Abstract
Background:
The health system in Ghana is severely underequipped to meet the needs of children with behavioral health problems. A substantial treatment gap exists among individuals with behavioral challenges, necessitating the implementation of an evidence-based intervention to address child behavioral challenges in Ghana. This article presents learning opportunities from the adaptation and initiation process of an evidence-based approach, the multiple-family group (MFG) intervention, aimed at addressing child behavioral challenges in northern Ghana.
Methods:
The MFG intervention will be tested and implemented in three schools selected through a clustered randomization process, with 60 child-caregiver dyads per school. Each school will be assigned to MFG delivery by parent peers, MFG delivery by School Health Education Program (SHEP) coordinators, or an intervention where students are supplied only with mental health wellness materials and educational supports. The providers will be assessed on a fidelity measure.
Results:
The approach of engaging stakeholders in Ghana is anticipated to prove challenging because multiple partners are involved in MFG implementation. Participants are expected to actively participate, however, given some changes to the protocol to adapt it to the Ghanaian context, including the types of MFG facilitators and sample size. Other anticipated challenges include obtaining permission from key partners such as the education authorities, timing of the study within the academic calendar in Ghana, and meeting the high expectations of school authorities for the study.
Next steps:
The MFG intervention will be delivered by parent peers and SHEP coordinators at the selected schools.
Editor’s Note:
In partnership with Milton L. Wainberg, M.D., Psychiatric Services is publishing protocols to address the gap between global mental health research and treatment. These protocols present largescale, global mental health implementation studies soon to begin or under way. Taking an implementation science approach, the protocols describe key design and analytic choices for delivery of evidence-based practices to improve global mental health care. This series represents the best of our current science, and we hope these articles inform and inspire.
The importance of improving child behavioral health in sub-Saharan Africa has been recognized. Studies indicate that from 2000 to 2015, sub-Saharan Africa’s population grew by 49%, yet the number of person-years lost to disability due to mental and substance use disorders increased by 52% (1). In 2015, 17.9 million years of healthy life were lost because of mental health problems in sub-Saharan Africa. Mental disorders were almost as important a cause of years lost to disability as were infectious and parasitic diseases, which accounted for 18.5 million years lost to disability in this geographical area (2). Sub-Saharan Africa’s population is expected to double over the next three decades (3), and the pressures on young people, who across the region already are struggling to earn a livelihood in highly competitive labor markets, are likely to go up (1). Many will experience psychological problems as they fail to realize their ambitions because of mental disorders, which need to be addressed as part of the United Nations’ Sustainable Development Goals (4, 5)
The sub-Saharan African country Ghana has a need for increased attention to child behavioral health disorders affecting their daily functioning (6). At the national level, measures such as the Children’s Act, 1998 have been put in place to ensure that children receive care. The act aims at reforming and consolidating the laws relating to children, including rights of the child, care and adoption, child labor, and apprenticeship.
Many of these measures are to be enforced by state agencies such as the ministries and municipal and district assemblies, nongovernmental organizations (NGOs), and civil society organizations. Article 37(2)(b) of the Constitution of Ghana states that “the state shall enact appropriate laws to assure the protection and promotion of all other basic human rights and freedoms, including the rights of the disabled, the aged, children and other vulnerable groups in the development processes.” These are commitments of the state and other institutions to ensure that children are provided with the requisite protection to enable them to realize their developmental milestones. The expectation is that these legal provisions would be accompanied by appropriate mental health systems such that children in Ghana will not experience any major behavioral health problems.
In Ghana, most of the population comprises children, yet the Ghanaian health system is severely underequipped to meet the needs of children with behavioral health problems (7). Although evidence-based practices that support child mental health exist in other countries, such as the United States, steps to take them to scale have been plagued by challenges related to uptake, implementation, integration, and sustainability, especially in sub-Saharan Africa (8). It is estimated that nearly 500 million people, most of whom live in poverty and in low- and middle-income countries, have behavioral health challenges (9). The World Health Organization (WHO) estimates that prevalence rates of these challenges may be even higher (at 20%) (10). Additionally, the WHO estimates that more than 2 million people in Ghana have some form of mental disorder, of whom about one-third (650,000) may have severe mental disorders (9). There is a substantial treatment gap (i.e., a significant number of people with mental disorders who are unable to access treatment) among individuals with mental disorders in Ghana, estimated at >90% of all individuals in need of treatment (9, 11). Moreover, many individuals experience considerable delays while seeking early mental health interventions from available qualified professionals or at facilities that manage behavioral health problems, which results in poor clinical and functional outcomes (12–14).
Lack of evidence-based care at the community level, especially in care-deprived areas such as Ghana’s northern region, leaves those seeking mental health treatment with mainly religious services (such as prayer camps) and traditional healers as their only options. For children with disruptive behavior disorders who do not get the required treatment, the lack of mental health services becomes a serious concern because the disorders usually persist through adolescence into adulthood (12, 15–17).
Children with disruptive behavior disorders have an increased risk for dropping out of school, substance use and abuse, delinquency, incarceration, criminal behaviors, and premature death (12). Some studies have linked specific risk factors such as poverty, low parental educational attainment, maternal depression, harsh parenting, poor parent-child relationships, stress, and orphanhood to increased incidence of disruptive behavior disorders among children (14). Outcomes associated with disruptive behavior disorders have been noted to include academic problems, social impairment, higher incidence of chronic general medical problems, unemployment and legal problems, and substance abuse and violence among adults (12, 13, 18–21).
Prevalence rates of disruptive behavior disorders ranging from 12% to 33% have been reported in some sub-Saharan African countries (22–27). In Ghana, the most commonly reported disruptive behavior disorder, with a prevalence rate of 12.8%, is attention-deficit hyperactivity disorder, whose rates are higher among boys (14.4%) than girls (10.5%) (28). Mental health service in Ghana is available at most levels of care. However, most of the care is provided through specialized psychiatric hospitals (close to the capital and servicing only a small proportion of the population), with relatively lower levels of government provision and funding for general hospital and primary health care–based services. The few community-based services that are provided are private (9). Given the serious consequences of failing to intervene as disruptive behavior disorders begin to emerge, it is imperative that effective and scalable solutions for child behavioral health be discovered, while recognizing the challenges the country faces in meeting the educational and mental health care needs of its large youth population (7). The growing recognition in Ghana that investing in child behavioral health is important may lead to innovative changes in the behavioral health system (29).
OBJECTIVE AND HYPOTHESES
The primary purpose of this planned study is to explore whether the short- and long-term effects of a modified multiple-family group (MFG) intervention can improve the behaviors of children with disruptive behavior problems and their families in northern Ghana. The MFG is a family-centered, group-delivered, evidence-informed, and manualized intervention that targets youths with oppositional defiant disorder or conduct disorder. As part of the SMART Africa Study funded by the National Institute of Mental Health (NIMH) and led by Brown School at Washington University in St. Louis, the research team is implementing a pilot cluster-randomized clinical trial, with a learning agenda designed to fit the Ghanaian context, that seeks to address serious disruptive behaviors among children in Ghana. School Health Education Program (SHEP) coordinators and parent peers will deliver the MFG because both groups are available and directly involved with the school system. Box 1 summarizes the design and key challenges and advantages of the study.
BOX 1. Design and key challenges and advantages of the multiple-family group (MFG) intervention study.
Study Design
The study will recruit 180 child-caregiver dyads across the three study conditions (N=360) from three public primary schools.
The study’s intervention facilitators include the School Health Education Program coordinators and parent peers.
Key Challenges
Delays in obtaining permission for the MFG intervention study from the education authorities
Timing of the study within Ghana’s academic calendar
High expectations of school authorities regarding benefits of study participation
Key Advantages
Adaptation of the Ugandan MFG intervention to the local context in Ghana’s northern regions
High levels of enthusiasm among parents and teachers to be part of the MFG study
Positive responses from school administrators
Discussions among school authorities and parents/caregivers about child disruptive behavior
The hypotheses about the outcomes of the MFG intervention are the following. Children who participate in MFG with their families will display significantly reduced behavioral conduct difficulties and increased functioning over time compared with those in a comparison condition. Children in the parent peer–delivered condition will experience greater improvement in conduct than children assigned to two other study conditions. Initially, we expect that SHEP coordinators will adhere to MFG administration with higher fidelity than parent peers; yet, with training and ongoing supervision, we anticipate that these differences will decrease over time.
METHODS
Overview
The SMART Africa–Ghana study aims to investigate both short- and long-term improvements in the conduct of children with disruptive behavior issues in Ghana who are given the MFG intervention. The study seeks to examine the adaptation of the MFG intervention and its implementation protocol originally developed in Uganda to the Ghanaian context. It aims to ascertain findings on the implementation, fidelity, and sustainability of two MFG intervention approaches delivered by trained parent peers and SHEP coordinators rather than by community health workers who delivered the MFG intervention in Uganda. This study also will examine the multilevel factors that influence intervention implementation, uptake, sustainability, and outcomes. The MFG intervention will use the knowledge, skills, abilities, and tools (KSAT) criteria that require facilitators to be trained in these four domains and pass a test assessing facilitator proficiency of KSAT at ≥85%. Facilitators who do not pass the test will be retrained and required to retake the test until they pass it. During the MFG implementation period, facilitators will receive 2 hours per month of group supervision across sites while the MFGs are in progress. The members of the research team trained in the MFG intervention are required to participate in every MFG session that provides ongoing support, supervision, and troubleshooting for facilitators.
All study procedures were approved by the Washington University in St. Louis Internal Review Board (no. 2016011088) and the in-country ethical review board of the Ghana Health Service (GHS-ERC:04/03/2016). The study procedures were also approved by the data safety and monitoring board at the NIMH. All study participants will meet the research team and provide informed consent and child assent.
Study Procedures
The adapted Ghanaian protocol design was based on a pilot version of an Ugandan study, representing a scale-up of the MFG intervention that recruited participants (N=3,000 child-caregiver dyads) from 30 public primary schools in five districts in southwestern Uganda (7). In the Ugandan project, children recruited into the study were between ages 8 and 13 years and enrolled in grades 2–7.
The Ghanaian study has been designed as a small-scale pilot project incorporating lessons learned from Uganda. Specifically, the Ghana study recruited participants (N=300 child-caregiver dyads) from three public primary schools located in the Tamale and Sagnarigu districts in Ghana’s northern region. The children recruited were between 8 and 13 years old and enrolled in grades 2–5, mirroring the recruitment protocol used in the Ugandan scale-up study. The differences in the classes and ages is due to some of the pupils starting school at a later age in Ghana.
The facilitators in the MFG intervention in Ghana include the SHEP coordinators and parent peers, whereas the facilitators in the Uganda intervention included community health workers (CHWs) and parent peers. Therefore, implementing the pilot version of the larger Ugandan study required assessing the contextual environment in Ghana to determine the feasibility of implementing the adapted MFG protocol to scale. This contextual evaluation required an assessment involving key stakeholders to determine the ideal sample population, MFG intervention modality, facilitators, and specific districts in northern Ghana, which is the optimal place where the schools and participants would be recruited.
The eligible schools in the two districts were identified and selected on the basis of student census and location such that the selected intervention schools from the two districts would be far apart to avoid exchange of intervention information among the schools whose pupils are study participants. A total of 102 schools representing urban and nonurban communities were initially identified. The schools included 48 from the Sagnarigu district, a nonurban region, and 54 from the Tamale metropolitan district, a more urban and more economically developed region. The households in Sagnarigu district consist mostly of subsistence farmers, and those from the Tamale metropolitan district include a relatively educated population with a mixture of white- and blue-collar professions. It is the fourth-largest metropolitan city in Ghana with a population of about half a million (roughly divided evenly by gender) and an annual population growth rate of about 3% (30).
Figure 1 summarizes the school sampling process. The geographic stratification of the schools’ locations and the use of clustered random sampling resulted in the selection of six schools. The study has three study arms, with each arm having two schools, from which one school each was then randomly selected for inclusion in the study. The three final schools were assigned as follows: the adapted MFG delivered by parent peers in Sagnarigu, MFG delivered by SHEP coordinators in Tamale, and a school also in Tamale for a comparison intervention where students are supplied only with mental health wellness materials and educational supports, such as books.
FIGURE 1. The multiple-family group (MFG) intervention sampling processa.
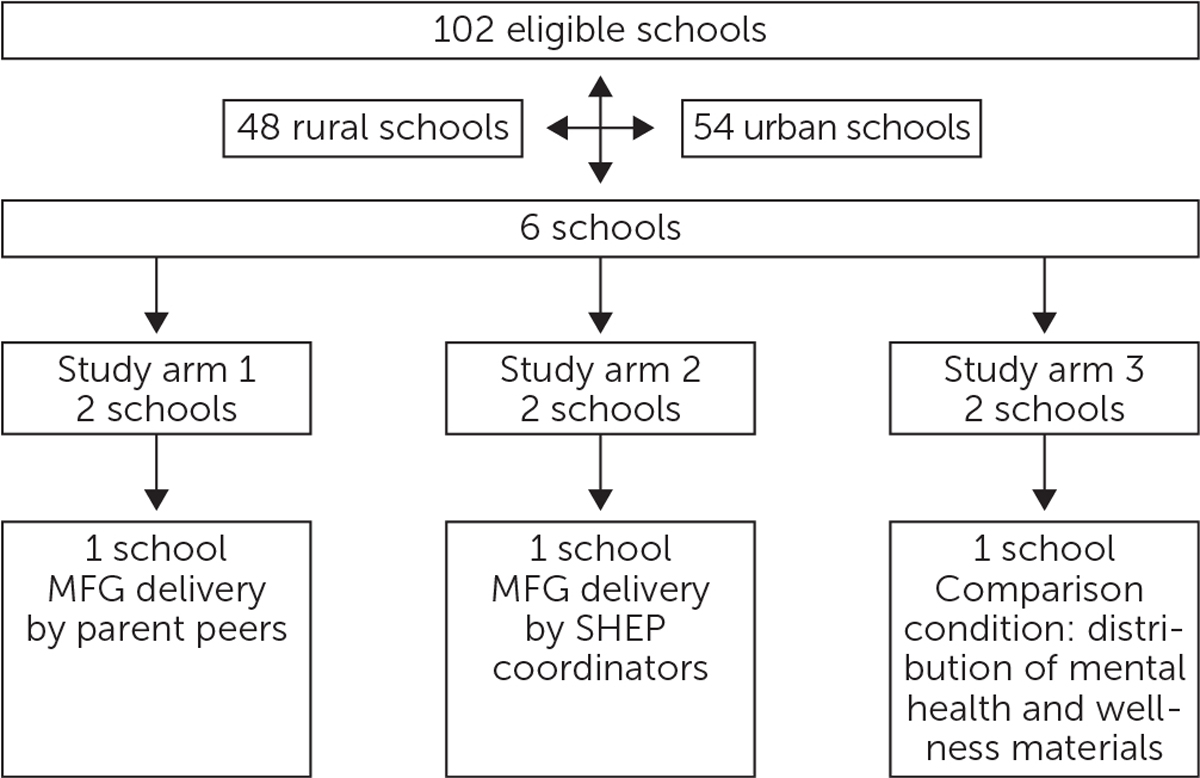
a SHEP, School Health Education Program.
Summary of Measures
After consent procedures are completed, the screening measures administered to the children will include the Disruptive Behavior Disorder Rating Scale (31), IOWA Conners Scale (32), and Impairment Scale (33). If a child meets the criteria for a clinically significant behavioral problem on any of the scales, the child will have met the criterion for the presence of behavioral difficulties and be considered “positive” for a behavioral disorder. A child who does not show evidence of disruptive behavior disorder on any of the scales will be considered “negative.” For evidence of fidelity to the MFG intervention, the SHEP coordinators and parent peers will complete a fidelity assessment checklist on completion of the MFG intervention (34).
Analysis Strategy
We will first conduct interitem reliability analyses by using confirmatory factor analytic perspectives for all scales and examine correlations across time and construct. Summarized scoring procedures are available for the scales proposed, but multiplicity of scores in particular domains may yield multicollinearity; thus, factor analysis (35) and chi-squared automatic interaction detector (CHAID) algorithms will be used to identify the strongest variables (i.e., family-level, facilitator, or school variables) that affect children’s behavioral health. The Exhaustive CHAID method will be used to explore how various groups of predictor variables relate to behavior outcomes. Analyses will then be performed to compare the descriptive and clinical characteristics among the schools in the three study arms to ensure that randomization was achieved. The structural equations model will be used to compare the performances of SHEP coordinators and parent peers on the MFG intervention.
Community Involvement: Recruitment and Training
In the school assigned to the parent peer–delivered MFG intervention, the community and parents will be engaged first, with the research team reaching out to the school’s administration, specifically the school principal/head teacher. This engagement will be followed by a meeting with the parent-teacher association (PTA) to explain the program. The school administration and the PTA then will send out flyers providing an overview of the study and inviting parents to a meeting. At this meeting, interested parents who agree to participate will be offered training as a parent peer who delivers the MFG. Another meeting will be organized with the principal/head teacher, PTA, and students, where the research team provides an overview of the study and addresses questions and concerns.
After the meetings, four parents will be selected for the parent peer–delivered MFG condition, and at the school assigned as the SHEP coordinator–delivered condition, four SHEP coordinators will be selected. Because delivery by SHEP coordinators will be the first of the MFG administrations to be implemented, the SHEP coordinators will be provided the KSAT training. They will be tested as described earlier and will be expected to pass before facilitating MFG sessions. They will also receive training in health assessment, home and school outreach, and facilitation of health-related workshops.
Sample and Recruitment of Adult Caregivers and Children
Parents and children interested in participating in the MFG intervention will be able to meet individually with the research team and be provided detailed information about the study; parents and children will be invited to provide written informed consent and assent, respectively.
On the basis of the meetings with the schools and parents and the stakeholder meetings, the initial goal of 300 child-caregiver dyads was scaled back to a more manageable number (i.e., 180) given the overall aim of the study: capacity building and the feasibility of testing whether the MFG delivered by parent peers or the SHEP coordinators will have the greatest impact on addressing child behavioral health disorders in Ghana’s northern region. Because the study is a pilot based on the larger Ugandan study and lack of capacity on the ground in Ghana, a smaller sample was suggested because it is anticipated to yield the desired outcome of MFG feasibility in predominantly poor communities. In total, the study will recruit 180 child-caregiver dyads in all of the three study conditions (N=360). Specifically, we will enroll an average of 60 children per school and 60 of their adult caregivers.
Additionally, the intervention arms will recruit in total eight facilitators: parent peers (N=4) and SHEP coordinators (N=4). School principals from each of the treatment arms will be interviewed to explore their experiences with implementing the MFG. They will also be requested to provide a narrative account of barriers and facilitators encountered.
Inclusion and Exclusion Criteria
The inclusion criteria for child-caregiver dyads include the following: an adult caregiver of a child enrolled in primary school and age 8–13 years willing and able to consent and available for research and intervention activities and a child age 8–13 enrolled in primary school (grades 2–5) screened for oppositional defiant disorder and conduct disorder as described above. The child and caregiver will be invited to the study, and a full baseline assessment will be completed before the start of MFG meetings. The family will be enrolled for the MFG meetings, but all families in the school community can participate in these meetings to decrease stigma and to enhance functioning of all attending families. Children and caregivers can complete a shortened version of the baseline assessment before the MFG meetings. The child and caregiver will be assessed at each time point with the shortened versions of the assessment batteries. If during these assessments the child meets the criteria for a disruptive behavior disorder, both the child and the caregiver will complete the full version of the assessment batteries.
The inclusion criteria for the MFG parent-peer facilitators are the following: caregivers who agree to be trained in providing support to families and SHEP coordinators who work within the basic school settings providing health-related counseling. School principals will be included if they oversee schools where the MFG intervention will be tested.
Any caregiver who lacks an understanding of the study and participant rights will be excluded from the study. The research team will evaluate comprehension by asking caregivers and children to explain their understanding of the study, what their participation entails, and the intervention’s risks and benefits. The research team will also use open-ended questions to ensure that all aspects of the study are understood by potential participants. A consent process checklist will be used to document comprehension. Prospective participants will also be excluded when either the child or the caregiver refuses to participate in the study, as will be parent peers, SHEP coordinators, and school principals who refuse to participate.
Stakeholder Engagement
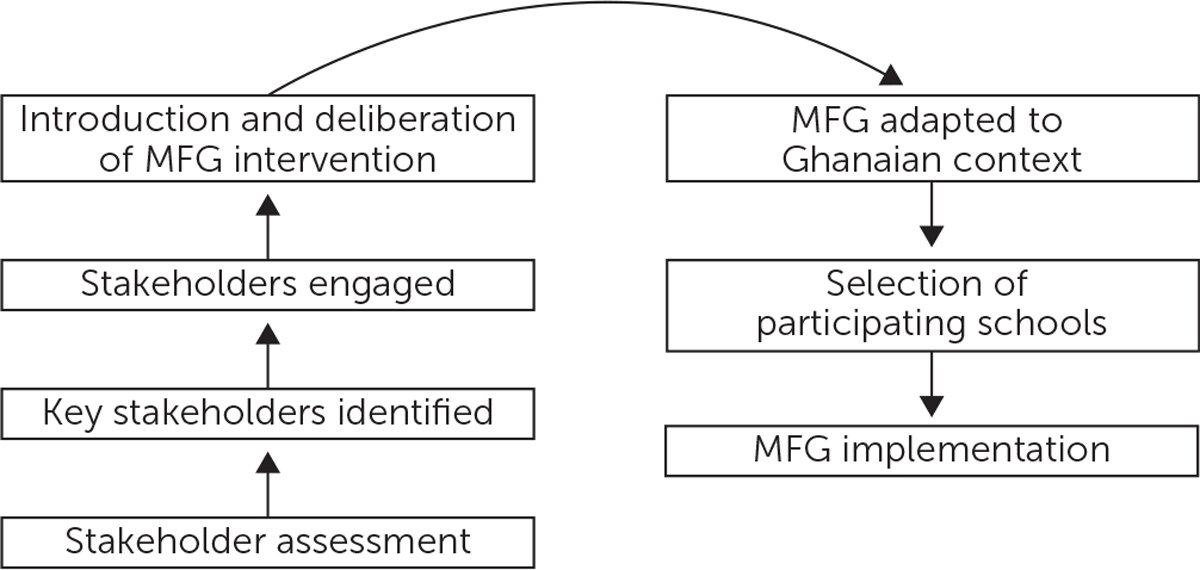
The study processes will engage key partners and stakeholders in consultative meetings. A stakeholder assessment first will be conducted to identify potential stakeholders with vested interest and authority to support the study’s implementation in Ghana. They will include government officials representing the Ministries of Health and Education; other agencies, including the Ghana Mental Health Authority; the public psychiatric hospital; NGOs; and the university community, particularly the schools of public health and social work.
In the engagement session, stakeholders will be expected to provide input on how the MFG can be effectively adapted for implementation in Ghana. We expect inputs regarding the use of SHEP coordinators, rather than CHWs as used in Uganda, to deliver one of the intervention arms of the study. Using SHEP coordinators will be more appropriate in Ghana’s context because they are already embedded in the foundational schools and provide health-related education and guidance to students, unlike the CHWs, who are based at local health centers and may not have the requisite training and background to engage elementary school pupils in a nonhealth facility setting. We also will seek the views of stakeholders on the choice of BasicNeeds–Ghana, an NGO, as an implementation partner. This NGO already works on mental health with schools in the northern region and has experience working with and engaging the SHEP coordinators in the basic schools. The stakeholders’ input will therefore be crucial to the study’s setup in Ghana.
The study team will work closely with school authorities in preselecting/selecting pupils and will brief caregivers and preselected children on the study objectives. Participants will be taken through the consent and assent process and be provided details about the study procedures, and any concerns will be addressed. Figure 2 summarizes the implementation process.
FIGURE 2. The multiple-family group (MFG) intervention implementation process.
Study Challenges: Participants Consenting and Assenting
Some challenges we envisage are related to study participants, stakeholders, and implementation partners. For example, we foresee some communication challenges with participants. Although Tamale has been urbanizing rapidly at a 20% rate per annum (36) and seen a proliferation of cellular phone use (37), not all recruited caregivers may have working cellular phones, presenting a barrier to reach out to them in order to ask for their participation in the MFG processes. Study researchers will have to use alternative communication methods with such caregivers, including sending reminder messages about session periods through the school administration. Another challenge will be that participants may expect that the study will provide solutions to their family’s sociobehavioral and economic difficulties, including providing them with monetary compensation to alleviate their household burdens. Other participants may expect immediate solutions to the behavioral challenges their children face.
RESULTS
This article outlines the processes intended for the adaptation and implementation of the MFG intervention, with the aim of improving child behavioral challenges in Ghana. Our approach consists of initiating an extensive collaborative process by assessing, engaging, and ensuring active participation of stakeholders and to involve and engage the study’s ultimate beneficiaries (38). However, we anticipate some challenges, such as delays in obtaining permission from education authorities and timing of the study within the academic calendar in Ghana.
To obtain permission to conduct the planned interventions, the project team will make early contacts with the Ghana Education Service (GES) authorities and brief them on the project. We anticipate some delays in securing official letters from the northern regional and the Tamale metropolitan directors of GES. This could delay engaging schools within the target location and commencing MFG activities in the selected schools.
The academic term in Ghana spans 12–16 weeks. The first week is usually used for settling the pupils, and the last 2 weeks are for examinations. The remaining weeks will be fewer than is required for full implementation of the MFG intervention. The intervention may therefore extend into the next term of the academic calendar. Moreover, during holidays, some children travel out of their localities, which will prevent completion of the intervention by all pupils and parents. To overcome this hurdle and accommodate other contingencies that may arise, the period for completion will be adjusted.
Another challenge will be high expectations of school authorities with regard to the benefits from participating in the study. School principals will be informed explicitly about these benefits. However, they also likely will expect that participating pupils will be supported in their education and that their school will receive educational, teaching, and learning materials as well as infrastructural improvements. Teachers will also expect monetary compensation for their role in mobilizing and organizing pupils and their caregivers.
NEXT STEPS
The implementation of the MFG intervention in Ghana and its adaptation to local contextual factors have been well received and have raised expectations for systemic changes to the behavior and educational attainment of children in Ghana. The high level of enthusiasm among parents and teachers about the implementation of this project is very assuring. The adaptation of the MFG protocol to the Ghanaian local context and key lessons learned and challenges encountered will lead to discussions among school authorities and parents and caregivers about child disruptive behavior. Such discussions may help manage stigma about these behavioral issues among families and at school and higher system levels, including Ghana’s health and educational systems.
HIGHLIGHTS.
Behavioral health systems that address behavioral health problems among children are underequipped in Ghana.
Evidence-based approaches such as the multiple-family group (MFG) intervention may help address child behavioral challenges.
Current efforts are focused on implementing the MFG intervention at selected schools in Ghana, with MFG being delivered by parents or School Health Education Program coordinators.
Acknowledgments
This study was supported by National Institute of Mental Health (NIMH) award U19 MH-110001, and this article is part of a series of NIMH-funded protocols focused on Global Mental Health Implementation Science. This study was registered March 16, 2017, at ClinicalTrials.gov (ID: NCT03081195). The authors are grateful to Sandow Azuure Stanislaus, B.A., Hannan Legend, B.A., Yaro Francis, B.A., and the staff of BasicNeeds–Ghana. The authors thank pupils of the selected primary schools and their head teachers for participating in the study and the parents and teachers who contributed to the adaptation of the multiple-family group content and delivery in the Ghanaian context. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the National Institutes of Health. At the time of this writing, data collection is under way; once complete, the NIMH will make the data publicly available.
Footnotes
The authors report no financial relationships with commercial interests.
Contributor Information
Emmanuel Asampong, School of Public Health, University of Ghana, Accra
Abdallah Ibrahim, School of Public Health, University of Ghana, Accra
Ozge Sensoy-Bahar, Brown School, Washington University in St. Louis
Kingsley Kumbelim, BasicNeeds, Tamale, Ghana
Peter B. Yaro, BasicNeeds, Tamale, Ghana
Mary M. McKay, Brown School, Washington University in St. Louis
Fred M. Ssewamala, Brown School, Washington University in St. Louis
REFERENCES
- 1.Sankoh O, Sevalie S, Weston M: Mental health in Africa. Lancet Glob Health 2018; 6:e954–e955 [DOI] [PubMed] [Google Scholar]
- 2.Global Health Estimates 2016: Burden of Disease by Cause, Age, Sex, by Country and by Region, 2000–2016. Geneva, World Health Organization, 2018. https://www.who.int/healthinfo/global_burden_disease/estimates/en. Accessed Sept 16, 2020 [Google Scholar]
- 3.World Population Prospects: The 2017 Revision. New York, United Nations Department of Economic and Social Affairs Population Division, 2017. https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html. Accessed Sept 16, 2020 [Google Scholar]
- 4.Next Generation Kenya: Listening to the Voices of Young People. Manchester, United Kingdom, British Council, 2018. https://www.britishcouncil.org/sites/default/files/h198_next_generation_kenya_a4_final_web.pdf [Google Scholar]
- 5.United Nations Development Programme: Sustainable Development Goals. New York, United Nations, 2018. https://unfoundation.org/what-we-do/issues/sustainable-development-goals/?gclid=EAIaIQobChMIspDs9sHu6wIVkojICh361QASEAAYASAAEgLcDvD_BwE. Accessed Sept 16, 2020 [Google Scholar]
- 6.Ogundele MO: Behavioural and emotional disorders in childhood: a brief overview for paediatricians. World J Clin Pediatr 2018; 7:9–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ssewamala FM, Sensoy Bahar O, McKay MM, et al. : Strengthening mental health and research training in sub-Saharan Africa (SMART Africa): Uganda study protocol. Trials 2018; 19:423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ibrahim A, Esena RK, Aikins M, et al. : Assessment of mental distress among prison inmates in Ghana’s correctional system: a cross-sectional study using the Kessler Psychological Distress Scale. Int J Ment Health Syst 2015; 9:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cortina MA. Sodha A. Fazel M. et al. Prevalence of child mental health problems in sub-Saharan Africa: a systematic review. Arch Pediatr Adolesc Med 2012; 166:276–281 [DOI] [PubMed] [Google Scholar]
- 10.Roberts M, Mogan C, Asare JB: An overview of Ghana’s mental health system: results from an assessment using the World Health Organization’s Assessment Instrument for Mental Health Systems (WHO-AIMS). Int J Ment Health Syst 2014; 8:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization, World Psychiatric Association, International Association for Child, Adolescent Psychiatry, Allied Professions: Atlas: Child and Adolescent Mental Health Resources, Global Concerns, Implications for the Future. Geneva, World Health Organization, 2005 [Google Scholar]
- 12.Kieling C, Baker-Henningham H, Belfer M, et al. : Child and adolescent mental health worldwide: evidence for action. Lancet 2011; 378:1515–1525 [DOI] [PubMed] [Google Scholar]
- 13.Burke JD, Loeber R, Birmaher B: Oppositional defiant disorder and conduct disorder: a review of the past 10 years, part II. J Am Acad Child Adolesc Psychiatry 2002; 41:1275–1293 [DOI] [PubMed] [Google Scholar]
- 14.Belfer ML: Child and adolescent mental disorders: the magnitude of the problem across the globe. J Child Psychol Psychiatry 2008; 49:226–236 [DOI] [PubMed] [Google Scholar]
- 15.Ssewamala FM, Nabunya P, Ilic V, et al. : Relationship between family economic resources, psychosocial well-being, and educational preferences of AIDS-orphaned children in southern Uganda: baseline findings. Glob Soc Welf 2015; 2:75–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loeber R, Green SM, Lahey BB, et al. : Findings on disruptive behavior disorders from the first decade of the Developmental Trends Study. Clin Child Fam Psychol Rev 2000; 3:37–60 [DOI] [PubMed] [Google Scholar]
- 17.Loeber R, Burke JD, Lahey BB, et al. : Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry 2000; 39:1468–1484 [DOI] [PubMed] [Google Scholar]
- 18.Hawkins JD, Catalano RF, Miller JY: Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull 1992; 112:64–105 [DOI] [PubMed] [Google Scholar]
- 19.Carlson CL, Tamm L, Hogan AE: The child with oppositional defiant disorder and conduct disorders in the family; in Handbook of Disruptive Behavior Disorders. Edited by Quay HE, Hogan AE. New York, Plenum Press, 1999, pp 337–352 [Google Scholar]
- 20.Lendingham JE: Children and adolescents with oppositional defiant disorder and conduct disorder in the community: experiences at school and with peer; in Handbook of Disruptive Behavior Disorders. Edited by Quay HE, Hogan AE. New York, Plenum Press, 1999 [Google Scholar]
- 21.Bellis MA, Lowey H, Leckenby N, et al. : Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J Public Health (Oxf) 2014; 36:81–91 [DOI] [PubMed] [Google Scholar]
- 22.Washburn JJ, Teplin LA, Voss LS, et al. : Psychiatric disorders among detained youths: a comparison of youths processed in juvenile court and adult criminal court. Psychiatr Serv 2008; 59:965–973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farrington DP: The Twelfth Jack Tizard Memorial Lecture. The development of offending and antisocial behaviour from childhood: key findings from the Cambridge Study in Delinquent Development. J Child Psychol Psychiatry 1995; 36:929–964 [DOI] [PubMed] [Google Scholar]
- 24.Kazdin AE: Conduct Disorders in Childhood and Adolescence, 2nd ed. Thousand Oaks, CA, Sage, 1995 [Google Scholar]
- 25.Apkan MU, Ojinnaka NC, Ekanem E: Behavioral problems among schoolchildren in Nigeria. S Afr J Psychiatry 2010; 16:50–55 [Google Scholar]
- 26.Ashenafi Y, Kebede D, Desta M, et al. : Prevalence of mental and behavioural disorders in Ethiopian children. East Afr Med J 2001; 78:308–311 [PubMed] [Google Scholar]
- 27.Cortina MA, Sodha A, Fazel M, et al. : Prevalence of child mental health problems in sub-Saharan Africa: a systematic review. Arch Pediatr Adolesc Med 2012; 166:276–281 [DOI] [PubMed] [Google Scholar]
- 28.Liang H, Flisher AJ, Chalton DO: Mental and physical health of out of school children in a South African township. Eur Child Adolesc Psychiatry 2002; 11:257–260 [DOI] [PubMed] [Google Scholar]
- 29.Afeti K, Nyarko SH: Prevalence and effect of attention-deficit/hyperactivity disorder on school performance among primary school pupils in the Hohoe Municipality, Ghana. Ann Gen Psychiatry 2017; 16:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Damba OT, Abarike MA, Nabilse CK, et al. : Urban poverty analysis in Tamale. UDS International Journal of Development 2019. https://www.gidrn.com/docs/GIRDN_Report_06.pdf
- 31.Pelham WE Jr, Fabiano GA, Massetti GM: Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol 2005; 34:449–476 [DOI] [PubMed] [Google Scholar]
- 32.Waschbusch DA, Willoughby MT: Parent and teacher ratings on the IOWA Conners Rating Scale. J Psychopathol Behav Assess 2008; 30:180–192 [Google Scholar]
- 33.Fabiano GA, Pelham WE Jr, Waschbusch DA, et al. : A practical measure of impairment: psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. J Clin Child Adolesc Psychol 2006; 35:369–385 [DOI] [PubMed] [Google Scholar]
- 34.McKay M, Block M, Mellins C, et al. : Adapting a family-based HIV prevention program for HIV-infected preadolescents and their families: youth, families and health care providers coming together to address complex needs. Soc Work Ment Health 2007; 5:355–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Costello AB: Getting the most from your analysis. Pract Assess, Res Eval 2009; 12:131–146 [Google Scholar]
- 36.World Health Organization and World Organization of Family Doctors: Integrating Mental Health Into Primary Care: A Global Perspective. Geneva, WHO Press, 2008 [Google Scholar]
- 37.Fuseini I, Kemp J: Characterising urban growth in Tamale, Ghana: an analysis of urban governance response in infrastructure and service provision. Habitat Int 2016; 56:109–123 [Google Scholar]
- 38.Oteng-Ababio M: Crossing conceptual boundaries: re-envisioning coordination and collaboration among women for sustainable livelihoods in Ghana. Local Environ 2018; 23:316–334 [Google Scholar]


