Abstract
Aim
To examine the incidence of intrapartum-related neonatal encephalopathy, and neonatal mortality and neurodevelopmental outcomes associated with it in low-income and middle-income countries.
Methods
Reports were included when neonatal encephalopathy diagnosed clinically within 24 hours of birth in term or near-term infants born after intrapartum hypoxia-ischaemia defined as any of the following: (1) pH≤7.1 or base excess ≤−12 or lactate ≥6, (2) Apgar score ≤5 at 5 or 10 min, (3) continuing resuscitation at 5 or 10 min or (4) no cry from baby at 5 or 10 min. Peer-reviewed articles were searched from Ovid MEDLINE, Cochrane, Web of Science and WHO Global Index Medicus with date limits 1 November 2009 to 17 November 2021. Risk of bias was assessed using modified Newcastle Ottawa Scale. Inverse variance of heterogenicity was used for meta-analyses.
Results
There were 53 reports from 51 studies presenting data on 4181 children with intrapartum-related neonatal encephalopathy included in the review. Only five studies had data on incidence, which ranged from 1.5 to 20.3 per 1000 live births. Neonatal mortality was examined in 45 studies and in total 636 of the 3307 (19.2%) infants died. Combined outcome of death or moderate to severe neurodevelopmental disability was reported in 19 studies and occurred in 712 out of 1595 children (44.6%) with follow-up 1 to 3.5 years.
Conclusion
Though there has been progress in some regions, incidence, case mortality and morbidity in intrapartum-related neonatal encephalopathy has been static in the last 10 years.
PROSPERO registration number
CRD42020177928.
Keywords: epidemiology, paediatrics, indices of health and disease and standardisation of rates, systematic review
WHAT IS ALREADY KNOWN ON THIS TOPIC
Intrapartum-related neonatal encephalopathy is one of the leading causes of newborn death and disability in low-income and middle-income countries.
WHAT THIS STUDY ADDS
Although mortality and morbidity associated with intrapartum-related neonatal encephalopathy have been at large static in over the last 10 years, some hospitals in middle-income countries report outcomes similar to high-income settings.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Given the scarcity of population-based data, more research on the epidemiology of intrapartum-related neonatal encephalopathy is needed to inform policy makers on progress at national and subnational levels, especially focusing on the poorest children.
Background
Neonatal encephalopathy (NE) is a syndrome of disturbed neurological function presenting during the first days of life.1 Hallmarks of NE include decreased level of consciousness or seizures, difficulty with initiating and maintaining respiration, and altered tone and reflexes.1 Intrapartum-related hypoxia-ischaemia is the most common cause of NE and one of the top three causes of neonatal death globally.2 Nearly half of the survivors of intrapartum-related NE risk neurodevelopmental disability including cerebral palsy (CP), intellectual impairment, deafness and blindness.2 3 These risks are related to the severity of encephalopathy commonly graded as mild, moderate or severe, or grade I, II, III, respectively, based on early neurological examination.4 Intrapartum-related NE is a term primarily used in reference to term and near-term infants.1
The most recent systematic review and meta-analysis from 20133 estimated 1.15 million cases of intrapartum-related NE globally per year resulting in 287 000 neonatal deaths and 233 000 moderate or severe disabilities: 96% occurred in low-income and middle-income countries (LMICs).3 Given global increase in facility deliveries5 and improved neonatal resuscitation6 during the decade that has elapsed since, the situation has likely changed. Without data, though, the task of the policymakers becomes near impossible. Reducing the burden of intrapartum-related NE is one of the key factors for achieving the Every Newborn Action Plan.7 We, therefore, conducted a systematic review of intrapartum-related NE in LMICs with the objective of quantifying the following parameters: (1) incidence, (2) neonatal mortality and (3) neurodevelopmental outcomes at follow-up of ≥1 year.
Methods
Preferred Reporting Items for Systematic Reviews and Meta-Analyses 20208 guidelines were followed and the study protocol was registered beforehand in PROSPERO database (CRD42020177928).
Eligibility criteria
Types of reports
All article types (observational and trial based) providing information on incidence, neonatal mortality or childhood neurodevelopmental outcomes of NE in humans were considered for inclusion. Qualitative studies, reviews, protocols, conference abstracts, editorials and opinion pieces were excluded.
Additional study characteristics
Only data from LMICs classified by World Bank country and lending groups at the median year of data collection were considered.9 Only reports published after 1 November 2009 were included as this was the last date searched by Lee et al in their previous review3 and as changes in peripartum care reduce the relevance of older studies.5 6 No language restrictions were applied.
Types of study participants
Neonatal encephalopathy
NE was defined clinically as disturbed neurological function diagnosed using criteria proposed by Sarnat and Sarnat or another validated scale within 24 hours of birth.4 A cut-off of 24 hours was selected to ensure early onset of symptoms commensurate with a hypoxic-ischaemic origin while acknowledging that the symptoms evolve over the first week of life.4 Due to limited availability in LMICs, electroencephalographic confirmation and neuroimaging were not mandated.
Relation to intrapartum events
Evidence of intrapartum hypoxia-ischaemia was required for inclusion to distinguish from other similar clinical phenotypes.10 Any of the following parameters was accepted for inclusion1 11:
Abnormal umbilical cord blood or neonatal blood sample within 1 hour of birth (pH ≤7.1 or base excess ≤ −12 or lactate ≥6).11
Apgar score ≤5 at 5 or 10 min.11
Ongoing neonatal resuscitation at 5 or 10 min.11
No cry from baby at 5 or 10 min.
Studies where stated hypoxia-ischaemia criteria were not fully concordant, but sentinel data were provided were discussed and decided case by case.
Gestational age
Gestational age limit was set to ≥35+0 weeks defined by last menstrual period, first trimester ultrasound, fundal height or Ballard score.1 11 Lack of data on gestational age or mixing term and preterm infants <35 weeks of gestation in the report led to exclusion of the study to avoid contamination by non-hypoxic-ischaemic preterm brain injury.12
Additional exclusion criteria
Studies reporting NE due to other specified causes, such as hyperbilirubinaemia, and those where the whole cohort had some specific risk factor such as maternal hypertension rendering the sample non-representative of the normal population were excluded.
Types of outcomes
Reports were included if they included data on one or more of the outcomes below regardless of the original study purpose.
Inclusion criteria for objective 1
Main outcome was incidence of intrapartum-related NE in a birth cohort of a defined size regardless of the denominator used.
Inclusion criteria for objective 2
Main outcome was incidence of mortality in children with intrapartum-related NE either during the neonatal period (first 28 days of life) or until discharge from hospital.
Inclusion criteria for objective 3
Main outcome was incidence of death or moderate to severe disability at follow-up of 1–17 years defined similar to a previous systematic review11 as any grade of CP, intellectual impairment (IQ≥2 SD below mean), blindness (vision<6/60 in both eyes), or developmental delay using a validated instrument.13 In difference to Jacobs et al,11 any form of deafness was considered and in studies using Bayley Scales of Infant and Toddler Development version II (BSID-II) cut-off of < −2 SD or <70 was used to define moderate to severe disability whereas in BSID-III, < −1 SD or <85 was used for the same as these have been found to be equivalent.14
Secondary outcomes were CP, developmental delay assessed with any validated developmental assessment tool,13 blindness, deafness, epilepsy and neuropsychiatric disorders. Reports without developmental assessment were excluded.
Information sources and search strategy
The following databases were interrogated with the help of a librarian at Uppsala University, Sweden: Ovid MEDLINE, Cochrane, Web of Science and WHO Global Index Medicus. Search terms related to neonate AND encephalopathy AND LMIC using the Cochrane EPOC LMIC filter version 3 were combined, and the complete searches are presented in online supplemental table 1. This search strategy had not been previously validated. A search was performed for dates 1 November 2009 to 10 June 2020 and this was later updated on 18 November 2021.
bmjgh-2022-010294supp001.pdf (1.4MB, pdf)
Personal records and reference lists of related reviews were hand searched for further publications.11 15–29
Study selection
Records identified were exported to Zotero reference management software (V.5.0.96.3, Roy Rosenzweig Center for History and New Media, Virginia, USA) for removal of duplicates and then transferred to Rayyan (Rayyan Systems, Cambridge, Massachusetts, USA) for blinded screening of title and abstract by two independent reviewers (AJK and SW). Screening questions based on inclusion and exclusion criteria were developed and piloted a priori (online supplemental figure 1). Disagreements were discussed between the two reviewers. Google Translate was used for translation of abstracts when necessary. Full-text articles of records included in the first stage were retrieved and, when not found, the first authors were contacted via email or, when email was not available, via ResearchGate (ResearchGate, Germany) to request access. If no answer was received within 1 month, the article was excluded.
Full-text screening was done similarly using a prepiloted flow chart (online supplemental figure 2) with results independently recorded on Excel sheets (V.2108, Microsoft, USA). Results were compared and disagreements solved with an arbitrator (NB). Kappa score was calculated to quantify the level of agreement between the reviewers. Reasons for study exclusion in full-text screening stage were recorded in online supplemental table 2). No contact was made with authors to request missing, ambiguous or unprocessed data. If several reports using data from the same study patients were identified, only the report with most complete data was included. Reviewers were not blinded to report authors, institutions or journals. Articles written in languages not understood by the review team were translated into English by people fluent in the language.
Data collection process and data items
Study data were extracted by single reviewer (AJK) on an Excel sheet. Unclear cases were discussed with a second reviewer (NB).
The following background data were recorded: first author and publication year; country/ies; World Bank country income group (low, lower middle or upper middle)9 and national neonatal mortality rate (NMR, low<5/1000, mid 5–15/1000 and high >15/1000 live births)30 at median year of data collection; whether a population or hospital-based study; level of hospital; study design; case definition of NE; definition of intrapartum hypoxia-ischaemia; gestational age; exclusion criteria; number of cases classified as mild, moderate and severe NE; sex; type of intervention provided during neonatal period.
In terms of denominator (objective 1), we accepted both term live births and all births during the study period. Numerators for objective 2 were: number of deaths, duration of follow-up and attrition rate and for objective 3: the number of deaths; length of follow-up; attrition rate; definition(s) of abnormal neurodevelopmental outcome(s) and number of children with abnormal outcome(s). Neurodevelopmental outcomes were subcategorised by type when possible.
All outcome data were disaggregated by the severity of intrapartum-related NE when possible.4 Data on intervention and control arms in trials were collected separately. One report could contribute data to several objectives.
Risk of bias in individual studies
Risk of bias was assessed by discussion between two reviewers (AJK and SW) using the Newcastle Ottawa Scale for cohort studies.31 The original tool was modified by removing questions related to comparability of cohorts. The modified version had two questions related to selection of the cohort and three related to outcome assessment with each question awarded maximum one star (table 1, online supplemental table 3).
Table 1.
Overview of the included reports disaggregated by type(s) of outcome(s) reported
| Author, reference, year | Country | Study type | Intervention | Cases | NOS |
| Incidence | Max 2+3 | ||||
| Yang, 201948 | China | Cohort | Unclear | 262 | 2+0 |
| Incidence and neonatal mortality | Max 2+3/2+3 | ||||
| Horn, 201347 | South Africa | Retrospective observational | Unclear | 110 * | 2+1/1+1 |
| Moshiro, 201939 | Tanzania | Prospective observational | NT | 146 | 0+1/0+2 |
| Niaz, 202150 | Pakistan | Prospective observational | Unclear | 122† | 1+1/0+2 |
| Incidence, neonatal mortality and developmental outcome | Max 2+3/2+3+3 | ||||
| Lally, 201438 | India | Prospective observational | TH in 31% | 54 | 0+2/0+2+2 |
| Neonatal mortality | Max 2+3 | ||||
| Aly, 201572 | Egypt | RCT | TH+Melatonin Vs. TH | 30 | 0+3 |
| Bharadwaj, 201273 | India | RCT | TH vs NT | 130 | 0+2 |
| Biselele, 201337 | Congo DR | Prospective observational | NT | 44 | 0+2 |
| Biselele, 202074 | Congo Dr | Pilot/case-series | 2-Iminobiotin | 7 | 0+2 |
| Biselele, 201845 | Congo Dr | Prospective observational | NT | 57 | 1+2 |
| Biselele, 201457 | Congo Dr | Prospective observational | NT | 19 | 0+1 |
| Bozkurt, 202175 | Turkey | Retrospective observational | TH | 166 | 0+1 |
| El Shimi, 201451 | Egypt | RCT | EPO vs TH vs NT | 30 | 0+2 |
| Enweronu‐Laryea, 201954 | Ghana | Cohort | Passive TH | 13 | 1+1 |
| Hassanein, 201755 | Egypt | Case-Control | Unclear | 20 | 0+1 |
| Horn, 201052 | South Africa | Case Series | TH | 5 | 0+2 |
| Horn, 201276 | South Africa | Case Series | TH | 14 | 0+2 |
| Kinoshita, 202177 | Brazil | Retrospective observational | TH (FGP) | 71 | 0+1 |
| Martínez-Hernández, 202078 | Mexico | Before-After Study | EPO+TH (WBC vs SHC) | 12 | 0+1 |
| Oliveira, 201879 | India | Prospective observational | TH | 82 | 0+2 |
| Surmeli Onay, 202180 | Turkey | Before-After Study | TH vs TH+Aminophylline | 34 | 0+0 |
| Prashantha, 201981 | India | Before-After Study | TH (PCM vs FGP) | 62 | 0+1 |
| Shabeer,ठ201782 | India | Before-After Study | TH (PCM vs FGP) | 68 | 0+1 |
| Shrestha, 202083 | Nepal | Prospective observational | NT | 20¶ | 0+1 |
| Tanigasalam, 201656 | India | RCT | TH (FGP) vs NT | 120 | 0+2 |
| Thomas,** 201884 | India | Prospective observational | TH (PCM) | 103 | 0+1 |
| Umran, 201640 | Iraq | Case- Control | NT | 29 | 0+1 |
| Variane, 201785 | Brazil | Prospective observational | TH | 17 | 0+0 |
| Yang and Li, 202086 | China | RCT | TH (48 hours) vs TH (72 hours) vs NT | 92 | 0+2 |
| Neonatal mortality and developmental outcome | MAX 2+3+3 | ||||
| Aker,‡ 202187 | India | RCT | TH (PCM) vs NT | 49 | 0+3+3 |
| Catherine,**†† 202188 | India | RCT | TH (PCM) vs NT | 158 | 0+1+3 |
| Catherine,**†† 202089 | India | RCT | TH (PCM) vs NT | 158 | 0+1+3 |
| Celik,‡‡ 201553 | Turkey | RCT | TH SHC vs WBC | 7 | 0+2+3 |
| Celik,‡‡ 201690 | Turkey | RCT | TH SHC vs WBC | 29 | 0+2+3 |
| Das, 201791 | India | RCT | TH (FGP) vs NT | 60 | 0+3+3 |
| Gucuyener, 201260 | Turkey | Case Series | TH | 10 | 0+3+2 |
| Jia, 201841 | China | Non-random trial | TH early vs TH late vs NT | 152 | 0+2+2 |
| Khuwuthyakorn, 202192 | Thailand | Observational | TH | 23 | 0+1+3 |
| Malla, 201759 | India | RCT | EPO vs NT | 100 | 1+3+3 |
| Maoulainine, 201749 | Morocco | Non-random comparison | TH 50%, NT 50% | 38 | 1+1+1 |
| Perez, 201893 | Brazil | Cohort | TH (LFU) | 53 | 0+1+3 |
| Procianoy, 202094 | Brazil | Prospective observational | TH | 72 | 0+2+3 |
| Sun, 201244 | China | RCT | TH vs NT | 51 | 1+3+3 |
| Thayyil, 202146 | 3 Countries | RCT | TH vs NT | 408 | 1+1+2 |
| Valera, 201595 | Argentina | Observational | TH | 27 | 0+3+3 |
| Zhou,§ 201042 | China | RCT | TH vs NT | 194 | 1+1+2 |
| Zhu, 200996 | China | RCT | EPO vs NT | 167 | 1+2+2 |
| Zou,§ 201943 | China | RCT | TH vs NT | 99 | 1+2+3 |
| Developmental outcome | MAX 2+3 | ||||
| Ballot, 202058 | South Africa | Cohort | TH in 58% | 99 | 0+2 |
| Charki, 202097 | India | Non-Random Comparison | TH vs NT | 210 | 0+1 |
| Koshy,§ 201198 | India | Prospective observational | TH | 20 | 0+2 |
| Mbatha, 202199 | South Africa | Retrospective observational | TH in 73% | 155 | 0+2 |
| Weng, 2021100 | China | Before-After | TH vs NT | 61 | 0+3 |
NOS = Newcastle-Ottawa Scale of bias evaluation consisting of two questions related to selection of cohort and three questions related to reporting of outcome (see online supplemental table 3).
*Included several definitions of hypoxia-ischaemia and NE. N=110 = widest definition available.
†Recruited 45 children with gestational age 34+0…36+6 that were excluded from the neonatal mortality analysis.
§Koshy 2011 presents follow-up data for some of the children that were potentially included by Shabeer et al82.
¶Recruited 84 children with Apgar <7 at 5 min. Out of those, 20 fulfilled the inclusion criteria of pH<7.05 and only those were included.
††Same patients in both reports by Catherine, but different outcomes are reported.
‡‡Mostly same patients in both reports by Celik. Only cases with grade I were included from Çelik et al53 as the outcomes of grade II–III cases were reported in Celik et al90 that includes five additional children.
EPO, erythropoietin; FGP, frozen gel packs; LFU, laminar flow unit; NT, standard care with normothermia; PCM, phase-changing material; RCT, randomized-controlled trial; SHC, selective head cooling; TH, therapeutic hypothermia; WBC, whole body cooling.
bmjgh-2022-010294supp002.pdf (66KB, pdf)
Synthesis of results
We expected substantial clinical and methodological heterogenicity between the included studies whereby narrative synthesis was prioritised. This included describing the methodological characteristics of each study, their settings and individual strengths and limitations.32 33 Particular attention was paid to comparison of study findings between different geographical and economic contexts.
The three objectives of the review guided grouping of the reports into tables and figures. Forest plots of the prevalence of main outcomes with point estimate and 95% CIs calculated by Freeman-Tukey double arcsine transformation were presented.34 Inverse variance of heterogenicity model was chosen for meta-analyses as it is suitable for pooling data from heterogeneous studies of varying sizes.35 All analyses were made by using MetaXL V.5.3 (EpiGear International, Sunrise Beach, Queensland, Australia) add-in in Excel. For objective 1, a population-based rather than hospital-based incidence was mandated for meta-analysis due to wide context related variability. For objectives 2 and 3, data were separated by neonatal intervention status and duration of follow-up.
Subgroup analyses by grade of intrapartum-related NE were planned a priori. However, as limited data were available, we combined grades II and III together. Statistical heterogenicity was analysed with I² analysis and >50% considered a sign of high heterogenicity in which case further subgroup analyses post hoc were considered. Sensitivity analysis of stepwise removal of each study were done for all estimates to see if any single study was inflicting disproportionate effect on the results.
Risk of bias across studies
A funnel plot of studies included for the forest plots was examined as an indication of potential publication bias.36
Patient and public involvement
No patients were involved in the design and conduct of this study.
Results
Study selection
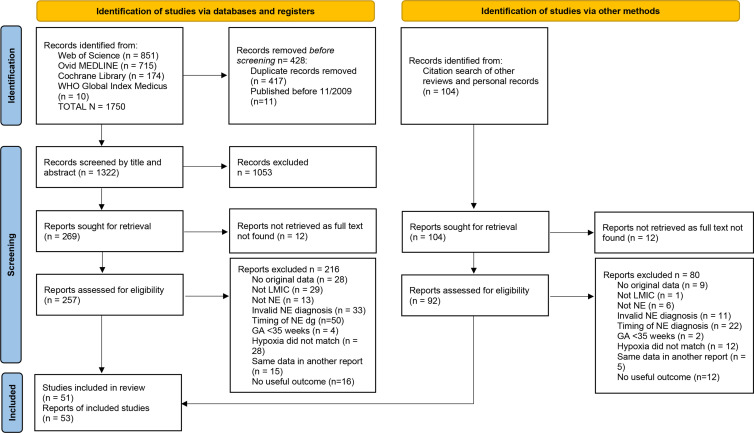
The final search produced 1750 records and after removing 417 duplicates and 11 reports published prior to November 2009, 1322 unique reports remained (figure 1). All articles included an abstract in English. There were 121 cases of conflicts between the reviewers during title and abstract screening, which were solved by discussion. The 269 reports identified were sought for retrieval and complemented by 104 reports found from other sources.
Figure 1.
PRISMA 2020 flow chart of study inclusion, from Page et al.8 PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols. GA, gestational age; LMIC, low- and middle-income country; NE, neonatal encephalopathy.
Screening of full text resulted in 53 reports from 51 studies being included in the review. There were 35 cases of conflict between the reviewers, which were solved by arbitration (88.2% agreement, Cohen’s kappa=0.55, moderate agreement). Translation into English was done for 13 reports (8 from Chinese, 2 from Turkish and 1 from Russian). Reasons for excluding reports in the full-text screening stage are presented in online supplemental table 2.
Study characteristics
Characteristics of the included reports are presented in table 1. The studies included 4181 children with intrapartum-related NE. When looking at only those nine studies37–45 that recruited and reported all NE grades indiscriminately, the distribution of severity was 334/858 (38.9%) mild, 292/858 (34.0%) moderate and 232/858 (27.0%) severe NE. Sex of the newborn was reported in 38 studies and pooled prevalence of male sex was 63% (95% CI 58% to 69%, I2=80%) (online supplemental figure 3).
The studies included data from 18 countries with 14 reports from Africa, 6 from Americas, 34 from Asia and none from Oceania or Europe with Turkey classified as part of Asia. Low-income countries were presented in 5 reports, lower-middle in 23 reports and upper-middle-income countries in 25 reports. National NMR was low in 1, medium in 24 and high in 27 reports at the time of data collection. One study presented data from both from a low NMR setting (Sri Lanka) and high mortality settings (Bangladesh and India)46 (online supplemental table 4).
bmjgh-2022-010294supp003.pdf (169.9KB, pdf)
The vast majority (45/51) of studies were conducted in either university or tertiary hospitals and only two studies from China and South Africa, respectively, claimed to be population-based.47 48 Inclusion criteria used in the individual studies varied widely and are presented in online supplemental table 4. Therapeutic hypothermia was routinely used in 21 and trialled in 18 of the 53 reports.
Bias evaluation of the included studies
Results of the risk of bias evaluation are presented in table 1 and online supplemental table 3. No report achieved full scores. Major shortcomings were identified in the representativeness of the data with only three papers scoring a star in this question.47–49 Reports about neonatal mortality and developmental outcomes had better scores for case ascertainment than those where incidence of intrapartum-related NE was examined. About half of the reports had issues with incomplete follow-up, which might further bias the results.
No obvious asymmetry implying publication bias was observed in the funnel plots presented in online supplemental figures 4 and 5, but the results were scattered due to high heterogenicity.
Results of individual studies and syntheses
Studies reporting incidence
Data on incidence of intrapartum-related NE are presented in table 2. Incidence of all grade NE ranged from 20.3/1000 live births50 to 1.5/1000 term live births48 depending on study setting and location (median 4.7/1000 live births, five studies). Only two population-based studies were included whereby no meta-analysis was conducted.47 48 One was examining different definitions of intrapartum-related NE in Cape Town, South Africa, and in this paper the incidence of any grade NE ranged from 2.3 to 4.3 per 1000 live births.47 The second presented data from 27 hospitals in China with incidence of any grade of NE 1.5 per 1000 live births.48
Table 2.
Studies reporting incidence of intrapartum-related neonatal encephalopathy
| Author (ref) | Country | Definition of denominator | Reported incidence | Incidence/1000 | |
| Horn, 201347 | South Africa | All live births (incl. home births) | All grades | N/A | 2.3…4.3/1000 |
| Grade I | N/A | 0.4…1.3/1000 | |||
| Grades II–III | N/A | 1.5…3.7/1000 | |||
| Lally, 201438 | India | All births in the hospital | All grades | 54/11 532 | 4.7/1000 |
| Moshiro, 201939 | Tanzania | All live births in the hospital | All grades | 146/10 320 | 14.1/1000 |
| Grade I | 113/10 320 | 10.9/1000 | |||
| Grade II | 16/10 320 | 1.6/1000 | |||
| Grade III | 17/10 320 | 1.6/1000 | |||
| Grades II–III | 33/10 320 | 3.2/1000 | |||
| Niaz, 202150 | Pakistan | All births in the hospital | All grades | 122/5986 | 20.3/1000 |
| Grade I | 61/5986 | 10.2/1000 | |||
| Grade II | 42/5986 | 7.0/1000 | |||
| Grade III | 19/5986 | 32./1000 | |||
| Grades II–III | 61/5986 | 10.2/1000 | |||
| Yang, 201948 | China | Term live births in the 27 hospitals | All grades | 262/175 223 | 1.5/1000 |
N/A, Not Available.
The hospital-based studies on incidence came from India,38 Pakistan50 and Tanzania39 all of which had high national NMR at the time of data collection.
Studies reporting neonatal mortality
Neonatal mortality associated with intrapartum-related NE was reported in 45 studies (online supplemental table 5). In total, 636 of the 3307 (19.2%) included neonates died. Mortality ranged from 19/30 (63.3%) in a small Egyptian trial comparing conventional care with therapeutic hypothermia and erythropoietin51 to 0/5 in a case series of therapeutic hypothermia in South Africa52 and 1/51 (2.0%) in a cooling trial in a tertiary centre in China.44
bmjgh-2022-010294supp004.pdf (61.2KB, pdf)
There were limited data available for neonatal mortality disaggregated by severity of NE. Only 10 reports included data on mortality associated with grade I intrapartum-related NE.37–40 44 45 53–56 In total, 22/236 (9.3%) mild NE cases died. Four reports included at least one death in patients with mild NE.39 40 45 57
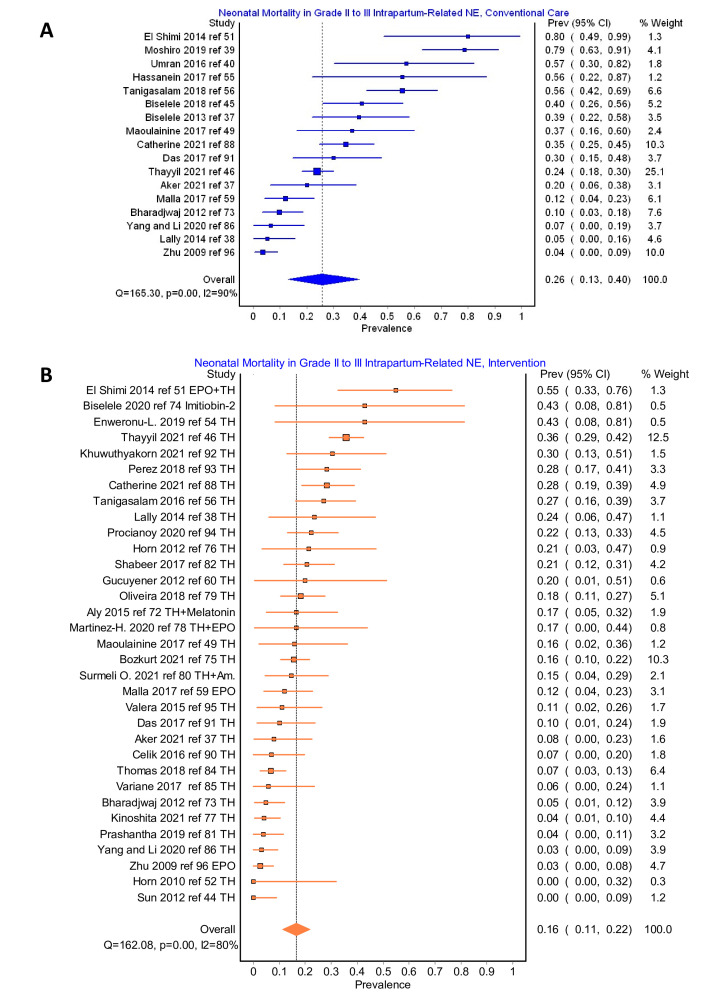
Figure 2 presents neonatal mortality in infants with grade II and III intrapartum-related NE. Data were split by intervention status during neonatal period. Pooled mortality in the conventional care group was 35.7% (95% CI 14% to 41%, I2=80%, 17 studies) and in the intervention group 15.8% (95% CI% 11 to 22%, I2=90%, 33 studies).
Figure 2.
Prevalence of neonatal mortality in children with grades II–III intrapartum-related neonatal encephalopathy (NE) in (A) conventional care group, (B) intervention group. Prevalence of 1.0 = 100% mortality. Am, aminophylline; EPO, erythropoietin; TH, therapeutic hypothermia.
Results of the post hoc subgroup analyses of neonatal mortality by national NMR and World Bank country income group were heterogenous (online supplemental figure 6). Sensitivity analysis with stepwise removal of studies only changed the pooled point estimates by few percentage points.
Studies reporting neurodevelopmental outcome
Neurodevelopmental follow-up of at least 1 year was conducted in 23 studies (online supplemental table 6). No studies continued follow-up beyond 3.5 years precluding inference on neuropsychiatric conditions. A combined outcome of death or moderate to severe neurodevelopmental disability was reported in 19 studies with 1595 children with any grade of NE of whom 712 (44.6%) had adverse outcome.
bmjgh-2022-010294supp005.pdf (116.6KB, pdf)
Only three studies provided data on outcomes of children with mild NE.42 53 58 None of the seven children treated with normothermia in Turkey had death or moderate to severe disability at 12 months’ age.53 In a therapeutic hypothermia trial in China, 6 out of 19 cooled and 7 out of 15 normothermic infants had moderate intellectual disability (Gesell Child Development Age Scale 70–84) at 18 months’ age while none died or had severe disability.42 A cohort study from South Africa reported that 1 out of 14 infants with mild NE developed CP at follow-up of mean 14.3 months.58
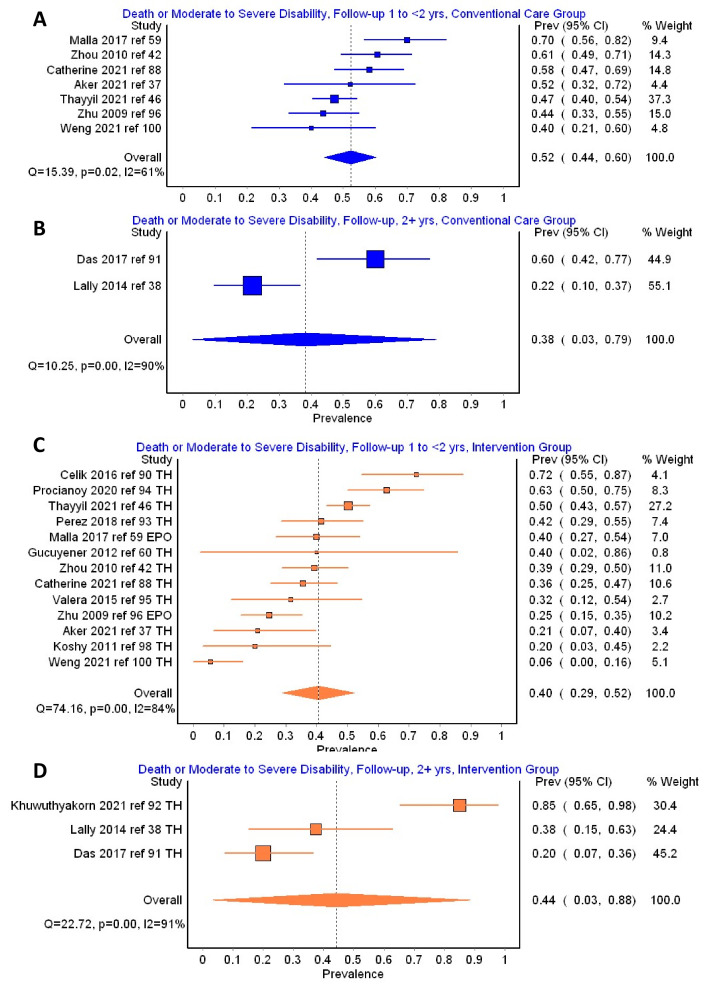
Figure 3 shows the combined outcome of death or moderate to severe developmental disability in children with grade II or III intrapartum-related NE from 16 studies where these data could be extracted. All these studies were either intervention trials or used therapeutic hypothermia as part of routine care and the results are split by intervention status and duration of follow-up. Children in conventional care group had somewhat higher incidence of the combined outcome than those in the intervention group at 1–2 years’ follow-up (52% (95% CI 44% to 66%, I2=61%, 7 studies) vs 40% (95% CI 29% to 52%, I2=84%, 13 studies)). Only three studies had follow-up longer than two or more years. No single study had overwhelming impact in the results in a sensitivity analysis.
Figure 3.
Prevalence of death or moderate to severe neurodevelopmental disability associated with grades II–III intrapartum-related neonatal encephalopathy in (A) conventional care group with follow-up 1 to <2 years, (B) conventional care group with follow-up ≥2 years, (c) intervention group with follow-up 1 to <2 years, (D) intervention group with follow-up ≥2 years. Prevalence of 1.0=100% adverse outcome. EPO, erythropoietin; TH, therapeutic hypothermia.
CP in survivors was evaluated in 11 reports (914 children, mean incidence 16.7%, online supplemental table 6 and online supplemental figure 7). In infants surviving grades II–III intrapartum-related NE, incidence of CP ranged from 29/84 (34.5%) at mean age of 19 months in a trial of erythropoietin in India59 to 3/38 (7.9%) at mean age of 3.4 years in another Indian cohort where one-third of the children were treated with hypothermia.38 In one Turkish case series, none of the three children surviving therapeutic hypothermia treatment had CP by the age of 12 months.60
Discussion
This systematic review identified 53 reports from 51 studies reinforcing the scale of intrapartum-related NE in terms of burden of disease, death and disability in LMICs.
Estimates of NE incidence ranged from 1.5 to 20.3/1000 births comparable to 2013 review by Lee et al.3 A study from China reported low NE incidence at 1.5/1000 term live births48 resembling levels seen in high-income countries with low NMR.3 61 Low incidence combined with excellent outcomes reported in other studies included in the review is in line with recent Global Burden of Disease data indicating that the burden of NE in China is rapidly decreasing62 with the rider that assessment bias cannot be ruled out in the register based incidence study.
NE-related neonatal mortality and adverse neurodevelopmental outcome were associated with all grades of intrapartum-related NE. There was scarcity of data on grade I NE, but the result shows that in LMIC settings, even mild NE carries a risk of neonatal mortality in addition to early disability reported previously from high-income settings.63 We do not have the data to speculate about later childhood neuropsychiatric issues and future studies should extend their follow-up to include also these outcomes.64
Studies reporting data on combined grades II–III intrapartum-related NE produced the most comparable estimates of neonatal mortality and neurodevelopmental outcomes. Similar to Lee et al,3 the highest mortality was seen in studies from high national NMR settings when no neuroprotective interventions during the newborn period were provided (pooled mortality 32% (95% CI 16% to 49% vs 28% (95% CI 19% to 37%) reported by Lee et al.3).
The combined outcome of death or moderate to severe neurodevelopmental disability occurred on average at similar rate as in the original cooling trials, where its pooled incidence was 31.7% in the intervention arm and 61.4% in the control group.11 Overall, our review showed better outcomes in studies where infants received therapeutic hypothermia or other neuroprotective interventions during neonatal period, but the pooled results in figures are not comparable as different studies were included in each group. This area is currently highly controversial in the light of the HELIX multicentre trial where cooling was predictive of a significantly neonatal higher mortality,46 the interpretation of which is causing difficulty for institutions and policy makers. Several meta-analyses with conflicting results have been recently published on efficacy of therapeutic hypothermia in LMICs.16 65 66
Though we cannot extrapolate from the data exactly which single interventions will have the greatest impact on neonatal and childhood neurodevelopmental outcomes, it is likely, that a combined approach including improved antenatal care, adolescent health, family planning and access to hospital delivery centres rather than a silo-driven policy will be required to reduce the disease burden.7
Strengths
Our review has several strengths, including up-to-date data, PRISMA adherence, clear a priori assessment processes and a wide geographical spread of studies.
Limitations
NE is a challenging diagnosis and only a minority of papers reported standardisation of the criteria. We cannot be sure that all the infants fulfilling the inclusion criteria were true cases of intrapartum-related NE but tried to minimise this by only including studies where intrapartum hypoxia-ischaemia could be presumed with a high degree of certainty. Indirectly, this led to exclusion of studies from lower levels of care with limited access to physicians trained in NE assessment. Remaining heterogenicity in inclusion criteria of individual studies partly explains the wide differences in the reported outcomes.
Only two of the included studies were population-denominator based and the substantial heterogenicity in outcomes is likely to reflect both true variance between populations and methodological differences. The meta-analysis results should, therefore, be interpreted with caution. The preponderance of intervention studies from tertiary level referral hospitals from middle-income countries is likely to have further limited generalisability, but on the other hand use of therapeutic hypothermia is already widespread in such settings.67–70 Further limitation on interpretation of the forest plots is that the Freeman Tukey back-transformation is prone to producing misleading results when sample sizes vary greatly, but we did not observe such issue in our data.71
Lastly, although we conducted a systemic search of databases, 12 of the 53 included articles were identified from other sources indicating that the search terms used were not optimal and potential articles might have been missed. The Cochrane EPOC LMIC filter has not been validated and NE has no MeSH term whereby terms related to hypoxia-ischaemia were used instead. Chinese language databases and grey literature were not searched.
Conclusion
Though there has been progress in some regions, the incidence, neonatal mortality and morbidity of intrapartum-related NE has in most LMICs been static in the 10 years since the last review.
Acknowledgments
Authors would like to thank Uppsala University librarian Kazuko Gustafsson for conducting the literature searches, and Melissa Öztürk, Yaqing Gao and Otto Haapsamo for translation of articles.
Footnotes
Handling editor: Seema Biswas
Twitter: @Ashish_K_C
Contributors: AJK, AKC, HL, JW and NB conceptualised and designed the study. AJK, NB and SW collected and interpreted the data. AJK drafted the work and all authors revised it critically, approved the final version and agree to be accountable for all aspects of the work. AKC is responsible for the overall content as the guarantor and accept full responsibility for the finished work and the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data extracted from the articles for the analyses presented in this review are available in online supplemental tables.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study is a review of already published research and no ethical permit was sought for its conduct.
References
- 1.Executive summary: neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of obstetricians and Gynecologists' Task force on neonatal encephalopathy. Obstet Gynecol 2014;123:896–901. 10.1097/01.AOG.0000445580.65983.d2 [DOI] [PubMed] [Google Scholar]
- 2.GBD 2019 Under-5 Mortality Collaborators . Global, regional, and national progress towards sustainable development goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the global burden of disease study 2019. Lancet 2021;398:870–905. 10.1016/S0140-6736(21)01207-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee ACC, Kozuki N, Blencowe H, et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr Res 2013;74 Suppl 1:50. 10.1038/pr.2013.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol 1976;33:696–705. 10.1001/archneur.1976.00500100030012 [DOI] [PubMed] [Google Scholar]
- 5.Campbell OMR, Calvert C, Testa A, et al. The scale, scope, coverage, and capability of childbirth care. Lancet 2016;388:2193–208. 10.1016/S0140-6736(16)31528-8 [DOI] [PubMed] [Google Scholar]
- 6.Versantvoort JMD, Kleinhout MY, Ockhuijsen HDL, et al. Helping babies breathe and its effects on intrapartum-related stillbirths and neonatal mortality in low-resource settings: a systematic review. Arch Dis Child 2020;105:127–33. 10.1136/archdischild-2018-316319 [DOI] [PubMed] [Google Scholar]
- 7.Lawn JE, Blencowe H, Oza S, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet 2014;384:189–205. 10.1016/S0140-6736(14)60496-7 [DOI] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 2021;18:e1003583. 10.1371/journal.pmed.1003583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Bank . World bank country and lending groups, 2020. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed 25 Jul 2020].
- 10.Sandoval Karamian AG, Mercimek-Andrews S, Mohammad K, et al. Neonatal encephalopathy: etiologies other than hypoxic-ischemic encephalopathy. Semin Fetal Neonatal Med 2021;26:101272. 10.1016/j.siny.2021.101272 [DOI] [PubMed] [Google Scholar]
- 11.Jacobs SE, Berg M, Hunt R, et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev 2013;2013:CD003311. 10.1002/14651858.CD003311.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gopagondanahalli KR, Li J, Fahey MC, et al. Preterm hypoxic-ischemic encephalopathy. Front Pediatr 2016;4:114. 10.3389/fped.2016.00114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boggs D, Milner KM, Chandna J, et al. Rating early child development outcome measurement tools for routine health programme use. Arch Dis Child 2019;104:S22–33. 10.1136/archdischild-2018-315431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jary S, Whitelaw A, Walløe L, et al. Comparison of Bayley-2 and Bayley-3 scores at 18 months in term infants following neonatal encephalopathy and therapeutic hypothermia. Dev Med Child Neurol 2013;55:1053–9. 10.1111/dmcn.12208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milner KM, Neal EFG, Roberts G, et al. Long-term neurodevelopmental outcome in high-risk newborns in resource-limited settings: a systematic review of the literature. Paediatr Int Child Health 2015;35:227–42. 10.1179/2046905515Y.0000000043 [DOI] [PubMed] [Google Scholar]
- 16.Abate BB, Bimerew M, Gebremichael B, et al. Effects of therapeutic hypothermia on death among asphyxiated neonates with hypoxic-ischemic encephalopathy: a systematic review and meta-analysis of randomized control trials. PLoS One 2021;16:e0247229. 10.1371/journal.pone.0247229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang W, Ma J, Danzeng Q, et al. Safety of moderate hypothermia for perinatal hypoxic-ischemic encephalopathy: a meta-analysis. Pediatr Neurol 2017;74:51–61. 10.1016/j.pediatrneurol.2017.04.023 [DOI] [PubMed] [Google Scholar]
- 18.Garg B, Sharma D, Bansal A. Systematic review seeking erythropoietin role for neuroprotection in neonates with hypoxic ischemic encephalopathy: presently where do we stand. J Matern Fetal Neonatal Med 2018;31:3214–24. 10.1080/14767058.2017.1366982 [DOI] [PubMed] [Google Scholar]
- 19.Ivain P, Montaldo P, Khan A, et al. Erythropoietin monotherapy for neuroprotection after neonatal encephalopathy in low-to-middle income countries: a systematic review and meta-analysis. J Perinatol 2021;41:1–7. 10.1038/s41372-021-01132-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Razak A, Hussain A. Erythropoietin in perinatal hypoxic-ischemic encephalopathy: a systematic review and meta-analysis. J Perinat Med 2019;47:478–89. 10.1515/jpm-2018-0360 [DOI] [PubMed] [Google Scholar]
- 21.Ouwehand S, Smidt LCA, Dudink J, et al. Predictors of outcomes in hypoxic-ischemic encephalopathy following hypothermia: a meta-analysis. Neonatology 2020;117:411–27. 10.1159/000505519 [DOI] [PubMed] [Google Scholar]
- 22.Rossi AC, Prefumo F. Antepartum and intrapartum risk factors for neonatal hypoxic-ischemic encephalopathy: a systematic review with meta-analysis. Curr Opin Obstet Gynecol 2019;31:410–7. 10.1097/GCO.0000000000000581 [DOI] [PubMed] [Google Scholar]
- 23.Tann CJ, Martinello KA, Sadoo S, et al. Neonatal encephalopathy with group B streptococcal disease worldwide: systematic review, investigator group datasets, and meta-analysis. Clin Infect Dis 2017;65:S173–89. 10.1093/cid/cix662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Wincoop M, de Bijl-Marcus K, Lilien M, et al. Effect of therapeutic hypothermia on renal and myocardial function in asphyxiated (near) term neonates: a systematic review and meta-analysis. PLoS One 2021;16:e0247403. 10.1371/journal.pone.0247403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krishnan V, Kumar V, Variane GFT, et al. Need for more evidence in the prevention and management of perinatal asphyxia and neonatal encephalopathy in low and middle-income countries: a call for action. Semin Fetal Neonatal Med 2021;26:101271. 10.1016/j.siny.2021.101271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pauliah SS, Shankaran S, Wade A, et al. Therapeutic hypothermia for neonatal encephalopathy in low- and middle-income countries: a systematic review and meta-analysis. PLoS One 2013;8:e58834. 10.1371/journal.pone.0058834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Workineh Y, Semachew A, Ayalew E, et al. Prevalence of perinatal asphyxia in East and central Africa: systematic review and meta-analysis. Heliyon 2020;6:e03793. 10.1016/j.heliyon.2020.e03793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee CYZ, Chakranon P, Lee SWH. Comparative efficacy and safety of neuroprotective therapies for neonates with hypoxic ischemic encephalopathy: a network meta-analysis. Front Pharmacol 2019;10:1221. 10.3389/fphar.2019.01221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Igboanugo S, Chen A, Mielke JG. Maternal risk factors for birth asphyxia in low-resource communities. A systematic review of the literature. J Obstet Gynaecol 2020;40:1039–55. 10.1080/01443615.2019.1679737 [DOI] [PubMed] [Google Scholar]
- 30.UNICEF, WHO, World Bank Group and United Nations . UN Inter-agency group for child mortality estimation (UN IGME), 2020. Available: https://childmortality.org/data [Accessed 28 Mar 2022].
- 31.Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet], 2014. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Accessed 28 Jul 2022].
- 32.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKenzie J, Brennan S. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, et al., eds. Cochrane Handbook for systematic reviews of interventions version 6.2. Wiley, 2021. [Google Scholar]
- 34.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Statist. 1950;21:607–11. 10.1214/aoms/1177729756 [DOI] [Google Scholar]
- 35.Doi SAR, Barendregt JJ, Khan S, et al. Advances in the meta-analysis of heterogeneous clinical trials I: the inverse variance heterogeneity model. Contemp Clin Trials 2015;45:130–8. 10.1016/j.cct.2015.05.009 [DOI] [PubMed] [Google Scholar]
- 36.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Biselele T, Naulaers G, Bunga Muntu P, et al. A descriptive study of perinatal asphyxia at the university hospital of Kinshasa (Democratic Republic of Congo). J Trop Pediatr 2013;59:274–9. 10.1093/tropej/fmt011 [DOI] [PubMed] [Google Scholar]
- 38.Lally PJ, Price DL, Pauliah SS, et al. Neonatal encephalopathic cerebral injury in South India assessed by perinatal magnetic resonance biomarkers and early childhood neurodevelopmental outcome. PLoS One 2014;9:e87874. 10.1371/journal.pone.0087874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moshiro R, Perlman JM, Mdoe P, et al. Potential causes of early death among admitted newborns in a rural Tanzanian Hospital. PLoS One 2019;14:e0222935. 10.1371/journal.pone.0222935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Umran RMR, Al-Tahir M, Jagdish D, et al. Insulin-Like growth factor-1 levels in term newborns with hypoxic-ischemic encephalopathy. Am J Perinatol 2016;33:640–5. 10.1055/s-0036-1571319 [DOI] [PubMed] [Google Scholar]
- 41.Jia W, Lei X, Dong W, et al. Benefits of starting hypothermia treatment within 6 h vs. 6-12 h in newborns with moderate neonatal hypoxic-ischemic encephalopathy. BMC Pediatr 2018;18:50. 10.1186/s12887-018-1013-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou W-hao, Cheng G-qiang, Shao X-mei, et al. Selective head cooling with mild systemic hypothermia after neonatal hypoxic-ischemic encephalopathy: a multicenter randomized controlled trial in China. J Pediatr 2010;157:367–3. 10.1016/j.jpeds.2010.03.030 [DOI] [PubMed] [Google Scholar]
- 43.Zou L, Yuan H, Liu Q, et al. Potential protective effects of bilirubin following the treatment of neonatal hypoxic-ischemic encephalopathy with hypothermia therapy. Biosci Rep 2019;39:1–8. 10.1042/BSR20182332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun J, Li J, Cheng G, et al. Effects of hypothermia on NSE and S-100 protein levels in CSF in neonates following hypoxic/ischaemic brain damage. Acta Paediatr 2012;101:e316–20. 10.1111/j.1651-2227.2012.02679.x [DOI] [PubMed] [Google Scholar]
- 45.Biselele T, Bambi J, Naulaers G, et al. Observational study shows that it is feasible to provide neuroprotective treatment for neonatal encephalopathy in low-income countries. Acta Paediatr 2018;107:1345–9. 10.1111/apa.14263 [DOI] [PubMed] [Google Scholar]
- 46.Thayyil S, Pant S, Montaldo P, et al. Hypothermia for moderate or severe neonatal encephalopathy in low-income and middle-income countries (HELIX): a randomised controlled trial in India, Sri Lanka, and Bangladesh. Lancet Glob Health 2021;9:e1273–85. 10.1016/S2214-109X(21)00264-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Horn AR, Swingler GH, Myer L, et al. Defining hypoxic ischemic encephalopathy in newborn infants: benchmarking in a South African population. J Perinat Med 2013;41:211–7. 10.1515/jpm-2012-0107 [DOI] [PubMed] [Google Scholar]
- 48.Yang W, Wang L, Tian T, et al. Maternal hypertensive disorders in pregnancy and risk of hypoxic-ischemia encephalopathy. J Matern Fetal Neonatal Med 2021;34:1754–62. 10.1080/14767058.2019.1647529 [DOI] [PubMed] [Google Scholar]
- 49.Maoulainine FMR, Elbaz M, Elfaiq S. Therapeutic hypothermia in asphyxiated neonates: experience from neonatal intensive care unit of university hospital of Marrakech. Int J Pediatr 2017:3674140. 10.1155/2017/3674140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Niaz H, Jalil J, Khan QZ, et al. Clinical profile and short term outcome of hypoxic ischemic encephalopathy among birth Asphxiated babies in a tertiary care hospital. PAFMJ 2021;71:24–8. 10.51253/pafmj.v71i1.3847 [DOI] [Google Scholar]
- 51.El Shimi MS, Awad HA, Hassanein SMA, et al. Single dose recombinant erythropoietin versus moderate hypothermia for neonatal hypoxic ischemic encephalopathy in low resource settings. J Matern Fetal Neonatal Med 2014;27:1295–300. 10.3109/14767058.2013.855894 [DOI] [PubMed] [Google Scholar]
- 52.Horn AR, Harrison MC, Linley LL. Evaluating a simple method of neuroprotective hypothermia for newborn infants. J Trop Pediatr 2010;56:172–7. 10.1093/tropej/fmp089 [DOI] [PubMed] [Google Scholar]
- 53.Çelik Y, Atıcı A, Gülaşı S, et al. The effects of selective head cooling versus whole-body cooling on some neural and inflammatory biomarkers: a randomized controlled pilot study. Ital J Pediatr 2015;41:79. 10.1186/s13052-015-0188-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Enweronu-Laryea C, Martinello KA, Rose M, et al. Core temperature after birth in babies with neonatal encephalopathy in a sub-Saharan African hospital setting. J Physiol 2019;597:4013–24. 10.1113/JP277820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hassanein SMA, Nasr Eldin MH, Amer HA, et al. Human umbilical cord blood CD34-positive cells as predictors of the incidence and short-term outcome of neonatal hypoxic-ischemic encephalopathy: a pilot study. J Clin Neurol 2017;13:84–90. 10.3988/jcn.2017.13.1.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tanigasalam V, Bhat V, Adhisivam B, et al. Does therapeutic hypothermia reduce acute kidney injury among term neonates with perinatal asphyxia?--a randomized controlled trial. J Matern Fetal Neonatal Med 2016;29:2544–7. 10.3109/14767058.2015.1094785 [DOI] [PubMed] [Google Scholar]
- 57.Biselele T, Naulaers G, Tady B. Evolution of the Thompson score during the first 6 H in infants with perinatal asphyxia. Acta Paediatr 2014;103:145–8. 10.1111/apa.12470 [DOI] [PubMed] [Google Scholar]
- 58.Ballot DE, Rakotsoane D, Cooper PA, et al. A prospective observational study of developmental outcomes in survivors of neonatal hypoxic ischaemic encephalopathy in South Africa. S Afr Med J 2020;110:308–12. 10.7196/SAMJ.2020.v110i4.14311 [DOI] [PubMed] [Google Scholar]
- 59.Malla RR, Asimi R, Teli MA, et al. Erythropoietin monotherapy in perinatal asphyxia with moderate to severe encephalopathy: a randomized placebo-controlled trial. J Perinatol 2017;37:596–601. 10.1038/jp.2017.17 [DOI] [PubMed] [Google Scholar]
- 60.Gucuyener K, Beken S, Ergenekon E, et al. Use of amplitude-integrated electroencephalography (aEEG) and near infrared spectroscopy findings in neonates with asphyxia during selective head cooling. Brain Dev 2012;34:280–6. 10.1016/j.braindev.2011.06.005 [DOI] [PubMed] [Google Scholar]
- 61.Kurinczuk JJ, White-Koning M, Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev 2010;86:329–38. 10.1016/j.earlhumdev.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 62.Ou Z, Yu D, Liang Y, et al. Global trends in incidence and death of neonatal disorders and its specific causes in 204 countries/territories during 1990–2019. BMC Public Health 2022;22:1–13. 10.1186/s12889-022-12765-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Conway JM, Walsh BH, Boylan GB, et al. Mild hypoxic ischaemic encephalopathy and long term neurodevelopmental outcome - A systematic review. Early Hum Dev 2018;120:80–7. 10.1016/j.earlhumdev.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 64.Marlow N, Shankaran S, Rogers EE, et al. Neurological and developmental outcomes following neonatal encephalopathy treated with therapeutic hypothermia. Semin Fetal Neonatal Med 2021;26:101274. 10.1016/j.siny.2021.101274 [DOI] [PubMed] [Google Scholar]
- 65.Mathew JL, Kaur N, Dsouza JM. Up-To-Date systematic review and meta-analysis of therapeutic hypothermia for neonatal encephalopathy: is the crown losing its Sheen? Indian Pediatr 2021;58:1189–91. 10.1007/s13312-021-2406-0 [DOI] [PubMed] [Google Scholar]
- 66.Bellos I, Devi U, Pandita A. Therapeutic hypothermia for neonatal encephalopathy in low- and middle-income countries: a meta-analysis. Neonatology 2022;119:300–10. 10.1159/000522317 [DOI] [PubMed] [Google Scholar]
- 67.Variane GF, Cunha LM, Pinto P, et al. Therapeutic hypothermia in Brazil: a MultiProfessional national survey. Am J Perinatol 2019;36:1150–6. 10.1055/s-0038-1676052 [DOI] [PubMed] [Google Scholar]
- 68.Wang Z, Zhang P, Zhou W, et al. Neonatal hypoxic-ischemic encephalopathy diagnosis and treatment: a national survey in China. BMC Pediatr 2021;21:261. 10.1186/s12887-021-02737-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Joolay Y, Harrison MC, Horn AR. Therapeutic hypothermia and hypoxic ischemic encephalopathy: opinion and practice of pediatricians in South Africa. J Perinat Med 2012;40:447–53. 10.1515/jpm-2011-0292 [DOI] [PubMed] [Google Scholar]
- 70.Chandrasekaran M, Swamy R, Ramji S, et al. Therapeutic hypothermia for neonatal encephalopathy in Indian neonatal units: a survey of national practices. Indian Pediatr 2017;54:969–70. 10.1007/s13312-017-1194-z [DOI] [PubMed] [Google Scholar]
- 71.Schwarzer G, Chemaitelly H, Abu-Raddad LJ, et al. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods 2019;10:476–83. 10.1002/jrsm.1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aly H, Elmahdy H, El-Dib M, et al. Melatonin use for neuroprotection in perinatal asphyxia: a randomized controlled pilot study. J Perinatol 2015;35:186–91. 10.1038/jp.2014.186 [DOI] [PubMed] [Google Scholar]
- 73.Bharadwaj SK, Bhat BV. Therapeutic hypothermia using gel packs for term neonates with hypoxic ischaemic encephalopathy in resource-limited settings: a randomized controlled trial. J Trop Pediatr 2012;58:382–8. 10.1093/tropej/fms005 [DOI] [PubMed] [Google Scholar]
- 74.Biselele T, Bambi J, Betukumesu DM, et al. A phase IIA clinical trial of 2-iminobiotin for the treatment of birth asphyxia in DR Congo, a low-income country. Paediatr Drugs 2020;22:95–104. 10.1007/s40272-019-00373-3 [DOI] [PubMed] [Google Scholar]
- 75.Bozkurt O, Yucesoy E. Acute kidney injury in neonates with perinatal asphyxia receiving therapeutic hypothermia. Am J Perinatol 2021;38:922–9. 10.1055/s-0039-1701024 [DOI] [PubMed] [Google Scholar]
- 76.Horn AR, Joolay Y, Tooke L, et al. A servo-assisted gel-pack cooling method for newborn infants with hypoxic-ischemic encephalopathy. J Trop Pediatr 2012;58:236–8. 10.1093/tropej/fmr069 [DOI] [PubMed] [Google Scholar]
- 77.Kinoshita AN, Magalhães M, Rodrigues DP, et al. Effectiveness of reaching and maintaining therapeutic hypothermia target temperature using low-cost devices in newborns with hypoxic-ischemic encephalopathy. Anat Rec 2021;304:1217–23. 10.1002/ar.24615 [DOI] [PubMed] [Google Scholar]
- 78.Martínez-Hernández A, Iglesias-Leboreiro J, Plascencia-Pimentel K, et al. Hipotermia terapéutica en recién nacidos Con encefalopatía hipóxico-isquémica. Rev. mex. pediatr 2020;87:176–82. [Google Scholar]
- 79.Oliveira V, Kumutha JR, E N, et al. Hypothermia for encephalopathy in low-income and middle-income countries: feasibility of whole-body cooling using a low-cost servo-controlled device. BMJ Paediatr Open 2018;2:e000245. 10.1136/bmjpo-2017-000245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Surmeli Onay O, Gunes D, Aydemir O, et al. A single dose of aminophylline administration during therapeutic hypothermia; does it make a difference in glomerular filtration rate? Eur J Pediatr 2021;180:3367–77. 10.1007/s00431-021-04128-6 [DOI] [PubMed] [Google Scholar]
- 81.Prashantha YN, Suman Rao PN, Nesargi S, et al. Therapeutic hypothermia for moderate and severe hypoxic ischaemic encephalopathy in newborns using low-cost devices - ice packs and phase changing material. Paediatr Int Child Health 2019;39:234–9. 10.1080/20469047.2018.1500805 [DOI] [PubMed] [Google Scholar]
- 82.Shabeer MP, Abiramalatha T, Smith A, et al. Comparison of two low-cost methods of cooling neonates with hypoxic ischemic encephalopathy. J Trop Pediatr 2017;63:174–81. 10.1093/tropej/fmw067 [DOI] [PubMed] [Google Scholar]
- 83.Shrestha S, Dhungana SP, Shrestha S, et al. Correlation of Thompson score in predicting early outcome of newborn with birth asphyxia. J Nepal Health Res Counc 2020;18:406–10. 10.33314/jnhrc.v18i3.2746 [DOI] [PubMed] [Google Scholar]
- 84.Thomas N, Abiramalatha T, Bhat V, et al. Phase Changing Material for Therapeutic Hypothermia in Neonates with Hypoxic Ischemic Encephalopathy - A Multi-centric Study. Indian Pediatr 2018;55:201–5. [PubMed] [Google Scholar]
- 85.Variane GFT, Magalhães M, Gasperine R, et al. Early amplitude-integrated electroencephalography for monitoring neonates at high risk for brain injury. J Pediatr 2017;93:460–6. 10.1016/j.jped.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 86.Yang T, Li S. Efficacy of different treatment times of mild cerebral hypothermia on oxidative factors and neuroprotective effects in neonatal patients with moderate/severe hypoxic-ischemic encephalopathy. J Int Med Res 2020;48:300060520943770. 10.1177/0300060520943770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Aker K, Thomas N, Adde L, et al. Prediction of outcome from MRI and general movements assessment after hypoxic-ischaemic encephalopathy in low-income and middle-income countries: data from a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 2022;107:32–8. 10.1136/archdischild-2020-321309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Catherine RC, Ballambattu VB, Adhisivam B, et al. Effect of therapeutic hypothermia on the outcome in term neonates with hypoxic ischemic Encephalopathy-A randomized controlled trial. J Trop Pediatr 2021;67:fmaa073. 10.1093/tropej/fmaa073 [DOI] [PubMed] [Google Scholar]
- 89.Catherine RC, Bhat BV, Adhisivam B, et al. Neuronal biomarkers in predicting neurodevelopmental outcome in term babies with perinatal asphyxia. Indian J Pediatr 2020;87:787–92. 10.1007/s12098-020-03283-2 [DOI] [PubMed] [Google Scholar]
- 90.Celik Y, Atıcı A, Gulası S, et al. Comparison of selective head cooling versus whole-body cooling. Pediatr Int 2016;58:27–33. 10.1111/ped.12747 [DOI] [PubMed] [Google Scholar]
- 91.Das S, Sarkar N, Bhattacharya M, et al. Neurological outcome at 30 months of age after mild hypothermia via selective head cooling in term neonates with perinatal asphyxia using low-cost CoolCap: a single-center randomized control pilot trial in India. J Pediatr Neurol 2017;15:157–65. 10.1055/s-0037-1603681 [DOI] [Google Scholar]
- 92.Khuwuthyakorn V, Kosarat S, Tantiprabha W, et al. Two-Year outcomes of therapeutic hypothermia in perinatal hypoxic–ischaemic encephalopathy cases at Chiang Mai university hospital. Arch Dis Child 2021;106:516–7. 10.1136/archdischild-2020-318880 [DOI] [PubMed] [Google Scholar]
- 93.Perez J. 53 newborns with hypoxic ischemic encephalopathy treated with hypothermia therapy using neonatal laminar flow unit. EC Paediatr 2018;7:1073–8. [Google Scholar]
- 94.Procianoy RS, Corso AL, Schoenardie BO, et al. Outcome and feasibility after 7 years of therapeutic hypothermia in southern Brazil. Am J Perinatol 2020;37:955–61. 10.1055/s-0039-1692388 [DOI] [PubMed] [Google Scholar]
- 95.Valera M, Berazategui JP, Saa G, et al. Implementation in Buenos Aires city of a program to prevent neurological damage caused by hypoxic-ischemic encephalopathy: therapeutic hypothermia. Arch Argent Pediatr 2015;113:437–43. 10.5546/aap.2015.eng.437 [DOI] [PubMed] [Google Scholar]
- 96.Zhu C, Kang W, Xu F, et al. Erythropoietin improved neurologic outcomes in newborns with hypoxic-ischemic encephalopathy. Pediatrics 2009;124:e218–26. 10.1542/peds.2008-3553 [DOI] [PubMed] [Google Scholar]
- 97.Charki S, Kalyanshettar SS, Singh S, et al. Experience of therapeutic hypothermia in neonates with perinatal asphyxia in a tertiary care center in North Karnataka, India. J Clin Neonatol 2020;9:175–81. 10.4103/jcn.JCN_85_19 [DOI] [Google Scholar]
- 98.Koshy B, Padankatti CS, George KC, et al. Neurodevelopmental outcome following whole body cooling for perinatal asphyxia. Indian Pediatr 2011;48:982–3. [PubMed] [Google Scholar]
- 99.Mbatha S, Nakwa FL, Thandrayen K, et al. Neurodevelopmental outcome in neonates with hypoxic-ischaemic encephalopathy managed with therapeutic hypothermia in a tertiary-level public hospital outside an intensive care unit setting. Paediatr Int Child Health 2021;41:171–6. 10.1080/20469047.2021.1967625 [DOI] [PubMed] [Google Scholar]
- 100.Weng B, Yan C, Chen Y, et al. Efficiency evaluation of neuroprotection for therapeutic hypothermia to neonatal hypoxic-ischemic encephalopathy. Front Neurosci 2021;15:668909. 10.3389/fnins.2021.668909 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-010294supp001.pdf (1.4MB, pdf)
bmjgh-2022-010294supp002.pdf (66KB, pdf)
bmjgh-2022-010294supp003.pdf (169.9KB, pdf)
bmjgh-2022-010294supp004.pdf (61.2KB, pdf)
bmjgh-2022-010294supp005.pdf (116.6KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data extracted from the articles for the analyses presented in this review are available in online supplemental tables.