Abstract
Background and Aims
Primiparous women experience high levels of anxiety before cesarean section. Therefore, this research aimed to investigate the effects of the Benson Relaxation Technique (BRT) and Music Therapy (MT) on the anxiety of primiparous women prior to cesarean section.
Methods
A randomized controlled trial was carried out on 105 women scheduled for cesarean section. They were randomly assigned into three groups: BRT, MT, and control (n = 35 per group). The women in the BRT and MT groups performed exercises and listened to music, respectively, for 20 minutes prior to cesarean section. The State Anxiety Inventory was used to measure the women's anxiety in the groups before and after the intervention.
Results
Within-group comparisons showed that the women in the BRT (t = 5.61, p < 0.001, effect size (Cohen's d) = 0.94) and MT (t = 3.83, p = 0.001, d = 0.64) groups had significantly lower anxiety after the interventions compared to before the interventions. Also, between-group comparisons revealed that anxiety after the intervention was significantly lower in the BRT and MT groups compared to the control group (p = 0.007).
Conclusions
Although both of the BRT and MT helped with the reduction of anxiety among primiparous women before cesarean section, the BRT was shown more effective. These nonpharmacologic methods are safe and cost-effective and can improve well-being among women undergoing this invasive procedure. They can be used along with pharmacologic methods for reducing overreliance on medications.
1. Introduction
The rate of cesarean section as a common surgical procedure has increased across the globe in the last decades [1, 2]. A recent statistic from 150 countries shows that 18.6% of all childbirths happen by cesarean section, ranging from 1.4% to 56.4%. Also, the cesarean section in Iran has the prevalence rate of 47.9%, which is higher than in other countries [3].
Women undergoing cesarean section mostly have high levels of preoperative anxiety [4–6]. Accordingly, 63–86% of women undergoing cesarean section experience preoperative anxiety, that is higher than anxiety before general surgeries [7–9]. Parity can affect childbirth anxiety. The results of previous studies on childbirth anxiety are inconsistent [10, 11], but it has been shown that primiparous women experience more anxiety than multiparous women at childbirth [4, 12]. Distress and anxiety are associated with the selection of cesarean section over vaginal delivery as the childbirth method by women [13]. Anxiety before cesarean section can influence satisfaction with childbirth, delay recovery, and the maternal perception of pain [14]. Also, it can increase requests for analgesic medications and length of hospital stay [15, 16]. Moreover, the level of perceived anxiety before childbirth is significantly associated with postpartum hemorrhage [17], postpartum bruxism, and temporomandibular disorder [18–22]. Women's mental state can have adverse effects on the fetus leading to fetal asphyxia, abnormal fetal heart rate patterns, low Apgar scores, and increased mortality [23].
Pharmacological methods are commonly used to manage preoperative anxiety among women before cesarean section. Most antianxiety medications can pass via the placenta and cause negative consequences for the fetus [24]. Therefore, the use of nonpharmacological methods for reducing anxiety among women undergoing cesarean section has been emphasized [24–27]. For instance, the effect of relaxation techniques on the alleviation of preoperative anxiety has been reported [28–30].
The Benson relaxation technique (BRT) is a common relaxation technique and has been recognized as one of the most appropriate and cost-effective methods for reducing health problems [31–33]. The accomplishment of relaxation does not require any special tool or physician's prescription and it can be used in various situations [34, 35]. The BRT, aside from its numerous advantages and the simplicity of its implementation, has no side effects on patients [36, 37]. The effect of the BRT on patient's anxiety has been investigated in patients with different health problems. For instance, BRT can decrease anxiety symptoms in patients undergoing hemodialysis [38], those admitted to the emergency department [39], with coronary artery disease [40], surgery candidates [28], and undergoing mastectomy [41].
Music therapy (MT) is another nonpharmacologic method for relieving patients' anxiety. The use of MT as a treatment method has a long history [42, 43]. Its effectiveness to reduce anxiety in patients with different health problems such as oncologic surgery [44], chronic obstructive pulmonary disease [45], and gynecological surgery [46] have been reported.
1.1. Objectives and Hypotheses
Preoperative anxiety and the use of medications for relieving it has negative consequences for the mother and the fetus. There is a need for safe methods that can reduce maternal anxiety and improve their wellbeing in women undergoing cesarean section. Therefore, this study aimed to investigate the effects of the BRT and MT on the anxiety of primiparous women prior to cesarean section. The research hypotheses were:
The BRT and MT relieve anxiety among primiparous women prior to cesarean section compared to the control group
The anxiety level among primiparous women receiving the BRT is similar to primiparous women receiving MT
2. Methods
2.1. Study Design and Setting
A parallel, three-armed, randomized controlled trial was performed. Pregnant women scheduled for cesarean section in four public hospitals in an urban area of Iran were the study participants. The study was carried out from September 2021 to December 2021. This article has been reported using the CONsolidated Standards of Reporting Trials (CONSORTs) (Supplementary file 1).
2.2. Sampling and Recruitment
Eligibility criteria for the selection of the participants were: primiparous; full consciousness; abilities to read and write in Farsi; no history of surgical procedures, mental illness, anxiety disorder, and hearing impairment; no experience of the use of relaxation methods in the past or taking herbal or medical sedatives; an anxiety score above 31 on the State Anxiety Inventory (SAI) [47] indicating a moderate to severe anxiety level. Changes in the women's and their fetuses' hemodynamic conditions, the need for additional medical care before cesarean section, and unwillingness to cooperate during the interventions led to their exclusion.
Based on the results of previous studies [36, 41], considering α = 0.05 and β = 80%, the sample size was estimated at 35 people in each group. After obtaining permissions from the university and hospital officials, the main researcher referred to the selected hospitals. A consecutive sampling method was used for the selection of women scheduled for cesarean section. Eligible participants were approached and sufficient explanations about the research aim and process were presented to them. Willing participants were included in the study and were randomly assigned to three groups as the BRT, MT, and control using the shuffling method via cards placed in opaque envelopes [48]. Code “A” was named as the BRT, code “B” as the MT, and code “C” as the control. The letters A, B, and C were written on cards and were placed in opaque envelopes. Each of the enrolled participants was requested to pick one of the envelopes to be assigned to the groups (Figure 1).
Figure 1.
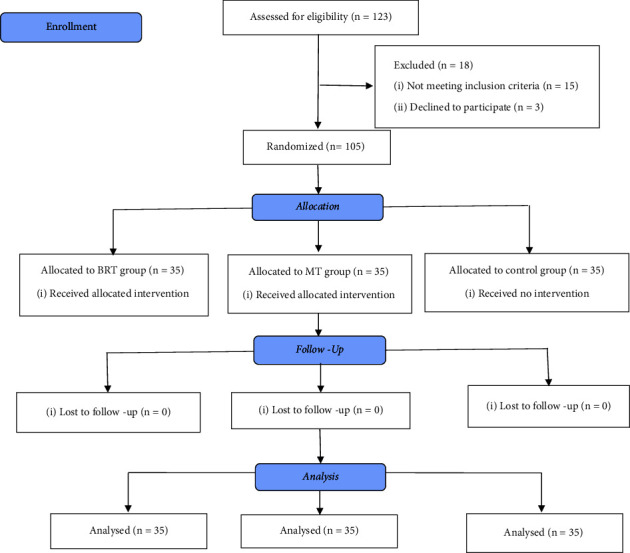
The process of the study is according to the CONSORT flow diagram (2010).
2.3. Data Collection
The demographic data questionnaire and the State Anxiety Inventory (SAI) were used.
2.3.1. Demographic Data Questionnaire
It included questions about the participants' age, marriage duration, level of education, job status, economic status, and living place. It was completed by the participants before the interventions in the women's surgical ward.
2.3.2. State Anxiety Inventory (SAI)
It contains 20 items that are scored using a four-point Likert scale ranging from 1 “not at all” to 4 “very much”. The range of scores is from 20 to 80, which is categorized from mild anxiety (score 20–31) to very severe anxiety (score above 76) [47]. For reliability, Cronbach's alpha coefficient and the test-retest reliability coefficient are reported 0.90 and 0.62, respectively [49]. The reliability of the Farsi version of SAI has been confirmed with a Cronbach's alpha coefficient of 0.90. The correlation between the observed and the real score is 0.97 [50]. The participants' anxiety was measured before and immediately after the interventions in the women's surgical ward.
2.4. Intervention
The interventions were performed two hours before the cesarean section. The participants in the BRT group were individually trained by the main researcher about how to perform this technique. To ensure the correct implementation of the technique, the participants were asked to explain it back to the researcher and modifications were made. In addition, the BRT was audio-recorded and was given to the participants to be played by an MP3 player in order to ensure of its correct implementation.
The BRT included four main principles. (i) Being placed in a quiet room in a perfectly comfortable position; (ii) taking a position and holding it for at least 20 minutes; (iii) having a mental focus on a subject or object through the repetition of a word or sound, or a pleasant feeling; (iv) having a positive attitude and mind free from thoughts, worries, and disturbances [33, 51]. The participants were placed in comfortable positions and were asked to close their eyes and focus on their breathing, to remove disturbing thoughts from their minds as much as possible. They were asked to choose a word that always reminded them of peace such as God, love, sea, and rainbow, and to start breathing deeply and regularly, inhale through the nose, exhale through the mouth, and repeat the selected sedative word. At the same time, they relaxed their muscles from the tips of their toes and continued them toward the upper body and head muscles until all muscles became fully relaxed. They were also asked not to think about the effectiveness of this method and to continue this exercise for at least twenty minutes. They were asked to open their eyes and stand still for a while to achieve the desired relaxation.
The MT group listened to nonverbal music, which was played for them for 20 minutes through an MP3 player. The song “Weightless,” by Macaroni Union, was selected and played as the nonverbal music for the MT group. Melodies in this song have no repeated pattern and steadily slow from sixty beats to fifty beats per minute over its 8 minutes duration [52].
The BRT and MT interventions were performed in the women's ward and in a private room. The “please do not enter” sign was hung on the participant's room door and their companions were asked to leave the room during the interventions. The participants in the control group only received routine nursing care. The control group received routine care that focused on a detailed explanation of the surgical procedure and recovery after cesarean section.
2.5. Ethical Considerations
The ethical approval was granted by the ethics committee of Alborz University of Medical Sciences (decree code: IR.ABZUMS.REC.1397.163). Also, the research protocol was registered at the Iranian Registry of Clinical Trials (IRCT) (code: IRCT20190408043199N1). Permissions to enter the hospitals were obtained from the relevant authorities. The participants were informed about their right to leave the study at any time without any consequence on their care. They were also assured of data confidentiality and their anonymity. The written consent form was signed by the participants before the study. Blinding of the researcher and the participants was impossible due to the nature of the interventions. However, the statistical specialist was blind to the group assignments to avoid bias during the data analysis.
2.6. Data Analysis
Descriptive statistics including mean, standard deviation, frequency, and percentage were used for summarizing the data. The Kolmogorov–Smirnov test was used to assess the normality of the data. A comparison of demographic characteristics between the study groups was conducted using the one-way ANOVA test and Chi-squared test. The One-way ANOVA test and paired samples t-test were used to compare between and within the groups' anxiety scores. To calculate the effect size as Cohen's d, the difference between the groups' means was divided into the pooled standard deviation. The data were analyzed using the SPSS v.25 and the significance level was set at p < 0.05.
3. Results
The eligibility of 123 women were assessed of which 15 women did not meet the criteria, and three women declined to participate. Therefore, 105 women were randomly assigned to the BRT (n = 35), MT (n = 35), and control (n = 35) groups. During the interventions, no sample dropping out was observed and data collected from all participants were used for the data analysis.
3.1. Demographic Characteristics of the Participants
The mean (SD) age of the participants in the BRT, MT, and control groups were 26.94 years (6.50 years), 29.97 (7.66), and 29.34 (6.68), respectively. The range of marriage duration was between 1 and 10 years with a mean (SD) of 5.25 y (2.66 y) in the BRT group, 4.94 (2.58) in the MT group, and 5.11 (2.69) in the control group. The highest frequency of educational level in the groups was for those under diploma. Other demographic characteristics have been listed in Table 1. No significant differences in the demographic characteristics between the groups were reported (p > 0.05).
Table 1.
The demographic characteristics of the participants in the groups.
| Variables | Groups N (%) | p value | ||
|---|---|---|---|---|
| BRT | MT | Control | ||
| Age; mean (SD), year | 26.94 (6.50) | 29.97 (7.66) | 29.34 (6.68) | 0.16a |
| Marriage duration; mean (SD), year | 5.25 (2.66) | 4.94 (2.58) | 5.11 (2.69) | 0.88a |
| Education level | 0.27b | |||
| Under diploma | 19 (54.3) | 20 (57.1) | 22 (62.9) | |
| Diploma | 4 (11.4) | 8 (22.9) | 8 (22.9) | |
| Academic | 12 (34.3) | 7 (20) | 5 (14.3) | |
| Job status | 0.08b | |||
| Housewife | 26 (74.3) | 19 (54.3) | 27 (77.1) | |
| Employed | 9 (25.7) | 16 (45.7) | 8 (22.9) | |
| Economic status (self-report) | 0.99b | |||
| Weak | 12 (34.3) | 2 (5.7) | 9 (25.7) | |
| Fair | 9 (25.7) | 12 (34.3) | 17 (48.6) | |
| Good | 14 (40) | 20 (57.1) | 9 (25.7) | |
| Living place | 0.33b | |||
| City | 34 (97.1) | 31 (88.6) | 31 (88.6) | |
| Village | 1 (2.9) | 4 (11.4) | 4 (11.4) | |
BRT: Benson's relaxation technique; MT: Music therapyaOne-way ANOVA testbChi-squared test.
3.2. Anxiety
The mean scores and SD of anxiety before and after the interventions in the groups have been presented in Table 2.
Table 2.
Mean scores of anxiety before and after the interventions in the groups.
| Variable | Time | Groups | F value | p valuea | ||
|---|---|---|---|---|---|---|
| BRT | MT | Control | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Anxiety | Before the intervention | 50.60 (1.30) | 49.42 (1.61) | 50.25 (1.36) | 0.17 | 0.83 |
| After the intervention | 42.31 (1.33) | 43.05 (1.19) | 48.31 (1.73) | 5.16 | 0.007 | |
|
| ||||||
| Intragroup comparison | t value | 5.61 | 3.83 | 1.21 | ||
| p valueb | <0.001 | 0.001 | 0.23 | |||
| Effect size (Cohen's d) | 0.94 | 0.64 | 0.20 | |||
BRT: Benson's relaxation technique; MT: Music therapyaOne-way ANOVA test;b Paired samples t-test.
Within-group comparisons showed that the participants in both the BRT (t = 5.61, p < 0.001, effect size (Cohen's d) = 0.94), and MT (t = 3.83, p = 0.001, d = 0.64) groups had statistically significant lower anxiety after the interventions compared to before the interventions. There was no statistically significant difference in the anxiety level before and after the interventions in the control group (t = 1.21, p = 0.23, Cohen's d = 0.20).
The between-group comparison revealed no statistically significant difference in anxiety between the BRT, MT, and control groups before the interventions (F = 0.17, p = 0.83). However, a statistically significant difference was observed in anxiety between the groups after the interventions (F = 5.16, p = 0.007). Multiple comparisons of Bonferroni showed a statistically significant difference between the BRT group (mean difference (MD) = −6.00, p = 0.01) and the MT group (MD = −5.25, p = 0.03) compared to the control group (Table 2). There was no evidence of complications resulting from the interventions or dissatisfaction with them in the intervention groups. Figure 2 illustrates changes in anxiety before and after the interventions in the groups.
Figure 2.
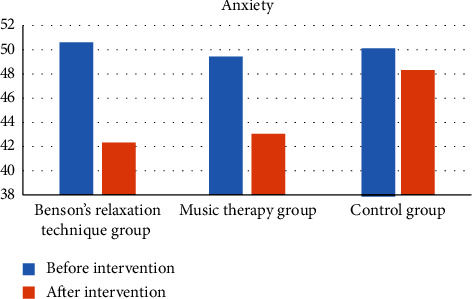
Comparison of anxiety between the study groups.
4. Discussion
This study aimed to investigate and compare the effects of the BRT and MT on anxiety among primiparous women before cesarean section. The results showed that the women's anxiety significantly decreased in the BRT and the MT groups compared to the control group.
The participants in the BRT group reported significantly lower anxiety after the intervention. Consistent with our findings, two recent studies from Iran [23] and Indonesia [53] reported that BRT reduced women's anxiety during the precesarean section period. Also, the effectiveness of the BRT on the reduction of anxiety before cataract surgery [54], gastrointestinal surgery [55], open-heart surgery [56], and angiography [57] were reported.
Anxiety, as an unpleasant mental feeling, is a natural response to potential dangers that stimulate the autonomic nervous system and trigger hormonal changes [4, 58]. Modulating neurohormonal responses in the hypothalamic, pituitary, and adrenal axes and increasing serotonin levels can regulate the secretion of cortisol and cause relaxation. Also, serotonin through facilitating the secretion of gamma-aminobutyric acid (GABA) leads to calming and modulating behavioral responses [59]. Moreover, reducing the activity of the sympathetic system and the secretion of endorphins play important roles in calming the person [60]. The BRT regulates the hypothalamus, inhibits sympathetic activity, reduces adrenaline, and increases endorphins [61] and serotonin levels [62]. Therefore, through these mechanisms anxiety can be alleviated [56].
According to our study findings, after the intervention, the participants in the MT group reported significantly lower anxiety. Similarly, the study by Kushnir et al. in Israel showed that listening to favorite music immediately prior to cesarean section decreased negative emotions including anxiety [25]. In addition, a study on Chinese women indicated that a preoperative music intervention reduced anxiety before cesarean section [63]. Another study revealed that MT not only had an effect on precesarean section anxiety but also had a lasting effect, and patients benefited from its antianxiety effects even after surgery [64]. Music can increase the stress threshold, eliminate negative emotions, regulate internal processes, create relaxed and calm states, and increase immunity, as well as the integration of psychosocial, physiological, and emotional states [65]. In addition, MT can provide direct physiological, psychological, and social-emotional benefits for patients [66]. This antianxiety effect of MT can be due to stimulating the brain and the release of hormones such as serotonin and endorphins [67].
In the present study, both the BRT and MT were effective in reducing the women's anxiety, but the BRT had more effect. The researchers found only one study comparing the effects of BRT and MT on anxiety. In an Iranian study [68], MT had a greater effect compared to the BRT on decreasing patients' anxiety levels before cardiac catheterization. This inconsistency may be due to difference in the method of MT. For instance, patients in the MT group had the right to choose music from four types of music [68] and also the nature of anxiety in the studies' partcipants was different. A previous study revealed that nature sounds and relaxation exercises were similarly effective in reducing preoperative anxiety [30]. However, further studies are needed to examine differences between BRT and MT in reducing preoperative anxiety.
In addition to the benefits of reducing precesarean anxiety using the BRT and MT, they also can have a notable effect on maternal and fetal outcomes. By stimulating the secretion of endorphins, these interventions can relieve pain, and by activating reward and pleasure centers in the brain, they can promote maternal-neonate contact, as well as promote the beginning of the breastfeeding process [69–71].
As the limitation of this study, it was impossible to provide a very quiet environment for conducting the intervention, which might have impacted anxiety in the participants. Moreover, anxiety was measured subjectively using a self-report questionnaire. Therefore, a more objective method for anxiety measurement should be used to reflect the effects of the interventions with more reliability.
4.1. Implication for Practice
One of the important roles of nurses during patient care is to identify patients' anxiety and apply the most effective method to improve their wellbeing [72, 73]. Also, nurses have the responsibility to consider the safety of the anxiety relieving method in patient care. Primiparous women often experience high anxiety levels in the precesarean period. Based on our study findings, both BRT and MT were effective in reducing precesarean anxiety, but BRT was more effective. The BRT and MT are cost-efficient, have no side effects, and are noninvasive. Therefore, it is suggested to use these interventions to decrease anxiety among pregnant women prior to cesarean section.
5. Conclusion
The BRT and MT can decrease anxiety in primiparous women before cesarean section. As safe and nonpharmacological methods, they can be used to reduce anxiety levels among them. Investigations to determine the persistence of the effects of these methods on anxiety during and after cesarean section is suggested. Future studies are suggested to investigate the combined effects of the BRT and MT on anxiety in primiparous women before cesarean section.
Acknowledgments
The present study was supported by Alborz University of Medical Sciences (Grant no. 3604397). The authors are grateful to the participants of this study.
Abbreviations
- BRT:
Benson's relaxation technique
- MT:
Music therapy
- SAI:
State anxiety inventory.
Data Availability
The complementary data used to support this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Authors' Contributions
All authors have made a substantial, direct, and intellectual contribution to the work and approved its final version for publication.
Supplementary Materials
The CONSORT checklist is presented in the supplementary file.
References
- 1.Abdelrahman A. H. N., Samy M. M., Shawky M. E. A., Azmy G. A. Subcutaneous tissue irrigation with povidone iodine in decreasing the rate of surgical site infection following cesarean section: (randomized control trial) QJM: International Journal of Medicine . 2020;113(1):hcaa056–20. doi: 10.1093/qjmed/hcaa056.020. [DOI] [Google Scholar]
- 2.Long Q., Kingdon C., Yang F., et al. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in China: a mixed-methods systematic review. PLoS Medicine . 2018;15(10) doi: 10.1371/journal.pmed.1002672.e1002672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Betrán A. P., Ye J., Moller A.-B., Zhang J., Gülmezoglu A. M., Torloni M. R. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One . 2016;11(2) doi: 10.1371/journal.pone.0148343.e0148343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun Y., Huang K., Hu Y., et al. Pregnancy-specific anxiety and elective cesarean section in primiparas: a cohort study in China. PLoS One . 2019;14(5) doi: 10.1371/journal.pone.0216870.e0216870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olieman R. M., Siemonsma F., Bartens M. A., Garthus-Niegel S., Scheele F., Honig A. The effect of an elective cesarean section on maternal request on peripartum anxiety and depression in women with childbirth fear: a systematic review. BMC Pregnancy and Childbirth . 2017;17(1):195–198. doi: 10.1186/s12884-017-1371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maleki M., Mardani A., Harding C., Basirinezhad M. H., Vaismoradi M. Nurses’ strategies to provide emotional and practical support to the mothers of preterm infants in the neonatal intensive care unit: a systematic review and meta-analysis. Women’s Health . 2022;18 doi: 10.1177/17455057221104674.174550572211046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beilin Y., Rosenblatt M. A., Bodian C. A., Lagmay-Aroesty M. M., Bernstein H. H. Information and concerns about obstetric anesthesia: a survey of 320 obstetric patients. International Journal of Obstetric Anesthesia . 1996;5(3):145–151. doi: 10.1016/s0959-289x(96)80021-5. [DOI] [PubMed] [Google Scholar]
- 8.Maheshwari D., Ismail S. Preoperative anxiety in patients selecting either general or regional anesthesia for elective cesarean section. Journal of Anaesthesiology Clinical Pharmacology . 2015;31(2):p. 196. doi: 10.4103/0970-9185.155148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferede Y. A., Bizuneh Y. B., Workie M. M., Admass B. A. “Prevalence and associated factors of preoperative anxiety among obstetric patients who underwent cesarean section”: a cross-sectional study. Annals of Medicine and Surgery . 2022;74 doi: 10.1016/j.amsu.2022.103272.103272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nekoee T., Zarei M. Evaluation the anxiety status of pregnant women in the third trimester of pregnancy and fear of childbirth and related factors. British Journal of Medicine and Medical Research . 2015;9(12):1–8. doi: 10.9734/bjmmr/2015/19784. [DOI] [Google Scholar]
- 11.Ali N. S., Azam I. S., Ali B. S., Tabbusum G., Moin S. S. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-basedcross-sectional study. The Scientific World Journal . 2012;2012:9. doi: 10.1100/2012/653098.653098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Çiçek Ö, Mete S. A common problem: fear of birth. Dokuz Eylül Üniversitesi Hemşirelik Fakültesi Elektronik Dergisi . 2015;8(4):263–268. [Google Scholar]
- 13.Zafarghandi N., Hadavand S., Torkestani F., Zaeri F., Variji M. Evaluation of anxiety and fear of labor in postpartum period. Journal of medical council of Islamic Republic of Iran . 2005;2(23):155–160. [Google Scholar]
- 14.Mousavi F. S., Golmakani N., Saki A. The relationship between postoperative pain after cesarean section with pre and postoperative anxiety. The Iranian Journal of Obstetrics, Gynecology and Infertility . 2016;19(24):1–10. [Google Scholar]
- 15.Schaal N. K., Hepp P., Heil M., et al. Perioperative anxiety and length of hospital stay after caesarean section - a cohort study. European Journal of Obstetrics & Gynecology and Reproductive Biology . 2020;248:252–256. doi: 10.1016/j.ejogrb.2020.03.045. [DOI] [PubMed] [Google Scholar]
- 16.Hepp P., The Magic Group, Hagenbeck C., et al. Measuring the course of anxiety in women giving birth by caesarean section:a prospective study. BMC Pregnancy and Childbirth . 2016;16(1):113–117. doi: 10.1186/s12884-016-0906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sadeghian A., Moghadam K. B., Baradaran R., Esmaeilzadeh M. H. Evaluation of the relationship between prenatal anxiety and intra-cesarean hemorrhage. International Journal of Medical Investigation . 2019;8(3):40–46. [Google Scholar]
- 18.Koca C., Yıldırım B., Şenyuva İ. Association between self-reported bruxism, peripartum depression and myogenous temporomandibular disorders among postpartum women in Turkey. Balkan Journal of Dental Medicine . 2021;25(3):139–146. doi: 10.2478/bjdm-2021-0022. [DOI] [Google Scholar]
- 19.Mayoral V. A., Espinosa I. A., Montiel ÁJ. Association between signs and symptoms of temporomandibular disorders and pregnancy (case control study) Acta Odontológica Latinoamericana: AOL . 2013;26(1):3–7. [PubMed] [Google Scholar]
- 20.Minervini G., Russo D., Herford A. S., et al. Teledentistry in the management of patients with dental and temporomandibular disorders. BioMed Research International . 2022;2022:7. doi: 10.1155/2022/7091153.7091153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minervini G., Fiorillo L., Russo D., et al. Prosthodontic treatment in patients with temporomandibular disorders and orofacial pain and/or bruxism: a review of the literature. Prosthesis . 2022;4(2):253–262. doi: 10.3390/prosthesis4020025. [DOI] [Google Scholar]
- 22.Minervini G., Del Mondo D., Russo D., Cervino G., D’Amico C., Fiorillo L. Stem cells in temporomandibular joint engineering: state of art and future persectives. Journal of Craniofacial Surgery . 2022;33(7):2181–2187. doi: 10.1097/scs.0000000000008771. [DOI] [PubMed] [Google Scholar]
- 23.Salmanzadeh A., Rahgoi A., Fallahi-Khoshknab M., Mohammadi-Shahbelaghi F., Rahgozar M. The Effect of Benson’s relaxation on pre-operative anxiety in Cesarean section in Nulliparus Women. Journal of Advanced Pharmacy Education & Research . 2018;8(S2):194–200. [Google Scholar]
- 24.Amiri A., Eslami J., Hatami N., Akbarzadeh M. The potential beneficial effects of education and familiarity with cesarean section procedure and the operating room environment on promotion of anxiety and pain intensity: a randomized controlled clinical trial. Journal of Education and Health Promotion . 2020;9(1):p. 240. doi: 10.4103/jehp.jehp_31_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kushnir J., Friedman A., Ehrenfeld M., Kushnir T. Coping with preoperative anxiety in cesarean section: physiological, cognitive, and emotional effects of listening to favorite music. Birth . 2012;39(2):121–127. doi: 10.1111/j.1523-536x.2012.00532.x. [DOI] [PubMed] [Google Scholar]
- 26.AjorPaz N., Ranjbar N. Effects of recitation of holy quran on anxiety of women before cesarean section: a randomize clinical trial. Qom University of Medical Sciences Journal . 2010;4(1):15–19. [Google Scholar]
- 27.Abadi F., Abadi F., Fereidouni Z., Amirkhani M., Karimi S., Najafi Kalyani M. Effect of acupressure on preoperative cesarean section anxiety. Journal of acupuncture and meridian studies . 2018;11(6):361–366. doi: 10.1016/j.jams.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Poorolajal J., Ashtarani F., Alimohammadi N. Effect of Benson relaxation technique on the preoperative anxiety and hemodynamic status: a single blind randomized clinical trial. Artery Research . 2017;17(C):33–38. doi: 10.1016/j.artres.2017.01.002. [DOI] [Google Scholar]
- 29.Vagnoli L., Bettini A., Amore E., De Masi S., Messeri A. Relaxation-guided imagery reduces perioperative anxiety and pain in children: a randomized study. European Journal of Pediatrics . 2019;178(6):913–921. doi: 10.1007/s00431-019-03376-x. [DOI] [PubMed] [Google Scholar]
- 30.Ertuğ N., Ulusoylu Ö, Bal A., Özgür H. Comparison of the effectiveness of two different interventions to reduce preoperative anxiety: a randomized controlled study. Nursing and Health Sciences . 2017;19(2):250–256. doi: 10.1111/nhs.12339. [DOI] [PubMed] [Google Scholar]
- 31.Benson H., Klipper M. Z. The Relaxation Response . NY, USA: Harpercollins; 1975. [Google Scholar]
- 32.Bagheri H., Moradi-Mohammadi F., Khosravi A., et al. Effect of Benson and progressive muscle relaxation techniques on sleep quality after coronary artery bypass graft: a randomized controlled trial. Complementary Therapies in Medicine . 2021;63 doi: 10.1016/j.ctim.2021.102784.102784 [DOI] [PubMed] [Google Scholar]
- 33.Rambod M., Pourali-Mohammadi N., Pasyar N., Rafii F., Sharif F. The effect of Benson’s relaxation technique on the quality of sleep of Iranian hemodialysis patients: a randomized trial. Complementary Therapies in Medicine . 2013;21(6):577–584. doi: 10.1016/j.ctim.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 34.Elali E., Mahdavi A., Jannati Y., Cherati J., Setareh J. Effect of benson relaxation response on stress among in hemodialysis patients. Journal of Mazandaran University of Medical Sciences . 2012;22(91):61–68. [Google Scholar]
- 35.Keihani Z., Jalali R., Shamsi M. B., Salari N. Effect of benson relaxation on the intensity of spinal anesthesia-induced pain after elective general and urologic surgery. Journal of PeriAnesthesia Nursing . 2019;34(6):1232–1240. doi: 10.1016/j.jopan.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 36.Zakerimoghadam M., Shaban M., Mehran A., Hashemi S. Effect of muscle relaxation on anxiety of patients undergo cardiac catheterization. Hayat . 2010;16(2):64–71. [Google Scholar]
- 37.Solehati T., Rustina Y. Benson relaxation technique in reducing pain intensity in women after cesarean section. Anesthesiology and Pain Medicine . 2015;5(3) doi: 10.5812/aapm.22236v2.e22236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gorji M. A., Ardebil M., Mahdavi A., Gorji A. M., Yazdani J. Implementing benson’s relaxation training in hemodialysis patients: changes in perceived stress, anxiety, and depression. North American Journal of Medical Sciences . 2013;5(9):536–540. doi: 10.4103/1947-2714.118917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ibrahim A., Koyuncu G., Koyuncu N., Suzer N. E., Cakir O. D., Karcioglu O. The effect of Benson relaxation method on anxiety in the emergency care. Medicine . 2019;98(21) doi: 10.1097/md.0000000000015452.e15452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sadeghimoghaddam S., Alavi M., Mehrabi T., Bankpoor-Fard A. The effect of two methods of relaxation and prayer therapy on anxiety and hope in patients with coronary artery disease: a quasi-experimental study. Iranian Journal of Nursing and Midwifery Research . 2019;24(2):102–107. doi: 10.4103/ijnmr.ijnmr_60_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parsa Yekta Z., Sadeghian F., Taghavi Larijani T., PhD, Mehran A. The comparison of two types of relaxation techniques on postoperative state anxiety in candidates for the mastectomy surgery: a randomized controlled clinical trial. International journal of community based nursing and midwifery . 2017;5(1):61–69. [PMC free article] [PubMed] [Google Scholar]
- 42.Najafi S., Zareipour H., Yekta T., Moaref A. The effect of music therapy on the level of anxiety and vital signs in patients undergoing trans-esophageal echocardiography. Journal of anesthesiology and pain . 2018;8(3):1–11. [Google Scholar]
- 43.Rolvsjord R., Stige B. Concepts of context in music therapy. Nordic Journal of Music Therapy . 2015;24(1):44–66. doi: 10.1080/08098131.2013.861502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Plapus-George D., Weiss C. Successful introduction of music therapy for post-operative pain, anxiety and nausea in the adult oncology patient. Journal of PeriAnesthesia Nursing . 2019;34(4):p. e42. doi: 10.1016/j.jopan.2019.05.100. [DOI] [Google Scholar]
- 45.Horuz D., Kurcer M. A., Erdoğan Z. The effect of music therapy on anxiety and various physical findings in patients with COPD in a pulmonology service. Holistic Nursing Practice . 2017;31(6):378–383. doi: 10.1097/hnp.0000000000000235. [DOI] [PubMed] [Google Scholar]
- 46.Xu X., Sun B. L., Huang F., et al. The impact of music on patient satisfaction, anxiety, and depression in patients undergoing gynecologic surgery. Journal of PeriAnesthesia Nursing . 2021;36(2):122–127. doi: 10.1016/j.jopan.2020.08.014. [DOI] [PubMed] [Google Scholar]
- 47.Spielberger C. D. State-Trait Anxiety Inventory. The Corsini Encyclopedia of Psychology . Hoboken, NJ, US: John Wiley & Sons; 2010. [Google Scholar]
- 48.Kim J., Shin W. How to do random allocation (randomization) Clinics in orthopedic surgery . 2014;6(1):103–109. doi: 10.4055/cios.2014.6.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spielberger C. D., Gorsuch R. L., Lushene R., Vagg P. R., Jacobs G. Manual for the State-Trait Anxiety Inventory . Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 50.Mahram B. Validation of Eshpil berger Anxiety Test in Mashhad . Tehran: University of Education; 1994. [Google Scholar]
- 51.Mirhosseini S., Mohammadi A., Rezaei M., Mirbagher Ajorpaz N. The effect of benson relaxation technique on the fatigue severity of patients with MS. Journal of Client-Centered Nursing Care . 2019;5(3):175–182. doi: 10.32598/jccnc.5.3.175. . [DOI] [Google Scholar]
- 52.Groarke J. M., Groarke A., Hogan M. J., Costello L., Lynch D. Does listening to music regulate negative affect in a stressful situation? Examining the effects of self-selected and researcher-selected music using both silent and active controls. Applied Psychology: Health and Well-Being . 2020;12(2):288–311. doi: 10.1111/aphw.12185. [DOI] [PubMed] [Google Scholar]
- 53.Pardede J. A., Tarigan I. The anxiety level of mother presectio caesar with Benson’s relaxation therapy. Jendela Nursing Journal . 2020;4(1):20–28. doi: 10.31983/jnj.v4i1.5801. [DOI] [Google Scholar]
- 54.Barabady A., Baghdassarians A., Memary E., Yazdani A., Barabady A., Sayadi S. Effect of Benson’s relaxation technique on propofol consumption and preoperative anxiety of patients undergoing cataract surgery. Anesthesiology and Pain Medicine . 2020;10(3) doi: 10.5812/aapm.100703.e100703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hasanpour-Dehkordi A., Solati K., Tali S. S., Dayani M. A. Effect of progressive muscle relaxation with analgesic on anxiety status and pain in surgical patients. British Journal of Nursing . 2019;28(3):174–178. doi: 10.12968/bjon.2019.28.3.174. [DOI] [PubMed] [Google Scholar]
- 56.Malmir M., Teimouri F., Pishgooie A., Dabaghi P. The Role of Benson´ s relaxation on reducing state anxiety on candidate of open heart surgery patient’s. Military Caring Sciences . 2015;2(3):182–190. doi: 10.18869/acadpub.mcs.2.3.182. [DOI] [Google Scholar]
- 57.Torabi M., Salavati M., Ghahri Sarabi A. R. Effect of foot reflexology massage and benson relaxation techniques on anxiety and physiological indexes of patients undergoing coronary heart angiography. Avicenna J Nurs Midwifery Care . 2012;20(1):63–73. [Google Scholar]
- 58.Woldegerima Y. B., Fitwi G., Yimer H., Hailekiros A. Prevalence and factors associated with preoperative anxiety among elective surgical patients at University of Gondar Hospital. Gondar, Northwest Ethiopia, 2017. A cross-sectional study. International Journal of Surgery Open . 2018;10:21–29. doi: 10.1016/j.ijso.2017.11.001. [DOI] [Google Scholar]
- 59.Nahayati M. A., Vaghar Seyyedin S. A., Bahrami-Taghanki H. R., Rezaee Z., Mehrpooya N., Rahimi H. Effect of acupressure on stress and anxiety of patients with multiple sclerosis: a sham-controlled randomized clinical trial. Complementary Medicine Journal . 2020;10(3):270–283. doi: 10.32598/cmja.10.3.1020.1. [DOI] [Google Scholar]
- 60.Lali M., Jouzi M., Moghimian M. The effect of back massage on anxiety components of mothers with preterm infants. Complementary Medicine journal . 2020;9(4):3902–3913. doi: 10.32598/cmja.9.4.933.1. [DOI] [Google Scholar]
- 61.Rahimi Bashar F., Vahedian-Azimi A., Salesi M., Hosseini S. M. The effect of progressive muscle relaxation on the outcomes of myocardial infarction: review study. Journal of military medicine . 2017;19(4):326–335. [Google Scholar]
- 62.Daube W. C., Jakobsche C. E. Biochemical effects of meditation: a literature review. Scholarly Undergraduate Research Journal at Clark . 2015;1(1):80–85. [Google Scholar]
- 63.Li Y., Dong Y. Preoperative music intervention for patients undergoing cesarean delivery. International Journal of Gynecology & Obstetrics . 2012;119(1):81–83. doi: 10.1016/j.ijgo.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 64.Hekmat-Afshar M., Hojjati H., Sharif nia S. H., Hojjati H., Salmasi E., Arazi S. The effect of music therapy on anxiety and pain in mothers after caesarean section surgery. Journal of Health and Care . 2012;14(3):16–22. [Google Scholar]
- 65.Mou Q., Wang X., Xu H., Liu X., Li J. Effects of passive music therapy on anxiety and vital signs in lung cancer patients undergoing peripherally inserted central catheter placement procedure. The Journal of Vascular Access . 2020;21(6):875–882. doi: 10.1177/1129729820908088. [DOI] [PubMed] [Google Scholar]
- 66.Lopez-Yufera E., López-Jornet P., Toralla O., Pons-Fuster López E. Non-pharmacological interventions for reducing anxiety in patients with potentially malignant oral disorders. Journal of Clinical Medicine . 2020;9(3):p. 622. doi: 10.3390/jcm9030622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Marwang S., Passe R., Aswan R., Triananinsi N., Iskandar N., Ohorella F. Effects of classical music therapy on anxiety level of caesarean section mother. Medico-Legal Update . 2020;20(3):806–810. [Google Scholar]
- 68.Hashemy S., Zakerimoghadam M. Comparative study of the effect of muscle relaxation and music therapy on anxiety level in patients waiting for cardiac catheterization. Iranian Journal of Cardiovascular Nursing . 2013;1(4):22–30. [Google Scholar]
- 69.Buckley S. J. Executive summary of hormonal physiology of childbearing: evidence and implications for women, babies, and maternity care. The Journal of Perinatal Education . 2015;24(3):145–153. doi: 10.1891/1058-1243.24.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Santiváñez-Acosta R., Tapia-López E.N., Santero M. Music therapy in pain and anxiety management during labor: a systematic review and meta-analysis. Medicina . 2020;56(10):p. 526. doi: 10.3390/medicina56100526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Radha C., Bommi K., Sumithra S. Effectiveness of benson’s relaxation therapy on pain and stress among post caesarean mothers. International Journal of Advances in Nursing Management . 2019;7(4):316–320. doi: 10.5958/2454-2652.2019.00074.x. [DOI] [Google Scholar]
- 72.Price B. Managing patients’ anxiety about planned medical interventions. Nursing Standard . 2017;31(47):53–63. doi: 10.7748/ns.2017.e10544. [DOI] [PubMed] [Google Scholar]
- 73.Eskandari S., Mirhaghjou S. N., Maleki M., Mardani A., Gholami M., Harding C. Identification of the range of nursing skills used to provide social support for mothers of preterm infants in neonatal intensive care. Critical care research and practice . 2021;2021(4):7. doi: 10.1155/2021/6697659.6697659 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The CONSORT checklist is presented in the supplementary file.
Data Availability Statement
The complementary data used to support this study are available from the corresponding author upon reasonable request.


