Abstract
Aims
Diagnostic Reasoning (DR) is an essential competency requiring mastery for safe, independent Nurse Practitioner (NP) practice, but little is known about DR content included in NP education programs. The aims of this study were to identify whether and how the concept of DR is addressed in NP education.
Design
We conducted a scoping review on DR‐related content and teaching innovations in U.S. primary care NP education programs, with implications for NP education programs worldwide. Concepts and principles with global applicability include: conducting focused and hypothesis‐directed histories and exams, generating the problem statement, formulating the differential diagnosis, appropriate and relevant diagnostic testing, determining the working diagnosis and developing evidence‐based, patient‐centred management plans.
Data sources
N = 1115 articles retrieved from Medline, Embase, PsycINFO, and CINAHL for the period 2005–2021. Forty‐one scholarly articles met inclusion/exclusion criteria.
Review methods
Data were extracted, synthesized and grouped by theoretical frameworks, content included, educational interventions and assessment measures.
Results
Most articles provided descriptions of approaches for teaching NP clinical or diagnostic reasoning. Ten papers directly referenced the current science and theory of DR.
Conclusion
The US NP education literature addressing DR is limited and demonstrates a lack of shared conceptualizations of DR. Whilst numerous components of DR are identifiable in the literature, a robust teaching/learning scholarship for DR has not yet been established in the US NP education literature.
Impact
Whilst primary care NP education programs are beginning to incorporate DR education into their curricula, little research has been conducted to demonstrate the effectiveness of educational outcomes. Increased integration of DR content into NP education is needed, including increased educational research on teaching DR competencies.
Patient or public contribution
No patient or public contribution was included in this review, as the public is generally not familiar with DR or its teaching approaches.
Keywords: advanced practice nursing, clinical reasoning, diagnosis, diagnostic reasoning, literature review, nurse practitioner, nurse practitioner education, nursing, nursing curriculum, scoping review
1. INTRODUCTION
In the domain of clinical reasoning for the healthcare clinical practice professions, diagnostic reasoning (DR) has been identified as an essential cognitive competency for safe and effective practice (Graber et al., 2018; IOM, 2015). DR can be defined as that component of clinical reasoning that focuses on getting to the clinical diagnoses and determining relevant management of the clinical problems (Nordick, 2021; Rajkomar & Dhaliwal, 2011). Effective DR has been linked to improved quality of care and care outcomes (Graber et al., 2018; IOM, 2015), and is necessary for clinical problem definition, reducing diagnostic error and determining appropriate management. Arguably, mastery of and accountability for DR is one of the key distinctions between Registered Nurse (RN) and Nurse Practitioner (NP) practice, yet recognition of DR as a unique and distinct process has been limited in the NP education literature. Little emphasis has been placed on understanding or developing this complex cognitive competency
Over the past two decades, diagnostic error has been recognized as a major contributor to health care quality and safety concerns (IOM, 2015). Estimates indicate that as many as one in 20 persons experience a diagnostic error in outpatient clinics annually (Singh et al., 2013, 2014), and that diagnostic error for hospitalized patients is associated with increased hospital mortality (Hautz et al., 2019; Sorinola et al., 2012). A diagnostic error has been attributed to errors in thinking (Croskerry, 2003; Elstein, 1999; Kassirer, 1989; Zhang, 2002), including insufficient knowledge, flaws in data gathering, ineffective approaches to information processing, or poor skills in monitoring one's thinking (Graber et al., 2005). Fortunately, the cognitive processes of diagnostic reasoning are amenable to correction and improvement through structured and intentional educational interventions (Boshuizen & Schmidt, 2019; Kiesewetter et al., 2013). In 2015, the National Academy of Medicine called for increased inclusion of DR education in health professions' curricula (IOM, 2015). Since then, DR has become a principal component of teaching clinical reasoning in medical education globally (Cooper et al., 2021; Englander et al., 2013; Gilkes et al., 2022; Olson et al., 2019).
In comparison, NP education has lagged in its incorporation of DR as central to advanced practice clinical reasoning. The International Council of Nurses (ICN) noted that, globally, advanced practice nurses, including clinical nurse specialists, nurse practitioners, nurse midwives and nurse anaesthetists are one of the fastest growing health professions, responsible for innovating health care systems, improving access to care, achieving better health outcomes, and reducing health care costs (ICN, 2021). With these developments and with the current ICN initiative to support the continued global evolution of advanced practice nursing (Schober & Stewart, 2019), it is imperative that advanced practice nursing education address the incorporation of DR education as a component of NP practice worldwide.
2. BACKGROUND
DR, a subset of clinical reasoning, is the cognitive process used to collect and interpret data to medically diagnose and treat patients (Nordick, 2021; Rajkomar & Dhaliwal, 2011). Whilst medicine sometimes uses the term clinical reasoning interchangeably with DR, in nursing practice the term clinical reasoning has a broader meaning, referring both to RN practice and decision making as well as to NP practice. For clarity in NP practice, DR can be understood as more specific to the cognitive processes of getting to and acting on the patient's medical diagnosis. Additional terms such as critical thinking, clinical decision making, and clinical judgement, are related but also less specific (see, for example, Hughes, 2008 and Victor‐Chmil, 2013), and do not necessarily capture the diagnostic process that occurs as central to NP practice. Differences between critical thinking, clinical reasoning, clinical judgement and DR are depicted in Figure 1. Capturing the complex cognitive skills required for the NP competency of diagnosing the patient's conditions requires exploration of the specific process of DR.
FIGURE 1.
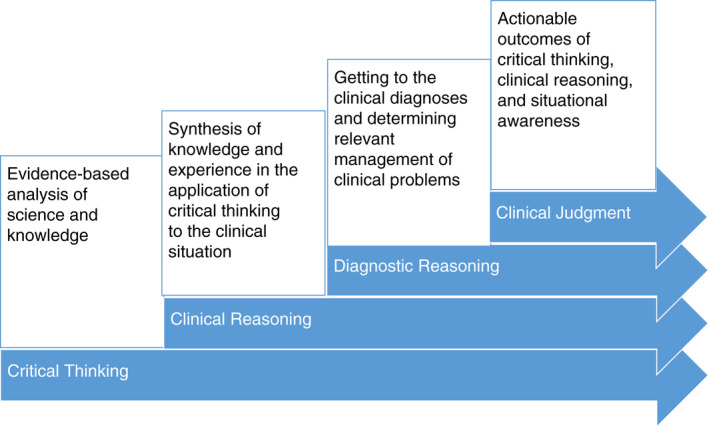
Comparison of critical thinking, clinical reasoning, diagnostic reasoning, and clinical judgement.
Theoretical frameworks used to explain DR have been well described and distinguish multiple cognitive processes, including how clinical content knowledge is stored and accessed (see, for example, Schmidt & Rikers, 2007); dual process reasoning (see Evans, 2008); and thinking about thinking (see Mamede et al., 2012). Whilst beyond the scope of this paper to describe the cognitive science of DR in detail, several summaries of DR are available (Bowen, 2006; Croskerry, 2009; Thammasitboon et al., 2018) and generally include the following: clinical knowledge development and organization (Charlin et al., 2007); patient interaction and encounter management skills (Hasnain et al., 2001); hypothesis‐directed history and exam skills (Thampy et al., 2019); script activation (Custers, 2015); problem representation (Bowen, 2006; Chang et al., 1998; Connor & Dhaliwal, 2015); analytic and non‐analytic thinking (Lambe et al., 2016); generating an appropriate and relevant differential diagnosis (Xu et al., 2021); appropriate and relevant diagnostic testing (Steiger et al., 2011); determining the working diagnosis (Charlin et al., 2007); developing an evidence‐based and patient‐centred management plan (Cooper et al., 2021); reflecting on one's DR competencies (Mamede et al., 2012; Olson et al., 2019). In NP practice, we would add to these frameworks the nursing perspectives of whole person care, foregrounding the NP provider‐patient relationship, and focusing on health promotion and well‐being as central to care. A glossary of relevant DR‐related concepts and terms can be found in Table 1; key elements of DR are shown in Figure 2.
TABLE 1.
. Glossary of diagnostic reasoning‐related concepts and terms
| DR‐related concept/term | Definition |
|---|---|
| Hypothetico‐deductive reasoning | The practice of analytically validating the provider's theories about patients' clinical problems by means of making inferences from the data, formulating hypotheses (premises), and deriving and testing conclusions. |
| Dual‐process reasoning |
The theory that two cognitive systems are used to reason, with one system making quick, automatic judgements based on associative and intuitive feedback, and the other system making more effortful and analytical judgements based on deliberate information searching and processing. From a functional perspective, the two systems are often jointly involved in decision making. Theoretically, the analytical system provides a monitoring function over the automatic system. |
| System 1 thinking |
Rapid, automated processing of information that is below the perceptible threshold of consciousness. Relies on contextual cues and recognition of similarities to previously encountered situations. More likely used in making more routine decisions or in familiar situations. |
| System 2 thinking |
A slower, more demanding system of thinking based on rational, deliberate judgement and conscious application of decision rules. More likely used in complex situations with ambiguous, non‐routine, or indeterminate problems. |
| Heuristics |
Simple decision strategies that base decisions on only a portion of the available information, focusing on a small number of relevant predictors. Heuristics are shortcuts used to simplify decision making in otherwise complex situations, frequently occurring as part of system 1 thinking. |
| Diagnostic error | Mistakes or failures in the diagnostic process leading to a mis‐, missed or delayed diagnosis |
| Illness scripts & schema |
Large chunks of information (“schema’), cognitively organized into prototypes and exemplars of disease manifestations known as “illness scripts.” Illness scripts provide structure, aligning clinical features of disease with the patient presentation. Script activation is theorized as one mechanism used to generate the differential and direct the patient evaluation. |
| Hypothesis‐driven history and exam |
Purposeful search for history and exam data to confirm or refute the differential, based on script activation and elaborated illness scripts. The use of focused history questions and physical exam to narrow the differential. |
| Differential diagnosis |
Differentiating between the probability of two or more diseases or conditions with similar symptoms or characteristics by systematically comparing and contrasting results of diagnostic activities. |
| Working diagnosis |
The likely, but unconfirmed, diagnosis, without ruling out other diseases. The result of refining a list of possible diagnoses as further information is obtained in the diagnostic process. |
| Problem representation statement |
Interpretive summary statement of the patient's presentation that captures key aspects most relevant to diagnosing the patient's condition (clinical context, risk factors, temporal pattern) using qualified medical terminology and clearly communicating the clinical inferences. |
| Clinical reasoning |
Discipline and context‐specific processes by which clinicians collect and interpret information to understand the patient's healthcare situation or problem, then plan and implement appropriate interventions. |
| Diagnostic reasoning |
A dynamic framework that guides providers' clinical reasoning processes as they strive to find correct diagnostic solutions. |
| Critical thinking |
Cognitive processes are used to analyse empirical knowledge, based on evidence and science. |
| Clinical reasoning |
Discipline‐specific process of synthesizing knowledge and experience in the application of critical thinking to the clinical situation. |
| Clinical judgement |
The actionable outcomes of critical thinking, clinical reasoning, and situational awareness. |
FIGURE 2.
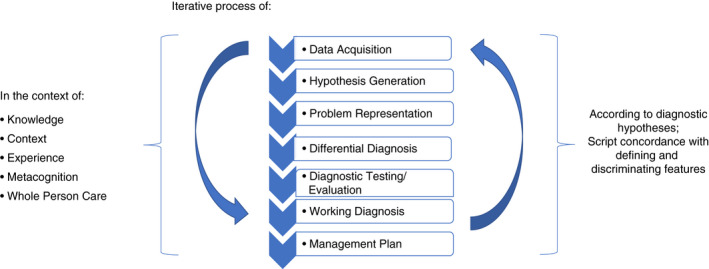
Key elements of diagnostic reasoning.
Research from around the world demonstrates that competency in DR is developed through intentional instruction and practice (Bowen, 2006; Friel & Chandar, 2021; Rencic et al., 2017; Singh et al., 2021; Xu et al., 2021). Strong clinical reasoning has been found to be associated with multiple advanced cognitive competencies, including the transfer of basic science knowledge to clinical problem‐solving (Castillo et al., 2018); an understanding of clinical reasoning concepts (Wu, 2018); building organized, problem‐specific knowledge structures (Custers, 2015; Lee et al., 2010); effective communication and purposeful interviewing (Hasnain et al., 2001); hypothesis‐directed data acquisition (Yudkowsky et al., 2009); synthesizing an accurate and descriptive representation of the problem (Bordage, 1994; Bowen, 2006; Braun et al., 2017); employing metacognition skills for further learning and development (Olson et al., 2019).
Traditionally, assimilation of clinical and DR processes in NP education has relied primarily on implicit learning through the preceptor‐led clinical practice component of the NP curriculum, with little incorporation into the didactic curriculum. However, the ability of practicing clinicians to teach clinical reasoning in general and DR, in particular, is highly variable. Challenges include lack of background in this area, clinician lack of awareness of underlying cognitive processes, and insufficient time. Research in medicine demonstrates that role‐modelling cannot be relied on for the development of effective diagnostic thinking in novice physicians (Audétat et al., 2013; Eva, 2004; Graber et al., 2018). Similarly, we would have little reason to believe that role‐modelling alone would be any less deficient for NP students. Thus, with the large body of evidence on clinical reasoning and DR now available, it is no longer sufficient to assume that clinical knowledge, experience, and preceptor role‐modelling will result in the level of diagnostic acumen required for safe and effective NP practice 1 .
The 2021 revisions to the American Association of Colleges of Nursing (AACN) advanced‐level nursing Essentials include teaching students to diagnose and to “…employ context‐driven, advanced reasoning to the diagnostic and decision‐making process” (AACN, 2021, p 30). Whilst the determination of the clinical diagnosis is also included as a National Organization of Nurse Practitioner Faculty (NONPF) core competency (NONPF, 2017), little guidance has emerged as to what content, processes or principles are needed to teach this complex process, nor is there consensus amongst NP faculty and scholars as to the relationship between clinical reasoning and DR. Despite these challenges, it is imperative that NP educators incorporate improved and intentional strategies for teaching DR to advance NP clinical reasoning practices and reduce the burden of diagnostic error. Such a refocusing of educational priorities becomes especially important with the massive growth of NP education programs worldwide and the increasing complexity of patients seen in NP practice.
3. THE REVIEW
3.1. Aims
To increase attention to the importance of DR knowledge, skills and attitudes for safe and effective NP practice, it is crucial that we examine existing evidence about DR‐related content in NP education programs. This scoping review explored whether and how the concept of DR is addressed in NP education programs in the United States (U.S.). Our specific aims were to
Describe the extent to which the scholarly literature about clinical reasoning in NP education includes content related to DR.
Identify how DR is defined in primary care NP education.
Describe the teaching methodologies used to educate NP students about DR‐related. knowledge, skills, and/or attitudes.
3.2. Design
We conducted a scoping review to systematically identify, classify, and synthesize the literature from the past 15 years, to describe the extent, current state, and impact of DR‐related education in U.S. primary care NP education programs. Because our expertise is relative to NP education in the U.S., we limited our review to U.S. NP education. Scoping review was selected as the appropriate methodology based on the complexity of the topic, limited uptake in the NP education literature, and lack of a previous comprehensive review in the NP education literature (Daudt et al., 2013). The review followed Arksey and O'Malley's (2005) five‐step framework: identifying the research question; identifying relevant studies; study selection; charting the data; and, collating, summarizing and reporting the results.
3.3. Search methods
We conducted a comprehensive search combining keywords and controlled vocabulary searching across four databases: Embase, Medline, and PsycINFO via Ovid, and CINAHL via EBSCO. The search was conducted in July 2020 and updated in November 2021. In accordance with best practices for comprehensive search strategies (Lefebvre et al., 2022), controlled vocabulary terms and keyword searching reflected the concepts of nurse practitioner education, clinical reasoning, and DR, which were combined using Boolean operators. No limitations were placed on the study design or the language of publication. Results were limited to publications since 2005, which reflects the 10‐year period in advance of the 2015 IOM report. To ensure no potentially relevant items were overlooked, hand‐searching of reference lists of relevant items was also conducted. The protocol for this review was registered in PROSPERO;® the complete search strategy is available in the online Supplemental Information.
Two independent reviewers screened titles and abstracts using Rayyan,® a web‐based tool designed to facilitate systematic review screening (Ouzzani et al., 2016). We included studies on U.S.‐based primary care NP programs that included one or more aspects of DR. These included studies describing concepts associated with DR, such as taking a patient history or developing a differential diagnosis, even if those studies did not use the terminology “diagnostic reasoning.” We excluded studies that did not include primary care NP education, were based outside of the U.S. or did not refer to DR or any of its component processes. We also excluded studies that focused exclusively on continuing education of practising NPs.
In the title and abstract screening phase, any conflicts were resolved through full team discussion. The process of two‐investigator independent screening and full team conflict resolution was repeated for a full‐text review of the articles. During the full‐text screening phase, the reason for exclusion was recorded and reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines (Page et al., 2021). Figure 3 provides the PRISMA diagram for this review.
FIGURE 3.
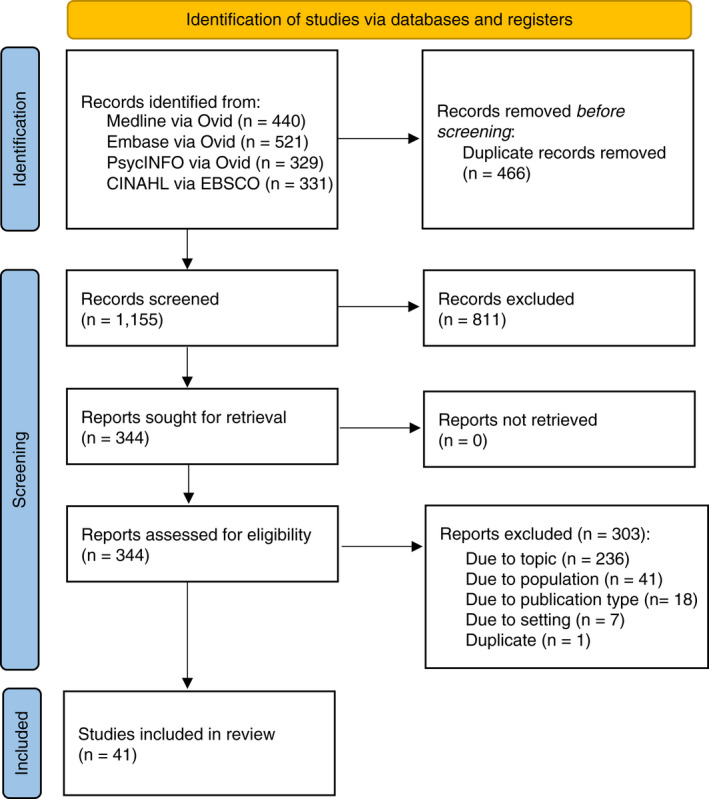
Preferred reporting items for systematic reviews and meta‐analyses (PRISMA) diagram.
3.4. Quality appraisal
A quality appraisal was initially completed; however, since scoping studies conventionally do not seek to assess the quality of the evidence (Arksey & O'Malley, 2005), the quality appraisal is not included here.
3.5. Data abstraction
One researcher initially developed the data abstraction form, which was then piloted by all four researchers for additional refinement. Data was collected using RedCap.® All team members participated in extracting data from the articles. Key data included (i) study aims/research questions/hypotheses; (ii) NP populations studied and demographic data; (iii) study design; (iv) independent and dependent variables, interventions/educational methodologies and measures specific to the interventions/methodologies; (v) definitions of, theoretical frameworks for, and/or components of DR‐related study components; (vi) major findings, additional findings, and limitations.
3.6. Synthesis
Tables were used to display the data from the scoping review. Categories of data analysed included theoretical frameworks used, content of the intervention, DR‐related components included, pedagogy used, specific educational interventions, assignments/activities, assessment/evaluation approaches, and assessment measures used. Additionally, our review utilized a descriptive qualitative thematic analysis of findings. One member of the review team conducted a thematic analysis. Codes were developed and themes were agreed on by all authors. Narratives describing the themes were then drafted.
4. RESULTS
4.1. Search outcome
Searches of databases identified 1621 items, of which 466 were duplicates. The remaining 1155 titles and abstracts were screened, with 811 excluded. The remaining 344 articles were screened in full text. Of the 344 items, 303 were excluded due to not focusing on diagnostic reasoning (236), not including primary care NP students (41), incorrect publication type such as a student thesis (18), wrong setting such as outside of the U.S. (7), or being a duplicate (1). The resulting 41 articles reflect 40 projects, as two papers presented different components from one study. See Table 2 for summary descriptions of the included articles.
TABLE 2.
Description of included articles
| Author (year) | Sample | Design | Purpose | Overall expected outcomes | Focus on diagnostic reasoning‐related educational component |
|---|---|---|---|---|---|
| Ballman et al. (2016) | NP students at a large Midwestern urban university | Case Report (Teaching) | Describe a virtual learning innovation to engage distance students in a differential diagnosis course | Integrative thinking, development of problem‐solving and clinical reasoning skills | Use of standardized patients, interactive case studies and subject matter experts in virtual encounters for focused histories, physical exams, and formulation of the differential |
| Beckham (2013) | 52 FNP students | Case Report (Teaching) with a retrospective comparison of student assessment outcomes | Compare longitudinal OSCE performance with clinical course grades to identify students who need additional support in developing clinical competencies | Critical thinking; integration of pathophysiology and pharmacology; Demonstration of safe practice | Six OSCE scenarios were delivered over a 2‐year period to assess skills in patient interaction, history taking, physical exam, identification of the abnormality, differential diagnosis, patient presentation, and documentation. OSCE scores were compared with scores for onsite clinical performance evaluation and two written clinical notes |
| Benbenek et al. (2016 | FNP, AGNP, WHNP, and CNM students in the final clinical course | Case Report (Teaching) | Describe the development, design and implementation of capstone OSCEs for summative evaluation of clinical competence | Demonstration of safe, entry‐level clinical practice | Six OSCE encounters were conducted over two days, to evaluate student readiness for safe beginning NP practice |
| Billings and Kowalski (2008) | Not applicable | Review of literature and description of teaching strategy | Describe “argument mapping” as a teaching technique to develop inferential thinking skills | Synthesize information, think critically, use clinical evidence appropriately, derive optimum clinical conclusions, refine clinical reasoning and decision making | Use of argument mapping as a cognitive strategy to foster advanced critical thinking and clinical decision making by moving from data to clinical impressions |
|
Bradford et al. (2021) |
CNM and WHNP students during covid | Case Report (Teaching) | Describe a variety of synchronous and asynchronous simulation approaches used to replace clinical experiences during covid | Developing and enhancing acquisition of clinical and communication skills, decision‐making, self‐confidence and readiness to begin or return to the clinical setting |
Obtain and interpret data, communicate, develop a diagnosis and management plan, and handle unpredictable patient behaviour. Clinical case presentation demonstrating clinical thinking and reasoning |
| Burt and Corbridge (2018) | 18 primary sources across NP and medical education and practice | Integrative review | Review the primary research on educational strategies for the development of diagnostic reasoning competencies | Ability to accurately diagnose patients based on symptom profiles; Accurate formulation of differential diagnoses; application of sound judgement to synthesize facts and apply them clinically | Major strategies included testing‐based approaches, simulation, reduction of cognitive biases, knowledge organization and active learning |
|
Burt, Corbridge, et al. (2021) |
37 RNs enrolled in the FNP option of the Doctor of Nursing Practice (DNP) program at a large Midwestern U.S. college of nursing |
Mixed methods, case study analysis with self‐explanation; reports qualitative findings. | Describe how NP students self‐explain during diagnostic reasoning | Leveraging study findings to foster diagnostic accuracy has the potential to improve diagnostic reasoning and improve patient outcomes. | Multiple clinical and biological inferential reasoning processes are used by novice as compared with more experienced NP students in diagnostic reasoning. Inferential reasoning approaches identified: risk stratifying; principle‐based reasoning; ruling out organ system or diagnosis; prioritizing information; connecting clinical information to organ system or diagnosis; classifying information; biological inferences |
|
Burt, Finnegan, et al. (2021) |
37 RNs enrolled in the FNP option of the Doctor of Nursing Practice (DNP) program at a large Midwestern U.S. college of nursing | Mixed methods, case study analysis with self‐explanation; reports quantitative findings | (a) Explore relationships between ways of self‐explaining and diagnostic accuracy levels and (b) compare differences between students of varying expertise in terms of self‐explaining and diagnostic accuracy | Leveraging study findings to foster diagnostic accuracy has the potential to improve diagnostic reasoning and improve patient outcomes. | Experienced NP students demonstrated greater use of clinical and biological inferential reasoning in their diagnostic reasoning as compared with novice NP students. |
| Calohan et al. (2016) | PMHNP students across a 2‐year curriculum | Case Report (Teaching) | Describe a longitudinal framework for PMHNP simulations to develop psychosocial assessment and management skills | Develop therapeutic communication and diagnostic reasoning skills to conceptualize, formulate and differentiate mental‐health specific diagnoses and individualized treatment plans | Three developmental simulation modules focused on therapeutic relationships, communication and biopsychosocial assessment; diagnostic reasoning and assessment; selecting appropriate therapeutic interventions |
| Colella and Beery (2014) | 150 distance learning and 141 on‐site NP students participating in a differential diagnosis course | Case Report (Teaching) with mixed methods cross‐sectional evaluation | Evaluate learning outcomes for distance as compared with on‐site learners on the accuracy of the differential diagnosis using virtual interactive case studies | Generation of an accurate list of possible diagnoses; Making the correct diagnosis; develop a working knowledge of the reasoning process | Compares outcomes for live standardized vs. virtual interactive case studies on the development of the differential. Virtual interactive case studies consisted of a simulated patient encounter with the student developing history questions, exam components, reviewing lab data and an ECG tracing and providing their diagnosis with rationale |
| Conelius et al. (2019) | 33 FNP students | Quasi‐experimental, mixed methods | Determine the effectiveness of simulated scenarios for student‐reported confidence in managing acute and chronic ‘on‐call’ scenarios | Clear, succinct communication; Incorporation of clinical knowledge; Development of appropriate differentials; Determination of management plan | Simulated “on‐call” experiences included a chief complaint and the reason for the telephone encounter with a faculty member in the role of the patient. Students were given 15 minutes to interact with the simulated patient and determine a management plan |
| Davis and Colella (2021) | Not reported | Case Report (Teaching) | Better prepare students for case presentation by introducing a structured approach | Improved student preparation in the basic skill of case presentation | Role‐play simulation on case presentation using the SNAPPS format for improved case presentation in clinical practice |
| Day et al. (2018) | 37 FNP students |
Case Report (Teaching) with detailed performance checklist |
Evaluate a video enhanced OSCE for formative assessment as compared with faculty clinical evaluation | Integration of didactic knowledge into clinical knowledge and skills | Sequential delivery of 16 video clips followed by scripted faculty questioning, with correct responses resulting in the release of the next video for progressive completion of the patient encounter. Designed for student demonstration of competency in history taking, interpretation of exam findings, differential diagnosis, formulation of management plans, patient education, consultation and referral and case presentation skills |
| Distler (2008) | NP students in the Advanced Health Assessment course |
Case Report (Teaching) w/ post‐course evaluation survey |
Describe a problem‐based learning approach for teaching health assessment, designed to improve student readiness for initial clinical experiences | Improving clinical competence; use of problem solving and hypothesis testing; diagnose and treat an ‘actor’ patient successfully | Included a presentation on the episodic visit process with video demonstrations; forums for the review of conditions and differentials; group discussion of patient scenarios; and a standardized patient encounter with a demonstration of an appropriate history, exam, determining the correct diagnosis and developing the treatment plan |
|
Downes et al. (2014) |
36 NP students in a dermatology elective course | Case Report (Teaching) | Describe a service‐learning opportunity to build competency in dermatology assessment and management | Prepare students for competency in the assessment and management of dermatologic conditions | 10 online modules focusing on dermatopathology, therapeutics, and legal/ethical issues of farm worker communities; interprofessional meetings and debriefings; dermatology service‐learning clinical experience at a migrant farm community with a focus on history taking, physical exam, correct identification of common skin conditions, appropriate treatment selection, presentation to faculty and encounter documentation |
| Durham et al. (2014) | 63 ANP and FNP students | Case Report (Teaching) | Describe a problem‐based learning approach to teaching dual process thinking in diagnostic reasoning |
Accelerating the development of diagnostic reasoning skills; foster the development of pattern recognition; reinforces the step‐wise diagnostic reasoning process of analytic reasoning; reorganization of learned cognitive patterns |
Four sets of PBL case studies with similar presenting signs and symptoms but differing diagnoses were presented over sequential 2‐week periods; illness script assignments were completed for the 1st and 3rd sets |
| Gatewood and De Gagne (2019) | 32 articles examining the One‐Minute Preceptor (OMP) model of providing clinical feedback | Systematic review | Integrate the current literature on the OMP approach to fostering students' development of clinical competence; identify relevance and utility for NPs | Emphasizes teaching and assessing cognitive skills, such as differential diagnosis, management plans and the presentation of diseases; improved critical thinking and student involvement in decision making | Major contributions of the OMP model are listed as improvement in clinical feedback; increased focus on cognitive skills and clinical reasoning; improved incorporation into the practice of 5 microskills (get a commitment, probe for evidence, teach a general rule, reinforce what was done well, correct mistakes) |
| Gorton and Hayes (2014) | 50 NP students from across the US | A cross‐sectional online survey using standardized critical thinking and clinical judgement instruments as compared with preceptor evaluations | Describe the relationship between critical thinking and clinical judgement in advanced practice nursing students | Ability to perform an accurate clinical assessment, identify patients' problems, and develop an appropriate plan of care are key components of practice; demonstrate clinical decision‐ making skills in the development of the differential diagnosis | The study found no statistically significant relationship between critical thinking skills as measured by the CCTST and clinical decision making as measured by the CDMNS. Highlights the challenge of defining critical thinking in advanced practice nursing and identifying appropriate outcome measures. |
| Granger et al. (2018) | NP students in health assessment and adult health didactic courses | Case Report (Teaching) | Describe unfolding case studies used to foster clinical reasoning abilities | Develop clinical reasoning and analytical skills necessary to deliver evidence‐based, holistic care in complex situations | 28 longitudinal unfolding case studies were introduced in faculty‐facilitated small groups in the health assessment course. In different groups in the adult health theory course, students completed the case studies including differential diagnosis and comprehensive management plans |
| Jeffries et al. (2011) | 36 1st year advanced practice nursing students across four universities | One‐group pre‐to‐post‐intervention design | Develop, implement, and evaluate outcomes of a cardiovascular assessment curriculum for advanced practice nurses at four institutions | Carry out accurate and appropriate patient assessments with identification of critical findings, including for the cardiovascular system | Development of a deliberate practice cardiovascular assessment curriculum; 12 cardiovascular case scenarios; completion of pretests to measure cardiovascular knowledge and physical assessment skills; an 8‐hour instructor‐led session combining didactic content and high‐fidelity simulator practice; followed by posttests measuring cardiovascular knowledge and physical assessment skills. The curriculum was found to increase students' skills in cardiovascular assessment and diagnostic reasoning |
| John et al. (2012) | 37 PNP and 40 FNP students | Case Report (Teaching) with repeat measures comparative design | Describe the diagnostic accuracy and self‐reported confidence levels of NP students using a diagnostic decision support system (DDSS) over their educational program and evaluate differences between PNP and FNP students | Use of diagnostic decision support to improve diagnostic accuracy | The Isabel IDEAS DDSS was implemented together with online cases into PNP and FNP curricula. Key history components and supporting diagnostics were entered into the Isabel IDEAS system. Information was provided about each differential diagnosis together with rationale, and each case's treatment was outlined including therapeutic interventions, counselling and education, health maintenance, referrals and follow‐up care |
| Johnson et al. (2018) | 15 FNP students in the initial advanced family nursing course | Case Report (Teaching) with pre‐to‐post intervention design | Describe the adequacy of interactive case studies (ICSs) to increase confidence in clinical decision making and presenting patient information to the preceptor | Confidence in making clinical decisions and presenting patient information to the clinical preceptor | Three ICSs were delivered, beginning with the CC and requiring students to identify components of the HPI, medical history, ROS and differential diagnoses. Exam findings were provided; students selected diagnostic testing, received results, determined a final diagnosis and documented their findings. Didactic content on presenting the patient to the preceptor was also provided. Students practised presenting the patient in role‐play. Student confidence levels increased in the five areas of collecting a focused health history, assessing the HEENT system, assessing the lungs, developing differential diagnoses, and presenting to the preceptor |
| Kelley et al. (2007) | 139 school/ faculty members of the National Health Service Corps Nurse Practitioner Faculty Advocate Network | Cross‐sectional survey, mixed methods | Describe advanced health assessment course content, curricular placement, teaching strategies and differences from undergraduate health assessment | Advanced practice nursing students extend RN health assessment skills by identifying causes of abnormal findings formulating a differential diagnosis | Major content areas were health history and interviewing, physical examination and developmental and functional assessment, with graduate health assessment courses characterized by increased depth and comprehensiveness, accompanied focus on differential diagnosis and abnormal findings |
| LaManna et al. (2019) | Not applicable | Review of literature and description of teaching strategies | Describe strategies and lessons learned by NP faculty to improve competence in diagnostic reasoning | Core competencies for NP practice include differentiating normal from abnormal findings, generating diagnostic hypotheses, utilizing diagnostic tests to formulate diagnoses, safe prescribing and effective verbal and written communication | Progressively complex simulated learning activities including episodic/ problem‐based patient evaluations, simulated on‐call experiences and decision‐tree exercises to support the development of diagnostic reasoning competencies |
| Lawson (2018) | 26 articles addressing the concept of coming to a medical diagnosis by NPs, NP students, physicians, physician assistants and medical students | Review of literature with theoretical sampling | Review the literature on diagnostic reasoning to discuss threats to diagnostic accuracy | The complex cognitive process used by clinicians to ascertain a correct diagnosis and prescribe appropriate treatment | An explicit definition of diagnostic reasoning is generally not provided. Common themes included cognitive biases and debiasing strategies, dual process theory, diagnostic error and patient harm. There is a lack of literature surrounding the diagnostic reasoning of NPs |
| Luke et al. (2021) | 95 primary care NP students in their 3rd clinical semester | Case Report (Teaching) with post‐activity evaluation | Implement virtual OSCEs using SPs and facilitate faculty evaluation of NP student clinical learning objectives | Demonstration of student clinical competence using a virtual OSCE platform | Virtual OSCE is used to evaluate student clinical competencies with emphasis on history taking, focused physical exam, formulating differential diagnoses, management and communication |
| Merritt (2020) | 17 FNP and PNP students in a 2nd semester diagnosis and management course | Case Report (Teaching) with cross‐sectional and pre‐post evaluation design | Measure and compare diagnostic accuracy and self‐reported competence of NP students using a simulated, computer‐based paediatrics visit using text messaging | Prepare nurse practitioner graduates to deliver safe and effective patient care using virtual visits. | Computer‐based text messaging simulation with care provider questions and caregiver responses, with the goal for the student to collect appropriate virtual history and physical exam information and develop a correct diagnosis and management plan |
| Moore and Hawkins‐Walsh (2020) | 8 FNP students | Case Report (Teaching) with faculty evaluation of student performance |
Pilot the use of an entrustable professional activities (EPA)‐based method of assessing NP student clinical competence via simulated clinical experiences |
Demonstration of entrustable clinical performance on the six designated EPAs. | Eight clinical scenarios were designed to assess student clinical competencies on six EPAs: gathering the history and performing the physical exam; prioritizing the differential diagnosis; recommending and interpreting diagnostic screening tests; entering and discussing orders; documenting the encounter; presenting the clinical encounter |
| O'Rourke and Zerwic (2016) | 52 NP students enrolled in their final semester and graduates in 3 months of program completion | Validity/ reliability testing using unfolding case studies (UCS) performance scores | Describe the development and initial reliability and validity testing of two UCSs and associated grading rubrics as a method to assess the decision‐making skills of NP students | Develop valid and reliable methods for evaluating NP students' clinical decision making | UCSs at two levels of complexity were developed around processes of data collection, data interpretation, and data evaluation with students asked to provide the most pertinent history questions and exam components, early differentials and relevant diagnostic testing, and development of a tentative final diagnosis |
| Payne (2015) | FNP and CNM students in the 2nd semester of the APRN program | Case Report (Teaching) | Describe the experience of introducing advanced practice registered nurses as specialized standardized patients (SSPs) into an advanced health assessment course to foster improved development of differential diagnoses | Ability to merge the patient history, chief complaint, and physical exam findings to develop differential diagnoses | Use of SPs with formal education above that of the student in simulated encounters to combine clinical skills with clinical reasoning focused on differential diagnosis development. SSPs were able to assist the student to broaden their thinking and evaluation, as well as correct their exam techniques |
| Pearson et al. (2012) | Not applicable | Case Report (Teaching) | Describe the process of designing a progressive NP student clinical evaluation tool based on competencies | Active involvement in critical thinking and clinical reasoning; ability to reason through complex, multifaceted problems, and to recognize potential and actual complications | Development of a 22‐item progressive clinical evaluation tool based on NONPF competencies, including (amongst others) appropriate history taking, appropriate and accurate physical exam, and diagnostic testing; formulates the differential; arrives at correct diagnosis; develops appropriate management plan |
| Posey et al. (2018) | 41 FNP and AGACNP students who had completed an advanced health assessment and diagnostic reasoning course | Four‐group randomized crossover design | Evaluate NP students' diagnostic reasoning performance in telehealth‐enabled (TSPE) versus face‐to‐face (FSPE) SP encounters using the Diagnostic Reasoning Assessment (DRA) tool |
Diagnostic reasoning is the ability to make an actionable diagnosis based on clinical data and is one of many essential NP independent practice competencies; the use of advanced assessment skills to differentiate between normal, variations of normal and abnormal findings and to employ screening and diagnostic strategies to develop correct diagnoses |
Participants were randomly assigned to one of four treatment groups: FSPE/pneumonia first, TSPE/pneumonia first, FSPE/asthma first or TSPE/asthma first; and exposed to two SP encounters. Faculty evaluators used the DRA to rate students' observed diagnostic reasoning performance and SOAP notes, and assessed whether their diagnoses were correct. Students who experienced TSPE first had significantly lower DRA scores than on their subsequent FSPE encounters; students who experienced either asthma or FSPE first were more likely to obtain the right diagnosis. Students were able to demonstrate equivalent diagnostic reasoning in TSPE and FSPE encounters |
| Quinlin et al. (2021) | 103 online FNP students | Case Report (Teaching) | Describes the development and implementation of an e‐visit OSCE to evaluate students' ability to provide care by telehealth. | Demonstration of competency in completing a simulated telehealth visit | Addresses history taking, analysis of findings, diagnosis, establishment of evidence‐based treatment plan and patient self‐management of illness |
| Raterink (2016) | Students in clinical experiences of a master's NP program over two semesters | Case Report (Teaching) | Describe reflective journaling as a tool to promote the development of critical thinking habits of mind and cognitive skills, to improve clinical decision making in NP students | Critical reflection is a way of developing clinical reasoning and imagination to help students examine what happened and what to consider when confronted with another similar clinical situation | Uses the Scheffer & Rubenfeld (2000) consensus statement on critical thinking in nursing to define habits of mind and cognitive skills. Implements of a three‐step reflective journaling activity to develop clinical reasoning: (1) description of a clinical vignette as reflective of a critical thinking habit or skill; (2) reflection on how the vignette may or may not support the specified element; (3) identification of alternative courses of action in a similar situation |
| Reinoso et al. (2018) | Students in 1st clinical rotation of the NP program | Case Report (Teaching) | Describe differential concept mapping as an approach to promote the development of deductive and inductive reasoning used in NP practice differential diagnosis, and clinical reasoning | Apply clinical reasoning to formulate the initial list of potential diagnoses and work through the evolving process to determine the correct diagnosis; making consistent, sound clinical decisions; skilled use of reasoning to analyse and synthesize clinical information in the context of a patient presentation | Symptom‐based template designed to foster differential diagnosis and NP clinical reasoning by replicating NP clinical thinking processes. The template assists the student to move from a chief complaint to potential diagnoses to intentional history gathering to priority exam components to diagnostic testing, resulting in a narrowed differential and final diagnosis |
| Schumaker and Bergeron (2016) | Not applicable | Case Report (Teaching) | Describe the use of the “clock model” for teaching clinical reasoning to NP students in the emergency department | Clinical reasoning involves both the use of the scientific method to analyse information and pattern recognition to deliberately reach a clinical decision; diagnostic reasoning is the complex process used to gather and analyse patient information, evaluate its significance, and weigh alternative actions | Embeds the concept of time in clinical reasoning by presenting clinical reasoning as a logical progression of 12 steps for information analysis and pattern recognition to reach a deliberate and timely clinical decision |
| Shawler (2008) | PMHNP students | Case Report (Teaching) | Describe the use of a series of simulated SP clinical scenarios with PMHNP students to build diagnostic reasoning skills | Build diagnostic reasoning skills to conceptualize case formulations and examine differential diagnoses related to mental disorders | Students received didactic content on a specific mental health disorder including assessment, diagnostic and screening tools. Videorecorded simulated SP encounters were conducted, followed by a student and faculty review of the recordings. Students self‐evaluated their interview skills, determined SP information critical to the diagnosis and determined working diagnoses for each scenario and additional data needed. A final and more complex scenario was accompanied by a comprehensive paper involving DSM categorization of data, formulation of a care plan and discussion of developmental issues |
| Surjadi et al. (2019) | AGPCNP students | Case Report (Teaching) | Describe AGPCNP curriculum reform using competency‐based clinical education including an entrustable professional activities (EPA) assessment process and evaluation tool to assess readiness for unsupervised clinical practice | Readiness for unsupervised clinical practice; Participation in increasingly complex practice‐based teaching/learning experiences and evaluations in a developmentally appropriate manner. | The EPA assessment tool focused on 6 major competencies: information gathering, physical examination, clinical judgement/ assessment, management plan, professionalism and overall clinical competence. Students improved in all competencies with the greatest improvements seen in the areas of clinical judgement/ assessment and management plan |
| Sweeney et al. (2017) | 1715 paid NP malpractice claims | Retrospective analysis of the National Practitioner Data Bank (NPDB) Public Use Data file | Analysis of NPDB malpractice data to characterize the most serious medical errors committed by NPs and identify opportunities to improve the NP curriculum | Formulating and revising nursing education curriculum to specifically address error‐prone clinical processes and situations | The most common type of error was diagnosis‐related, with ‘failure to diagnose’ and ‘delay to diagnosis’ contributing to the largest proportion of errors and “misdiagnosis” accounting for a small number of errors. Common themes of the malpractice claims demonstrating areas of weakness or deficiency included (1) patient‐provider communication, (2) ordering appropriate diagnostic tests and (3) referral and consultation |
| Tiffen et al. (2014) | 10 key informants and three published content experts | Review of literature with the key informant and expert panel survey and revision | Describe the process and outcomes of developing a preliminary definition and framework of NP clinical decision making. | Clinical decision making is a contextual, continuous, and evolving process, where data are gathered, interpreted and evaluated to select an evidence‐based choice of action | Defines NP clinical decision making as “a contextual, continuous, and evolving process, where data are gathered, interpreted and evaluated to select an evidence‐based choice of action.” The framework of clinical decision making depicts the clinician enacting four cognitive processes of data gathering, data interpretation, data evaluation, and decision choice in a fluid process influenced by attributes of the decision maker |
|
Weber and Snow (2006) |
NP faculty | Case Report (Teaching) | Describe an introductory PMHNP clinical management course included across all NP specialties | Recognize symptoms of common psychiatric disorders, know how to treat less complex mental illnesses, and know when to refer to psychiatric mental health providers | Focuses on screening, assessment, and treatment of major depression, postpartum depression, anxiety disorders, attention‐deficit/hyperactivity disorder (ADHD), delirium, dementia, and depression in the elderly, substance use screening, violence prevention, grief, end‐of‐life issues, mental status assessment techniques across the lifespan, use of complementary therapies, legal/ ethical issues about the right to refuse treatment and use of appropriate documentation |
4.2. Description of reviewed articles
The majority of papers were case reports of teaching interventions (n = 26; 63%), describing innovative teaching strategies aimed at enhancing NP students' clinical skills and decision‐making. Two additional papers (Billings & Kowalski, 2008; LaManna et al., 2019) were evidence‐based descriptions of teaching strategies without case‐based application.
The case reports varied in content, scope and teaching methodologies, as well as in their inclusion or evaluation of data. Authors used several common terms to describe the desired outcomes in NP student performance, most frequently including clinical reasoning (Ballman et al., 2016; Colella & Beery, 2014, Granger et al., 2018), diagnostic reasoning (Calohan et al., 2016; Durham et al., 2014; Schumaker & Bergeron, 2016; Shawler (2008; Weber & Snow, 2006) and critical thinking (Pearson et al., 2012; Raterink, 2016; Reinoso et al., 2018). Only two articles (Durham et al., 2014; Reinoso et al., 2018) directly discussed the two types of thinking that students engage in to develop the working diagnosis: type one (non‐analytic pattern recognition) and type two (analytic hypothetico‐deductive) thinking. Most of the case reports took place in one institution with convenience samples of various sizes. When specialty was reported, family NPs (FNPs; n = 9) were the most common specialty included in the case reports (Beckham, 2013; Benbenek et al., 2016; Day et al., 2018; Distler, 2008; Durham et al., 2014; John et al., 2012; Johnson et al., 2018; Luke et al., 2021; Quinlin et al., 2021). Later articles highlighted innovations developed in response to the COVID‐19 pandemic and/or to enhance learning for distance students. See Table 3 for descriptions of the educational interventions and measures used to assess DR‐related competencies.
TABLE 3.
DR‐related educational interventions and assessment measures used
| Educational intervention | Author (year) |
|---|---|
| Simulations | Bradford et al. (2021); Conelius et al. (2019); Calohan et al. (2016); Jeffries et al. (2011); LaManna et al. (2019); Merritt (2020); Payne (2015); Posey et al. (2018); Shawler (2008); Weber and Snow (2006); Davis and Colella (2021); |
| Objective structured clinical examinations (OSCEs) | Benbenek et al. (2016); Beckham (2013); Bradford et al. (2021); Calohan et al. (2016); Day et al. (2018); Luke et al. (2021); Payne et al. (2015); Quinlin et al. (2021); Shawler, (2006) |
| Interactive and unfolding case studies | Ballman et al. (2016); Colella and Beery (2014); Granger et al. (2018); John et al. (2012); Johnson et al. (2018) |
| Focused assignments and activities | Durham et al. (2014); Billings and Kowalski (2008); LaManna et al. (2019); Reinoso et al. (2018; John et al. (2012) |
| Problem‐based learning (PBL) | Distler (2008); Durham et al. (2014) |
| Role play scenarios | Davis and Colella (2021; Johnson et al. (2018); Merrit (2020) |
| Service‐learning clinic | Downes et al. (2014) |
| Assessment measures | |
| Faculty‐developed practice performance evaluation tool | Beckham (2013); Benbenek et al. (2016); Day et al. (2018); O'Rourke and Zerwic (2016); Payne (2015); Posey et al. (2018); Weber and Snow (2006); Moore and Hawkins‐Walsh (2020) |
| Student self‐perception | Conelius et al. (2019); Jeffries et al. (2011); John et al. (2012); Johnson et al. (2018); Merritt (2020); Shawler (2008) |
| Student satisfaction | Day et al. (2018); Distler (2008); Downes et al. (2014); Jeffries et al. (2011); Luke et al. (2021) |
| Assignment scoring | Colella and Beery (2014); Durham et al. (2014); Granger et al. (2018); John et al. (2012) |
| Faculty clinical evaluation |
Downes et al. (2014); Pearson et al. (2012); Surjadi et al. (2019) |
| Faculty feedback | Calohan et al. (2016); Shawler (2008) |
| Standardized patient feedback | Benbenek et al. (2016); Calohan et al. (2016); Shawler (2008) |
| Objective testing | Jeffries et al. (2011); Merritt (2020) |
| Preceptor evaluation | Gorton and Hayes (2014) |
| Self‐reflection | Raterink 2016 |
| Student peer feedback | Calohan et al. (2016) |
| Clinical papers | Weber and Snow (2006) |
| Course grades | Beckham (2013) |
Thirteen papers were reports of primary research. All but two studies were published in the past seven years. The research papers varied in design and included qualitative (n = 2; Burt, Corbridge, et al., 2021; Tiffen et al., 2014), quantitative (n = 6; Burt, Finnegan, et al., 2021; Gorton & Hayes, 2014; Jeffries et al., 2011; O'Rourke & Zerwic, 2016; Posey et al., 2018; Sweeney et al., 2017), mixed methods (n = 2; Conelius et al., 2019; Kelley et al., 2007), and literature reviews (n = 3; Burt & Corbridge, 2018; Gatewood & De Gagne, 2019; Lawson, 2018). Like the case reports, the research typically evaluated a teaching strategy, using convenience samples recruited from individual NP programs in which the reported innovation/intervention or study took place. The NP specialties represented and student placement in the program varied across the studies. Four studies (Burt, Corbridge, et al., 2021; Burt, Finnegan, et al., 2021; Lawson, 2018; Posey et al., 2018) specifically addressed an aspect of DR. Amongst the literature reviews, all but one addressed teaching strategies.
4.3. Themes identified from the included articles
Three main content themes were identified in the review: (1) Commonly referenced DR components include conducting a focused, intentional history and exam, identifying the differential diagnosis, determining a working or final diagnosis and developing an evidence‐based plan of care; (2) ‘Clinical Reasoning’ and ‘diagnostic reasoning’ are the most commonly identified conceptualizations of the cognitive process for NP practice; (3) Attention to the development of clinical thinking is a highly valued NP curricular outcome with multiple teaching strategies used.
4.3.1. Commonly referenced DR components
Whether or not the paper specifically endorsed DR as its conceptual framework or utilized language specific to DR frameworks, strong elements of DR were identified in virtually all of the papers (see Table 4). These included: patient‐provider interaction (n = 11); focused and hypothesis‐directed history‐taking (n = 22) or physical exam (n = 20); appropriate and relevant differential diagnosis with rationale (n = 17); illness script or schema for knowledge organization and pattern recognition (n = 2); articulation of concise and accurate patient presentation (n = 8); appropriate and relevant diagnostic testing (n = 11); determining the working diagnosis (n = 15); developing an evidence‐based, patient‐centred management plan (n = 16); specifying next steps and appropriate follow‐up (n = 3); consultation and/or referral as needed (n = 5); providing clear and appropriate health promotion; education and counselling (n = 5); reflection and metacognition (n = 7); developing advanced integrative thinking skills (n = 16). Table 4 provides a listing of each of the articles representing these DR components, their expected outcomes, and how the component was taught or evaluated.
TABLE 4.
. Diagnostic reasoning‐related content included in primary care NP education
| DR‐related content area | References | Expected component outcomes | How taught (T) / evaluated (E) |
|---|---|---|---|
| Patient‐Provider Interaction |
Beckham (2013); Benbenek et al. (2016; Calohan et al. (2016); Conelius et al. (2019); Downes et al. (2014); LaManna et al. (2019); Pearson et al. (2012); Schumaker and Bergeron (2016); Shawler (2008); Surjadi et al. (2019); Sweeney et al/ (2017) |
Organization of the encounter; strong empathy, connection and interaction with patient; open‐ended questions; minimal medical jargon; clear communication; effective therapeutic communication; respect for patient dignity and worth; therapeutic communication and relationship building; communicates effectively with team members; demonstrates cultural awareness and sensitivity; reviews chart prior to patient encounter; completes the encounter in a timely manner; maintains professional standards; Sets the context for further interaction; determine the meaning of the illness to the patient and assess this in realms that address the whole person; effective interviewing strategies to calm, focus and reassure the anxious patient; communication techniques that foster patient confidence and trust; professional and respectful interactions with patients and members of the interprofessional team; responsible and follows through on tasks; recognizing and overcoming barriers to practicing patient‐centred care in the current demanding health care delivery system |
OSCEs (T, E); Capstone OSCEs (E); Developmental OSCEs (T, E); Simulated “on‐call” scenarios (T); Service‐learning clinic (T, E); Use of the clock model (T); Simulated PMHNP SP clinical scenarios (T, E); Entrustable professional activities assessment process and evaluation tool (E); Education to prevent medical error (T); |
| Focused and hypothesis‐directed history taking |
Ballman et al. (2016); Beckham (2013); Benbenek et al. (2016; Colella and Beery (2014); Conelius et al. (2019); Day et al. (2018); Distler (2008); Downes et al. (2014); Durham et al. (2014); Granger et al. (2018); John et al. (2012); Johnson et al. (2018); LaManna et al. (2019); Merritt (2020); O‐Rourke & Zerwic (2016); Payne (2015); Pearson et al. (2012); Posey et al. (2018); Reinoso et al. (2018); Schumaker and Bergeron (2016); Shawler (2008); Surjadi et al. (2019) |
Patient‐centred, organized, appropriately focused, validated; pertinent positives and negatives in the differential; systematic and comprehensive for CC; demonstrates knowledge of underlying pathophysiology; recognize the connection between pathology and physical findings; appropriate level of specificity vs comprehensiveness; identify the chief complaint and patient's motivation for seeking care; develop an overall idea of who the patient is; accurate, complete symptom description |
Simulated virtual encounters (T); OSCEs (T, E); Capstone OSCEs (E); Simulated “on‐call” scenarios (T); Video‐enhanced OSCEs (T, E); problem‐based learning (T, E); Service‐learning clinic (T, E); problem‐based learning with illness script assignments (T, E); longitudinal unfolding case studies (T, E); Isabel IDEAS DDSS implementation (T, E); interactive case studies with preceptor presentation (T); computer‐based text messaging simulation (T, E); unfolding case studies (E); clinical reasoning‐focused primary care case studies (T); differential concept map activities (T); use of the clock model (T); simulated PMHNP SP clinical scenarios (T, E); entrustable professional activities assessment process and evaluation tool (E) |
| Focused and hypothesis‐directed physical exam | Ballman et al. (2016); Beckham (2013); Benbenek et al. (2016; Colella and Beery (2014); Day et al. (2018); Distler (2008); Downes et al. (2014); Durham et al. (2014); Granger et al. (2018); Jeffries et al. (2011); Johnson et al. (2018); LaManna et al. (2019); Merritt (2020); O‐Rourke & Zerwic (2016); Payne (2015); Pearson et al. (2012); Posey et al. (2018); Reinoso et al. (2018); Schumaker and Bergeron (2016); Surjadi et al. (2019) |
Organized, relevant, correct technique; Coordinated and skilled; Based on the CC; Differentiates normal and abnormal findings; branching exams as indicated; recognize the connection between pathology and physical findings; mastery of the exam room equipment; Determining the level of urgency/ acuity; group symptoms and consider potential underlying causes; logical exam sequence and appropriate manoeuvres; physical exam findings are reproducible; appropriate infection control; patient respect and privacy |
Simulated virtual encounters (T); OSCEs (T, E); capstone OSCEs (E); virtual interactive case studies (T); video‐enhanced OSCEs (T, E); problem‐based learning (T, E); service‐learning clinic (T, E); problem‐based learning with illness script assignments (T, E); longitudinal unfolding case studies (T, E); deliberate practice cardiovascular assessment curriculum (T, E); interactive case studies with preceptor presentation (T); computer‐based text messaging simulation (T, E); unfolding case studies (E); clinical reasoning‐focused primary care case studies (T); differential concept map activities (T); use of the clock model (T); entrustable professional activities assessment process and evaluation tool (E) |
| Appropriate and relevant differential diagnosis with rationale |
Ballman et al. (2016); Benbenek et al. (2016; Colella and Beery (2014); Conelius et al. (2019); Day et al. (2018); Durham et al. (2014); Granger et al. (2018); John et al. (2012); LaManna et al. (2019); O‐Rourke & Zerwic (2016); Payne (2015); Pearson et al. (2012); Posey et al. (2018); Reinoso et al. (2018); Schumaker and Bergeron (2016); Surjadi et al. (2019); Weber and Snow (2006) |
List of differentials with rationale. Ability to determine correct differential diagnoses. Appropriate based on clinical findings. Ability to interpret the know data by specifying an early differential. Identifies patients whose health needs are urgent or critical. Formulate and prioritize the differential. Analyse and interpret findings. Match findings from the patient's history and physical examination with those expected in each diagnosis. Eliminate those conditions in the differential diagnosis that do not match the patient's assessment findings. Prioritization of multiple risk factors/problems |
Simulated virtual encounters (T); OSCEs (T, E); capstone OSCEs(E); virtual interactive case studies (T); simulated ‘on‐call’ scenarios (T); video‐enhanced OSCEs (T, E); problem‐based learning with illness script assignments (T, E); longitudinal unfolding case studies (T, E); medical mystery simulation exercise (T); Isabel IDEAS DDSS implementation (T, E); unfolding case studies (E); differential concept map activities (T); use of the clock model (T); entrustable professional activities assessment process and evaluation tool (E) |
| Illness scripts or schema for clinical knowledge organization and pattern recognition |
Cognitive retrieval of pathological causes. Retrieval of domain knowledge and applying it during clinical encounters. Pattern recognition to organize discriminating features of a disease or symptom. Use of intentional strategies to organize and prioritize the differential |
Problem‐based learning with illness script assignments (T, E); VINDICATES ME mnemonic for organizing differentials (T) | |
| Articulation of concise and accurate patient presentation |
Beckham (2013); Billings and Kowalski (2008); Downes et al. (2014); Durham et al. (2014); Johnson et al. (2018); Pearson et al. (2012); Schumaker and Bergeron (2016); Surjadi et al. (2019) |
Strong, organized presentation; Includes differentials, final diagnosis, rationale, management plan. Demonstrates synthesis of information, clarity about the problem and deliberate reasoning. Succinct presentation of findings. Presentation is thorough, concise and organized. Provide a clear account of the patient's condition and care plan to other providers. Complete problem identification |
OSCEs (T, E). Argument mapping (T). Service‐learning clinic (T, E). Problem‐based learning with illness script assignments (T, E). Interactive case studies with preceptor presentation (T). Use of the clock model (T). Entrustable professional activities assessment process and evaluation tool (E) |
| Appropriate and relevant diagnostic testing |
Ballman et al. (2016); Colella and Beery (2014); Hall et al. (2010); John et al. (2012); Johnson et al. (2018); LaManna et al. (2019); O‐Rourke & Zerwic (2016); Pearson et al. (2012); Schumaker and Bergeron (2016); Shawler (2008); Weber and Snow (2006) |
Deciding what tests to order; Interpret laboratory data and diagnostic testing results. Selecting image modalities that are cost‐effective whilst detecting enough information to formulate the correct diagnosis. Determine relevant diagnostic data needed. Confirm likely diagnoses through purposeful investigation. Selection of evidence‐based diagnostic testing. Consideration of cost, risks and benefits, and sensitivity and specificity of testing |
Simulated virtual encounters (T). Virtual interactive case studies (T). PBL imaging workshop. Medical mystery simulation exercise (T). Isabel IDEAS DDSS implementation (T, E). Interactive case studies with preceptor presentation (T). Unfolding case studies (E). Use of the clock model (T). Simulated PMHNP SP clinical scenarios (T, E) |
| Determining the working diagnosis | Beckham (2013); Benbenek et al. (2016; Calohan et al. (2016); Colella and Beery (2014); Distler (2008); Downes et al. (2014); Durham et al. (2014); Johnson et al. (2018); Merrritt (2020); O‐Rourke & Zerwic (2016); Pearson et al. (2012); Posey et al. (2018); Reinoso et al. (2018); Schumaker and Bergeron (2016); Sweeney et al. (2017) | Articulates correct diagnosis with rationale. Uses evidence‐based clinical reasoning in formulating a diagnosis. Synthesize and assimilate elements of the bio‐psycho‐social assessment into conclusions that are diagnostically accurate. Correct identification of common conditions. Evaluate the data and develop a tentative final diagnosis. Develop an accurate and actionable diagnosis. Synthesize all the data to come up with an overall picture of the patient. Confirmatory process of determining both medical and nursing diagnoses. Ensuring timely diagnoses |
OSCEs (T, E). Capstone OSCEs (E). Developmental OSCEs (T, E). Virtual interactive case studies (T). Problem‐based learning (T, E). Service‐learning clinic (T, E). Problem‐based learning with illness script assignments (T, E). Medical mystery simulation exercise (T). Interactive case studies with preceptor presentation (T). Computer‐based text messaging simulation (T, E). Unfolding case studies (E). Differential concept map activities (T). Use of the clock model (T). Education to prevent medical error (T) |
| Developing an evidence‐based, patient‐centred management plan |
Benbenek et al. (2016; Calohan et al. (2016); Conelius et al. (2019); Downes et al. (2014); Durham et al. (2014); Granger et al. (2018); John et al. (2012); Johnson et al. (2018); LaManna et al. (2019); Merrritt (2020); Pearson et al. (2012); Reinoso et al. (2018); Schumaker and Bergeron (2016); Shawler (2008); Surjadi et al. (2019); Weber and Snow (2006) |
Evidence‐based, includes rationale. Negotiation of mutually acceptable plan. Develop individualized treatment plans that are evidenced‐ based and encompass patient safety. Safe prescribing. Incorporates costs in decision making. Discuss options for care. Use of evidence‐based resources and guidelines. Consider comprehensive, holistic treatment needs. Begins initial treatment protocol on the basis of the working diagnosis. Evidenced‐based therapeutic interventions; Includes patient's/caregiver's preferences related to therapeutic interventions |
Capstone OSCEs (E). Developmental OSCEs (T, E). Simulated ‘on‐call’ scenarios (T). Problem‐based learning (T, E). Service‐learning clinic (T, E). Problem‐based learning with illness script assignments (T, E). Longitudinal unfolding case studies (T, E). Medical mystery simulation exercise (T). Isabel IDEAS DDSS implementation (T, E). Interactive case studies with preceptor presentation (T). Computer‐based text messaging simulation (T, E). Clinical reasoning‐focused primary care case studies (T). Differential concept map activities (T). Use of the clock model (T). Simulated PMHNP SP clinical scenarios (T, E). Entrustable professional activities assessment process and evaluation tool (E) |
|
Specifying next steps and appropriate follow‐up |
Calohan et al. (2016); Pearson et al. (2012); Schumaker and Bergeron (2016) |
Assess the impact of treatment interventions. Establish criteria for determining treatment effectiveness. Consider the natural course of the disease, complications (natural and iatrogenic) that can arise and type of follow‐up needed to monitor and prevent or treat such complications |
Developmental OSCEs (T, E); Use of the clock model (T) |
| Consultation and/or referral as needed | Benbenek et al. (2016; Day et al. (2018); Schumaker and Bergeron (2016); Surjadi et al. (2019); Sweeney et al. (2017) |
Referral to community resources and other health disciplines; Recognition of when a condition is beyond their ability to diagnose or treat; learning the health care resource landscape of the community served; Building and accessing networks for consultation |
Capstone OSCEs (E); Video‐enhanced OSCEs (T, E). Use of the clock model (T). Entrustable professional activities assessment process and evaluation tool (E). Education to prevent medical error (T) |
|
Providing clear and appropriate health promotion, education, and counselling |
Benbenek et al. (2016; Calohan et al. (2016); Granger et al. (2018); Pearson et al. (2012); Surjadi et al. (2019) |
Providing appropriate health promotion and Counselling; Providing relevant individualized education. Appropriate screening studies. Explanation to the patient of the risks/benefits of the proposed treatment plan. Relevant health care maintenance interventions |
Capstone OSCEs (E); Developmental OSCEs (T, E). Longitudinal unfolding case studies (T, E). Entrustable professional activities assessment process and evaluation tool (E) |
|
Reflection and metacognition |
Benbenek et al. (2016; Calohan et al. (2016); Colella and Beery (2014); Granger et al. (2018); Lawson (2018); Raterink (2016); Sweeney et al. (2017) |
Develop reflective practice skills. Identify individual areas for improvement. Intentional learning from practice experiences. Learning from mistakes. Meaning making. Better understanding of the scope of their role as advanced practice nurses. Adoption of debiasing strategies to decrease diagnostic error. Develop awareness of unconscious tendencies toward nonanalytic thought and self‐monitor for when more analytic thought is necessary. Increased awareness of critical thinking components. Analyse patient safety initiatives and foster a work culture in which it is safe to report errors; Identifying actual or potential failures in processes and systems that lead to breakdowns and errors |
Capstone OSCEs (E); Developmental OSCEs (T, E). Virtual interactive case studies (T). Simulated ‘on‐call’ scenarios (T). Longitudinal unfolding case studies (T, E). Reflective journaling activity (T). Education to prevent medical error (T) |
| Development of advanced integrative thinking skills |
Benbenek et al. (2016; Billings and Kowalski (2008); Burt and Corbridge (2018); Conelius et al. (2019); Distler (2008); Durham et al. (2014); Granger et al. (2018); Raterink (2016); Schumaker and Bergeron (2016); Surjadi et al. (2019); Tiffen et al. (2014); Weber and Snow (2006) |
Evidence‐based clinical decision making. Synthesize information, think critically, use clinical evidence appropriately. Ongoing, iterative process that occurs dynamically as relationships evolve. Thinking on their feet. Use of problem‐solving and hypothesis testing. Hypothetico‐deductive, analytic reasoning processes. Dual process thinking; Management of uncertainty. Iterative process of noticing, interpreting, and responding with an emphasis on understanding the patient as a person. Use inquiry to investigate less common diagnoses. Enhanced critical thinking skills and habits to improve clinical decision making. Combined nursing process and information processing to gather and analyse patient information, evaluate its significance, and weigh alternative actions. Advocate for policy change for community‐ level primary, secondary, and tertiary prevention. Demonstrates accurate judgement, synthesis and caring in patient care. Demonstrates cost and efficiency considerations in patient care. Clinical decision making is a contextual, continuous and evolving process, where data are gathered, interpreted and evaluated to select an evidence‐based choice of action. Ethical decision making |
Capstone OSCEs (E). Argument mapping (T). Simulated ‘on‐call’ scenarios (T). Problem‐based learning (T, E). Longitudinal unfolding case studies (T, E). Medical mystery simulation exercise (T). Reflective journaling activity (T). Use of the clock model (T). Entrustable professional activities assessment process and evaluation tool (E). Conceptual framework for NP clinical decision making (T) |
4.3.2. ‘Clinical reasoning’ and ‘diagnostic reasoning’ are the most commonly identified conceptualizations of the cognitive process for NP practice
Variability was seen in the conceptual frameworks used to capture cognitive processes of problem‐solving in NP practice (see Table 5). Ten papers specifically used DR as the conceptual framework. Nine papers used clinical reasoning as the overall conceptual framework, whilst clinical decision making was used in five papers. Less frequently used terms included critical thinking and clinical judgement. Another 12 used other frameworks or were atheoretical. Table 5 provides a delineation of the cognitive conceptual frameworks used. Few of the papers provided a definition of diagnostic or clinical reasoning, though several either listed or addressed components of the NP thinking process.
TABLE 5.
Conceptualizations of the cognitive processes for NP practice
| Cognitive process for NP practice | Author (year) |
|---|---|
| Diagnostic reasoning | Burt and Corbridge (2018); Burt, Corbridge, et al. (2021); Burt, Finnegan, et al. (2021); Calohan et al. (2016); Durham et al. (2014); LaManna et al. (2018); Lawson (2018); Payne (2015); Posey et al. (2018); Shawler (2008) |
| Clinical reasoning | Ballman et al. (2016); Benbenek et al. (2016); Bradford et al. (2021); Gatewood & DeGagne (2019); Granger et al. (2018); Pearson et al. (2012); Reinoso et al. (2018); Schumaker & Bergeron, (2016); Winkelman et al. (2012) |
| Clinical decision making | Billings and Kowalski (2008); Iverson et al. (2018); Johnson et al. (2018); O'Rourke and Zerwic (2016); Tiffen et al. (2014) |
| Clinical thinking | Gorton and Hayes (2014); Pearson et al. (2012); Raterink (2016) |
| Clinical judgement | Gorton and Hayes (2014); Surjadi et al. (2019) |
4.3.3. Attention to the development of NP clinical thinking
Most of the papers in our review addressed the importance of developing clinical thinking as a highly valued curricular outcome of NP education programs with multiple teaching strategies used. In only three papers (Luke et al., 2021; Moore & Hawkins‐Walsh, 2020; Quinlin et al., 2021) was clinical thinking not directly addressed. In these papers, emphasis was placed on the demonstration of observable clinical skills rather than the cognitive processes underlying those functions. That clinical thinking or cognitive processing was a valued component of clinical problem solving could be inferred from the overall stated goal of many of the papers. See Table 2 for examples of the papers' stated overall expected outcomes, including those related to NP clinical thinking.
5. DISCUSSION
5.1. Findings based on our aims
The purpose of this review was to understand whether and how the concept of DR is addressed in NP education. The current focus on safety in healthcare in combination with expanding NP roles for meeting the world's healthcare needs intensifies the importance of preparing NPs to accurately diagnose and treat conditions and avoid the diagnostic error. Based on recommendations from the DR literature, such an initiative requires intentional curricular incorporation of DR content, competencies, and pedagogies to adequately develop the complex inferential thinking skills needed.
Despite a comprehensive search of the US literature addressing clinical reasoning in NP education, few papers directly addressed the topic of DR. Most of the papers across all clinical reasoning topics and study types were case reports of program‐specific teaching strategies to enhance student skills and decision making. Overall, the pooled body of literature represents a relatively small number of students with limited reporting on student outcomes. This lack of a robust body of literature poses challenges for educators wishing to adopt best practices and improve student learning outcomes relative to DR.
5.2. AIM 1: Extent to which the scholarly literature about clinical reasoning in nurse practitioner education includes content related to DR
Whether or not a specific focus on DR was a stated purpose of an article, numerous components of DR were identified, referenced, or alluded to in the papers. The most frequently identified element of DR in the NP education literature was the inclusion of a focused and intentional history and exam, followed by the establishment of an appropriate differential diagnosis, determining the working or final diagnosis, and developing an evidence‐based, patient‐centred management plan. Whilst reassuring to find these components of DR, they were not typically described in ways that demonstrated intentional use of a DR theoretical framework. Their incorporation into NP educational interventions was often more representative of mastering a functional approach to practice, rather than giving priority to the complex inferential thinking characterizing DR. Though many of the reports focused on distinct cognitive components of DR, the learning activity generally was not linked to an overall program of DR learning objectives.
Interestingly, the least commonly reported component of DR found in our search (use of illness scripts or schema for organizing knowledge and pattern recognition) is arguably one of the most important elements for developing accurate inferential thinking in the DR process. Information processing theory stipulates that diagnostic competency requires the ability to quickly and reliably access a well‐developed, accurate, and well‐organized clinical knowledge base, arrive at a situationally appropriate interpretation of the data and generate an appropriate and relevant differential diagnosis. From this perspective, clinical knowledge is organized into encapsulated prototypes and exemplars known as illness scripts that serve as mental constructs of disease manifestations (Charlin et al., 2007; Ledford & Nixon, 2015; Schmidt & Rikers, 2007). Retrieving the relevant clinical knowledge is known as script activation (Ledford & Nixon, 2015), which allows processes of comparison and pattern recognition, directly connecting the NP's reasoning process to the robustness and organization of their clinical knowledge base
Additionally, although the quality of the patient presentation was highlighted in several papers, none specifically framed the patient presentation from the DR perspective as an accurate and relevant problem representation statement (PRS). In DR theory, the PRS is conceptualized as the inferential and decision‐making link between clinical information from the patient encounter, the provider's clinical knowledge base, and the differential diagnosis (Bowen, 2006). A well‐formulated PRS clearly aligns the provider's interpretation of the presenting data with the relevant illness scripts, leading to the differential diagnosis as well as allowing the listener to fully understand the problem and arrive at an accurate differential (Ledford & Nixon, 2015). The PRS demonstrates the provider's ability to cognitively transform the patient's story into a meaningful clinical problem through interpretation and mental abstraction, which facilitates generating the diagnosis (Bowen, 2006). Bordage and Lemieux (1991) demonstrated that more expert diagnosticians arrive at deeper and more abstract representations of the problem, using semantic associations to interpret clinical data and generate diagnoses. This is an important distinction between the PRS of DR and the more straightforward reporting of data typical of nursing practice, distinguishing as well the difference between good and not‐so‐good diagnostic thinking. As noted by Bordage and Lemieux, in the absence of an effective PRS, multiple diagnoses were generated as signs and symptoms came and went, resulting in ‘…a list of unrelated and unexplored diagnoses with no global representation of the case’ (p. S71). For effective DR, synthesizing, qualifying and making medical inferences from the data is needed, as opposed to straightforward reporting of uninterpreted data, even if thorough, concise and organized.
5.3. AIM 2: Definition of diagnostic reasoning in primary care NP education
Overall, we did not find a standardized, conceptually grounded, or evidence‐based definition or conceptual model of DR in the NP education literature. ‘Clinical reasoning’ and ‘diagnostic reasoning’ were used with the equal frequency as the most commonly identified conceptualizations of the cognitive process for NP practice. Other terms included clinical decision making, clinical judgement and critical thinking. Rarely, however, were definitions or links to a body of literature or theory provided. Not infrequently, when terms other than DR were used, general nursing reasoning processes were referenced rather than the advanced inferential thinking and medical diagnostic skills required for DR. This finding shows a lack of consistent language and conceptualization about the cognitive process for NP practice, potentially contributing to differing and sometimes contradictory curricular goals and student outcomes.
Such a diversity of terms and conceptualizations is not surprising. Higgs (2019) argues that clinical reasoning paradigms arise from discipline‐specific cultures of professional practice, with practice‐specific ontologies and epistemologies framing professional paradigms. The knowledge of a specific profession is embedded in its practice. For NP practice, disciplinary knowledge arises from combined foundations in RN practice and medicine. Most practising NPs, NP faculty, and NP scholars, however, have a much stronger grounding in the clinical reasoning theories of nursing than in medicine. The component of NP knowledge arising from nursing is oriented to caring for person, health and environment, whilst the component adopted from medicine is oriented toward the diagnosis and treatment of disease. NP practice has thus had to innovate clinical reasoning strategies that incorporate both caring for the person and treating disease, with the cognitive habits of RN practice difficult to dislodge. In NP practice, we can see the indication of greater comfort with the clinical reasoning models from general nursing in the mostly uncritical adoption of RN clinical reasoning models. This is problematic, as the goals of general nursing differ significantly from NP practice, emphasizing care and health optimization rather than disease management and cure. Only more recently, with the increasing complexity and independence of NP practice and with the call for competency‐based NP education, has there been an intentional examination of the need for NP clinical reasoning frameworks more clearly aligned with disease management. Whilst the medical framework of DR provides a good solution, intentional incorporation of the contemporary science and theory of DR was present only in a small number of the papers in our review. It is clear that a shared understanding of DR has not yet been established across NP education.
5.4. AIM 3: Teaching methodologies used to educate NP students about diagnostic reasoning‐related knowledge, skills and/or attitudes
When DR‐related knowledge, skills, or attitudes were addressed in the papers, multiple methodologies were utilized for content delivery, including numerous high‐impact, interactive and transformational learning strategies. Despite the lack of a common language and goals specific to DR, it is clear that attention to the development of clinical thinking is a highly valued NP curricular outcome with multiple teaching strategies used. This finding corresponds well to the current literature in both medical and nursing education that clinical thinking is a core practice competency that must be intentionally and effectively taught, reinforced, role‐modelled and practised, to reliably achieve the desired clinical thinking competencies (see Cooper et al., 2021; Graber et al., 2018; Higgs et al., 2019; IOM, 2015; Trowbridge et al., 2015).
Educational interventions included interactive case studies, simulations, OSCEs, PBL, and numerous focused assignments and activities. All of these methodologies have in common an approach to teaching that emphasizes active learning and experiential approaches with practice in the application of knowledge, decision making and clinical reasoning, as recommended in best practices for competency development (Frank et al., 2010; Hodges et al., 2019). In addition to emphasizing the development of clinical skills, most of the papers included elements of debrief or reflection by students and faculty post‐implementation. Although specific outcomes of these reflective practices were infrequently described, participants valued reflection and inclusion of a feedback loop.
5.5. Summary of findings from the scoping review
Findings from this scoping review relative to teaching DR in U.S. NP education programs can be summarized as follows: (1) overall there is a dearth of U.S. NP education literature addressing DR; (2) the literature that is available demonstrates a limited conceptual understanding of the science and theory of DR; (3) DR has not yet been clearly differentiated from standard nursing clinical reasoning, which poses challenges to developing shared and systemized approaches to teaching and evaluating DR; (4) while multiple components of DR are identifiable in the literature, these rarely come together to express clear and explicit goals for student competencies around DR; (5) a robust teaching/learning scholarship for DR has not yet been established in the NP education literature. Not only has intentional curricular incorporation of DR not yet been realized, our review demonstrates that we have not yet established a shared understanding of DR and its relationship to clinical reasoning at the advanced nursing practice level. The review underscores the compelling need to develop and disseminate a more systematic approach to teaching and evaluating DR. Whilst challenging, NP scholarship about teaching DR is in need of increased scientific rigour with stronger conceptual ties to the science and principles of DR, and to pedagogical best practices.
5.6. Challenges in conducting the review
Due to the limited number of papers directly addressing DR, refinement of the addressed concept was required over time. Efforts evolved to focus on mapping terms related to the concept of DR, as the term ‘diagnostic reasoning’ was infrequently used in NP education literature. One risk of this approach was the inclusion of articles that did not directly or intentionally address DR. This was true in this scoping review and required careful consideration of the nuances of each article and its focus, to remove those that did not directly apply whilst not omitting relevant articles because of not incorporating specific terminology.
Additionally, our review utilized a descriptive qualitative thematic analysis of findings. It must be stated, however, that themes identified from a scoping review do not necessarily describe the state of the concept investigated. In our review, whilst most articles (68%) focused on innovative teaching strategies that contained elements of DR, few papers addressed the concept of DR in its entirety. Whilst apparent that components of DR are valued in NP education, simply mapping those components does not fully reflect whether DR is sufficiently addressed in NP education.
Finally, in conducting the review, we found it necessary to reduce our original study aims to the three presented in this paper. Three additional aims that focused on identifying DR‐related learning outcomes, student assessment, and educational barriers and facilitators could not be completed, as this content was insufficiently addressed in the reviewed literature. Thus, the unaccomplished aims become part of the future implications of our review.
5.7. Strengths and limitations of the review
Our scoping review has several strengths. We conducted a comprehensive search of the literature based on established methodological frameworks and in compliance with best practices. Our screening and selection process was done in duplicate by two independent reviewers, whilst our data extraction process was completed by two reviewers who extracted data from a subset of eligible studies to ensure good agreement between the extractors. Amongst the authors, two individuals have completed the Society to Improve Diagnosis in Medicine (SIDM, https://www.improvediagnosis.org/) fellowship on DR, so were well versed in the topic.
Despite the methodological strengths of this review, there are several limitations. The exclusion of articles published prior to 2005 and outside of the US may have resulted in otherwise relevant publications being eliminated from this study. Additionally, the focus on primary care NP education literature excluded articles focusing on DR in acute care NP programs, a practice domain for which this topic is also highly relevant. Finally, since scoping reviews do not require a risk of bias assessment, no conclusions about the quality of the evidence are made. The findings of the scoping review are descriptive and exploratory, demonstrating that whilst elements of DR are commonly referred to in the NP education literature, the overall concept of DR rarely occurs and methods of evaluating the elements of DR are varied and not always reported.
5.8. Recommendations and future implications
Based on our findings in comparison to calls to action for decreasing diagnostic error and increased teaching of DR, actions are needed across several sectors to support and ensure increased incorporation of DR competencies into NP education programs.
5.8.1. Faculty development
Our review suggests that NP faculty development around teaching and conducting scholarship in DR may be necessary. We speculate that stronger faculty expertise is needed in DR science, models, frameworks, language, concepts and competencies. Such expertise would assist in building shared understandings of DR and clinical reasoning, their differences and similarities, relationships between them, levelling across nursing practice, and essential student competencies. Few studies in our review used a validated measurement tool to determine if students had met appropriate learning objectives, and many used indirect measures such as student and faculty satisfaction or self‐reported knowledge or confidence levels as the primary assessment mechanism. The use of such indirect measures as a proxy for skills attainment is problematic and subject to response bias and does not address the concern for DR competency development. Specific areas for NP faculty teaching and scholarship development include a stronger focus on clinical reasoning science and theory in general and diagnostic reasoning in particular; the development of a common language for teaching, discussing and conducting research in DR; increased specificity in the development of competency‐based pedagogies for DR; and approaches for conducting more robust educational research.
5.8.2. Curriculum development
DR curriculum development is a specific need. Content for teaching and evaluating DR can be developed from the existing DR theory, science, and evolving practice guidelines. SIDM, for example, has developed an interprofessional consensus curriculum (Olson et al., 2019) with individual, team‐based and system‐level competencies. Numerous curricular components, milestones for assessing competencies, assessment/evaluation tools and robust scholarship approaches can be found both in the SIDM resources (see Thammasitboon et al., 2018) and in the literature, and are continuously evolving. NP faculty scholars will need to examine the effect of DR‐related teaching interventions on NP student learning and identify measurable outcomes that can guide the assessment of DR‐related competencies. With the development of DR content and assessment approaches for NP education, it will be vital to ensure that the signature qualities of NP practice beyond diagnostic expertise also remain foregrounded in NP education, including but not limited to priorities on patient‐centred care, health promotion and prevention, patient‐provider care partnerships and attention to comprehensive determinants of health.
5.8.3. Alignment with regulatory bodies
There is a need to increase the incorporation of DR competencies, goals and objectives into the regulatory statements of NP education, certification, licensing and accreditation bodies. Since these are the organizations whose statements and guidelines regulate core components of NP education programs, a necessary step is increased incorporation of evidence‐based DR outcome expectations into their guidelines and expectations. Best practice would base such guidelines in DR science, focused specifically on the teaching of DR.
5.8.4. Preceptor development
Preceptor development in DR may be an additional necessary component to support student learning. Whilst NPs who practice closely with medical colleagues have no doubt been exposed to practice expectations for DR, it is likely that fewer have learned specific DR language, theory, and clinical processes sufficient for intentional mentoring of NP students in these practices.
6. CONCLUSION
Although there are encouraging signs of incorporating certain components of DR into U.S. primary care NP education, considerably more work is needed to build DR as an intentional and explicit thread across NP practice and didactic curricula. Shared conceptual frameworks, content outlines, competency measures, integrated pedagogical strategies, assessment/ evaluation approaches, validated tools and research protocols are needed to document the impact of DR curricular incorporation on student outcomes. Key stakeholders (regulatory bodies, nursing publishers and NP faculty) should take action to support the incorporation of evidence‐based DR content and competencies, to strengthen the delivery of safe and effective NP care through the more focused and intentional cognitive processes that characterize DR. As NP programs build DR content and expertise, care must be taken to retain the comprehensive, holistic, and patient‐centred perspectives that characterize NP practice.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE*):
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data.
Drafting the article or revising it critically for important intellectual content.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
CONFLICTS OF INTEREST
There are no conflicts of interest by the authors.
CLINICAL RESOURCES
Society to Improve Diagnosis in Medicine, https://www.improvediagnosis.org/
Supporting information
Data S1
Smith, S. K. , Benbenek, M. M. , Bakker, C. J. , & Bockwoldt, D. (2022). Scoping review: Diagnostic reasoning as a component of clinical reasoning in the U.S. primary care nurse practitioner education. Journal of Advanced Nursing, 78, 3869–3896. 10.1111/jan.15414
Endnote
Some scholars (see Monteiro et al., 2020, for example) have argued that clinical thinking skills cannot be reliably taught; rather, the development of these skills is the result of many years of clinical experience and expertise. We take the opposite perspective: namely, that effective and well‐developed clinical thinking skills must be taught in order to develop safe and effective NP practice at the independent provider level. Such clinical thinking skills are best represented as contextualized knowing, occurring in specific patient‐provider relationships, settings, presentations, and sets of concerns, and requiring a well‐developed clinical knowledge base for application to the identified problems. The clinical thinking skills of DR and the advanced clinical knowledge base to which they are applied are inseparable. Both require extensive development through the curricula of NP education programs and continued development through experience and expertise.
DATA AVAILABILITY STATEMENT
Data methods used in the analysis, coding and materials used to conduct the research will be made available to any researcher from the corresponding author, for purposes of reproducing the results or replicating the procedure.
REFERENCES
- American Association of Colleges of Nursing . (2021). The essentials Core competencies for professional nursing education. https://www.aacnnursing.org/AACN‐Essentials
- Arksey, H. , & O'Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Audétat, M.‐C. , Laurin, S. , Sanche, G. , Béïque, C. , Fon, N. C. , Blais, J.‐G. , & Charlin, B. (2013). Clinical reasoning difficulties: A taxonomy for clinical teachers. Medical Teacher, 35(3), e984–e989. 10.3109/0142159X.2012.733041 [DOI] [PubMed] [Google Scholar]
- Ballman, K. , Garritano, N. , & Beery, T. (2016). Broadening the reach of standardized patients in nurse practitioner education to include the distance learner. Nurse Educator, 41(5), 230–233. [DOI] [PubMed] [Google Scholar]
- Beckham, N. D. (2013). Objective structured clinical evaluation effectiveness in clinical evaluation for family nurse practitioner students. Clinical Simulation in Nursing, 9(10), e453–e459. [Google Scholar]
- Benbenek, M. , Dierich, M. , Wyman, J. , Avery, M. , Juve, C. , & Miller, J. (2016). Development and implementation of a capstone objective structured clinical examination in nurse practitioner and nurse‐midwifery programs. Nurse Educator, 41(6), 288–293. [DOI] [PubMed] [Google Scholar]
- Billings, D. M. , & Kowalski, K. (2008). Teaching tips. The Journal of Continuing Education in Nursing, 39(6), 246–247.18557281 [Google Scholar]
- Bordage, G. (1994). Elaborated knowledge. Academic Medicine, 69(11), 883–885. 10.1097/00001888-199411000-00004 [DOI] [PubMed] [Google Scholar]
- Bordage, G. , & Lemieux, M. (1991). Semantic structures and diagnostic thinking of experts and novices. Academic Medicine, 66, S70–S72. [DOI] [PubMed] [Google Scholar]
- Boshuizen, H. P. A. , & Schmidt, H. G. (2019). The development of clinical reasoning expertise. In Higgs, et al. (Eds.), Clinical reasoning in the health professions (4th ed., pp. 57–65). Elsevier. [Google Scholar]
- Bowen, J. L. (2006). Educational strategies to promote clinical diagnostic reasoning. New England Journal of Medicine, 355, 2217–2225. [DOI] [PubMed] [Google Scholar]
- Braun, L. T. , Zottmann, J. M. , Adolf, C. , Lottspeich, C. , Then, C. , Wirth, S. , Fischer, M. R. , & Schmidmaier, R. (2017). Representation scaffolds improve diagnostic efficiency in medical students. Medical Education, 51(11), 1118–1126. 10.1111/medu.13355 [DOI] [PubMed] [Google Scholar]
- Bradford, H. M. , Farley, C. L. , Escobar, M. , Heitzler, E. T. , Tringali, T. , & Walker, K. C. (2021). Rapid Curricular Innovations During COVID‐19 Clinical Suspension: Maintaining Student Engagement with Simulation Experiences. Journal of Midwifery and Women’s Health, 66(3), 366–371. [DOI] [PubMed] [Google Scholar]
- Burt, L. , & Corbridge, S. (2018). Teaching diagnostic reasoning: A review of evidence‐based interventions. International Journal of Nursing Education Scholarship, 15(1), 1–3. 10.1515/ijnes-2018-0003 [DOI] [PubMed] [Google Scholar]
- Burt, L. , Corbridge, S. , Corte, C. , Quinn, L. , & Finnegan, L. (2021). Ways that nurse practitioner students self‐explain during diagnostic reasoning. Diagnosis, 9(1), 40–49. 10.1515/dx-2020-0136 [DOI] [PubMed] [Google Scholar]
- Burt, L. , Finnegan, L. , Schwartz, A. , Corte, C. , Quinn, L. , Clark, L. , & Corbridge, S. (2021). Diagnostic reasoning: Relationships among expertise, accuracy, and ways that nurse practitioner students self‐ explain. Diagnosis, 9(1), 50–58. 10.1515/dx-2020-0137 [DOI] [PubMed] [Google Scholar]
- Calohan, J. , Pauli, E. , Combs, T. , Creel, A. , Convoy, S. , & Owen, R. (2016). Using simulation in a psychiatric mental health nurse practitioner doctoral program. Journal of Professional Nursing: Official Journal of the American Association of Colleges of Nursing, 32(6), 458–462. [DOI] [PubMed] [Google Scholar]
- Castillo, J.‐M. , Park, Y. S. , Harris, I. , Cheung, J. J. H. , Sood, L. , Clark, M. D. , Kulasegaram, K. , Brydges, R. , Norman, G. , & Woods, N. (2018). A critical narrative review of transfer of basic science knowledge in health professions education. Medical Education, 52(6), 592–604. 10.1111/medu.13519 [DOI] [PubMed] [Google Scholar]
- Chang, R. W. , Bordage, G. , & Connell, K. J. (1998). The importance of early problem representation during case presentations. Academic Medicine, 73(10), S109–S111. [DOI] [PubMed] [Google Scholar]
- Charlin, B. , Boshuizen, H. P. , Custers, E. J. , & Feltovich, P. J. (2007). Scripts and clinical reasoning. Medical Education, 41, 1178–1184. [DOI] [PubMed] [Google Scholar]
- Colella, C. L. , & Beery, T. A. (2014). Teaching differential diagnosis to nurse practitioner students in a distance program. Journal of Nursing Education, 53(8), 433–438. [DOI] [PubMed] [Google Scholar]
- Conelius, J. , Grossman, S. , & Becht, L. (2019). Interprofessional “on‐call” e‐learning for family nurse practitioner students: Preparing for primary care across the life span. Journal of the American Association of Nurse Practitioners, 31(2), 104–109. [DOI] [PubMed] [Google Scholar]
- Connor, D. M. , & Dhaliwal, G. (2015). When less is more for the struggling clinical reasoner. Diagnosis, 2(3), 159–162. 10.1515/dx-2015-0014 [DOI] [PubMed] [Google Scholar]
- Cooper, N. , Bartlett, M. , Gay, S. , Hammond, A. , Lillicrap, M. , Matthan, J. , & Singh, M. (2021). Consensus statement on the content of clinical reasoning curricula in undergraduate medical education. Medical Teacher, 43(2), 152–159. 10.1080/0142159X.2020.1842343 [DOI] [PubMed] [Google Scholar]
- Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78(8), 775–780. 10.1097/00001888-200308000-00003 [DOI] [PubMed] [Google Scholar]
- Croskerry, P. (2009). A universal model of diagnostic reasoning. Academic Medicine, 84(8), 1022–1028. 10.1097/ACM.0b013e3181ace703 [DOI] [PubMed] [Google Scholar]
- Custers, E. J. F. M. (2015). Thirty years of illness scripts: Theoretical origins and practical applications. Medical Teacher, 37(5), 457–462. 10.3109/0142159X.2014.956052 [DOI] [PubMed] [Google Scholar]
- Daudt, H. M. , van Mossel, C. , & Scott, S. J. (2013). Enhancing the scoping study methodology: A large, inter‐professional team's experience with Arksey and O'Malley's framework. BMC Medical Research Methodology, 13(1), 48. 10.1186/1471-2288-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, L. , & Colella, C. (2021). Use of role‐play simulation to improve nurse practitioner Students' case presentation: An innovative educational approach for the distance learner. Nurse Educator, 46(2), 63–64. 10.1097/NNE.0000000000000862 [DOI] [PubMed] [Google Scholar]
- Day, C. , Barker, C. , Bell, E. , Sefcik, E. , & Flournoy, D. (2018). Flipping the objective structured clinical examination: A teaching innovation in graduate nursing education. Nurse Educator, 43(2), 83–86. [DOI] [PubMed] [Google Scholar]
- Distler, J. W. (2008). Using problem‐based learning in teaching advanced health assessment: An innovative approach. Topics in Advanced Practice Nursing, 8(2), 3. [Google Scholar]
- Downes, E. A. , Connor, A. , & Howett, M. (2014). An innovative approach to enhance dermatology competencies for advanced practice nurses: Service‐learning with a migrant farm worker health clinic. The Journal of Nursing Education, 53(12), 710–713. [DOI] [PubMed] [Google Scholar]
- Durham, C. O. , Fowler, T. , & Kennedy, S. (2014). Teaching dual‐process diagnostic reasoning to doctor of nursing practice students: Problem‐based learning and the illness script. Journal of Nursing Education, 53(11), 646–650. [DOI] [PubMed] [Google Scholar]
- Elstein, A. S. (1999). Heuristics and biases. Academic Medicine, 74(7), 791–794. 10.1097/00001888-199907000-00012 [DOI] [PubMed] [Google Scholar]
- Englander, R. , Cameron, T. , Ballard, A. J. , Dodge, J. , Bull, J. , & Aschenbrener, C. A. (2013). Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Academic Medicine, 88(8), 1088–1094. 10.1097/ACM.0b013e31829a3b2b [DOI] [PubMed] [Google Scholar]
- Eva, K. W. (2004). What every teacher needs to know about clinical reasoning. Medical Education, 39(1), 98–106. 10.1111/j.1365-2929.2004.01972.x [DOI] [PubMed] [Google Scholar]
- Evans, J. S. B. T. (2008). Dual‐processing accounts of reasoning, judgment, and social cognition. American Review of Psychology, 59, 255–278. 10.1146/annurev.psych.59.103006.093629 [DOI] [PubMed] [Google Scholar]
- Frank, J. R. , Snell, L. S. , Ten Cate, O. , Holboe, E. S. , Carraccio, C. , Swing, S. R. , Harris, P. , Glasgow, N. J. , Campbell, C. , Deeth, D. , Harden, R. M. , Lobst, W. , Long, D. M. , Mungroo, R. , Richardson, D. L. , Sherbino, J. , Silver, I. , Taber, S. , Talbot, M. , & Harris, K. A. (2010). Competency‐based medical education: Theory to practice. Medical Teacher, 32, 638–645. 10.3109/0142159X.2010.501190 [DOI] [PubMed] [Google Scholar]
- Friel, D. D. , & Chandar, K. (2021). Teaching diagnostic reasoning to medical students: A four‐step approach. Perspectives in Biology and Medicine, 64(4), 557–586. [DOI] [PubMed] [Google Scholar]
- Gatewood, E. , & De Gagne, J. C. (2019). The one‐minute preceptor model: A systematic review. Journal of the American Association of Nurse Practitioners, 31(1), 46–57. [DOI] [PubMed] [Google Scholar]
- Gilkes, L. , Kealley, N. , & Frayne, J. (2022). Teaching and assessment of clinical diagnostic reasoning in medical students. Medical Teacher, 1–7, 650–656. 10.1080/0142159X.2021.2017869 [DOI] [PubMed] [Google Scholar]
- Gorton, K. L. , & Hayes, J. (2014). Challenges of assessing critical thinking and clinical judgment in nurse practitioner students. The Journal of Nursing Education, 53(3), S26–S29. [DOI] [PubMed] [Google Scholar]
- Graber, M. , Franklin, N. , & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165(13), 1493–1499. [DOI] [PubMed] [Google Scholar]
- Graber, M. L. , Rencic, J. , Rusz, D. , Papa, F. , Croskerry, P. , Zierler, B. , Harkless, G. , Giuliano, M. , Schoenbaum, S. , Colford, C. , Cahill, M. , & Olson, A. P. J. (2018). Improving diagnosis by improving education: A policy brief on education in healthcare professions. Diagnosis, 5(3), 107–118. 10.1515/dx-2018-0033 [DOI] [PubMed] [Google Scholar]
- Granger, T. , Zappas, M. , Walton‐Moss, B. , & O'Neilla, S. P. (2018). A patient panel of case studies to teach across the family nurse practitioner curriculum. Journal of Nursing Education, 57(8), 512. 10.3928/01484834-20180720-14 [DOI] [PubMed] [Google Scholar]
- Hasnain, M. , Bordage, G. , Connell, K. J. , & Sinacore, J. M. (2001). History‐taking behaviors associated with diagnostic competence of clerks: An exploratory study. Academic Medicine, 76(10 SUPPL), S14–S17. 10.1097/00001888-200110001-00006 [DOI] [PubMed] [Google Scholar]
- Hautz, W. E. , Kämmer, J. E. , Hautz, S. C. , Sauter, T. C. , Zwaan, L. , Exadaktylos, A. K. , Birrenbach, T. , Maier, V. , Müller, M. , & Schauber, S. K. (2019). Diagnostic error increases mortality and length of hospital stay in patients presenting through the emergency room. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 27(1), 54. 10.1186/s13049-019-0629-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgs, J. (2019). Reinterpreting clinical reasoning: A model of encultured decision‐making practice capabilities. In Higgs J., Jensen G. M., Loftus S., & Christensen N. (Eds.), Clinical reasoning in the health professions (4th ed., pp. 13–31). Elsevier. [Google Scholar]
- Higgs, J. , Jensen, G. , Loftus, S. , & Christensen, N. (Eds.). (2019). Clinical reasoning in the health professions (4th ed.). Elsevier. [Google Scholar]
- Hodges, A. L. , Konicki, A. J. , Talley, M. H. , Bordelon, C. J. , Holland, A. C. , & Galin, F. S. (2019). Competency‐based education in transitioning nurse practitioner students from education into practice. Journal of the American Association of Nurse Practitioners, 32, 675–682. 10.1097/JXX0000000000000327 [DOI] [PubMed] [Google Scholar]
- Hughes, R. (2008). Patient safety and quality: An evidence‐based handbook for nurses. Agency for Healthcare Research and Quality, US Department of Health and Human Services. [PubMed] [Google Scholar]
- Institute of Medicine . (2015). Improving diagnosis in health care. National Academies Press. 10.17226/21794 [DOI] [PubMed] [Google Scholar]
- International Council of Nurses . (2021). International nursing conference shines a spotlight on advanced practice nursing. International Council of Nurses. [Press release]. https://www.icn.ch/news/international‐nursing‐conference‐shines‐spotlight‐advanced‐practice‐nursing [Google Scholar]
- Iverson, L. , Connelly, S. , & Potthoff, M. (2018). Teaching about Zebras. Journal of Nursing Education, 57(2), 126–126. [DOI] [PubMed] [Google Scholar]
- Jeffries, P. R. , Beach, M. , Decker, S. I. , Dlugasch, L. , Groom, J. , Settles, J. , & O'Donnell, J. M. (2011). Multi‐ center development and testing of a simulation‐based cardiovascular assessment curriculum for advanced practice nurses. Nursing Education Perspectives (National League for Nursing), 32(5), 316–322. [DOI] [PubMed] [Google Scholar]
- John, R. M. , Hall, E. , & Bakken, S. (2012). Use of the Isabel decision support system to improve diagnostic accuracy of pediatric nurse practitioner and family nurse practitioner students. NI 2012: 11th International congress on nursing informatics, June 23‐27, 2012, Montreal, Canada. International congress in nursing informatics (11t:2012:Montreal, Quebec), 2012, 194. [PMC free article] [PubMed]
- Johnson, R. , Clark, R. , & O'Brien, T. (2018). Improving family nurse practitioner Students' confidence for clinical decision making and presenting patient information to the preceptor. Journal of Doctoral Nursing Practice, 11(2), 114–118. [DOI] [PubMed] [Google Scholar]
- Kassirer, J. P. (1989). Diagnostic reasoning. Annals of Internal Medicine, 110(11), 893. 10.7326/0003-4819-110-11-893 [DOI] [PubMed] [Google Scholar]
- Kelley, F. J. , Kopac, C. A. , & Rosselli, J. (2007). Advanced health assessment in nurse practitioner programs: Follow‐up study. Journal of Professional Nursing, 23(3), 137–143. [DOI] [PubMed] [Google Scholar]
- Kiesewetter, J. , Ebersbach, R. , Görlitz, A. , Holzer, M. , Fischer, M. R. , & Schmidmaier, R. (2013). Cognitive problem solving patterns of medical students correlate with success in diagnostic case solutions. PLoS One, 8(8), e71486. 10.1371/journal.pone.0071486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaManna, J. B. , Guido‐Sanz, F. , Anderson, M. , Chase, S. K. , Weiss, J. A. , & Blackwell, C. W. (2019). Teaching diagnostic reasoning to advanced practice nurses: Positives and negatives. Clinical Simulation in Nursing, 26, 24–31. [Google Scholar]
- Lambe, K. A. , O'Reilly, G. , Kelly, B. D. , & Curristan, S. (2016). Dual‐process cognitive interventions to enhance diagnostic reasoning: A systematic review. BMJ Quality and Safety, 25, 808–820. 10.1136/bmjqs-2015-004417 [DOI] [PubMed] [Google Scholar]
- Lawson, T. N. (2018). Diagnostic reasoning and cognitive biases of nurse practitioners. Journal of Nursing Education, 57(4), 203–208. [DOI] [PubMed] [Google Scholar]
- Ledford, C. H. , & Nixon, L. J. (2015). General teaching techniques. In Higgs J., Jensen G. M., Loftus S., & Christenson N. (Eds.), Teaching clinical reasoning (pp. 77–116). American College of Physicians. [Google Scholar]
- Lee, A. , Joynt, G. M. , Lee, A. K. T. , Ho, A. M. H. , Groves, M. , Vlantis, A. C. , Ma, R. C. W. , Fung, C. S. C. , & Aun, C. S. T. (2010). Using illness scripts to teach clinical reasoning skills to medical students. Family Medicine, 42(4), 255–261. [PubMed] [Google Scholar]
- Lefebvre, C. , Glanville, J. , Briscoe, S. , Featherstone, R. , Littlewood, A. , Marshall, C. , Metzendorf, M. I. , Noel‐Storr, A. , Paynter, R. , Rader, T. , Thomas, J. , & Wieland, L. S. (2022, 2022. Available from). Searching for and selecting studies. In Higgins J. P. T., Thomas J., Chandler J., Cumpston M., Li T., Page M. J., & Welch V. A. (Eds.), Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022, chapter 4). Cochrane. www.training.cochrane.org/handbook [Google Scholar]
- Luke, S. , Petitt, E. , Tombrella, J. , & McGoff, E. (2021). Virtual evaluation of clinical competence in nurse practitioner students. Medical Science Educator, 31(4), 1267–1271. 10.1007/s40670-021-01312-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamede, S. , van Gog, T. , Moura, A. S. , de Faria, R. M. D. , Peixoto, J. M. , Rikers, R. M. J. P. , & Schmidt, H. G. (2012). Reflection as a strategy to foster medical students' acquisition of diagnostic competence. Medical Education, 46, 464–472. 10.1111/j.1365-2923.2012.04217.x [DOI] [PubMed] [Google Scholar]
- Merritt, L. S. (2020). Preparing nurse practitioner students for virtual visits: An innovative computer‐ based text‐messaging simulation. Clinical Simulation in Nursing, 43, 17–20. [Google Scholar]
- Monteiro, S. , Sherbino, J. , Sibbald, M. , & Norman, G. (2020). Critical thinking, biases and dual processing: The enduring myth of generalisable skills. Medical Education, 54, 66–73. 10.1111/medu.13872 [DOI] [PubMed] [Google Scholar]
- Moore, J. , & Hawkins‐Walsh, E. (2020). Evaluating nurse practitioner student competencies: Application of entrustable professional activities. Journal of Nursing Education, 59(12), 714–720. 10.3928/01484834-20201118-11 [DOI] [PubMed] [Google Scholar]
- National Organization of Nurse Practitioner Faculties . Nurse practitioner core competencies content. National Organization of Nurse Practitioner Faculties. 2017. https://www.nonpf.org/page/14 [Google Scholar]
- Nordick, C. L. (2021). Integrating strategies for improving diagnostic reasoning and error reduction. Journal of the American Association of Nurse Practitioners, 33(5), 366–372. 10.1097/JXX.0000000000000464 [DOI] [PubMed] [Google Scholar]
- Olson, A. , Rencic, J. , Cosby, K. , Rusz, D. , Papa, F. , Croskerry, P. , Zierler, B. , Harkless, G. , Giuliano, M. A. , Schoenbaum, S. , Colford, C. , Cahill, M. , Gerstner, L. , Grice, G. R. , & Graber, M. L. (2019). Competencies for improving diagnosis: An interprofessional framework for education and training in health care. Diagnosis, 6(4), 335–341. 10.1515/dx-2018-0107 [DOI] [PubMed] [Google Scholar]
- O'Rourke, J. , & Zerwic, J. (2016). Measure of clinical decision‐making abilities of nurse practitioner students. The Journal of Nursing Education, 55(1), 18–23. [DOI] [PubMed] [Google Scholar]
- Ouzzani, M. , Hammady, H. , Fedorowicz, Z. , & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews, 10(1), 89. 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne, L. K. (2015). Using specialized standardized patients to improve differential diagnoses. The Nurse Practitioner, 40(6), 50–54. [DOI] [PubMed] [Google Scholar]
- Pearson, T. , Garrett, L. , Hossler, S. , McConnell, P. , & Walls, J. (2012). A progressive nurse practitioner student evaluation tool. Journal of the American Academy of Nurse Practitioners, 24(6), 352–357. [DOI] [PubMed] [Google Scholar]
- Posey, L. , Pintz, C. , Quiping, L. K. , Slaven‐Lee, P. , & Chen, C. (2018). Comparing nurse practitioner student diagnostic reasoning outcomes in telehealth and face‐to‐face standardized patient encounters. Journal of Nursing Regulation, 9(3), 27–35. [Google Scholar]
- Quinlin, L. , Clark, G. M. , Nikolai, C. , & Teall, A. M. (2021). Development and implementation of an e‐visit objective structured clinical examination to evaluate student ability to provide care by telehealth. Journal of the American Association of Nurse Practitioners, 33(5), 359–365. 10.1097/JXX.0000000000000409 [DOI] [PubMed] [Google Scholar]
- Rajkomar, A. , & Dhaliwal, G. (2011). Improving diagnostic reasoning to improve patient safety. The Permanente Journal, 15(3), 68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raterink, G. (2016). Reflective journaling for critical thinking development in advanced practice registered nurse students. Journal of Nursing Education, 55(2), 101–104. [DOI] [PubMed] [Google Scholar]
- Reinoso, H. , Bartlett, J. L. , & Bennett, S. L. (2018). Teaching differential diagnosis to nurse practitioner students. The Journal for Nurse Practitioners, 14(10), e207–e212. [Google Scholar]
- Rencic, J. , Trowbridge, R. L. , Fagan, M. , Szauter, K. , & Durning, S. (2017). Clinical reasoning education at US medical schools: Results from a National Survey of internal medicine clerkship directors. Journal of General Internal Medicine, 32(11), 1242–1246. 10.1007/s11606-017-4159-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt, H. G. , & Rikers, R. M. (2007). How expertise develops in medicine: Knowledge encapsulation and illness script formation. Medical Education, 41, 1133–1139. [DOI] [PubMed] [Google Scholar]
- Schober, M. , & Stewart, D. (2019). Developing a consistent approach to advanced practice nursing worldwide. International Nursing Review, 66(2), 151–153. 10.1111/inr.12524 [DOI] [PubMed] [Google Scholar]
- Schumaker, R. H. , & Bergeron, K. (2016). The clock model: A tool for clinical reasoning in the emergency department. The Journal for Nurse Practitioners, 12(7), 467–472. [Google Scholar]
- Shawler, C. (2008). Standardized patients: A creative teaching strategy for psychiatric‐mental health nurse practitioner students. Journal of Nursing Education, 47(11), 528–531. [DOI] [PubMed] [Google Scholar]
- Singh, H. , Giardina, T. D. , Meyer, A. N. D. , Forjuoh, S. N. , Reis, M. D. , & Thomas, E. J. (2013). Types and origins of diagnostic errors in primary care settings. JAMA Internal Medicine, 173(6), 418–425. 10.1001/jamainternmed.2013.2777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, H. , Meyer, A. N. D. , & Thomas, E. J. (2014). The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving US adult populations. BMJ Quality and Safety, 23(9), 727–731. 10.1136/bmjqs-2013-002627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, M. , Collins, L. , Farrington, R. , Jones, M. , Thampy, H. , Watson, P. , Warner, C. , Wilson, K. , & Grundy, J. (2021). From principles to practice: Embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. Diagnosis, 9(2), 184–194. 10.1515/dx-2021-0031 [DOI] [PubMed] [Google Scholar]
- Sorinola, O. O. , Weerasinghe, C. , & Brown, R. (2012). Preventable hospital mortality: Learning from retrospective case record review. JRSM Short Reports, 3(11), 1–10. 10.1258/shorts.2012.012077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger, S. , Praschinger, A. , Kletter, K. , & Kainberger, F. (2011). Diagnostic grand rounds: A new teaching concept to train diagnostic reasoning. European Journal of Radiology, 78, 349–352. 10.1016/j.ejrad.2009.05.015 [DOI] [PubMed] [Google Scholar]
- Surjadi, M. , Stringari‐Murray, S. , & Saxe, J. M. (2019). Entrustable professional activities in nurse practitioner education. The Journal for Nurse Practitioners, 15(5), e97–e102. [Google Scholar]
- Sweeney, C. F. , Lemahieu, A. , & Fryer, G. E. (2017). Nurse practitioner malpractice data: Informing nursing education. Journal of Professional Nursing, 33(4), 271–275. [DOI] [PubMed] [Google Scholar]
- Thammasitboon, S. , Rencic, J. J. , Trowbridge, R. L. , Olson, A. P. J. , Sur, M. , & Dhaliwal, G. (2018). The assessment of reasoning tool (ART): Structuring the conversation between teachers and learners. Diagnosis, 5(4), 197–203. 10.1515/dx-2018-0052 [DOI] [PubMed] [Google Scholar]
- Thampy, H. , Willert, E. , & Ramani, S. (2019). Assessing clinical reasoning: Targeting the higher levels of the pyramid. Journal of General Internal Medicine, 34(8), 1631–1636. 10.1007/s11606-019-04953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiffen, J. , Corbridge, S. J. , & Slimmer, L. (2014). Enhancing clinical decision making: Development of a contiguous definition and conceptual framework. Journal of Professional Nursing, 30(5), 399–405. [DOI] [PubMed] [Google Scholar]
- Trowbridge, R. L. , Rencic, J. J. , & Durning, S. L. (2015). Teaching clinical reasoning. American College of Physicians. [Google Scholar]
- Victor‐Chmil, J. (2013). Critical thinking versus clinical reasoning versus clinical judgment. Nurse Educator, 38(1), 34–36. 10.1097/NNE.0b013e318276dfbe [DOI] [PubMed] [Google Scholar]
- Weber, M. T. , & Snow, D. (2006). An introductory clinical core course in psychiatric management: An innovative lifespan course blending all nurse practitioner majors. Perspectives in Psychiatric Care, 42(4), 245–251. [DOI] [PubMed] [Google Scholar]
- Wu, A. W. (2018). Reaching common ground: The role of shared mental models in patient safety. Journal of Patient Safety and Risk Management, 23(5), 183–184. 10.1177/2516043518805326 [DOI] [Google Scholar]
- Xu, H. , Benson, W. G. , Soh, J. Y. S. , & Ponnamperuma, G. G. (2021). Methods to improve diagnostic reasoning in undergraduate medical education in the clinical setting: A systematic review. General Internal Medicine, 36(9), 2745–2754. 10.1007/s11606-021-06916-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yudkowsky, R. , Otaki, J. , Lowenstein, T. , Riddle, J. , Nishigori, H. , & Bordage, G. (2009). A hypothesis‐driven physical examination learning and assessment procedure for medical students: Initial validity evidence. Medical Education, 43(8), 729–740. 10.1111/j.1365-2923.2009.03379.x [DOI] [PubMed] [Google Scholar]
- Zhang, J. (2002). Medical error: Is the solution medical or cognitive? Journal of the American Medical Informatics Association, 9(90061), 75S–77S. 10.1197/jamis [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Data Availability Statement
Data methods used in the analysis, coding and materials used to conduct the research will be made available to any researcher from the corresponding author, for purposes of reproducing the results or replicating the procedure.


