Abstract
Background and Aims
People with substance use disorders (SUDs) frequently present to treatment with polysubstance use and mental health comorbidities. Different combinations of substance use and mental health problems require different treatment approaches. Our study aimed to: (i) identify the shared substance use classes among young people at treatment admission, (ii) determine which mental health symptoms, quality of life (QoL) and service types were associated with the identified substance use classes, and (iii) prospectively determine which substance use classes and service types were more likely to complete treatment.
Design
Cross‐sectional and prospective study using service and outcome data.
Setting
Substance use treatment services in Queensland and New South Wales, Australia.
Participants
De‐identified service and outcome measure data were extracted from the files of 744 clients aged 18–35 years (48% male) admitted into seven residential and four day‐treatment programmes.
Measurements
Substance use and severity among tobacco, alcohol, cannabis, cocaine, amphetamine‐type stimulants, opioids, sedatives and inhalants. Other variables included: depression, anxiety, post‐traumatic stress and psychotic symptoms, as well as QoL.
Findings
Latent class analysis identified three polysubstance use classes: wide‐ranging polysubstance users (WRPU; 22.45%), primary amphetamine users (56.45%) and alcohol and cannabis users (21.10%). The WRPU class had higher odds of psychotic symptoms than the alcohol and cannabis use class [odds ratio (OR) = 1.30; 95% confidence interval (CI) = 1.11–1.11]; and double the odds of residential programme enrolment than those in the amphetamine use class (OR = 2.35; 95% CI = 1.50–3.68). No other class differences on mental health or QoL variables were found. Clients enrolled in day‐programmes had higher odds of completing treatment.
Conclusions
There appear to be high levels of polysubstance use among young people entering substance use treatment in Australia. Wide‐ranging polysubstance users were more likely to report psychotic symptoms and be enrolled into a residential programme than primary amphetamine users and alcohol and cannabis users.
Keywords: Comorbidity, outpatient treatment, polysubstance use, psychosis, residential treatment
INTRODUCTION
The demand for treatment of substance use disorders (SUDs) greatly outweighs the resources available world‐wide [1, 2]. Attrition rates can be higher than 50% in the first month of treatment [3, 4]; relapse rates as high as 85% have been reported following a first treatment episode [5] and treatment outcomes beyond 12 months are largely unknown [6]. Limited information is available regarding which substance use treatments or services may be most effective for different types of presentations, particularly those with polysubstance use and comorbid mental health problems [7, 8]. The objective of this study was to more clearly understand the substance use characteristics of people entering and completing substance use treatment to inform referral pathways and the development of more individualized intervention approaches.
People entering treatment services commonly report using multiple substances (polysubstance use) on the same or separate occasions [9]. Certain combinations of substances have countering effects on the central nervous system, and may be used to manage withdrawal or the sedating impacts of a substance (e.g. methamphetamines followed by opioids [10, 11]). Conversely, combining substances with similar psychoactive effects may enhance their benefits. For example, using alcohol alongside benzodiazepines augments the sedating properties of each substance [10]. Polysubstance use disorders are more difficult to treat than single SUDs, and are associated with more adverse substance use, mental health and physical health outcomes [12, 13, 14].
SUDs are highly comorbid with other mental health disorders [15, 16], particularly among polysubstance users [17]. Comorbid presentations in treatment are diverse, and most commonly include mood [18, 19], anxiety [20, 21], eating [22] and post‐traumatic stress disorders (PTSDs) [23, 24]. There is also a high prevalence of positive psychotic symptoms and schizophrenia [25, 26]. The relationship between mental health and SUDs is bidirectional [27, 28, 29, 30], and different mental health symptoms may be associated with using different clusters of substances to achieve the desired effects (e.g. for intoxication, energy or alleviating distress [31]). Substance use problems and disorders reach their peak between 18 and 25 years of age, but the average age for first receiving substance use treatment is 34 years [32, 33, 34]. Despite this, few studies have investigated the effectiveness of substance use treatment in this age group. For young people with severe and complex substance use, residential treatment is a common recovery pathway [6, 35]. Services provide live‐in treatment through structured group and individual programmes delivering psychoeducation, counselling and recovery support throughout a specified time‐period. There is limited quality of evidence for the effectiveness of residential treatment for substance use problems [6]. People who receive it tend to achieve positive outcomes, particularly if they complete treatment [6]. However, little is known about what types or length of residential treatment are most effective, or which individuals are more likely to complete treatment. Day‐services are also available, which deliver structured group programmes for a specified length of time while individuals live in their usual environment. Even less is known about the outcomes of these programmes, including which people are most likely to benefit from or complete treatment. Focusing upon day and residential modalities is important, due to many substance use programmes utilizing this structure. Furthermore, day‐programmes are increasing in popularity. However, little is known about the characteristics of people attending them, and whether their outcomes differ from residential treatment modalities.
Latent class analysis (LCA) is a person‐centred statistical approach which identifies clusters of individuals (also known as classes) that have similar patterns of substance use [36]. This approach can help to characterize heterogeneous populations such as people in treatment for SUDs. Existing research utilizing LCA has typically examined substance use classes in nationally representative general population samples [37, 38], which have limited applicability in treatment settings.
Two studies have used LCA to identify substance use classes among people in substance use treatment. A study conducted among 825 people seeking outpatient treatment for cannabis use found a wide‐ranging substance use class, a cannabis, alcohol and tobacco class and a cannabis and tobacco class [39]. A second study conducted in 493 women accessing substance use treatment services found a four‐class solution, including amphetamine polysubstance users, alcohol users, cannabis and alcohol users and other polysubstance users [40]. Both studies examined the association between the identified substance use classes and mental health outcomes. Connor et al. [39] found the wide‐ranging substance use class had more severe depression, anxiety, positive psychotic and manic symptoms than those in a cannabis, alcohol and tobacco class and more severe anxiety than the cannabis and tobacco class. Rodriguez et al. [40] found the amphetamine polysubstance use class reported higher levels of psychological distress than the alcohol‐only class at service entry. Those in the amphetamine polysubstance use class had better psychological distress and quality of life (QoL) outcomes than those in the alcohol‐only class after 60 days of treatment. Finally, a LCA study focusing on QoL outcomes among 9958 people attending various substance use services found that both substance use and psychological distress was highest in the low QoL class [41]. Together, research suggests that polysubstance users are likely to have poorer mental health and QoL outcomes more broadly, which may negatively impact the trajectory of treatment. However, these studies were conducted among treatment‐seeking samples of cannabis users [39] and women who completed routine outcomes at service entry and after 60 days within treatment [40]. Research is yet to identify substance use classes or their association with mental health symptoms, QoL or treatment completion in a large sample of young men and women receiving treatment for a broad range of substances in residential and day‐programmes.
The current study aimed to: (i) identify the substance use classes of young people (aged 18–35 years) entering residential or day‐treatment programmes for substance use; (ii) determine how mental health symptoms, QoL and service type (residential or day‐programme) are associated with these substance use classes; and (iii) prospectively determine which substance use classes and service types are more likely to complete the treatment episode. The outcomes of this study will have broad implications for treatment services.
We expect:
-
i
to identify multiple latent classes that reflect the complexity of treatment‐receiving individuals with SUDs, and
-
ii
that the presence of more severe depression, anxiety, post‐traumatic and psychotic symptoms will be associated with wider range polysubstance use classes.
Given that people who access residential treatment tend to have more severe substance use, we anticipate that:
-
iii
classes characterized by greater polysubstance use will be less likely to complete treatment.
METHOD
Procedure and setting
We obtained de‐identified routinely collected data from 744 clients aged 18–35 years [meanage = 28.30, standard deviation (SD) = 4.28] out of a total of 1671 people who were admitted into 11 treatment services for substance use between March 2020 and April 2021. Only 744 individuals aged between 18 and 35 years were included in this study. Treatment services included seven residential and four day‐programmes in Queensland and northern New South Wales, Australia. All services run 6‐week rehabilitation programmes predominantly comprised of group‐based treatment, case management, counselling support and referrals to specialist support (e.g. psychiatry). In cases of multiple admissions, the client's first admission data were included. Clients completed self‐report outcome measures upon service entry as part of the standard service entry process. Individual consent was not obtained prior to sourcing the data, as participants consent to their de‐identified data being utilized for research purposes at service entry. Treatment cessation data (treatment completion and reason for dropout) were extracted in late August 2021. Ethical approval was obtained from the University of Queensland Human Research Ethics Committee. The analysis was not pre‐registered, and our results should be considered exploratory.
Measures
Demographic and treatment information
Demographic information included age, sex, source of income, employment, reason for treatment cessation and the primary substance for which participants sought treatment. Treatment completion was defined as clients who completed a single treatment episode without involuntary or voluntary discharge from the service.
Substance use
Substance use severity was measured using the alcohol, smoking and substance involvement screening test (ASSIST [42]). This measure assessed past 3‐month frequency of use of eight different substance use types (tobacco, alcohol, cannabis, cocaine, amphetamine‐type stimulants, opioids, sedatives and inhalants). Seven additional questions evaluated the consequences of each substance used in the past 3 months. A total individual score was obtained for each substance (ranging from 0 to 39) that is then categorized by severity based on World Health Organization (WHO)‐recommended ranges [42]. For alcohol, a score of 0–10 is low risk, 11–26 moderate risk and 27+ high risk. For all other substances, 0–3 is categorized as low risk, 4–26 moderate risk and 27+ high risk. Scores were categorized as low, medium and high based on this severity for each drug and were used in a LCA (Aim 1).
Mental health symptoms and QoL
Participants completed the primary care PTSD screen for DSM‐5 (PC‐PTSD‐5; a five‐item measure for PTSD symptoms associated with experiencing a traumatic event [43]), the generalized anxiety disorder scale (GADS; a seven‐item measure of generalized anxiety during the past 2 weeks [44]), the patient health questionnaire (PHQ; a nine‐item measure of depressive symptoms during the past 2 weeks [45]), the psychosis screener (PS; a seven‐item measure of psychotic symptoms during the past 12 months [46]) and the Australian treatment outcomes profile QoL scale (a 10‐item measure of overall QoL based on physical and psychological wellbeing [47]). Total scores on all measures were used in the analyses. Higher scores indicated higher mental health symptom severity and poorer QoL. Positive psychotic symptoms are indicated by a score of three or more on the PS.
Statistical analyses
Data were analysed using Mplus [48] and Stata [49]. LCA was conducted to identify the substance use classes of people entering residential or day‐treatment programmes for substance use (Aim 1). Participants were classified into their latent subgroups based on substance use severity on the ASSIST (low, medium, high) among seven substances: tobacco, alcohol, cannabis, cocaine, amphetamine‐type stimulants, opioids and sedatives. LCA identified clusters of substance users based on the similarities of their responses on each substance use type. The analysis was performed iteratively through two‐ to six‐class models. The optimal class solution was determined based on the Akaike's information criterion (AIC), Bayesian information criterion (BIC) and sample size‐adjusted BIC (SSaBIC) compared across classes, where a lower value indicates a balance between model fit and parsimony [50, 51]. The Vuong‐Lo–Mendell–Rubin (LMR‐LRT) ratio test and adjusted ratio tests were used to evaluate the improvement of model fit between classes [52]. A significant LMR‐LRT P‐value indicates that the inclusion of one more class (k class model) fits better than a k‐1 class model [50]. Classification quality was evaluated through entropy, where values range from 0 to 1, and an entropy value closer to 1 indicates a clear separation of classes.
The association between class type, mental health, enrolment service type and QoL (Aim 2) was investigated using a multinomial logistic regression (controlling for age and sex). Substance use classes were used as the outcome variables. Mental health, enrolment service type and QoL were used as predictor variables (see Table 4). A separate logistic regression analysis investigated the association between substance use class on treatment completion (yes/no) (Aim 3). Multiple comparisons were corrected using a Bonferroni adjustment (αaltered = 0.05/24) setting the significance level at 0.00208. Missing values for mental health and QoL outcomes (m = 98) were imputed prior to the multinomial logistic regression analysis using the iterative Markov chain Monte Carlo method in Stata [53]. No other missing data were present. Class uncertainty was accounted for by using a weighted analysis with BCH (Bolck, Croon & Hagenaars) weights from each latent class [54].
TABLE 4.
Multinomial logistic regression examining the association of mental health symptoms, service type and quality of life (QoL) with substance use class membership (n = 744)
| Outcome class | Comparator class | Predictor | OR (95% CI) | SE | Z | P |
|---|---|---|---|---|---|---|
| Alcohol and cannabis use (n = 157) | Wide‐ranging polysubstance use (n = 167) | Sexa | 0.95 (0.60–1.51) | 0.23 | −0.21 | 0.830 |
| Age | 0.98 (0.93–1.51) | 0.03 | −0.60 | 0.550 | ||
| Service typeb | 1.33 (0.77–1.04) | 0.28 | 1.02 | 0.307 | ||
| QoL | 0.96 (0.87–2.28) | 0.05 | −0.89 | 0.374 | ||
| Depression | 0.98 (0.93–1.05) | 0.03 | −0.79 | 0.431 | ||
| Anxiety | 1.04 (0.98–1.03) | 0.03 | 1.41 | 0.158 | ||
| Psychosis | 1.30 (1.11–1.11) | 0.08 | 3.28 | 0.001* | ||
| PTSD | 1.10 (0.98–1.52) | 0.06 | 1.69 | 0.092 | ||
| Amphetamine use (n = 420) | Wide‐ranging polysubstance use (n = 167) | Sexa | 1.81 (1.22–2.67) | 0.20 | 2.97 | 0.003 |
| Age | 0.96 (0.92–1.00) | 0.02 | −1.93 | 0.054 | ||
| Service typeb | 2.35 (1.50–3.68) | 0.23 | 3.72 | 0.000* | ||
| QoL | 0.96 (0.89–1.04) | 0.04 | −0.94 | 0.349 | ||
| Depression | 1.03 (0.98–1.08) | 0.02 | 1.24 | 0.214 | ||
| Anxiety | 1.04 (0.99–1.10) | 0.03 | 1.68 | 0.093 | ||
| Psychosis | 1.07 (0.95–1.21) | 0.06 | 1.09 | 0.275 | ||
| PTSD | 1.09 (0.99–1.20) | 0.05 | 1.68 | 0.092 | ||
| Alcohol and cannabis use (n = 157) | Amphetamine use (n = 420) | Sexa | 0.53 (0.36–0.78) | 0.20 | −3.23 | 0.001* |
| Age | 1.03 (0.98–1.07) | 0.02 | 1.23 | 0.219 | ||
| Service typeb | 0.56 (0.37–0.86) | 0.22 | −2.65 | 0.008 | ||
| QoL | 0.99 (0.92–1.08) | 0.04 | −0.12 | 0.904 | ||
| Depression | 0.95 (0.91–1.00) | 0.02 | −2.15 | 0.031 | ||
| Anxiety | 1.00 (0.95–1.05) | 0.03 | 0.00 | 0.999 | ||
| Psychosis | 1.21 (1.05–1.40) | 0.07 | 2.7 | 0.007 | ||
| PTSD | 1.01 (0.92–1.12) | 0.05 | 0.29 | 0.773 |
CI, confidence interval; OR, odds ratio; PTSD, post‐traumatic stress syndrome; SE, standard error.
*P < 0.002. Reference categories were malesa for sex and bresidential enrolments for service type. OR = odds ratio; CI = confidence interval; SE = standard error; PTSD = post‐traumatic stress syndrome.
RESULTS
Client characteristics
Information on demographic, mental health, QoL and primary substance use variables is presented in Table 1. Clients (n = 744) were primarily admitted to a residential treatment service (n = 519), and 321 clients (43.10%) completed treatment. Information on the sex, age and primary substance type of all clients admitted to the services during the study time‐frame is provided in Supporting information, SS2. There were differences in age, but no differences in sex between the sample used for the analysis and all clients admitted into the service.
TABLE 1.
Demographic, mental health, quality of life (QoL) and primary substance type for the current treatment episode of people attending residential and day substance use treatment services aged 18–35 years
| Demographic factors | |||
|---|---|---|---|
| Characteristic | Total sample (n = 744) | Residential programme (n = 519) | Day programme (n = 225) |
| Age, mean (SD) | 28.3 (4.28) | 28.15 (4.29) | 28.65 (4.23) |
| Sex, n (%) | |||
| Male | 354 (48) | 242 (47) | 112 (50) |
| Female | 390 (53) | 277 (53) | 113 (50) |
| Income source (%) | |||
| Full‐time employment | 34 (5) | 12 (2.3) | 22 (10) |
| Part‐time employment | 28 (4) | 15 (3) | 13 (6) |
| Unemployment benefit | 527 (71) | 387 (75) | 140 (62) |
| Pension (aged, disability) | 72 (10) | 49 (9) | 23 (10) |
| No income | 14 (2) | 14 (3) | |
| Other/not stated | 69 (9) | 42(8) | 24 (10) |
| Treatment completion (%) | 321 (43) | 209 (40) | 112 (50) |
| Substance use | |||
|---|---|---|---|
| Primary drug type, a n (%) | |||
| Amphetamine‐type stimulants (methamphetamine, MDMA, amphetamines) | 389 (52) | 262 (51) | 127 (57) |
| Methamphetamine | 375 (50) | 254 (49) | 121 (54) |
| Amphetamines (including speed) | 10 (2) | 6 (1) | |
| Alcohol | 194 (26) | 153 (30) | 42 (19) |
| Cannabinoids | 89 (12) | 55 (11) | 34 (15) |
| Heroin | 12 (2) | 10 (2) | |
| Opioids (buprenorphine, fentanyl, morphine, oxycodone) | 10 (2) () | 10 (2) | |
| Benzodiazepines | 16 (2) | 12 (2) | |
| Gamma‐hydroxybutyric acid | 8 (1) | 6 (1) | |
| Cocaine | 8 (1) | ||
| Other | 18 (2) | 7 (1) | 10 (4) |
| Injecting drug use (n) | |||
| Life‐time | 129 | 85 | 44 |
| Past 3 months | 243 | 170 | 73 |
| Mental health, QoL, mean (SD) | |||
|---|---|---|---|
| Depression | 13.85 (7.13) | 14.12 (7.31) | 13.29 (7.16) |
| Anxiety | 11.39 (6.32) | 11.66 (6.42) | 10.62 (6.04) |
| PTSD | 2.46 (2.16) | 2.44 (2.15) | 2.50 (2.17) |
| Positive screen b n (%) | 325 (43.68) | 222 (42.77) | 103 (45.77) |
| Psychosis | 1.44 (1.57) | 1.46 (1.56) | 1.39 (1.59) |
| Positive screen c n (%) | 97 (13.03) | 69 (13.29) | 28 (12.44) |
| QoL | 5.06 (2.94) | 4.39 (2.98) | 4.59 (2.82) |
Blank cells are estimates fewer than five people and were removed to maintain patient confidentiality.
As indicated by asking clients for the substance they are seeking treatment for during the current treatment episode;
as indicated by a score of three or more on the primary care post‐traumatic stress disorder (PC‐PTSD)‐5 and
three or more on the psychosis screener.
Primary reasons for treatment cessation included: non‐compliance (e.g. displays of aggression; n = 97), treatment cessation against formal advice (n = 65) and leaving without notice (n = 53). The mean anxiety and depression scores were above moderate to severe clinical cut‐offs [55, 56]; 43.68% of people screened positively for PTSD on the PC‐PTSD‐5 and 13% screened positively on the PS.
Aim 1: LCA of substance use classes
Model fit statistics for each class are presented in Table 2. The three‐class solution produced the lowest BIC. Based on LMR‐LRT values, the four‐class model did not fit the data better than the three‐class model and the three‐class model did not fit the data better than the two‐class model. The six‐class solution produced the lowest AIC and SSaBIC. Fit statistics varied considerably for the five‐ and six‐class solutions, were very close for the four‐ to six‐class solutions and the LMR tests indicated improvements with each increase in class. Additions in class did not indicate an improved model fit, and each increase in class size separated the substances into more distinct categories through isolating substances, which was inconsistent with our research aims to investigate shared substance use classes. Therefore, the classes were examined based on interpretability [48]. The three‐class solution was selected as the optimal solution, as it yielded clear classification between substance groups which was more parsimonious, interpretable and provided adequate class sizes.
TABLE 2.
Model fit indices of two to six classes
| Classes | AIC | SSaBIC | BIC | LMR test | LMR P‐value | Adjusted LMR | Adjusted LMR P‐value | BLRT | BLRT P‐value | Entropy |
|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 9224.536 | 9271.947 | 9376.734 | −4835.165 | 0.000 | 507.280 | 0.000 | −4835.165 | 0.000 | 0.803 |
| 3 | 9134.907 | 9206.741 | 9365.510 | −4579.27 | 0.114 | 122.539 | 0.116 | −4579.268 | 0.000 | 0.712 |
| 4 | 9057.030 | 9153.287 | 9366.037 | −4517.45 | 0.166 | 110.891 | 0.168 | −4517.454 | 0.000 | 0.708 |
| 5 | 9029.867 | 9150.547 | 9417.278 | −4461.52 | 1.000 | 60.624 | 1.000 | −4461.515 | 0.000 | 0.706 |
| 6 | 9001.382 | 9146.486 | 9467.198 | −4430.93 | 0.977 | 61.934 | 0.978 | −4430.933 | 0.000 | 0.782 |
AIC, Akaike information criterion; BIC, Bayesian information criterion; BLRT, bootstrap likelihood ratio test; LMR, Vuong‐Lo–Mendell–Rubin ratio test; SSaBIC, sample‐size‐adjusted BIC.
Figure 1 shows the probability of substance use for each class. Class 1 was characterized by wide‐ranging substance use (WRPU) across all categories except cocaine, with high engagement with alcohol, amphetamine and cannabis and moderate engagement with sedatives and opioids, with a prevalence estimate of 167 (22.45%). Class 2 was characterized by high amphetamine use, moderate tobacco and cannabis use and low involvement across all other substance use categories (primary amphetamine use class). The prevalence estimate for this class was 420 (56.45%). Class 3 was characterized by using predominantly alcohol, followed by cannabis and tobacco and no involvement with other substances (alcohol and cannabis use class). The prevalence estimate for this class was 157 (21.10%). All classes engaged in tobacco use, with the WRPU having the greatest engagement.
FIGURE 1.
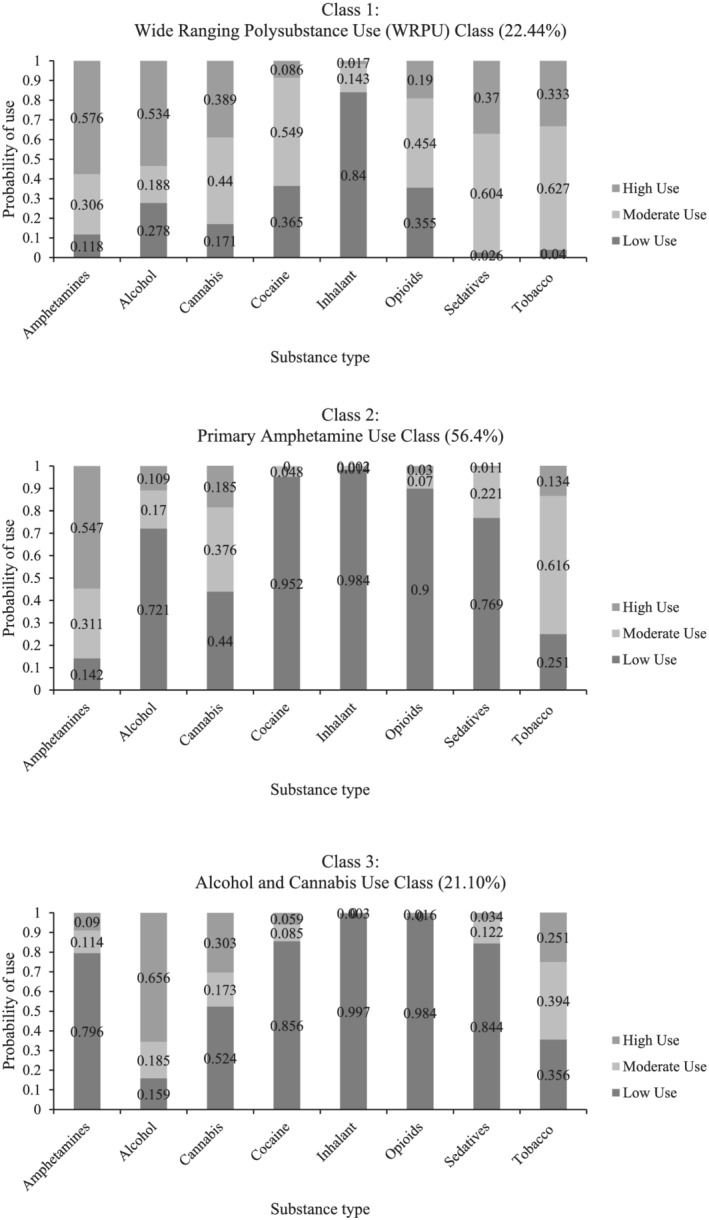
Probability of substance involvement by class from the three‐class solution. Class 1 had high engagement with most drug types. Class 2 was characterized by predominant amphetamine use and class 3 used mainly alcohol and cannabis
Aim 2: Association between substance use class, mental health symptoms, QoL and service enrolment type
Class differences on demographics, mental health variables, program enrolment and completion are reported in Table 3.
TABLE 3.
Class differences in sex, age, service enrolment type, treatment completion, mental health symptoms and quality of life (QoL)
| Variable | Class 1: WRPU (n = 167) | Class 2: Primary amphetamine users (n = 420) | Class 3: Alcohol and cannabis users (n = 157) |
|---|---|---|---|
| Demographics | |||
| Sex, n % male | 87 (52.09) | 178 (42.38) | 90 (57.32) |
| Age (mean, SD) | 27.67 (4.59) | 28.58 (3.94) | 28.19 (4.72) |
| Residential programme (n, % residential) | 135 (80.83) | 266 (63.33) | 119 (75.79) |
| Day programme treatment completion (n, %) | 14 (43.75) | 75 (48.70) | 23 (60.52) |
| Residential treatment completion (n, %) | 55 (40.74) | 102 (38.35) | 52 (43.69) |
| Mental health (mean, SD) | |||
| Depression | 16.68 (6.87) | 12.48 (7.22) | 14.46 (7.06) |
| Anxiety | 14.08 (5.83) | 10.29 (6.37) | 11.49 (5.91) |
| Experienced or witnessed a traumatic event (n, %) | 128 (76.64) | 284 (43.80) | 102 (64.96) |
| PTSD | 3.96 (1.46) | 3.46 (1.72) | 3.43 (1.69) |
| Psychosis | 1.85 (1.61) | 1.38 (1.61) | 1.07 (1.32) |
| QoL | 3.56 (2.64) | 4.96 (3.01) | 4.47 (2.80) |
PTSD, post‐traumatic stress syndrome; SD, standard deviation; WRPU, wide ranging polysubstance users.
We conducted multinomial logistic regressions with simultaneous entry to examine whether the severity of mental health symptoms, QoL and enrolment service type of clients was associated with substance use class membership (Table 4).
Males had lower odds of belonging to the amphetamine use class [odds ratio (OR) = 0.53, P = 0.001; 95% confidence interval (CI) = 0.36–0.78] compared to the alcohol and cannabis use class. Attending a residential programme was associated with a significant increase in the odds of belonging to the WRPU class (OR = 2.35, P < 0.001; 95% CI = 1.50–3.68) compared to the amphetamine use class. Individuals with a higher psychosis score were more likely to belong to the WRPU class (OR = 1.30, P = 0.001; 95% CI = 1.11–1.11) than the alcohol and cannabis class.
Aim 3: Association between substance use class and treatment completion
A separate multinomial logistic regression analysis investigated whether substance use class prospectively predicted treatment completion (Aim 3). Substance use class was not a significant predictor of treatment completion (the Results Table is presented in Supporting information, SS1).
DISCUSSION
The first aim of this study was to identify the substance use classes of young people entering substance use treatment services. LCA identified a three‐class solution: (i) a WRPU class that had high past‐3‐month use among most substance types, characterized by severe alcohol and amphetamine use, in addition to elevated cannabis and opioid use, (ii) a primary‐amphetamine use class, representing more than half of the sample, characterized predominantly by amphetamine use alongside low‐level use of cannabis and alcohol and (iii) a cannabis and alcohol use class, the least prevalent in the sample, characterized by high alcohol and cannabis use and moderate tobacco use.
While LCA findings are difficult to compare, our identified classes are similar to a study conducted in women accessing substance treatment services which found a four‐class solution, including amphetamine polysubstance users, an alcohol‐only class, a cannabis and alcohol class and other polysubstance users [40]. Epidemiological studies utilizing LCA have also found three class solutions that include wide‐ranging substance users (including polysubstance use involving legal and illegal substances), amphetamine‐only users and a class characterized by more commonly used substances (e.g. alcohol, tobacco and cannabis use [10, 37]).
The second aim examined the association between substance use class, mental health symptoms, QoL and service type. The WRPU class had 1.3 times the odds of experiencing psychotic symptoms than the alcohol and cannabis class. No other significant differences in the mental health symptoms or QoL were found across classes. This is partially consistent with our hypothesis, based on previous research in treatment‐specific settings, that the WRPU class would display more severe depression, anxiety, PTSD and psychotic symptoms [39, 40]. Connor et al. [39] also found that wide‐ranging substance users were more likely to have positive psychotic symptoms than a cannabis, alcohol and tobacco class. However, previous research used different measures of depression and anxiety symptoms (e.g. Kessler [10], general health questionnaire) and did not include a measure of PTSD symptoms. Moreover, all classes in our study showed above moderate mental health symptoms, suggesting that further research is needed among treatment‐receiving groups of substance users, as comorbidity of SUD and mental health problems occurred throughout all classes.
The WRPU class engaged in severe amphetamine use in addition to cannabis, alcohol and opioid use. The dose–response relationship between psychotic symptoms and disorders in amphetamine and cannabis use is well established [57, 58]. Amphetamine use alone or in combination with cannabis may increase the risk of psychotic symptoms [29]. However, the primary‐amphetamine use class (with moderate cannabis use) did not report more psychotic symptoms than either the WRPU or alcohol and cannabis class. This suggests that the sheer magnitude of polysubstance use in the WRPU class may have increased the risk of psychotic symptoms, rather than the effects of a specific substance. Polysubstance use could therefore also be a marker of increased vulnerability to psychopathology overall. Alternatively, polysubstance users may use multiple or different combinations of substances to self‐regulate mental health symptoms, reduce withdrawal symptoms or enhance the effects of a certain substance [27, 28, 59].
Regarding gender‐specific differences, males had lower odds of belonging to the alcohol and cannabis class than the class of primary‐amphetamine use, and approached significance compared to the WRPU class. This may reflect the higher rates of life‐time and past 12‐month amphetamine use found in males compared to females in the general population [60].
As anticipated, people attending a residential programme had double the odds of belonging to the WRPU class compared to the amphetamine use class. This probably reflects the need for more intensive treatment in the WRPU group, due to the primacy of their wide‐ranging use. Patients characterized by polysubstance use in outpatient settings report the least self‐efficacy to maintain abstinence [14]. Previous research suggests that better substance use outcomes are achieved in residential settings providing integrated treatment for mental health comorbidities [61, 62]. On a service level, the WRPU class highlights the need to assess for and target the multiple morbidities that people present with using high‐intensity, integrated treatment [9, 10, 63]; for example, by including specialist‐delivered interventions for a specific disorder (e.g. psychosis), as well as more broad, organizational approaches that facilitate recovery across multiple psychosocial domains. However, it is also important to consider that the prevalence of WRPU was small (22%).
Our final aim was to prospectively determine which substance use classes are more likely to complete treatment. Contrary to predictions, substance use class type did not predict treatment completion. Treatment completion is a known predictor of substance use recovery [64, 65], especially in residential treatment settings [6]. Completion rates below 50% were observed in our sample, regardless of whether the client was enrolled in a residential or day‐treatment programme. This is consistent with previous research conducted among various substance use treatment settings, where treatment dropout rates have ranged from 40 to 59% [66, 67, 68]. Such retention rates highlight the need to continue refining treatment services to improve retention. As 18–35 years is a critical point of substance use intervention, focusing upon treatment retention in young people specifically is important for substance use prevention strategies. While some individuals may require lengthier and more intensive treatment, integrated and individualized treatment methods are also required more broadly to provide a solution to the treatment attrition rates observed in this and other studies. Currently, treatment provided by alcohol and other drug (AOD) services predominantly consists of counselling or assessment and education, which falls outside the evidence base for effectively treating comorbidities through evidence‐based programmes such as cognitive behaviour therapy (CBT) (e.g. [69, 70]). Furthermore, previous research has shown that early attrition from substance use treatment is associated with the perceived importance of addressing emotional or psychological problems over problematic substance use [71]. This suggests that addressing mental health problems early in a client's admission may increase motivation to remain in substance use treatment.
Our study had several strengths and limitations. To the best of our knowledge, this is the first study that investigated substance use classes and their mental health associates among young people who are accessing residential and day‐treatment. The study included a large sample of young people admitted to treatment for a broad range of substance use problems and used a comprehensive set of mental health measures. The age, sex and primary substance type of participants are consistent with national residential treatment data showing that 66% of clients are male, 61% are aged between 20 and 39 years and amphetamines, alcohol and cannabis are the most common substances for which people seek help [4]. This suggests that current findings are generalizable to young people aged 18–35 years accessing residential treatment programmes in Australia. However, the generalizability of results to day‐programmes is unknown, as very little is known about the characteristics of people seeking this type of treatment. While the impact of class membership upon treatment completion was examined, we were unable to investigate whether class membership predicted treatment outcomes. However, the structure and content of the treatment programme delivered across and within the seven residential and four day substance‐use services included in this study probably varied, and our results should be interpreted with caution due to small sample sizes in some services. Investigating treatment completion within services delivering more consistent treatment programmes would have provided more insights into which substance use classes were more likely to complete treatment. Our definition of treatment completion was limited by the data collected and may not reflect the client completing a full treatment programme or recovering fully from substance use. Longitudinal outcomes are warranted to further understanding treatment types and recovery.
CONCLUSIONS
Our study sheds light on the high levels of polysubstance use and co‐occurring mental health problems among young people entering substance use treatment. People with wide‐ranging polysubstance use may be more likely to experience additional clinical complexities than single substance users, including psychosis. Future research is required to increase the understanding of the patterns of polysubstance use and comorbid mental health problems that young people present with in treatment; and develop more integrated treatments targeted toward the multiple morbidities this population experiences.
DECLARATION OF INTERESTS
None to declare.
AUTHOR CONTRIBUTIONS
Valeriya Mefodeva: Conceptualization; data curation; formal analysis. Molly Carlyle: Formal analysis; methodology; supervision; validation. Zoe Walter: Validation. Gary Chan: Methodology; software; supervision. Leanne Hides: Conceptualization; methodology; resources; supervision.
Supporting information
Data S1. Data proving de identified demographic information per each residential and day program (service types) included in the study.
Data S2. Demographic information of people attending residential and day services outside the age range specified for the study.
Data S3. Table for Aim three of this study examining the association of treatment completion (predictor) on substance use class membership (N = 744).
ACKNOWLEDGEMENTS
This study was funded by the Australian Government Department of Health awarded to the National Centre for Youth Substance Use Research (NCYSUR) under the Drug and Alcohol Prevention Program. L.H. is supported by a National Health and Medical Research Council Senior Research Fellowship. The funding source had no involvement in the study design, collection, analysis and interpretation of data, or writing of the report. Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians. Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
Mefodeva V, Carlyle M, Walter Z, Chan G, Hides L. Polysubstance use in young people accessing residential and day‐treatment services for substance use: substance use profiles, psychiatric comorbidity and treatment completion. Addiction. 2022;117(12):3110–3120. 10.1111/add.16008
Funding information None.
REFERENCES
- 1. Ritter A, Chalmers J, Gomez M. Measuring unmet demand for alcohol and other drug treatment: The application of an Australian population‐based planning model. J Stud Alcohol Drugs. 2019;18:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Degenhardt L, Glantz M, Evans‐Lacko S, Sadikova E, Sampson N, Thornicroft G, et al. Estimating treatment coverage for people with substance use disorders: an analysis of data from the world mental health surveys. World Psychiatry. 2017;16:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Basu D, Ghosh A, Sarkar S, Patra BN, Subodh B, Mattoo SK. Initial treatment dropout in patients with substance use disorders attending a tertiary care de‐addiction Centre in North India. Indian J Med Res. 2017;146:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Australian Institute of Health and Welfare (AIHW) . Alcohol and Other Drug Treatment Services in Australia Annual Report Canberra, Australia: AIHW; 2021. [Google Scholar]
- 5. Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Annu Rev Clin Psychol. 2007;3:257–84. [DOI] [PubMed] [Google Scholar]
- 6. de Andrade D, Elphinston RA, Quinn C, Allan J, Hides L. The effectiveness of residential treatment services for individuals with substance use disorders: a systematic review. Drug Alcohol Depend. 2019;201:227–35. [DOI] [PubMed] [Google Scholar]
- 7. Manning V, Garfield JBB, Best D, Berends L, Room R, Mugavin J, et al. Substance use outcomes following treatment: findings from the Australian patient pathways study. Aust NZ J Psychiatry. 2016;51:177–89. [DOI] [PubMed] [Google Scholar]
- 8. Kingston RE, Marel C, Mills KL. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug Alcohol Rev. 2017;36:527–39. [DOI] [PubMed] [Google Scholar]
- 9. Crummy EA, O'Neal TJ, Baskin BM, Ferguson SM. One is not enough: understanding and modeling polysubstance use. Front Neurosci. 2020;14:569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Connor JP, Gullo MJ, White A, Kelly AB. Polysubstance use: diagnostic challenges, patterns of use and health. Curr Opin Psychiatry. 2014;27:269–75. [DOI] [PubMed] [Google Scholar]
- 11. Trujillo KA, Smith ML, Guaderrama MM. Powerful behavioral interactions between methamphetamine and morphine. Pharmacol Biochem Behav. 2011;99:451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang L, Min JE, Krebs E, Evans E, Huang D, Liu L, et al. Polydrug use and its association with drug treatment outcomes among primary heroin, methamphetamine, and cocaine users. Int J Drug Policy. 2017;49:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gjersing L, Bretteville‐Jensen AL. Patterns of substance use and mortality risk in a cohort of ‘hard‐to‐reach’ polysubstance users. Addiction. 2018;113:729–39. [DOI] [PubMed] [Google Scholar]
- 14. Timko C, Ilgen M, Haverfield M, Shelley A, Breland JY. Polysubstance use by psychiatry inpatients with co‐occurring mental health and substance use disorders. Drug Alcohol Depend. 2017;180:319–22. [DOI] [PubMed] [Google Scholar]
- 15. Kranzler HR, Rounsaville BJ. Dual Diagnosis and Treatment: Substance Abuse and Comorbid Medical and Psychiatric Disorders New York, MY: Marcel Dekker Inc.; 1998. [Google Scholar]
- 16. Couwenbergh C, van den Brink W, Zwart K, Vreugdenhil C, van Wijngaarden‐Cremers P, van der Gaag RJ. Comorbid psychopathology in adolescents and young adults treated for substance use disorders. Eur Child Adolesc Psychiatry. 2006;15:319–28. [DOI] [PubMed] [Google Scholar]
- 17. Erfan S, Hashim AH, Shaheen M, Sabry N. Effect of comorbid depression on substance use disorders. Subst Abuse. 2010;31:162–9. [DOI] [PubMed] [Google Scholar]
- 18. Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar‐Gaziola S, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the international consortium in psychiatric epidemiology. Addict Behav. 1998;23:893–907. [DOI] [PubMed] [Google Scholar]
- 19. Quello SB, Brady KT, Sonne SC. Mood disorders and substance use disorder: a complex comorbidity. Sci Pract Perspect. 2005;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res. 2008;42:230–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co‐occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:807–16. [DOI] [PubMed] [Google Scholar]
- 22. Holderness CC, Brooks‐Gunn J, Warren MP. Co‐morbidity of eating disorders and substance abuse review of the literature. Int J Eat Disord. 1994;16:1–34. [DOI] [PubMed] [Google Scholar]
- 23. Chilcoat HD, Menard C. Epidemiological Investigations: Comorbidity of Posttraumatic Stress Disorder and Substance Use Disorder. In: Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders Washington, DC: American Psychological Association; 2003. p. 9–28. [Google Scholar]
- 24. Stewart SH, Conrod PJ. Psychosocial models of functional associations between posttraumatic stress disorder and substance use disorder. In: Ouimette P, Brown PJ, editorsTrauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders Washington, DC: American Psychological Association; 2003. p. 29–55. [Google Scholar]
- 25. Helseth V, Samet S, Johnsen J, Bramness JG, Waal H. Independent or substance‐induced mental disorders? An investigation of comorbidity in an acute psychiatric unit. J Dual Diagn. 2013;9:78–86. [Google Scholar]
- 26. Andersson HW, Lilleeng SE, Ruud T, Ose SO. Substance use among patients in specialized mental health services in Norway: prevalence and patient characteristics based on a national census. Nord J Psychiatry. 2021;75:160–9. [DOI] [PubMed] [Google Scholar]
- 27. Sharkansky EJ, Brief DJ, Peirce JM, Meehan JC, Mannix LM. Substance abuse patients with posttraumatic stress disorder (PTSD): identifying specific triggers of substance use and their associations with PTSD symptoms. Psychol Addict Behav. 1999;13:89. [Google Scholar]
- 28. Khantzian EJ. The self‐medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4:231–44. [DOI] [PubMed] [Google Scholar]
- 29. Hides L, Chan G, Dawe S, McKetin R, Kavanagh DJ, Young RM, et al. Direction of the relationship between methamphetamine use and positive psychotic symptoms in regular methamphetamine users: evidence from a prospective cohort study. Br J Psychiatry. 2021;219:361–7. [DOI] [PubMed] [Google Scholar]
- 30. Hides L, Dawe S, Kavanagh D, Young RM. Psychotic symptom and cannabis relapse in recent‐onset psychosis prospective study. Br J Psychiatry. 2006;189:137–43. [DOI] [PubMed] [Google Scholar]
- 31. Boys A, Marsden J, Strang J. Understanding reasons for drug use amongst young people: a functional perspective. Health Educ Res. 2001;16:457–69. [DOI] [PubMed] [Google Scholar]
- 32. Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav. 2012;37:747–75. [DOI] [PubMed] [Google Scholar]
- 33. National Institute on Alcohol Abuse and Alcoholism (NIAAA) . Young adult drinking. Alcohol alert. Rockville, MD: NIAAA; 2006.
- 34. Substance Abuse and Mental Health Services Administration . Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H‐41, HHS Publication No. (SMA) 11–4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011, p. 201.
- 35. Reif S, George P, Braude L, Dougherty RH, Daniels AS, Ghose SS, et al. Residential treatment for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. 2014;65:301–12. [DOI] [PubMed] [Google Scholar]
- 36. Vermunt JK, Magidson J. Latent class analysis. Sage Encycl Soc Sci Res Methods. 2004;2:549–53. [Google Scholar]
- 37. Chan G, Connor J, Hall W, Leung J. The changing patterns and correlates of population‐level polysubstance use in Australian youth: a multi‐group latent class analysis of nationally representative samples spanning 12 years. Addiction. 2020;115:145–55. [DOI] [PubMed] [Google Scholar]
- 38. Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on alcohol and related conditions. Addiction. 2007;102:94–104. [DOI] [PubMed] [Google Scholar]
- 39. Connor J, Gullo M, Chan G, Young R, Hall W, Feeney G. Polysubstance use in cannabis users referred for treatment: drug use profiles, psychiatric comorbidity and cannabis‐related beliefs. Front Psychol. 2013;4:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rodriguez AS, Robinson LD, Kelly PJ, Hudson S. Polysubstance use classes and health outcomes among women attending specialist substance use treatment services. Drug Alcohol Rev. 2022;41:488–500. [DOI] [PubMed] [Google Scholar]
- 41. Kelly PJ, Robinson LD, Baker AL, Deane FP, Osborne B, Hudson S, et al. Quality of life of individuals seeking treatment at specialist non‐government alcohol and other drug treatment services: a latent class analysis. J Subst Abuse Treat. 2018;94:47–54. [DOI] [PubMed] [Google Scholar]
- 42. Henry‐Edwards S, Humeniuk R, Ali R, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Guidelines for Use in Primary Care Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 43. Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins‐Guarnieri MA, et al. The primary care PTSD screen for DSM‐5 (PC‐PTSD‐5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31:1206–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med. 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- 45. Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Degenhardt L, Hall W. The association between psychosis and problematical drug use among Australian adults: findings from the National Survey of Mental Health and Well‐being. Psychol Med. 2001;31:659–68. [DOI] [PubMed] [Google Scholar]
- 47. Ryan A, Holmes J, Hunt V, Dunlop A, Mammen K, Holland R, et al. Validation and implementation of the Australian treatment outcomes profile in specialist drug and alcohol settings. Drug Alcohol Rev. 2014;33:33–42. [DOI] [PubMed] [Google Scholar]
- 48. Muthén L, Muthén B. Mplus. Statistical analysis with latent variables. User's guide. Los Angeles, CA: Muthén L, Muthén B; 2009, p. 7. [Google Scholar]
- 49. IBM Corporation . IBM SPSS Statistics for Windows (version 25.0 Armonk). Armonk, NY: IBM Corp; 2017. [Google Scholar]
- 50. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model Multidiscip J. 2007;14:535–69. [Google Scholar]
- 51. Bozdogan H. Model selection and Akaike's information criterion (AIC): the general theory and its analytical extensions. Psychometrika. 1987;52:345–70. [Google Scholar]
- 52. Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–78. [Google Scholar]
- 53. Gilks WR, Richardson S, Spiegelhalter D. Markov Chain Monte Carlo in Practice New York, NY: Chapman and Hall/CRC Press; 1995. [Google Scholar]
- 54. Vermunt JK. Latent class modeling with covariates: two improved three‐step approaches. Polit Anal. 2010;18:450–69. [Google Scholar]
- 55. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med. 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- 56. Kroenke K, Spitzer RL, Williams JBW. The PHQ‐9. J Gen Intern Med. 2001;16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Paparelli A, Di Forti M, Morrison PD, Murray RM. Drug‐induced psychosis: how to avoid star gazing in schizophrenia research by looking at more obvious sources of light. Front Behav Neurosci. 2011;5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bramness JG, Gundersen ØH, Guterstam J, Rognli EB, Konstenius M, Løberg E‐M, et al. Amphetamine‐induced psychosis—a separate diagnostic entity or primary psychosis triggered in the vulnerable? BMC Psychiatry. 2012;12:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ullman SE, Relyea M, Peter‐Hagene L, Vasquez AL. Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addict Behav. 2013;38:2219–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Australian Institute of Health and Welfare (AIHW) . National Drug Strategy Household Survey 2019 Canberra, Australia: AIHW; 2020. [Google Scholar]
- 61. Schoenthaler SJ, Blum K, Fried L, Oscar‐Berman M, Giordano J, Modestino EJ, et al. The effects of residential dual diagnosis treatment on alcohol abuse. J Syst Integr Neurosci. 2017;3. 10.15761/JSIN.1000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Daughters SB, Magidson JF, Anand D, Seitz‐Brown CJ, Chen Y, Baker S. The effect of a behavioral activation treatment for substance use on post‐treatment abstinence: a randomized controlled trial. Addiction. 2018;113:535–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Solmi F, Mohammadi A, Perez JA, Hameed Y, Jones PB, Kirkbride JB. Predictors of disengagement from early intervention in psychosis services. Br J Psychiatry. 2018;213:477–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Onken LS, Blaine JD, Boren JJ. Treatment for drug addiction: it won't work if they don't receive it. NIDA Res Monogr. 1997;165:1–3. [PubMed] [Google Scholar]
- 65. Hubbard RL, Marsden ME, Rachal J, Harwood HJ, Cavanaugh ER, Ginzburg HM. Drug abuse treatment: a national study of effectiveness Chapel Hill, NC, University of North Carolina Press; 1989. [Google Scholar]
- 66. Myers B, Williams PP, Govender R, Manderscheid R, Koch JR. Substance abuse treatment engagement, completion and short‐term outcomes in the Western cape province, South Africa: findings from the service quality measures initiative. Drug Alcohol Depend. 2018;185:278–84. [DOI] [PubMed] [Google Scholar]
- 67. Kamp F, Proebstl L, Hager L, Schreiber A, Riebschläger M, Neumann S, et al. Effectiveness of methamphetamine abuse treatment: predictors of treatment completion and comparison of two residential treatment programs. Drug Alcohol Depend. 2019;201:8–15. [DOI] [PubMed] [Google Scholar]
- 68. Harley M, Pit SW, Rees T, Thomas S. Completion rates and psychosocial intervention effectiveness in an Australian substance use therapeutic community. Subst Abuse Treat Prev Policy. 2018;13:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Marcel C, Mills K, Teesson M. Guidelines on the management of co‐occurring alcohol and other drug and mental health conditions in alcohol and other drug treatment settings. Section B6. Managing and treating specific disorders 2018. Available at: https://comorbidityguidelines.org.au/guidelines/. Accessed 15 August 2021.
- 70. Marel C, Mills KL, Kingston R, Gournay K, Deady M, Kay‐Lambkin F et al. Co‐occurring alcohol and other drug and mental health conditions in alcohol and other drug treatment settings: Illustrations. Sydney, Australia: National Drug and Alcohol Research Centre; 2016.
- 71. Resko SM, Mendoza NS. Early attrition from treatment among women with cooccurring substance use disorders and PTSD. J Soc Work Pract Addict. 2012;12:348–69. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Data proving de identified demographic information per each residential and day program (service types) included in the study.
Data S2. Demographic information of people attending residential and day services outside the age range specified for the study.
Data S3. Table for Aim three of this study examining the association of treatment completion (predictor) on substance use class membership (N = 744).


