Abstract
Background:
Clozapine is the only medication licenced for patients with psychosis that is resistant to conventional antipsychotic treatment. However, despite its effectiveness, it remains widely underutilised. One contributory factor for this may be clinicians’ lack of confidence around the management of clozapine.
Objective:
We conducted a survey of clinicians working in Early Intervention in Psychosis (EIP) services to determine their training needs for clozapine management in EIP services.
Methods:
An electronic survey was made available to all clinicians working in EIP services in England. The survey assessed confidence and training needs regarding managing clozapine in patients with treatment-resistant psychosis. Quantitative data were analysed using total mean scores and the Mann–Whitney U test.
Results:
In all, 192 (27%) of approximately 700 clinicians from 35 EIP services completed the survey. Approximately half (54%) had not received training on treatment with clozapine. Experience of training was higher in prescribers than non-prescribers, and among medical than non-medical clinicians. Previous training was associated with significantly higher confidence in offering clozapine and managing treatment-resistant psychosis (p < 0.001). Confidence levels with managing treatment-resistant psychosis and clozapine were relatively high (mean = 4 out of 5, SD = 1). Respondents were most confident about monitoring mental health response to treatment (mean = 5, SD = 1). Participants were least confident about how to discontinue clozapine treatment safely (mean = 3, SD = 1).
Conclusion:
Most clinicians working in EIP have not received training on the use of clozapine. This may account, in part, for the underutilisation of clozapine in EIP services. The provision of training in the identification of treatment-resistant psychosis and the use of clozapine will likely improve the detection and management of treatment resistance in the early phase of psychosis.
Keywords: clozapine, early intervention, treatment-resistant psychosis, training
Introduction
Up to a third of patients with a diagnosis of psychosis are treatment-resistant, defined as the persistence of symptoms despite trials of two or more antipsychotics.1 Clozapine is the gold-standard treatment for such patients,2,3 but is often not offered until years after patients meet criteria for treatment resistance, leading to poorer clinical outcomes and increased health costs.2,4 One factor behind this delay may be a lack of confidence among clinicians in managing patients on clozapine. In particular, clinician concerns about adverse drug reactions and the need for regular monitoring with clozapine may contribute towards a reluctance to prescribe clozapine, so-called ‘clozaphobia’.5,6 Other suggested contributors to clozapine’s underuse include a lack of prescribing experience among clinicians.7
In the United Kingdom, Early Intervention in Psychosis (EIP) services provide a comprehensive range of psychological, social and pharmacological interventions to patients experiencing a first episode of psychosis.8 Recent studies have shown that treatment-resistant psychosis (TRP) is evident in around 25% of patients in UK EIP services.9,10 However, very few of these patients are offered clozapine.9 This may be because, traditionally, the management of TRP has not been a focus of EIP, and therefore, EIP teams have not had the experience or training in this area.
Improving clozapine use is a priority across UK EIP services.11,12 This is based on evidence that delays in clozapine initiation are associated with inferior clinical outcomes - in particular, a reduction in the probability of response.13,14 Despite these recommendations, there is no established or consistent approach to the training of clinicians on clozapine use in the context of EIP services.4 Moreover, to our knowledge, the training needs for EIP clinicians regarding clozapine are unknown. Understanding the specific training needs of EIP clinicians would be informative to mental health services to design a training programme that could be delivered to address this knowledge and skills gap.
The present study aimed to assess the proportion of EIP clinicians who have received training in the management of TRP. Specifically, we (1) assessed clinician confidence around the diagnosis of TRP, clozapine initiation, monitoring and management of adverse effects; and (2) compared confidence in prescribing clozapine between those who had previously received training and those who had not.
Methods
We undertook an online nationwide survey of clinicians working in EIP services in England, consisting of approximately 700 clinicians. We utilised the Checklist for Reporting Results of Internet E-Surveys in designing the survey.15
Survey design
The survey was developed by a multidisciplinary team consisting of psychiatrists, specialist pharmacists, psychologists and occupational therapists. It comprised 17 items divided into three sections: demographic information, such as sex and the number of years in practice (n = 7); training experience in TRP identification and clozapine management, including previous training, adequacy of training provided and further training needs (n = 3); and confidence around identifying TRP and clozapine management (n = 7). For the latter section, respondents rated their confidence in six different aspects of TRP and clozapine management using a 5-point Likert-type scale. These were: identifying TRP, offering clozapine, physical health monitoring of patients initiated on clozapine, monitoring mental state response to treatment, managing side effects and discontinuing clozapine. Participants were also asked if clozapine discontinuation guidelines would be beneficial.
The survey was disseminated using Qualtrics XM (Provo, Utah, USA). A pilot study of clinicians (n = 60) was initially conducted within the South London and Maudsley NHS Foundation Trust to assess item range and variance, as well as content and clarity. The final version (available on request) took a median of 7 min to complete (interquartile range: 5–11 min).
Participants and ethical considerations
A total of 109 EIP services in England were approached via email and asked to disseminate the survey to their clinicians. These services were identified using the NHS triangulation tool that showed each service that contributed data to the National Clinical Audit of Psychosis. Thirty-five NHS Trusts agreed to disseminate the survey. The survey was accessible for 12 weeks. Ethical approval was obtained from King’s College London (MRSU-20/21-25297). Individual participants gave informed consent prior to beginning the survey online.
Statistical analysis
A composite mean score was calculated from the six Likert-type questions regarding clinician confidence around clozapine. Survey items concerning training and confidence on aspects of clozapine were described using means and standard deviations. The confidence mean score was tested for the assumption of normal distribution using Shapiro–Wilk test of normality. A Mann–Whitney U test was conducted with a significance level of p < 0.05. We compared the composite confidence score for those who had received clozapine training versus those that had not received training. Data were analysed using R.16
Results
Sample characteristics
In all, 192 clinicians completed the survey. The mean age was 43 (range: 22–64) years. The most common profession was nurses (50%), followed by psychiatrists (16%) and other health care professionals (11%). Forty-eight (25%) of the responders were prescribers (Table 1).
Table 1.
Survey respondents.
| Respondent characteristics | Sample (n = 192) |
|---|---|
| Sex (%)a | |
| Female | 133 (69.3) |
| Mean age (years, SD) | 42.8 (10.8) |
| Self-reported professionb (%) | |
| Nurse | 95 (49.5) |
| Psychiatrist | 30 (15.6) |
| Other | 21 (10.9) |
| Psychologist | 17 (8.9) |
| Social worker | 15 (7.8) |
| Consultant psychiatrist | 9 (4.7) |
| Pharmacist | 3 (1.6) |
| Clinical experience (%) | |
| 0–5 years | 54 (28.1) |
| 6–10 years | 36 (18.8) |
| 11–20 years | 46 (24.0) |
| 21+ years | 48 (25.0) |
| Prescribera (%) | |
| Prescriber | 48 (25.0) |
| Non-prescriber | 142 (74.0) |
| Care coordinator (%)a | |
| Care coordinator role | 100 (52.1) |
| Non-care coordinator role | 90 (46.9) |
Missing data in two respondents
Missing data in eight respondents.
Training
Of the 192 respondents to the question, 37% (n = 71) reported that they had received dedicated clozapine training and 54% (n = 103) had not received training; 9% (n = 17) of the respondents were not sure or did not answer. The mean number of years of clinical experience for respondents who received training was 17 years (SD = 10) versus 12 years (SD = 10) for respondents who had not received training.
Among prescribers (n = 48), 60% (n = 29) reported that they had received training, whereas among non-prescribers (n = 142), 30% (n = 42) reported that they had received training. Overall, 78% of the sample (n = 150) indicated that they would probably or definitely benefit from more training; 10% (n = 20) were unsure and 10% (n = 19) said they would probably or definitely not benefit.
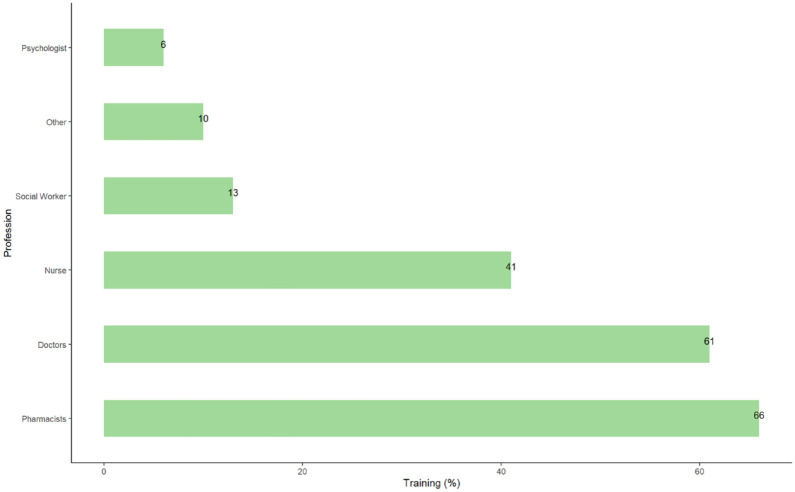
Among psychiatrists (n = 39), 61% reported that they received training and 28% (n = 11) had not. Among non-psychiatrists (n = 151), 30% (n = 46) reported that they had received training and 60% (n = 91) had not. Training experience by profession is shown in Figure 1.
Figure 1.
Self-reported clozapine training levels by profession.
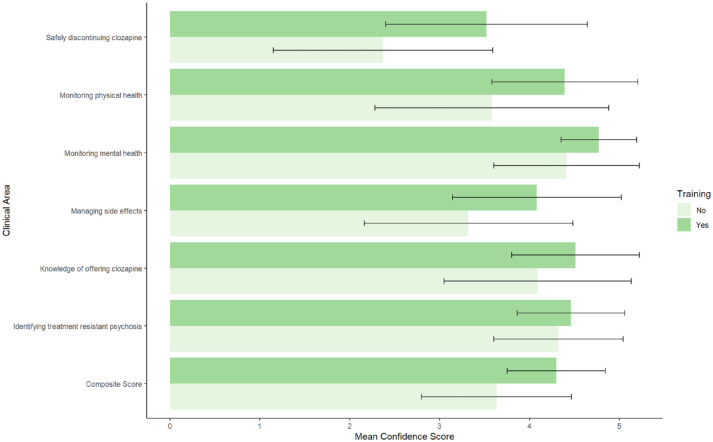
Confidence
Participants were asked to describe their confidence levels with managing TRP and clozapine (Figure 2). Of 183 respondents, the mean composite confidence score was 4 (SD = 1) out of 5. Respondents were most confident about monitoring mental health response to treatment (mean = 5, SD = 1). Participants were least confident about how to discontinue clozapine treatment safely (mean = 3, SD = 1). In total, 92% (n = 169) of respondents felt that a guideline on clozapine discontinuation guidelines would be beneficial. A Shapiro–Wilk test found the confidence data set to be non-Gaussian in distribution. Confidence levels were statistically higher in those who previously received training compared with those who did not (z = –5.2. p < 0.001). Mean item scores and standard deviations are displayed in Figure 2.
Figure 2.
Mean confidence scores around clozapine management among EI clinicians by training.
For individual clinical areas, 5 would present a high level of confidence while a score closer to 1 represents a lower level of confidence in relation to that item. Error bars represent standard deviation.
Discussion
Summary of findings
In a national survey of clinicians working in EIP services, we found that fewer than half had received training on clozapine treatment in early TRP. Training rates were higher among prescribers compared with non-prescribers and medical compared with non-medical clinicians. Despite reasonably high confidence levels around the identification of TRP and management of clozapine treatment, most respondents indicated that they would benefit from additional training. Respondents particularly lacked confidence about the discontinuation of clozapine treatment, with most indicating that they would benefit from guidelines on this. Exploratory analysis revealed that clinicians who had received training had greater confidence around clozapine medicines management.
Comparison with other studies
To the best of our knowledge, this is the first study to assess the confidence, attitudes, practice and training needs of EIP clinicians around clozapine medicines management. Our findings indicate that clinicians who had previously received training were significantly more confident with clozapine management compared with those who had no previous training. A recent survey by Dvalishvili et al.17 measured psychiatry residents’ level of comfort in prescribing clozapine in the United States finding very high levels of confidence around prescribing clozapine. On the contrary, a US-based survey of 164 trainee psychiatrists by Singh et al.18 reported that just half of respondents were ‘somewhat or very comfortable’ initiating clozapine treatment and just under half of respondents were uncomfortable. This variation may be attributed to differences in experience and exposure to prescribing clozapine. More specifically, in the former study, all participants reported previously prescribing clozapine. Whereas, in the second study, only two-thirds of respondents indicated experience of prescribing clozapine. Notably, the majority of respondents in the Singh et al.18 study stated that more exposure to clozapine management would increase comfort in treatment initiation. In our study, confidence levels were high around clozapine management; however, most respondents acknowledged that they would benefit from more dedicated training which suggests that the current approaches are inadequate for a practice behaviour change. In a survey of UK-based psychiatrists, over 75% reported having good training in using clozapine.19 Notably, only 7% of respondents in this survey were practicing in EIP services. However, even in this sample, there were notable knowledge gaps – such as the risk of severe neutropenia changing with time and the benefits of clozapine in substance misuse and suicidal risk. Overall, this suggests that a dedicated training programme on clozapine would be beneficial for clinicians across professions.
Training and Facilitators
Calls for organisational and educational efforts to promote evidence-based psychiatric treatments, including clozapine in TRP, have been made for well over a decade.20–22 Importantly, such training has been shown to be effective in improving prescriber confidence and clozapine use in some locations in the United States.20,22 In our survey, 78% of respondents felt that they would benefit from further training. In addition, the results of our survey suggest that EIP clinicians felt that training was an important component in addressing clozapine underuse. Notably, a training programme established to facilitate nurse-led clozapine clinics in Australia not only led to increased clinician knowledge but also improved clinical outcomes and decreased adverse events.23 Unfortunately, at present, there is no established approach to the training of clozapine medicine management in TRP for clinicians more broadly in the United Kingdom or indeed globally. As demonstrated by preliminary local data from the United States, training clinicians in the use of clozapine may not only improve antipsychotic prescribing and address geographical variability, but also minimise delay in offering clozapine to those who may benefit.20 More specifically, by combining educational actions with other interventions such as online support for prescribers and patients, Carruthers et al.24 reported a 40% increase in clozapine trials in New York. This is particularly important for early identification of TRP as recent evidence shows that individuals may respond less well to clozapine the longer its initiation is delayed. For example as in a Danish registry study, each prior antipsychotic trial resulted in a 8–11% lower likelihood of response to clozapine.13
Clinical implications and limitations
Despite around 25% of EIP patients meeting criteria for TRP, most EIP clinicians have not been trained in its management. It is noteworthy that clinicians working within EIP services are not well versed in using the only medication that is effective for TRP. While there is no specific training in general for clinicians who decide to practice in EIPs, there appears to be an unmet need for training in this area. It is plausible that this training need extends to other psychosis services and existing training programmes for psychiatrists. Implementation of such training may lead to the earlier detection of TRP and the earlier initiation of treatment with clozapine, although empirical evidence is required to assess this. The training of non-prescribers such as care co-ordinators is important, as they typically interact more with patients than prescribers and are thus best placed to monitor, identify and escalate adverse effects and concerns with clozapine treatment in a timely manner. One limitation of our study is the low response rate, although this is a common issue when undertaking surveys of clinicians.25 In particular, the key decision maker in determining whether to initiate clozapine is usually the responsible clinician, but we received only nine responses from consultant psychiatrists. Nevertheless, this is the largest study to date in the field, with responses from 35 EIP services. Moreover, it is plausible that non-respondents from our survey received less training and were less confident in clozapine management. A further limitation is that we do not know the total number of EIP clinicians working in the participating teams, so our response rate is an estimate.
Conclusion
The results of this study suggest that most clinicians in EIP teams in England have not received dedicated training in the treatment of patients with clozapine. This likely contributes to underutilisation of clozapine in EIP services. This issue could be addressed by the development of specific guidelines and training in this area, particularly around the identification of TRP, initiation and discontinuation of clozapine treatment.
Acknowledgments
None.
Footnotes
ORCID iDs: Ebenezer Oloyede  https://orcid.org/0000-0003-1352-4017
https://orcid.org/0000-0003-1352-4017
David Taylor  https://orcid.org/0000-0002-2557-1710
https://orcid.org/0000-0002-2557-1710
Graham Blackman  https://orcid.org/0000-0001-7025-8670
https://orcid.org/0000-0001-7025-8670
Contributor Information
Ebenezer Oloyede, South London and Maudsley NHS Foundation Trust, London, UK; Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, DeCriesney, London, UK.
Bethany Mantell, Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK.
Julie Williams, Health Service and Population Research Department, Centre for Implementation Science, King’s College London, London, UK.
Serena Lai, South London and Maudsley NHS Foundation Trust, London, UK.
Sameer Jauhar, South London and Maudsley NHS Foundation Trust, London, UK; Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK.
David Taylor, South London and Maudsley NHS Foundation Trust, London, UK; Institute of Pharmaceutical Science, King’s College, London.
James H. MacCabe, South London and Maudsley NHS Foundation Trust, London, UK Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK; NIHR Biomedical Research Centre for Mental Health South London and Maudsley NHS, London, UK.
Robert Harland, South London and Maudsley NHS Foundation Trust, London, UK.
Philip McGuire, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford, Oxfordshire, UK.
Graham Blackman, South London and Maudsley NHS Foundation Trust, London, UK; Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK.
Declarations
Ethics approval and consent to participate: The study was approved by the King’s College London Ethics Committee (MRSU-20/21-25297). Individual participants gave informed consent prior to beginning the survey online.
Consent for publication: Not applicable.
Author contributions: Ebenezer Oloyede: Conceptualization; Formal analysis; Methodology; Validation; Writing – original draft.
Bethany Mantell: Data curation; Formal analysis; Methodology; Writing – review & editing.
Julie Williams: Methodology; Writing – review & editing.
Serena Lai: Writing – review & editing.
Sameer Jauhar: Writing – review & editing.
David Taylor: Writing – review & editing.
James H. MacCabe: Writing – review & editing.
Robert Harland: Writing – review & editing.
Philip McGuire: Supervision; Writing – review & editing.
Graham Blackman: Conceptualization; Supervision; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
The authors declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: D.T. is the Editor-in-Chief of Therapeutic Advances in Psychopharmacology; therefore, the peer-review process was managed by alternative members of the Board and the submitting Editor was not involved in the decision-making process.
Availability of data and materials: Authors had free access to the anonymised study data. The data that support the findings of this study are available from the corresponding author, E.O., upon reasonable request.
References
- 1. Howes OD, McCutcheon R, Agid O, et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry; 2017; 174: 216–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oloyede E, Casetta C, Dzahini O, et al. There is life after the UK clozapine central non-rechallenge database. Schizophr Bull 2021; 47: 1088–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oloyede E, Whiskey E, Casetta C, et al. Relaxation of the criteria for entry to the UK Clozapine Central Non-Rechallenge Database: a modelling study. Lancet Psychiatry; 2022; 9: 636–644. [DOI] [PubMed] [Google Scholar]
- 4. Whiskey E, Barnard A, Oloyede E, et al. An evaluation of the variation and underuse of clozapine in the United Kingdom. Acta Psychiatr Scand 2021; 143: 339–347. [DOI] [PubMed] [Google Scholar]
- 5. Pandarakalam JP. The art of clozapine therapy and ‘clozaphobia’. BMJ 2019; 364: l484. [DOI] [PubMed] [Google Scholar]
- 6. Cetin M. Clozaphobia: fear of prescribers of clozapine for treatment of schizophrenia. Klinik Psikofarmakoloji Bülteni / Bull Clin Psychopharmacol 2014; 24: 295–301. [Google Scholar]
- 7. Verdoux H, Quiles C, Bachmann CJ, et al. Prescriber and institutional barriers and facilitators of clozapine use: a systematic review. Schizophr Res; 2018; 201: 10–19. [DOI] [PubMed] [Google Scholar]
- 8. Singh SP. Early intervention in psychosis. Br J Psychiatry 2010; 196: 343–345. [DOI] [PubMed] [Google Scholar]
- 9. Stokes I, Griffiths SL, Jones R, et al. Prevalence of treatment resistance and clozapine use in early intervention services. Bjpsych Open 2020; 6: e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Siskind D, Orr S, Sinha S, et al. Rates of treatment-resistant schizophrenia from first-episode cohorts: systematic review and meta-analysis. Br J Psychiatry; 2022; 220: 115–120. [DOI] [PubMed] [Google Scholar]
- 11. Nikolić N, Hill K, Campbell E, et al. Early access to clozapine in Early Intervention in Psychosis: hope vs reality. Early Interv Psychiatry; 2021; 15: 193–200. [DOI] [PubMed] [Google Scholar]
- 12. Royal College of Psychiatrists. The quality standards for early intervention in psychosis services (2nd ed.), 2021, https://www.rcpsych.ac.uk/docs/default-source/improving-care/ccqi/quality-networks/early-intervention-in-psychosis-teams-(eipn)/quality-standards-for-eip-services-2nd-edition.pdf?sfvrsn=131a6e4e_2 (accessed 31st May 2022).
- 13. Nielsen J, Nielsen RE, Correll CU. Predictors of clozapine response in patients with treatment-refractory schizophrenia: results from a Danish Register Study. J Clin Psychopharmacol 2012; 32: 678–683. [DOI] [PubMed] [Google Scholar]
- 14. Üçok A, Çikrikçili U, Karabulut S, et al. Delayed initiation of clozapine may be related to poor response in treatment-resistant schizophrenia. Int Clin Psychopharmacol 2015; 30: 290–295. [DOI] [PubMed] [Google Scholar]
- 15. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res 2004; 6: e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Team RC. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2022. [Google Scholar]
- 17. Dvalishvili M, Miller BJ, Surya S. Comfort level and perceived barriers to clozapine use: survey of general psychiatry residents. Acad Psychiatry 2021; 45: 528–529. [DOI] [PubMed] [Google Scholar]
- 18. Singh B, Hughes AJ, Roerig JL. Comfort level and barriers to the appropriate use of clozapine: a preliminary survey of US psychiatric residents. Acad Psychiatry 2020; 44: 53–58. [DOI] [PubMed] [Google Scholar]
- 19. Tungaraza TE, Farooq S. Clozapine prescribing in the UK: views and experience of consultant psychiatrists. Ther Adv Psychopharmacol 2015; 5: 88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Freudenreich O, Henderson DC, Sanders KM, et al. Training in a clozapine clinic for psychiatry residents: a plea and suggestions for implementation. Acad Psychiatry; 2013; 37: 27–30. [DOI] [PubMed] [Google Scholar]
- 21. Joober R, Boksa P. Clozapine: a distinct, poorly understood and under-used molecule. J Psychiatry Neurosci 2010; 35: 147–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cotes RO, Janjua AU, Broussard B, et al. A comparison of attitudes, comfort, and knowledge of clozapine among two diverse samples of US psychiatrists. Community Ment Health J 2022; 58: 517–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clark SR, Wilton L, Baune BT, et al. A state-wide quality improvement system utilising nurse-led clinics for clozapine management. Australas Psychiatry 2014; 22: 254–259. [DOI] [PubMed] [Google Scholar]
- 24. Carruthers J, Radigan M, Erlich MD, et al. An initiative to improve clozapine prescribing in New York State. Psychiatric Services 2016; 67: 369–371. [DOI] [PubMed] [Google Scholar]
- 25. Wiebe ER, Kaczorowski J, MacKay J. Why are response rates in clinician surveys declining. Can Fam Physician 2012; 58: e225–e228. [PMC free article] [PubMed] [Google Scholar]