Abstract
By the end of 2021, approximately 15% of U.S. adults remained unvaccinated against COVID-19, and vaccination initiation rates had stagnated. We used unsupervised machine learning (K-means clustering) to identify clusters of unvaccinated respondents based on Behavioral and Social Drivers (BeSD) of COVID-19 vaccination and compared these clusters to vaccinated participants to better understand social/behavioral factors of non-vaccination. The National Immunization Survey Adult COVID Module collects data on U.S. adults from September 26–December 31,2021 (n = 187,756). Among all participants, 51.6% were male, with a mean age of 61 years, and the majority were non-Hispanic White (62.2%), followed by Hispanic (17.2%), Black (11.9%), and others (8.7%). K-means clustering procedure was used to classify unvaccinated participants into three clusters based on 9 survey BeSD items, including items assessing COVID-19 risk perception, social norms, vaccine confidence, and practical issues. Among unvaccinated adults (N = 23,397), 3 clusters were identified: the “Reachable” (23%), “Less reachable” (27%), and the “Least reachable” (50%). The least reachable cluster reported the lowest concern about COVID-19, mask-wearing behavior, perceived vaccine confidence, and were more likely to be male, non-Hispanic White, with no health conditions, from rural counties, have previously had COVID-19, and have not received a COVID-19 vaccine recommendation from a healthcare provider. This study identified, described, and compared the characteristics of the three unvaccinated subgroups. Public health practitioners, healthcare providers and community leaders can use these characteristics to better tailor messaging for each sub-population. Our findings may also help inform decisionmakers exploring possible policy interventions.
Keywords: SARS-CoV-2, COVID-19 vaccines, Vaccine hesitancy, Cluster analysis, Health policy, Health communication
1. Introduction
Receiving a COVID-19 vaccination is important both to prevent COVID-19-related morbidity and mortality and to slow the spread of SARS-CoV-2, the virus that causes COVID-19. Though COVID-19 vaccination is recommended for adults, by the end of 2021, approximately 15% of U.S. adults remained unvaccinated against COVID-19, and vaccination initiation rates had stagnated (Centers for Disease Control and Prevention, 2022c, Centers for Disease Control and Prevention, 2022d). The Behavioral and Social Drivers (BeSD) of Vaccination framework was built on the Increasing Vaccine Model, which identified thinking and feeling, social processes, and practical issues as the behavioral and social drivers of COVID-19 vaccination (Brewer, 2021; Brewer et al., 2017). The National Immunization Survey Adult COVID Module (NIS-ACM) was initiated in April 2021 in response to the COVID-19 pandemic, to assess COVID-19 vaccine coverage in adults over 18 years, and to provide nationally representative estimates of the BeSD of COVID-19 vaccination (Centers for Disease Control and Prevention, 2022b).
Recent COVID-19 research identified many population characteristics associated with low vaccination coverage or higher vaccine hesitancy, including younger age, racial/ethnic minority groups, less education, unemployment, no health insurance, living in rural or socially vulnerable areas, and no health condition that may put them at higher risk for COVID-19 (Khairat et al., 2022; Lu et al., 2022; Saelee et al., 2022). However, it's important to recognize that the unvaccinated population may have different underlying reasons for vaccine hesitancy, and these differences can be assessed by BeSD framework domains/items. Further examination, identification, and characterization of sub-groups with similar BeSD assessment scores could provide better understanding of shared root causes underlying disparate unvaccinated population. The present study used cluster analysis, an unsupervised machine learning, to identify three clusters of unvaccinated survey respondents based on the BeSD domains: vaccine confidence (e.g., perceived importance and safety of COVID-19 vaccine), risk perception (concern about getting COVID-19), social norms (e.g., vaccination status of friends and families) and practical issues (e.g., availability and accessibility of vaccine). Cluster analysis is an inductive exploratory technique that uncovers structures without existing hypothesis (Wu, 2012). The clusters identified could provide additional information on the characteristics of this unvaccinated population. The objectives of this study were to compare these identified unvaccinated clusters to vaccinated participants to better understand reasons for non-vaccination and to describe the demographic and other characteristics of these clusters.
2. Methods
2.1. Participants and survey description
The NIS-ACM is a nationally representative survey of non-institutionalized U.S. adults aged ≥18 years that uses a random-digit–dialed sample of cellular telephone numbers (Wolter et al., 2017). Data collected during September 26 through December 31, 2021, were used for these analyses. Response rates were calculated for three approximate monthly analytic periods: September 26–October 30, October 31–November 27, and November 28–December 31. Response rates for these three periods ranged from 20.9% to 23.4%, and the total sample size was 187,756. However, 911 participants with incomplete data on COVID-19 vaccine status or BeSD items were excluded, leaving an analytic sample of 186,845. The survey collected detailed demographic information from the participants, including gender, age, race/ethnicity, education, household income and county of residence. Receipt of ≥1 dose of COVID-19 vaccine was assessed with the question “Have you received at least one dose of a COVID-19 vaccine?” Those responding “no” were asked “How likely are you to get a COVID-19 vaccine? Would you say you would definitely get a vaccine, probably get a vaccine, probably not get a vaccine, definitely not get a vaccine, or are not sure?” Data were weighted to represent the noninstitutionalized U.S. adult population aged ≥18 years and calibrated within states by age and sex for each monthly analytic period to COVID-19 vaccine administration data reported to CDC by state and jurisdictional health departments as of mid-month (Centers for Disease Control and Prevention, 2022a).
2.2. Statistical analysis
K-means clustering was used to classify unweighted, unvaccinated participants into three clusters based on nine survey items related to behavioral and social drivers of COVID-19 vaccination, including four items assessing vaccine confidence (perceived importance, safety, information-seeking behavior, regret about not having a COVID-19 vaccine), two items assessing risk perception (concern about getting COVID-19, mask-wearing behavior), one item assessing social norms (e.g., vaccination status of friends and families) and two items assessing practical issues (e.g., availability, accessibility), as presented in Table 1 . The K-means model is an unsupervised machine learning algorithm that uses Euclidean distances and clusters observations with a standard iterative algorithm for minimizing the sum of squared distances from the cluster means (Wu, 2012). Once clusters were identified, weighted means of all nine BeSD items on behavioral and social drivers were compared among the four groups using a one-way ANOVA test. Statistical significance was set at α = 0.05. Because the large sample size of the study yielded small p-values (p < 0.01) for all one-way ANOVA tests, even those with relatively small differences among groups, the effect sizes (F-values) were reported in lieu of p-values when comparing the BeSD item means among groups. Descriptive analyses were performed using SUDAAN to compare demographic characteristics (e.g., sex, race/ethnicity, education, income, health conditions) between the vaccinated group (Cluster 0) and the three identified unvaccinated clusters (Cluster 1–3). Chi-square tests were performed to access categorical demographic differences among the four groups. The 95% confidence intervals were reported for both means and percentages and were used for pairwise comparisons.
Table 1.
Nine survey items used to assess behavioral and social drivers (BeSD) of COVID-19 vaccination, National Immunization Survey-Adult COVID Module, September 26–December 31,2021.
| BeSD items | Label | Value |
|---|---|---|
| Item 1: How concerned are you about getting COVID-19? | Not at all concerned A little concerned Moderately concerned Very concerned |
1 2 3 4 |
| Item 2: In the past 7 days, how often have you worn a mask when going into indoor public spaces like restaurants, stores, or other businesses? | Never or rarely Sometimes Often Always |
1 2 3 4 |
| Item 3: In the past month, how often have you tried to find information about COVID-19 vaccines? | Never Rarely Sometimes Often |
1 2 3 4 |
| Item 4: How much do you agree with the following statement: If I do not get a COVID-19 vaccine, I will regret it / if I had not gotten a COVID-19 vaccine, I would have regretted it. | Do not agree Somewhat agree Strongly agree Very strongly agree |
1 2 3 4 |
| Item 5: How safe do you think a COVID-19 vaccine is for you? | Not at all safe Somewhat safe Very safe Completely safe |
1 2 3 4 |
| Item 6: How important do you think getting a COVID-19 vaccine is to protect yourself against COVID-19? | Not at all important A little important Somewhat important Very important |
1 2 3 4 |
| Item 7: If you had to guess, about how many of your family and friends have received a COVID-19 vaccine? | None Some Many Almost all |
1 2 3 4 |
| Item 8: How difficult would it be for you / was it for you to get a COVID-19 vaccine? | Very difficult Somewhat difficult A little difficult Not at all difficult |
1 2 3 4 |
| Item 9: I can get a COVID-19 vaccine if I want to (asked only of unvaccinated respondents). | Do not agree Somewhat agree Strongly agree Very strongly agree |
1 2 3 4 |
The study was reviewed by Centers for Disease Control and Prevention (CDC) and conducted consistent with applicable federal law and CDC policy.
3. Results
Among all participants, 79.0% received at least one dose of COVID-19 vaccine. Based on participants' answers to the BeSD questions, K-means cluster analysis identified three distinct clusters within the unvaccinated adult population (labeled Clusters 1, 2, and 3), with 5406 (24.2%), 6242 (27.1%), and 11,749 (48.8%) participants, respectively.
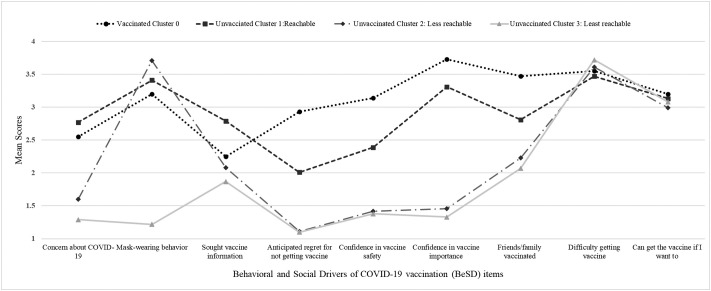
Table 2 and Fig. 1 present the comparison of the weighted means of the nine survey items on BeSD factors among the four clusters, including the vaccinated group (Cluster 0) and the three unvaccinated groups. The weighted percentages for the four clusters in the population were: 79.0% (Cluster 0), 5.1% (Cluster 1), 5.7% (Cluster 2), and 10.3% (Cluster 3). The minimum score for the nine survey items was 1 and the maximum score was 4, with all items scaled in the same direction such that higher numbers indicate greater vaccine confidence, greater COVID risk perception, more favorably perceived social norms towards COVID vaccine and fewer practical issues related to vaccine accessibility. Based on the distribution of means of the BeSD items between clusters, to facilitate interpretation of results, we labeled the Cluster 0 as “Vaccinated” group, Cluster 1 as unvaccinated “Reachable” group, Cluster 2 as unvaccinated “Less reachable” group, and Cluster 3 as unvaccinated “Least reachable” group.
Table 2.
Mean scores of responses to behavioral and social drivers of COVID-19 vaccination (BeSD) items among vaccinated and unvaccinated clusters, National Immunization Survey-Adult COVID Module, September 26–December 31,2021.
| Weighted percentage | Total1 (N= 186,845) |
Vaccinated cluster 0 (N = 163,448) |
Unvaccinated cluster 1: Reachable (N = 5406) |
Unvaccinated cluster 2: Less reachable (N = 6242) |
Unvaccinated cluster 3: Least reachable (N = 11,749) |
F-value |
|---|---|---|---|---|---|---|
| – |
78.99 (78.55–79.42) |
5.08 (4.84–5.32) |
5.68 (5.43–5.94) |
10.25 (9.93–10.58) |
– |
|
| Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | |||
| Item 1: Concern about COVID-19 (risk perception) | 2.38 (2.37–2.39) | 2.55 (2.54–2.56) | 2.77 (2.72–2.82) | 1.60 (1.56–1.64) | 1.29 (1.27–1.31) | 1562 |
| Item 2: Mask-wearing behavior | 3.04 (3.03–3.05) | 3.20 (3.19–3.21) | 3.41 (3.36–3.45) | 3.71 (3.69–3.73) | 1.22 (1.20–1.23) | 19,956 |
| Item 3: Sought vaccine information | 2.23 (2.22–2.24) | 2.25 (2.24–2.26) | 2.79 (2.74–2.85) | 2.08 (2.02–2.13) | 1.87 (1.83–1.91) | 356 |
| Item 4: Anticipated regret for not getting vaccine | 2.59 (2.58–2.61) | 2.93 (2.92–2.94) | 2.01 (1.96–2.06) | 1.11 (1.09–1.13) | 1.10 (1.09–1.12) | 589 |
| Item 5: Confidence in vaccine safety | 2.86 (2.85–2.87) | 3.14 (3.13–3.15) | 2.39 (2.34–2.43) | 1.42 (1.39–1.45) | 1.38 (1.36–1.41) | 804 |
| Item 6: Confidence in vaccine importance | 3.34 (3.33–3.35) | 3.73 (3.72–3.73) | 3.31 (3.28–3.35) | 1.46 (1.43–1.50) | 1.33 (1.31–1.36) | 4574 |
| Item 7: Friends/family vaccinated (social norms) | 3.22 (3.21–3.23) | 3.47 (3.46–3.47) | 2.81 (2.77–2.86) | 2.23 (2.20–2.27) | 2.07 (2.04–2.09) | 417 |
| Item 8: Difficulty getting vaccine | 3.56 (3.56–3.57) | 3.55 (3.54–3.56) | 3.47 (3.43–3.52) | 3.61 (3.57–3.65) | 3.72 (3.69–3.74) | 45 |
| Item 9: Can get the vaccine if I want to (self-efficacy) | 3.08 (3.06–3.10) | 3.20 (3.15–3.25) | 3.13 (3.09–3.17) | 2.99 (2.94–3.03) | 3.08 (3.05–3.11) | 11 |
Footnote 1: The original sample size was 187,756. However, 911 participants with incomplete data on COVID-19 vaccine status or BeSD items were excluded, leaving an analytic sample of 186,845.
Fig. 1.
Comparison of mean scores of responses to behavioral and social drivers of COVID-19 vaccination (BeSD) items among vaccinated and unvaccinated clusters, National Immunization Survey-Adult COVID Module, September 26–December 31,2021.
The vaccinated group and all unvaccinated clusters had high and relatively similar scores (smallest F-values/effect size among all BeSD items) regarding difficulty getting the vaccine (F-value = 45) and being able to get the vaccine if they wanted to (F-value = 11). The unvaccinated “Reachable” group (Cluster 1) reported the highest vaccine information seeking behavior among the four clusters (Fig. 1), and resembled the vaccinated cluster (differed by a mean of <0.50) in terms of perceived importance of the vaccine (mean = 3.73 for Cluster 0 “Vaccinated” vs mean = 3.31 for Cluster 1 “Reachable”) and concern about COVID-19 (mean = 2.55 for Cluster 0 “Vaccinated” vs mean = 2.77 for Cluster 1 “Reachable”). In comparison, the unvaccinated “Less reachable” group (Cluster 2) reported lower concern (mean = 1.60), and the unvaccinated “Least reachable” group (Cluster 3) reported the lowest concern (mean = 1.29) among the four groups. The unvaccinated “Less reachable” group (Cluster 2) reported highest mask frequency (mean = 3.71), while unvaccinated Cluster 3 reported lowest mask wearing behavior (mean = 1.22) among the four groups.
The unvaccinated “Reachable” group (Cluster 1) had lower scores than the vaccinated cluster for anticipated regret if one did not get the COVID-19 vaccine (mean = 2.93 for Cluster 0 “Vaccinated” vs mean = 2.01 for Cluster 1 “Reachable”), perceived vaccine safety (mean = 3.14 for Cluster 0 “Vaccinated” vs mean = 2.39 for Cluster 1 “Reachable”), and perceived family/friends vaccinated (mean = 3.47 for Cluster 0 “Vaccinated” vs mean = 2.81 for Cluster 1 “Reachable”). Compared with unvaccinated “Reachable” group (Cluster 1), unvaccinated “Less reachable” and “Least reachable” groups (Clusters 2 and 3) had similar lower mean values in the domains of anticipated regret if one did not get the COVID-19 vaccine (mean = 1.11 for Cluster 2 “Less reachable”, mean = 1.10 for Cluster 3 “Least reachable”) and perceived vaccine safety (mean = 1.42 for Cluster 2 “Less reachable”, mean = 1.38 for Cluster 3 “Least reachable”).
Table 3 presents data on willingness to be vaccinated across the three unvaccinated clusters. The “Reachable” group (Cluster 1) had the highest percentage of people who were willing to get vaccinated or unsure (53.0% reported probable/definite intent to get vaccinated, 28.2% were unsure, and 18.8% reported they probably/definitely would not get vaccinated). Compared with the “Reachable” group (Cluster 1), the “Less reachable” group (Cluster 2), had a lower percentage of adults who were willing to get vaccinated and a higher percentage with probable or no intent to get vaccinated (10.0% reported probable/definite intent to get vaccinated, 19.6% were unsure, 22.7% reported they probably would not get vaccinated, and 47.7% reported they definitely would not get vaccinated). The majority of the “Least reachable” group (Cluster 3), had no intent to get vaccinated (6.5% reported probable/definite intent to get vaccinated, 10.7% were unsure, 18.0% reported they probably would not get vaccinated, and 64.8% reported they definitely would not get vaccinated).
Table 3.
Reported intention to receive COVID-19 vaccine among the unvaccinated clusters, National Immunization Survey-Adult COVID Module, September 26–December 31,2021.
| Sample size (N) | Total (N = 23,397) |
Cluster 1: Reachable (n = 5406) |
Cluster 2: Less reachable (n = 6242) |
Cluster 3: Least reachable (n = 11,749) |
|
|---|---|---|---|---|---|
| Weighted percent (95% CI) | Weighted percent (95% CI) | Weighted percent (95% CI) | Weighted percent (95% CI) | ||
| Definitely plan to get vaccinated | 1817 | 8.1 (7.5–8.8) | 24.9 (22.9–27.1) | 3.1 (2.4–4.0) | 2.5 (2.1–3.1) |
| Probably will get vaccinated | 2303 | 10.6 (9.9–11.4) | 28.1 (25.9–30.4) | 6.9 (5.8–8.2) | 4.0 (3.4–4.8) |
| Unsure | 3940 | 17.3 (16.4–18.3) | 28.2 (26.1–30.5) | 19.6 (17.9–21.6) | 10.7 (9.6–11.8) |
| Probably will not get vaccinated | 3987 | 17.7 (16.8–18.7) | 11.7 (10.0–13.5) | 22.7 (20.7–24.8) | 18.0 (16.7–19.3) |
| Definitely will not get vaccinated | 11,131 | 46.2 (45.0–47.5) | 7.1 (5.9–8.6) | 47.7 (45.3–50.0) | 64.8 (63.1–66.4) |
Abbreviations: CI = confidence interval.
Detailed demographic characteristics of the three unvaccinated clusters and vaccinated participants are shown in Table 4 . Chi-square tests for all demographic characteristics yielded small p-values (p < 0.01) due to large sample size, thus p-values were not included in the Table 4. Compared with the unvaccinated groups, participants in the vaccinated group were more likely to have >12 years of education (34.4%), to report a health condition associated with high risk of COVID-19 (32.7%), to be insured (92.3%), to have a household income above $75,000 (46.9%), to live in metropolitan statistical area (MSA) principal and MSA non-principal areas (88.0%), to have received a vaccine other than COVID-19 in the past two years (64.5%), to report previously had COVID-19 (19%), to have received a COVID-19 vaccine recommendation from a HCP (46.9%), and to have a COVID-19 vaccine requirement at work or school (32.9%).
Table 4.
Demographic and other characteristics of vaccinated and unvaccinated clusters, National Immunization Survey-Adult COVID Module, September 26–December 31, 2021.
| Sample size (N) |
Totala (N = 186,845) |
Vaccinated Cluster 0 (n = 163,448) |
Unvaccinated Cluster 1: Reachable (n = 5406) |
Unvaccinated Cluster 2: Less reachable (n = 6242) |
Unvaccinated Cluster 3: Least reachable n = 11,749) |
|
|---|---|---|---|---|---|---|
| Weighted percent (95% CI) |
Weighted percent (95% CI) | Weighted percent (95% CI) | Weighted percent (95% CI) | Weighted percent (95% CI) |
||
| Age (mean) | 186,484 | 61.0 (59.9–62.2) | 63.1 (61.9–64.4) | 48.2 (43.3–53.1) | 53.7 (47.7–59.6) | 55.1 (51.0–59.2) |
| Gender | ||||||
| Male | 88,980 | 48.4 (47.9–48.9) | 47.1 (46.6–47.6) | 46.5 (44.0–48.9) | 46.2 (43.8–48.5) | 60.8 (59.1–62.4) |
| Female | 97,298 | 51.6 (51.1–52.1) | 52.9 (52.4–53.4) | 53.5 (51.1–56.0) | 53.8 (51.5–56.2) | 39.2 (37.6–40.9) |
| Age group | ||||||
| 18–24 | 16,749 | 12.4 (12.0–12.7) | 10.5 (10.2–10.8) | 22.4 (20.4–24.5) | 18.5 (16.7–20.4) | 18.2 (16.9–19.6) |
| 25–39 | 44,585 | 25.9 (25.5–26.3) | 22.4 (22.0–22.8) | 39.3 (36.9–41.8) | 40.9 (38.6–43.2) | 38.1 (36.4–39.8) |
| 40–49 | 28,960 | 16.0 (15.7–16.4) | 15.4 (15.0–15.7) | 16.4 (14.6–18.3) | 19.9 (18.0–21.8) | 18.9 (17.5–20.3) |
| 50–64 | 51,871 | 24.3 (23.9–24.7) | 26.1 (25.6–26.5) | 16.5 (14.8–18.4) | 15.5 (14.1–17.1) | 19.7 (18.4–21.0) |
| 65–74 | 29,117 | 12.7 (12.4–13.0) | 15.1 (14.7–15.5) | 3.7 (2.8–4.7) | 3.5 (2.8–4.4) | 3.4 (2.9–4.0) |
| 75+ | 13,351 | 8.7 (8.4–9.0) | 10.6 (10.2–10.9) | 1.8 (1.4–2.4) | 1.8 (1.3–2.4) | 1.8 (1.3–2.3) |
| Race/ethnicity | ||||||
| White, non-Hispanic | 118,476 | 62.2 (61.7–62.7) | 61.9 (61.4–62.4) | 45.9 (43.4–48.4) | 51.9 (49.5–54.3) | 78.3 (76.7–79.7) |
| Black, non-Hispanic | 21,238 | 11.9 (11.6–12.2) | 11.7 (11.4–12.0) | 22.7 (20.7–24.9) | 18.8 (17.1–20.6) | 4.0 (3.3–4.8) |
| Hispanic | 24,505 | 17.2 (16.8–17.6) | 17.5 (17.1–17.9) | 23.7 (21.6–25.8) | 19.2 (17.3–21.2) | 10.7 (9.6–11.9) |
| Other | 18,239 | 8.7 (8.4–9.0) | 8.9 (8.6–9.1) | 7.7 (6.5–9.1) | 10.1 (8.6–11.8) | 7.0 (6.2–8.0) |
| Education | ||||||
| Less than high school (< 12 years) | 45,503 | 39.0 (38.5–39.5) | 35.9 (35.4–36.4) | 53.5 (51.0–56.0) | 51.5 (49.1–53.8) | 48.7 (47.0–50.5) |
| High school (=12 years) | 52,073 | 30.6 (30.2–31.1) | 29.7 (29.2–30.2) | 33.1 (30.8–35.6) | 34.4 (32.2–36.7) | 34.4 (32.9–36.1) |
| Some college | 47,486 | 19.2 (18.8–19.5) | 21.1 (20.7–21.5) | 10.2 (9.0–11.7) | 10.7 (9.4–12.1) | 13.5 (12.4–14.7) |
| College graduate | 37,414 | 11.2 (11.0–11.5) | 13.3 (13.0–13.6) | 3.1 (2.4–4.1) | 3.4 (2.8–4.3) | 3.4 (2.9–3.9) |
| Health conditions associated with high risk of COVID-19b | ||||||
| With health conditions | 56,614 | 29.5 (29.1–29.9) | 32.7 (32.2–33.2) | 23.9 (21.8–26.1) | 18.1 (16.3–20.0) | 13.7 (12.7–14.9) |
| No health conditions | 127,850 | 70.5 (70.1–70.9) | 67.3 (66.8–67.8) | 76.1 (73.9–78.2) | 81.9 (80.0–83.7) | 86.3 (85.1–87.3) |
| Disabilitiesc | ||||||
| Disabilities | 17,237 | 9.8 (9.5–10.1) | 10.0 (9.7–10.4) | 13.3 (11.8–15.0) | 8.0 (6.9–9.2) | 7.2 (6.3–8.2) |
| No disabilities | 169,999 | 90.2 (89.9–90.5) | 90.0 (89.6–90.3) | 86.7 (85.0–88.2) | 92.0 (90.8–93.1) | 92.8 (91.8–93.7) |
| Health insurance | ||||||
| Insurance | 168,303 | 89.9 (89.6–90.2) | 92.3 (92.0–92.6) | 78.8 (76.7–80.8) | 80.9 (78.9–82.8) | 81.7 (80.2–83.0) |
| No insurance | 14,179 | 10.1 (9.8–10.4) | 7.7 (7.4–8.0) | 21.2 (19.2–23.3) | 19.1 (17.2–21.1) | 18.3 (17.0–19.8) |
| Income | ||||||
| Below poverty | 16,765 | 14.1 (13.7–14.5) | 12.4 (12.0–12.8) | 30.1 (27.5–32.9) | 23.0 (20.7–25.4) | 14.2 (12.9–15.6) |
| Above poverty, <$75 k | 57,884 | 42.0 (41.4–42.5) | 40.7 (40.1–41.3) | 47.4 (44.5–50.3) | 48.1 (45.4–50.8) | 45.9 (43.9–47.8) |
| Above poverty, ≥75 k | 70,600 | 44.0 (43.4–44.5) | 46.9 (46.3–47.4) | 22.5 (20.1–25.0) | 28.9 (26.5–31.4) | 40.0 (38.1–41.9) |
| Social vulnerability index (SVI)d | ||||||
| Low SVI | 57,614 | 28.5 (28.1–28.9) | 29.1 (28.7–29.6) | 23.1 (20.9–25.5) | 21.2 (19.4–23.2) | 30.4 (28.8–32.1) |
| Moderate SVI | 60,610 | 39.3 (38.8–39.8) | 39.3 (38.8–39.8) | 38.8 (36.3–41.4) | 41.0 (38.6–43.5) | 38.3 (36.5–40.1) |
| High SVI | 46,949 | 32.2 (31.8–32.7) | 31.6 (31.1–32.1) | 38.1 (35.6–40.6) | 37.7 (35.4–40.1) | 31.3 (29.7–33.0) |
| Urbanicity | ||||||
| MSA, principal city | 64,886 | 32.9 (32.5–33.3) | 33.9 (33.4–34.4) | 36.0 (33.7–38.4) | 35.5 (33.2–37.8) | 22.2 (20.9–23.7) |
| MSA, non-principal city | 87,453 | 53.3 (52.9–53.8) | 54.1 (53.6–54.6) | 48.3 (45.8–50.7) | 48.8 (46.5–51.2) | 52.5 (50.8–54.2) |
| Non-MSA | 35,417 | 13.8 (13.5–14.1) | 12.0 (11.7–12.3) | 15.7 (14.0–17.5) | 15.7 (14.2–17.4) | 25.3 (23.8–26.7) |
| Received vaccine other than COVID-19 in past 2 years | ||||||
| Yes | 113,303 | 55.4 (54.9–55.9) | 64.5 (64.0–65.0) | 29.8 (27.5–32.1) | 19.8 (18.1–21.6) | 17.7 (16.5–19.0) |
| No | 73,286 | 44.6 (44.1–45.1) | 35.5 (35.0–36.0) | 70.2 (67.9–72.5) | 80.2 (78.4–81.9) | 82.3 (81.0–83.5) |
| Essential worker statuse | ||||||
| Essential worker | 58,244 | 30.7 (30.3–31.2) | 29.8 (29.3–30.3) | 30.0 (27.8–32.4) | 32.3 (30.2–34.6) | 37.2 (35.6–38.9) |
| Not essential worker | 126,075 | 69.3 (68.8–69.7) | 70.2 (69.7–70.7) | 70.0 (67.6–72.2) | 67.7 (65.4–69.8) | 62.8 (61.1–64.4) |
| Previous COVID-19 infection | ||||||
| Yes | 37,750 | 23.3 (22.9–23.8) | 19.0 (18.6–19.4) | 37.3 (34.9–39.8) | 36.5 (34.3–38.7) | 43.1 (41.4–44.8) |
| No | 147,607 | 76.7 (76.2–77.1) | 81.0 (80.6–81.4) | 62.7 (60.2–65.1) | 63.5 (61.3–65.7) | 56.9 (55.2–58.6) |
| Received healthcare provider (HCP) recommendation for COVID-19 vaccine | ||||||
| HCP recommendation | 84,920 | 43.7 (43.2–44.2) | 46.9 (46.4–47.4) | 42.0 (39.5–44.6) | 31.0 (29.0–33.2) | 26.9 (25.4–28.4) |
| No HCP recommendation | 100,797 | 56.3 (55.8–56.8) | 53.1 (52.6–53.6) | 58.0 (55.4–60.5) | 69.0 (66.8–71.0) | 73.1 (71.6–74.6) |
| Work or school vaccination requirement | ||||||
| Requirement | 48,997 | 27.3 (26.9–27.8) | 32.9 (32.4–33.4) | 12.7 (11.1–14.4) | 8.1 (6.8–9.6) | 6.1 (5.2–7.1) |
| No requirement | 109,987 | 72.7 (72.2–73.1) | 67.1 (66.6–67.6) | 87.3 (85.6–88.9) | 91.9 (90.4–93.2) | 93.9 (92.9–94.8) |
The original sample size was 187,756. However, 911 participants with incomplete data on COVID-19 vaccine status or BeSD items were excluded, leaving an analytic sample of 186,845.
Health conditions associated with high risk of COVID-19 include cancer, liver disease, overweight, pregnancy, sickle cell disease, smoking, organ or blood transplant, stroke or cerebrovascular disease, substance use disorders, chronic kidney disease, chronic lung disease, dementia or other neurological condition, diabetes, down syndrome, health conditions, HIV infection, immunocompromised state, and others.
Disability was defined as having serious difficulty seeing, hearing, walking, remembering, making decisions, or communicating.
SVI was categorized as low, moderate, or high based on county of residence using tertiles of SVI score as cut-points. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
Essential workers were defined as first responders, frontline or essential workers who work at locations or settings such as healthcare, social service, preschool or daycare, K-12 schools, death care, correctional facilities, food and beverage stores, food manufacturing facilities, agriculture, forestry, fishing or hunting, and others.
The unvaccinated “Reachable” group (Cluster 1) reported the highest percentage of respondents who were non-Hispanic Black (22.7%) and Hispanic (23.7%), and who lived below the poverty level (30.1%). Compared with the other two unvaccinated clusters, the unvaccinated “Reachable” group (Cluster 1) reported higher percentage of health conditions (23.9%) and disability (13.3%), as well as a higher proportion who had received a non-COVID-19 vaccine in the past 2 years (29.8%). By contrast, respondents of the unvaccinated “Least reachable” group (Cluster 3) had the highest average age among the three unvaccinated clusters (mean = 55.1), and were more likely to be male (60.8%), non-Hispanic White (78.3%), employed as essential workers (37.2%), have previously had COVID-19 (43.1%), report no health conditions (86.3%), from non-MSAs (25.3%), have not received any other vaccines in the past two years (82.3%), and not have received a recommendation for COVID-19 vaccine from a healthcare provider (73.1%). Unvaccinated “Reachable” group (Cluster 1) was more likely than the other two unvaccinated clusters to have received a provider recommendation for COVID-19 vaccination (42.0% compared with 31.0% and 26.9% for clusters 2 and 3, respectively).
4. Discussion
Identifying different subgroups within the unvaccinated population and understanding the characteristics and social and behavioral factors of COVID-19 vaccine can help to differentiate those who may be more responsive to messaging about COVID-19 vaccines. In the present study, we examined the social and behavioral drivers of COVID-19 vaccination and provided machine-learning generated (i.e., predicted by the data rather than explicitly specified by a programmer) clusters based on behavioral and social factors of the sub-populations who are not vaccinated. Public health practitioners, health care providers, and jurisdictions can use these findings to tailor messaging, and the findings also may be useful to decisionmakers exploring policy options to increase vaccine uptake. We found that the clusters formed using the behavioral and social drivers of vaccine uptake also clearly separated unvaccinated persons by levels of intent to get vaccinated, providing support for the usefulness of the BeSD framework (Wolter et al., 2017).
The four clusters had very similar scores on the marker of COVID-19 vaccine accessibility, all having high agreement with the statement “I can get the vaccine if I want to” and low perceived difficulty getting the COVID-19 vaccine. This suggests that practical issues obtaining access to the COVID-19 vaccine were not perceived as a major barrier for COVID-19 primary series vaccination among most adults in the United States during September to December 2021.
The unvaccinated “Reachable” group (Cluster 1) was similar to the vaccinated group in terms of concern about COVID-19 and believing the vaccine is important. However, they were less likely to perceive the vaccine as safe, to express regret for not getting vaccinated, and to have vaccinated friends and family, suggesting vaccination is less of a social norm for this group. This reachable group also had the highest vaccine information seeking behavior scores of all clusters, suggesting that the reachable group may be receptive to information on vaccine safety and effectiveness and shared personal experiences from friends and family who received the vaccine. Previous research has found that vaccination of friends and family or a prestigious expert scientist/president/politician could potentially lower vaccine hesitancy (Salali and Uysal, 2021). Tailored efforts can help promote vaccine confidence and increase community level COVID-19 vaccine education and information distribution (e.g., selecting vaccine ambassadors) and may help to reduce misinformation (Clay et al., 2021; Nguyen et al., 2022; Quinn et al., 2017). Providing information regarding COVID-19 vaccine safety and effectiveness through trusted channels in accessible formats using plain language offers alternatives that may be a safeguard from mis- and disinformation, especially among populations with limited health literacy (Turhan et al., 2022). Engaging healthcare providers and community leaders to highlight the safety and effectiveness of the COVID-19 vaccine could be effective strategies in this cluster (Clay et al., 2021).
This “Reachable” cluster differs from the “Less reachable” and the vaccinated clusters not only by BeSD factors, but also socio-demographically: the “Reachable” cluster has the highest percentage of non-Hispanic Black and Hispanic participants and the highest percentage of respondents below the poverty level among the four groups and had a higher proportion of respondents living in the most socially vulnerable areas (highest social vulnerability index scores) than the vaccinated group. Our study reinforced previous research that non-Hispanic Black and Hispanic persons and persons with lower income and who live in socially vulnerable or rural areas had higher COVID-19 vaccine hesitancy (DiRago et al., 2022; Litaker et al., 2021; Momplaisir et al., 2021). Acknowledging the role of structural barriers to healthcare (e.g., transportation, wait time, co-payments) and their contribution to vaccine hesitancy, misinformation, and distrust of healthcare can help form and craft messaging around promoting vaccine confidence in this group (Bogart et al., 2021; Freed et al., 2013; Rusoja and Thomas, 2021; Yearby et al., 2022).
The vaccinated group reported the highest percentage of receipt of a recommendation for vaccination from a healthcare provider (HCP), reinforcing the association of a provider recommendation with vaccine uptake (Nguyen et al., 2021). While lower than the vaccinated, the reachable cluster was more likely to report receipt of a HCP recommendation than other unvaccinated clusters, suggesting that HCP recommendations might be effective in encouraging less reachable persons to become more amenable to COVID-19 vaccination. HCP recommendations remain one of the most effective ways to increase vaccination uptake, especially among vaccine hesitant persons (Mazor and Fisher, 2021; Rhodes et al., 2020; Wang and Liu, 2021). It is critical for HCPs to be equipped with information on vaccine efficacy and safety, including the most current guidelines, acknowledging patients' concerns about COVID-19 vaccines, practicing respectful engagement and patient empowerment, and using motivational interviewing techniques (Brewer et al., 2017; Lin et al., 2021; Opel et al., 2015; Rutten et al., 2021).
In contrast to the Cluster 1 (the “Reachable”), where just over 50% of respondents expressed a definite or probable intent to get vaccinated, Clusters 2 (the “Less reachable”) and 3 (the “Least reachable”) had very low proportions of respondents who intended to receive a COVID-19 vaccine. While the “Less reachable” and “Least reachable” groups had similar BeSD scores on most domains, they differed for mask-wearing behavior, with the “Less reachable” group having the highest score of all clusters and the “Least reachable” group reporting very low mask frequency. This suggests that the “Less reachable” cluster, although reporting low concern about COVID-19, still adhered to other COVID-19 mitigation policies. Although school or work requirements for COVID-19 vaccination were reported by only a small proportion of Cluster 2, vaccination policies, mandates, and requirements at different population levels (e.g., state, local, organizational) have been shown to be very effective in increasing vaccination coverage (Cataldi et al., 2020; Gostin, 2021).
The “Least reachable” group (Cluster 3) expressed the lowest intent to be vaccinated: 65% reported that they definitely would not get a COVID-19 vaccine. This group had the highest percentage of persons who were White males, from non-MSA areas, have previously had COVID-19, and reported they did not receive non-COVID vaccines. The average age of the “Least reachable” group was the highest of the three unvaccinated clusters. These findings align with previous research and ongoing Kaiser Family Foundation survey findings, which have shown that respondents who are White, living in rural areas, and identify as Republican were consistently the most likely to report that they definitely will not get a COVID-19 vaccine (Alcendor, 2021; Kaiser Family Foundation, 2022). The “Least reachable” group also comprises the largest percentage of the population who remained unvaccinated, suggesting that after eight months of the U.S. COVID-19 vaccination program (until the study period), the majority of people willing to be vaccinated had done so.
Previous literature supports that individuals who do not believe COVID-19 exists were found less likely to install contact-tracing apps, undertake health protective behaviors, get tested and vaccinated against COVID-19, and were more likely to report not supporting mask use, social distancing, or COVID-19 vaccines (Juanchich et al., 2021; Taylor and Asmundson, 2021; Zajenkowska et al., 2021). Previous research has found limited effect of health messaging in this population (Lin et al., 2021). Using messages and narratives that align with individuals' core values may shift certain views on preventive behaviors (e.g., DeMora et al. found that health protective behavioral information embedded within religious or patriotic messages may encourage mask use among White evangelical Christians), and alternative strategies and techniques for health communication (e.g., using narratives or stories that highlight personal choice, and using reactance to strengthen the message, such as “You have a right to get vaccinated to stay safe. Don't let anyone take away your right”) may be effective for increasing vaccination intent among the “Least reachable” group (DeMora et al., 2021; Taylor and Asmundson, 2021).
The findings in this study are subject to several limitations. First, response rates were low (approximately 20%), but are consistent with other National Immunization Surveys and other surveys using RDD (Centers for Disease Control and Prevention, 2022b; Pew Research Center, 2017). Adjustments and weighting methods were used to reduce bias and errors (e.g., noncoverage, nonresponse, measurement, sampling) in estimators of vaccine coverage. However, errors in estimates might remain after weighting for household nonresponse and incomplete sample frame (households with only landline or no telephone service were excluded). Second, vaccination receipt was self-reported and subject to recall and misclassification bias. However, survey weights were calibrated to COVID-19 vaccine administration data to mitigate possible bias from incomplete sample frame, nonresponse, and misclassification of vaccination status. Third, we assumed that the relationship between behavioral and social drivers and vaccine uptake remained constant over the three-month data collection period. Clusters of unvaccinated persons may change over time and might vary if stratified by geographic area or sociodemographic characteristics.
5. Conclusions
In the present study, we presented the differences in social and behavioral factors of vaccination among adults unvaccinated for COVID-19 and provided a comprehensive profile of the sub-populations who may be willing but are not yet vaccinated, as well as those who are least reachable. Public health practitioners, healthcare providers and community leaders can use these characteristics to better tailor messaging for each sub-population. Our findings may also help inform decisionmakers exploring possible policy interventions.
Disclosure
The authors report no conflicts of interest. No funding was provided for this activity; all investigators were employed by their respective affiliated institutions.
CRediT authorship contribution statement
Lu Meng: Conceptualization, Methodology, Software, Writing – original draft. Nina B. Masters: Conceptualization, Writing – original draft. Peng-Jun Lu: Validation, Writing – review & editing. James A. Singleton: Supervision, Conceptualization, Methodology, Writing – review & editing. Jennifer L. Kriss: Writing – review & editing. Tianyi Zhou: Validation, Visualization. Debora Weiss: Writing – review & editing. Carla L. Black: Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
The authors do not have permission to share data.
References
- Alcendor D.J. Targeting COVID vaccine hesitancy in rural communities in Tennessee: implications for extending the COVID-19 pandemic in the south. Vaccines. 2021;9(11):1279. doi: 10.3390/vaccines9111279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart L.M., Ojikutu B.O., Tyagi K., Klein D.J., Mutchler M.G., Dong L., Lawrence S.J., Thomas D.R., Kellman S. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among Black Americans living with HIV. J. Acquir. Immune Defic. Syndr. (1999) 2021;86(2):200. doi: 10.1097/QAI.0000000000002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer N.T. What works to increase vaccination uptake. Acad. Pediatr. 2021;21(4):S9–S16. doi: 10.1016/j.acap.2021.01.017. [DOI] [PubMed] [Google Scholar]
- Brewer N.T., Chapman G.B., Rothman A.J., Leask J., Kempe A. Increasing vaccination: putting psychological science into action. Psychol. Sci. Public Interest. 2017;18(3):149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- Cataldi J.R., Kerns M.E., O’Leary S.T. Evidence-based strategies to increase vaccination uptake: a review. Curr. Opin. Pediatr. 2020;32(1):151–159. doi: 10.1097/MOP.0000000000000843. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention About COVID-19 Vaccine Delivered and Administration Data. 2022. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/distributing/about-vaccine-data.html Retrieved from.
- Centers for Disease Control and Prevention About the National Immunization Surveys (NIS) 2022. https://www.cdc.gov/vaccines/imz-managers/nis/about.html Retrieved from.
- Centers for Disease Control and Prevention COVID Data Tracker: COVID-19 Vaccinations in the United States. 2022. https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total Retrieved from.
- Centers for Disease Control and Prevention Stay Up to Date With Your COVID-19 Vaccines. 2022. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html#recommendations Retrieved from.
- Clay K., Hiller A., Hopkins R., Jacobs A., Janezko L., Hummer S.M., Ng C., Ramakrishnan A., Repetski T., Rodriguez L., Simpson R., Sorenson B., Weinstein N., Hopkins R., et al. COVID-19 Vaccination Field Guide:12 Strategies for Your Community. 2021. https://www.cdc.gov/vaccines/covid-19/downloads/vaccination-strategies.pdf Retrieved from.
- DeMora S.L., Merolla J.L., Newman B., Zechmeister E.J. Reducing mask resistance among white evangelical Christians with value-consistent messages. Proc. Natl. Acad. Sci. 2021;118(21) doi: 10.1073/pnas.2101723118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiRago N.V., Li M., Tom T., Schupmann W., Carrillo Y., Carey C.M., Gaddis S.M. COVID-19 vaccine rollouts and the reproduction of urban spatial inequality: disparities within large US cities in march and April 2021 by racial/ethnic and socioeconomic composition. J. Urban Health. 2022:1–17. doi: 10.1007/s11524-021-00589-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed C.R., Hansberry S.T., Arrieta M.I. Social Determinants, Health Disparities and Linkages to Health and Health Care. vol. 31. Emerald Group Publishing Limited; 2013. Structural and hidden barriers to a local primary health care infrastructure: autonomy, decisions about primary health care, and the centrality and significance of power; pp. 57–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostin L.O. Paper Presented at the JAMA Health Forum. 2021. COVID-19 vaccine mandates—A wider freedom. [DOI] [PubMed] [Google Scholar]
- Juanchich M., Sirota M., Jolles D., Whiley L.A. Are COVID-19 conspiracies a threat to public health? Psychological characteristics and health protective behaviours of believers. Eur. J. Soc. Psychol. 2021;51(6):969–989. doi: 10.1002/ejsp.2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation KFF COVID-19 Vaccine Monitor-An Ongoing Research Project Tracking the Public's Attitudes and Experiences with COVID-19 Vaccinations. 2022. https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/?utm_source=web&utm_medium=trending&utm_campaign=COVID-19-vaccine-monitor#politics Retrieved from.
- Khairat S., Zou B., Adler-Milstein J. Factors and reasons associated with low COVID-19 vaccine uptake among highly hesitant communities in the US. Am. J. Infect. Control. 2022;50(3):262–267. doi: 10.1016/j.ajic.2021.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C., Mullen J., Smith D., Kotarba M., Kaplan S.J., Tu P. Healthcare providers’ vaccine perceptions, hesitancy, and recommendation to patients: a systematic review. Vaccines. 2021;9(7):713. doi: 10.3390/vaccines9070713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litaker J.R., Tamez N., Lopez Bray C., Durkalski W., Taylor R. Sociodemographic factors associated with vaccine hesitancy in Central Texas immediately prior to COVID-19 vaccine availability. Int. J. Environ. Res. Public Health. 2021;19(1):368. doi: 10.3390/ijerph19010368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu P.J., Hung M.C., Jackson H.L., Kriss J.L., Srivastav A., Yankey D., Santibanez T.A., Lee J.T., Meng L., Razzaghi H., Black C.L. COVID-19 vaccination and intent for vaccination of adults with reported medical conditions. Am. J. Prev. Med. 2022;63(5):760–771. doi: 10.1016/j.amepre.2022.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazor K., Fisher K. A Direct Recommendation From a Doctor May be the Final Push Someone Needs to get Vaccinated. 2021. https://theconversation.com/a-direct-recommendation-from-a-doctor-may-be-the-final-push-someone-needs-to-get-vaccinated-165155 Retrieved from.
- Momplaisir F.M., Kuter B.J., Ghadimi F., Browne S., Nkwihoreze H., Feemster K.A., Frank I., Faig W., Shen A.K., Offit P.A., Green-McKenzie J. Racial/ethnic differences in COVID-19 vaccine hesitancy among health care workers in 2 large academic hospitals. JAMA Netw. Open. 2021;4(8):e2121931. doi: 10.1001/jamanetworkopen.2021.21931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L.H., Joshi A.D., Drew D.A., Merino J., Ma W., Lo C.H., Kwon S., Wang K., Graham M.S., Polidori L., Menni C., Sudre C.H., Anyane-Yeboa A., Astley C.M., Warner E.T., Hu C.Y., Selvachandran S., Davies R., Nash D., Franks P.W., Wolf J., Ourselin S., Steves C.J., Spector T.D., Chan A.T., COPE Consortium Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nat Commun. 2022;13(1):636. doi: 10.1038/s41467-022-28200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen K.H., Yankey D., Lu P.J., Kriss J.L., Brewer N.T., Razzaghi H., Meghani M., Manns B.J., Lee J.T., Singleton J.A. Report of health care provider recommendation for COVID-19 vaccination among adults, by recipient COVID-19 vaccination status and attitudes—United States, April–September 2021. Morb. Mortal. Wkly Rep. 2021;70(50):1723. doi: 10.15585/mmwr.mm7050a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel D.J., Mangione-Smith R., Robinson J.D., Heritage J., DeVere V., Salas H.S., Taylor J.A. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. Am. J. Public Health. 2015;105(10):1998–2004. doi: 10.2105/AJPH.2014.302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center What Low Response Rates Mean for Telephone Surveys. 2017. https://assets.pewresearch.org/wp-content/uploads/sites/12/2017/05/12154630/RDD-Non-response-Full-Report.pdf Retrieved from.
- Quinn S.C., Hilyard K.M., Jamison A.M., An J., Hancock G.R., Musa D., Freimuth V.S. The influence of social norms on flu vaccination among African American and white adults. Health Educ. Res. 2017;32(6):473–486. doi: 10.1093/her/cyx070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes M.E., Sundstrom B., Ritter E., McKeever B.W., McKeever R. Preparing for a COVID-19 vaccine: a mixed methods study of vaccine hesitant parents. J. Health Commun. 2020;25(10):831–837. doi: 10.1080/10810730.2021.1871986. [DOI] [PubMed] [Google Scholar]
- Rusoja E., Thomas B. The COVID-19 pandemic, Black mistrust, and a path forward. EClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten L.J.F., Zhu X., Leppin A.L., Ridgeway J.L., Swift M.D., Griffin J.M., Jacobson R.M. Paper Presented at the Mayo Clinic Proceedings. 2021. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelee R., Zell E., Murthy B.P., Castro-Roman P., Fast H., Meng L., Shaw L., Gibbs-Scharf L., Chorba T., Harris L.Q., Murthy N. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020–January 31, 2022. Morb. Mortal. Wkly Rep. 2022;71(9):335. doi: 10.15585/mmwr.mm7109a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salali G.D., Uysal M.S. Effective incentives for increasing COVID-19 vaccine uptake. Psychol. Med. 2021:1–3. doi: 10.1017/S0033291721004013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Asmundson G.J. Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turhan Z., Dilcen H.Y., Dolu İ. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr. Psychol. 2022:1–10. doi: 10.1007/s12144-021-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Liu Y. Multilevel determinants of COVID-19 vaccination hesitancy in the United States: a rapid systematic review. Prev. Med. Rep. 2021;101673 doi: 10.1016/j.pmedr.2021.101673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolter K.M., Smith P.J., Khare M., Welch B., Copeland K.R., Pineau V.J., Davis N. Statistical methodology of the national immunization survey, 2005-2014. National center for health statistics. Vital Health Stat. 2017;2022(Mar 28) https://www.cdc.gov/nchs/data/series/sr_01/sr01_061.pdf Retrieved from. [PubMed] [Google Scholar]
- Wu J. Advances in K-Means Clustering. Springer; 2012. Cluster analysis and K-means clustering: an introduction; pp. 1–16. [Google Scholar]
- Yearby R., Clark B., Figueroa J.F. Structural racism in historical and modern US health care policy: study examines structural racism in historical and modern US health care policy. Health Aff. 2022;41(2):187–194. doi: 10.1377/hlthaff.2021.01466. [DOI] [PubMed] [Google Scholar]
- Zajenkowska A., Nowakowska I., Bodecka-Zych M., Rajchert J., Kaźmierczak I., Jakubowska A., Pinkham A.E. Defense mechanisms and borderline personality organization among COVID-19 believers and non-believers during complete lock-down. Front. Psychiatr. 2021;1427 doi: 10.3389/fpsyt.2021.700774. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.