Abstract
Resilience and optimism may not only have main effects on health outcomes, but may also moderate and buffer negative effects of stressors. We examined whether dispositional resilience and optimism moderate the associations between HIV-related stigma in health care settings and health-related outcomes (trust in HIV health care providers and depression symptoms) among women living with HIV (WLHIV). One thousand four hundred five WLHIV in nine US cities completed validated questionnaires for cross-sectional analyses. Higher self-reported experienced and anticipated stigma and lower resilience and optimism were associated with higher depression symptoms and with lower trust in HIV providers. Importantly, resilience moderated the effects of experienced stigma (but not of anticipated stigma): When resilience was high, the association of experienced stigma with higher depression symptoms and lower trust in HIV providers was weaker compared with when resilience was low. Further, significant moderation effects suggested that when optimism was high, experienced and anticipated stigma was both less strongly associated with depression symptoms and with lower trust in one's HIV care providers compared with when optimism was low. Thus, the effects of experienced stigma on depression symptoms and provider trust were moderated by both resilience and optimism, but the effects of anticipated stigma were moderated only by optimism. Our findings suggest that in addition to their main effects, resilience and optimism may function as buffers against the harmful effects of stigma in health care settings. Therefore, optimism and resilience may be valuable intervention targets to reduce depression symptoms or improve trust in providers among populations that experience or anticipate stigma, such as WLHIV.
Keywords: HIV, stigma, resilience, depression, trust, optimism, moderation, provider
Introduction
People living with HIV (PLHIV) may experience stigma associated with their HIV status, which has negative effects on their physical and mental well-being.1–6 When HIV-related stigma manifests in health care settings, PLHIV may find themselves distrusting their providers or avoiding the health care environment, possibly leading to medication nonadherence and missing clinic visits, which can have downstream negative consequences on HIV care outcomes.7,8 While there is some research on the associations among stigma, depression, and trust in one's provider, an understanding of the mechanisms that mediate or moderate these associations is notably missing. This is especially true for the population of women living with HIV (WLHIV), who are less likely than men to adhere to treatment and achieve viral suppression.9
Two personal characteristics that may buffer against harmful structural and interpersonal factors such as stigma are resilience and optimism. Resilience and optimism have been shown to serve as protective factors among people living with other chronic health conditions such as cancer and cardiovascular disease.10,11 In this study, we examined how resilience and optimism may moderate the association of experienced and anticipated stigma in health care settings with depression and trust in health care providers among WLHIV enrolled in the Women's Interagency HIV Study (WIHS),12 a multi-site cohort study that is now known as The Multicenter AIDS Cohort (MACS)-WIHS Combined Cohort Study (MWCCS).
Studies suggest that HIV-related stigma is associated with suboptimal HIV health behaviors and outcomes, including missed visits, lower treatment self-efficacy,13 nonadherence to treatment, and reductions in viral load suppression rates.2–5 Stigma occurs when a group has an attribute that is perceived as discrediting in society.14 This attribute devalues individuals belonging to the group. HIV-related stigma that occurs in health care settings is particularly harmful, since these environments should be stigma-free and propatient regardless of patient circumstances.15 Stigma within health care settings can exacerbate negative physical and mental health outcomes,16 and eliminating stigma in clinic settings is a shared goal of public health and medicine.17 Further, many WLHIV may experience intersectional stigma related to having multiple stigmatized traits, such as living with HIV, being a woman, living in poverty, and identifying as a person of color, and these experiences of stigma can also be associated with poor physical and mental health.18
Individual characteristics may buffer against the negative effects of experiencing or anticipating stigma from others.19 PLHIV with such protective characteristics may be able to resist the negative implications of stigma from others in terms of how they feel about themselves and about the health care system in general. Coping theories posit that the effect of stressful situations on emotional well-being depends on how individuals appraise the situation and which strategies they use to cope with the situation.20 Previous literature has applied the stress and coping framework to conceptualize individual differences in response to stigma and discrimination21 and found that coping resources such as optimism can buffer the negative effects of stigma.22
Coping resources include situational factors (e.g., social support) and individual difference factors. Two individual difference factors that may buffer against harmful structural and interpersonal factors such as stigma are resilience and optimism. Resilience is “adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress,” or “bouncing back” from challenging or unanticipated circumstances.23 Limited research among PLHIV suggests that resilience is associated with better health outcomes, improved quality of life, and successful aging.24,25 Resilience theories suggest that while resilience can have a main effect on the psychosocial well-being and adjustment, perhaps the most important contribution of resilience is its ability to attenuate (i.e., moderate) the negative effects of negative life events and stressors on psychosocial functioning.23 Therefore, we examined whether resilience could buffer the negative effects of social stigma on depression symptoms and health care provider trust.
Optimism encompasses a sense of hopefulness, a belief that situations will sort themselves and produce positive outcomes.26 There is some research suggesting that optimism is associated with reduced anxiety and depression among PLHIV, which can then be linked to improved HIV care outcomes.27 Theoretically, optimism may have main effects on health outcomes as well as moderating the effects of stress and adversity, and there is research providing support for both of these mechanisms.26,28
In the present study, we examined how resilience and optimism moderate the associations that stigma experienced and anticipated in health care settings has with depression symptoms and with trust in health care providers among WLHIV. Depression is particularly prevalent among WLHIV29 and depression symptoms increase the likelihood of failure across the HIV continuum of care.30 Therefore, understanding the interplay between stigma and depression symptoms could be important. Our other outcome, trust in HIV care providers, is at the foundation of quality health care. HIV research suggests that when clinical providers are perceived as trustworthy, their patients' outcomes are better across the continuum of care.31–33 Since WLHIV in the United States disproportionately identify as Black or Latina, and racism and the resulting provider mistrust among people of color also fuel health disparities,34 examining determinants of provider trust among WLHIV is warranted and findings could produce actionable insights.35
According to recent theories, medical mistrust is a rational response to structural and interpersonal stigma experiences with the aim of preventing future mistreatment.36 We argue that stigma experienced and anticipated in health care settings may have important effects on provider trust and understanding factors that may buffer these effects is important both theoretically and practically.
Methods
Participants and procedures
Participants included 1405 WLHIV from the WIHS, a multi-site cohort study12 that is now known as the MWCCS. Participants at all nine sites of the WIHS including New York (Bronx and Brooklyn), Washington DC, Chicago, San Francisco, Georgia (Emory), Alabama and Mississippi (UAB-MS), Florida (Miami), and North Carolina (UNC) completed measures related to patient/health care provider relationships for this study. These data were merged with the data collected for the larger WIHS. The study was approved by the Institutional Review Board at each site.
Measures
Experienced HIV-related stigma in health care settings
We assessed experienced HIV-related stigma in health care settings using a 6-item measure adapted from the experienced stigma subscale measuring HIV-related stigma among health facility staff.37 (e.g., “Healthcare workers talked badly about people living with HIV”) are rated on a 5-point Likert-type scale (1 = Never, 5 = Almost always). Previous research suggests that this adapted measure shows good internal reliability and validity (significant associations with HIV-related health outcomes).7 In this study, Cronbach's alpha coefficient was 0.75.
Anticipated HIV-related stigma in health care settings
The 3-item anticipated HIV stigma in health care settings subscale of the HIV Stigma Framework Scale38 was used. A sample item is “Healthcare workers will avoid touching me.” Responses were recorded using a 5-point Likert-type scale (1 = Very unlikely, 5 = Very likely). In the current study, Cronbach's alpha reliability coefficient was 0.89.
Trust in HIV care providers
We assessed trust in one's HIV care providers using the validated 8-item Safran Physician Trust Subscale39 (e.g., “Your HIV care providers care as much as you do about your health”) rated on a 5-point Likert-type scale ranging from 1 (Strongly disagree) to 5 (Strongly agree). In this study, Cronbach's alpha reliability coefficient was 0.82.
Depression symptoms
The 20-item validated Center for Epidemiological Studies Depression (CES-D) scale (e.g., “I was bothered by things that usually don't bother me”) was used to assess depression symptoms.40 Response options include rarely (<1 day), some (1–2 days), occasionally (3–4 days), and most (5–7 days). Higher scores indicate the presence of greater depressive symptomatology.
Resilience
Dispositional resilience was assessed with the 10-item version of the Connor–Davidson Resilience Scale (CD-RISC).41,42 Items (e.g., “I am able to adapt when changes occur”) are rated on a 5-point Likert-type scale (1 = not true at all, 5 = true nearly all the time), with higher scores indicating higher resilience. In the current study, Cronbach's alpha reliability coefficient was 0.91.
Optimism
We assessed optimism using the 6-item Life-Outcomes Orientation Test-Revised.43,44 Items (e.g., “In uncertain times, I usually expect the best”) are rated on a 5-point Likert-type scale (1 = I disagree a lot, 5 = I agree a lot) with higher scores indicating higher optimism. In this study, Cronbach's alpha reliability coefficient was 0.66.
Statistical analyses
In separate analyses, we examined whether resilience and optimism moderate the effect of experienced or anticipated stigma on depression symptoms and on provider trust. For this, we conducted moderation analyses using the PROCESS macro for SPSS.45 Associations are reported as regression coefficients with 95% percentile confidence intervals (CIs). For statistically significant interaction effects, we examined simple slopes (regression coefficients for the independent variable) at 1 standard deviation (SD) above and below the mean of each moderator. All analyses were cross-sectional, adjusting for age, level of education, income, patient race, provider race, and illicit drug use.
Results
Descriptive statistics of the sample are presented in Table 1. Results of the regression analyses (adjusted for covariates) are presented in Table 2.
Table 1.
Descriptive Statistics of the Sample (N = 1405)
| Variable | n | % |
|---|---|---|
| Patient race | ||
| White | 204 | 14.5 |
| African American | 1060 | 75.4 |
| Other | 141 | 10.0 |
| HIV care provider race | ||
| White | 793 | 56.4 |
| African American | 243 | 17.3 |
| Other | 346 | 24.6 |
| Education | ||
| No school | 4 | 0.3 |
| Grades 1–6 | 21 | 1.5 |
| Grades 7–11 | 424 | 30.2 |
| Completed high school | 452 | 32.2 |
| Some college | 393 | 28.0 |
| Completed 4-year college | 79 | 5.6 |
| Attended/completed graduate school | 31 | 2.2 |
| Income | ||
| ≤$6000 | 153 | 10.9 |
| $6001–12,000 | 505 | 35.9 |
| $12,001–18,000 | 205 | 14.6 |
| $18,001–24,000 | 116 | 8.3 |
| $24,001–30,000 | 78 | 5.6 |
| $30,001–36,000 | 71 | 5.1 |
| $36,001–75,000 | 152 | 10.5 |
| ≥$75,000 | 63 | 4.5 |
| Illicit drug use in the last 6 months | ||
| Yes | 347 | 24.7 |
| No | 1057 | 75.3 |
| Mean (SD) | Range | |
|---|---|---|
| Age | 51.24 (9.09) | 28–82 |
| Experienced HIV stigma | 1.17 (0.41) | 1–5 |
| Anticipated HIV stigma | 1.47 (0.81) | 1–5 |
| Depression symptoms | 12.17 (11.57) | 0–54 |
| Trust in HIV providers | 4.24 (0.65) | 1–5 |
| Resilience | 4.02 (0.73) | 1–5 |
| Optimism | 3.85 (0.75) | 1–5 |
SD, standard deviation.
Table 2.
Coefficients and Confidence Intervals of Moderation Analyses
| Outcome: DEP | B (SE) | 95% CI |
Outcome: TCP | B (SE) | 95% CI |
||
|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | ||||
| ES | 3.78 (0.65) | 2.50 | 5.07 | ES | −0.26 (0.04) | −0.34 | −0.18 |
| RES | −7.09 (0.37) | −7.83 | −6.36 | RES | 0.28 (0.02) | 0.24 | 0.33 |
| ES × RES | −1.94 (0.72) | −3.36 | −0.53 | ES × RES | 0.14 (0.05) | 0.05 | 0.23 |
| AS | 1.50 (0.34) | 0.83 | 2.16 | AS | −0.18 (0.02) | −0.22 | −0.14 |
| RES | −7.22 (0.38) | −7.97 | −6.48 | RES | 0.27 (0.02) | 0.23 | 0.32 |
| AS × RES | −0.10 (0.40) | −0.88 | 0.68 | AS × RES | 0.04 (0.02) | −0.01 | 0.09 |
| ES | 3.10 (0.68) | 1.77 | 4.43 | ES | −0.23 (0.04) | −0.31 | −0.14 |
| OPT | −6.94 (0.37) | −7.66 | −6.22 | OPT | 0.19 (0.02) | 0.14 | 0.23 |
| ES × OPT | −3.30 (0.89) | −5.05 | −1.55 | ES × OPT | 0.26 (0.06) | 0.14 | 0.37 |
| AS | 1.31 (0.34) | 0.64 | 1.98 | AS | −0.18 (0.02) | −0.23 | −0.14 |
| OPT | −7.00 (0.37) | −7.73 | −6.27 | OPT | 0.18 (0.02) | 0.14 | 0.23 |
| AS × OPT | −1.00 (0.47) | −1.92 | −0.07 | AS × OPT | 0.08 (0.03) | 0.02 | 0.14 |
Level of education, income, patient race, provider race, and illicit drug use were used as covariates.
AS, anticipated stigma; CI, confidence interval; DEP, depression symptoms; ES, experienced stigma; OPT, optimism; RES, resilience; SE, standard error; TCP, trust in HIV care providers.
Experienced HIV stigma in health care settings and resilience
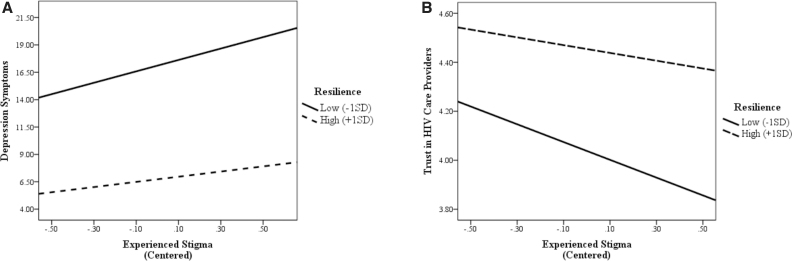
First, we examined the association that experienced stigma, resilience, and their interaction have with depression symptoms (adjusting for covariates). Both main effects were significant (suggesting higher experienced stigma and lower resilience are associated with higher depression symptom severity). Importantly, the interaction term was also significant [B = −1.94, standard error (SE) = 0.72, p = 0.007, CI (−3.36 to −0.53)]. Simple slope analyses (again adjusting for covariates) suggested that experienced stigma has a stronger positive association with depression symptoms at low (−1 SD) levels of resilience [B = 5.21, SE = 0.80, p = 0.000, CI (3.63 to 6.78)], compared with high (+1 SD) levels of resilience [B = 2.36, SE = 0.88, p = 0.007, CI (0.64 to 4.08); see Fig. 1A]. That is, in addition to having a main effect on lower depression symptoms, resilience also moderates the association between experienced stigma and depression symptoms.
FIG. 1.
(A, B) Interaction between resilience and experienced stigma in health care settings on depressive symptoms and trust in HIV care providers.
Similarly, we examined the association that experienced stigma and resilience have with trust in HIV care providers. Both main effects were significant (Table 2, right-hand side). The interaction effect between experienced stigma and resilience was again significant [B = 0.14, SE = 0.05, p = 0.003, CI (0.05 to 0.23)]. Simple slope analyses suggested that experienced stigma has a stronger negative association with trust in HIV care providers at low levels of resilience [B = −0.36, SE = 0.05, p = 0.000, CI (−0.46 to −0.26)] compared with high levels of resilience [B = −0.15, SE = 0.05, p = 0.003, CI (−0.26 to −0.05); see Fig. 1B].
Anticipated HIV stigma in health care settings and resilience
Next, we assessed the association of anticipated stigma and resilience with depression symptoms. The interaction term between anticipated stigma and resilience was not significant [B = −0.10, SE = 0.40, p = 0.797, CI (−0.88 to 0.68)]. Similarly, the interaction between anticipated stigma and resilience was not significant when trust in HIV care providers was the outcome [B = 0.04, SE = 0.02, p = 0.104, CI (−0.01 to 0.09)].
Experienced HIV stigma in health care settings and optimism
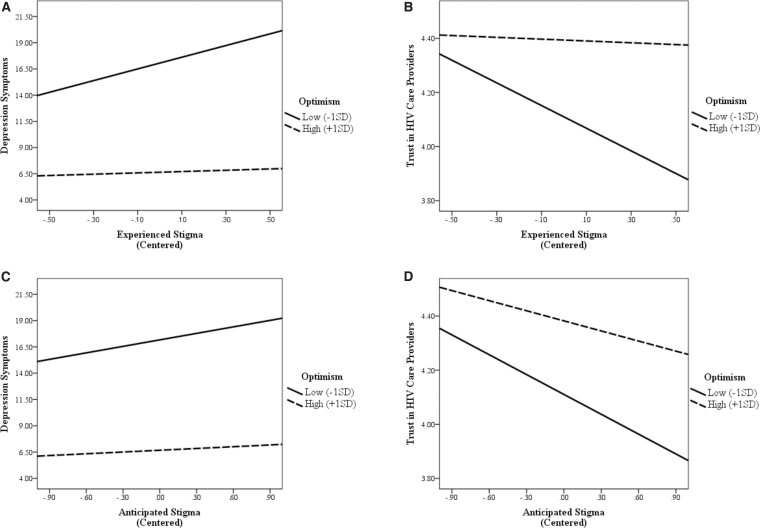
We examined whether the association between experienced stigma and depression symptoms was moderated by optimism. Results indicated a significant interaction effect between experienced stigma and optimism [B = −3.30, SE = 0.89, p = 0.000, CI (−5.05 to −1.55)]. Simple slope analyses suggested that at low levels of optimism, experienced stigma is significantly associated with depression symptoms [B = 5.57, SE = 0.82, p = 0.000, CI (3.96 to 7.19)], but not at high levels of optimism [B = 0.62, SE = 1.06, p = 0.557, CI (−1.46 to 2.71); see Fig. 2A]. Similarly, the association between experienced stigma and trust in HIV care providers was significantly moderated by optimism [B = 0.26, SE = 0.06, p = 0.000, CI (0.14 to 0.37)].
FIG. 2.
(A–D) Interaction between optimism and experienced and anticipated stigma in health care settings on depressive symptoms and trust in HIV.
Simple slope analyses suggested that at low levels of optimism, experienced stigma is significantly associated with lower trust in HIV care providers [B = −0.42, SE = 0.05, p = 0.000, CI (−0.52 to −0.31)], but not at high levels of optimism [B = −0.03, SE = 0.07, p = 0.620, CI (−0.16 to 0.10); see Fig. 2B].
Anticipated HIV stigma in health care settings and optimism
Finally, we assessed the association that anticipated stigma and optimism have with depression symptoms. This analysis indicated a significant interaction effect between anticipated stigma and optimism [B = −1.00, SE = 0.47, p = 0.034, CI (−1.92 to −0.07)]. Simple slope analyses suggested that anticipated stigma is significantly associated with depression symptoms at low levels of optimism [B = 2.06, SE = 0.45, p = 0.000, CI (1.16 to 2.95)], but not at high levels of optimism [B = 0.56, SE = 0.52, p = 0.287, CI (−0.47 to 1.59); see Fig. 2C]. Similarly, the interaction effect between anticipated stigma and optimism on trust in HIV providers was significant [B = 0.08, SE = 0.03, p = 0.006, CI (0.02 to 0.14)].
Simple slope analyses suggested that the association between anticipated stigma and trust in HIV care providers was stronger at low levels of optimism [B = −0.24, SE = 0.03, p = 0.000, CI (−0.30 to −0.19)] compared with high levels of optimism [B = −0.12, SE = 0.03, p = 0.000, CI (−0.19 to −0.06); see Fig. 2D]. All coefficients and CIs for main and interaction (moderation) effects are presented in Table 2.
Discussion
Our results suggest that higher self-reported levels of experienced stigma and anticipated stigma in health care settings are associated with higher depression symptoms as well as with lower levels of trust in HIV providers. We also found buffering effects of resilience and optimism in many of these associations. Higher levels of experienced stigma were associated with higher levels of depression symptoms and lower levels of trust in providers at both high and low levels of resilience. However, significant interaction effects and follow-up simple slope analyses indicated that when resilience was low, the association between experienced stigma and depression symptoms was stronger compared with the association when high levels of resilience were reported. Similarly, when resilience was low, the association between experienced stigma and lack of trust in one's providers was stronger compared with the association at high levels of resilience.
Our analyses suggest that resilience not only has a main effect on (lower) depression symptoms and (higher) provider trust, but may also function as a buffer against the harmful effects of stigma experienced in health care settings. In contrast, we did not observe a buffering effect of resilience when examining the association between anticipated stigma and depression symptoms or trust in care providers.
We found similar results when using optimism as a potential moderator of experienced stigma. When optimism was low, experienced stigma was significantly associated with depression symptoms and with trust in one's HIV care providers. However, when optimism was high, not only was depression lower and trust higher, the association that experienced stigma has with depression symptoms and provider trust was no longer significant as well.
The associations between anticipated HIV stigma in health care settings and both outcomes were also significantly moderated by optimism. Anticipated stigma was associated with depression symptoms when optimism was low but not when optimism was high. Further, when the level of optimism was low, the negative effect of anticipated stigma on trust in one's provider was significantly stronger than when compared with higher levels of optimism.
Thus, the effect of anticipated stigma was moderated by optimism, but not by resilience. However, for experienced stigma, the moderating effects of resilience were generally stronger compared with the moderating effects of optimism. It is possible that optimism, which by definition is a future-oriented construct,22 interacts more strongly with anticipated stigma (also a future-oriented construct). It is also possible that optimism shows a delayed effect (which we could not capture in this study), whereas resilience has a more immediate effect on outcomes (since it helps to cope with stressors that have already happened).
Our study had several limitations. The data were cross-sectional, limiting our ability to infer causality. Self-report measures were used for most constructs, which may introduce response bias. We only measured individual resilience, whereas the need to assess interpersonal and community resilience for PLHIV has been identified.46 A strong focus on individual resilience may be criticized for downplaying the need for social and structural change.47 The sample consisted of women enrolled in an observational cohort study. Therefore, results may not generalize to men or people with HIV not in a cohort study. Even though the WIHS was initially established to be representative of WLHIV in the United States with respect to overall demographics, participants are now older than the general population of WLHIV in the United States. Another limitation is that no data were available on how many participants in the cohort declined to participate in our substudy.
Despite these limitations, our findings suggest that optimism and resilience may be valuable change objectives to target within interventions that aim to reduce depression symptoms or improve trust in providers, and by extension improve engagement in the health care system, among populations that experience or anticipate stigma, such as WLHIV. Results suggest that WLHIV who are low in resilience or optimism and high in experienced or anticipated stigma are especially vulnerable and may benefit from such interventions, which should also address structural factors contributing to worse outcomes for WLHIV.48
Acknowledgments
Data in this article were collected by the WIHS, now the MWCCS. MWCCS (principal investigators): Atlanta CRS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-HL146241; Baltimore CRS (Todd Brown and Joseph Margolick), U01-HL146201; Bronx CRS (Kathryn Anastos, David Hanna, and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01-HL146202; Data Analysis and Coordination Center (Gypsyamber D'Souza, Stephen Gange and Elizabeth Topper), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Chicago-Northwestern CRS (Steven Wolinsky), U01-HL146240; Northern California CRS (Bradley Aouizerat, Jennifer Price, and Phyllis Tien), U01-HL146242; Los Angeles CRS (Roger Detels and Matthew Mimiaga), U01-HL146333; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-HL146203; Pittsburgh CRS (Jeremy Martinson and Charles Rinaldo), U01-HL146208; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom, and Deborah Konkle-Parker), U01-HL146192; UNC CRS (Adaora Adimora and Michelle Floris-Moore), U01-HL146194.
The authors gratefully acknowledge the contributions of the study participants and dedication of the staff at the MWCCS sites.
Author Disclosure Statement
The authors have no conflicts of interest.
Funding Information
The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional cofunding from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD), the National Institute on Aging (NIA), the National Institute of Dental & Craniofacial Research (NIDCR), the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Neurological Disorders and Stroke (NINDS), the National Institute of Mental Health (NIMH), the National Institute on Drug Abuse (NIDA), the National Institute of Nursing Research (NINR), the National Cancer Institute (NCI), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and Other Communication Disorders (NIDCD), the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the National Institute on Minority Health and Health Disparities (NIMHD), and in coordination and alignment with the research priorities of the National Institutes of Health (NIH), Office of AIDS Research (OAR).
MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR003098 (JHU ICTR), UL1-TR001881 (UCLA CTSI), P30-AI-050409 (Atlanta CFAR), P30-AI-073961 (Miami CFAR), P30-AI-050410 (UNC CFAR), P30-AI-027767 (UAB CFAR), and P30-MH-116867 (Miami CHARM). Funding was also provided by the NIMH, R01MH104114 and the NIDA, R03DA052180.
References
- 1. Herek GM, Saha S, Burack J. Stigma and psychological distress in people with HIV/AIDS. Basic Appl Soc Psych 2013;35(1):41–54. [Google Scholar]
- 2. Yigit I, Bayramoglu Y, Weiser SD, et al. Changes in internalized stigma and HIV health outcomes in individuals new to HIV care: The mediating roles of depression and treatment self-efficacy. AIDS Patient Care STDS 2020;34(11):491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: I mediating role of depression. AIDS 2019;33(3):571–576; doi: 10.1097/QAD.0000000000002071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rice WS, Crockett KB, Mugavero MJ, et al. Association between internalized HIV-related stigma and HIV care visit adherence. J Acquir Immune Defic Syndr 2017;76(5):482–487; doi: 10.1097/qai.0000000000001543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Christopoulos KA, Neilands TB, Hartogensis W, et al. Internalized HIV stigma is associated with concurrent viremia and poor retention in a cohort of US patients in HIV care. J Acquir Immune Defic Syndr 2019;82(2):116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: Evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med 2012;156(11):817–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kay ES, Rice WS, Crockett KB, et al. Experienced HIV-related stigma in health care and community settings: Mediated associations with psychosocial and health outcomes. J Acquir Immune Defic Syndr 2018;77(3):257–263; doi: 10.1097/qai.0000000000001590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Turan B, Rogers AJ, Rice WS, et al. Association between perceived discrimination in healthcare settings and HIV medication adherence: Mediating psychosocial mechanisms. AIDS Behav 2017;21:3431–3439; doi: 10.1007/s10461-017-1957-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crepaz N, Tang T, Marks G, et al. Viral suppression patterns among persons in the United States with diagnosed HIV infection in 2014. Ann Intern Med 2017;167(6):446–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Seiler A, Jenewein J. Resilience in cancer patients. Front Psychiatry 2019;10:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Park JW, Mealy R, Saldanha IJ, et al. Multilevel resilience resources and cardiovascular disease in the United States: A systematic review and meta-analysis. Health Psychol 2022;41(4):278–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Adimora AA, Ramirez C, Benning L, et al. Cohort profile: The Women's Interagency HIV Study (WIHS). Int J Epidemiol 2018;47(2):393i–394i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Seghatol-Eslami VC, Dark HE, Raper JL, et al. Interpersonal and intrapersonal factors as parallel independent mediators in the association between internalized HIV stigma and ART adherence. J Acquir Immune Defic Syndr 2017;74:e18–e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goffman E. Stigma; Notes on the Management of Spoiled Identity. Prentice-Hall: Englewood Cliffs, NJ; 1963. [Google Scholar]
- 15. Budhwani H, De P. Perceived stigma in health care settings and the physical and mental health of people of color in the United States. Health Equity 2019;3(1):73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kay ES, Batey DS, Mugavero MJ. The HIV treatment cascade and care continuum: Updates, goals, and recommendations for the future. AIDS Res Ther 2016;13(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Batey DS, Whitfield S, Mulla M, et al. Adaptation and implementation of an intervention to reduce HIV-related stigma among healthcare workers in the United States: Piloting of the FRESH workshop. AIDS Patient Care STDS 2016;30(11):519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rice WS, Logie CH, Napoles TM, et al. Perceptions of intersectional stigma among diverse women living with HIV in the United States. Soc Sci Med 2018;208:9–17; doi: 10.1016/j.socscimed.2018.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Turan B, Crockett KB, Buyukcan-Tetik A, et al. Buffering internalization of HIV stigma: Implications for treatment adherence and depression. J Acquir Immune Defic Syndr 2019;80(3):284–291; doi: 10.1097/qai.0000000000001915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Folkman S, Lazarus RS. The relationship between coping and emotion: Implications for theory and research. Soc Sci Med 1988;26(3):309–317. [DOI] [PubMed] [Google Scholar]
- 21. Major B, Quinton WJ, McCoy SK. Antecedents and Consequences of Attributions to Discrimination: Theoretical and Empirical Advances. In: Advances in Experimental Social Psychology. (Zanna MP. ed.) Academic Press; 2002; Vol. 34, pp. 251–330. [Google Scholar]
- 22. Kaiser CR, Major B, McCoy SK. Expectations about the future and the emotional consequences of perceiving prejudice. Pers Soc Psychol Bull 2004;30(2):173–184. [DOI] [PubMed] [Google Scholar]
- 23. Garmezy N, Masten AS, Tellegen A. The study of stress and competence in children: A building block for developmental psychopathology. Child Dev 1984;55:97–111. [PubMed] [Google Scholar]
- 24. Fazeli PL, Hopkins CN, Wells A, et al. Examining the acceptability of a resilience building intervention among adults aging with HIV. J Assoc Nurses AIDS Care 2022;33(2):155–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fletcher FE, Sherwood NR, Rice WS, et al. Resilience and HIV treatment outcomes among women living with HIV in the United States: A mixed-methods analysis. AIDS Patient Care STDS 2020;34(8):356–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kleiman EM, Chiara AM, Liu RT, et al. Optimism and well-being: A prospective multi-method and multi-dimensional examination of optimism as a resilience factor following the occurrence of stressful life events. Cogn Emot 2017;31(2):269–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Willie TC, Overstreet NM, Peasant C, et al. Anxiety and depressive symptoms among people living with HIV and childhood sexual abuse: The role of shame and posttraumatic growth. AIDS Behav 2016;20(8):1609–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Alloy LB, Clements CM. Illusion of control: Invulnerability to negative affect and depressive symptoms after laboratory and natural stressors. J Abnorm Psychol 1992;101(2):234. [DOI] [PubMed] [Google Scholar]
- 29. Nanni MG, Caruso R, Mitchell AJ, et al. Depression in HIV infected patients: A review. Curr Psychiatry Rep 2015;17(1):1–11. [DOI] [PubMed] [Google Scholar]
- 30. Koenig LJ, O'Leary A. Improving health outcomes for women with HIThe potential impact of addressing internalized stigma and depression. AIDS 2019;33(3):577–579. [DOI] [PubMed] [Google Scholar]
- 31. Graham JL, Giordano TP, Grimes RM, et al. Influence of trust on HIV diagnosis and care practices: A literature review. J Int Assoc Physicians AIDS Care (Chic) 2010;9(6):346–352. [DOI] [PubMed] [Google Scholar]
- 32. Dale SK, Bogart LM, Wagner GJ, et al. Medical mistrust is related to lower longitudinal medication adherence among African-American males with HIV. J Health Psychol 2016;21(7):1311–1321; doi: 10.1177/1359105314551950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Thrasher AD, Earp JAL, Golin CE, et al. Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. J Acquir Immune Defic Syndr 2008;49(1):84–93; doi: 10.1097/QAI.0b013e3181845589. [DOI] [PubMed] [Google Scholar]
- 34. Saha S, Jacobs EA, Moore RD, et al. Trust in physicians and racial disparities in HIV care. AIDS Patient Care STDS 2010;24(7):415–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Budhwani H, Yigit I, Ofotokun I, et al. Examining the relationships between experienced and anticipated stigma in health care settings, patient–provider race concordance, and trust in providers among women living with HIV. AIDS Patient Care STDS 2021;35(11):441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bogart LM, Takada S, Cunningham WE. Medical mistrust, discrimination, and the domestic HIV epidemic. In: HIV in US Communities of Color. (Ojikutu BO, Stone VE. eds.) Springer, Cham, 2021; pp. 207–231. [Google Scholar]
- 37. Nyblade L, Jain A, Benkirane M, et al. A brief, standardized tool for measuring HIV-related stigma among health facility staff: Results of field testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. J Int AIDS Soc 2013;16(3 Suppl 2):18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Earnshaw VA, Smith LR, Chaudoir SR, et al. HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS Behav 2013;17(5):1785–1795; doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Safran DG, Kosinski M, Tarlov AR, et al. The primary care assessment survey: Tests of data quality and measurement performance. Med Care 1998;36(5):728–739. [DOI] [PubMed] [Google Scholar]
- 40. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385–401. [Google Scholar]
- 41. Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor–Davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress 2007;20(6):1019–1028. [DOI] [PubMed] [Google Scholar]
- 42. Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress Anxiety 2003;18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 43. Herzberg PY, Glaesmer H, Hoyer J. Separating optimism and pessimism: A robust psychometric analysis of the revised Life Orientation Test (LOT-R). Psychol Assess 2006;18(4):433. [DOI] [PubMed] [Google Scholar]
- 44. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67(6):1063–1078. [DOI] [PubMed] [Google Scholar]
- 45. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications: New York; 2017. [Google Scholar]
- 46. Dulin AJ, Dale SK, Earnshaw VA, et al. Resilience and HIV: A review of the definition and study of resilience. AIDS Care 2018;30(Suppl 5):S6–S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gill R, Orgad S. The amazing bounce-backable woman: Resilience and the psychological turn in neoliberalism. Sociol Res Online 2018;23(2):477–495. [Google Scholar]
- 48. Whittle HJ, Leddy AM, Shieh J, et al. Precarity and health: Theorizing the intersection of multiple material-need insecurities, stigma, and illness among women in the United States. Soc Sci Med 2020;245:112683. [DOI] [PMC free article] [PubMed] [Google Scholar]