Abstract
Objective
Decision-making regarding end-of-life care (EOLC) place causes psychological burden on families and 70% of bereaved families have regrets. Healthcare professionals need to support families to prevent regrets. This study aims to clarify the relationship between the factors related to the decision-making methods used to choose a place of care for terminal cancer patients and the regret experienced by bereaved families.
Methods
Participants were 1110 bereaved family members of patients with cancer. The questionnaire items were as follows: the agreement between patients and their families regarding their preferred place of EOLC, decision-making methods, satisfaction with the factors involved in the decision-making processes, experience regarding communication with medical personnel, and regret experienced by the bereaved families.
Results
This analysis included 332 valid responses from 343 respondents. The regret score was significantly lower for the group wherein patients and their caregivers/families had similar preferences regarding the EOLC place (P < 0.001). Regret scores were significantly higher in the physician-led decision-making group (vs. positive role group P = 0.004, vs. shared role group P = 0.014). The regret scores for the bereaved family members were negatively correlated with the satisfaction scores for “friend support,” “relationship with doctor,” “information,” “explanation by doctor,” “thought as oneself,” and “participation in the decision” (ρ = −0.207–0.400, P ≤ 0.001).
Conclusions
To reduce bereaved families' regret, family members should know the patients’ preferred place of EOLC, and patients and their families should be supported by physicians and nurses to understand their options and participate in the decision-making process.
Keywords: Decision-making, End-of-Life, Regret, Bereaved family, Japan
Introduction
Terminally ill patients with cancer prefer to live where they like,1,2 with approximately 60% of Japanese patients preferring home death.3 More than 40% of patients with cancer in Europe and the US die at home,1,4 whereas according to a survey, about 85% of patients with cancer in Japan die at hospitals.5 Hence, there is a gap between the ideal and reality. Effective decision-making and staying where they like are components of a good death,6 and patients should be involved in decision-making about the care they receive. However, decision-making about their treatment was required for about 43% of the dying people, and 70% of them lacked the capacity.7 Therefore, expressing their preferences regarding death to their families and health professionals before the patients lose this capacity is essential.
Cancer treatment guidelines recommend early discussion on goals of care with patients with a life expectancy of less than 1 year.8 End-of-life care (EOLC) discussions are widespread in other countries.1,9 However, approximately 50% of the Japanese people have never discussed medical care during end-of-life stages with their families or medical professionals.10 Therefore, family members’ role in choosing a place for care is significant as they face psychological burdens. Approximately 70% of bereaved families experience regrets related to the decision-making process of choosing an EOLC place.11 The intensity of regret correlates with that of grief,12 and 2.3% of bereaved families of patients with cancer may have complicated grief.13 Since complicated grief is associated with mental and cardiac disorders, decreased quality of life, and suicidal ideation,14,15 supporting families during decision-making processes is important for them to make informed decisions while considering all options.
Three types of regret relate to cancer treatment: outcome regret, option regret, and process regret.16 Matching the patients' preferred and actual EOLC place positively impacts patients' quality of life and the mental health of bereaved families.17 Bereaved families of patients at their preferred place have lower levels of regret. People experience regret when they make decisions without sufficient information or with poor deliberation, even if the decision outcome is good.18,19 Regret is also correlated with satisfaction with decision-making.20 Factors related to decision-making processes include participation in the process, communication with healthcare providers, preferences of both patients and their families, the symptom control status, and the amount of information required based on the patient's situation and to compare options.11,21, 22, 23, 24 According to a previous study, “families' preferences for an EOLC place” and “communication with healthcare providers during decision-making processes” determined regret among bereaved families of patients with cancer.11 However, in this study, EOLC places were limited to hospice/palliative care units (PCUs). In addition, the study did not examine the relationship between bereaved families' regrets and the following factors: Satisfaction with “support provided through communication in the decision-making process,” “information,” “participation in the decision,” and “agreement between patients and their families.” By clarifying the relationship between these influencing factors and the bereaved families' regrets, we propose suggestions for care that would reduce bereaved families' regret.
This study aims to clarify the relationship between the factors related to the decision-making process when choosing an EOLC place for terminal cancer patients and the bereaved families’ regrets. In this study, EOLC is defined as comprehensive and specialized care for cancer patients in their preferred place of death.
Methods
We conducted a cross-sectional, anonymous survey.
Participants
The inclusion criteria for the bereaved families were as follows: (1) a primary caregiver of an adult patient with cancer ; (2) aged 20 years or older (the age of adulthood in Japan); (3) lost a loved one to cancer more than 6 months but less than 3 years ago; and (4) capable of completing a self-reported questionnaire. These criteria were determined while considering the participants’ psychological burdens and general time of recovery from grief due to the loss of a family member. In addition, to avoid recall bias, we determined these criteria based on previous studies. The exclusion criterion was that the patient had received life-saving treatments at the time of death or died in the intensive care unit.
Data collection
The facilities were selected using the snowball sampling method. We explained the purpose of the study to the management in one of the designated cancer care hospitals in Tokyo and requested their cooperation in our research. We also requested cooperation from the president of the Japan Association for Home Hospice and obtained his consent. Further, we asked the members' institution, via a newsletter, to cooperate in this study. Questionnaires in a self-addressed envelope were sent to the bereaved family members of patients with cancer by 19 institutions. Data were collected from July to December 2016.
Measurements
The questionnaire, which was developed based on previous studies, included questions regarding the participants' demographic data, experience regarding their communication with healthcare providers in the decision-making process, satisfaction with each factor in the decision-making process, satisfaction with palliative care, and bereaved families’ regret about the decision.
The regret of bereaved family members regarding the decision
The regret scale developed by Shiozaki et al is a measurement used to evaluate the bereaved families' degree of regret regarding decisions made at the time of transition to a hospice/PCU.25 This has two subscales. The decision-making process and its consequences were evaluated using four items (ie. “It was the right decision,” “I would make the same decision if I had to do it again,” “I am satisfied with the decision,” and “I regret the decision”). Another four items measured severity and intensity of regret (“Once I start thinking about possible outcomes of different decisions, I find it difficult to think about other matters,” “I had difficulty concentrating on daily activities because I could not stop thinking about regret,” “I could not stop thinking that the situation might have changed if I had made a different decision,” and “I regret the decision”). The scale comprises seven items. Participants were evaluated using a 5-point Likert scale (0: strongly disagree to 4: strongly agree). A high total score indicates stronger regret. The scores were calculated according to the score calculation method of Shiozaki et al. Reliability was assessed using Cronbach's alpha coefficient of the two subscales. It was .79 for decisional regret and .85 for intrusive thoughts. For validation, a high degree of fit has been obtained by confirmatory factor analysis (CFA; GFI = 0.97; AGFI = 0.92; CFI = 0.99; RMSEA = 0.05), and this scale had sufficient convergent validity with the Care Evaluation Scale, SF-8. The study's purpose was explained to the scale developer, and permission to use the scale was obtained. This study's participants included not only PCU or hospice patients but also patients who received care at home. Therefore, we conducted a factor analysis for the PCU or hospice group and the home group and confirmed that the regret scale structure was the same for both groups.
Experience of communication
Ten items from the questionnaire developed by Shiozaki et al were partially modified and included in this study's questionnaire.11 All items were scored on a 5-point Likert scale (1: disagree to 5: agree). These questions are not a part of the scale that calculates the sum of 10 items but asks about individual communication experiences. These evaluate each item. It was necessary to modify the wording for the bereaved families of the patients who chose home care. Two items (“Choosing a hospice/palliative care unit and discontinuing treatment for cancer were discussed at the same time” and “We were told that we will continue to provide medical care even after the patient moved to a hospice or palliative care unit.”) were modified as follows: “Choosing an EOLC place and discontinuing treatment for cancer were discussed simultaneously.” “We were told, ‘We will continue to provide medical care even after the patient moved to an EOLC place.’”
Satisfaction with decision-making
Using Kokubu's satisfaction scale, we rated the bereaved family members' satisfaction with the decision-making process.26 The questionnaire included five items indicating satisfaction with the relationship with the healthcare provider and the support of family and friends, three items indicating satisfaction with the information obtained and explanations, and two items indicating satisfaction with the degree of participation in the decision-making process. We asked the family members to rate these items based on a 4-point Likert scale (1: not at all satisfied to 4: very satisfied). High scores indicate that participants have increased satisfaction. Cronbach's alpha was 0.78 for all items.
Care evaluation scale (CES)
The care evaluation scale (CES) is used to indicate the quality of hospice and palliative care, from the perspective of bereaved families.27 The CES comprises 10 domains with 28 attributes. Participants rated the necessity for improvement using a 6-point Likert scale, from “improvement is not necessary (1)” to “improvement is highly necessary (6).” The total score was based on a 100-point scale, with higher scores indicating greater satisfaction. Cronbach's alpha was 0.98 for all items. Intraclass correlation coefficient in the test–retest examination was 0.57. The CFA reproduced a third ordered factor structure with acceptable fit indices: Chi-square (df = 388) = 879.20, P < 0.001; GFI = 0.84; AGFI = 0.81; CFI = 0.93; RMSEA = 0.072.
Participant characteristics
We inquired information, from the bereaved families, regarding the following 12 items: age of patients and caregivers, their gender, the relationship between patients and caregivers, patients' primary cancer sites, time passed after death, EOLC place, the match between the patients’ preferred and actual EOLC place, decision-making method, the agreement between patients and primary caregivers regarding their preferred EOLC places, and agreement among family members. The degree of agreement was evaluated based on a 5-point Likert scale, with higher scores indicating agreement in the preferences regarding the EOLC places.
Data analysis
The bereaved families' regret scores were compared, based on gender, relationship to the deceased person, the EOLC places, match between the patients' preferred and actual EOLC places, the degree of agreement regarding the intention to use the EOLC place, and decision-making method used for the Kruskal–Wallis test. In addition, the Bonferroni method was used for multiple comparison tests. We classified the decision-making method into three categories: “patient or family decided” and “patient or family decided with physician's opinion” as patient or family-led (positive role); “physician, patient, and family discussed and decided” as a shared role; and “physician decided with patient or family's opinion” and “physician decided” as physician-led (passive role).
Spearman's correlation coefficient was calculated to examine the relationship between the patients' age, participants' age, communication experiences with healthcare providers, the satisfaction level with each factor of the decision-making process, and the bereaved families' regret. Based on previous studies' results,11,16,18 we used the patients' satisfaction with palliative care and the patients' age at death as adjustment factors in the correlation analysis.
SPSS® ver. 24 was used as the statistical software. An alpha of .05 was used to determine statistical significance.
Ethical approval
This study's ethical approval was granted by the institutional review boards of St. Luke's International University (Approval No. 16-A005) and all participating institutions. The research request form clearly stated the purpose, methods, and freedom to participate in the study. Further, it stated that the researcher obtained the participants' addresses only after their consent, that the survey was conducted by researchers who were independent of the institution where the patients and participants received care, and who should be contacted in case of psychological distress caused by participation in the study. Returning of questionnaires was regarded as consent to participate in the study. The collected data were anonymized to maintain individuals' confidentiality.
Results
The number of participants and response rate
This study involved 1110 bereaved families at 19 facilities in 8 prefectures; further, we sent questionnaires to 489 people, among whom 343 responded (response rate: 70.1%). Ten participants did not meet the participant eligibility criteria and one participant did not indicate their EOLC place; therefore, 332 participants were analyzed.
Participant data
Table 1 summarizes the basic attributes of the participants and the deceased.
Table 1.
Characteristics of participants.
| Characteristics | Total |
Palliative care unit/hospice |
Home |
Other hospital/facility |
Residential Hospice |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| Gender (n = 332) | ||||||||||
| Male | 181 | 54.5 | 70 | 46.1 | 100 | 60.2 | 10 | 83.3 | 1 | 50.0 |
| Female | 151 | 45.5 | 82 | 53.9 | 66 | 39.8 | 2 | 16.7 | 1 | 50.0 |
| Primary cancer site (n = 320) | ||||||||||
| Lung | 75 | 23.4 | 31 | 21.4 | 34 | 21.0 | 9 | 81.8 | 1 | 50.0 |
| Stomach/Esophagus | 51 | 15.9 | 18 | 12.4 | 32 | 19.8 | 1 | 9.1 | 0 | 0 |
| Colorectum/rectum | 31 | 9.7 | 17 | 11.7 | 13 | 8.0 | 0 | 0 | 1 | 50.0 |
| Breast | 29 | 9.1 | 26 | 17.9 | 3 | 1.9 | 0 | 0 | 0 | 0 |
| Liver/Gall bladder/Pancreas | 52 | 16.3 | 20 | 13.8 | 32 | 19.8 | 0 | 0 | 0 | 0 |
| Other | 82 | 25.6 | 33 | 22.8 | 48 | 29.6 | 1 | 9.1 | 0 | 0 |
| Age (years) (mean ± SD) (n = 332) |
72.0 |
±12.8 |
70.3 |
±13.5 |
73.3 |
±12.2 |
72.5 |
±10.8 |
85.0 |
±1.4 |
| Breaved family members |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
| Gender (n = 326) | ||||||||||
| Male | 93 | 28.5 | 53 | 35.1 | 39 | 24.1 | 1 | 9.1 | 0 | 0 |
| Female | 233 | 71.5 | 98 | 64.9 | 123 | 75.9 | 10 | 90.9 | 2 | 100.0 |
| Relationship to decedent (n = 332) | ||||||||||
| Spouse | 169 | 50.9 | 70 | 46.1 | 92 | 55.4 | 6 | 50.0 | 1 | 50.0 |
| Children | 129 | 38.9 | 61 | 40.1 | 61 | 36.7 | 6 | 50.0 | 1 | 50.0 |
| Parent | 11 | 3.3 | 4 | 2.6 | 7 | 4.2 | 0 | 0 | 0 | 0 |
| Other | 23 | 6.9 | 17 | 11.2 | 6 | 3.6 | 0 | 0 | 0 | 0 |
| Age (years) (mean ± SD) (n = 323) | 62.2 | ±12.3 | 60.5 | ±12.1 | 64.2 | ±12.3 | 55.5 | ±11.4 | 67.5 | ±17.7 |
| Months after death (mean ± SD) (n = 332) | 20.8 | ±8.1 | 20.1 | ±8.3 | 21.4 | ±7.9 | 18.6 | ±8.6 | 28.0 | ±5.7 |
| Satisfaction with decision-making (mean ± SD) (n = 269) | 31.2 | ±5.7 | 32.0 | ±5.4 | 30.6 | ±5.6 | 28.6 | ±8.2 | 20.0 | ±.00 |
| Care Evaluation Scale (mean ± SD) (n = 264) | 77.6 | ±19.5 | 80.5 | ±19.9 | 75.8 | ±17.9 | 62.0 | ±23.5 | 62.8 | ±5.5 |
EOLC place, agreement between patients and participants’ preferences
The actual EOLC places for most patients included PCUs, hospices, and their homes. Regarding whether the patients' preferred and actual places of care matched, 231 (69.6%) respondents answered yes, 30 (9.0%) answered no, 52 (15.7%) did not know the patient's original preference, and 19 (5.7%) did not answer. Most bereaved family members of patients who spent time in PCUs, hospices, or at home indicated a match between the patients' actual and preferred places of care (69.1% in PCUs or hospices and 82.5% at home). Conversely, most bereaved family members of patients who spent time in other hospitals or facilities indicated that a match between the patients' preferred places of care did not match the actual places of care (66.7%).
The responses regarding the agreement between patients and participants’ preferences were as follows: “Not applicable” 14 (4.2%), “Not really applicable” 16 (4.8%), “Neither applicable nor not applicable” 55 (16.6%), “Applicable” 123 (37.0%), “Very much applicable” 118 (35.5%); and “No response” 6 (1.8%). Approximately 70% of the participants answered that their intended places of treatment were consistent with those preferred by the patients.
Regarding the agreement among family members, 21 (6.3%) of respondents answered “not applicable or not very applicable,” 28 (8.4%) answered “neither applicable nor not very applicable,” 267 (80.4%) answered “applicable or very applicable,” and 16 (4.8%) did not answer. Approximately 80% of the bereaved families answered that the preferences of primary caregivers, other family members, and their patient were consistent with each other.
Out of 308 evaluable bereaved families, 95 (30.8%) had regrets. The mean regret score was 5.43 (SD 5.76).
Relationship between regrets scores and characteristics
The relationship between gender, relationship to the decedent, and bereaved families’ regret scores was analyzed. There were no differences in regret scores by gender (mean score of males = 5.72 [SD 5.22], mean score of females = 5.31 [SD 5.31], U = 8871.5 [P = 0.181]) or relationship of survivors (mean score of spouses = 6.05 [SD 6.28], mean score of children = 4.72 [SD 4.68], mean score of parents = 6.22 [SD 7.39], χ2 = 0.974 [P = 0.615]).
Correlation analysis was conducted to clarify the relationship between bereaved family members' age, patients' age, and regret scores. The regret scores were not correlated with bereaved family members' age (ρ = −0.016, P = 0.780) and patients’ age (ρ = −0.113, P = 0.048).
Bereaved families’ regret regarding their choice of EOLC place
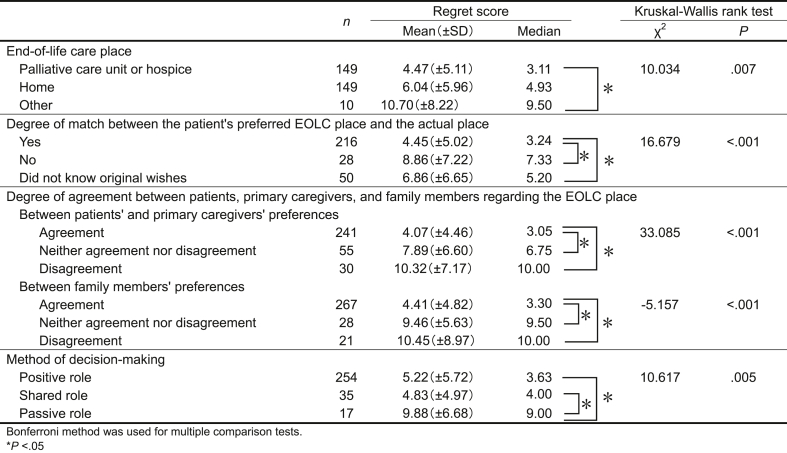
The participants' regret scores were compared based on the EOLC place, match between the patients’ preferred and actual places, the degree of agreement regarding the preferred EOLC place, and decision-making method. The results are shown in Table 2.
Table 2.
Differences in the regret scores of bereaved families by item.
Comparison of regret scores among EOLC places
The relationship between EOLC places and bereaved families’ regret scores was analyzed, showing that the regret scores for those with patients in other hospitals or facilities group were higher, compared with the scores for those with patients in the PCU or hospice group and at home group (P = 0.023).
Comparison of regret scores by the matching degree between patients’ preferred place and the actual place
The relationship between regret scores and the matching degrees between the patients' preferred EOLC locations and actual locations was analyzed and shown as significant (P < 0.001). The group that answered that the patients’ preferred place of care matched the actual place of care had a significantly lower regret score than did the other two groups (vs. “no” group P = 0.001, vs. “did not know the original wish” group P = 0.031).
Comparing regret scores according to the degree of agreement between patients, primary caregivers, and family members regarding the EOLC place
The regret scores for the group in which patients and primary caregivers agreed on the EOLC place were significantly lower, compared with those for the other two groups (neither group P < 0.001, disagreement group P < 0.001).
Similarly, the group in which the patients, primary caregivers, and other family members agreed on the place of treatment had significantly lower regret scores, compared with the other two groups (neither group P < 0.001, disagreement group P = 0.010).
Comparison of regret scores based on decision-making method for selecting an EOLC place
After comparing the regret scores using the decision-making method, the “passive role” of physician-led group had significantly higher regret scores compared to the other two groups of physician–patient/family collaborations, patient or family-led (vs. positive role group P = 0.004, vs. shared role group P = 0.014).
Relationship between the degree of satisfaction with each factor considered when selecting EOLC places and the regret of bereaved families
Correlation analysis was conducted to clarify the relationship between satisfaction with the decision-making process and regret experienced by the bereaved [Table 3]. The bereaved families' regret scores were significantly negatively correlated with the following items of satisfaction with the decision-making process: “friends’ support,” “relationship with physician,” “information,” “explanation by physician,” “thought as oneself,” and “participation in the decision” (ρ = −0.207 to 0.400, P ≤ 0.001).
Table 3.
Relationship between the degree of satisfaction with each factor in the decision-making process of selecting an end-of-the life care place and the regret scores of the bereaved family.
| Variables | Mean (±SD) | Correlation coefficienta,b | P |
|---|---|---|---|
| Satisfaction with decision making | |||
| Family's support (n = 253) | 3.46 (±0.78) | −0.113 | 0.073 |
| Friends' support (n = 242) | 3.07 (±0.94) | −0.207 | 0.001 |
| Peer support (n = 242) | 2.21 (±1.00) | −0.197 | 0.002 |
| Relationship with physicians (n = 257) | 3.26 (±0.92) | −0.320 | <0.001 |
| Relationship with nurses (n = 257) | 3.49 (±0.72) | −0.169 | 0.007 |
| Information (n = 257) | 3.15 (±0.84) | −0.306 | <0.001 |
| Explanation by physician (n = 255) | 3.09 (±0.95) | −0.229 | <0.001 |
| Explanation by nurses (n = 256) | 3.11 (±0.92) | −0.173 | 0.005 |
| Thought as oneself (n = 256) | 3.29 (±0.73) | −0.400 | <0.001 |
| Participation in the decision (n = 255) | 3.39 (±0.72) | −0.392 | <0.001 |
Spearman's rank correlation coefficient.
The level of satisfaction with palliative care and the patient's age at death were used as adjustment factors.
We conducted a correlational analysis to determine which communication experiences with healthcare providers, in the process of choosing a place, are associated with decisional satisfaction [Table 4]. Six experiences were significantly correlated with the decisional satisfaction items associated with regret by the bereaved. These include the following: “I could fully discuss what I did not understand”; “They listened to my specific concerns and feelings about what to do in the future”; “I could consult with them in accordance with their mental preparation process”; “We talked, specifically, about what I can do as a future goal”; “I could discuss the latest treatment”; and “We were told that they would continue to provide medical care, even after the patient moved to a new place.” (ρ = −0.226 to 0.519, P < 0.001).
Table 4.
Correlation between communication experiences with healthcare providers and each satisfaction factor in the decision-making process of selecting an end-of-the life care place.
| Communication experiences | Satisfaction with decision-making |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Family’s support | Friends’ support∗ | Peer support | Relationship with physicians∗ | Relationship with nurses | Information∗ | Explanation by physician∗ | Explanation by nurses | Thought as oneself∗ | Participation in the decision∗ | |
| I could fully discuss what I did not understand. | 0.077 | 0.117‡ | 0.273‡ | 0.463‡ | 0.395‡ | 0.490‡ | 0.500‡ | 0.441‡ | 0.283‡ | 0.283‡ |
| They listened to my specific concerns and feelings about what to do in the future. | 0.028 | 0.148† | 0.191‡ | 0.488‡ | 0.398‡ | 0.443‡ | 0.519‡ | 0.450‡ | 0.251‡ | 0.271‡ |
| I could consult with them in accordance with their mental preparation process. | 0.094 | 0.226‡ | 0.233‡ | 0.406‡ | 0.348‡ | 0.404‡ | 0.452‡ | 0.408‡ | 0.233‡ | 0.286‡ |
| Choosing an EOLC place and discontinuing treatment for cancer were discussed simultaneously. | 0.127† | 0.077 | 0.002 | 0.097 | 0.107 | 0.050 | 0.162‡ | 0.138† | 0.180‡ | 0.176‡ |
| We talked, specifically, about what I could do as a future goal. | 0.079 | 0.188‡ | 0.136† | 0.460‡ | 0.336‡ | 0.349‡ | 0.479‡ | 0.405‡ | 0.234‡ | 0.272‡ |
| I could discuss the latest treatment. | 0.090 | 0.157† | 0.242‡ | 0.302‡ | 0.157† | 0.261‡ | 0.354‡ | 0.212‡ | 0.089 | 0.117 |
| We were told, “There was nothing we could do for the patient.” | −0.012 | −0.088 | −0.017 | −0.163† | −0.148† | −0.095 | −0.164† | −0.083 | −0.027 | −0.046 |
| We were told that the patient could be discharged when the condition improved and think about returning to the general ward for treatment. | −0.005 | −0.035 | 0.043 | 0.062 | 0.089 | 0.038 | 0.094 | 0.118 | −0.070 | −0.051 |
| We were told, “We will continue to provide medical care even after the patient moved to an EOLC place.” | 0.109 | 0.056 | 0.030 | 0.185‡ | 0.186‡ | 0.124† | 0.243‡ | 0.213‡ | 0.057 | 0.061 |
| The healthcare providers said, “I think this is the best choice.” | 0.102 | −0.043 | 0.047 | 0.079 | 0.076 | 0.065 | 0.130† | 0.057 | −0.001 | 0.038 |
Spearman's correlation coefficient was calculated to examine. The level of satisfaction with palliative care and the patient's age at death were used as adjustment factors.
∗: Satisfaction items that were significantly correlated with the bereaved families' regret scores, †: P < 0.05, ‡: P < 0.01.
Discussion
This survey revealed that the regret experienced by bereaved families concerning their decisions when selecting EOLC places for patients with terminal cancer was related to the agreement between the patients and their families regarding their preferred places for care, satisfaction with “friends’ support,” “relationship with physicians,” “information,” “explanation by physicians,” and “participation in the decision.”
Participants’ characteristics and their states of regret
Approximately 50% of the patients with cancer in this study stayed in PCUs or hospices, while the rest stayed at home, and for approximately 70% of the patients, their preferred and actual EOLC places matched. In addition, 82% of the respondents played a positive role in the decision-making process, and more than 70% of the respondents indicated that their intended places of care were consistent with those preferred by the patients, the primary caregivers, and other family members. In a previous study,11 65.3% of the respondents played a positive role in the decision-making process. In this study's target population, both patients and family members actively participated in decision-making processes and made choices in accordance with the patients' wishes.
Regarding satisfaction with palliative care, the mean CES scores for participants who chose PCUs, hospices, or their homes as their EOLC places were high and comparable to the scores of previous studies.28 The participants in this study were highly satisfied with the palliative care they received.
In this study, approximately 70% of the bereaved families had no regrets at all, while in a previous study,11 approximately 30% of the bereaved families had no regrets; the participants in this study had low regret scores. The association between characteristics and bereaved families' regret was significantly weak, with identification of only the patients' age. This could be because of the selection bias caused by the questionnaire mailing method. In addition, the “Cancer Control Act” was enacted in 2006 in Japan, and the Basic Plan to Promote Cancer Control Programs was formulated based on this law. The overall goals of the plan were to alleviate the suffering of all patients with cancer and their families and to improve their quality of life. We considered that another reason for the reduced regrets was that the public's awareness of quality of life and participation in medical care had increased since then.
Relationship between patients and family members' preferences regarding EOLC places, decision-making methods, and regret of the bereaved
The bereaved families' regret scores were significantly higher in the group that answered “other” as the EOLC place. Moreover, for more than 60% of the group of patients who spent time in “PCUs,” “hospices,” or at “home,” their actual place of care matched their preferred places, whereas more than 60% of the patients who spent time in “other” places did not match their preferred and actual places of care. Therefore, it is important for patients to spend time in their preferred places of care. The results were consistent with those of previous studies, which indicate that matching patients' preferred EOLC places with their actual place of death affects their quality of life and the bereaved families’ depression and grief.17
In addition, the regret score was significantly lower for the group in which the patients, primary caregivers, and family members had the same preferences regarding the place of care. Regret regarding what was not done was stronger than that for what was done.12,18 One reason why some bereaved families had no regrets is that they felt that they had respected the patients' wishes regarding end-of-life decision-making.19 Therefore, all family members need to discuss the patient's preferences regarding the place of care, and they all need to agree on their preferences to reduce regrets, such as “I should have listened to the patient's preferences at that time.”
After comparing regret scores based on the decision-making method, the “passive role” group had significantly higher regret scores than the “positive role” and “shared role” groups. We suggest that increasing active participation in decision-making may reduce the regret experienced by the bereaved. As Japanese people do not normally verbalize the death of their close ones, it can be inferred that it is not easy for patients and their families to discuss places of terminal care. Therefore, it is more effective for the patients and their families if healthcare providers initiate and support the discussion. We also propose that having a collaborative decision-making process that involves healthcare providers, including the option of letting them decide, is helpful. However, this study's results cannot be applied to a wide range of populations because it could not examine the crossover between the decision-making methods desired by the participants and the actual decision-making methods. When actually providing support, it is necessary to do so in accordance with a patient and the family's preferred decision-making method.
Further, the “shared role” group is based on the assessment that a bereaved family made the decision in collaboration with the physician. It is not clear whether healthcare providers supported decisions based on their understanding of shared decision-making (SDM). SDM is associated with the understanding of a patient's illness and satisfaction with the decision-making method.29 Evaluation by healthcare providers is also necessary to ensure that decisions are made collaboratively. Although the regret scores between the “positive role” group and the “shared role” group were similar, it is possible that regret would be reduced if healthcare providers who understood SDM provided decision-making support. We need to assess the knowledge and practice of SDM among healthcare providers. We also need to verify whether regret scores are lower when both the healthcare providers and the patients, as well as their families, perceive SDM.
Relationship of each satisfaction factor with decision-making and regret of the bereaved
In this study, the bereaved families' regret was less for those who were satisfied with the following items of the decision-making process: the degree of “participation in the decision,” “relationship with physician,” the “information,” “explanation by physician,” and “friends’ support.” The bereaved who were satisfied with these items of the decision-making process experienced less regret. This study found no relationship between bereaved families' regret and their satisfaction with nurses. This may have been influenced by the fact that not all participants received care from visiting nurses or discharge coordinating nurses and that the participants had experienced a high level of satisfaction with palliative care.
From Table 4, the experience regarding the communication with healthcare providers, which was related to all the factors of decision satisfaction that correlated with regret of the bereaved, was the ability to consult with them in accordance with their mental preparation. In the decision-making process of choosing an EOLC place, a family is often forced to discontinue aggressive cancer treatment simultaneously; therefore, the psychological burden on the family is heavy. Furthermore, as the family members’ readiness regarding the decision-making is diverse, it is necessary to consider their thoughts and feelings at all times and to proceed with explanations in accordance with their mental readiness.
As people often experience conflicts in decision-making processes related to health problems, information and participation are considered as central to reducing stress.30 The experience of discussing the latest treatments, fully discussing unclear issues, and specifically discussing future goals may promote a family's participation in the decision-making and reduce decisional regret because of poorly considered choices. Healthcare providers need to understand and communicate with family members whose situations fluctuate depending on the patient's ever-changing condition.
Implications for nursing
Based on the related factors revealed in this study, to reduce the regret experienced by bereaved family members, the family members need to know about the patients' preferences regarding the place of care, ensure their preferences are consistent, and support, and thus encourage participation in the decision-making processes. Approximately 50% of Japanese people have never discussed medical care during the end-of-life stage because they lack opportunities, do not perceive the discussions as necessary, and do not know what to discuss.10 The results showed that spending the final days in the patient's preferred place and matching the agreement between the patient and the family on the EOLC place were associated with fewer regrets. This study also supported the results of previous research.17 Based on these findings, it will be important for nurses to confirm the patient's and family's preferences and support them in making decisions that consider both parties' preferences, situations, and the process they have spent their lives in, given that the risk of regret for bereaved families may increase when the patients and their families do not have the same preferences regarding EOLC place.
The low regret scores were associated with bereaved families’ thought as themselves regarding the choice for the EOLC place, being satisfied with their participation, and not making a physician-led decision. Therefore, families should be supported to participate in decision-making. Nonetheless, when facilitating participation in decision-making, some patients may not want their families to be involved.31 Nurses need to understand the kind of participation the patient and family prefer and support them to participate in decision-making in a way that is preferable to each patient and family.
It is also important that bereaved families can consult with healthcare providers according to their mental preparation process, as this is relevant to many of the decision-making satisfaction items. Nurses need to check whether the patients and families are ready to make decisions in their daily interactions. Nurses should also act as a bridge, checking the family's understanding of the advantages and disadvantages of each option, understanding their concerns, facilitating discussions between families and patients or physicians, and providing supplementary explanations to clear up any doubts. Hence, as the family's satisfaction with the relationship with physicians, the explanation by physicians, and the information obtained increases, the bereaved family's regrets may decrease.
Limitations
This study was a retrospective survey of bereaved families who had been bereaved for more than 6 months but less than 3 years; therefore, the results may have been influenced by recall bias.
In this analysis, the direct correlation coefficients between each variable and the bereaved families’ regret scores were calculated; these variables are thought to influence each other. For further research, the relationships among the related factors and the power of their effects should be examined using methods such as covariance structure analysis.
This study's data were obtained from participants who agreed to participate and who could fill in the questionnaires. As the respondents of the questionnaire were participants with low regret scores, some related factors may not have been detected.
Conclusions
The regrets experienced by bereaved families were related to the following factors: patients' stay at their preferred EOLC place, agreement of preferences between patients, primary caregivers, and family members, satisfaction with decision-making methods, “friends' support,” “relationship with physician,” “information,” “explanation by physician,” “thought as oneself,” and “participation in the decision-making. To reduce the regret of the bereaved family, family members should have the opportunities to know the patients’ preferences regarding the EOLC place and to support and thus encourage participation in the decision-making processes.
Acknowledgments
The authors would like to thank the bereaved families and the collaborators at each facility for cooperating with the survey.
Author contributions
Conceived and designed the analysis: Aiko Okimura, Naoko Hayashi.
Collected the data: Aiko Okimura.
Performed the analysis: Aiko Okimura, Naoko Hayashi.
Wrote the paper: Aiko Okimura, Naoko Hayashi.
Declaration of competing interest
None declared.
Funding
This work was supported by JSPS KAKENHI (Grant No. JP17H04444).
Ethics statement
This study's ethical approval was granted by the institutional review boards of St. Luke's International University (Approval No. 16-A005) and all participating institutions.
References
- 1.Rebecca S., Eve R., Alex G.S., et al. Preferred and actual place of death in haematological malignancies: a report from the UK haematological malignancy research network. BMJ Support Palliat Care. 2021;11:7–16. doi: 10.1136/bmjspcare-2019-002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jonas N., Carl B., Georg H., Tobias C., Michael B., Stefan B. End-of-life care: where do cancer patients want to die? A systematic review. Asia Pac J Clin Oncol. 2017;13:356–364. doi: 10.1111/ajco.12678. [DOI] [PubMed] [Google Scholar]
- 3.The Nippon Foundation. National Survey results on how to face end of life. Available from: https://www.nippon-foundation.or.jp/who/news/pr/2021/20210329-55543.html. [accessed 3 October 2022].
- 4.Fumiko C., Arif H.K., Thomas W.L., Yousuf Z S., Gita S., Junzo P.C. Place of death for patients with cancer in the United States, 1999 through 2015: racial, age, and geographic disparities. American Cancer Society. 2018;124:4408–4419. doi: 10.1002/cncr.31737. [DOI] [PubMed] [Google Scholar]
- 5.Ministry of Health, Labour and Welfare. Survey of bereaved family members on the medical care received by the patient: Report on the results of the survey in 2018. Available from:: https://www.mhlw.go.jp/content/10901000/000860135.pdf. [accessed 3 October 2022].
- 6.Miyashita M., Morita T., Sato K., Hirai K., Shima Y., Uchitomi Y. Good Death Inventory: a measure for evaluating good death from the bereaved family member's perspective. J Pain Symptom Manag. 2008;35:486–498. doi: 10.1016/j.jpainsymman.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Maria J.S., Scott Y.H.K., Kenneth M.L. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362:1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michael H.L., Anthony B., Costantino B., et al. Palliative care clinical practice guidelines in Oncology. J. Natl Compr Canc Netw. 2009;7:436–473. doi: 10.6004/jnccn.2009.0031. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence. NICE impact end of life care for adults. Available from: https://www.nice.org.uk/Media/Default/About/what-we-do/Into-practice/measuring-uptake/End-of-life-care-impact-report/nice-impact-end-of-life-care.pdf. [accessed 3 October 2022].
- 10.Ministry of Health, Labour and Welfare. Report on the 29th fiscal year of the Heisei period Survey on Attitudes toward Medical Care in the Final Stage of Life. Available from: https://www.mhlw.go.jp/toukei/list/dl/saisyuiryo_a_h29.pdf. Japanese. [last accessed on 2022 Jan 25].
- 11.Shiozaki M. The Japan Hospice and Palliative Care Evaluation Study. Seikaisya; Tokyo: 2010. Determinants of bereaved families' regret regarding decision-making when admitted to a hospice/palliative care unit; pp. 43–47. Japan Hospice Palliative Care Foundation. [Japanese] [Google Scholar]
- 12.Shiozaki M., Nakazato K. Regret and mental health in the bereaved family: action versus inaction. The Japanese Society of Social Psychology. 2010;25:211–220. [Japanese] [Google Scholar]
- 13.Sakaguchi Y., Miyashita M., Morita T., Tsuneto S., Shima Y. Complicated grief, depressive symptoms, and suicidial ideation among the bereaved whose family member died at palliative care units. Palliat Care Res. 2013;8:203–210. [Japanese] [Google Scholar]
- 14.Holly G.P., Andrew J.B., Stanislav V.K., et al. Traumatic grief as a risk factor for mental and physical morbidity. Am J Psychiatr. 1997;154:616–623. doi: 10.1176/ajp.154.5.616. [DOI] [PubMed] [Google Scholar]
- 15.Carol H.O. The impact of complicated grief on mental and physical health at various points in the bereavement process. Death Stud. 2003;27:249–272. doi: 10.1080/07481180302887. [DOI] [PubMed] [Google Scholar]
- 16.Connolly T., Reb J. Regret in cancer-related decisions. Health Psychol. 2005;24:29–34. doi: 10.1037/0278-6133.24.4.S29. [DOI] [PubMed] [Google Scholar]
- 17.Shutoh M. The Japan Hospice and Palliative Care Evaluation Study3. Seikaisya; Tokyo: 2016. A study on the factors considered important when deciding on a place of treatment and the match between the desired place of treatment and the actual place of treatment; pp. 55–59. Japan Hospice Palliative Care Foundation. [Japanese] [Google Scholar]
- 18.Zeelenberg M., Pieters R. A theory of regret regulation 1.0. J Consum Psychol. 2007;17:3–18. [Google Scholar]
- 19.Shiozaki M., Sanjo M., Yoshida S., et al. Exploratory qualitative study of regret stemming from ending terminal treatment and psychological coping among the bereaved family members of cancer patients: what does the family regret about terminal treatment choices and Why? Palliat Care Res. 2017;12:753–760. [Japanese] [Google Scholar]
- 20.Brehaut J.C., O'Connor A.M., Wood T.J., et al. Validation of a decision regret scale. Med Decis Making. 2003;23:281–292. doi: 10.1177/0272989X03256005. [DOI] [PubMed] [Google Scholar]
- 21.Jack A.C., Thomas S.I., Rebecca A.S., et al. Patients' perceptions of quality of life after treatment for early prostate cancer. J Clin Oncol. 2003;21:3777–3784. doi: 10.1200/JCO.2003.02.115. [DOI] [PubMed] [Google Scholar]
- 22.Yoshida S., Kojima M. Recognition of the condition of the patients with recurring pulmonary malignancies who decided to be admitted to palliative care units and factors influencing decision-making at the setting of palliative treatment and care. J Sch Nursing. 2006;12:59–65. Osaka Prefecture University [Japanese] [Google Scholar]
- 23.Sakai K., Tsukahara C., Iwaki N., Makino T. Factors influencing advanced cancer patient and their family decision-making about treatment place. Ishikawa J Nurs. 2011;8:41–50. [Japanese] [Google Scholar]
- 24.Sakurai C., Majima T. ‘Yure’ in decisions by families of cancer patients regarding the transition to terminal palliative care. J Cult Nurs Studies. 2013;5:20–27. [Japanese] [Google Scholar]
- 25.Shiozaki M., Hirai K., Dohke R., et al. Measuring the regret of bereaved family members regarding the decision to admit cancer patients to palliative care units. Psycho Oncol. 2008;17:926–931. doi: 10.1002/pon.1312. [DOI] [PubMed] [Google Scholar]
- 26.Kokufu H. Conflict accompanying the choice of initial treatment in breast cancer patients. Jpn J Nurs Sci. 2012;9:177–184. doi: 10.1111/j.1742-7924.2011.00200.x. [DOI] [PubMed] [Google Scholar]
- 27.Morita T., Hirai K., Sakaguchi Y., et al. Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. J Pain Symp Manag. 2004;27:492–501. doi: 10.1016/j.jpainsymman.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 28.Miyashita M., Morita T., Sato K., Tsuneto S., Shima Y. A nationwide survey of quality of end-of-life cancer care in designated cancer centers, inpatient palliative care units, and home hospices in Japan: the J-HOPE study. J Pain Symp Manag. 2015;50:38–47. doi: 10.1016/j.jpainsymman.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 29.Shay L.A., Lafata J.E. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making. 2015;35:114–131. doi: 10.1177/0272989X14551638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O'Connor A.M. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 31.Kishino M., Clare E.S., Oladayo A., Jonathan K. Family involvement in advance care planning for people living with advanced cancer: a systematic mixed-methods review. Palliat Med. 2022;36:462–477. doi: 10.1177/02692163211068282. [DOI] [PMC free article] [PubMed] [Google Scholar]