI] [PubMed] [Google Scholar]
- [36].Westergaard HB. Danish national in-vitro fertilization registry 1994 and 1995: a controlled study of births, malformations and cytogenetic findings. Hum Reprod. 1999;14:1896–902. [DOI] [PubMed] [Google Scholar]
- [37].Wellesley D, Boyd P, Dolk H, et al. An aetiological classification of birth defects for epidemiological research. J Med Genet. 2005;42:54–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Katalinic A, Rosch C, Ludwig M; German ICSI Follow-Up Study Group. Pregnancy course and outcome after intracytoplasmic sperm injection: a controlled, prospective cohort study. Fertil Steril. 2004;81:1604–16. [DOI] [PubMed] [Google Scholar]
- [39].Ooki S. Maternal age and birth defects after the use of assisted reproductive technology in Japan, 2004-2010. Int J Womens Health. 2013;5:65–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Klemetti R, Mika G, Tiina S, et al. Children born after assisted fertilization have an increased rate of major congenital anomalies. Fertil Steril. 2005;84:1300–7. [DOI] [PubMed] [Google Scholar]
- [41].Wennerholm UB, Bergh C, Hamberger L, et al. Incidence of congenital malformations in children born after ICSI. Hum Reprod. 2000:4. [DOI] [PubMed] [Google Scholar]
- [42].Ericson A, Kallen B. Congenital malformations in infants born after IVF: a population-based study. Hum Reprod. 2001;16:504–9. [DOI] [PubMed] [Google Scholar]
- [43].Arendt LH, Lindhard MS, Kjersgaard C, et al. Parental subfertility and hypospadias and cryptorchidism in boys: results from two Danish birth cohorts. Fertil Steril. 2018;110:826–32. [DOI] [PubMed] [Google Scholar]
- [44].Reefhuis J, Honein M, Rasmussen S, et al. Assisted reproductive techniques and the risk of oral clefts: data from the national birth defects prevention study, 1997-2000. Am J Epidemiol. 2004:S7. [Google Scholar]
- [45].Ooki S. Birth defects in singleton versus multiple ART births in Japan (2004-2008). J Pregnancy. 2011;2011:285706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Kallen B, Finnstrom O, Lindam A, et al. Congenital malformations in infants born after in vitro fertilization in Sweden. Birth Defects Res A Clin Mol Teratol. 2010;88:137–43. [DOI] [PubMed] [Google Scholar]
- [47].Olson CK, Keppler-Noreuil KM, Romitti PA, et al. In vitro fertilization is associated with an increase in major birth defects. Fertil Steril. 2005;84:1308–15. [DOI] [PubMed] [Google Scholar]
- [48].Fedder J, Loft A, Parner ET, et al. Neonatal outcome and congenital malformations in children born after ICSI with testicular or epididymal sperm: a controlled national cohort study. Hum Reprod. 2012:1. [DOI] [PubMed] [Google Scholar]
- [49].Simpson JL. Birth defects and assisted reproductive technologies. Semin Fetal Neonatal Med. 2014;19:177–82. [DOI] [PubMed] [Google Scholar]
- [50].Feng C, Li-Quan W, Min-Yue D, et al. Assisted reproductive technology may increase clinical mutation detection in male offspring. Fertil Steril. 2008;90:96. [DOI] [PubMed] [Google Scholar]