Abstract
Aims
Effective and safe decongestion remains a major goal for optimal management of patients with acute heart failure (AHF). The effects of the sodium–glucose cotransporter 2 inhibitor empagliflozin on decongestion-related endpoints in the EMPULSE trial (NCT0415775) were evaluated.
Methods and results
A total of 530 patients hospitalized for AHF were randomized 1:1 to either empagliflozin 10 mg once daily or placebo for 90 days. The outcomes investigated were: weight loss (WL), WL adjusted for mean daily loop diuretic dose (WL-adjusted), area under the curve of change from baseline in N-terminal pro-B-type natriuretic peptide levels, hemoconcentration, and clinical congestion score after 15, 30, and 90 days of treatment. Compared with placebo, patients treated with empagliflozin demonstrated significantly greater reductions in all studied markers of decongestion at all time-points, adjusted mean differences (95% confidence interval) at Days 15, 30, and 90 were: for WL −1.97 (−2.86, −1.08), −1.74 (−2.73, −0.74); −1.53 (−2.75, −0.31) kg; for WL-adjusted: −2.31 (−3.77, −0.85), −2.79 (−5.03, −0.54), −3.18 (−6.08, −0.28) kg/40 mg furosemide i.v. or equivalent; respectively (all P < 0.05). Greater WL at Day 15 (i.e. above the median WL in the entire population) was associated with significantly higher probability for clinical benefit at Day 90 (hierarchical composite of all-cause death, heart failure events, and a 5-point or greater difference in Kansas City Cardiomyopathy Questionnaire total symptom score change from baseline to 90 days) with the win ratio of 1.75 (95% confidence interval 1.37, 2.23; P < 0.0001).
Conclusion
Initiation of empagliflozin in patients hospitalized for AHF resulted in an early, effective and sustained decongestion which was associated with clinical benefit at Day 90.
Keywords: SGLT-2 inhibitor, Decongestion, Acute heart failure, Empagliflozin
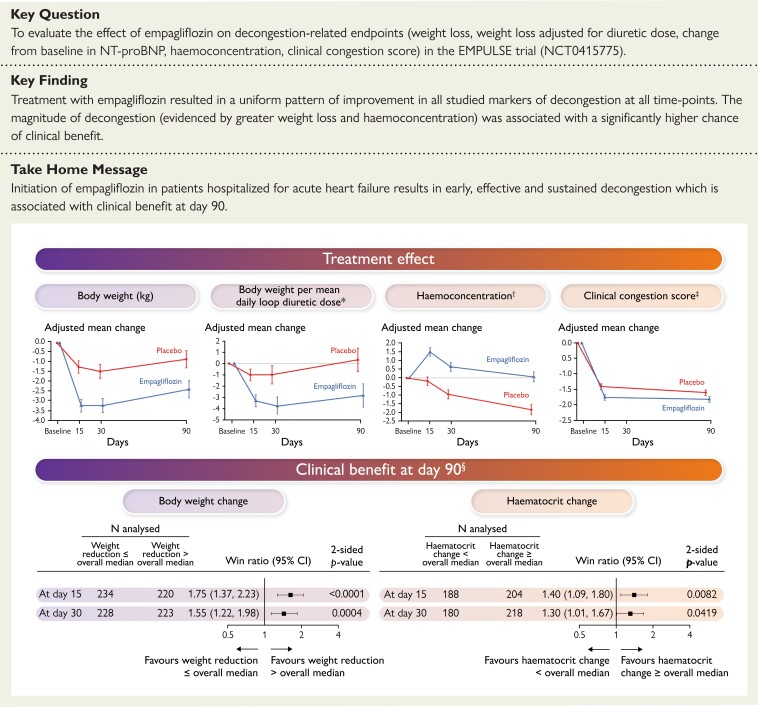
Structured Graphical Abstract
Structured Graphical Abstract.
Empagliflozin in acute heart failure: the EMPULSE Trial. CI, confidence interval. Data shown for the treatment effect graphs are adjusted mean change from baseline, with error bars representing standard error. *The units of weight changes per mean daily loop diuretic dose are presented in kg/40 mg of intravenous furosemide (or 80 mg of oral furosemide) or equivalent. The equivalent to 40 mg of furosemide was defined as 20 mg of torasemide or 1 mg of bumetanide. †Measured as changes in haematocrit (%). ‡Calculated as a sum of the points allocated for dyspnoea, orthopnoea and fatigue. For each variable, a 0- to 3-point scale has been used, where points were allocated for: absence (0 points), seldom (1 point), frequent (2 points), and continuous (3 points) based on the frequency of the clinical sign. §The hierarchy and the components of the primary outcome measured by the win ratio: 1. Time to all-cause death; 2. Number of heart failure (HF) events (including hospitalizations for HFs, urgent HF visits and unplanned outpatient visits); 3. Time to first HF event; 4. ≥5 point difference in change from baseline in KCCQ total symptom score (KCCQ-TSS) after 90 days of treatment.
See the editorial comment for this article ‘Assessing and treating congestion in acute decompensated heart failure: are we seeing the light at the end of the tunnel?’, by Alexandre Mebazaa et al., https://doi.org/10.1093/eurheartj/ehac680.
Introduction
Congestion is a leading pathophysiological and clinical feature of heart failure (HF) and a major cause of underlying HF hospitalizations.1–3 In patients with acute HF (AHF) residual congestion at discharge contributes to readmission and predicts a poor outcome,4 thus safe and effective decongestion remains the principal goal of AHF therapy.1–3 Diuretics are first-line therapy in patients with AHF, but a poor diuretic response, impaired kidney function or electrolyte abnormalities may hamper their use.5 Therefore, there is a clinical need for novel decongestive therapies.
Sodium–glucose cotransporter 2 (SGLT-2) inhibitors have unambiguously shown favourable, multidirectional impact on the natural course and prognosis in patients with chronic HF and have become a cornerstone of guideline-recommended pharmacological therapy.6,7 Although the mechanisms underlying such beneficial effects of SGLT-2 inhibitors still remain elusive, the diuretic/natriuretic effect with an ability to facilitate safely a response to ‘conventional’ diuretics, has been implied as at least partially responsible.8–10 Whether SGLT-2 inhibitors can exert the same decongestive efficacy in the settings of AHF has not yet been established.11,12 In the EMPULSE (EMPagliflozin in patients hospitalized with acUte heart faiLure who have been StabilizEd) trial, early initiation of SGLT-2 inhibitor empagliflozin in patients hospitalized for AHF after initial stabilization led to a statistically significant and clinically meaningful benefit within 90 days after randomization.13,14 Here, we aimed to analyse a spectrum of potential decongestive effects of empagliflozin compared with placebo in addition to standard medical treatment in the EMPULSE trial. Thus, we evaluated the effects of empagliflozin on pre-specified, decongestion-related endpoints of the study and explored whether decongestion itself translates into clinical benefit.
Methods
Study design
EMPULSE (ClinicalTrials.gov NCT0415775) was a multinational, multicentre, randomized, double-blind trial designed to evaluate the effects of oral empagliflozin compared with placebo on clinical benefit, safety, and tolerability in AHF. In the study, patients admitted to the hospital for AHF after initial stabilization were 1:1 randomized to receive either 10 mg empagliflozin (once daily) or placebo for 90 days. The detailed description of the study design as well as the results of the main study have been published elsewhere.13,14 In brief, to be eligible to enter the study, patients must have been admitted to the hospital with the primary diagnosis of AHF and treated with a minimum dose of 40 mg of intravenous furosemide (20 mg for Japanese patients) or equivalent. They also must have had dyspnoea (exertional or at rest) and at least two of the following four signs: (i) congestion on chest X-ray, (ii) rales on chest auscultation, (iii) clinically relevant oedema (e.g. ≥1+ on a 0 to 3+ scale), (iv) elevated jugular venous pressure. The key exclusion criteria were: AHF primarily triggered by pulmonary embolism, cerebrovascular accident or acute myocardial infarction; Type 1 diabetes mellitus; treatment with SGLT-1 or SGLT-2 inhibitors in the 90 days prior to randomization and estimated glomerular filtration rate (eGFR) <20 mL/min/1.73 m2 or dialysis requirement. During the hospitalization, the eligible patients were randomized (between 24 h and Day 5 from admission) into the study after an initial stabilization that was defined as: systolic blood pressure ≥100 mmHg with no symptoms of hypotension (in the preceding 6 h); no increase of intravenous diuretic dose (for 6 h prior to randomization); no intravenous vasodilators (6 h prior to randomization); and/or inotropic drugs (24 h prior to randomization).
The primary outcome was defined as clinical benefit measured by the stratified win ratio. The order and components of the primary outcome was: time to all-cause death, number of HF events (including hospitalizations for HF, urgent HF visits, and unplanned outpatient visits), time to first HF event, and a ≥5 point difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire total symptom score (KCCQ-TSS) after 90 days of treatment. An increase in the KCCQ score represents an improvement in patient-reported quality in life, while a decrease reflects worsening. The change from baseline in KCCQ-TSS score after 90 days of treatment was selected as a component of the primary endpoint in the EMPULSE trial, as it best quantifies symptom frequency and severity. Of note, we have recently demonstrated that, in the EMPULSE trial, empagliflozin significantly improved all key KCCQ domains, including not only TSS, but also clinical summary score, and overall summary score, which collectively encompass symptoms, physical function, quality of life, and social function.15
The study fulfilled the requirements stated in the Declaration of Helsinki and was independently approved by the ethics committees at each participating centre; written informed consent was obtained from each participant. Boehringer Ingelheim and Eli Lilly sponsored the trial.
Endpoints of the present analysis
The pre-specified, decongestion-related endpoints relevant for this analysis were: weight loss, weight loss adjusted per mean daily loop diuretic dose, the area under the curve (AUC) of change from baseline in log-transformed in N-terminal pro-B-type natriuretic peptide levels (over 30 days of treatment), hemoconcentration (measured as changes in haematocrit), and clinical congestion score. This score was calculated as a sum of the points allocated for the following signs and symptoms: dyspnoea, orthopnoea, and fatigue. For each variable a 0- to 3-point scale has been used, where points were allocated for: absence (0 points), seldom (1 point), frequent (2 points), and continuous (3 points) based on the frequency of the clinical sign. The units of weight changes per mean daily loop diuretic dose are presented in kg/40 mg of intravenous furosemide (or 80 mg of oral furosemide) or equivalent. The equivalent to 40 mg of furosemide was defined as 20 mg of torasemide or 1 mg of bumetanide. Of note, weight loss adjusted to diuretic dose is an acceptable metric of diuretic response.16,17 The units of loop diuretic doses are presented in mg of intravenous furosemide, or equivalent. To enable combined summaries of oral and intravenous loop diuretics, oral dose levels were halved (e.g. 80 mg of oral furosemide was considered equivalent to 40 mg of intravenous furosemide).16,17 The decongestion-related endpoints were evaluated at Days 15, 30, and 90 of treatment.
Statistical analyses
We analysed the differences between treatment groups in change from baseline value at Days 15, 30, and 90 separately, using mixed effects models for repeated measures adjusted for HF status and baseline value by visit interaction for the following endpoints: body weight, body weight per mean daily loop diuretic dose (kg/40 mg furosemide or equivalent), loop diuretic dose level, clinical congestion score, haematocrit, and KCCQ-TSS.
In the analyses of the weight change per mean daily loop diuretic dose at Days 15, 30, and 90, we excluded patients who missed more than 1 day of loop diuretic dosing during the relevant period. The same approach was used to analyse the mean daily loop diuretic doses.
The AUC of change from baseline in log-transformed NT-proBNP level over 15/30/90 days of treatment was analysed by analysis of covariance (ANCOVA). Based on literature reviews, NT-proBNP level is regarded as log-normally distributed, therefore, values were log-transformed prior to analysis. The linear trapezoidal rule was used to calculate the AUC after the log-transformation was applied to each value. The model included log(baseline NT-proBNP) as a linear covariate and HF status and treatment group as fixed effects.
ANCOVA was also used to analyse the mean daily dose of loop diuretics from the day after randomization until initial hospital discharge. The model included mean daily dose of loop diuretic until day before randomization as a linear covariate and the treatment group as a fixed effect.
In a post hoc analysis, patients were divided into two subgroups, based on weight loss at Day 15: (i) >overall median weight reduction, (ii) ≤overall median weight reduction. The same was done at Day 30. In addition, subgroups were formed within treatment groups at Days 15 and 30 (>treatment group median weight reduction, ≤treatment group median weight reduction).
To evaluate the effects on the primary hierarchical composite endpoint of clinical benefit across these subgroups, we conducted post hoc analyses comparing patients > overall median weight reduction with those ≤ overall median weight reduction, stratified by treatment group. The same procedure has been also replicated for median change in haematocrit (≥each treatment group median change vs. <each treatment group median change) at Days 15 and 30. Each comparison of two patients followed the hierarchy of comparing time to death, number of HF events, time to HF event, or a 5 point or greater difference in change from baseline in KCCQ-TSS at Day 90, until the conclusion of a win or loss or otherwise concluding by a tie, as previously described. We calculated the win ratio as the number of wins in the empagliflozin group divided by the number of losses within each treatment group stratum. A multiple imputation approach, according to whether patients were on-treatment or off-treatment, was used to impute missing data for the KCCQ-TSS, as previously described.16–19 The detailed explanation of methods used to analyse multiple endpoints and its assumptions is presented in the methodology section of the Supplementary material online.
All analyses were performed with SAS software, version 9.3 or higher (SAS Institute). P-values of 0.05 were considered statistically significant, and were not adjusted for multiple comparisons.
Results
Baseline characteristics
The study population consisted of 530 patients (265 in each treatment arm) with median (Q1–Q3): age 71 (61–78) years, ejection fraction 32 (23–45) %, and NT-proBNP 3242 (1725–6104) pg/mL at baseline. The treatment arms were balanced with regard to demographics, baseline clinical and laboratory profile (details are presented in Table 1). The median (interquartile range) time from hospital admission to initial stabilization and subsequent randomization was 3 (2–4) days. There was no difference in median time to randomization between empagliflozin: 3 (2–4) days and placebo group: 3 (2–4) days.
Table 1.
Characteristics of the patients at baseline
| Empagliflozin (n = 265) median (IQR) or n (%) |
Placebo (n = 265) median (IQR) or n (%) |
|
|---|---|---|
| Age (years) | 71 (62–78) | 70 (59–78) |
| Sex | ||
| Men | 179 (67.5) | 172 (64.9) |
| KCCQ-TSS | 37.5 (20.8–58.3) | 39.6 (22.4–58.3) |
| NT-proBNP (pg/mL) | 3299 (1843–6130) | 3106 (1588–6013) |
| Blood pressure (mmHg) | ||
| Systolic | 120 (109.0–135.0) | 122 (110.0–138.0) |
| Diastolic | 72.0 (64.0–82.0) | 74.0 (67.0–80.0) |
| Body weight (kg) | 82.0 (70.0–98.8) | 82.3 (70.3–100.0) |
| Body-mass index (kg/m2) | 28.3 (24.5–32.5) | 29.1 (24.7–33.6) |
| Clinical congestion score | 3.0 (1.0–4.0) | 2.0 (1.0–4.0) |
| Left ventricular ejection fraction (%) | 31.0 (23.0–45.0) | 32.0 (22.5–49.0) |
| ≤40% | 182 (68.7) | 172 (64.9) |
| >40% | 76 (28.7) | 93 (35.1) |
| Missing | 7 (2.6) | 0 |
| Estimated GFR (mL/min/1.73 m2) | 50.0 (36.0–65.0) | 54.0 (39.0–70.0) |
| <30 mL/min/1.73 m2 | 27 (10.2) | 24 (9.1) |
| Missing | 16 (6.0) | 14 (5.3) |
| Hemoglobin (g/dL) | 13.2 (11.8–14.8) | 13.4 (11.8–14.8) |
| Haematocrit (%) | 40.0 (36.0–45.0) | 41.0 (36.0–45.0) |
| Medical history | ||
| Diabetes | 124 (46.8) | 116 (43.8) |
| Hypertension | 205 (77.4) | 221 (83.4) |
| Myocardial infarction | 66 (24.9) | 62 (23.4) |
| Atrial fibrillation | 134 (50.6) | 128 (48.3) |
| CABG or PCI | 78 (29.4) | 78 (29.4) |
| Valvular heart diseasea | 173 (65.3) | 167 (63.0) |
| Heart failure status | ||
| Decompensated CHFb | 177 (66.8) | 178 (67.2) |
| Acute de novoc | 88 (33.2) | 87 (32.8) |
| Medication | ||
| ACE inhibitor and/or ARB and/or ARNi | 186 (70.2) | 185 (69.8) |
| ACE inhibitor | 88 (33.2) | 89 (33.6) |
| ARB | 64 (24.2) | 52 (19.6) |
| ARNi | 36 (13.6) | 45 (17.0) |
| Beta-blocker | 213 (80.4) | 208 (78.5) |
| MRA | 151 (57.0) | 125 (47.2) |
| Loop diuretic | 233 (87.9) | 204 (77.0) |
| Any diuretic (loop, thiazides, or other) | 248 (93.6) | 232 (87.5) |
| Thiazides | 31 (11.7) | 23 (8.7) |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; ARNi, angiotensin receptor neprilysin inhibitor; CABG, coronary artery bypass graft; CHF, chronic heart failure; GFR, glomerular filtration rate; MRA, mineralocorticoid receptor antagonist; NYHA, New York Heart Association; PCI, percutaneous coronary intervention.
Reported by treating physicians. Patients with hemodynamically significant (severe) uncorrected primary cardiac valvular disease planned for surgery or intervention during the course of the study were excluded from the study. Patients with secondary mitral regurgitation or tricuspid regurgitation due to dilated cardiomyopathy were not excluded unless planned for surgery or intervention during the course of the study.
Patients, who had already diagnosed chronic heart failure before admission to the hospital.
Patients with the first diagnosis of heart failure at admission to the hospital.
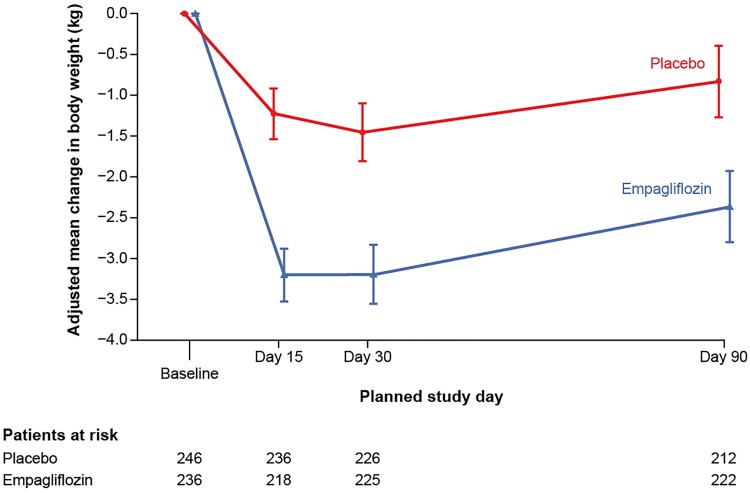
Impact of empagliflozin on weight loss
At baseline, body weight did not differ between groups: 86.7 (SD 26.1) for empagliflozin and 86.8 (SD 24.2) kg for placebo, respectively. At Day 15, patients treated with empagliflozin had significantly greater weight loss than those receiving placebo: adjusted mean difference (95% confidence interval, CI): −1.97 (−2.86, −1.08) kg, P < 0.0001. Analogously, there was a sustained, significantly greater weight loss among patients receiving empagliflozin vs. placebo at Days 30 and 90, adjusted mean differences (95% CI): −1.74 (−2.73, −0.74), P = 0.0007 and −1.53 (−2.75, −0.31) kg, P = 0.0137, respectively. The longitudinal changes in body weight in both treatment arms during the study are presented in Table 2 and in Figure 1.
Table 2.
Effect of Empagliflozin on weight change and weight change per mean daily loop diuretic dose
| Endpoint | Day | Adjusteda mean (SE) | Adjusteda mean difference (95% confidence interval), P-value | |
|---|---|---|---|---|
| Empagliflozin | Placebo | |||
| Body weight change from baseline (kg) | 15 | −3.20 (0.32) | −1.23 (0.32) | −1.97 (−2.86, −1.08), <0.0001 |
| 30 | −3.19 (0.36) | −1.45 (0.36) | −1.74 (−2.73, −0.74), 0.0007 | |
| 90 | −2.36 (0.44) | −0.83 (0.44) | −1.53 (−2.75, −0.31), 0.0137 | |
| Body weight change from baseline per mean daily loop diuretic dose (kg/40 mg furosemide or equivalent) | 15 | −3.33 (0.53) | −1.02 (0.52) | −2.31 (−3.77, −0.85), 0.0020 |
| 30 | −3.80 (0.81) | −1.01 (0.81) | −2.79 (−5.03, −0.54), 0.0152 | |
| 90 | −2.85 (1.04) | 0.33 (1.05) | −3.18 (−6.08, −0.28), 0.0319 | |
Adjusted for HF status and baseline value by visit interaction.
Figure 1.
The trajectories of adjusted mean changes in body weight during the study in empagliflozin and placebo arms.
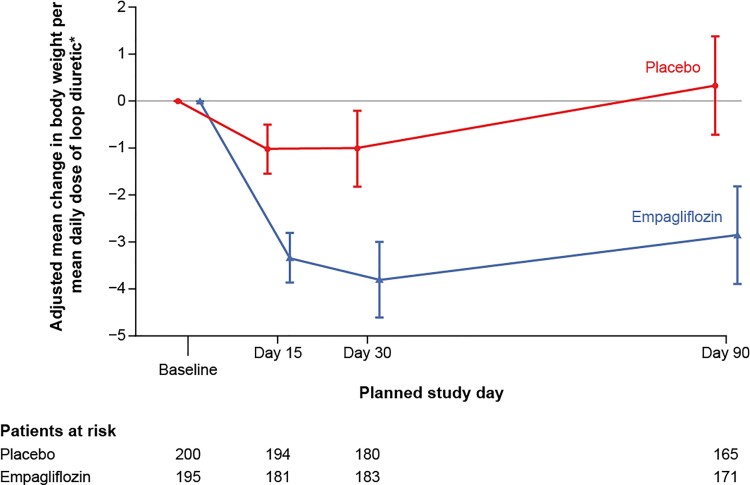
Impact of empagliflozin on weight loss adjusted per mean daily loop diuretic dose
At baseline, diuretics were used in 248 (93.6%) patients in the empagliflozin arm and in 232 (87.5%) in the placebo arm. The total dose of iv or oral diuretics was greater in those receiving empagliflozin vs. placebo during the initial hospital stay (see Supplementary material online, Table S1). However, the adjusted mean difference (95% CI) between treatment groups in the mean daily dose of iv or oral loop diuretics from the day after randomization until hospital discharge 6.98 (−8.59, 22.56) mg of iv furosemide (or equivalent) was not statistically significant (P = 0.38). Patients allocated to empagliflozin did not receive significantly greater doses of diuretics, when compared with placebo, adjusted mean difference (95% CI) at Day 15: 6.7 (−1.0, 14.4), P = 0.0862, at Day 30: 5.3 (−1.6, 12.3), P = 0.1295, and at Day 90: 3.1 (−3.4, 9.6) mg of iv furosemide (or equivalent), P = 0.3488.
Patients receiving empagliflozin had significantly greater weight loss adjusted per daily diuretic dose at all investigated time-points. The adjusted mean difference (95% CI) in weight change per mean daily loop diuretic dose between empagliflozin and placebo were: −2.31 (−3.77, −0.85) (kg/40 mg of furosemide), P = 0.002 (at Day 15), −2.79 (−5.03, −0.54), P = 0.0152 (at Day 30), and −3.18 (−6.08, −0.28), P = 0.0319 (at Day 90), respectively. The longitudinal changes of mean values of body weight per mean daily loop diuretic dose in both study arms during the study are presented in Table 2 and Figure 2.
Figure 2.
The trajectories of adjusted mean changes in body weight per mean daily dose of loop diuretics during the study in empagliflozin and placebo arms.
Changes in Nt-proBNP
There was a significant reduction in the AUC of NT-proBNP from baseline up to Days 15 and 30 in the empagliflozin arm when compared with placebo, adjusted geometric mean ratio (95% CI): 0.92 (0.86, 0.98) P = 0.010 and 0.90 (0.82, 0.98) P = 0.018, respectively. The difference did not maintain statistical significance when assessed at Day 90: 0.89 (0.79, 1.00) P = 0.056 (Table 3).
Table 3.
Effect of Empagliflozin on other markers of decongestion
| Endpoint | Day | Adjusteda mean (SE) | Adjusteda mean difference (95% confidence interval), P-value | |
|---|---|---|---|---|
| Empagliflozin | Placebo | |||
| Clinical congestion score change from baseline (points) | 15 | −1.78 (0.09) | −1.43 (0.09) | −0.34 (−0.60, −0.09), 0.0079 |
| 90 | −1.85 (0.09) | −1.63 (0.09) | −0.23 (−0.47, 0.02), 0.0668 | |
| Haematocrit change from baseline (%) | 15 | 1.53 (0.25) | −0.18 (0.25) | 1.71 (1.02, 2.40), <0.0001 |
| 30 | 0.65 (0.26) | −0.96 (0.26) | 1.62 (0.88, 2.35), <0.0001 | |
| 90 | 0.07 (0.29) | −1.87 (0.30) | 1.94 (1.11, 2.76), <0.0001 | |
| AUC of change from baseline in NT-proBNP (pg/mLadays) | 15 | 12.69b | 13.80b | 0.92c (0.86, 0.98), 0.0101 |
| 30 | 24.07b | 26.77b | 0.90c (0.82, 0.98), 0.0176 | |
| 90 | 63.50b | 71.30b | 0.89c (0.79, 1.00), 0.0562 | |
Clinical congestion score and haematocrit were adjusted for HF status and baseline value by visit interaction. NT-proBNP was adjusted for HF status and log-transformed baseline value.
Adjusted geometric mean.
Adjusted geometric mean ratio.
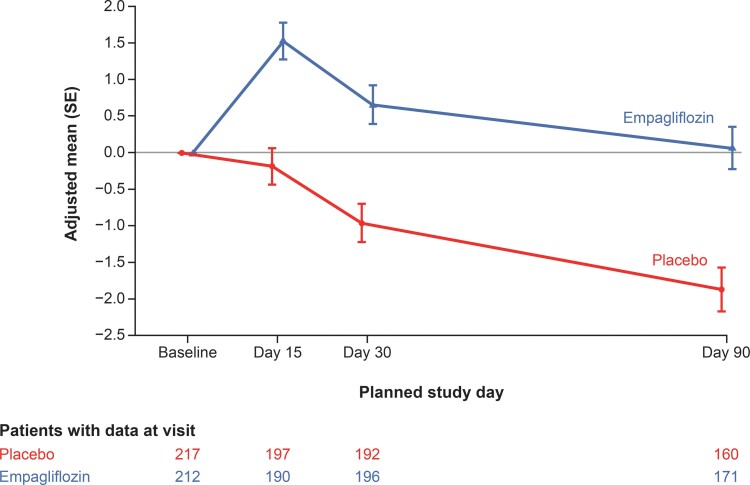
Hemoconcentration (changes in haematocrit)
There was no difference in the mean baseline haematocrit value between placebo and empagliflozin: 40.73 (SD 6.36) vs. 40.40 (SD 6.17) %, respectively. The haematocrit significantly rose in the empagliflozin group when compared with placebo at all time-points: adjusted mean differences (95% CI) were 1.71 (1.02, 2.4), 1.62 (0.88, 2.35), and 1.94 (1.11, 2.76), at Days 15, 30, and 90, respectively, all P < 0.0001 (Figure 3, Table 3).
Figure 3.
The trajectories of adjusted mean changes in haematocrit during the study in empagliflozin and placebo arms.
Change in clinical congestion score
At baseline, the mean clinical congestion score did not differ between study groups: placebo 2.77 (SD 2.14) vs. empagliflozin 2.92 (SD 2.12) points. Patients allocated to empagliflozin had a greater score reduction in comparison to placebo at Day 15; adjusted mean difference (95% CI): −0.34 (−0.60, −0.09) P < 0.01, which at Day 90 reduced to: −0.23 (−0.47, 0.02), P = 0.067 (Table 3).
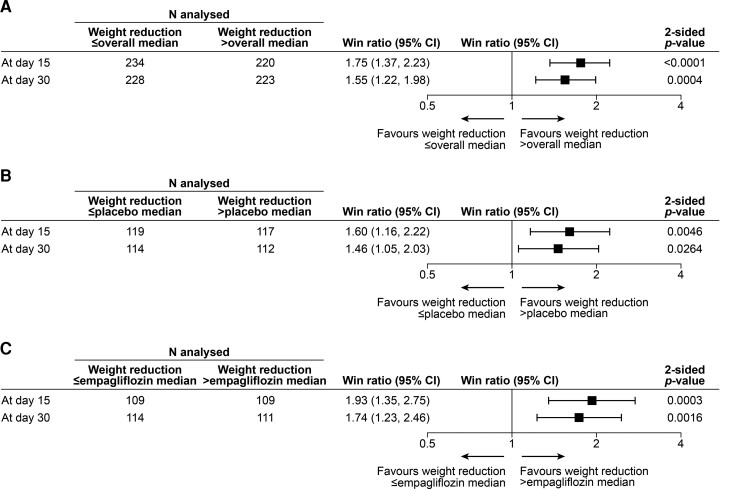
The effect of body weight loss and haematocrit change on clinical benefit at 90 days
Finally, we aimed to explore if the magnitude of decongestion itself (expressed by weight loss) was associated with clinical benefit at Day 90. In the overall population, the median weight change at Days 15 and 30 were −1.0 kg at both time-points. Patients with greater weight loss (i.e. above median weight reduction) at Days 15 and 30 were more likely to experience clinical benefit at Day 90, the win ratios (95% CI) were: 1.75 (1.37, 2.23) and 1.55 (1.22, 1.98), P < 0.0001 and P = 0.0004, respectively (Figure 4A).
Figure 4.
The win ratios for primary efficacy outcome* at Day 90 by median weight change at Days 15 and 30 in (A) the entire population (stratified by treatment group), (B) the placebo arm only (unstratified), and (C) the empagliflozin arm only (unstratified). *Hierarchical composite of death, number of heart failure events, time to first heart failure event and change from baseline in KCCQ-TSS after 90 days of treatment. The win ratio was calculated using a non-parametric generalized pairwise comparison procedure; data are presented as the point estimate and 95% CI with a two-sided P-value.
This analysis was also performed separately in each treatment arm (within each treatment arm clinical benefit at Day 90 was compared below vs. above median weight change at Days 15 and 30). The median (IQR) weight change at Days 15 and 30 in the placebo group were −0.7 (−2.90, 1.15) and −0.5 (−3.60, 1.5) kg, respectively; while the median weight change in the empagliflozin arm were: −1.6 (−6.00, 0.00) and −1.7 (−5.60, 0.60) kg, respectively. Patients with greater weight loss (above the median weight reduction) were more likely to experience clinical benefit within each treatment arm. In the placebo group the patients with a higher reduction of weight at Days 15 and 30 had a higher proportion of wins in the hierarchical clinical composite study outcome: win ratio (95% CI) 1.60 (1.16, 2.22) and 1.46 (1.05, 2.03), respectively, both P < 0.05. Analogously, patients in the empagliflozin arm with a greater weight reduction at Days 15 and 30 had a higher proportion of wins: win ratio (95% CI) 1.93 (1.35, 2.75) and 1.74 (1.23, 2.46), respectively, both P < 0.01 (Figure 4B and C).
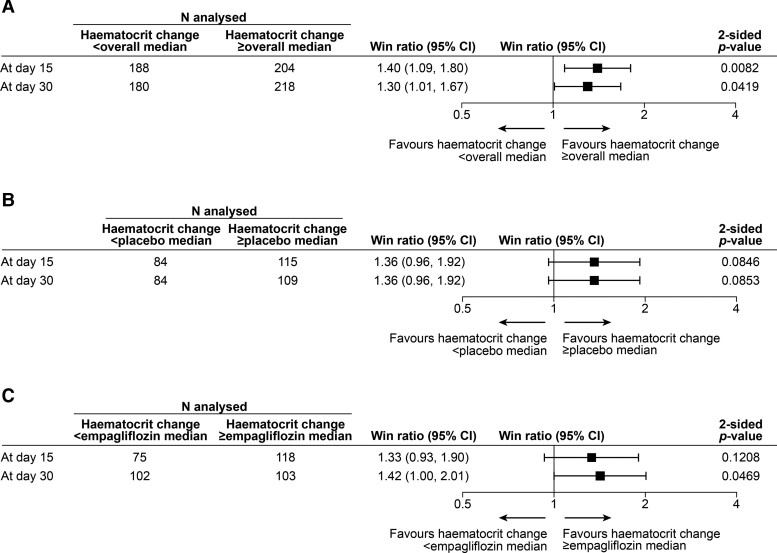
In the overall population, the median changes in haematocrit at Days 15 and 30 were: 1.0% and 0.0%, respectively. Patients with greater haematocrit increase (i.e. above median) at Days 15 and 30 were more likely to experience clinical benefit at Day 90, the win ratios (95% CI) were: 1.40 (1.09, 1.80) and 1.30 (1.01, 1.67), P = 0.0082 and P = 0.0419, respectively (Figure 5A).
Figure 5.
The win ratios for primary efficacy outcome* at Day 90 by median haematocrit change at Days 15 and 30 in (A) the entire population (stratified by treatment group), (B) the placebo arm only (unstratified), and (C) the empagliflozin arm only (unstratified). *Hierarchical composite of death, number of heart failure events, time to first heart failure event and change from baseline in KCCQ-TSS after 90 days of treatment. The win ratio was calculated using a non-parametric generalized pairwise comparison procedure; data are presented as the point estimate and 95% CI with a two-sided P-value.
This analysis was also performed separately in each treatment arm (within each treatment arm clinical benefit at Day 90 was compared below vs. above median change in haematocrit at Days 15 and 30). The median (IQR) changes in haematocrit at Days 15 and 30 in the placebo group were 0.0 (−2.0, 2.0) and −1.0 (−3.0, 1.0) %, respectively; while the median changes in haematocrit in the empagliflozin arm were: 1.0 (−1.0, 4.0) and 1.0 (−2.0,4.0) %, respectively. There was a strong trend toward more pronounced clinical benefit among patients with a greater increase in haematocrit (above the median) with the win ratios (95% CI) at Days 15 and 30 in the placebo group: 1.36 (0.96, 1.92) and 1.36 (0.96, 1.92), respectively, and in the empagliflozin group 1.33 (0.93, 1.90) and 1.42 (1.00, 2.01) (Figure 5B and C).
Discussion
There are several novels and clinically relevant findings of the present analyses. Initiation of empagliflozin in patients hospitalized for AHF resulted in an early (seen already at the first assessment at Day 15), clinically meaningful and sustainable (present until Day 90) decongestion. Of note, compared with placebo, treatment with empagliflozin resulted in an uniform pattern of significantly greater changes in all studied markers of decongestion at nearly all time-points. The magnitude of decongestion (as evidenced by greater weight loss) was associated with clinical benefit (Structured Graphical Abstract).
Congestion is a major reason leading to cardiac decompensation, thus indisputably considered as a key therapeutic target in AHF. Achieving complete decongestion at hospital discharge and its maintenance during the early, post-discharge period independently predicts better outcomes.20,21 During this period, which comprises the vulnerable first weeks after discharge, patients carry the highest risk of HF decompensation. Therefore, optimization of decongestive therapy is one of the fundamental goals to prevent future death and HF rehospitalization. In this context, SGLT-2 inhibitors, which tend to facilitate decongestion in patients with chronic HF9,10 may offer an incremental clinical benefit. However, the evidence on the decongestive effects of SGLT-2 inhibitors in the settings of AHF is still very limited. In the SOLOIST-WHF trial which recruited diabetic patients with AHF, sotagliflozin therapy initiated either before (in nearly half of the population) or shortly after hospital discharge, significantly reduced cardiovascular deaths and HF hospitalizations.22 However, there are no further reports available, primarily focusing on the analysis of decongestive effects of sotagliflozin from this trial. Another much smaller study, comprising 80 patients with AHF, reported that symptomatic improvement, reduction in NT-proBNP, and diuretic response were similar with empagliflozin and placebo.11 However, in this study patients (with and without diabetes mellitus) were randomized to therapy within the first 24 h of presentation to the hospital and all the endpoints were evaluated during 4 days after randomization.11 Of note, patients receiving empagliflozin had an increased cumulative urinary volume and a more negative fluid balance, and additional diuretic effect was linked to the presence of urinary glucose.11,12 It may suggest that the effect of empagliflozin in AHF is entirely different or at least complementary to loop diuretics and further suggests the potential incremental decongestive effect of empagliflozin in the settings of AHF.12 To the best of our knowledge, this is the first comprehensive longitudinal evidence of the decongestive effects of empagliflozin in patients hospitalized with a primary diagnosis of AHF (across the whole spectrum of baseline ejection fraction and history of HF preceding hospital admission) which may translate into clinical benefit.
An accurate estimation and classification of congestion in AHF still remains an unmet need and has been the subject of numerous studies.1,3 An application of clinical score based on physical examination has rather limited value, and often needs to be combined with additional biomarkers and imaging modalities. Thus, in this study we used several pre-defined measures allowing comprehensive, repeated assessment of congestion in a large cohort of patients discharged from the hospital. One of them was patient’ weight loss monitored at Days 15, 30, and 90. We are fully aware of the limitations of weight assessments as a surrogate of congestion status; however, it is still the most frequent and practical tool used in the everyday clinical practice, widely recommended by the guidelines.6 The weight loss may naturally be also a result of meaningful negative caloric balance (that may be facilitated by SGLT-2 inhibitors), but this mechanism usually needs more time to be achieved and detected.8 Thus, we believe that an early weight loss seen already at Day 15 (first assessment) and Day 30 (favouring by ∼2 kg patients receiving empagliflozin) reflects mainly facilitation of an excretion of fluid overload and confirms fast and effective decongestion, which is maintained until Day 90 (while the weight tended to return to baseline values in patients receiving placebo). Of importance, as the other indices of decongestion (namely: NT-proBNP and clinical congestion score, hemoconcentration) all followed the same pattern, we believe it further supports our assumption.
In this analysis, additionally to weight loss that proxies decongestion, we also used weight loss adjusted per total dose of diuretics used, which is a widely recognized marker of diuretic response/decongestive efficacy.16,23 Although, these two metrics are interrelated, they provide slightly different clinical information and in the previous studies weight loss indexed to total diuretic dose appeared to provide incremental and independent prognostic information.23 Our findings suggest that empagliflozin added to standard therapy improves diuretic efficacy, and this effect is becoming evident at Day 15 and sustained until Day 90. At hospital admission, patients allocated to the empagliflozin arm tended to be receiving more diuretics (despite randomization), which however did not impact the results (baseline-adjusted comparisons were performed and presented). Importantly, the difference in diuretic use was not statistically significant at subsequent study visits (Days 15, 30, and 90) adjusted for the baseline values. Importantly, adjustment for total diuretic use throughout the study confirmed statistically greater reduction in weight loss which suggests greater diuretic efficacy of active treatment.
Patients receiving empagliflozin demonstrated significantly higher values of haematocrit at all time-points vs. those receiving placebo but also tended to have an increase in haematocrit (vs. baseline values) at Days 15 and 30 (with a return to baseline values at Day 90), whereas there was a constant drop in haematocrit in the placebo group. It seems to support the view that treatment with empagliflozin results in haemoconcentration and can revert a gradual attenuation of intravascular decongestion (as evidenced by a gradual drop in haematocrit) seen in AHF patients receiving only standard diuretic therapy. Haemoconcentration (an increase in haematocrit) indicates an effective intravascular decongestion, when the rate of diuresis exceeds the plasma refill rate from the extravascular space. However, with time despite the maintenance of diuretic therapy (and often stable weight), there may be a recurrence of intravascular volume overload. As reported by Testani et al. in patients with AHF, an early haemoconcentration with subsequent haemodilution is not associated with clinical benefit in contrast to late and sustained increase in haematocrit/haemoconcentration.24 Our results can indicate a specific decongestive pattern associated with empagliflozin treatment in AHF, which can be characterized as an early and sustained intravascular decongestion paralleled with significant weight drop indicating also an effective fluid removal from the extravascular (interstitial) space. Recently Mullens et al. hypothesized that SGLT-2 inhibitors may act as a smart diuretic through incremental osmotic diuresis, should improve plasma refill rate and facilitate removal of the fluid overload from intra- and extravascular compartments.25 Our data indirectly support this view.
The initiation of empagliflozin after clinical stabilization led to a greater reduction in the NT-proBNP, which was evident already at Day 15 and sustained until Day 90. The beneficial effect of empagliflozin on NT-proBNP, which has been used in this analysis as an index of an effective decongestion, can be also interpreted in a broader context linking decongestion with attenuating neurohormonal activation and hemodynamic stress. Of importance, a decrease in the level of natriuretic peptides from admission to an early post-discharge phase is a strong predictor of reduced risk of HF worsening.26
Lastly, while exploratory, the magnitude of decongestion itself (defined as weight reduction exceeding the median reduction for each group) was associated with better outcome (in the entire cohort and in both study arms separately). As the study was not designed to answer the question of the mechanism of SGLT-2 inhibitor action, we may only speculate that effective decongestion is one of the mechanisms that translates into overall clinical success of the drug in AHF.
Limitations
The relatively modest number of patients enrolled to the study may be considered as a potential limitation and the use of inclusion and exclusion criteria which limit the generalizability of the presented data. We did not monitor patient weight during the entire hospital stay, thus would not be able to compare our data with other studies mainly focusing on the clinical implication of decongestion achieved during the in-hospital phase. Importantly though, we provided the analysis on an early post-discharge, the most vulnerable phase of the disease. The study was not designed to perform mechanistic insight into decongestion/diuretic response, so there are some data lacking, such as an analysis of urinary electrolytes, markers of tubular function/damage, which would add some pathophysiological background to reported results in our paper, that would be valuable. We believe that an impact of empagliflozin on the indices of decongestion reflects its true clinical effect irrespective of a difference in baseline diuretic distribution. Lastly, multicovariate adjustment of the win ratio is methodologically limited, as it can be stratified only by categorical variables. Thus, in the presented analysis the win ratio was stratified only by treatment group, which is an obvious limitation.
Conclusion
Initiation of empagliflozin in AHF patients after initial in-hospital stabilization resulted in an early, effective and sustained improvements in all decongestion indexes, which was associated with clinical benefit at Day 90.
Supplementary Material
Acknowledgements
The trial design was developed by the academic members of the Executive Committee in cooperation with representatives from Boehringer Ingelheim (BI), who were also represented in the Executive Committee of the trial. The Executive Committee provided oversight of the trial’s conduct together with the sponsor. Boehringer Ingelheim had the organizational oversight for the EMPULSE trial, which included trial conduct, supervision and monitoring of the enrolling study centres, data collection, storage, and analysis. The statistical analyses of the trial were performed by the sponsor with oversight by the Executive Committee. An independent data and safety monitoring committee reviewed the safety data. Figure support, was provided by Michael Trim at 7.4 Limited, Bollington, Cheshire, UK, and supported financially by BI. General administrative support in relation to development of the final submission package was supported financially by BI.
Contributor Information
Jan Biegus, Institute of Heart Diseases, Wroclaw Medical University, ul. Borowska 213, Wroclaw 50-556, Poland.
Adriaan A Voors, Department of Cardiology, University of Groningen, University Medical Center Groningen, Hanzeplein 1, P.O Box 30001, 9700 RB Groningen, HPC AB 31, The Netherlands.
Sean P Collins, Department of Emergency Medicine, Vanderbilt University Medical Center, Nashville, TN, USA; Geriatric Research and Education Clinical Care, Tennessee Valley Healthcare Facility VA Medical Center, Nashville, TN, USA.
Mikhail N Kosiborod, Saint Luke's Mid America Heart Institute, University of Missouri-Kansas City, Kansas City, MO, USA; The George Institute for Global Health and the University of New South Wales, Sydney, New South Wales, Australia.
John R Teerlink, Section of Cardiology, San Francisco Veterans Affairs Medical Center and School of Medicine, University of California San Francisco, 4150 Clement Street San Francisco, CA 94121, USA.
Christiane E Angermann, Comprehensive Heart Failure Center Würzburg, University and University Hospital Würzburg, and Department of Medicine 1, University Hospital Würzburg, Am Schwarzenberg 15, Haus A15 97078 Würzburg, Germany.
Jasper Tromp, Saw Swee Hock School of Public Health, National University of Singapore, the National University Health System, Singapore; 12 Science Drive 2, #10-01, Singapore 117549.
Joao Pedro Ferreira, Université de Lorraine, Inserm, Centre d'Investigations Cliniques Plurithématique 1433, and Inserm U1116, CHRU, F-CRIN INI-CRCT (Cardiovascular and Renal Clinical Trialists), Nancy, France; UnIC@RISE, Department of Surgery and Physiology, Cardiovascular Research and Development Center, University of Porto, Porto, Portugal.
Michael E Nassif, Saint Luke's Mid America Heart Institute and the University of Missouri, Kansas City, MO, USA.
Mitchell A Psotka, Inova Heart and Vascular Institute, Falls Church, VA, 3300 Gallows Road Falls Church, Virginia 22042, USA.
Martina Brueckmann, Boehringer Ingelheim International GmbH, Binger Straße 173, 55216 Ingelheim am Rhein, Germany; First Department of Medicine, Faculty of Medicine Mannheim, University of Heidelberg, Theodor-Kutzer-Ufer 1-3, 68167 Mannheim, Germany.
Afshin Salsali, Novo Nordisk pharmaceutical company, Vandtårnsvej 110, 2860 Søborg, Copenhagen, Denmark; Faculty of Medicine, Rutgers University, New Brunswick, NJ, 125 Paterson street, New Brunswick, NJ 08901, USA.
Jonathan P Blatchford, Elderbrook Solutions GmbH, Sky Tower, Borsigstr. 4, D-74321 Bietigheim-Bissingen, Germany.
Piotr Ponikowski, Institute of Heart Diseases, Wroclaw Medical University, ul. Borowska 213, Wroclaw 50-556, Poland.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
The trial was funded by the Boehringer Ingelheim and Eli Lilly and Company Diabetes Alliance.
Data availability
To ensure independent interpretation of clinical study results and enable authors to fulfill their role and obligations under the ICMJE criteria, Boehringer Ingelheim grants all external authors access to relevant clinical study data. In adherence with the Boehringer Ingelheim Policy on Transparency and Publication of Clinical Study Data, scientific and medical researchers can request access to clinical study data after publication of the primary manuscript in a peer-reviewed journal, regulatory activities are complete and other criteria are met. Researchers should use the https://vivli.org/ link to request access to study data and visit https://www.mystudywindow.com/msw/datasharing for further information.
References
- 1. Boorsma EM, ter Maaten JM, Damman K, Dinh W, Gustafsson F, Goldsmith S, et al. Congestion in heart failure: a contemporary look at physiology, diagnosis and treatment. Nat Rev Cardiol 2020;17:641–655. 10.1038/s41569-020-0379-7 [DOI] [PubMed] [Google Scholar]
- 2. Chioncel O, Mebazaa A, Harjola VPP, Coats AJ, Piepoli MF, Crespo-Leiro MG, et al. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC Heart Failure Long-Term Registry. Eur J Heart Fail 2017;19:1242–1254. 10.1002/ejhf.890 [DOI] [PubMed] [Google Scholar]
- 3. Gheorghiade M, Follath F, Ponikowski P, Barsuk JH, Blair JEA, Cleland JG, et al. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure. Committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail 2010;12:423–433. 10.1093/eurjhf/hfq045 [DOI] [PubMed] [Google Scholar]
- 4. Rubio-Gracia J, Demissei BG, ter Maaten JM, Cleland JG, O’Connor CM, Metra M, et al. Prevalence, predictors and clinical outcome of residual congestion in acute decompensated heart failure. Int J Cardiol 2018;258:185–191. 10.1016/j.ijcard.2018.01.067 [DOI] [PubMed] [Google Scholar]
- 5. Mullens W, Damman K, Harjola VPP, Mebazaa A, Brunner-La Rocca HPP, Martens P, et al. The use of diuretics in heart failure with congestion—a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2019;21:137–155. 10.1002/ejhf.1369 [DOI] [PubMed] [Google Scholar]
- 6. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–3726. 10.1093/eurheartj/ehab368 [DOI] [PubMed] [Google Scholar]
- 7. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022;145:e895–e1032. 10.1161/CIR.0000000000001063 [DOI] [PubMed] [Google Scholar]
- 8. Seferović PM, Fragasso G, Petrie M, Mullens W, Ferrari R, Thum T, et al. Sodium–glucose co-transporter 2 inhibitors in heart failure: beyond glycaemic control. A position paper of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2020;22:1495–1503. 10.1002/ejhf.1954 [DOI] [PubMed] [Google Scholar]
- 9. Griffin M, Rao VS, Ivey-Miranda J, Fleming J, Mahoney D, Maulion C, et al. Empagliflozin in heart failure: diuretic and cardiorenal effects. Circulation 2020;142:1028–1039. 10.1161/CIRCULATIONAHA.120.045691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mordi NA, Mordi IR, Singh JS, Mccrimmon RJ, Struthers AD, Lang CC. Renal and cardiovascular effects of SGLT2 inhibition in combination with loop diuretics in patients with type 2 diabetes and chronic heart failure: the RECEDE-CHF trial. Circulation 2020;142:1713–1724. 10.1161/CIRCULATIONAHA.120.048739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Damman K, Beusekamp JC, Boorsma EM, Swart HP, Smilde TDJ, Elvan A, et al. Randomized, double-blind, placebo-controlled, multicentre pilot study on the effects of empagliflozin on clinical outcomes in patients with acute decompensated heart failure (EMPA-RESPONSE-AHF). Eur J Heart Fail 2020;22:713–722. 10.1002/ejhf.1713 [DOI] [PubMed] [Google Scholar]
- 12. Boorsma EM, Beusekamp JC, ter Maaten JM, Figarska SM, Danser AHJ, van Veldhuisen DJ, et al. Effects of empagliflozin on renal sodium and glucose handling in patients with acute heart failure. Eur J Heart Fail 2020;23:68–78. 10.1002/ejhf.2066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tromp J, Ponikowski P, Salsali A, Angermann CE, Biegus J, Blatchford J, et al. Sodium–glucose co-transporter 2 inhibition in patients hospitalized for acute decompensated heart failure: rationale for and design of the EMPULSE trial. Eur J Heart Fail 2021;23:826–834. 10.1002/ejhf.2137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Voors AA, Angermann CE, Teerlink JR, Collins SP, Kosiborod M, Biegus J, et al. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: a multinational randomized trial. Nat Med 2022;28:568–574. 10.1038/s41591-021-01659-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kosiborod MN, Angermann CE, Collins SP, Teerlink JR, Ponikowski P, Biegus J, et al. Effects of empagliflozin on symptoms, physical limitations and quality of life in patients hospitalized for acute heart failure—results from the EMPULSE trial. Circulation 2022;146:279–288. 10.1161/CIRCULATIONAHA.122.059725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Valente MA, Voors AA, Damman K, Van Veldhuisen DJ, Massie BM, O’Connor CM, et al. Diuretic response in acute heart failure: clinical characteristics and prognostic significance. Eur Heart J 2014;35:1284–1293. 10.1093/eurheartj/ehu065 [DOI] [PubMed] [Google Scholar]
- 17. Dong G, Qiu J, Wang D, Vandemeulebroecke M. The stratified win ratio. J Biopharm Stat 2018;28:778–796. 10.1080/10543406.2017.1397007 [DOI] [PubMed] [Google Scholar]
- 18. Dong G, Li D, Ballerstedt S, Vandemeulebroecke M. A generalized analytic solution to the win ratio to analyze a composite endpoint considering the clinical importance order among components. Pharm Stat 2016;15:430–437. 10.1002/pst.1763 [DOI] [PubMed] [Google Scholar]
- 19. Pocock SJ, Ariti CA, Collier TJ, Wang D. The win ratio: a new approach to the analysis of composite endpoints in clinical trials based on clinical priorities. Eur Heart J 2012;33:176–182. 10.1093/eurheartj/ehr352 [DOI] [PubMed] [Google Scholar]
- 20. Bettencourt P, Azevedo A, Pimenta J, Friões F, Ferreira S, Ferreira A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation 2004;110:2168–2174. 10.1161/01.CIR.0000144310.04433.BE [DOI] [PubMed] [Google Scholar]
- 21. Kociol RD, McNulty SE, Hernandez AF, Lee KL, Redfield MM, Tracy RP, et al. Markers of decongestion, dyspnea relief, and clinical outcomes among patients hospitalized with acute heart failure. Circ Heart Fail 2013;6:240–245. 10.1161/CIRCHEARTFAILURE.112.969246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med 2021;384:117–128. 10.1056/NEJMoa2030183 [DOI] [PubMed] [Google Scholar]
- 23. Voors AA, Davison BA, Teerlink JR, Felker GM, Cotter G, Filippatos G, et al. Diuretic response in patients with acute decompensated heart failure: characteristics and clinical outcome—an analysis from RELAX-AHF. Eur J Heart Fail 2014;16:1230–1240. 10.1002/ejhf.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Testani JM, Brisco MA, Chen J, McCauley BD, Parikh CR, Tang WHW. Timing of hemoconcentration during treatment of acute decompensated heart failure and subsequent survival: importance of sustained decongestion. J Am Coll Cardiol 2013;62:516–524. 10.1016/j.jacc.2013.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mullens W, Martens P. Empagliflozin and renal sodium handling: an intriguing smart osmotic diuretic. Eur J Heart Fail 2021;23:79–82. 10.1002/ejhf.2086 [DOI] [PubMed] [Google Scholar]
- 26. Savarese G, Musella F, D’Amore C, Vassallo E, Losco T, Gambardella F, et al. Changes of natriuretic peptides predict hospital admissions in patients with chronic heart failure. A meta-analysis. JACC Heart Fail 2014;2:148–158. 10.1016/j.jchf.2013.11.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
To ensure independent interpretation of clinical study results and enable authors to fulfill their role and obligations under the ICMJE criteria, Boehringer Ingelheim grants all external authors access to relevant clinical study data. In adherence with the Boehringer Ingelheim Policy on Transparency and Publication of Clinical Study Data, scientific and medical researchers can request access to clinical study data after publication of the primary manuscript in a peer-reviewed journal, regulatory activities are complete and other criteria are met. Researchers should use the https://vivli.org/ link to request access to study data and visit https://www.mystudywindow.com/msw/datasharing for further information.