Abstract
Aims
This study explores experiences of childhood cancer survivors and their parents with a combined physical and social activity intervention during treatment, including how the survivors and their parents perceive physical activity post‐treatment.
Design
A process evaluation using semi‐structured interviews.
Methods
Using a criterion‐sampling strategy, 18 Danish childhood cancer survivors (aged 11–18 years) and their parents were interviewed from September 2019 through May 2020. Data analysis used an inductive thematic approach focused on meaning.
Results
Three themes emerged: (1) being physically active during hospitalization; (2) peers as motivators and (3) physical activity post‐treatment. During hospitalization, daily motivation to do physical activity was dependent on the daily well‐being, that is, presence of the side effects from the child's treatment. Healthy classmates provided distraction, reduced loneliness and promoted normality for those hospitalized. For most of the survivors, their healthy peers provided motivation for being physically active during treatment. When surplus energy was lacking, some survivors preferred doing physical activity alone with a professional. Those who were physically active in the hospital sustained being physically active post‐treatment while their parents continued seeking advice about appropriate activity levels.
Conclusion
Childhood cancer survivors and their parents benefited from the intervention which also provided guidance to remaining physically active post‐treatment. This was particularly true for the participants with leukaemia.
Impact
Healthcare professionals should support children with cancer to be physically active during hospitalization. Including social and physical components in their care plan and being aware of individual preferences is pivotal to improving the survivors' level of physical and social well‐being during and post‐treatment.
Patient or Public Contribution
The participants were involved in designing the interview guides to ensure that the interview guides were understandable for the participants to provide rich descriptions of their experiences with a physical and social activity intervention during hospitalization.
Keywords: cancer, childhood cancer survivors, nursing, parents, peer motivation, physical activity, psychosocial, qualitative study, transition
1. INTRODUCTION
The treatment for childhood cancer is often intense and can cause muscle strength loss, impaired physical function and behavioural problems (Braam et al., 2016; Ness et al., 2015; Nielsen et al., 2020). Moreover, the treatment often requires long and recurring hospitalizations resulting in prolonged absences from school and a dramatic reduction in peer interactions (Helms et al., 2016; Warner et al., 2016). The combination of being physically impaired, school absence and lacking peer interactions can negatively impact quality of life for the child with cancer (Germain et al., 2019). Identifying potential facilitators and barriers for physical activity during cancer treatment is pivotal to countering physical inactivity post‐treatment (Grimshaw et al., 2020; Thorsteinsson et al., 2017). According to the Medical Research Council's (MRC) guidance for complex interventions, process evaluation can be useful when investigating how the intended audience is impacted by the intervention (Moore et al., 2015). In this study, process evaluation was conducted after the childhood cancer survivors had participated in the intervention to understand how they perceived and experienced the intervention.
1.1. Background
Refined treatment for childhood cancer has positively impacted the 5‐year cancer survival rates (Armstrong et al., 2014). As survival rates improve, however, minimizing treatment late effects comes to the forefront of promoting long‐term health and development for these survivors (Barrett et al., 2020; Schmiegelow & Frandsen, 2018). Regular physical activity is beneficial for children with cancer both physically and socially as it can ward off treatment‐related fatigue and depression by stimulating endorphins (Speyer et al., 2010).
Research has shown that parents and peers are pivotal motivators for children and adolescents to undertake physical activity as they can offer emotional support and establish routines during cancer treatment (Thorsteinsson et al., 2019; Zecevic et al., 2010). However, various barriers to physical activity in childhood cancer exist. Parents of these survivors point to the following contributing barriers during treatment: treatment side effects, restricted movement, loss of independence, isolation and low motivation (Grimshaw et al., 2020). Cancer treatment is often also described as stressful for both the child and his/her parents due to feeling overwhelmed by the cancer diagnosis, having to keep abreast of various medical appointments, and not least focusing on recovery (Beeler et al., 2021; Götte et al., 2014). All this may not allow parents to prioritize physical activity during treatment. The parents themselves can also be considered as potential barriers; for example, when they dismiss the importance of physical activity rehabilitation or when they fail to motivate their child to be physically active post‐treatment (Cheung et al., 2021; Wakefield et al., 2011). Parents may also be unaware of the importance of being physically active as a childhood cancer survivor (Cheung et al., 2021; Mizrahi et al., 2020). Earlier studies report that the combination of cancer treatment and reduced peer interaction during treatment affect the cancer survivors' ability and desire to be physically active and ultimately lowers the child's health‐related quality of life post‐treatment (Ness et al., 2009; Vannatta et al., 2007). Thus, to target and ameliorate their impaired physical, social and academic functioning, a multimodal intervention was designed for implementation during the children's cancer treatment. The intervention included in‐hospital supervised physical activity combined with co‐admission days by healthy classmates as the link between the hospital and the child's school peer group (Nielsen et al., 2020; Thorsteinsson et al., 2013).
2. THE STUDY
2.1. Aims
This study explores experiences of childhood cancer survivors and their parents with a physical and social activity intervention during cancer treatment, including how the survivors and their parents perceive physical activity post‐treatment.
2.2. Design
We designed a qualitative descriptive study using in‐depth semi‐structured interviews. Qualitative description research offers the opportunity to gather direct rich descriptions of the phenomena of interest from the people involved (Bradshaw et al., 2017). In health care research, this methodology is often used to learn from the descriptions gained from the participants. The knowledge gained from the participants' descriptions can be used to influence interventions (Sullivan‐Bolyai et al., 2005). The qualitative descriptive design offered detailed descriptions of the intervention during cancer treatment from the involved participants. The knowledge gained from the participants' descriptions can be used to design future physical and social activity interventions.
2.3. Setting
The study is embedded in the REhabilitation including Social and Physical Activity and Education in Children and Teenagers with Cancer (RESPECT) Study. RESPECT is a Danish nationwide, controlled rehabilitation study initiated in 2013, that includes children with cancer aged 6–18 years. Its purpose is to examine the academic, social and physical rehabilitation of children with cancer throughout the treatment trajectory and is embedded in the work structure of the Center for Integrated Rehabilitation of Cancer Patients (CIRE) programme (Adamsen et al., 2020).
2.4. Intervention components
The intervention included three components; (1) an educational session on cancer and cancer treatment; (2) visits by classmates (“ambassadors”) during hospitalization and (3) supervised in‐hospital physical activity. A full description of the components is available in previous articles from the RESPECT study (Lindgren et al., 2017; Nielsen et al., 2020; Thorsteinsson et al., 2013). The intensity of the programme has been published elsewhere (Thorsteinsson et al., 2017).
When feasible, the child with cancer participated in a supervised in‐hospital physical activity intervention (the RESPECT physical activity programme) (Nielsen et al., 2020). This programme consisted of various tailored physical activities, that is, game‐based activity, walking, running, endurance and strength building. The individual sessions were 5–30 min whereas the group sessions were 30–120 min. The group sessions included all admitted children and their ambassadors. Physical activity sessions were held either in the child's hospital room or at a nearby gym (Nielsen et al., 2020). The sessions were led by two exercise professionals associated with the RESPECT Study. Each session was designed to consider the child's daily well‐being status (i.e. presence of nausea, pain, dizziness or other treatment side effects) and physical capability and as such the intensity of the sessions was individualized. See Table 1 for RESPECT activity programme details.
TABLE 1.
The in‐hospital RESPECT activity programme. From Nielsen et al. (2020)
| Weekday | Monday | Tuesday | Wednesday | Thursday | Friday | Weekends |
|---|---|---|---|---|---|---|
| Ambassador visits | Planning ambassador visit | Ambassador visit | Planning ambassador visit | Ambassador visit | No ambassador activity | No ambassador activity |
| Training | Training | Training | Training | Training | Training | No training |
| Able to walk/not isolated |
Individual session 5–30 min Cardiorespiratory fitness Muscle strength Balance |
Group session with the ambassadors 30–120 min Cardiorespiratory fitness Muscle strength Balance |
Individual session 5–30 min Cardiorespiratory fitness Muscle strength Balance |
Group session with the ambassadors 30–120 min Cardiorespiratory fitness Muscle strength Balance |
Individual session 5–30 min Cardiorespiratory fitness Muscle strength Balance |
No training |
| Able to walk/isolated |
Individual session 5–30 min Cardiorespiratory fitness Muscle strength Balance |
Individual session with the ambassadors 5–30 min Cardiorespiratory fitness Muscle strength Balance |
Individual session 5–30 min Cardiorespiratory fitness Muscle strength Balance |
Individual session with the ambassadors 5–30 min Cardiorespiratory fitness Muscle strength Balance |
Individual session 5–30 min Cardiorespiratory fitness Muscle strength Balance |
No training |
| Bedridden |
Individual session 5–30 min Muscle strength |
Individual session with the ambassadors 5–30 min Muscle strength |
Individual session 5–30 min Muscle strength |
Individual session with the ambassadors 5–30 min Muscle strength |
Individual session 5–30 min Muscle strength |
No training |
2.5. Sample/participants
A criterion‐based sampling strategy was used to select participants from the RESPECT cohort (n = 120). Participants were sampled in dyads (survivors with their parents) and as such selection was based on the dyads that matched the inclusion criteria. If matches were identified, parents of the matched children were contacted by the project nurse either by mail or telephone. Participants were found eligible if the cancer survivor: (1) was between the age of 9–18 years at the time of the interview; (2) was at least 1‐year post‐treatment and (3) had been enrolled in the RESPECT Study's intervention group during treatment. Exclusion criteria were the inability to speak Danish, presence of cognitive dysfunction or mental retardation. As we wanted to gain insight into the participants' descriptions of their participation in the RESPECT physical activity intervention, a conscious attempt was made to include childhood cancer survivors who had required long treatment episodes as they would have had more exposure to the physical and social impacts of treatment. The childhood cancer survivors included in the study were diagnosed with: tumours located in the central nervous system (n = 1); leukaemia (n = 11); extracranial solid tumour (n = 3); Hodgkin's lymphoma (n = 1) and non‐Hodgkin's lymphoma (n = 2). See Table 2 for participant characteristics. Twenty childhood cancer survivors were asked to participate in the interviews. As the sampling was done in dyads, two childhood cancer survivors declined as their parents' unwillingness to participate in the study. In total, 18 childhood cancer survivors (8 females; 10 males) aged 11–18 years (mean = 14) and 19 parents (14 mothers; 5 fathers) participated in the study. In one parent interview, two parents participated. In total, 36 interviews were conducted. All survivors participating in this study had been enrolled in the RESPECT physical activity programme during treatment. The recruitment process is described in Figure 1.
TABLE 2.
Participant demographics
| Childhood cancer survivors (n = 18) | Ambassadors (n = 36) | |
|---|---|---|
| Gender | ||
| Male | 10 | 20 |
| Female | 8 | 16 |
| Type of cancer | ||
| Leukaemia | 11 | |
| Central nervous system tumour | 1 | |
| Extracranial solid tumours | 3 | |
| Hodgkin lymphoma | 1 | |
| Non‐Hodgkin lymphoma | 2 | |
| Age | ||
| Age at time of diagnosis (years) | 10.5 (6–16) | 10.5 (6–16) |
| Age at time of data collection (years) | 13.5 (11–18) | |
| Length of treatment period (days) | (120–1059) | |
| Years after ended treatment | 2.5 (1–5) | |
| In hospital stays (days) | 125 (47–188) | |
| Training sessions | 35 (9–66) | |
| Ambassador co‐admissions (n) | 11 (6–26) | |
| Parents (n = 19) | |
|---|---|
| Mothers | 14 |
| Fathers | 5 |
| Married/in a relationship | 15 |
| Working full‐time | 17 |
| Working part‐time | 2 |
| Education | |
| Less than 9th grade | 1 |
| 9th grade or 10th grade | |
| Highschool | |
| Vocational education | 3 |
| Short‐cycle tertiary education (below 3 years) | 2 |
| Bachelor's or equivalent education (3–4 years) | 9 |
| Master's or equivalent education (5 years and above) | 3 |
| Doctoral or equivalent level | |
Note: Age is presented in median and (range). Length of treatment is presented in (range). Years after ended treatment, in‐hospital stays, training sessions and ambassador co‐admissions are presented in median and (range).
FIGURE 1.
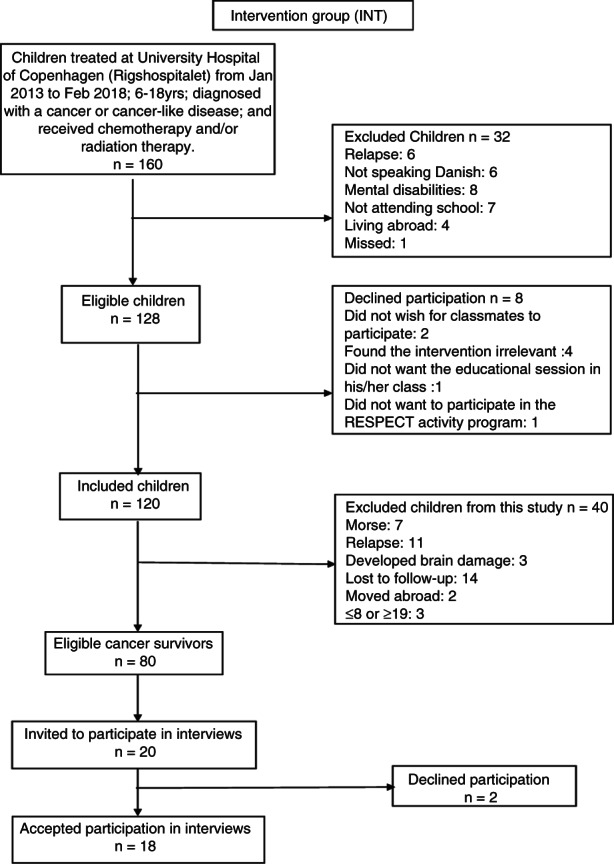
Recruitment process
2.6. Data collection
This study does not include data from the experiences of the classroom educational sessions on cancer as this aspect has been highlighted in earlier articles from the RESPECT Study (Ingersgaard et al., 2021; Lindgren et al., 2017; Thorsteinsson et al., 2013). Rather, the current study focuses on the physical and social aspects of RESPECT.
Two semi‐structured interview guides were developed, that is, one for the childhood cancer survivors and another for the parents. The interview guides were designed to elicit participant experiences on the following themes: (1) overall perception of RESPECT; (2) physical activity a component of the hospitalization care plan; (3) physical activity in general; (4) knowledge gained from the intervention programme and (5) physical activity post‐treatment. Open‐ended questions were raised to encourage participants to reflect on their experiences (Bradshaw et al., 2017). The interviewer (NNP) had not previously been involved with the RESPECT Study, thus ensuring that participants were able to express themselves freely. Participants were interviewed individually in person, once from September 2019 through May 2020. The childhood cancer survivors were interviewed separately from their parents. Interviewers were conducted: in the participant's home (n = 26) or in a private room at the hospital (n = 10), depending on the participant's preference. The duration of the interviews ranged from 13 to 65 min (mean: 32 min) and were audio‐recorded and transcribed ad verbatim.
2.7. Ethical considerations
The Regional Ethics Committee for the Capital Region (file. 3‐2012‐105) and the Danish Data Protection Agency (file. 2007‐58‐0015/nr.30‐0734) approved the RESPECT Study. RESPECT is registered at ClinicalTrials.gov (files: NCT01772849 and NCT01772862) and complies with the Helsinki II Declaration norms and subsequent amendments. Parents of children under the age of 16 gave verbal and written consent as did the adolescents aged 16 years and above. All participants were informed of their right to withdraw from the study at any time.
2.8. Data analysis
The transcripts were analysed and discussed by first authors NNP and HBL. An inductive thematic analysis focusing on meaning was used (Clarke et al., 2015).
The data were organized and coded using NVivo 12 coding software. The thematic analysis included the following steps: (1) the transcripts were read repeatedly until NNP gained an in‐depth understanding of the content; (2) all transcripts data were initially coded and later assigned meaning units agreed upon between the first authors NNP and HBL; (3) the meaning units were then analysed and reassembled into themes; (4) the themes were reviewed to ensure that all the coded data was included, after which the themes were examined in relation to the entire dataset to ensure that the analysis represented the entire body of data and (5) the themes and names were finalized and all authors agreed on their ultimate selection. The authors experienced minor disagreements about wordings and how findings should be presented. However, these were resolved through compromise and agreement of highest credibility selections.
2.9. Rigour
To ensure trustworthiness of this study, we used Bradshaw et al. and their demonstration of four principles for trustworthiness in qualitative descriptive research (Bradshaw et al., 2017). Their four principles stemmed from Lincoln and Guba's four principles (credibility; dependability; confirmability; and transferability) for trustworthiness in qualitative research (Lincoln & Guba, 1986). To ensure transferability, we purposefully sampled participants with mixed sex, varying ages of the survivors, and included their parents. Furthermore, sampling was done following in‐hospital‐based treatment days. All contributed to rich descriptions of the intervention. To strengthen the data credibility, we used an independent interviewer and semi‐structured interviews with open‐ended questions to offer the opportunity for participants to elaborate on issues vital to them within and beyond the pre‐determined themes. To ensure the confirmability of this study, the interviews were audio‐recorded and description of demographics of the participants were provided (Table 2). A native‐speaking medical writer compared the English version with the Danish version to ensure translation accuracy and that all concepts were captured correctly and were accurately interpreted across languages. All authors approved all translations.
3. FINDINGS
The study participants included 18 childhood cancer survivors (n = 56% males) aged 11–18 years (age median = 14) and their parents (n = 19). The survivors had completed their treatment between 1 and 5 years prior to being interviewed. Inductive analysis of the dyads' (survivors and their parents) experiences resulted in following themes: (1) being physically active during hospitalization; (2) peers as motivators and (3) physical activity post‐treatment. The themes captured insights into how the dyads experienced the RESPECT Study's physical activity programme and perceived physical activity post‐treatment.
3.1. Being physically active during hospitalization
Overall, the hospital‐based physical activity programme was found to be favourable to both the children and parents, who described it as a positive learning experience, a huge support during treatment and motivational for engaging in further physical activity during and post‐treatment. Most of the survivors (n = 15) stated that they had participated in the physical activity sessions whenever they were not significantly affected by treatment side effects. Some survivors (n = 4) found the sessions challenging and exhausting due to the treatment's impact on their body, that is, breathlessness when walking the hallway, feeling fatigued or nauseous.
In contrast, five survivors informed that they could have done more physical activity and that the sessions were not challenging enough. Although all the survivors (n = 18) had participated in the sessions during their hospitalization, three of them could only vaguely recall being physically active. These three survivors remembered walking the hallways or from their bed to their hospital room door, but they did not associate that with being physically active. The survivors agreed, however, that the sessions were a good diversion while in the hospital. One girl explained:
It [physical activity] was hard but it was very nice to get up and move around because, otherwise, you didn't get much of a chance (Female, aged 13 years)
Although most of the survivors (n = 16) and their parents (n = 16) had an overall positive view of the RESPECT physical activity programme, few of the survivors (n = 2) and their parents (n = 2) reported negative experiences. Three survivors described intermittently feeling too ill to participate, which proved demotivating for them. One boy explained:
I was in bad shape. I was sick even before he [the physical activity professional] came to ask me to participate, and I know that I'd be more ill if I went with him. So, there was no real bonus in it for me to go. (Male, aged 13 years)
From the parents' perspective, the RESPECT physical activity programme could have offered more individual sessions. As one mother explained:
I would have liked to have seen more individual training for him while we were there [in hospital]. Perhaps also because he [the child] became more withdrawn whenever other kid participated. (Mother to 16 years‐old male)
Few survivors (n = 3) described not wanting to participate in group sessions as they lacked the surplus energy. They would have preferred using the physical activity professionals as personal trainers at those times. Their parents (n = 3) felt that the professionals did not motivate their child enough during the sessions, which resulted in the child not fully benefiting from the programme. As one mother explained:
I think they [the physical activity professionals] could have pushed her more. They didn't need to leave it up to them [the children] to [decide to] participate. They could have just told her it was a part of being in RESPECT.” (Mother to 12‐year‐old female)
The parents (n = 3) were unsure whether their child's participation in the intervention had any impact on their child being physically active during treatment or during the first‐year post‐treatment. However, most of the survivors (n = 14) explained that they continued be physically active afterwards. Some survivors (n = 4) did not resume the same physical activities as prior to their diagnosis but instead found new ones, that is, horseback riding, badminton and swimming. Most of the survivors (n = 15) and their parents (n = 15) experienced that the survivors were unafraid of being physically active post‐treatment. The parents (n = 15) described the survivors as having developed a different perspective of physical activity because they were physically active during treatment.
3.2. Peers as motivators
Most of survivors (n = 16) and their parents (n = 16) agreed that using classmates as ambassadors offered emotional support during hospitalization. Ambassador actions during visits included combatting the child's feelings of isolation from school and their social networks as well as deviating their focus away from the cancer experience and towards a sense of normality. Most of the survivors (n = 15) were more motivated to get out of bed during ambassador visits. As one boy explained:
I liked it. Having your friends visit and staying in touch with your class. But it was more the fact that it was an escape from just being in the hospital. And the part about working outs was also nice because you could do it with those you knew. (Male, aged 18 years)
The dyads (n = 31) agreed that physical and social activities tended to merge as the ambassadors, who provided a social dimension, also participated in the physical activity sessions alongside the survivors. As one mother described:
[…] his ambassadors did the same exercises as he did, and he could see that he was lagging a bit behind them […], that they always did a bit more than he could. He was eager to come in first place every time, so he pushed himself to do the same exercises as they did. (Mother to 14‐year‐old male)
However, two survivors declined having ambassadors as their treatment occurred during the summer school break. Although the survivors (n = 15) and their parents (n = 16) agreed that the ambassadors were motivators for survivors' participation in the sessions, some survivors (n = 5) recalled a disparity between the two groups. As one girl explained:
They could do more stuff than me, and that was kind of annoying because they were better than me. But at the same time, it was nice not to have to do it alone (Female, aged 13 years)
Despite the differences between them and the ambassadors, most of the survivors (n = 15) experienced the sessions to be more fun when their classmates were there rather than having to do the sessions alone with the professionals. For some of the survivors (n = 8), these ambassadorships led to deeper friendships post‐treatment.
The survivors (n = 8) who remained connected with their ambassadors found that the latter continued to support them post‐treatment. One girl explained:
I appreciated them [the ambassador visits] very much. It's easier to speak with those who were there during my treatment than with friends I've known since I was ten years old. They understand things differently […]. They know what it's like to be sick and not be able to talk with your parents about not having hair or having a bloated face […] Those things that other people just don't get (Female, aged 17 years)
A few of the survivors (n = 3) lost contact with their ambassadors as they had to repeat a school year or change schools altogether. However, these survivors found new friends with whom they could exercise. Most survivors (n = 16) noticed that they did not lag far behind their healthy peers during physical activities post‐treatment.
3.3. Physical activity post‐treatment
The survivors (n = 18) and their parents (n = 19) were taught the importance of physical activity during the programme and how cancer and its treatment can impact the child's physical function. Most parents (n = 17) expressed an understanding of this importance and several of the parents stated that their child also benefited from receiving guidance from the professionals. As one father explained:
I really do think it [RESPECT] helped him. It made him more aware of how important it is to stay physically active. (Father to 13‐year‐old male)
Many parents (n = 15) felt supported during the treatment because the physical activity professionals guided them in their role as part‐time trainers, motivators and caregivers. This guidance provided parents with the tools needed to fulfil the expectation placed on them. As one mother explained:
I asked the physical activity professionals what she was capable of doing if he thought she could do this or the other. He told me that there were no limitations and that we should let her go as far as she felt she could. We kept using that physical activity professional [for guidance] even after we came home (Mother to 11‐year‐old female)
The dyads (n = 31) agreed that the survivors who were active during treatment experienced an easier transition post‐treatment. However, the view of the survivors differed from that of their parents about the motivation for being physically active post‐treatment. Some parents (n = 6) felt that their personal support to their child was the motivation. As one mother explained:
I think it's very demanding on parents. Being active can mean a lot of things. If parents don't feel like doing it then it doesn't amount to anything. In fact, it's up to the parents to figure out what triggers their child. Because if it interests them [the children] then it's easier to motivate them. (Mother to 11‐year‐old female)
In contrast with their parents, most of the survivors (n = 16) looked to peers for support in being physically active and doing physical activities with peers positively impacted their physical and emotional well‐being. As one girl explained:
I think you need to find something you're interested in. That'll quickly motivate you to keep going and you also find friends who are interested in the same things. I just think it's important to get back to it [physical activity] right away because it does something for your body (Female, aged 17 years)
The dyads' understanding of the importance of physical activity continued post‐treatment. Most parents (n = 14) felt that they succeeded in motivating their children to be physically active, but some parents (n = 5) felt that more guidance on structuring physical or school activities would have been useful to ease the transition post‐treatment.
4. DISCUSSION
Semi‐structured interviews were used to explore experiences of young cancer survivors (aged 11–18 years) and their parents with a combined physical and social activity intervention during cancer treatment; including the programme's impact on the survivors' ability to be physically active post‐treatment. This study showed that a physical activity programme during treatment can enhance the survivors' and their parents' (dyads) views of how important physical activity can be during rehabilitation. Additionally, the knowledge they gained from the intervention proved useful to them post‐treatment.
In this study, the survivors had different physical activity needs during treatment. For example, some survivors found the sessions to be challenging while other survivors did not. This suggests that it is important to consider individual needs when promoting physical activity during hospitalization. When children with cancer participate in physical activity during treatment, they are susceptible to side effects (Nielsen et al., 2018). In the present study, survivors who experienced treatment side effects preferred doing sessions only with professionals. Some survivors found the presence of other children in the sessions to be generally demotivating. These findings suggest that while physical activity during hospitalization is feasible, professionals should adjust sessions to meet individual preferences. This finding is further supported by Lam et al. (2020) and shows that using a physical activity coach during treatment can increase the children with cancer's knowledge and confidence in doing physical activity.
Our findings show that most of the survivors found ambassador participation in the sessions to be motivating and as such ambassador support did reinforce survivor participation. This finding confirms previous research proposing that children and adolescents diagnosed with cancer are most likely to be motivated to engage in physical activity if they participate with their peers or receive positive feedback about their ability to be physically active (Mizrahi et al., 2020). Similar findings from the RESPECT study show that being physically active in a social context, for example, with ambassadors was motivating (Thorsteinsson et al., 2019). Our findings show that the social aspect of being physically active continued to motivate the survivors post‐treatment. This finding builds on previous research showing that adolescents with good peer support tend to participate in physical activity more than those who do not (Heitzler, 2010; Strauss et al., 2001). Earlier findings from the RESPECT Study suggest that a mutual understanding between survivors and their healthy peers can be developed if interventions include healthy peers during the child with cancer's rehabilitation (Ingersgaard et al., 2021). The present study also supports the recommendation that professionals working with children with cancer during hospitalization should facilitate contact between the child and their peers.
Research shows that children with cancer and their parents tend to believe that physical activity during treatment induces or worsens side effects, for example, fatigue (Cheung et al., 2021; Lam et al., 2017). A central finding of this study is that witnessing their child receiving professional guidance and observation during physical activities resulted in the parents developing a positive attitude towards physical activity and encouraging their child to be active post‐treatment. As such, the present study underscores the importance of professional guidance as a tool for challenging misconceptions about physical activity during cancer treatment. Previous research shows that parents with a positive attitude towards physical activity have a greater chance of motivating their children to engage regularly in physical activity (Brockman et al., 2009; Zecevic et al., 2010).
Our findings show that parents felt responsible for motivating their child to be physically active post‐treatment. Similar findings reported that childhood cancer survivors may be more influenced by parents to do physical activities than by their healthy peers, due to developmental disruption caused by having a cancer diagnosis and being hospitalized (Gilliam & Schwebel, 2013). In contrast, the present study shows that survivors consider their peers and their own understanding of the importance of physical activity to be the main motivators post‐treatment. These findings support Yao and Rhodes (2015) suggestion that when childhood cancer survivors go through puberty, modelling behaviours of peers over those of their parents motivates them more to doing physical activity. Healthcare professionals can benefit from this study's findings to better understand dyadic experiences with physical activity during and post‐treatment. Furthermore, healthcare professionals should motivate the child with cancer to be physically active during treatment by including peers and parents in sessions. As treatment is dynamic and the child with cancer's needs vary throughout the process, healthcare professionals should use an explorative approach when motivating the child with cancer. To ensure the possibility of being physically active, healthcare professionals should include physical activities within the care plan. Post‐treatment, healthcare professionals should be encouraged to explore facilitators and barriers to survivors doing physical activity and provide them with the necessary support.
4.1. Strength and limitations
In the RESPECT Study, authors MKF and TT assumed the role of physical activity professionals and worked with the survivors during their treatment. This is considered a potential bias as they may have assumed a more positive outlook when writing this article. However, to accommodate this potential bias and to strengthen this study's credibility, an independent interviewer was included, and the authors (MKF and TT) were excluded from any data analysis. An additional strength was the fact that the interviews were conducted in person. The face‐to‐face interaction helped the interviewer to establish a relationship with the participants, thus facilitating the discussion of sensitive topics. Our attempt to include childhood cancer survivors with long treatment episodes were successful which resulted in comprising mainly former leukaemia patients (61%). This is considered a limitation, as the study findings may not be representative of the overall diversity of childhood cancer. Furthermore, there may be differences in diagnoses and treatments and their impact on survivors' ability to be physically active post‐treatment. This aspect was not explored in this study.
Another limitation is that the parents' recall may have been influenced by the survivors' current physical and social activity level and as such may have affected their responses at the time of the interviews, for example, being selective by offering statements confined to things that impressed them most. The importance of physical activity is a widely accepted norm in the daily lives of children and adolescents in Denmark. Accordingly, the parents may have expressed their desire to promote physical activity in their daily lives because the interviewer may view this attitude as favourable. Consequently, this may have affected the trustworthiness of the study.
The study findings may be transferable to other paediatric oncology settings as the knowledge about professional guidance and the importance of peer support during and post‐treatment may be used across disease groups and cultures. We acknowledge that other frameworks may have been useful tools to discover other important dimensions of the participants' experiences. Future studies that focus on exercise may find these frameworks useful when conducting qualitative research.
5. CONCLUSION
Childhood cancer survivors and their parents benefited from participating in an intervention where physical and social activities were combined. The study findings indicate that the dyads understood the importance of being physically active during hospitalization and their appreciation of it continued post‐treatment. Physical activity support varied according to the daily health status of the survivors during treatment.
The importance of including peers in physical activities with survivors should not be underestimated, however, sensitivity of individual preferences should be considered. Differentiating between ages, needs and motivation would be valuable when designing future physical activity interventions during treatment for children with cancer.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version and made substantial contributions to the design of this study and the interpretation of data. Furthermore, all authors have revised the article critically to ensure intellectual content.
FUNDING INFORMATION
The Danish Childhood Cancer Foundation, The Danish Cancer Society; The Novo Nordisk Foundation; Lundbeck Foundation; Toyota Foundation; Familien Hede Nielsens Foundation; ML Jørgensen and Gunnar Hansens Foundation; Arvid Nilssons Foundation; Aase og Ejnar.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15381.
Supporting information
Appendix S1
ACKNOWLEDGEMENT
This work is part of Childhood Oncology Network Targeting Research, Organization & Life expectancy (CONTROL) and supported by Danish Cancer Society (R‐257‐A14720) and the Danish Childhood Cancer Foundation (2019‐5934).
Petersen, N. N. , Larsen, H. B. , Pouplier, A. , Schmidt‐Andersen, P. , Thorsteinsson, T. , Schmiegelow, K. , & Fridh, M. K. (2022). Childhood cancer survivors' and their parents' experiences with participation in a physical and social intervention during cancer treatment: A RESPECT study. Journal of Advanced Nursing, 78(11), 3806–3816. 10.1111/jan.15381
Natasha Nybro Petersen and Hanne Bækgaard Larsen shared first authorship.
DATA AVAILABILITY STATEMENT
Research data is not shared.
REFERENCES
- Adamsen, L. , Larsen, H. B. , Jarden, M. , Moeller, T. , Piil, K. , & Quist, M. (2020). Exercise in cancer survivors CIRE—Horizon 2020. https://www.cancer.dk/dyn/resources/File/file/5/6655/1505472246/exercise‐in‐cancer‐survivors.pdf
- Armstrong, G. T. , Kawashima, T. , Leisenring, W. , Stratton, K. , Stovall, M. , Hudson, M. M. , Sklar, C. A. , Robison, L. L. , & Oeffinger, K. C. (2014). Aging and risk of severe, disabling, life‐threatening, and fatal events in the childhood cancer survivor study. Journal of Clinical Oncology, 32(12), 1218–1227. 10.1200/jco.2013.51.1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett, P. M. , Mullen, L. , & McCarthy, T. (2020). Enduring psychological impact of childhood cancer on survivors and their families in Ireland: A national qualitative study. European Journal of Cancer Care, 29(5), e13257. 10.1111/ecc.13257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeler, D. , Pare‐Blagoev, E. J. , Jacobson, L. A. , & Ruble, K. (2021). Educating childhood cancer survivors: A qualitative analysis of parents mobilizing social and cultural capital. Journal of Cancer Education, 36(4), 819–825. 10.1007/s13187-020-01709-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braam, K. I. , Van Der Torre, P. , Takken, T. , Veening, M. A. , Van Dulmen‐Den Broeder, E. , & Kaspers, G. J. (2016). Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database of Systematic Reviews, 3, CD008796. 10.1002/14651858.cd008796.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw, C. , Atkinson, S. , & Doody, O. (2017). Employing a qualitative description approach in health care research. Global Qualitative Nursing Research, 4, 74228. 10.1177/2333393617742282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockman, R. , Jago, R. , Fox, K. R. , Thompson, J. L. , Cartwright, K. , & Page, A. S. (2009). "get off the sofa and go and play": Family and socioeconomic influences on the physical activity of 10‐11 year old children. BMC Public Health, 9, 253. 10.1186/1471-2458-9-253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung, A. T. , Li, W. H. C. , Ho, L. L. K. , Chan, G. C. F. , & Chung, J. O. K. (2021). Parental perspectives on promoting physical activity for their children surviving cancer: A qualitative study. Patient Education and Counseling, 104(7), 1719–1725. 10.1016/j.pec.2020.11.009 [DOI] [PubMed] [Google Scholar]
- Clarke, V. , Braun, V. , & Hayfield, N. (2015). Thematic analysis. In Smith J. A. (Ed.), Qualitative psychology: A practical guide to research methods (pp. 222–248). SAGE Publications. [Google Scholar]
- Germain, N. , Aballéa, S. , & Toumi, M. (2019). Measuring health‐related quality of life in young children: How far have we come? Journal of Market Access & Health Policy, 7(1), 1618661. 10.1080/20016689.2019.1618661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliam, M. B. , & Schwebel, D. C. (2013). Physical activity in child and adolescent cancer survivors: A review. Health Psychology Review, 7(1), 92–110. 10.1080/17437199.2011.603641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Götte, M. , Kesting, S. , Winter, C. , Rosenbaum, D. , & Boos, J. (2014). Experience of barriers and motivations for physical activities and exercise during treatment of pediatric patients with cancer. Pediatric Blood & Cancer, 61(9), 1632–1637. 10.1002/pbc.25071 [DOI] [PubMed] [Google Scholar]
- Grimshaw, S. L. , Taylor, N. F. , Mechinaud, F. , Conyers, R. , & Shields, N. (2020). Physical activity for children undergoing acute cancer treatment: A qualitative study of parental perspectives. Pediatric Blood & Cancer, 67(6), e28264. 10.1002/pbc.28264 [DOI] [PubMed] [Google Scholar]
- Heitzler, C. (2010). Evaluating a model of youth physical activity. American Journal of Health Behavior, 34(5), 593–606. 10.5993/ajhb.34.5.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms, A. S. , Schmiegelow, K. , Brok, J. , Johansen, C. , Thorsteinsson, T. , Simovska, V. , & Larsen, H. B. (2016). Facilitation of school re‐entry and peer acceptance of children with cancer: A review and meta‐analysis of intervention studies. European Journal of Cancer Care, 25(1), 170–179. 10.1111/ecc.12230 [DOI] [PubMed] [Google Scholar]
- Ingersgaard, M. V. , Fridh, M. K. , Thorsteinsson, T. , Adamsen, L. , Schmiegelow, K. , & Baekgaard Larsen, H. (2021). A qualitative study of adolescent cancer survivors perspectives on social support from healthy peers – A RESPECT study. Journal of Advanced Nursing, 77(4), 1911–1920. 10.1111/jan.14732 [DOI] [PubMed] [Google Scholar]
- Lam, K. K. , Ho Cheung William, L. , Ho, K. Y. E. , Chung, O. K. J. , & Chan, C. F. G. (2017). Factors contributing to the low physical activity level for Hong Kong Chinese children hospitalised with cancer: An exploratory study. Journal of Clinical Nursing, 26(1–2), 190–201. 10.1111/jocn.13495 [DOI] [PubMed] [Google Scholar]
- Lam, K. K. W. , Li, W. H. C. , Chung, J. O. K. , Ho, K. Y. , Xia, W. , Cheung, A. T. , Chiu, S. Y. , Lam, H. S. , & Chan, G. C. F. (2020). Promoting physical activity among children with cancer through an integrated experiential training programme with coaching: A qualitative study. Patient Education and Counseling, 103(6), 1230–1236. 10.1016/j.pec.2020.02.001 [DOI] [PubMed] [Google Scholar]
- Lincoln, Y. S. , & Guba, E. G. (1986). But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Directions for Program Evaluation, 1986(30), 73–84. 10.1002/ev.1427 [DOI] [Google Scholar]
- Lindgren, L. H. , Schmiegelow, K. , Helms, A. S. , Thorsteinsson, T. , & Larsen, H. B. (2017). In sickness and in health: Classmates are highly motivated to provide in‐hospital support during childhood cancer therapy. Psychooncology, 26(1), 37–43. 10.1002/pon.4094 [DOI] [PubMed] [Google Scholar]
- Mizrahi, D. , Wakefield, C. E. , Simar, D. , Ha, L. , McBride, J. , Field, P. , Cohn, R. J. , & Fardell, J. E. (2020). Barriers and enablers to physical activity and aerobic fitness deficits among childhood cancer survivors. Pediatric Blood & Cancer, 67(7), e28339. 10.1002/pbc.28339 [DOI] [PubMed] [Google Scholar]
- Moore, G. F. , Audrey, S. , Barker, M. , Bond, L. , Bonell, C. , Hardeman, W. , Moore, L. , O'Cathain, A. , Tinati, T. , Wight, D. , & Baird, J. (2015). Process evaluation of complex interventions: Medical Research Council guidance. BMJ, 350, h1258. 10.1136/bmj.h1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ness, K. K. , Kaste, S. C. , Zhu, L. , Pui, C.‐H. , Jeha, S. , Nathan, P. C. , Inaba, H. , Wasilewski‐Masker, K. , Shah, D. , Wells, R. J. , Karlage, R. E. , Robison, L. L. , & Cox, C. L. (2015). Skeletal, neuromuscular and fitness impairments among children with newly diagnosed acute lymphoblastic leukemia. Leukemia & Lymphoma, 56(4), 1004–1011. 10.3109/10428194.2014.944519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ness, K. K. , Leisenring, W. M. , Huang, S. , Hudson, M. M. , Gurney, J. G. , Whelan, K. , Hobbie, W. L. , Armstrong, G. T. , Robison, L. L. , & Oeffinger, K. C. (2009). Predictors of inactive lifestyle among adult survivors of childhood cancer. Cancer, 115(9), 1984–1994. 10.1002/cncr.24209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen, M. K. F. , Christensen, J. F. , Frandsen, T. L. , Thorsteinsson, T. , Andersen, L. B. , Christensen, K. B. , Nersting, J. , Faber, M. , Schmiegelow, K. , & Larsen, H. B. (2018). Testing physical function in children undergoing intense cancer treatment—a RESPECT feasibility study. Pediatric Blood & Cancer, 65(8), e27100. 10.1002/pbc.27100 [DOI] [PubMed] [Google Scholar]
- Nielsen, M. K. F. , Christensen, J. F. , Frandsen, T. L. , Thorsteinsson, T. , Andersen, L. B. , Christensen, K. B. , Wehner, P. S. , Hasle, H. , Adamsen, L. O. , Schmiegelow, K. , & Larsen, H. B. (2020). Effects of a physical activity program from diagnosis on cardiorespiratory fitness in children with cancer: A national non‐randomized controlled trial. BMC Medicine, 18(1), 175. 10.1186/s12916-020-01634-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmiegelow, K. , & Frandsen, T. L. (2018). The cost of cure. Lancet Haematol, 5(11), e504–e505. 10.1016/s2352-3026(18)30070-x [DOI] [PubMed] [Google Scholar]
- Speyer, E. , Herbinet, A. , Vuillemin, A. , Briançon, S. , & Chastagner, P. (2010). Effect of adapted physical activity sessions in the hospital on health‐related quality of life for children with cancer: A cross‐over randomized trial. Pediatric Blood Cancer, 55(6), 1160–1166. 10.1002/pbc.22698 [DOI] [PubMed] [Google Scholar]
- Strauss, R. S. , Rodzilsky, D. , Burack, G. , & Colin, M. (2001). Psychosocial correlates of physical activity in healthy children. Archives of Pediatrics & Adolescent Medicine, 155(8), 897–902. 10.1001/archpedi.155.8.897 [DOI] [PubMed] [Google Scholar]
- Sullivan‐Bolyai, S. , Bova, C. , & Harper, D. (2005). Developing and refining interventions in persons with health disparities: The use of qualitative description. Nursing Outlook, 53(3), 127–133. 10.1016/j.outlook.2005.03.005 [DOI] [PubMed] [Google Scholar]
- Thorsteinsson, T. , Helms, A. S. , Adamsen, L. , Andersen, L. B. , Andersen, K. V. , Christensen, K. B. , Hasle, H. , Heilmann, C. , Hejgaard, N. , Johansen, C. , Madsen, M. , Madsen, S. A. , Simovska, V. , Strange, B. , Thing, L. F. , Wehner, P. S. , Schmiegelow, K. , & Larsen, H. B. (2013). Study protocol: Rehabilitation including social and physical activity and education in children and teenagers with cancer (RESPECT). BMC Cancer, 13, 544. 10.1186/1471-2407-13-544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsteinsson, T. , Larsen, H. B. , Schmiegelow, K. , Thing, L. F. , Krustrup, P. , Pedersen, M. T. , Christensen, K. B. , Mogensen, P. R. , Helms, A. S. , & Andersen, L. B. (2017). Cardiorespiratory fitness and physical function in children with cancer from diagnosis throughout treatment. BMJ Open Sport & Exercise Medicine, 3(1), e000179. 10.1136/bmjsem-2016-000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsteinsson, T. , Schmiegelow, K. , Thing, L. F. , Andersen, L. B. , Helms, A. S. , Ingersgaard, M. V. , Lindgren, L. H. , & Larsen, H. B. (2019). Classmates motivate childhood cancer patients to participate in physical activity during treatment: A qualitative study. European Journal of Cancer Care, 28(5), e13121. 10.1111/ecc.13121 [DOI] [PubMed] [Google Scholar]
- Vannatta, K. , Gerhardt, C. A. , Wells, R. J. , & Noll, R. B. (2007). Intensity of CNS treatment for pediatric cancer: Prediction of social outcomes in survivors. Pediatric Blood & Cancer, 49(5), 716–722. 10.1002/pbc.21062 [DOI] [PubMed] [Google Scholar]
- Wakefield, C. E. , McLoone, J. K. , Butow, P. , Lenthen, K. , & Cohn, R. J. (2011). Parental adjustment to the completion of their child's cancer treatment. Pediatric Blood & Cancer, 56(4), 524–531. 10.1002/pbc.22725 [DOI] [PubMed] [Google Scholar]
- Warner, E. L. , Kent, E. E. , Trevino, K. M. , Parsons, H. M. , Zebrack, B. J. , & Kirchhoff, A. C. (2016). Social well‐being among adolescents and young adults with cancer: A systematic review. Cancer, 122(7), 1029–1037. 10.1002/cncr.29866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao, C. A. , & Rhodes, R. E. (2015). Parental correlates in child and adolescent physical activity: A meta‐analysis. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 10. 10.1186/s12966-015-0163-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zecevic, C. A. , Tremblay, L. , Lovsin, T. , & Michel, L. (2010). Parental influence on young Children's physical activity. International Journal of Pediatrics, 2010, 1–9. 10.1155/2010/468526 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
Research data is not shared.


