Abstract
Purpose
This study examined the prospective association between CGM-derived glycemic variability (GV) and glycemic control (GC) parameters in the first and second trimester, with subsequent diagnosis of GDM in the early third trimester.
Methods
In a longitudinal observational study, 60 study participants in the first trimester (9–13 weeks’ gestation), and 53 participants (18–23 weeks’ gestation) in the second trimester of pregnancy had CGM data extracted after a minimum of 8 days’ wear time (up to 14 days). At 24–31 weeks’ gestation, participants underwent a 75 g, 2-hour oral glucose-tolerance test as per IADPSG criteria to diagnose GDM. GV parameters examined in both first and second trimesters were mean amplitude of glycemic excursion (MAGE), standard deviation (SD), mean glucose, and coefficient of variation (CV). GC parameters measured were J-Index and percentage of time spent in glucose target ranges.
Results
The first trimester SD and MAGE were significantly higher in participants subsequently diagnosed with GDM (SD adjusted median 1.31 [interquartile range 1.2–1.3] mmol/L; MAGE 3.26 [3.2–3.3] mmol/L) than those who were not (SD 1.01 [0.9–1.0] mmol/L, MAGE 2.59 [2.4–2.6] mmol/L; p<0.05). Similarly, second trimester SD and MAGE were also significantly higher in participants subsequently diagnosed with GDM (SD 1.35 [1.3–1.4] mmol/L; MAGE 3.32 (3.31–3.41) mmol/L) than those who were not (SD 0.99 [0.98–1.01] mmol/L, MAGE 2.42 [2.42–2.55] mmol/L; p<0.05). Associations between SD and MAGE with GDM outcomes were adjusted for prepregnancy BMI and ethnicity. There were nonsignificant trends of higher J-Index scores in the first and second trimester, higher CV in the first trimester only, and higher mean in the second trimester only in participants diagnosed with GDM. Other study parameters measured were not significantly different between groups (p>0.003).
Conclusion
Our study suggests the potential value of CGM-derived SD and MAGE in early pregnancy as potential predictors of subsequent GDM diagnosis.
Keywords: continuous glucose monitoring, glycemic parameters, glycemic control, diabetes in pregnancy
Introduction
Gestational diabetes mellitus (GDM) is an abnormal glucose metabolism where blood glucose does not reach the level of overt DM with onset or first recognition during pregnancy.1 The Growing Up in Singapore Towards Healthy Outcomes (GUSTO) birth cohort study found that risk factors alone did not sufficiently predict GDM risk and failed to detect half the GDM cases in Asian women. Therefore, pregnant women in Singapore are now universally screened for GDM to avoid underdiagnosis to ensure optimal maternal and fetal outcomes.2 However, large-scale randomized controlled trials have shown that although screening and treatment for GDM are associated with improved short-term maternal and neonatal outcomes,3 they still fail to reduce rates of long-term outcomes, such as childhood obesity.4
GDM is typically diagnosed using an oral glucose-tolerance test (OGTT) between 24 and 28 weeks of gestation. However, prospective studies have observed higher fetal adiposity5 and growth velocity6 as early as 20 weeks of gestational age, preceding the clinical diagnosis of GDM at 24–28 weeks of gestation.5,6 This was corroborated by Graca et al,7 who reported increased amniotic fluid glucose concentrations representing maternal plasma glucose (PG) transported across the placenta as early as the second trimester in women later diagnosed with GDM. In a retrospective cohort study, “early GDM” diagnosis (at an average of 17 weeks’ gestation) in pregnant women had better composite neonatal outcomes than their later-diagnosed peers (>24 weeks), despite arguably representing a higher-risk cohort.8 These findings indicate that the effects of hyperglycemia of GDM mothers on the offspring are apparent at earlier time points (early second trimester), pointing to the potential advantages of an earlier diagnosis over current recommended guidelines.
Glycemic variability (GV) is defined as the degree to which blood glucose level fluctuates between high and low levels, and is emerging as an important metric used to characterize and detect subtle abnormalities in glucose metabolism under usual ambulatory conditions.9 With the advent of continuous glucose monitoring (CGM), it is is feasible to analyze changes in GV indicators and to assess glycemic control (GC) throughout the day.10 Furthermore, the clinical utility of CGM to analyze GV and GC has been well demonstrated in DM patients (type 1 and type 2) by predicting risks of DM complications.11,12 In GDM patients, GV parameters have been reported to be significantly higher in patients with GDM than those who did not develop GDM.13–17 Contrary to those studies, there have been reports of no significant differences18 or only borderline differences19 in GV parameters between patients with GDM and those without. However, all existing publications were either case–control13,14,19 or cross-sectional association studies15–18 that examined CGM-derived parameters only after GDM diagnosis. To the best of our knowledge, there have been no published studies that have assessed GV and GC parameters in early pregnancy as possible predictors of subsequent GDM diagnosis. Furthermore, available studies were primarily conducted in Western populations13,15,17–19 and were not aligned with the standardized core CGM metrics for clinical practice, which include a CGM wear time for a recommended 14 days to determine long-term GC20 and analysis of percentage time spent in glucose target ranges.11
To fill this gap in the literature, we aimed to study the prospective association between CGM-derived GV parameters and “time in ranges” in the first and second trimesters of pregnancy with subsequent diagnosis of GDM in the early third trimester using data from participants in the Integrating the Use of Calibration-Free Continuous Monitoring for Pregnancy Glucose Profiling (I-PROFILE) study. We chose to include a range of GV and GC parameters that are clinically relevant9 and suitable for GDM pregnant women,2 which include mean amplitude of glycemic excursion (MAGE), standard deviation (SD), mean glucose, and percentage coefficient of variation (%CV), used commonly in available studies as measures of GV.12 The J-Index and percentage of time spent in range (%TIR), time above target range (%TAR), and time below target range (%TBR), measured as GC parameters.11,21 The J-Index is a parameter of glucose control,22 while MAGE quantifies major swings in glycemia and excludes minor ones, and are considered the gold standard for assessing intraday GV.23 During pregnancy in women with type 1 or 2 DM and GDM, the overall goal is to increase %TIR while reducing %TAR, %TBR and GV.11 In this study, we hypothesized that there would be higher mean glucose, SD, %CV, %TAR, %TBR, and MAGE and lower J-Index and %TIR in the first and second trimesters of pregnancy in participants who were subsequently diagnosed with GDM than those who were not.
Methods
Participants
We used data from the I-PROFILE study, which recruited 216 pregnant Singapore citizens or permanent residents in their first trimester of pregnancy between December 2018 and January 2022. This prospective observational study was conducted at KK Women’s and Children’s Hospital (KKH), which is a major public hospital in Singapore. Inclusion criteria were women of Chinese, Malay, or Indian descent, aged ≥21 years, and with singleton pregnancies. Those with serious skin conditions (eg, eczema) that might interfere with or those with preexisting chronic diseases (eg, kidney disease, type 1 or type 2 DM) were excluded from participation. As KKH is part of a group of health-care institutions in Singapore called SingHealth, it is under the SingHealth Centralised Institutional Review Board (CIRB) purview. Therefore, this study received its ethics approval from the SingHealth CIRB (2018/2128). All participants gave written informed consent in accordance with the Declaration of Helsinki. The clinical trial identification number is NCT05123248.
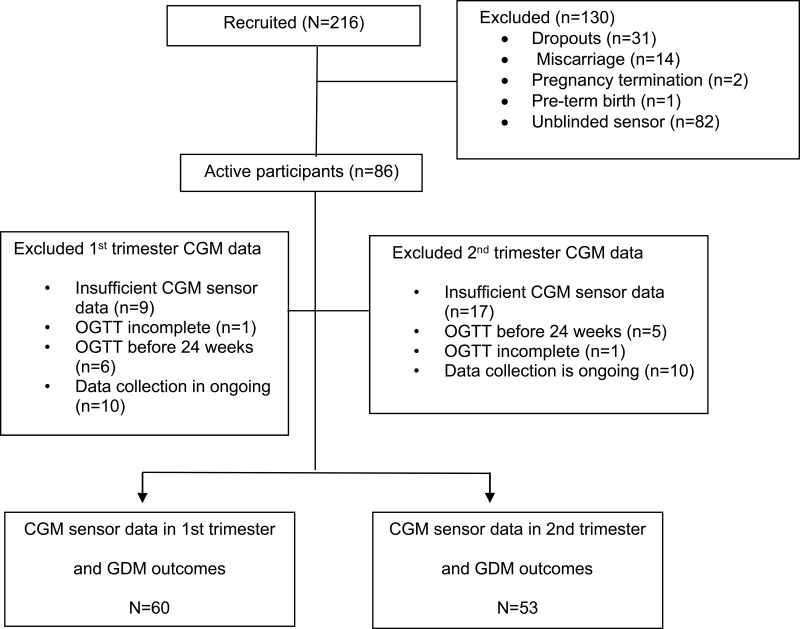
In the first trimester (9–13 weeks’ gestation) and second trimester (18–23 weeks’ gestation), there were 60 and 53 pregnant women, respectively, with complete CGM data and GDM outcomes (Figure 1). A subset of 49 participants with complete datasets at both these time points in the first and second trimesters were used for sensitivity analyses. Finally, a subset of 39 participants with complete datasets at three time points (9–13 weeks’ gestation, 18–23 weeks’ gestation, and 24–31 weeks’ gestation) were used to examine overall trends in these parameters across the three trimesters of pregnancy.
Figure 1.
Flow chart of study participants.
Continuous Glucose Monitoring in the First and Second Trimesters
At the recruitment visit in the first trimester of pregnancy, participants had a CGM sensor (FreeStyle Libre Pro, Abbott Diabetes Care, Alameda, CA) inserted on the back of either the right or left upper arm (day 0), which was worn for 14 days, when glucose levels were recorded from interstitial fluid every 15 minutes. Participants wore the sensor without a reader. Neither the participant nor the study team members had access to the data recorded by the CGM sensor at this point in time. After the 14 days, participants were required to scan the sensor using the blinded reader or with the assistance of a clinical research coordinator at their scheduled clinic visit, and the data from the reader were downloaded to a research computer. Participants had a new CGM sensor inserted in the second trimester, third trimester, and at the postnatal visit (only if they had developed GDM) according to the scheduled iPROFILE clinic visits (Supplementary Figure 1). Data from the sensor were extracted for use with a minimum wear time of 8 of 14 days (60% of data captured) if it had fallen off or been removed before the completion of the 14 days. Variables calculated from CGM readings for each participant were MAGE, SD, mean glucose, %CV, %TIR, and J-Index. %TIR was defined as %TIR 3.5–7.8 mmol/L, %TAR >7.8 mmol/L, and %TBR <3.5 mmol/L.11 Extracted CGM data were used to calculate mean glucose, SD, MAGE, %CV, and J-Index with EasyGV 9.0.R2.
Ascertainment of Gestational Diabetes Mellitus in the Early Third Trimester
Participants underwent a 75 g OGTT at 24–31 weeks’ gestation. Fasting (FG), 1-h PG (1hPG) and 2hPG concentrations were obtained using an automated biochemical analyzer (Abbott Alinity). PG concentrations were used to classify GDM according to the International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria: if any one of the PG values was at or above the thresholds of 5.1 mmol/L for FPG, 10.0 mmol/L 1hPG, and 8.5 mmol/L for 2hPG.
Data Collection
Participants had data collected in the first trimester of pregnancy at 9–13 weeks and at 18–23 weeks’ gestation in the second trimester of pregnancy. Questionnaires were administered to collect information on demographics, socioeconomic status, lifestyle, and obstetric and medical history. Prepregnancy weight was self-reported, while height at early pregnancy was measured at the prenatal care clinic at KKH using an Avamech B1000-M. Prepregnancy body-mass index (BMI; kg/m2) was calculated .
Statistical Analysis
Univariate analyses were conducted to compare demographic factors, anthropometric measurements, medical history, OGTT readings, and GV and GC parameters between participants with GDM and participants without GDM. Group differences were evaluated using Student’s t-test or the Wilcoxon rank-sum test for continuous variables, and x2 and Fisher’s exact tests were used for categorical variables. Descriptive statistics for numerical variables are presented as means ± SD or medians (interquartile range) and n (%) for categorical variables. Statistical significance was determined at p<0.05 for demographic data. Statistical significance used to examine the association between CGM-derived GV and GC parameters was identified by two-sided p<0.003, determined by applying Bonferroni corrections accounting for the maximum 16 exposure variables examined in this study, and to minimize type I errors due to multiple comparisons, while values of p<0.05 were reported as trends. Adjusted mean or adjusted mean and median values of the GV and GC parameters were presented by accounting for prepregnancy BMI and ethnicity when examining associations between GV and GC parameters with GDM outcomes. Statistical analyses were performed using Stata software version 13.1 (StataCorp LP, College Station, TX, USA).
Results
Baseline Characteristics of Study Participants
Sixty participants were assessed for GDM diagnosis (n=10) at a mean gestational age of 26.4±1.7 weeks. The group diagnosed with GDM also had higher prepregnancy BMI (28.1±7.4 vs 23.9±5.4 kg/m2, p=0.04) and higher 1-hour OGTT values (11.2±3.6 vs 7.21±1.2 mmol/L, p=0.006) than those who did not develop GDM (n=50) (Table 1). The characteristics of the participants who were included (n=60) and excluded (n=156) in the analyses were not significantly different (p>0.05), except that the group of patients excluded from the analysis had a history of GDM (9.68%) while the group included in the analysis did not (0, p=0.012 Supplementary Table S1).
Table 1.
Baseline Characteristics of the 60 Pregnant Study Participants with GDM and Without GDM Outcomes
| Maternal Characteristics (n=60)* | GDM (n=10) | Non-GDM (n=50) | p |
|---|---|---|---|
| Ethnicity, n (%) | 0.62 | ||
| Chinese | 7 (70.0) | 30 (60.0) | |
| Malay | 2 (20.0) | 17 (34.0) | |
| Indian | 0 (0) | 1 (2.0) | |
| Others | 1 (10.0) | 2 (4.0) | |
| Education, n (%) | 0.91 | ||
| Secondary and below | 1 (10) | 5 (11.1) | |
| College and above | 9 (90) | 40 (88.9) | |
| Family history of diabetes, n (%) | 6 (60.0) | 21 (42.0) | 0.33 |
| History of Gestational diabetes mellitus, n (%) | 0 (0.00) | 0 (0.00) | 1.00 |
| Parity, n (%) | 4 (40.0) | 31 (62.0) | 0.22 |
| Age (years), mean ± SD | 30.6±4.4 | 30.6±3.9 | 0.96 |
| %Pre-pregnancy BMI (kg/m2), mean ± SD | 28.1±7.4 | 23.9±5.4 | 0.04 |
| Mean gestational age of GDM diagnosis (weeks), mean ± SD | 26.4±1.7 | – | – |
| FPG from OGTT (mmol/L), mean ± SD | 5.58±2.2 | 4.30±0.3 | 0.10 |
| 1 h glucose (mmol/L), mean ± SD | 11.2±3.6 | 7.21 ±1.2 | 0.006 |
| 2 h glucose (mmol/L), mean ± SD | 8.12±3.3 | 6.05±1.2 | 0.08 |
| Mean CGM wear-time (days), mean ± SD | 13.5±1.5 | 13.7±0.8 | 0.67 |
Notes: The p value significance is set at p<0.05. *Missing data: Education (n=5); pre-pregnancy BMI (n=1).
Abbreviations: FPG, fasting plasma glucose; GDM, gestational diabetes mellitus; BMI, body mass index; OGTT, oral glucose tolerance test.
CGM Glycemic Profiles Between Patients Who Developed GDM and Patients Who Did Not
CGM parameters of participants in the first trimester of pregnancy who developed GDM and those who did not are presented in Table 2. CGM application in the first trimester at an average of 11 weeks of gestational age was associated with higher SD (adjusted median [IQR] 1.31 (1.2–1.3) vs 1.01 [0.9–1.0] mmo/L, p= 0.001) and higher MAGE (3.26 [3.2–3.3] vs 2.59 [2.4–2.6] mmol/L, p=0.002) in participants who were subsequently diagnosed with GDM at average of 26 weeks gestational age. There were also nonsignificant trends of higher J-Index and %CV in participants who developed GDM than participants who did not (p<0.05). CGM application in the second trimester of pregnancy at an average of 20 weeks of gestational age was also associated with both higher SD (1.35 [1.3–1.4] vs 0.99 [0.98–1.0] mmol/L, p=0.002) and higher MAGE (3.32 [3.3–3.4] vs 2.42 [2.4–2.5] mmol/L, p<0.001; Table 3), as well as nonsignificant trends of higher mean and J-Index values in participants who developed GDM compared to those who did not (p<0.05). Other parameters analyzed, such as %TIR, %TAR, and %TBR, did not display trends or significant differences in the first or second trimesters with GDM development (p>0.003).
Table 2.
Glycemic Variability in the 1st Trimester in Pregnant Women with and without GDM (n=60)
| CGM Parameters (n=60) | GDM (n=10) Adjusted Median (IQR) | Non-GDM (n=50) Adjusted Median (IQR) | Adjusted p* |
|---|---|---|---|
| First trimester | |||
| Gestational age at CGM application (weeks), mean ± SD | 11.1±1.2 | 11.1±1.4 | 0.93 |
| Mean glucose (mmol/L) | 4.43 (4.2–4.6) | 4.07 (4.0–4.2) | 0.20 |
| J-Index | 10.0 (8.8–10.4) | 8.26 (7.1–9.8) | 0.04 |
| MAGE (mmol/L) | 3.26 (3.2–3.3) | 2.59 (2.4–2.6) | 0.002 |
| SD (mmol/L) | 1.31 (1.27–1.32) | 1.01 (0.95–1.02) | 0.001 |
| CV (%), adjusted mean ± SD | 28.3±1.6 | 24.3±1.1 | 0.007 |
| TIR (%), adjusted mean ± SD | 68.9±5.4 | 69.2±3.9 | 0.51 |
| TBR (%), adjusted mean ± SD | 26.9±5.7 | 30.3±4.2 | 0.84 |
| TAR (%) | 4.30 (3.96–4.40) | 0.59 (0.20–0.93) | 0.05 |
Notes: *p values were adjusted for maternal pre-pregnancy BMI and ethnicity Data was expressed as adjusted median (interquartile range) unless otherwise stated. The p value significance is set at p<0.003.
Abbreviations: GDM, gestational diabetes mellitus; BMI, body mass index; CGM, continuous glucose monitoring; %CV, coefficient of variation; SD, standard deviation; MAGE, Mean amplitude of glycemic excursions; GA, gestational age; %TAR, percentage of time above target range; %TIR, percentage of time in range; %TBR, percentage of time below target range.
Table 3.
Glycemic Variability in the 2nd Trimester in Pregnant Women with and without GDM (n=53)
| CGM Parameters (n=53) | GDM (n=9) Adjusted Median (IQR) | Non-GDM (n=44) Adjusted Median (IQR) | Adjusted p* |
|---|---|---|---|
| Second trimester | |||
| Gestational age at CGM application (weeks), mean ± SD | 20.6±1.2 | 20.5±0.90 | 0.99 |
| Mean glucose (mmol/L) | 4.88 (4.8–5.1) | 4.09 (4.0–4.2) | 0.02 |
| J-Index | 13.5 (12.9–14.7) | 8.50 (8.1–9.2) | 0.007 |
| MAGE (mmol/L) | 3.32 (3.3–3.4) | 2.42 (2.4–2.5) | <0.001 |
| SD (mmol/L) | 1.35 (1.3–1.4) | 0.99 (0.98–1.01) | 0.003 |
| CV (%), adjusted mean ± SD | 27.5±2.4 | 24.4±1.7 | 0.13 |
| TIR (%), adjusted mean ± SD | 72.3±2.1 | 68.7±1.5 | 0.74 |
| TBR (%), adjusted mean ± SD | 19.8±4.4 | 30.5±3.2 | 0.35 |
| TAR (%) | 7.42 (6.4–9.4) | 0.33 (−0.03–1.7) | 0.07 |
Notes: Data was expressed as adjusted median (interquartile range) unless otherwise stated. The p value significance level is set at p<0.003. *p values were adjusted for maternal pre-pregnancy BMI and ethnicity.
Abbreviations: GDM, gestational diabetes mellitus; BMI, body mass index; CGM, continuous glucose monitoring; %CV, coefficient of variation; SD, standard deviation; MAGE, Mean amplitude of glycemic excursions; GA, gestational age; %TAR, percentage of time above target range; %TIR, percentage of time in range; %TBR, percentage of time below target range.
In sensitivity analyses of a subset of n=49 participants, similar nonsignificant trends (p<0.05) were observed in the first trimester, with SD and MAGE being higher in participants who developed GDM than thos who did not, and this was statistically significant only in the second trimester (SD 3.36 [3.3–3.4] vs 2.45 [2.4–2.5] mmol/L, p<0.001; MAGE 1.39 [1.3–1.4] vs 0.98 [0.9–1.0] mmol/L, p<0.001; Supplementary Table S2). Only the trends of SD and MAGE levels across the first, second, and third trimesters that showed statistical significance in the earlier analysis are presented in Supplementary Figure S2 and Supplementary Table S3 in a subset of 39 participants. Overall, the participants who were diagnosed with GDM at 24–31 weeks showed an overall trend of higher SD and MAGE that was already evident in first trimester, with values increasing by the second trimester and sustained through to the third trimester compared to those who were not diagnosed with GDM (Supplementary Figure S2). There were no statistically significant differences in SD and MAGE values between the two groups (p>0.003) in this subset of participants.
Discussion
Our study, which utilized CGM-derived data to analyze GV and GC parameters in early pregnancy (first and second trimester) with subsequent diagnosis of GDM in the early third trimester, is the first to have examined this prospective association using data collected from a longitudinal observational study. We are the only study thus far to report that SD and MAGE as CGM-derived GV parameters at 11 and 20 weeks of gestation were significantly associated with pregnant women subsequently diagnosed with GDM at an average of 26 weeks’ gestation. Our findings contribute to the much-needed evidence examining the value of CGM wearing and the use of such data early in pregnancy. It supports future studies on the possible use of CGM for risk prediction of subsequent GDM diagnosis to initiate early risk stratification, diagnosis, and lifestyle interventions.24
None of the existing studies examined the prospective association between SD and GDM.13,14,17,19 Moreover, of all these studies,13,14,17,19 only one reported a significant difference between subjects who developed GDM and those who did not.14 However, that study design was cross-sectional, where participants diagnosed with GDM at 24–28 weeks wore the CGM sensor for only a short duration of 3 days after the diagnosis.14 In contrast, our prospective study design measured SD prior to the diagnosis of GDM using data from longer CGM wear time of 8–14 days. In the other studies that had null findings, one examined SD in all three trimesters, with the outcome of GDM showing only a borderline significant association when compared to those who did not develop GDM in a small sample of 30 participants.19 One other study had inconsistent associations when examining SD in the second and third trimesters, and reported nonsignificantly higher SD only in the third trimester, but lower SD in the second trimester in GDM participants when compared to study participants without GDM.13 Comparisons with previous studies were also difficult because of the case–control13,14,19 and cross-sectional17 study designs versus our prospective association, short CGM wear times of between 4813,19 and 72 hours14 versus our longer wear time of 8–14 days, use of different GDM diagnostic criteria,13,14,19 while ours used the IADPSG criteria adopted by the World Health Organization for the diagnosis of GDM. So far, our study is the only one to show a significant prospective association between SD derived from CGM wear at both the first and second trimesters with a subsequent diagnosis of GDM.
MAGE as a GV parameter in association with GDM has only been published in three case–control studies, where GDM diagnosis preceded the measurement of MAGE using CGM.13,14,19 Su et al14 reported significantly higher levels of MAGE in pregnant women who were diagnosed with GDM than those who did not develop GDM and nonpregnant healthy women with normal glucose regulation. Similarly, Dalfra et al19 reported an overall trend of slightly higher MAGE levels across the first, second, and third trimesters of pregnancy in women who developed GDM than healthy patients, although the significance was borderline in a small sample of 30 subjects. When MAGE levels were assessed independently in the first and second trimesters of pregnancy in another study by Dalfa et al, they were reported to be lower in the second trimester, but higher in the third trimester in participants with GDM than participants without GDM.13 Both studies published by Dalfa et al used CGM data after a short wear time of 2 days,13,19 which might not be sufficient to optimally assess GC,25 and a GDM diagnosis across a wide time span with an average of 21 weeks of gestational age with an SD of 6.3 weeks, which might result in misclassifications,1 possibly explaining the discrepancies in their study13,19 findings with ours. Beyond the findings reported in these previous studies, our study further elucidates that other than SD, MAGE in early pregnancy (first and second trimesters) may be another CGM-derived measure suitable for exploring in future studies as a potential predictive marker for the diagnosis of GDM.
MAGE was the first DM-specific GV metric to be developed primarily to capture mealtime-related and intraday glucose excursions, and has been considered a gold standard for assessing GV. It has been associated with increased insulin resistance and early-phase insulin-secretion deterioration,14 which are characteristic of the pathophysiology of GDM and type 2 DM development.26 Furthermore, higher MAGE levels representing greater glucose fluctuations have been associated with adverse maternal and neonatal outcomes attributed to GDM, including large for gestational age, small for gestational age, higher birth weight, and neonatal hypoglycemia.27 In contrast, SD, which is also used as a measure of intraday glucose excursions has not been reported to be associated with maternal or neonatal outcomes.12
There was an overall trend of higher SD and MAGE levels across the first to the third trimester of pregnancy in participants diagnosed with GDM than participants who were not. Interestingly, there was also a subtle trend of increasing SD and MAGE from the first to the second trimester of pregnancy in patients with GDM. This observation can be explained by the physiological changes in the action and secretion of insulin, where serum insulin levels progressively increase from the first to the third trimester of pregnancy, signifying an increase in insulin resistance as the pregnancy advances.28 This can then be correlated with higher glucose variability exacerbated by glycemic instability in the later trimesters of pregnancy, as seen in a study by Dalfra et al.19 The authors of that study reported an overall increasing trend of GV parameters (MAGE, SD, continuous overlapping net glycemic action, IQR) from the first to the third trimester of pregnancy in both healthy pregnant women and pregnant women with GDM.19 Coupled with the available evidence from the literature, our findings firstly allude to inherent differences in SD and MAGE levels in pregnant women eventually diagnosed with GDM compared to those without GDM, and secondly these differences were likely to be more pronounced from the second trimester of pregnancy.
In our study, mean glucose, %CV, J-Index, %TIR, %TAR, and %TBR were not significantly associated with GDM outcomes. Across the existing literature, these CGM-derived parameters have not been shown to be consistently associated with GDM outcomes, despite such parameters as %CV being a recommended GV metric in clinical practice.11 Three studies reported mean glucose to be significantly higher in women who developed GDM,14,16,19 one study reported significant associations only in the second trimester, but not the third,13 while another three reported null associations.15,17,18 Only one other cross-sectional study analyzed %CV, J-Index, and time in glucose ranges (%TIR, %TBAR, and %TBR) and reported null associations with GDM outcomes.17
Our study has demonstrated the use of the CGM sensor during pregnancy to be a promising, valuable, and applicable technology that can be applied in clinical practice for gestational glucose profiling to determine GV and GC parameters in a convenient and pain-free manner. Detecting and monitoring GV is particularly important in the context of pregnancy, where greater GV and lower GC relate to poorer clinical outcomes,10,12,29 and our study has shown that CGM use in pregnancy can objectively and accurately measure these blood glucose variations across a 24-hour period for up to 14 days. The major contribution of this study is that the glucose variability readings from the sensor can be used in early pregnancy to identify those who might be at risk of developing GDM in index pregnancy. Preliminary findings from this study provide a framework for the possible design of future cohort studies on a larger scale to eventually develop and validate a risk-prediction model for GDM using SD and MAGE as GV markers in early pregnancy. Early risk prediction would lead to early risk stratification of pregnant women who are most of risk of developing GDM, and from there, intervention studies may be designed for better GDM management starting early in pregnancy.
Strengths and Limitations
Firstly, the strengths in our study lie in its prospective design, which enabled us to assess the temporal sequence between GV and GC parameters measured by CGM in the first and second trimesters of pregnancy with those who were subsequently diagnosed with GDM in the early third trimester of pregnancy. Unlike previously published studies, which were either case–control13,14,19 or cross-sectional15,17,18 and where the diagnosis of GDM preceded the application of CGM, our study had study participants don the CGM device during the first and second trimesters before OGTTs were conducted at 24–31 weeks to diagnose GDM. Secondly, our study has analyzed CGM data from an average of approximately 14 days wear time to acquire a more accurate and meaningful interpretation of the glucose data.25 The FreeStyle Libre has been shown to have good overall accuracy, especially considering that it measures glucose concentrations in extracellular fluid and does not need to be calibrated.30 However, it has been reported to measure systematically lower glucose concentrations (negative bias),31 which might explain the high percentages of TBR, although none of the participants reported hypoglycemia. Lastly, our study has limited generalizability due to the small sample and the number of GDM outcomes, and would need to be replicated in a larger sample.
Conclusion
We have shown an association between higher SD and MAGE in the first and second trimesters in women who were subsequently diagnosed with GDM in the early third trimester. We believe that early pregnancy presents a unique opportunity for early GDM risk stratification, and prediction of GDM development with the use of GV parameters derived from CGM to allow for earlier lifestyle interventions to prevent adverse maternal and child health outcomes.32
Acknowledgments
We would like to thank the participants and the Integrating the Use of Calibration-Free Continuous Monitoring for Pregnancy Glucose Profiling (I-Profile) study group, including:Ann Wright, Shephali Tagore, Bernard Su Min Chern, and Seng Bin Ang. We would also like to thank the clinical research coordinators Nurul Syaza Razali, Nurul Sakinah Razali, and Sally Mun Hua Chai for contributing to data collection.
Funding Statement
This research was supported by the Integrated Platform for Research in Advancing Metabolic Health Outcomes in Women and Children (IPRAMHO) — Singapore Ministry of Health National Medical Research Council Centre grant NMRC/CG/C008A/2017_KKH.
Abbreviations
GV, glycemic variability; GC, glycemic control; CGM, continuous glucose monitoring; GDM, gestational diabetes mellitus; OGTT, oral glucose-tolerance test; MAGE, mean amplitude glycemic excursion; CV, coefficient of variation; BMI, body-mass index; TAR, time above range; TBR, time below range; TIR, time in range.
Data Sharing
We would like to declare that at this moment the clinical trial data are unavailable for access or unsuitable to post because of patient confidentiality. However, all the data presented in this manuscript can be made available upon personal request from the corresponding author.
Ethics
The authors are accountable for all aspects of this study in ensuring that questions related to the accuracy or integrity of any part of the work were well investigated and resolved. The study was conducted based on the principles of Declaration of Helsinki and was authorized by the Sing Health Centralised Institutional Review Board (reference 2018/2128) All participants gave written informed consent in accordance with the Declaration of Helsinki. Clinical trial identification number: NCT05123248.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.López Stewart G. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization guideline. Diabetes Res Clin Pract. 2014;103(3):341–363. doi: 10.1016/j.diabres.2013.10.012 [DOI] [PubMed] [Google Scholar]
- 2.Chong YS, Cai S, Lin H, et al. Ethnic differences translate to inadequacy of high-risk screening for gestational diabetes mellitus in an Asian population: a cohort study. BMC Pregnancy Childbirth. 2014;14:345. doi: 10.1186/1471-2393-14-345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crowther CA, Hiller JE, Moss JR, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352(24):2477–2486. doi: 10.1056/NEJMoa042973 [DOI] [PubMed] [Google Scholar]
- 4.Gillman MW, Oakey H, Baghurst PA, Volkmer RE, Robinson JS, Crowther CA. Effect of treatment of gestational diabetes mellitus on obesity in the next generation. Diabetes Care. 2010;33(5):964–968. doi: 10.2337/dc09-1810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venkataraman H, Ram U, Craik S, Arungunasekaran A, Seshadri S, Saravanan P. Increased fetal adiposity prior to diagnosis of gestational diabetes in South Asians: more evidence for the ‘thin-fat’ baby. Diabetologia. 2017;60(3):399–405. doi: 10.1007/s00125-016-4166-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sovio U, Murphy HR, Smith GC. Accelerated fetal growth prior to diagnosis of gestational diabetes mellitus: a prospective cohort study of nulliparous women. Diabetes Care. 2016;39(6):982–987. doi: 10.2337/dc16-0160 [DOI] [PubMed] [Google Scholar]
- 7.Graca G, Duarte IF, Barros AS, et al. Impact of prenatal disorders on the metabolic profile of second trimester amniotic fluid: a nuclear magnetic resonance metabonomic study. J Proteome Res. 2010;9(11):6016–6024. doi: 10.1021/pr100815q [DOI] [PubMed] [Google Scholar]
- 8.Clarke E, Cade TJ, Brennecke S. Early pregnancy screening for women at high-risk of GDM results in reduced neonatal morbidity and similar maternal outcomes to routine screening. J Pregnancy. 2020;2020:9083264. doi: 10.1155/2020/9083264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Umpierrez GE, Pk B. Glycemic variability: how to measure and its clinical implication for type 2 diabetes. Am J Med Sci. 2018;356(6):518–527. doi: 10.1016/j.amjms.2018.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu Q, Aris IM, Tan KH, Li LJ. Application and utility of continuous glucose monitoring in pregnancy: a systematic review. Front Endocrinol. 2019;10:697. doi: 10.3389/fendo.2019.00697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42(8):1593–1603. doi: 10.2337/dci19-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu W, Wu N, Li L, OuYang H, Qian M, Shen H. A review of research progress on glycemic variability and gestational diabetes. Diabetes Metab Syndr Obes. 2020;13:2729–2741. doi: 10.2147/DMSO.S261486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dalfra MG, Sartore G, Di Cianni G, et al. Glucose variability in diabetic pregnancy. Diabetes Technol Ther. 2011;13(8):853–859. doi: 10.1089/dia.2010.0145 [DOI] [PubMed] [Google Scholar]
- 14.Su JB, Wang XQ, Chen JF, et al. Glycemic variability in gestational diabetes mellitus and its association with beta cell function. Endocrine. 2013;43(2):370–375. doi: 10.1007/s12020-012-9753-5 [DOI] [PubMed] [Google Scholar]
- 15.Mazze R, Yogev Y, Langer O. Measuring glucose exposure and variability using continuous glucose monitoring in normal and abnormal glucose metabolism in pregnancy. J Matern Fetal Neonatal Med. 2012;25(7):1171–1175. doi: 10.3109/14767058.2012.670413 [DOI] [PubMed] [Google Scholar]
- 16.Nigam A, Sharma S, Varun N, Munjal YP, Prakash A. Comparative analysis of 2-week glycaemic profile of healthy versus mild gestational diabetic pregnant women using flash glucose monitoring system: an observational study. BJOG. 2019;126(Suppl 4):27–33. doi: 10.1111/1471-0528.15849 [DOI] [PubMed] [Google Scholar]
- 17.Gaborova M, Donicova V, Bacova I, et al. Glycaemic variability and risk factors of pregnant women with and without gestational diabetes mellitus measured by continuous glucose monitoring. Int J Environ Res Public Health. 2021;18(7):3402. doi: 10.3390/ijerph18073402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cypryk K, Pertynska-Marczewska M, Szymczak W, Wilcynski J, Lewinski A. Evaluation of metabolic control in women with gestational diabetes mellitus by the continuous glucose monitoring system: a pilot study. Endocr Pract. 2006;12(3):245–250. doi: 10.4158/EP.12.3.245 [DOI] [PubMed] [Google Scholar]
- 19.Dalfra MG, Chilelli NC, Di Cianni G, et al. Glucose fluctuations during gestation: an additional tool for monitoring pregnancy complicated by diabetes. Int J Endocrinol. 2013;2013:279021. doi: 10.1155/2013/279021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edelman SV, Argento NB, Pettus J, Hirsch IB. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care. 2018;41(11):2265–2274. doi: 10.2337/dc18-1150 [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes A. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–S31. doi: 10.2337/dc20-S002 [DOI] [PubMed] [Google Scholar]
- 22.Wojcicki JM. “J”-index. A new proposition of the assessment of current glucose control in diabetic patients. Horm Metab Res. 1995;27(1):41–42. doi: 10.1055/s-2007-979906 [DOI] [PubMed] [Google Scholar]
- 23.Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295(14):1681–1687. doi: 10.1001/jama.295.14.1681 [DOI] [PubMed] [Google Scholar]
- 24.Lee KW, Ching SM, Ramachandran V, et al. Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2018;18(1):494. doi: 10.1186/s12884-018-2131-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riddlesworth TD, Beck RW, Gal RL, et al. Optimal sampling duration for continuous glucose monitoring to determine long-term glycemic control. Diabetes Technol Ther. 2018;20(4):314–316. doi: 10.1089/dia.2017.0455 [DOI] [PubMed] [Google Scholar]
- 26.Kautzky-Willer A, Prager R, Waldhausl W, et al. Pronounced insulin resistance and inadequate beta-cell secretion characterize lean gestational diabetes during and after pregnancy. Diabetes Care. 1997;20(11):1717–1723. doi: 10.2337/diacare.20.11.1717 [DOI] [PubMed] [Google Scholar]
- 27.Yu F, Lv L, Liang Z, et al. Continuous glucose monitoring effects on maternal glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus: a prospective cohort study. J Clin Endocrinol Metab. 2014;99(12):4674–4682. doi: 10.1210/jc.2013-4332 [DOI] [PubMed] [Google Scholar]
- 28.Sonagra AD, Biradar SM, D K, Murthy DSJ. Normal pregnancy- a state of insulin resistance. J Clin Diagn Res. 2014;8(11):CC01–CC03. doi: 10.7860/JCDR/2014/10068.5081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wyckoff JA, Brown FM. Time in range in pregnancy: is there a role? Diabetes Spectr. 2021;34(2):119–132. doi: 10.2337/ds20-0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bailey T, Bode BW, Christiansen MP, Klaff LJ, Alva S. The performance and usability of a factory-calibrated flash glucose monitoring system. Diabetes Technol Ther. 2015;17(11):787–794. doi: 10.1089/dia.2014.0378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olafsdottir AF, Attvall S, Sandgren U, et al. A clinical trial of the accuracy and treatment experience of the flash glucose monitor freestyle libre in adults with type 1 diabetes. Diabetes Technol Ther. 2017;19(3):164–172. doi: 10.1089/dia.2016.0392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Langer O, Yogev Y, Most O, Xenakis EM. Gestational diabetes: the consequences of not treating. Am J Obstet Gynecol. 2005;192(4):989–997. doi: 10.1016/j.ajog.2004.11.039 [DOI] [PubMed] [Google Scholar]