Abstract
We conducted a secondary analysis of discrete choice experiment (DCE) data from 395 couples enrolled in the Microbicide Trials Network (MTN)-045/CUPID study in Uganda and Zimbabwe to understand couple decision making around choice of multipurpose prevention technologies (MPTs) to prevent both HIV and pregnancy. Members of couples completed the same DCE, first separately then jointly, choosing between two hypothetical MPTs in a series of nine questions. Most couples either had similar preferences at the outset or had equal decision-making around MPTs (62%). Couples with male influence (17%) were more likely to use contraceptive pills with a male partner’s knowledge and couples with female influence (21%) were less likely to have shared decision making about family planning. Males influenced discussion around MPT duration, side effects, menstrual changes, and how the vagina feels during sex. Decision making was relatively shared, though decisions around certain attributes were more likely to be dominated by male partners.
Keywords: MPT, Couples, Decisions making, Discrete Choice Experiment
Introduction:
HIV and unintended pregnancy disproportionately affect women and adolescent girls in sub-Saharan Africa. Approximately 60% of new HIV infections in 2019 were in women in Eastern and Southern Africa, and 14 million unintended pregnancies occur in the region each year.(1,2) New Multipurpose prevention technologies (MPTs) are under development and designed for prevention of at least two sexual and reproductive health indications.(3) For example, products are currently being developed to simultaneously prevent both unintended pregnancy and HIV infection. However, past HIV prevention trials of oral pre-exposure prophylaxis (PrEP) and the dapivirine vaginal ring have shown that efficacy does not translate to effectiveness when products are not used as intended.(4–6) Therefore, it is critical for products to be designed to not only be efficacious, but to also consider the behaviors , preferences and needs of the product’s intended end-users.
Male partners’ attitudes and influence are a key determinant of female sexual and reproductive health outcomes including the use of HIV prevention strategies and contraceptive methods. Active involvement of male partners has been shown to increase women’s uptake of HIV testing (7) and oral PrEP,(8) use of the dapivirine vaginal ring, (9–12), uptake and adherence to antiretroviral treatment,(13,14) and women’s participation in microbicide studies as well as their product adherence.(9–12) Several studies have explored possible adverse effects of male involvement in women’s health and have identified potential drawbacks such as disruption of family relationships, conflict, intimate partner violence, and abandonment from partners and spouses.(15–18) Thus, balancing gender norms in which male partners assume a role in women’s reproductive decision-making alongside preservation of women’s autonomy is critical in couples-focused HIV prevention interventions.
By investigating the role that male partners can have in women’s preferences for MPTs, we sought to contribute to the knowledge base regarding how couples’ decision making can affect couple’s choices related to their sexual and reproductive health. We collected behavioral data during the Microbicide Trials Network (MTN)-045 study/CUPID, to evaluate couples’ preferences for various MPT attributes as well as how members within the couples influenced those preferences. In this paper, we assessed how choice of an MPT was influenced by members of a couple when asked to make choices together. More specifically, we sought to 1) to determine overall level of within-couple agreement and partner influence on one another; 2) characterize couples where the male or female partner had more influence over decision making; and 3) identify specific attributes where influence was wielded within the couple.
Materials and Methods:
Study Design and Population:
MTN 045 was designed to identify factors that may affect acceptability of and adherence to MPT product use by eliciting couples’ preferences about various drug delivery forms currently in the MPT product development pipeline. The focus on couples as end-users of future MPT products was intended to address gaps in understanding male partners’ interest in MPT products and their influences on women’s preferences for those products. The study enrolled 400 heterosexual couples in Uganda (N=200) and Zimbabwe (N=200) between November 2019 to December 2020. Eligible couples had been together for at least 3 months, were willing and able to provide consent, and expressed interest in contraception and/or HIV prevention. The female partner was required to be between the ages of 18 to 40 at enrollment and HIV negative by self-report. The male partner was required to be 18 years or older. Participants were excluded if they had a medical condition that could interfere with study participation including risk for intimate partner violence (IPV) as a result of study participation. Screening questions assessed perceived risk of IPV tied to study participation and the Investigator of Record had discretion to determine if participation was unsafe, based on these questions, and apply this as an exclusion criterion. Participants were recruited in Uganda and Zimbabwe through community meetings, stakeholder outreach, and community advisory board engagement activities. All participants provided written informed consent. The study was approved by the following Institutional Review Boards/Ethics Committees: Medical Research Council of Zimbabwe; Joint Research Ethics Committee for the University of Zimbabwe, Faculty of Medicine and Health Sciences and Parirenyatwa Group of Hospitals; Research Council of Zimbabwe; Chitungwiza City Health Department; Joint Clinical Research Centre Research Ethics Committee; Uganda National Council for Science and Technology; Johns Hopkins School of Medicine Institutional Review Board; Advarra Institutional Review Board.
This analysis includes data from 395 couples where both partners individually and couples jointly completed the same set of choices in a discrete choice experiment (5 couples did not complete the same set of questions). Additional details on the study are provided in another publication.(19)
Study Procedures:
All participants completed an individual questionnaire, an individual Discrete-Choice Experiment (DCE) and a joint DCE (completed by the couple together). Prior to completing the questionnaires, enrolled participants received an introduction to MPT products using standardized materials. Questionnaires were administered to each member of the couple separately and interviews were conducted in private rooms at the study clinics. Individual questionnaires included questions about behavioral and demographic information and an individual DCE to elicit preferences for MPT attributes. The DCE involved 9 choices between two hypothetical products (see Figure 1 for illustrative example). Attributes of the hypothetical products that were assessed included: 1) Product form (vaginal ring, oral tablets, vaginal insert or film); 2) Duration or frequency of use (before sex, daily, weekly, monthly); 3) Stomach cramps or nausea (rarely, frequently); 4) Menstrual changes (no changes, heavier bleeding, spotting or bleeding between menses); 5) Changes to how the vagina feels during sex (none, wetter, drier); and 6) Return to fertility (immediately, 3 months, 6 months). Following each choice question, participants were asked their preference between their chosen product and male condoms. The individual questionnaires were followed by a joint DCE that was completed by the couple together. The joint DCE included the same 9 choice set questions as the individual DCE. Participants completed interviews on a tablet computer, with assistance from a trained research interviewer. The DCE took approximately 20 (Inter Quartile Range (IQR) 13 – 26) minutes to complete, and participants were compensated for their time and effort, and/or reimbursed for travel to study visits and time away from work. Amounts were determined by each site and were $10 at the Zimbabwe site and $14 at the Uganda site.
Figure 1.
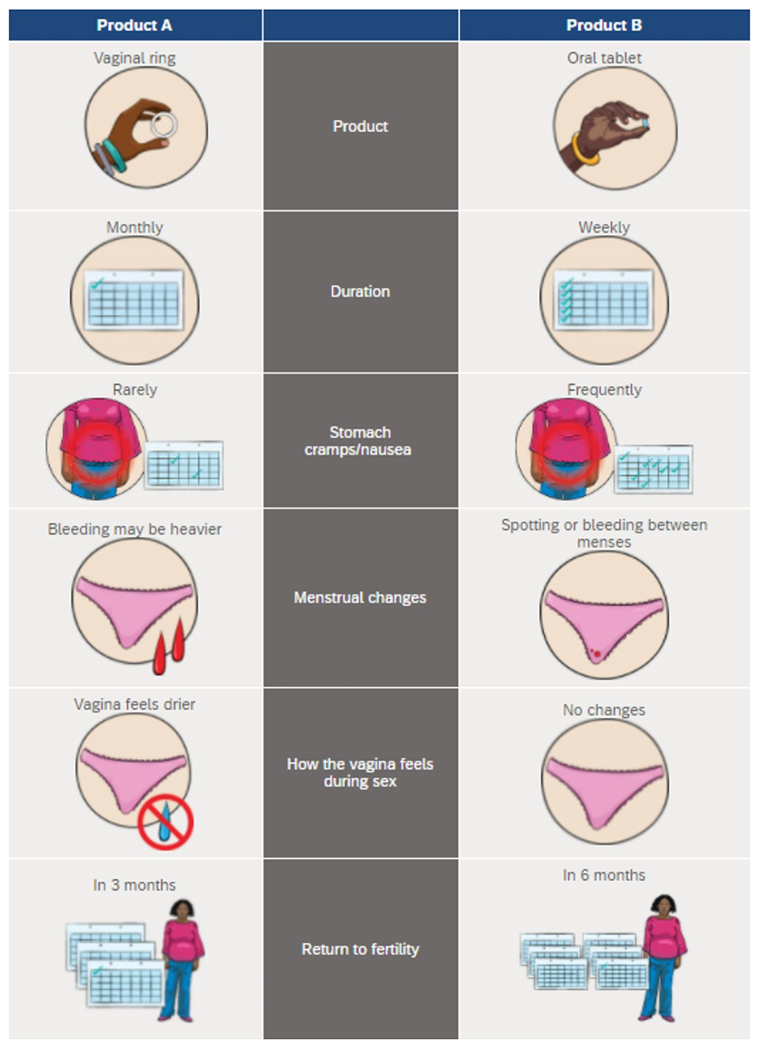
Example of a DCE choice set question. Participants were asked to select which MPT product they would want to use (females) or want their partner to use (males) for HIV and pregnancy prevention.
While completing the joint DCE, interviewers used a couple observation tool to capture couple dynamics. The tool draws on principles from psychology and couples counseling intervention research approaches to capture couple’s dynamics. (20,21) It included a checklist of attributes discussed and who dominated those discussions (male, female, both equally); and items adapted from two scales that assessed partner interaction: one focused on partner behaviors (cooperation, self-control and assertion subscale items) and the other on the emotional tone of partner interactions. (20,21) The scales were adapted by tailoring of the checklist items to align with the joint couple activity by assessing both individual attributes and overall decision making. Site teams were involved to ensure non-verbal cues assessed resonated culturally as indicating respect, connection, and intimacy. Interviewers underwent interactive training on use of the tool, including the role of self-awareness in observations. This was followed by a series of activities designed to establish interobserver reliability through review and discussion of each observation form category, practicing the tool based on videos of couples’ interactions, and review of results and discussion to gain consensus. Regular coaching in team meetings on use of the tool and shared information within and across sites on cases and rating decisions were conducted throughout the study. These were based on both individually and jointly observed sessions where two interviewers observed the same couple and compared and discussed areas of disagreement. Agreement on responses was also calculated within site with joint observations done on 107 couple interviews (23 couples in Uganda and 84 in Zimbabwe). Across sites, the average agreement was 92% (standard deviation (SD) 0.07). Agreement was, on average, 94% (SD 0.05) in Zimbabwe and 86% (SD 0.11) in Uganda.
Statistical analysis:
We used quantitative data from individual questionaries and DCEs conducted separately and jointly by the male and female partners within each couple. We also used quantitative data from the interviewer’s observation about who dominated the discussion during the joint DCE. First, we described characteristics of female and male partners within the overall study sample. We reported frequencies and percentages for categorical variables and medians with the interquartile range (IQR) for continuous variables. Measures were drawn from the Demographic and Health Survey (DHS), research conducted by our study teams previously, or from validated scales used in similar populations. Behavioral and demographic characteristics that were measured included age in years, duration of relationship (continuous years), parity (nulliparous vs. parous), education level, married or cohabitating with partner, individual or partner has other partners, perceived HIV risk, contraception method use, intimate partner violence (females only (22)), sexual relationship power score(23), fertility intentions, shared decision making and communication about family planning (DHS). Partner concurrency was defined as the participant or partner answering yes that they or their partner is married to or lives with someone else or has had other sexual partners in the last 3 months. Intimate partner violence was defined as any experience of emotional, physical, or sexual violence from partner in the last 12 months. Shared decision making was defined as both the male and female partner in the couple answering independently that family planning decisions are made together. Couple disagreement on fertility intentions were defined as one partner answering that is it “very/somewhat important” to avoid getting pregnant now while the other said it was “not at all important.” In addition, we described observational data about partner influences using the couple observation tool. Characteristics from the couple observation tool included whose opinion contributed more to the overall product choice (male, female, equal), who dominated the discussion overall and who dominated discussion on each potential attribute (product formulation, duration, side effects, menstrual changes, how the vagina feels during sex, and return to fertility).
Assessment of partner influence:
To determine overall level of agreement and influence of individual couple members on one another, we compared product choices during the individual DCE between individual members (male and female) and the overall couple choice. This was done to assess how male and female choices may have differed from the overall couple choice, potentially showing influence by one of the partners. We first determined the number of DCE selections where the female and male individual DCE choices matched one another out of a total of nine possible choices. This was done to assess the overall level of alignment between the couple. Then, among couples with low alignment (< 7 choices matching out of 9 which was around 75% of the population), we examined the number and proportion of DCE selections where the female and couple DCE choices matched one another and where the male and couple DCE matched one another. This was done to examine only those couples in which one partner could influence the other on decisions due to the underlying differences observed through the individual DCE choices. Among couples who were not aligned, we defined “male leaning” couples as couples who went with the male choice in ≥75% of choices and we defined “female leaning” couples as couples who went with the female choice in ≥75% of choices.
To characterize couples where the male or female partner had more influence over decision making, we used log-binomial models to estimate the prevalence ratio and corresponding 95% confidence intervals for the association between each predictor of interest and being “male leaning” or “female leaning.” Predictors of interest included demographic characteristics and sexual behaviors of the female partner, couple characteristics and characteristics from the couple observation tool regarding who dominated discussions. We focused on the female partner characteristics because we hypothesized that they may have the largest influence on product use by the female. To identify specific attributes where there was influence within the couple, we used a log-binomial model to estimate the prevalence ratio for associations between interviewer ratings from the couple observation tool about who dominated discussions on each attribute and being a male or female leaning couple. All models were adjusted for site (Uganda versus Zimbabwe).
Results:
We included 395 couples who participated in the MTN 045/CUPID study. The median age of the female partner was 26 years (interquartile range (IQR) 22-31) and was 31 for male partners (IQR 26-37) (Table 1). The median duration of relationships was 4 years (IQR 2-9) with most couples reporting that they made decisions about family planning jointly (75%, N=298). Most females were parous (77%, N=305), had a secondary school education (55%, N=219), and were married or cohabitating with a partner (86%, N=339). Most female partners had ever used contraception (84%, N=310), 15% without telling a partner (N=59), and the most common contraception method was oral contraception pills (33%, N=101). About half of women had ever experienced intimate partner violence (55%, N=219) and 37% in the past year (N=148). Females in a third of couples had low relationship power (34%, N=136).
Table 1:
Characteristics of 395 female and male partners from couples in Uganda and Zimbabwe
| Characteristics | Female Partner (N=395) | Male Partner (N=395) |
|---|---|---|
| N (%) | N (%) | |
| Age, median (IQR) | 26 (22,31) | 31 (26,37) |
| 18-24 | 235 (59,5) | 313 (79.2) |
| 25-40 | 160 (40.5) | 82 (20.8) |
| Relationship duration, median (IQR) | 4 (2,9) | 4 (2,9) |
| Married or cohabitating with partner | 339 (85.8) | 340 (86.7) |
| Parity median (IQR) | 2 (1,3) | 2 (1,3) |
| Nulliparous | 90 (22.8) | 88 (22.3) |
| Parous | 305 (77.2) | 307 (77.7) |
| Education level | ||
| Less than secondary school | 176 (44.6) | 122 (30.9) |
| Secondary school completed | 149 (37.7) | 152 (38.5) |
| At least some college/university | 70 (17.7) | 121 (30.6) |
| Perceived HIV risk score (range 0-7, female only), median (IQR) | 2 (1,4) | - |
| Ever used contraception without telling your partner (female only) | 59 (14.9) | - |
| Currently using contraception | 310 (83.8) | 289 (73.2) |
| Contraceptive method use, if using | ||
| Oral contraceptive pills | 101 (32.6) | 97 (33.6) |
| Injectable | 44 (14.2) | 52 (18.0) |
| Implant | 53 (17.1) | 42 (14.5) |
| Male condom | 40 (12.9) | 61 (21.1) |
| Vaginally inserted products (IUD, female condom) | 13 (4.2) | 9 (3.1) |
| Other (natural method, emergency contraception, sterilization) | 59 (19.0) | 28 (9.7) |
| Ever any violence: emotional, physical, or sexual violence (female only) | 219 (55.4) | |
| Past year any violence: emotional, physical, or sexual violence (female only) | 148 (37.5) | |
| Sexual relationship power score, median (IQR) | 2.6 (2.3, 2.9) | 2.8 (2.5, 3) |
| Low | 136 (34.4) | 69 (17.5) |
| Medium | 118 (29.9) | 164 (41.5) |
| High | 141 (35.7) | 162 (41.0) |
| Couple level derived measures | ||
| Either or both said uncomfortable talking about family planning with partner | 9 (2.3) | 9 (2.3) |
| Both said jointly making decisions about family planning | 298 (75.4) | 298 (75.4) |
| Couple disagrees on fertility intentions | 44 (11.1) | 44 (11.1) |
| Partnership concurrency - individual or partner has other partners | 83 (21.0) | 83 (21.0) |
Decision making regarding preferred MPT choices and preferred attributes was observed by interviewers to be relatively equal for most couples. According to the couple observation tool, 67% of couples had equal contribution to the conversation overall, and to most choices (62%; Table 2). When comparing individual DCE choices, 24% of couples (n=96) were well aligned in their personal choices (defined as >=7 out of 9 choices were the same), before doing the joint DCE exercise.
Table 2:
Couple’s observation data about which member of the couple dominated the conversation about the DCE overall and by attribute (N=395)
| Male dominated | Female dominated | Equal | Not discussed | |
|---|---|---|---|---|
| Who Dominated the Conversation Overall | 16% | 17% | 67% | NA |
| Whose Opinions Contributed Most to Choices | 13% | 26% | 62% | NA |
|
| ||||
| Specific Attribute | ||||
|
| ||||
| Form | 15% | 26% | 53% | 5% |
| Duration | 18% | 23% | 55% | 4% |
| Side effects | 18% | 32% | 48% | 2% |
| How vagina feels during sex | 35% | 13% | 47% | 5% |
| Effect on menses | 10% | 41% | 47% | 2% |
| Return to fertility | 23% | 20% | 54% | 4% |
There were 81 couples (21%) aligned with the female’s preferred product in ≥75% of choices where the members had disagreed in their personal selections; these couples were deemed female leaning. Sixty-nine couples (17%) were male leaning or selected the male’s preferred product in ≥75% of choice tasks where the members disagreed.
Male leaning couples were more likely to be using oral contraceptive pills versus other contraceptive methods (Prevalence Ratio (PR) 2.03; 95% Confidence interval (CI) 1.19, 3.48), and less likely to be using condoms for contraception compared to oral pills (PR 0.33; 95% CI 0.12, 0.94), and less likely to have a female partner ever use contraception without telling her partner (PR 0.29; 95% CI 0.09, 0.88), adjusting for site (Table 3). Male leaning couples were also more likely to have the male dominate the conversation overall (PR 1.88; 95% CI 1.23, 2.86), and less likely to have the female partner’s opinion contribute to the final product selection (PR 0.35, 95% CI 0.17, 0.75). They were also more likely to have shared decision making (PR 1.52; 95% CI 0.86, 2.67), although not statistically significant. Notably, ever experiencing violence (PR 1.04; 0.69, 1.59) and relationship power (Low power vs. high power PR 1.17; 95% CI 0.68, 1.99) were not associated with being in a male leaning couple.
Table 3:
Risk ratios and 95% confidence intervals for the association between female characteristics with male and female leaning choices
| Male Leaning (≥75% male choice) | Female Leaning (≥75% Female choice) | |
|---|---|---|
|
| ||
| Predictor | Adjusted Risk ratio (95% CI) | Adjusted Risk ratio (95% CI) |
| Age Female | ||
| 18-24 | 1.16 (0.77, 1.77) | 0.73 (0.49, 1.09) |
| 25-40 | 1 | 1 |
| Parity Female | ||
| Nulliparous | 1 | 1 |
| Parous | 1.49 (0.82, 2.71) | 1.06 (0.67, 1.66) |
| Relationship duration | 1.01 (0.97, 1.05) | 1.00 (0.97, 1.04) |
| Education level | ||
| Less than secondary school | 1 | 1 |
| Secondary school completed | 0.94 (0.57, 1.55) | 1.62 (1.00, 2.64) |
| At least some college/university | 0.80 (0.42, 1.53) | 1.52 (0.94, 2.48) |
| Individual or partner has other partners | 1.05 (0.63, 1.75) | 1.05 (0.67, 1.64) |
| Perceived HIV risk score | 0.98 (0.87, 1.11) | 1.00 (0.90, 1.11) |
| Married or cohabitating with boyfriend/girlfriend | 1.11 (0.57, 2.15) | 0.90 (0.54, 1.50) |
| Ever used contraception without telling your partner | 0.29 (0.09, 0.88) | 1.22 (0.75, 1.99) |
| Currently using contraception | 1.33 (0.71, 2.50) | 1.13 (0.73, 1.77) |
| Contraceptive method use, if using | ||
| Oral contraceptive pills | 1 | 1 |
| Injectable | 0.43 (0.17, 1.10) | 0.53 (0.21, 1.29) |
| Implant | 0.56 (0.29, 1.10) | 0.68 (0.34, 1.38) |
| Male condom | 0.33 (0.12, 0.94) | 0.60 (0.26, 1.39) |
| Vaginally inserted products (IUD, female condom) | 0.49 (0.13, 1.79) | 0.80 (0.28, 2.30) |
| Other (natural method, emergency contraception, sterilization) | 0.57 (0.25, 1.30) | 0.80 (0.38, 1.70) |
| Using Oral contraceptive pills versus other methods (yes/no) | 2.03 (1.19, 3.48) | 1.50 (0.84, 2.67) |
| Ever violence | 1.04 (0.69, 1.59) | 1.03 (0.71, 1.50) |
| Any violence in last 12 months | 0.72 (0.45, 1.15) | 0.96 (0.65, 1.42) |
| Sexual relationship power score | ||
| Low | 1.17 (0.68, 1.99) | 1.25 (0.80, 1.95) |
| Medium | 1.45 (0.88, 2.39) | 0.89 (0.54, 1.48) |
| High | 1 | 1 |
| Shared Decision-making for family planning- both partners | 1.52 (0.86, 2.67) | 0.67 (0.46, 0.99) |
| Which partner’s opinion contributed to the final product selections? | ||
| Male | 1.54 (0.97, 2.45) | 0.79 (0.38, 1.62) |
| Female | 0.35 (0.17, 0.75) | 1.65 (1.13, 2.42) |
| Equal | 1 | 1 |
| Who dominated the conversation overall? | ||
| Mostly Male | 1.88 (1.23,2.86) | 0.78 (0.44, 1.37) |
| Mostly Female | 0.47 (0.20, 1.11) | 1.22 (0.77, 1.94) |
| Equal | 1 | 1 |
Bold P<0.05
Female leaning couples were more likely to have a female partner who had completed secondary school compared to less than secondary school (PR 1.62; 95% CI 1.00, 2.64), were less likely to have shared decision making with a partner (PR 0.67; 95% CI 0.46, 0.99) and were more likely to have the female partner’s opinion contribute to the overall product choice (PR 1.65; 95% CI 1.13, 2.42).
Being in a male leaning couple was associated with having the male dominate conversations about duration (PR 1.84; 95% CI 1.17, 2.87), side effects (PR 1.62; 95% CI 1.00, 2.63) and menstrual changes (PR 1.71; 95% CI 1.00 2.93) (Table 4). Although not statistically significant, female leaning couples were more likely to have females dominate conversations about duration (PR 1.34; 95% CI 0.90, 2.00) and return to fertility (PR 1.30; 95% CI 0.84, 2.02). According to the couple observation tool (Table 4), in roughly 50% of couples, partners contributed equally to attribute discussions. When not equal, there were more couples where female partners dominated discussions about product form (26% female versus 15% male), duration (23% female versus 18% male), side effects (32% female versus 18% male), and effect on menses (41% female versus 10% male) whereas males were noted to dominate discussions about how the vagina feels during sex (35% male versus 13% female). Discussions about return to fertility were relatively equal (20% female, 23% male, 54% equal).
Table 4:
Prevalence ratios and corresponding 95% confidence intervals for the association between proportion of choices that were male and female leaning with observation of which partner dominated decision making related to each MPT attribute
| Male Leaning (≥75% male choice) | Female Leaning (≥75% female choice) | |
|---|---|---|
|
|
||
| Adjusted Prevalence ratio (95% CI) | Adjusted Prevalence ratio (95% CI) | |
| Product formulation | ||
| Male dominated | 1.22 (0.71, 2.10) | 0.77 (0.40, 1.45) |
| Female dominated | 0.78 (0.45, 1.35) | 1.16 (0.77, 1.75) |
| Equal | 1 | 1 |
| Not discussed | 1.31 (0.59, 2.91) | 0.82 (0.33, 2.02) |
| Duration | ||
| Male dominated | 1.84 (1.17, 2.87) | 0.60 (0.31, 1.15) |
| Female dominated | 0.78 (0.43, 1.42) | 1.34 (0.90, 2.00) |
| Equal | 1 | 1 |
| Not discussed | 0.92 (0.25, 3.37) | 0.91 (0.33, 2.49) |
| Side effects | ||
| Male dominated | 1.62 (1.00, 2.63) | 0.78 (0.44, 1.38) |
| Female dominated | 1.01 (0.61, 1.66) | 1.09 (0.72, 1.64) |
| Equal | 1 | 1 |
| Not discussed | - | 1.30 (0.42, 3.97) |
| Menstrual changes | ||
| Male dominated | 1.71 (1.00, 2.93) | 0.60 (0.26, 1.40) |
| Female dominated | 0.90 (0.56, 1.44) | 1.04 (0.71, 1.53) |
| Equal | 1 | 1 |
| Not discussed | 0.66 (0.10, 4.17) | 0.47 (0.07, 2.94) |
| How vagina feels during sex | ||
| Male dominated | 1.49 (0.96, 2.31) | 0.75 (0.48, 1.18) |
| Female dominated | 0.80 (0.36, 1.79) | 1.16 (0.68, 1.97) |
| Equal | 1 | 1 |
| Not discussed | 0.28 (0.04, 1.93) | 1.09 (0.54, 2.21) |
| Return to fertility | ||
| Male dominated | 1.43 (0.91, 2.26) | 1.00 (0.62, 1.62) |
| Female dominated | 0.65 (0.32, 1.32) | 1.30 (0.84, 2.02) |
| Equal | 1 | 1 |
| Not discussed | 2.06 (0.97, 4.37) | 0.62 (0.17, 2.26) |
Bold P<0.0
Discussion:
In this analysis of 395 couples who were asked to state their choices together about preferences for an MPT, decisions were mostly made jointly. Most couples either had similar preferences to begin with or shared in the decision-making. Only a fifth made choices leaning towards the female preferences and a fifth leaning towards the male partner’s preference. Couples with male influence were less likely to be using condoms and more likely to be using oral contraceptive pills with a partner’s knowledge of contraception use and to have the males dominate discussions overall. Couples with female influence were more likely to have a female partner with higher education and less likely to have shared decision-making about family planning. Areas where males influenced attribute preferences were duration, side effects, menstrual changes, and how the vagina feels during sex but not return to fertility or product form.
Within male dominated couples, women were less likely to report having used contraception in secret showing that they either already communicated with partners about family planning, perhaps because males in these relationships were more dominating about being included in decision making or females were unwilling to report secret use. These findings highlight the importance of tools, like decisions aids, that can facilitate conversations that may already be happening within couples to center women’s voices and opinions. On the other hand, female dominated couples were more likely to include a more educated female partner with less shared decision making. Women in these couples may have more autonomy to make product decisions on their own, not necessarily as a response to male opinion. Violence and power dynamics were not associated with male dominance in product selection, despite these being characteristics that have been typically associated with male domination and that were prevalent in this population. (15–18) The lack of association may be because the study enrolled couples with longer-term relationships who were willing to join a couple’s study together, or that these couples have preferences that are already aligned. The large percentage of couples with equal decision-making and the existing communication about product use within male dominated couples highlights the importance of engaging men in product choices.
Being in a male-leaning couple based on DCE choices was associated with the male partner dominating discussions about product duration, side effects, and menstrual changes. In the overall discussion, they were also observed by an interviewer to have an influence in discussions about how the vagina feels during sex. Females were observed to have more influence on discussions of product form and effects on menses when observed by the interviewer. Decision making tools could be tailored to focus on these topics where males and females have more discussion and disagreements in addition to product form. For male dominated couples, points of discussion could focus on duration, side effects, menstrual changes and how the vagina feels during sex, to ensure that the female partner perspective is heard on topics where the male partner may exert more influence. It should also be noted that both male-leaning and female-leaning were more likely to be using oral contraception pills after controlling for site – perhaps for different reasons. While we could not untangle the reasons in this analysis this finding highlights the diversity of users and reasons for choosing a product within a single product form (e.g. pills) and should be explored qualitatively in future research.
Our findings are from a non-random sample of participants with the expectation that couples enrolled together. The subset of couples that chose to participate in the study may therefore be different than the target population. However, characteristics of our sample on some indicators are similar to the most recent Demographic and Health Survey (DHS) data from Zimbabwe and Uganda. In the DHS surveys, 32.3% of women in Zimbabwe and 39.6% in Uganda had experienced sexual, physical, or emotional violence from a partner in the last 12 months,(24) compared to 37.5% in our study population. Roughly 76.2% of women in Zimbabwe and 62.0% of women from Uganda said that they make decisions jointly with their partner about using family planning in the DHS surveys, (24) compared to 75.4% of couples in our study who reported making decisions about family planning jointly. However, a higher percentage of women were using any method of contraception in our study (83.8%), compared to 67% of married women and 68% of sexually active unmarried women in the Zimbabwe DHS, and 39% of married women and 51% of sexually active unmarried women in the Uganda DHS .(24) The process of selecting a product together required couples to discuss and jointly make decisions which could have resulted in different choices than what would have been made by the same couple outside of the study. Additionally, behavioral and demographic characteristics including sexual behaviors (e.g., having other partners, contraception use without a partner’s knowledge) were self-reported and may be misreported due to social desirability bias.
Conclusions:
Among couples willing to enroll together in an HIV prevention study, decision making was relatively shared between members with some couples having one member dominate. However, what is true for the group is not necessarily true for the individual, which is also important to consider when counseling around choice/preferences in the real world. Women in male dominated couples were more likely to inform their partners about contraception use, suggesting that decision making tools may be especially helpful for facilitating discussions that are already occurring within these male dominated relationships. Decision making tools should be tailored to focus on topics where males and females have more disagreements and where males are likely to exert more influence including product duration, side effects, menstrual changes and how the vagina feels during sex. These findings highlight the importance of engaging men and ensuring that women’s preferences are still evident in couples’ choices.
Acknowledgements:
We would like to thank the study participants and study team.
Funding:
The MTN-045 study was designed and implemented by the Microbicide Trials Network (MTN). MTN was funded by the National Institute of Allergy and Infectious Diseases (UM1AI068633, UM1AI068615, UM1AI106707), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest or financial interests relevant to this article to disclose.
Ethics approvals: All study procedures were approved by the following ethics committees or institutional review boards: the Medical Research Council of Zimbabwe; the Joint Research Ethics Committee for the University of Zimbabwe, the Research Council of Zimbabwe Chitungwiza City Health Department; the Joint Clinical Research Centre Research Ethics Committee in Uganda; the Uganda National Council for Science and Technology; Johns Hopkins School of Medicine Institutional Review Board in the United States; and the Advarra Institutional Review Board in the United States.
Consent to participate: All participants provided written informed consent.
Consent for publication: N/A
Code availability: Code is available through the corresponding author
Availability of data and materials:
Study data are available upon request from the Microbicide Trials Network by submission of a Dataset Request Form available at http://www.mtnstopshiv.org/resources. The reason for the restriction on public data deposition is because of ethical and legal restrictions.
References:
- 1.Hubacher D, Mavranezouli I, McGinn E. Unintended pregnancy in sub-Saharan Africa: magnitude of the problem and potential role of contraceptive implants to alleviate it. Contraception [Internet]. 2008. Jul [cited 2021 May 18];78(1):73–8. Available from: https://pubmed.ncbi.nlm.nih.gov/18555821/ [DOI] [PubMed] [Google Scholar]
- 2.UNAIDS. UNAIDS data 2020 [Internet]. Geneva, Switzerland; 2020. [cited 2021 May 18]. Available from: https://www.unaids.org/sites/default/files/media_asset/2020_aids-data-book_en.pdf [Google Scholar]
- 3.Karim SA, Baxter C, Frohlich J, Karim QA. The need for multipurpose prevention technologies in sub-Saharan Africa [Internet]. Vol. 121, BJOG: An International Journal of Obstetrics and Gynaecology. Blackwell Publishing Ltd; 2014. [cited 2021 May 18]. p. 27–34. Available from: /pmc/articles/PMC4206830/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baeten JM, Haberer JE, Liu AY, Sista N. Preexposure prophylaxis for HIV prevention: Where have we been and where are we going? J Acquir Immune Defic Syndr [Internet]. 2013. Jul 1 [cited 2021 May 19];63(SUPPL. 2):S122. Available from: /pmc/articles/PMC3710117/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown ER, Hendrix CW, van der Straten A, Kiweewa FM, Mgodi NM, Palanee-Philips T, et al. Greater dapivirine release from the dapivirine vaginal ring is correlated with lower risk of HIV-1 acquisition: a secondary analysis from a randomized, placebo-controlled trial. J Int AIDS Soc [Internet]. 2020. Nov 1 [cited 2021 May 19];23(11). Available from: https://pubmed.ncbi.nlm.nih.gov/33206462/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Der Straten A, Van Damme L, Haberer JE, Bangsberg DR. Unraveling the divergent results of pre-exposure prophylaxis trials for HIV prevention. AIDS [Internet]. 2012. Apr 24 [cited 2021 May 19];26(7). Available from: https://pubmed.ncbi.nlm.nih.gov/22333749/ [DOI] [PubMed] [Google Scholar]
- 7.Sherr L. Fathers and HIV: Considerations for families [Internet]. Vol. 13, Journal of the International AIDS Society. Wiley-Blackwell; 2010. [cited 2021 May 19]. p. S4. Available from: /pmc/articles/PMC2890973/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr [Internet]. 2004. Dec 15 [cited 2021 May 19];37(5):1620–6. Available from: https://pubmed.ncbi.nlm.nih.gov/15577420/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roberts ST, Nair G, Baeten JM, Palanee-Philips T, Schwartz K, Reddy K, et al. Impact of Male Partner Involvement on Women’s Adherence to the Dapivirine Vaginal Ring During a Phase III HIV Prevention Trial. AIDS Behav. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montgomery CM, Lees S, Stadler J, Morar NS, Ssali A, Mwanza B, et al. The role of partnership dynamics in determining the acceptability of condoms and microbicides. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV [Internet]. 2008. Jul [cited 2021 May 19];20(6):733–40. Available from: https://pubmed.ncbi.nlm.nih.gov/18576176/ [DOI] [PubMed] [Google Scholar]
- 11.Montgomery ET, Van Der Straten A, Chidanyika A, Chipato T, Jaffar S, Padian N. The importance of male partner involvement for women’s acceptability and adherence to female-initiated HIV prevention methods in Zimbabwe. AIDS Behav [Internet]. 2011. Jul [cited 2021 May 19];15(5):959–69. Available from: https://pubmed.ncbi.nlm.nih.gov/20844946/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Montgomery ET, van der Straten A, Stadler J, Hartmann M, Magazi B, Mathebula F, et al. Male Partner Influence on Women’s HIV Prevention Trial Participation and Use of Pre-exposure Prophylaxis: the Importance of “Understanding.” AIDS Behav [Internet]. 2015. May 1 [cited 2021 May 19];19(5):784–93. Available from: /pmc/articles/PMC4416996/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nassali M, Nakanjako D, Kyabayinze D, Beyeza J, Okoth A, Mutyaba T. Access to HIV/AIDS care for mothers and children in sub-Saharan Africa: Adherence to the postnatal PMTCT program. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV [Internet]. 2009. Sep [cited 2021 May 19];21(9):1124–31. Available from: https://pubmed.ncbi.nlm.nih.gov/20024771/ [DOI] [PubMed] [Google Scholar]
- 14.Peltzer K, Sikwane E, Majaja M. Factors associated with short-course antiretroviral prophylaxis (dual therapy) adherence for PMTCT in Nkangala district, South Africa. Acta Paediatr Int J Paediatr [Internet]. 2011. Sep [cited 2021 May 19];100(9):1253–7. Available from: https://pubmed.ncbi.nlm.nih.gov/21366691/ [DOI] [PubMed] [Google Scholar]
- 15.Aarnio P, Olsson P, Chimbiri A, Kulmala T. Male involvement in antenatal HIV counseling and testing: Exploring men’s perceptions in rural Malawi. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV [Internet]. 2009. Dec [cited 2021 May 19];21(12):1537–46. Available from: https://pubmed.ncbi.nlm.nih.gov/20024733/ [DOI] [PubMed] [Google Scholar]
- 16.Betancourt TS, Abrams EJ, McBain R, Fawzi MCS. Family-centred approaches to the prevention of mother to child transmission of HIV [Internet]. Vol. 13, Journal of the International AIDS Society. Wiley-Blackwell; 2010. [cited 2021 May 19]. p. S2. Available from: /pmc/articles/PMC2890971/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiarie JN, Farquhar C, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Domestic violence and prevention of mother-to-child transmission of HIV-1. AIDS [Internet]. 2006. Aug [cited 2021 May 19];20(13):1763–9. Available from: /pmc/articles/PMC3384736/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Msuya SE, Mbizvo E, Uriyo J, Stray-Pedersen B, Sam NE, Hussain A. Predictors of failure to return for HIV test results among pregnant women in Moshi, Tanzania. J Acquir Immune Defic Syndr [Internet]. 2006. Sep [cited 2021 May 19];43(1):85–90. Available from: https://pubmed.ncbi.nlm.nih.gov/16878044/ [DOI] [PubMed] [Google Scholar]
- 19.Minnis A, Etima J, Quinn MS, Musara P, Kemigisha D, Browne E, et al. Heterosexual couples’ preferences for dual-purpose prevention products for HIV and pregnancy prevention: the CUPID Study (MTN-045) in Uganda and Zimbabwe. J Int AIDS Soc. 2021;24(S1):17–8. [Google Scholar]
- 20.Humbad MN, Donnellan MB, Klump KL, Burt SA. Development of the Brief Romantic Relationship Interaction Coding Scheme (BRRICS). J Fam Psychol [Internet]. 2011. Oct [cited 2021 Oct 25];25(5):759. Available from: /pmc/articles/PMC3339624/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anme T, Tokutake K, Tanaka E, Watanabe T, Tomisaki E, Mochizuki Y, et al. Short Version of the Interaction Rating Scale Advanced (IRSA-Brief) as a Practical Index of Social Competence Development. Int J Appl Psychol [Internet]. 2013. [cited 2021 Oct 25];3(6):169–73. Available from: http://article.sapub.org/10.5923.j.ijap.20130306.04.html [Google Scholar]
- 22.Garcia-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. WHO multi-country study on women’s health and domestic violence against women: summary report of initial results on prevalence, health outcomes and women’s responses [Internet]. Geneva: World Health Organization; 2015. Available from: http://www.who.int/reproductivehealth/publications/violence/24159358X/en/ [Google Scholar]
- 23.Pulerwitz J, Gortmaker SL, Dejong W. Measuring Sexual Relationship Power in HIV/STD Research. Sex Roles. 2000;42(7/8):637–60. [Google Scholar]
- 24.Demographic and Health Surveys. The DHS Program - Gender topic page [Internet]. 2021. [cited 2021 Sep 20]. Available from: https://dhsprogram.com/topics/gender/index.cfm [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Study data are available upon request from the Microbicide Trials Network by submission of a Dataset Request Form available at http://www.mtnstopshiv.org/resources. The reason for the restriction on public data deposition is because of ethical and legal restrictions.


