ABSTRACT
Objective
To investigate the diagnostic yield of clinical whole‐genome sequencing (WGS) in prenatally diagnosed non‐immune hydrops fetalis (NIHF).
Methods
This was a retrospective study of 23 fetuses with prenatally diagnosed NIHF, negative for trisomies and copy‐number variants, referred for analysis by WGS with an in‐silico panel of 281 genes associated with hydrops fetalis. Due to identification of a high proportion of causative variants in the HRAS gene in the main cohort, Sanger sequencing of HRAS was performed in a replication cohort, consisting of 24 additional fetuses with NIHF that were negative for trisomies and copy‐number variants and had not undergone WGS.
Results
Of the 23 fetuses in the main cohort, a molecular diagnosis was achieved in 12 (52.2%). Pathogenic or likely pathogenic variants were identified in seven genes: HRAS (n = 5), RIT1 (n = 2), FOXP3 (n = 1), GLB1 (n = 1), MAP2K1 (n = 1), PTPN11 (n = 1) and RASA1 (n = 1). The inheritance pattern of the 12 causative variants was autosomal dominant in 10 cases (HRAS, MAP2K1, PTPN11, RASA1, RIT1), autosomal recessive in one (GLB1) and X‐linked recessive in one (FOXP3). Of the 24 fetuses in the replication cohort, a pathogenic variant in HRAS was identified in one, resulting in an overall frequency of causative HRAS variants of 12.8% (6/47) in our two cohorts.
Conclusions
We demonstrate a diagnostic yield of 52% with clinical WGS in NIHF using an in‐silico panel of 281 genes. However, the high diagnostic yield may be attributed to the small sample size and possible over‐representation of severe phenotypes in the included fetuses. Bearing in mind that chromosomal abnormalities were excluded in our cohorts, a detection rate of up to 75% is possible in prenatally diagnosed NIHF when WGS analysis includes calling of chromosomal aberrations. © 2022 The Authors. Ultrasound in Obstetrics & Gynecology published by John Wiley & Sons Ltd on behalf of International Society of Ultrasound in Obstetrics and Gynecology.
Keywords: Costello syndrome, fetus, HRAS, hydrops fetalis, prenatal diagnosis, whole‐genome sequencing
Short abstract
Linked article: There is a comment on this article by Lin and Li. Click here to view the Correspondence.
This article's abstract has been translated into Spanish and Chinese. Follow the links from the abstract to view the translations.
RESUMEN
Rendimiento diagnóstico mediante la secuenciación del genoma completo y panel informático de 281 genes asociados a la hidropesía fetal no inmune en el ámbito clínico
Objetivo
Investigar el rendimiento diagnóstico de la secuenciación clínica del genoma completo (SGC) en la hidropesía fetal no inmune (HFNI) diagnosticada prenatalmente.
Métodos
Esta investigación fue un estudio retrospectivo de 23 fetos con diagnóstico prenatal de HFNI, negativos para trisomías y variantes del número de copias, remitidos para su análisis mediante SGC con un panel informático de 281 genes asociados a la hidropesía fetal. Debido a la identificación de una alta proporción de variantes causales en el gen HRAS en la cohorte principal, la secuenciación Sanger de HRAS se realizó en una cohorte de replicación, que consistía en 24 fetos adicionales con HFNI que eran negativos para trisomías y variantes del número de copias y que no habían sido sometidos a SGC.
Resultados
De los 23 fetos de la cohorte principal, se logró un diagnóstico molecular en 12 (52,2%). Se identificaron variantes patógenas o probablemente patógenas en siete genes: HRAS (n=5), RIT1 (n=2), FOXP3 (n=1), GLB1 (n=1), MAP2K1 (n=1), PTPN11 (n=1) y RASA1 (n=1). El patrón de herencia de las 12 variantes causales fue autosómico dominante en 10 casos (HRAS, MAP2K1, PTPN11, RASA1, RIT1), autosómico recesivo en uno (GLB1) y recesivo ligado al X en uno (FOXP3). De los 24 fetos de la cohorte de replicación, se identificó una variante patógena en HRAS en uno, lo que resultó en una frecuencia global de HRAS del 12,8% (6/47) en las dos cohortes.
Conclusiones
Se demuestra un rendimiento diagnóstico del 52% con SGC clínico en HFNI utilizando un panel informático de 281 genes. Sin embargo, el elevado rendimiento diagnóstico puede atribuirse al pequeño tamaño de la muestra y a la posible abundancia de fenotipos graves en los fetos incluidos. Teniendo en cuenta que en las cohortes se excluyeron las anomalías cromosómicas, es posible obtener una tasa de detección de hasta el 75% en la HFNI diagnosticada prenatalmente cuando el análisis de SGC incluye la identificación de aberraciones cromosómicas.
摘要
在临床中使用全基因组测序和 用计算机面板对与非免疫性胎儿水肿相关的281种基因诊断阳性率
目的
探讨临床全基因组测序(WGS)对产前诊断非免疫性胎儿水肿(NIHF)的诊断阳性率。
方法
这是一项回顾性研究,对 23 个 三体正常和基因组拷贝数变异的被诊断为 非免疫性水肿(NIHF)的胎儿 进行了回顾性研究,病例通过转诊对与胎儿水肿相关的 281 个基因组进行了全基因组测序(WGS)计算机面板分析 。由于在主要队列中发现了高比例的HRAS 基因的致病变异,因此在复制队列中对HRAS 进行 Sanger 测序,该队列由另外 24 个患有肺免疫性水肿(NIHF)的胎儿组成,这些胎儿的三体正常但基因组拷贝数变异且未进行 全基因组测序(WGS)。
结果
在 23个主队列的胎儿中,有12例实现了分子诊断(52.2%)。在七组基因中鉴定出致病性或可能的致病性变异:HRAS (n=5), RIT1 (n=2), FOXP3 (n=1), GLB1 (n=1), MAP2K1 (n=1), PTPN11 (n=1) and RASA1 (n=1). 12个致病变异的遗传模式为:常染色体显性10例,(HRAS, MAP2K1, PTPN11, RASA1, RIT1),常染色体隐性1例,(GLB1) X连锁隐性1例(FOXP3).在复制队列的24个胎儿中, 其中一个胎儿发现一种 HRAS基因的 致病性变异, 导致我们的两个队列中HRAS基因致病变异的总体频率为 12.8% (6/47)。
结论
使用一种可检测281组基因的计算机面板我们临床上用全基因组测序(WGS)检测非免疫性水肿(NIHF)的阳性检测率为52%。然而,高诊断率可能归结于样本量小以及所包含胎儿中严重表型可能的过度表现。考虑到我们的队列中排除了染色体异常,因此如果 全基因组测序(WGS) 分析包括染色体畸变时,产前诊断的非免疫性水肿( NIHF) 的检出率可能高达 75%。
CONTRIBUTION —
What are the novel findings of this work?
This is the first study to investigate the diagnostic yield of clinical whole‐genome sequencing in prenatally diagnosed non‐immune hydrops fetalis. An incremental diagnostic yield of 52% was demonstrated in cases in which chromosomal aberrations had been excluded.
What are the clinical implications of this work?
Due to the wide range of underlying genetic etiologies of non‐immune hydrops fetalis, a comprehensive approach is essential in the evaluation of affected cases. Whole‐genome sequencing offers a high diagnostic yield by enabling simultaneous detection of different genetic variants across the entire genome.
INTRODUCTION
Hydrops fetalis is defined as excessive fluid accumulation in two or more fetal compartments 1 , 2 . If no maternal red cell alloimmunization is detected, the condition is classified as non‐immune hydrops fetalis (NIHF) 2 . NIHF is associated with notable risks, and despite improvements in diagnosis and management, its mortality rate remains high 3 , 4 . Identification of the underlying genetic causes of NIHF depends on multiple factors, including the method used and severity of the phenotype. Up to 50% of prenatally diagnosed cases of NIHF are caused by chromosome aberrations, which means that genetic etiology remains undefined in around half of NIHF cases if examined only by chromosome analysis, including array‐based molecular cytogenetic analysis 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 .
Massively parallel sequencing (MPS) is used increasingly in clinical settings. A recent systematic review by Mone et al.14 demonstrated that exome sequencing afforded an average incremental diagnostic yield of 29% in NIHF over chromosomal microarray analysis (CMA) or karyotyping. Sparks et al.15 showed that approximately 30% of NIHF cases with an identified monogenic cause belonged to the group of RASopathies, primarily due to variants in PTPN11, causing Noonan syndrome, or in HRAS, causing Costello syndrome. In the systematic review by Mone et al.14, RASopathies comprised approximately 30% of NIHF cases diagnosed by exome sequencing, most of which were due to PTPN11 variants. Whole‐genome sequencing (WGS) may offer an even more comprehensive method for identifying the underlying cause of NIHF by enabling the simultaneous detection of coding and non‐coding single‐nucleotide variants (SNVs) and insertions and deletions (INDELs), as well as copy‐number variants (CNVs), short tandem repeats (STRs) and balanced chromosome aberrations. To the best of our knowledge, there are no previous studies evaluating prenatal diagnosis of NIHF using WGS in a clinical setting. Hence, the primary aim of this study was to determine the diagnostic yield of clinical WGS in detecting causative variants in prenatally diagnosed NIHF. The secondary aim was to investigate the genetic etiologies identified by WGS.
METHODS
Study population
This was a retrospective study of all prenatally diagnosed cases of NIHF referred for clinical WGS with a hydrops fetalis gene panel at the Department of Clinical Genetics, Karolinska University Hospital, Sweden, between 13 September 2017 and 1 April 2021. The study was approved by the Swedish Ethical Review Authority (reference number: 2020‐05297).
Hydrops fetalis was detected by prenatal ultrasound in all cases but one (Case 15, Table 1). No pathophysiological reason for hydrops was reported by the referring clinicians in any of the cases. Prior to WGS analysis, subjects were analyzed according to our routine clinical protocol, including quantitative fluorescent polymerase chain reaction (QF‐PCR) and in most cases CMA, in order to exclude cases with causative chromosomal aberrations. This resulted in inclusion of 23 fetuses without chromosomal abnormalities in the main cohort of the study (Table 1). Specifically, 20 cases had normal results on both QF‐PCR and CMA, two cases had normal results on QF‐PCR only and one case had normal results on QF‐PCR and karyotype analysis.
Table 1.
Clinical characteristics, pregnancy outcome and chromosomal analysis of 23 prenatally diagnosed cases of non‐immune hydrops fetalis
| Case | GA at referral (weeks) | Clinical information | Sample | Pregnancy outcome | Preceding genetic analysis |
|---|---|---|---|---|---|
| 1 | 19 + 3 | Hydrops fetalis, oligohydramnios and fetal akinesia | Lung tissue | TOP | QF‐PCR: XY; CMA: normal |
| 2 | 18 + 0 | Hydrops fetalis | Lung tissue | Miscarriage | QF‐PCR: XX; CMA: normal |
| 3 | 18 + 0 | Hydrops fetalis | Lung tissue | Miscarriage | QF‐PCR: XX; CMA: normal |
| 4 | 30 + 0 | Hydrops fetalis | CVS | IUFD | QF‐PCR: XY; CMA: normal |
| 5 | 21 + 0 | Hydrops fetalis, suspected hypertelorism, low‐set ears, hepatomegaly, abnormal hands and short extremities | Spleen tissue | TOP | QF‐PCR: XX; CMA: normal |
| 6 | 20 + 1 | Hydrops fetalis, hygroma, pelvic cyst and unilateral renal agenesis | AC | TOP | QF‐PCR: XX; CMA: normal |
| 7 | 29 + 0 | Hydrops fetalis, polyhydramnios and unilateral multicystic dysplastic kidney | AC | IUFD | QF‐PCR: XX; CMA: normal |
| 8 | 18 + 2 | Hydrops fetalis, IUGR, suspected atrial septal defect | Lung tissue | Miscarriage | QF‐PCR: XX; CMA: normal |
| 9 | 14 + 2 | Hydrops fetalis, hygroma | CVS | TOP | QF‐PCR: XY; CMA: normal |
| 10 | 12 + 2 | Hydrops fetalis, hygroma and liver calcifications | Lung tissue | TOP | QF‐PCR: XY; CMA: normal |
| 11 | 24 + 1 | Initially dichorionic diamniotic twin pregnancy: Twin 1 missed miscarriage, Twin 2 hydrops fetalis | CVS | IUFD | QF‐PCR: XX |
| 12 | 19 + 0 | Hydrops fetalis, IUGR, micrognathia, low‐set ears, camptodactyly, lung hypoplasia and liver calcification | Lung tissue | Miscarriage | QF‐PCR: XY; CMA: normal |
| 13 | 18 + 0 | Hydrops fetalis with prior nuchal translucency thickness 4.4 mm | Lung tissue | Miscarriage | QF‐PCR: XX; CMA: normal |
| 14 | 13 + 0 | Hydrops fetalis | CVS | TOP | QF‐PCR: XY; CMA: normal |
| 15 | 36 + 5 | Consanguineous marriage, three previous pathological pregnancies with hydrops fetalis; current pregnancy with IUFD but no sign of hydrops fetalis at time of assessment | Lung tissue | IUFD | QF‐PCR: XY; karyotype analysis (on CVS): XY |
| 16 | 18 + 0 | Hydrops fetalis and IUGR | AC | Miscarriage | QF‐PCR: XY; CMA: normal |
| 17 | 23 + 0 | Resolving hydrops fetalis, micropenis, cardiomegaly and increased nuchal fold | CVS | Live birth | QF‐PCR: XY; CMA: normal |
| 18 | 30 + 2 | Severe hydrops fetalis | AC | Live birth | QF‐PCR: XY; CMA: normal |
| 19 | 19 + 6 | Hydrops fetalis | AC | TOP | QF‐PCR: XX |
| 20 | 19 + 2 | Hydrops fetalis with multiple malformations | Lung tissue | TOP | QF‐PCR: XX; CMA: normal |
| 21 | 28 + 0 | Hydrops fetalis | AC | IUFD | QF‐PCR: XY; CMA: normal |
| 22 | 13 + 2 | Mild hydrops fetalis | CVS | Live birth | QF‐PCR: XY; CMA: normal |
| 23 | 32 + 4 | Hydrops fetalis | AC | IUFD | QF‐PCR: XY; CMA: normal |
Clinical information was obtained from referral letters regarding ultrasound findings and autopsy reports, as applicable.
AC, amniocentesis; CMA, chromosomal microarray analysis; CVS, chorionic villus sampling; GA, gestational age; IUFD, intrauterine fetal demise; IUGR, intrauterine growth restriction; QF‐PCR, quantitative fluorescence polymerase chain reaction (targeting chromosomes 13, 18, 21, X and Y); TOP, termination of pregnancy.
Depending on specific sample availability in each pregnancy, fetal samples for DNA extraction were obtained via amniocentesis (n = 7), chorionic villus sampling (n = 6) or sampling of frozen fetal tissue (n = 10). The latter was performed at postmortem examination following miscarriage, intrauterine fetal demise (IUFD; defined as fetal demise > 22 weeks' gestation) or termination of pregnancy. Gestational age at referral ranged from 13 to 37 weeks. Twelve of the 23 pregnancies ended in miscarriage or IUFD, eight pregnancies were terminated and three pregnancies resulted in a live birth.
Due to identification by WGS of a high proportion of causative variants in the HRAS gene in our main cohort, Sanger sequencing of HRAS was performed in a separate replication cohort. This included 24 fetuses with NIHF and normal results on CMA, but for whom WGS analysis had not been requested by the referring clinician.
Whole‐genome sequencing
WGS of genomic DNA extracted from the fetal samples was performed in a collaborating laboratory (Clinical Genomics; Science for Life Laboratory, Solna, Sweden). The detailed process for WGS analysis and variant calling has been described previously 16 , 17 . Briefly, extracted DNA was converted to sequencing libraries using a PCR‐free paired‐end protocol: Illumina TruSeq DNA PCR‐free (Illumina Inc., San Diego, CA, USA) for inputs > 1000 ng or Lucigen NxSeq AmpFREE Low DNA (Lucigen Corp., Middleton, WI, USA) for inputs > 100 ng. Sequencing was performed on the Illumina Hiseq X Ten (n = 10) or Illumina NovaSeq 6000 (n = 13) platforms (Illumina Inc.). Bioinformatics analysis was conducted using the Mutation Identification Pipeline (MIP) framework 18 . FASTQ data were aligned to the human reference genome (hg19) prior to variant calling, which included SNVs, INDELs, structural variants (SVs), STRs and copy‐number identification of the SMN1 and SMN2 genes. Subsequently, variants were annotated and prioritized based on factors such as variant type, mode of inheritance and allele frequency, before being transferred to Scout, a graphical user interface for MPS data and metadata 17 .
Clinical variant interpretation was performed by filtering the called variants against an in‐silico gene panel comprising 281 genes known to be associated with hydrops fetalis (Table S1). This clinical gene panel is updated regularly (typically 2–4 times per year) based on literature searches and comparisons to publicly available gene lists from other genetic laboratories. Variants were filtered further so that only exonic and predicted splice variants were retained regarding SNVs, INDELs and SVs. The minor allele frequencies of the variants were annotated according to the Genome Aggregation Database (gnomAD) 19 and a local in‐house database, and variants with minor allele frequencies of > 1% were excluded. Remaining variants were then classified into five categories (benign, likely benign, uncertain significance, likely pathogenic and pathogenic) according to the guidelines of the American College of Medical Genetics and Genomics 20 . Single pathogenic variants in autosomal recessive disease genes were excluded if a compound variant was not detected. Finally, a multidisciplinary team assessed the remaining putatively causative variants based on available prenatal phenotype and pedigree information, which in most cases was extracted from referral letters. Autopsy reports were reviewed in cases of miscarriage/IUFD and pregnancy termination. The primary analyses were performed using proband‐only (fetal without parental) samples. Parental samples were obtained only if needed to classify a variant of uncertain significance or to investigate recurrence risk.
CNV analysis
In addition to the analysis of genetic aberrations included in the hydrops fetalis gene panel, a whole‐genome analysis of large CNVs, corresponding to a CMA, was performed using vcf2cytosure 21 . This enables visualization and interpretation of CNVs in CytoSure Interpret Software (Oxford Gene Technology, Begbroke, UK), which is used routinely in our laboratory to analyze CMA data.
HRAS sequencing
All four coding exons and intron–exon boundaries of HRAS (NM_176795.4) were amplified by PCR and sequenced according to standard Sanger methodology (primers and PCR conditions are available on request).
RESULTS
The main study cohort included 23 fetuses without chromosomal aberrations. Clinical WGS analysis using an in‐silico hydrops fetalis gene panel resulted in a molecular diagnosis in 52.2% (12/23) of the studied NIHF cases. A summary of the causative variants detected by WGS is presented in Table 2. The causative variants were located in seven genes, namely HRAS (5/12, 41.7%), RIT1 (2/12, 16.7%), FOXP3 (1/12, 8.3%), GLB1 (1/12, 8.3%), MAP2K1 (1/12, 8.3%), PTPN11 (1/12, 8.3%) and RASA1 (1/12, 8.3%). Of the 12 causative variants, three (25.0%) were novel, comprising one missense variant in HRAS (c.182A>G; p.(Gln61Arg)), one 278‐bp hemizygous deletion in FOXP3 (Figure 1) and one frameshift variant in RASA1. Three variants of uncertain significance were identified in three different genes (PIEZO1, SOS2 and FLT4), but reclassified as likely benign after analysis of parental samples. No SVs or STRs were identified, nor abnormal copy‐number variation in the SMN1 and SMN2 genes. No large CNVs were detected in the vcf2cytosure analysis, which was expected as most of the cases had been analyzed previously with CMA.
Table 2.
Summary of 12 causative variants detected by whole‐genome sequencing in 23 prenatally diagnosed cases of non‐immune hydrops fetalis
| Gene (transcript) | Case | Coding change | Zygosity | ACMG class | Diagnosis | Inheritance mode | Parental source |
|---|---|---|---|---|---|---|---|
| FOXP3 (NM_014009.3) | 12 | c.(1045‐219)_1104del | Hemi | L‐path | Immunodysregulation, polyendocrinopathy and enteropathy, X‐linked (IPEX) (OMIM #304790) | XLR | Mat |
| GLB1 (NM_000404.4) | 15 | c.1077del; p.(Val360Tyrfs*23) | Hom | Path | GM1 gangliosidosis (OMIM #230500, 230 600, 230 650) | AR | Mat/pat |
| HRAS (NM_176795.4) | 5 | c.35G>A; p.(Gly12Asp) | Het | Path | Costello syndrome (OMIM #218040) | AD | DN |
| 10 | c.38G>A; p.(Gly13Asp) | Het | Path | Costello syndrome* | AD | DN | |
| 13 | c.38G>A; p.(Gly13Asp) | Het | Path | Costello syndrome* | AD | NA | |
| 14 | c.38G>A; p.(Gly13Asp) | Het | Path | Costello syndrome* | AD | NA | |
| 3 | c.182A>G; p.(Gln61Arg) | Het | L‐path | Costello syndrome* | AD | NA | |
| MAP2K1 (NM_002755) | 19 | c.158T>C; p.(Phe53Ser) | Het | Path | Cardiofaciocutaneous syndrome 3 (OMIM #615279) | AD | NA |
| PTPN11 (NM_002834) | 21 | c.215C>G; p.(Ala72Gly) | Het | Path | Noonan syndrome 1 (OMIM #163950) | AD | NA |
| RASA1 (NM_002890) | 23 | c.2299del; p.(Ser767Argfs*7) | Het | Path | Capillary malformation‐ arteriovenous malformation 1 (OMIM #608354) | AD | DN |
| RIT1 (NM_006912.6) | 9 | c.229G>A; p.(Ala77Thr) | Het | Path | Noonan syndrome, type 8 (OMIM #615355) | AD | DN |
| 6 | c.270G>A; p.(Met90Ile) | Het | Path | Noonan syndrome, type 8* | AD | DN |
OMIM as above.
ACMG, American College of Medical Genetics and Genomics; AD, autosomal dominant; AR, autosomal recessive; DN, de novo; hemi, hemizygous; het, heterozygous; hom, homozygous; L‐path, likely pathogenic; mat, maternal; NA, not applicable; pat, paternal; path, pathogenic; XLR, X‐linked recessive.
Figure 1.
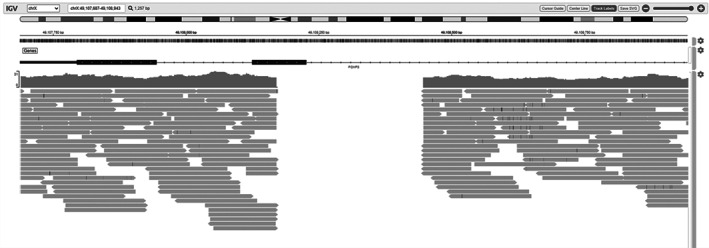
Integrative Genomics Viewer (IGV) showing 278‐bp deletion in FOXP3 gene in Case 12. Since FOXP3 is located on X chromosome and Case 12 was male, IGV shows complete lack of reads within the gene, indicating hemizygous deletion.
The inheritance patterns of the causative variants were 10/12 autosomal dominant (HRAS, MAP2K1, PTPN11, RASA1 and RIT1), 1/12 autosomal recessive (GLB1) and 1/12 X‐linked recessive (FOXP3). Parental samples were obtained in seven (58.3%) of the 12 cases with a detected causative variant. Both of the RIT1 variants were de novo, as were the two tested HRAS variants and the RASA1 variant. The homozygous GLB1 variant was inherited from parents who were both heterozygous carriers. The deletion in FOXP3 was detected in a male fetus. The parental samples showed that it was inherited from the mother, which is in line with the mode of inheritance of an X‐linked disease.
In order to investigate further the high number of HRAS variants in our cohort, Sanger sequencing of HRAS was performed on a separate replication cohort of 24 NIHF cases. In one (4.2%) of these 24 samples, a pathogenic variant of HRAS (c.35G>A; p.(Gly12Asp)) was detected. This means that the overall frequency of causative HRAS variants in our two cohorts was 12.8% (6/47).
DISCUSSION
In this study of prenatally diagnosed cases of NIHF prescreened for chromosomal aberrations, clinical WGS using an in‐silico hydrops fetalis gene panel detected a causative variant in 52.2% of fetuses. To the best of our knowledge, this is the first study to evaluate the diagnostic yield of WGS in NIHF. Our findings suggest that WGS could be an effective first‐line test for NIHF and, considering that up to 50% of prenatally diagnosed cases of NIHF are caused by chromosomal aberrations 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , indicate that the diagnostic yield of WGS could be as high as 75%.
The diagnostic yield of WGS in this study is higher than the 29% incremental yield reported in a previous systematic review evaluating prenatal exome sequencing for the diagnosis of NIHF14. This disparity may be explained by the small sample size of this study and our inclusion of NIHF cases in which the referring clinician requested specifically analysis with the hydrops fetalis gene panel. As WGS is still considered relatively expensive, it is likely to be offered to more severely affected fetuses, potentially creating a selection bias in our cohort. The possible over‐representation of severe cases in our cohort is underlined by the fact that approximately half of the pregnancies ended in miscarriage or IUFD. Possible selection bias may also explain why only one causative variant in HRAS was detected by Sanger sequencing in the 24 additional NIHF cases for which a gene panel had not been requested. Due to the diversity and rarity of genetic etiologies of NIHF, a comprehensive evidence‐based approach is essential to the evaluation of these cases. WGS enables the simultaneous detection of different genetic variants across the entire genome, from single nucleotides to whole chromosomes. Exome sequencing often requires adjunctive CMA in order to detect CNVs. Thus, WGS has the potential to yield a more efficient diagnosis compared with exome sequencing alone. Because this study was performed in a clinical setting, only exonic and predicted splice variants were included regarding SNVs, INDELs and SVs. This, combined with our use of a singleton gene panel rather than a trio analysis, might have reduced the diagnostic yield of WGS by preventing the identification of novel genes and novel variants in non‐coding regions of known genes. Unlike exome sequencing, our approach with WGS, including the analysis of large CNVs, enabled the investigation of not only SNVs and INDELs but also CNVs of different sizes, SVs, STRs and copy‐number identification of the SMN1 and SMN2 genes. However, only one of the detected variants in this study, the 278‐bp deletion in FOXP3, could have been a borderline case for detection by exome sequencing. Further research is needed to determine the precise yield of WGS in cases of NIHF and its clinical applicability considering the time constraints of an ongoing pregnancy.
In this study, WGS identified causative variants in 12/23 analyzed NIHF cases, comprising seven different genes associated with seven different diagnoses (Table 2). Most (5/7, 71.4%) of the detected diagnoses belonged to RASopathies, with a causative variant found in HRAS, MAP2K1, PTPN11, RASA1 or RIT1. This is in line with previous studies on NIHF, albeit with a slightly higher proportion of RASopathies 14 , 15 . Interestingly, we found an unexpectedly high incidence of Costello syndrome, as causative variants in HRAS were detected in 5/12 (41.7%) cases receiving a molecular diagnosis.
The most frequently reported germline HRAS variants are de‐novo variants affecting glycine in codon 12 or 13, of which the most common are p.(Gly12Ser) and p.(Gly12Ala) 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 . Accordingly, we found that four of five identified HRAS variants were located in these codons, whereas the fifth was located in codon 61. Germline variants and somatic variants in sporadic tumors share codons 12 and 13 as mutational hotspots in HRAS, while codon 61 has been regarded to be a mutational hotspot only in sporadic tumors 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 . A literature search identified only one reported case of a germline variant located in codon 61 of the HRAS gene in an individual diagnosed with Costello syndrome 31 . The fetus presented with nuchal edema, polyhydramnios and signs of fetal akinesia, and exome sequencing detected a likely pathogenic missense variant (c.183G>C; p.(Gln61His)) in codon 61 of HRAS 31. This case, together with the variant detected in this study (c.182A>G; p.(Gln61Arg)), suggests that germline variants in codon 61 of the HRAS gene should be taken into account when interpreting results from MPS.
This study highlights the benefits of MPS in prenatal diagnosis. A genetic diagnosis is important for parents and clinicians as it offers an explanation, informs the prognosis, guides prenatal and postnatal care and enables adequate estimation of the recurrence risk in future pregnancies. In this study, 83.3% of identified causative variants were autosomal dominant. Detection of inherited causative variants, i.e. GLB1 and FOXP3 variants, offers families the possibility of prenatal diagnosis or preimplantation genetic testing in future pregnancies.
In summary, in a cohort of 23 prenatally diagnosed cases of NIHF in which chromosomal aberrations had been excluded, a genetic etiology was established in 52% using WGS with an in‐silico hydrops fetalis gene panel. Considering that up to 50% of prenatally diagnosed cases of NIHF are attributed to chromosomal aberrations, a detection rate of up to 75% may be expected when using WGS including an analysis of chromosome aberrations. Most of the causative variants were found in HRAS, highlighting Costello syndrome as an important cause of NIHF.
Supporting information
Table S1 Content of targeted in‐silico hydrops fetalis whole‐genome sequencing gene panel
ACKNOWLEDGMENTS
We thank Pia Ostergaard for her help with establishing our hydrops fetalis gene list. We also thank Nina Jäntti for helping with Sanger sequencing.
Disclosures
E.I. was supported by grants from Stockholm County Council (FoUI‐961 392), Karolinska Institutet and Sällsyntafonden. E.W. received grants from Stockholm County Council and Sällsyntafonden. A.L. was supported by grants from the Stockholm County Council, Swedish Research Council and the Swedish Brain Foundation.
DATA AVAILABILITY STATEMENT
The data are not publicly available due to the sensitivity of the clinical data.
REFERENCES
- 1. Jones DC. Nonimmune fetal hydrops: diagnosis and obstetrical management. Semin Perinatol 1995; 19: 447–461. [DOI] [PubMed] [Google Scholar]
- 2. Warsof SL, Nicolaides KH, Rodeck C. Immune and non‐immune hydrops. Clin Obstet Gynecol 1986; 29: 533–542. [DOI] [PubMed] [Google Scholar]
- 3. Santo S, Mansour S, Thilaganathan B, Homfray T, Papageorghiou A, Calvert S, Bhide A. Prenatal diagnosis n‐immune hydrops fetalis: what do we tell the parents? Prenat Diagn 2011; 31: 186–195. [DOI] [PubMed] [Google Scholar]
- 4. Whybra C, Källén K, Hansson SR, Gunnarsson R. Non‐immune hydrops fetalis was rare in Sweden during 1997–2015, but cases were associated with complications and poor prognosis. Acta Paediatr 2020; 109: 2570–2577. [DOI] [PubMed] [Google Scholar]
- 5. Deng Q, Fu F, Yu Q, Li R, Li F, Wang D, Lei T, Yang X, Liao C. Nonimmune hydrops fetalis: Genetic analysis and clinical outcome. Prenat Diagn 2020; 40: 803–812. [DOI] [PubMed] [Google Scholar]
- 6. Gimovsky AC, Luzi P, Berghella V. Lysosomal storage disease as an etiology of nonimmune hydrops. Am J Obstet Gynecol 2015; 212: 281–290. [DOI] [PubMed] [Google Scholar]
- 7. Halliday J, Lumley J, Bankier A. Karyotype abnormalities in fetuses diagnosed as abnormal on ultrasound before 20 weeks' gestational age. Prenat Diagn 1994; 14: 689–697. [DOI] [PubMed] [Google Scholar]
- 8. Hanna JS, Neu RL, Lockwood DH. Prenatal cytogenetic results from cases referred for 44 different types of abnormal ultrasound findings. Prenat Diagn 1996; 16: 109–115. [DOI] [PubMed] [Google Scholar]
- 9. Ota S, Sahara J, Mabuchi A, Yamamoto R, Ishii K, Mitsuda N. Perinatal and one‐year outcomes of non‐immune hydrops fetalis by etiology and age at diagnosis. J Obstet Gynaecol Res 2016; 42: 385–391. [DOI] [PubMed] [Google Scholar]
- 10. Rizzo N, Pittalis MC, Pilu G, Perolo A, Banzi C, Visentin A, Bovicelli L. Distribution of abnormal karyotypes among malformed fetuses detected by ultrasound throughout gestation. Prenat Diagn 1996; 16: 159–163. [DOI] [PubMed] [Google Scholar]
- 11. Shaffer LG, Rosenfeld JA, Dabell MP, Coppinger J, Bandholz AM, Ellison JW, Ravnan JB, Torchia BS, Ballif BC, Fisher AJ. Detection rates of clinically significant genomic alterations by microarray analysis for specific anomalies detected by ultrasound. Prenat Diagn 2012; 32: 986–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sparks TN, Thao K, Lianoglou BR, Boe NM, Bruce KG, Datkhaeva I, Field NT, Fratto VM, Jolley J, Laurent LC, Mardy AH, Murphy AM, Ngan E, Rangwala N, Rottkamp CAM, Wilson L, Wu E, Uy CC, Valdez Lopez P, Norton ME; University of California Fetal–Maternal Consortium (UCfC) . Nonimmune hydrops fetalis: identifying the underlying genetic etiology. Genet Med 2019; 21: 1339–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang S, Lei C, Wu J, Sun H, Yang Y, Zhang Y, Sun X. A Retrospective Study of Cytogenetic Results From Amniotic Fluid in 5328 Fetuses With Abnormal Obstetric Sonographic Findings. J Ultrasound Med 2017; 36: 1809–1817. [DOI] [PubMed] [Google Scholar]
- 14. Mone F, Eberhardt RY, Hurles ME, Mcmullan DJ, Maher ER, Lord J, Chitty LS, Dempsey E, Homfray T, Giordano JL, Wapner RJ, Sun L, Sparks TN, Norton ME, Kilby MD. Fetal hydrops and the Incremental yield of Next‐generation sequencing over standard prenatal Diagnostic testing (FIND) study: prospective cohort study and meta‐analysis. Ultrasound Obstet Gynecol 2021; 58: 509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sparks TN, Lianoglou BR, Adami RR, Pluym ID, Holliman K, Duffy J, Downum SL, Patel S, Faubel A, Boe NM, Field NT, Murphy A, Laurent LC, Jolley J, Uy C, Slavotinek AM, Devine P, Hodoglugil U, Van Ziffle J, Sanders SJ, MacKenzie TC, Norton ME; University of California Fetal–Maternal Consortium; University of California, San Francisco Center for Maternal–Fetal Precision Medicine . Exome Sequencing for Prenatal Diagnosis in Nonimmune Hydrops Fetalis. N Engl J Med 2020; 383: 1746–1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lindstrand A, Eisfeldt J, Pettersson M, Carvalho CMB, Kvarnung M, Grigelioniene G, Anderlid BM, Bjerin O, Gustavsson P, Hammarsjö A, Georgii‐Hemming P, Iwarsson E, Johansson‐Soller M, Lagerstedt‐Robinson K, Lieden A, Magnusson M, Martin M, Malmgren H, Nordenskjöld M, Norling A, Sahlin E, Stranneheim H, Tham E, Wincent J, Ygberg S, Wedell A, Wirta V, Nordgren A, Lundin J, Nilsson D. From cytogenetics to cytogenomics: whole‐genome sequencing as a first‐line test comprehensively captures the diverse spectrum of disease‐causing genetic variation underlying intellectual disability. Genome Med 2019; 11: 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stranneheim H, Lagerstedt‐Robinson K, Magnusson M, Kvarnung M, Nilsson D, Lesko N, Engvall M, Anderlid BM, Arnell H, Johansson CB, Barbaro M, Björck E, Bruhn H, Eisfeldt J, Freyer C, Grigelioniene G, GutavssonP, Hammarsjö A , Hellström‐Pigg M, Iwarsson E, Jemt A, Laaksonen M, Enoksson SL, Malmgren H, Naess K, Nordenskjöld M, Oscarson M, Pettersson M, Rasi C, Rosenbaum A, Sahlin E, Sardh E, Stödberg T, Tesi B, Tham E, Thonberg H, Töhönen V, von Döbeln U, Vassiliou D, Vonlanthen S, Wikström AC, Wincent J, Winqvist O, Wredenberg A, Ygberg S, Zetterström RH, Marits P, Soller MJ, Nordgren A, Wirta V, Lindstrand A, Wedell A. Integration of whole genome sequencing into a healthcare setting: high diagnostic rates across multiple clinical entities in 3219 rare disease patients. Genome Med 2021; 13: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stranneheim H, Engvall M, Naess K, Lesko N, Larsson P, Dahlberg M, Andeer R, Wredenberg A, Freyer C, Barbaro M, Bruhn H, Emahazion T, Magnusson M, Wibom R, Zetterström RH, Wirta V, von Döbeln U, Wedell A. Rapid pulsed whole genome sequencing for comprehensive acute diagnostics of inborn errors of metabolism. BMC Genomics 2014; 15: 1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, Collins RL, Laricchia KM, Ganna A, Birnbaum DP, Gauthier LD, Brand H, Solomonson M, Watts NA, Rhodes D, Singer‐Berk M, England EM, Seaby EG, Kosmicki JA, Walters RK, Tashman K, Farjoun Y, Banks E, Poterba T, Wang A, Seed C, Whiffin N, Chong JX, Samocha KE, Pierce‐Hoffman E, Zappala Z, O'Donnell‐Luria AH, Minikel EV, Weisburd B, Lek M, Ware JS, Vittal C, Armean IM, Bergelson L, Cibulskis K, Connolly KM, Covarrubias M, Donnelly S, Ferriera S, Gabriel S, Gentry J, Gupta N, Jeandet T, Kaplan D, Llanwarne C, Munshi R, Novod S, Petrillo N, Roazen D, Ruano‐Rubio V, Saltzman A, Schleicher M, Soto J, Tibbetts K, Tolonen C, Wade G, Talkowski ME; Genome Aggregation Database Consortium , Neale BM, Daly MJ, DG MacArthur. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 2020; 581: 434–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Richards S, Aziz N, Bale S, Bick D, Das S, Gastier‐Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL; ACMG Laboratory Quality Assurance Committee . Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015; 17: 405–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. vcf2cytosure . https://github.com/NBISweden/vcf2cytosure.
- 22. Aoki Y, Niihori T, Kawame H, Kurosawa K, Ohashi H, Tanaka Y, Filocamo M, Kato K, Suzuki Y, Kure S, Matsubara Y. Germline mutations in HRAS proto‐oncogene cause Costello syndrome. Nat Genet 2005; 37: 1038–1040. [DOI] [PubMed] [Google Scholar]
- 23. Estep AL, Tidyman WE, Teitell MA, Cotter PD, Rauen KA. HRAS mutations in Costello syndrome: detection of constitutional activating mutations in codon 12 and 13 and loss of wild‐type allele in malignancy. Am J Med Genet A 2006; 140: 8–16. [DOI] [PubMed] [Google Scholar]
- 24. Gripp KW, Lin AE, Stabley DL, Nicholson L, Scott CI Jr, Doyle D, Aoki Y, Matsubara Y, Zackai EH, Lapunzina P, Gonzalez‐Meneses A, Holbrook J, Agresta CA, Gonzalez IL, Sol‐Church K. HRAS mutation analysis in Costello syndrome: genotype and phenotype correlation. Am J Med Genet A 2006; 140: 1–7. [DOI] [PubMed] [Google Scholar]
- 25. Kerr B, Delrue MA, Sigaudy S, Perveen R, Marche M, Burgelin I, Stef M, Tang B, Eden OB, O'Sullivan J, De Sandre‐Giovannoli A, Reardon W, Brewer C, Bennett C, Quarell O, M'Cann E, Donnai D, Stewart F, Hennekam R, Cavé H, Verloes A, Philip N, Lacombe D, Levy N, Arveiler B, Black G. Genotype‐phenotype correlation in Costello syndrome: HRAS mutation analysis in 43 cases. J Med Genet 2006; 43: 401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lin AE, Alexander ME, Colan SD, Kerr B, Rauen KA, Noonan J, Baffa J, Hopkins E, Sol‐Church K, Limongelli G, Digilio MC, Marino B, Innes AM, Aoki Y, Silberbach M, Delrue MA, White SM, Hamilton RM, O'Connor W, Grossfeld PD, Smoot LB, Padera RF, Gripp KW. Clinical, pathological, and molecular analyses of cardiovascular abnormalities in Costello syndrome: a Ras/MAPK pathway syndrome. Am J Med Genet A 2011; 155A: 486–507. [DOI] [PubMed] [Google Scholar]
- 27. McCormick EM, Hopkins E, Conway L, Catalano S, Hossain J, Sol‐Church K, Stabley DL, Gripp KW. Assessing genotype‐phenotype correlation in Costello syndrome using a severity score. Genet Med 2013; 15: 554–557. [DOI] [PubMed] [Google Scholar]
- 28. Schulz AL, Albrecht B, Arici C, van der Burgt I, Buske A, Gillessen‐Kaesbach G, Heller R, Horn D, Hübner CA, Korenke GC, König R, Kress W, Krüger G, Meinecke P, Mücke J, Plecko B, Rossier E, Schinzel A, Schulze A, Seemanova E, Seidel H, Spranger S, Tuysuz B, Uhrig S, Wieczorek D, Kutsche K, Zenker M. Mutation and phenotypic spectrum in patients with cardio‐facio‐cutaneous and Costello syndrome. Clin Genet 2008; 73: 62–70. [DOI] [PubMed] [Google Scholar]
- 29. Zampino G, Pantaleoni F, Carta C, Cobellis G, Vasta I, Neri C, Pogna EA, De Feo E, Delogu A, Sarkozy A, Atzeri F, Selicorni A, Rauen KA, Cytrynbaum CS, Weksberg R, Dallapiccola B, Ballabio A, Gelb BD, Neri G, Tartaglia M. Diversity, parental germline origin, and phenotypic spectrum of de novo HRAS missense changes in Costello syndrome. Hum Mutat 2007; 28: 265–272. [DOI] [PubMed] [Google Scholar]
- 30. Bos JL. Ras oncogenes in human cancer: a review. Cancer Res 1989; 49: 4682–4689. [PubMed] [Google Scholar]
- 31. Reischer T, Liebmann‐Reindl S, Bettelheim D, Balendran‐Braun S, Streubel B. Genetic diagnosis and clinical evaluation of severe fetal akinesia syndrome. Prenat Diagn 2020; 40: 1532–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Content of targeted in‐silico hydrops fetalis whole‐genome sequencing gene panel
Data Availability Statement
The data are not publicly available due to the sensitivity of the clinical data.


