Abstract
Objectives
To conceptualize new methods for integrating patient-centered measurement into team-based care.
Methods
A standalone portal was introduced into a rural clinic to support conceptualization of new methods for integration of patient-centered measurement in team-based care. The portal housed mental health-related online resources, three patient-reported measures and a self-action plan. Six providers and four patients used the portal for four months. Our data collection techniques included clinic discussions, one-on-one interviews, workflow diagrams and data generated through the portal. Analysis was supported through coding interview transcripts, looking across multiple sources of research data and research team discussions.
Results
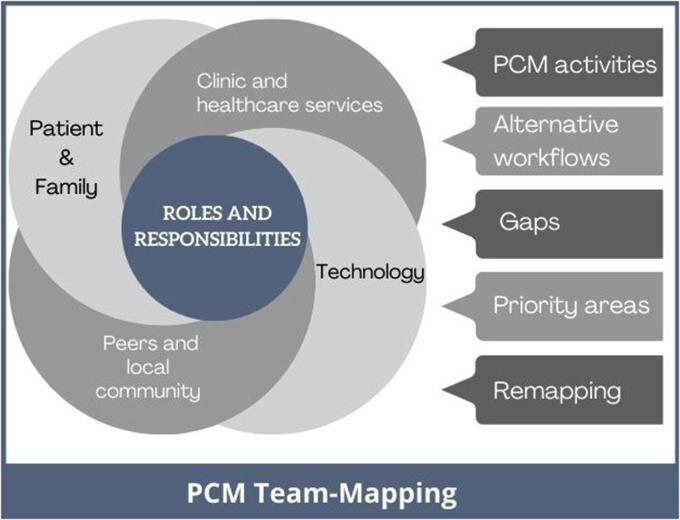
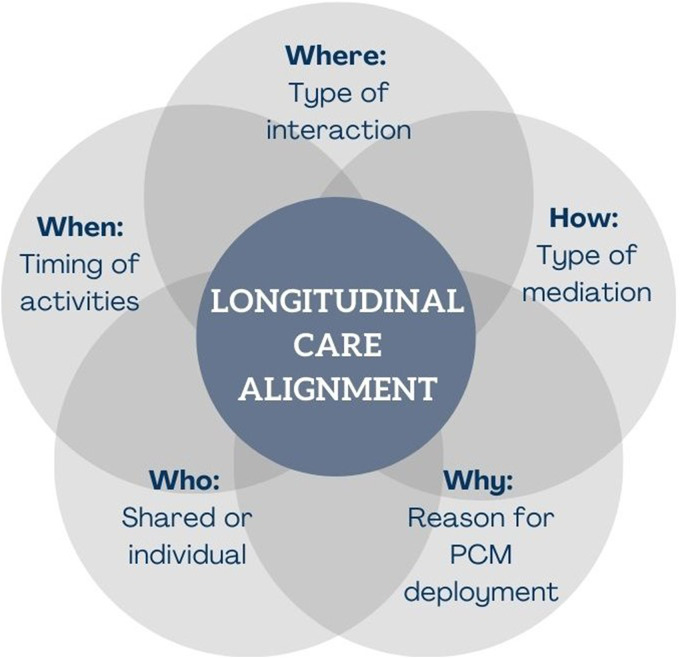
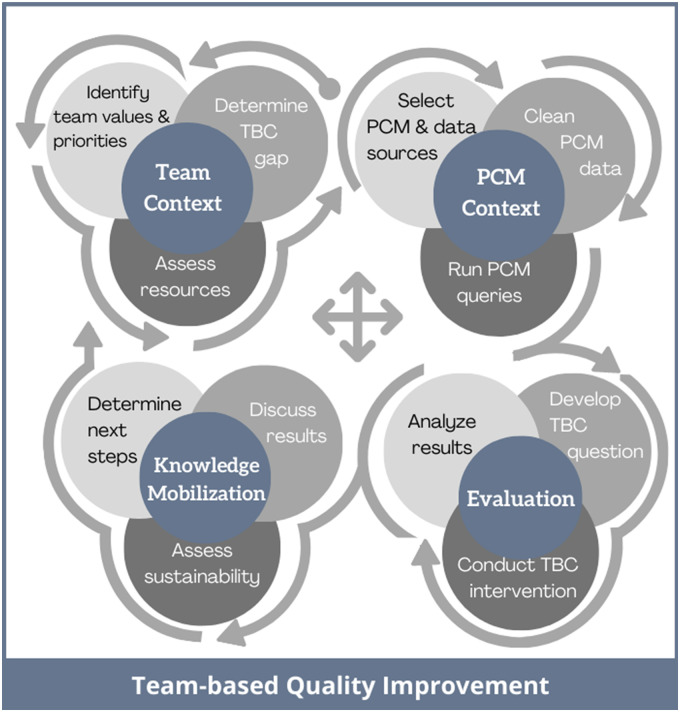
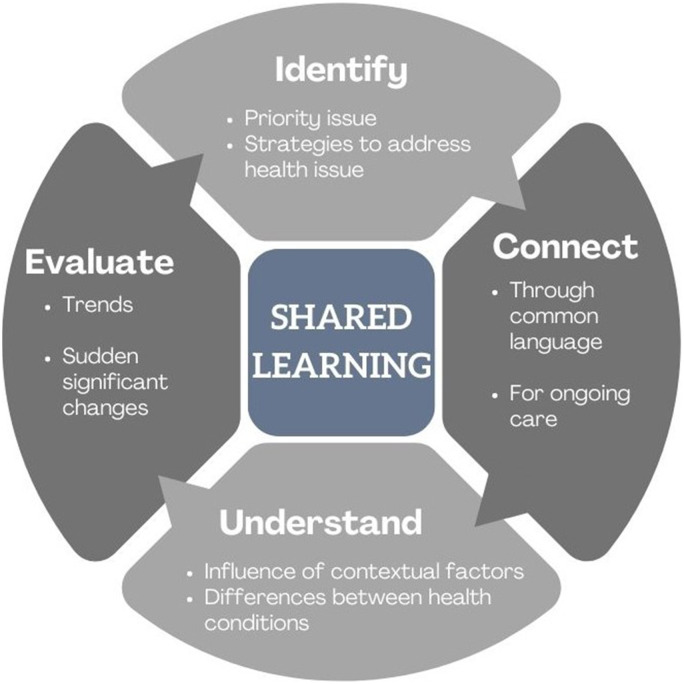
Our research team conceptualized five team-based patient-centered measurement methods through this study. Patient-centered measurement Team Mapping offfers a technique to provide greater clarity of care-team roles and responsibilities in data collected through patient-centered measurement. Longitudinal Care Alignment can guide the care-team on incorporating patient-centered measurement into ongoing provider–patient interactions. Digital Tool Exploration can be used to evaluate a team's readiness toward digital tool adoption, and the impact of these tools. Team-based quality improvement serves as a framework for engaging teams in patient-centered quality improvement. Shared learning is a method that promotes patientprovider interactions that validate patient's perspectives of their care.
Conclusion
The portal illuminated new methods for the integration of patient-centered measurement in team-based care. The first three proposed patient-centered measurement methods provides ways to assess how a clinic can incorporate patient-centered measurement methods into team-based care. The latter two methods focus on the aim of patient-generated data in which patient's values and perspectives are represented and quality of patient-centered care can be evaluated. Further testing is needed to assess the utility of these patient-centered measurement methods across different clinical settings and domains.
Keywords: Patient-centered care, patient participation, patient-reported outcome measures, patient generated health data, patient portals, quality assurance, health care, shared decision-making
Introduction
Patient-centered measurements
Patient-centered measurement (PCM) has been conceptualized as a way forward to patient-centered care, in which patient's values and perspectives are prioritized in the delivery of their care.1–7 PCMs include patient-reported experience measures (PREMs),3 patient-reported outcome measures (PROMs),1 patient self-action plans and patient-generated health data (e.g., measures of symptom management, such as blood pressure).4 Such effort is recognized as key to a team-based approach, in which patients’ values are represented and providers are more fully informed of patients’ current health status.5–7 PCMs can also inform a care team on their performance and areas to target for improved quality of care.1,3 Although there is some evidence that the inclusion of PCMs in routine practice can improve the care process, health outcomes, and patient involvement and satisfaction,1,3,8–11 the adoption of PCMs is limited.
Digital technologies
Challenges for PCM use include integration into clinical workflow, technology access, clinician's perceptions on the value of PCM and clinician's limited knowledge of effectively using PCMs to support care decisions.12,13 Possible technologies involved in PCM collection and use include standalone systems, tethered patient portals and built-in electronic medical record (EMR) functions, and tablets or smart phones.14,15 As these technologies are not fully integrated into routine practice, their introduction can result in unanticipated changes to clinic workflow that may discourage PCM adoption. Practice guidance suggests that successful PCM implementation requires vision, leadership, commitment, practice change, and cultural shift at multiple health-system levels.16–18
Patient's medical home as a model for team-based care
The study was conducted in the context of the Canadian Patient's Medical Home (PMH) model. According to the College, PMH is a ‘family practice defined by its patients as the place they feel most comfortable presenting and discussing their personal and family health and medical concerns’,19.p2. Viewed as the future model of family practice,19 Canadian jurisdictions have implemented and adapted the PMH model in multiple ways taking into account local context and healthcare infrastructures.20–22 Since its conceptualization in the 1960s, the PMH has evolved into a patient-centered, team-based primary care practice model that focuses on patients’ healthcare supports and needs in an integrated, coordinated manner.23–25 The revised 2019 Canadian PMH model consists of 10 pillars organized into three themes: foundations, functions, and ongoing development 19,26–28 (see Supplemental File 1 for an illustration of the three divisions of the ten pillars). For example, in British Columbia, PMH provide patients longitudinal care (the foundations), by working with and creating a team-based practice (functions) and expanding their network of provider's supports in the community or region (ongoing development).29–31
Literature is sparse on how PMHs can help advance PCM methods to support effective use of PCM in team-based care. While there are studies on incorporating patient voices,32,33 and patient-reported experiences and outcomes 34–36 in evaluating PMH performance, we are not aware of studies that examine how PMHs can help advance PCM methods, particularly in resource-limited settings.37 Thus, there is a need for new PCM methods that take into account the nuances in the PMH model of team-based care, and use of digital tools for team-based care. To address this knowledge gap, we conducted an exploratory field study in a rural PMH practice. Our aim was to conceptualize new ways of incorporating PCM into team-based care as part of the PMH model.
Methods
Study domain, design, site and participants
A multi-method exploratory study was conducted from February 2020 to April 2021 in a rural community setting in British Columbia. Further details of our integrated knowledge translation methodological approach are reported in a separate publication.38 Mental health was selected as the domain for focus, as it is a high priority area for British Columbia.39 The site was recruited with the help of a regional Division of Family Practice that provides professional and community support to local clinics. The clinic is a rural family practice consisting of multiple physicians, each supported by a medical office assistant. In addition, there is a registered nurse and social worker who have their time allocated across multiple clinics.
Participants included four patients, two family physicians, one nurse, one social worker, and two medical office assistants from a private clinic that uses PMH as its model of care. The patient participants were individuals with anxiety and/or depression recruited with the help of the clinic. Research team members consisted of patient partners within the region, clinicians and researchers. Our collaborators were two quality-improvement professionals from the region, and an industry partner.
Patient portal and interventions
The patient portal was a standalone web-based commercial product from our industry partner,40 and included a selection of educational resources and PCMs focused on mental health (See Supplemental File 2 for further details on the portal). Articles on mental health were created from online resources provided through the BC Ministry of Health and provincial mental health association,41 and the local community. To create additional value in accessing the patient portal, we also added educational articles on a coronavirus disease 2019 (COVID-19) government tax rebate, the purpose of PCM, technology resources, and how to set goals for behaviour change. An article on where to access academic lay abstracts was also added in response to patient-participants’ requests for more advanced mental health and scientific resources. PCMs included a self-action plan for depression,42 Patient Health Questions-9 (PHQ9),43 General Anxiety Disorder-7 (GAD-7),44 Patient-Reported Outcomes Measurement Information System (PROMIS) self-efficacy,45,46 and a subset of questions from the patient experience survey used in the regional Division.47
Participants were offered the use of the portal at no cost for a 4-month period. As the portal was not tethered to the EMR, one provider simulated interoperability by transferring PCM data from the portal to the EMR in three ways: (a) into an existing PCM-specific section of EMR; (b) as a PDF document; and (c) overall PCM score in encounter notes. The portal also lacked customizable reminder functions and alerts on fluctuations in patient scores. As such, the provider scheduled reminders to review scores and send articles and questionnaires to patients every 2 weeks.
Data collection
Due to the pandemic, interactions among providers, patients and the research team took place virtually through phone, emails, Zoom meetings and the portal. Publicly available information on the clinic, the regional Division, and the region's community health profile were reviewed to provide the study context.
Initial exploration included a virtual team mapping session 48 with the clinic. This helped the team explore how PCM and the portal could be used with patients living with anxiety and/or depression. Patient personas (simulated cases built from local evidence) were created to guide the discussion (see Supplemental File 3 for an overview of the steps involved in team-mapping). The 2-hour team-mapping session was recorded, and a summary document was provided to the clinic. A follow-up session involved reviewing the team-mapping outputs with the clinic to demonstrate how they could work together, and how PCM could be used to inform practice for patients with mental health concerns.
Also included in the discussion were the patient portal used in the study, different quality improvement support options available from the regional Division, and gaps and priorities identified by the care team. From the sessions, a number of new roles and tasks were identified for care team members, patients and the PCM tool. Workflows were created to illustrate these roles and tasks and were used as prompts during follow-up interviews with the care team members. Through this process, a clinician was identified as the primary contact who we worked closely with in preparing for the portal trial. We also worked closely with our industry partner in determining what currently was possible in the portal that could address workflow concerns.
Following these sessions, patients and providers used the portal over a four-month period. During the portal trial period, we continued to work with providers in the iterative development of workflows focused on distinct activities for integrating PCM into routine practice. We also conducted virtual one-on-one interviews with provider and patient participants to learn about their perceptions, preferences, and concerns related to the integration of PCM. Two researchers co-facilitated and recorded separate summary notes of the interviews.
Data analysis
Our qualitative analysis involved a process of systematic text condensation, in which we looked across the multiple forms of data to get an overall sense of the whole.49 One researcher proposed preliminary themes based on the data.49 A codebook (see Supplemental File 4) was created with the research team which consisted of codes for preliminary themes and context. One researcher coded the interview summary notes through AtlasTi, and coding reports and original data were reviewed by two additional research team members. PCM data collected through the patient portal were compared with the information disclosed through patient and provider interviews. Three researchers looked across coded interview data, team mapping report and workflow diagrams to further develop the themes. The process of reflection within the team involved developing new workflow diagrams, iterative writing, and collating data in PowerPoint to assist discussion during monthly research team meetings. Recognizing that we had a limited sample size, we also brought in existing theories that could inform the conceptualization of our PCM methods.50 Through these multiple processes, the team transformed the preliminary themes into PCM methods that could communicate a credible, full story.49
Results
We met with the clinic through one team-mapping session, one follow-up group session and one to three individual interviews (see Supplemental File 5 for team mapping output on one persona). Four workflows were created with the clinic to understand the different processes, activities, and digital tools that could be used for PCM with their team,38 and a workflow was created during the end-of-study analysis (see Supplemental File 6 for the workflow diagram). Three patients used the portal for the full trial period, and one patient stopped using the portal after 3 months. The three patients consistently completed the measures that were sent out each week and referenced specific sections of the weekly educational resources during the interviews.
Through our qualitative analysis, we identified five areas focused on PCM use and integration. These are (a) Identifying Team's Roles and Responsibilities; (b) Aligning Care Team Activities with Current Resources; (c) Accessing Multiple Digital Tools; (d) Advancing Team-based Care through Existing Databases and (e) Representing Patients’ Values and Perspectives. We conceptualized five new PCM methods based on these five key areas (a) PCM Team mapping; (b) Longitudinal Care Alignment; (c) Digital Tool Exploration; (d) Team-based Quality Improvement and (e) Shared Learning.
The next sections provide an overview of the five areas that informed the creation of these five PCM methods for team-based care. Each section ends with an illustration and a table to detail the techniques and concepts within the proposed PCM method. Supplemental File 7 provides an audit trail on the data sources and theoretical frameworks which informed the development of the five methods.
Identifying team's roles and responsibilities
We initially defined the care-team members as patients, family members, providers (i.e., staff and clinician) and analysts. However, we expanded our definition after one patient emphasized the importance of bringing peers into their circle of care in understanding the lived experience of illness.
From the team mapping session, a number of new roles and responsibilities were identified for the team in using the PCM tool/portal. For the nurse, they were to monitor and triage the PCM results. Patients’ roles included: completing PCMs at home and reviewing their results. The analysts were tasked with collecting and analyzing PREMs, supporting the care-team in reviewing patient feedback, and facilitating quality-improvement cycles. Desired portal features for PCM included showing trends, alerting significant changes and description of providers’ roles. Key findings from the team mapping included (a) the clinic had limited capacity to take on quality improvement or practice change initiatives and (b) the nurse was best suited to monitor PCM via the portal as long as it was made clear the responses would only be reviewed during clinic working hours.
During the interviews, providers reiterated the need for a team-support role to tailor relevant online resources for patients, monitor their PCM data, and follow up with them as needed. One provider commented they saw few patients for chronic care and only had occasional follow-up calls, suggesting their team role was underutilized. Patients mentioned they were not aware of what roles the nurse and social worker played in relation to their care. One patient reiterated the need for tailored descriptions of provider roles.
Our first proposed PCM method is based on the importance of identifying team's roles and responsibilities when introducing PCM into team-based care. Figure 1 and Table 1 detail this first proposed method, PCM Team-Mapping.
Figure 1.
Patient-centered measurement (PCM) team-mapping method.
Table 1.
Patient-centered measurement (PCM) team-mapping method.
| Description: Provides clarity of care team roles and responsibilities, where the team consists of patients, providers (i.e.,, staff and clinicians) and analysts, and may extend to family members, community members and peers. | |
| Possible Tools and Resources: Mind mapping tools 51, team-mapping tools 48, personas 48, trained facilitator 48, group interviews 52, community resources 48, community health profile 53, PCM best practice guidance 54 | |
| Leads the team1 through mapping exercise(s) to: | |
| |
| |
| |
| |
| |
Aligning care team activities with current resources
The limited time and resources of the clinic influenced how PCMs were being used. Patient participants recognized rural resources were often limited (e.g., counselling), and were aware of the time and resource constraints of the providers. Under their current fee-for-service funding model, physicians described feeling pressed for time. As such, their focus was mostly to address the patient's current clinical concern during a visit. They suggested that if PCM data were readily available, they would review PCM scores but not individual responses or trends. Other care-team members preferred a more longitudinal view to help create patient-specific care plans but recognized the need for workflow adjustments. The clinic also had to consider the timing and process for deploying a PCM and sending reminders for incomplete measures.
The use of PCM was also influenced by contextual factors. Different ways of conducting the visit (in-person or virtual) and collecting the PCM data (i.e., through the portal or paper) influenced how the PCM would be viewed and potentially discussed during a visit. The purpose of a visit also played a critical role in whether or not a PCM was viewed by the physician. Most patient participants had appointments for medication renewals or follow-up care for another health condition, and their PCMs were not discussed at these visits. One physician indicated to patients that they would review the PCMs during the annual mental health visit. The reason for deploying the PCM (i.e., for an upcoming visit, for ongoing monitoring, or patient-initiated for self-care) also impacted how the PCM was shared.
To align care time activities with current resources, our second proposed method is focused on the ‘why’, ‘when’, ‘where’, ‘how’ and ‘who’ in aligning PCM to care-team activities. Figure 2 and Table 2 introduce this second PCM method of Longitudinal Care Alignment, which considers timing and context of different care activities for ongoing use of PCM in day-to-day practice and for team-patient interactions.
Figure 2.
Longitudinal care alignment method.
Table 2.
Longitudianl care alignment method.
| Description: Offers guidance for the care team on incorporating patient-centered measurement (PCM) into day-to-day practice, during care team member–patient interactions, and for longitudinal care. | |
| Possible Tools and Resources: Workflow diagramming tools 55, mind mapping tools 51, PCM best practice guidance 54, interviews 52 | |
| Is focused on the following questions: | |
| Why |
|
| When |
|
| Where |
|
| How |
|
| Who |
|
Accessing multiple digital tools
The pandemic led to greater use of digital tools by the team in the form of email communications and virtual visits, which added to the complexity of care delivery. The technologies included the standalone portal, clinic EMR, external data repositories, web-based online resources, virtual meeting tools and computers, Smartphones or landline phones. The sudden transition to remote visits meant that both providers and patients could potentially view the completed measures together through their computer screens. However, none of the patients considered logging into the portal prior to the clinic visit. One patient mentioned how they were less likely to accurately report PCM scores during an in-person visit, as they were often deployed in public settings such as waiting rooms. A virtual waiting room offered a new possibility for patients to complete measures in less public spaces. An example of new opportunities for digital tools was also introduced when a patient spoke about a virtual visit with a resident doctor. As this provider was not a study participant, they did not know where to look in the EMR for the Patient Health Questions-9 (PHQ-9) score. The resident suggested to the patient that they both ‘Goggle’ the measure, which enabled them to talk through each question before deciding on a medication change.
The lack of interoperability across the portal, EMR and broader technologies was frequently mentioned. Although one provider simulated linkage between the portal and EMR, they commented that the effort was not scalable or sustainable after the study ended. There was also a lack of interoperability for services outside of the clinic. The regional health authority had its own tethered portal for patients living in that region that was not integrated with the clinic EMR or the standalone portal used in the study. As services were not available locally, patients were referred to specialists outside of their health authority. One patient expected PCMs would be discussed during care visits and readily shared with providers outside of the clinic. This patient stopped completing the measures near the end of the study. During the interviews the patient mentioned the severity of their illness, being online impacting their chronic pain, and disappointment in not having PCM discussed during their care visits.
Our third proposed method explores the impact of multiple digital tools being introduced to support care encounters. Figure 3 and Table 3 detail this PCM method of Digital Tool Exploration in assessing the impact and readiness for digital tools introduced through PCM and virtual care.
Figure 3.
Digital tool exploration method.
Table 3.
Digital tool exploration.
| Description: Takes into account different types, stages, ranges and levels of technology, in assessing patient's and providers’' readiness toward adoption of digital tools, and the impact of these tools on patient-centered measurement (PCM) adoption. | |
| Possible tools and resources: Electronic medical record, patient portal, mobile technologies, phone, virtual meeting tools, external database repositories 57,58, digital health best practice guidance 54 | |
| Involves evaluating: | |
| Readiness |
|
| Impact |
|
Advancing team-based care through existing databases
Through discussions with our collaborators and providers, we found multiple population-level quality-of-care initiatives that could translate to PCM. For example, panel management involves cleaning EMR data in order to run queries to identify and proactively manage specific patient populations.60 PCM could potentially be integrated into this panel as a way to track significant changes in scores for patients diagnosed with a mental health condition. We discussed how a query could be used to identify and screen patients for changes in mental health, especially if they had high PHQ-9 or GAD-7 scores. However, we found that the different preferences for where to store the PCM score in the EMR made the cleaning of these data challenging for panel management, which was in the early adoption stages. One physician had cleaned up his panel for mental health but did not reference any queries. When we discussed the local community health profile as a possible source for identifying queries to run, the physician thought it was a good idea, but did not know how to take the next step for more advanced analytics.
We also discussed two ongoing initiatives focused on quality improvement, Canadian Primary Care Sentinel Surveillance Network (CPCSSN) 57 and the BC Health Data Coalition.58 Both expanded a panel beyond a single provider and involved EMR data being extracted and loaded into database repositories for analysis and comparison with other clinics across the region. However, the value of these databases was questioned by the physicians since data within one of the repositories, although cleaned, was typically six months old. Although the other platform allowed immediate data extraction, there was no comparable data cleaning available.
Efficiency was a common term used by physicians when asked about these different initiatives. They found that current quality improvement initiatives did not translate to their day-to-day practice. The lack of reimbursement codes for PCM data collection further discouraged integration. There were also the questions of ‘so-what’ and ‘when is good enough, good enough?’. The physicians suggested the additional resources to help with population screening would be too costly to ‘deliver perfect healthcare to everyone’, and questioned whether these initiatives are truly empowering for a patient when it is the clinic identifying when a patient may need care.
In BC, panel management is described in three phases: empanelment, panel clean-up and panel optimization (access to updated data).60 What we heard was distinctly missing in these phases were the steps required to understand how to proactively manage the panel. Discussions with quality improvement professionals from the region revealed that while they were there to support the clinic, they would need to know the state of the empanelment, be familiar with the different EMRs being used in the region, and understand how the clinic would like to make use of patient panel queries (e.g., which patient populations and issues to focus on). Periodic ‘data parties’ for clinics were offered to discuss the value of certain quality measures and what was best practice. However, one physician found that even after this training, the queries took extensive time as often the provider had to relearn the system. Although team members understood some of the basic analytics, they had not been trained to conduct the necessary advanced EMR data analysis.
Our fourth proposed PCM method is focused on evaluating quality improvements introduced through team-based care, and whether the team itself is being successful in these endeavours. Figure 4 and Table 4 detail this PCM method on Team-based Quality Improvement, which is focused on population-level data sources for improving the quality of team-based care.
Figure 4.
Team-based quality improvement method.
Table 4.
Team-based quality improvement method.
| Description: Applies expanded data sources and quality measures focused on improving care team performance and provider–patient interactions. Based on the Plan-Do-Study-Act Quality Improvement Framework 54,59,61 and Integrated Knowledge to Action Framework 62. | |
| Possible Tools and Resources: EMR, patient portal, database query tools 57,58, PCM best practice guidance 63, community health profiles 53 | |
| The following stages may be revisited as the team learns more: | |
| Team Context |
|
| PCM Context |
|
| Evaluation |
|
| Knowledge mobilization |
|
PCM: patient-centered measurement; EMR: electronic medical record.
Representing patients’ values and perspectives
‘Validation’ was a common term used by patients when asked about completing the measures. Specifically, PCMs provided opportunities for checking in with oneself, feeling more confident to seek support, self-learning, and to focus and identify the priority health issue. This was demonstrated by the patient who walked through the PHQ-9 with the resident and described it as ‘unexpectedly rewarding and validating … and quintessential learning … for the doctors in understanding’. It allowed them to use the language of providers and ‘to be on the same page’, and when walking through the measures together, they felt it changed the decision on medication choice. Yet in the next visit, a different resident did not offer any suggestion other than to book an appointment. The patient felt that they were back to square one in not knowing where to begin.
Although one patient remarked that the questionnaires and online resources did not offer anything new, they found the information ‘absolutely important and I use it every day’. One patient found the ‘questions in measures probe different things that I am aware impact me’, and used the example of their sudden weight loss, which may not have been picked up in a visit (even more relevant in a virtual visit). Patients appreciated being able to complete multiple measures, as it gave different insights into their illness. For example, one patient referenced the PROMIS self-efficacy when they said focusing in ‘on self-confidence is huge as I find this to be a difficult aspect of the disease’, while the PHQ-9 and GAD-7 made them realize the distinction between the two realms, and that they wanted to better understand their anxiety.
The provider who oversaw the distribution of information sources was new to the clinic and did not know the patients well enough to send customized information and thus the resources did not always connect with patients. Patients found it equally valuable to have access to tailored online resources. When asked about completing open-text measures one patient mentioned how ‘it allowed me to see where I am at, acknowledging the depression when you put it down in the action plan’. Resources that offered personal stories were valued for providing motivation through the ‘voice’ that is often needed to make significant changes for oneself and others. In the past, the patient had offered to collate relevant information and make it available at the clinic. They saw the potential of the portal to support a peer network, in which patients could share illness experiences and develop a programme that takes action. The doctor said he was being ‘visionary’, with both knowing that ‘it was the next step to make best medical help available in this town and acknowledging the importance of lived experience’.
One provider offered an example of when they applied judgment after noticing a sudden change in score and called the patient to suggest follow up. However, that provider also indicated that they had no formal education on interpreting PCM scores and had to determine how to evaluate the measures by doing an online search. This highlights a potential opportunity for a PCM portal in which educational resources are expanded to patients and providers and focused on interpreting PCM scores and trends.
Our fifth proposed method is focused on this concept of validation that was introduced by patients, in providing opportunities for patients to have their perceptions of their health and illness recognized, valued and acknowledged. Figure 5 and Table 5 details the final PCM method of Shared Learning, which is informed by patients’ self-validation of their health issues. Most significantly, the learning is not unidirectional, but a shared process that align with patients’ values and context with current healthcare needs and strategies.
Figure 5.
Shared learning method.
Table 5.
Shared learning method.
| Description: Promotes provider–patient interactions and engagements that are guided by PCM as the basis for patient's self-validation of health issues, and team's valuing of what matters most to patients. It involves using PCM to encourage opportunities for the team to identify, connect, evaluate and understand in aligning with the patient's values, context and health status. | |
| Possible tools and resources: EMR, patient portal, PCM outputs, community and educational resources 41, PCM interpretation guidance,43,44,63 PCM follow-up actions | |
| Involves the four actions | |
| Connect |
|
| Evaluate |
|
| Understand |
|
| Identify |
|
PCM: patient-centered measurement; EMR: electronic medical record.
Discussion
In this study, we conceptualized five virtual team-based PCM methods in the PMH context. They were (a) PCM Team Mapping, (b) Longitudinal Care Alignment, (c) Digital Tool Exploration, (d) Team-based Quality Improvement, and (e) Shared Learning. Application of these five methods is further illustrated by a series of scenarios and videos provided on our web site.62 Working with patients and providers broadened our understanding of PCM methods beyond issues of EMR integration.63–65 Our proposed PCM methods complement many of the attributes identified by Weir et al. 66 in their study on contextual information in the electronic health record design for team-based care. We offer ways that PCM can be integrated into digital tools and team roles and responsibilities, so that information is useful, timely, context-specific, valuable, and matches with the team members’ goals.66
Through PCM Team Mapping, we identified new activities for the nurse to initiate, monitor, and triage PCM data collection and use. The discussion helped providers understand how PCM could be incorporated into their practice and workflow. The decisions are consistent with current shifts in PMH in introducing new team roles for nurses, social workers and other health professionals.67–71 Our PCM method on Longitudinal Care Alignment highlighted temporal and technological considerations for a team to incorporate PCM into their day-to-day practice and for ongoing team interactions. Our PCM method on Digital Tool Exploration recognized the varying levels of patients and providers’ technology readiness that could affect the extent to which PCM would be incorporated into routine practice. These findings are consistent with the experiences and lessons of leading organizations in PCM implementation, use and evaluation.16,54
Two of our methods focus on PCM's aim in improving the quality of care, in which patients’ values and perspectives are represented in decision-making. The method of Team-based Quality Improvement offers a framework for engaging teams in patient-centered quality improvement. Quality improvement initiatives through team-based panel management or PCM have demonstrated only small, incremental change to services and unclear impacts.9 To facilitate meaningful quality of care improvement requires dedicated time, professional development, mentorship, engaged leadership, ongoing organizational support, and a shift away from fee-for service.72–74 There is also a need for developing team-dedicated resources on clinical information technologies that support teams in shared decision-making.72 The findings that informed our PCM Shared Learning method were also similar to Reis’ et al. 33 study, where patients preferred a collaborative, problem-solving partnership but recognized boundaries for what additional support they wanted from their providers. The systematic review by Lordon et al. 75 also found that patients desired their providers to be applying their PCM data, yet providers had differing options in how active their role should be in viewing these data.
The shift to virtual care due to the pandemic has introduced an unprecedented opportunity to reinvent PCM-informed care in creative ways. However, the repeated reference to efficiency that we heard during the study underscores the importance of being mindful of potential burnout 76 when additional tasks for PCM are added, without a change in resources for workflows. We also heard from patients that they were aware of the extensive workload of providers, and as such appreciated that the portal tools offered a place for validation. We aim to address these different values by offering multiple methods for the integration and use of PCM that illuminate different values and perspectives and readiness within the care-team.
Limitations
To further understand the current implications of the proposed PCM methods on team-based care, Table 6 provides a summary of strengths and current gaps. There were also limitations in our study design. The study site was a rural practice with a small care-team and few patient participants, which may not be representative of larger clinics or other rural settings. No audios were recorded for the interviews. To minimize any inconsistencies, two researchers took notes during the interviews recorded in the collated summary when they had different interpretations. The study was conducted during the pandemic which made the recruitment of patients particularly challenging. The portal was utilized for four months with limited functionality.
Table 6.
Practice and research implications of the proposed patient-centered measurement (PCM) method.
| Strengths: |
|
| Current gaps: |
|
Malterud's et al. 50 concepts of information power demonstrates how we addressed the smaller sample size and limitations of our study, in considering specificity of experiences, scope, analysis strategy, quality of dialogue and application of theory. For specificity of experiences, not all of the patients identified with their mental health diagnosis and did not have the opportunity to use the portal during their clinic visit. In addition, the clinic's adoption of the PMH model was relatively recent, so had limited experience in working as a team. Our aim was also relatively broad in scope in looking to conceptualize PCM methods within team-based care. As the measures were focused on mental health, further research is required to evaluate the transferability of the PCM methods to other health domains.
To address the limitations in our information power, we collected and analyzed across multiple forms of data for a single case. The richness of our data was obtained by conducting multiple interviews with the patient participants where we built rapport over time, and based on their feedback sequentially introduced different forms of PCM and educational resources into the portal. In developing the PCM methods, we also looked to existing theories and literature that fit well with our data.50
Conclusion
The adoption of PMH in primary care provided an opportunity to conceptualize team-based PCM methods in new ways. We conceptualized five different approaches that can be used to optimize the use of PCM and help advance patient-oriented research and patient-centered care in the PMH context, especially for resource-limited settings. The introduction of the portal illuminated new methods for the integration of PCM in team-based care. The first three proposed PCM methods offer different ways of assessing clinic resources and roles for incorporating PCM methods into team-based care. Methods four and five are focused on the aim of patient-generated data in which patients’ values and perspectives are represented in their care decision, and the team's quality of care is evaluated through a patient-centered lens. Further research is needed to assess the transferability and utility of these methods in different clinical settings and health domains.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-2-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-3-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-4-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-5-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-6-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-7-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Acknowledgments
The study was conducted during the pandemic when all of us were being impacted by changing healthcare resources. We want to extend our thanks to all the patient and provider participants who shared their insights over the course of the study, to our collaborators at the Kootenay Boundary Division of Family Practice and our industry partner Cambian Business Services Inc.
Appendix
EMR: electronic medical record
GAD-7: General Anxiety Disorder-7
PCM: patient-centered measurement
PES: Patient Experience Survey
PGHD: Patient-generated health data
PHQ-9: Patient Health Questions-9
PMH: Patient's Medial Home
PREMs: Patient-reported experience measures
PROMIS: Patient-Reported Outcomes Measurement Information System
PROMs: Patient-reported outcomes measures
Footnotes
Contributorship: MA and FL drafted the manuscript, and all co-authors reviewed it. MA and FL created the tables. MA created the figures in the main document. MS provided domain expertise in developing method four and wrote the different scenarios. MA was involved in gaining ethics approval, recruiting patients, coordinating all team and clinic meetings, and coding of interviews transcripts. MP and SF facilitated the team mapping session. SD and MA conducted the patient and clinic participant interviews. SD developed the workflow diagrams. FL, MS and MA analyzed the data in developing the methods and scenarios. MS and PB were our patient partners on the grant. DL provided domain expertise on electronic patient-reported outcomes. All authors were part of the funding grant that supported the development of the five methods. All authors gave approval of the submitted manuscript and agreed to be accountable for ensuring the integrity of the manuscript.
Data availability statement: De-identified data from the study in form of workflow diagrams have been provided in another paper.38 The interview data generated during the current study cannot be shared publicly in order to maintain the privacy of individuals that participated in the study.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: The study had institutional ethics board approvals (BC20-0087 and H19-03855).
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided by The BC SUPPORT (Support for People and Patient-Oriented Research and Trials) Unit Methods Cluster on Patient-Centered Measurement (grant #PCM 003).
Guarantor: MA.
Informed consent: All participants completed an online consent form.
ORCID iDs: Marcy G Antonio https://orcid.org/0000-0001-9332-8512
Selena Davis https://orcid.org/0000-0003-4542-3341
Supplemental material: Supplemental material for this article is available online.
References
- 1.Black N. Patient reported outcome measures could help transform healthcare. Br Med J 2013; 346: f167. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd H, Wheat H, Horrell J, et al. Patient-reported measures for person-centered coordinated care: a comparative domain map and web-based compendium for supporting policy development and implementation. JMIR 2018; 20(2): e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlesinger M, Grob R, Shaller D. Using patient-reported information to improve clinical practice. Health Ser Res 2015; 50(Suppl 2): 2116–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen DJ, Keller SR, Hayes GR, et al. Integrating patient-generated health data into clinical care settings or clinical decision-making: lessons learned from project HealthDesign. JMIR Hum Factors 2016; 3(2): e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell P, Wynia M, Golden R, et al. Core principles & values of effective team-based health care. Discussion Paper, Institute of Medicine, NAM Perspectives, https://nam.edu/wp-content/uploads/2015/06/VSRT-Team-Based-Care-Principles-Values.pdf (2012, accessed 05 October 2021).
- 6.Cheng F, Waddell K, Wilson MG. Rapid synthesis: determining the features of person-centered models of care that patients value. Hamilton, Canada: McMaster Health Forum, 29 March 2018, http://hdl.handle.net/11375/23789 (2018, accessed 17 September 2021).
- 7.Desomer A, Van den Heede K, Triemstra M, et al. Use of patient-reported outcome and experience measures in patient care and policy. Health Services Research (HSR). Brussels: Belgian Healthcare Knowledge Centre (KCE), https://www.nivel.nl/sites/default/files/bestanden/KCE_use_of_PROM_PREM.pdf? (2018, accessed 05 October 2021).
- 8.Ishaque S, Karnon J, Chen G, et al. A systematic review of randomised controlled trials evaluating the use of patient-reported outcome measures (PROMs). Qual Life Res 2019; 28: 567–592. [DOI] [PubMed] [Google Scholar]
- 9.Gleeson H, Calderon A, Swami V, et al. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open 2016; 6: e011907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boyce MB, Browne JP, Greenhalgh J. The experiences of professionals with using information from patient-reported outcome measures to improve the quality of healthcare: a systematic review of qualitative research. BMJ Qual Saf 2014; 23: 508–518. [DOI] [PubMed] [Google Scholar]
- 11.Bastemeijer CM, Boosman H, van Ewijk H, et al. Patient experiences: a systematic review of quality improvement interventions in a hospital setting. Patient Relat Outcome Meas 2019; 10: 157–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Field J, Holmes MM, Newell D. PROMs data: can it be used to make decisions for individual patients? A narrative review. Patient Relat Outcome Meas 2019; 10: 233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster A, Croot L, Brazier J, et al. The facilitators and barriers to implementing patient reported outcome measures in organizations delivering health related services: a systematic review of reviews. JPRO 2018; 2: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basch E, Babera L, Kerrigan CL, et al. Implementation of patient-reported outcomes in routine medical care. Am Soc Clin Oncol Educational Book 2018; 23:38: 122–134. [DOI] [PubMed] [Google Scholar]
- 15.Snyder C, Wu AW. (eds) Users’ guide to integrating patient-reported outcomes in electronic health records. Baltimore, MD: Johns Hopkins University. Funded by Patient-Centered Outcomes Research Institute (PCORI), https://www.pcori.org/document/users-guide-integrating-patient-reported-outcomes-electronic-health-records (2017, accessed 17 Sep 2021).
- 16.International Society for Quality of Life Research (prepared by Aaronson N, Elliott T, Greenhalgh J, et al. User’s guide to implementing patient-reported outcomes assessment in clinical practice Version 2, https://proms.waitematadhb.govt.nz/assets/Uploads/Implementing-PROMs-in-Clinical-Practice.pdf (2015, accessed 17 September 2021).
- 17.Chan EH, Edwards TC, Haywood K, et al. Implementing patient-reported outcome measures in clinical practice: a companion guide to the ISOQOL user’s guide. Qual Life Res 2019; 28: 621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramsey D, Seth P. Me to we: introducing collaborative elements in the electronic record. BCMJ 2017; 59(10): 507–511. [Google Scholar]
- 19.The College of Family Physicians of Canada. Summary of a new vision for Canada: Family practice - the patient’s medical home. Mississauga, ON: College of Family Physicians of Canada, https://patientsmedicalhome.ca/files/uploads/PMH2019Summary_ENG.pdf. (2019, accessed 17 September 2021).
- 20.Akhtar S, Loganathan M, Nowaczynski M, et al. Aging at home: a portrait of home-based primary care across Canada. Healthcare Q 2019; 22(1): 30–35. [DOI] [PubMed] [Google Scholar]
- 21.Hefford B. The patient medical home: working together to create an integrated system of care. BCMJ 2017; 59(1): 15–17. [Google Scholar]
- 22.Katz A, Herpai N, Smith G, et al. Alignment of Canadian primary care with the patient medical home model: a QUALICO-PC study. Ann Fam Med 2017; 15(3): 230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zutshi A, Peikes D, Smith K, et al. The medical home: what do we know, what do we need to know? A review of the earliest evidence on the effectiveness of the patient-centered medical home model. Agency Healthc Res Pol, 2011; 12(14): 0020-1-EF, https://www.ahrq.gov/sites/default/files/wysiwyg/ncepcr/tools/PCMH/the-medical-home-what-do-we-know.pdf. (2011, accessed 17 Sep 2021). [Google Scholar]
- 24.Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med 2013; 158(3): 169–178. [DOI] [PubMed] [Google Scholar]
- 25.Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. JGIM 2010; 25(6): 601–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The College of Family Physicians of Canada. Patient’s medical home 2019 quick reference, https://patientsmedicalhome.ca/files/uploads/PMH2019_QuickRef_ENG_Final.pdf (2019, accessed 17 September 2021).
- 27.Lemire F. Refreshing the patient’s medical home: new vision for providing exceptional care in family practice. Can Family Physician 2019; 65(2): 152. [PMC free article] [PubMed] [Google Scholar]
- 28.The College of Family Physicians of Canada. A vision for Canada: family practice - the patient’s medical home, https://patientsmedicalhome.ca/resources/past-vision-papers/2011-pmh-vision-paper/ (2011, accessed 17 Sep 2021).
- 29.General Practice Services Committee. System change: patient medical homes, https://gpscbc.ca/what-we-do/system-change/patient-medical-homes (2020, accessed 17 September 2021).
- 30.General Practice Services Committee. The difference: patient medical homes and primary care networks, https://gpscbc.ca/sites/default/files/uploads/GPSC%20Infosheet%20PMHPCN%20Difference.pdf. (accessed 17 Sep 2021).
- 31.General Practice Services Committee. What we do: clinical networks, https://gpscbc.ca/what-we-do/system-change/clinical-networks (2020, accessed 17 September 2021).
- 32.Haesebaert J, Samson I, Lee-Gosselin H, et al. “They heard our voice!” patient engagement councils in community-based primary care practices: a participatory action research pilot project. RIE 2020; 6(54): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reis J, Juker D, Volk M, et al. Patients’ expectations for and experiences with primary healthcare services received from a patient centered medical home. Patient Educ Couns 2020; 103(6): 1223–1229. [DOI] [PubMed] [Google Scholar]
- 34.Aysola J, Schapira MM, Huo H, et al. Organizational processes and patient experiences in the patient-centered medical home. Med Care 2018; 56(6): 497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wen J, Schulman KA. Can team-based care improve patient satisfaction: a systematic review of randomized controlled trials. PLoS ONE 2014; 9(7): e100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jaén CR, Ferrer RL, Miller WL, et al. Patient outcomes at 26 months in the patient-centered medical home national demonstration project. Ann Fam Med 2010; 8(Suppl1): S57–S67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murphy P, Burge F, Wong ST. Measurement and rural primary healthcare: a scoping review. Rural Remote Health 2019; 19(3): 4911. [DOI] [PubMed] [Google Scholar]
- 38.Davis S, Antonio M, Smith M, et al. Paving the way for electronic patient-centered measurement in team-based primary health care: an integrated knowledge translation approach. JMIR Form Res 2022; 6(3): e33584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.BC Ministry of Health. A pathway to hope: A roadmap for making mental health and addictions care better for people in British Columbia, 2019, https://www2.gov.bc.ca/gov/content/governments/about-the-bc-government/mental-health-and-addictions-strategy (2019, accessed 17 September 2021).
- 40.Cambian.com. Cambian, https://www.cambian.com/ (no date, accessed 17 September 2021).
- 41.BC Ministry of Health. BC Guideline.ca: depression resource guide for patients, https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/depression_resource_guide_patients.pdf (2013, accessed 17 September 2021).
- 42.AAFP.org. Depression self-action plan adapted from Amann, https://www.aafp.org/dam/AAFP/documents/patient_care/nrn/depression-self-care-action-plan.pdf (no date, accessed 17 September 2021).
- 43.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16(9): 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spitzer RL, Kroenke K, Williams JBWet al. et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 45.Ader DN. Developing the patient-reported outcomes measurement information system (PROMIS). Med Care 2007. 45(5), 1–2. [Google Scholar]
- 46.PROMIS Health Organization. PROMIS self-efficacy - short Form, https://www.healthmeasures.net/explore-measurement-systems/promis. (2017, accessed 17 September 2021).
- 47.Divisions of Family Practice - Kootenay Boundary. Kootenay Boundary patient experience survey (KB-PES), https://divisionsbc.ca/kootenay-boundary/patient-experience-survey (2019, accessed 17 September 2021).
- 48.Price M, Bellwood P, Hill TT, et al. Team mapping: a novel method to help community primary healthcare practices transition to team-based care. Healthc Q 2020; 22(4): 33–39. [DOI] [PubMed] [Google Scholar]
- 49.Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health 2012; 40(8): 795–805. [DOI] [PubMed] [Google Scholar]
- 50.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Heal Res 2016; 26(13): 1753–1760. [DOI] [PubMed] [Google Scholar]
- 51.Burgess-Allen J, Owen-Smith V. Using mind mapping techniques for rapid qualitative data analysis in public participation processes. Heatlh Expect 2010; 13(4): 406–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tritter JA, Landstad BJ. Focus groups. In: Pope C, Mays N. (eds) Qualitative research in healthcare. 4th ed. Oxford: John Wiley and Sons Ltd., 2020, Ch. 5, pp.57–66. [Google Scholar]
- 53.Bazemore AW, Cottrell EK, Gold R, et al. "Community health vital signs": incorporating geocoded social determinants into electronic health records to promote patient and population health. JAMIA 2016; 23: 407–410. [DOI] [PubMed] [Google Scholar]
- 54.LeRouge C, Austin E, Lee J, et al. ePROs in clinical care: guidelines and tools for health systems, https://epros.becertain.org/tools-resources/resources/printable-toolkit (2020, accessed 19 September 2021).
- 55.University of North Carolina Institute for Healthcare Quality Improvement. Process mapping, https://www.med.unc.edu/ihqi/resources/process-mapping/ (2022, accessed 11 October 2021).
- 56.Hinton S, Ryan S. Interviews. In: Pope C, Mays N. (eds) Qualitative research in healthcare. 4th ed. Oxford: John Wiley and Sons Ltd., 2020, Ch. 4, pp.43–55. [Google Scholar]
- 57.Canadian Primary Care Sentinel Surveillance Network (CPCSSN). Welcome to CPCSSN, https://cpcssn.ca/ (2021, Accessed 17 September 2021).
- 58.Health Data Coalition (HDC). Welcome to the health data coalition, https://hdcbc.ca/ (2022, accessed 17 September 2021).
- 59.Agency for Healthcare Research and Quality. Evaluation toolkit. Version 3, https://www.infoway-inforoute.ca/en/component/edocman/996-evaluation-toolkit/view-document?Itemid=101 (no date, accessed 11 October 2021).
- 60.General Practice Services Committee (GPSC). System change: panel management, https://gpscbc.ca/what-we-do/system-change/panel-management (2020, accessed 17 September 2021).
- 61.Langley GL, Moen R, Nolan KM, et al. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Francisco: Jossey-Bass Publishers, 2009. [Google Scholar]
- 62.Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? JCEHP 2006; 26(1): 13–24. [DOI] [PubMed] [Google Scholar]
- 63.UMHS Depression Guideline. PHQ-9 questionnaire for depression scoring and interpretation guide, https://www.med.umich.edu/1info/FHP/practiceguides/depress/score.pdf (accessed 11 October 2021).
- 64.Agency for Healthcare Research and Quality. Health literacy universal precautions toolkit, 2nd edition: plan-do-study-act (PDSA) directions and examples, https://www.ahrq.gov/health-literacy/improve/precautions/tool2b.html (2020, accessed 11 October 2021).
- 65.University of Victoria. Patient-centred measurement in team-based care, pcmintbc.uvic.ca (2022, accessed 11 October 2021).
- 66.Demiris G, Iribarren SJ, Sward K, et al. Patient generated health data use in clinical practice: a systematic review. Nurs Outlook 2019; 67(4): 311–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tiase VL, Hull W, McFarland MM, et al. Patient-generated health data and EHR integration: a scoping review. JAMIA Open 2020; 3(4): 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wu DTY, Xin C, Bindhu S, et al. Clinician perspectives and design implications in using patient-generated health data to improve mental health practices: mixed methods study. JMIR Form Res 2020; 4(8): e18123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Weir CR, Staggers N, Gibson B, et al. A qualitative evaluation of the crucial information necessray in EHR design to support patient-centered medical home care. BMC Medical Inform 2015; 15(30): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bauer L, Bodenheimer T. Expanded roles of registered nurses in primary care delivery of the future. Nurs Outlook 2017; 65(5): 624–632. [DOI] [PubMed] [Google Scholar]
- 71.Conrad D, Alfredson K. Expanding the primary care patient-centered medical home through new roles for registered nurses. JIEP 2016; 5: 59–64. [Google Scholar]
- 72.Fraser MW, Lombardi BM, Wu S, et al. Integrated primary care and social work: a systematic review. J Soc Soc Work Res 2018; 9(2): 179–215. [Google Scholar]
- 73.Howard J, Miller WL, Willard-Grace R, et al. Creating and sustaining care teams in primary care: perspectives from innovative patient centered medical homes. Qual Prim Care 2018; 27(3): 123–129. [DOI] [PubMed] [Google Scholar]
- 74.Ashcroft R, McMillan C, Ambrose-Miller W, et al. The emerging role of social work in primary healthcare: a survey of social workers in Ontario family health teams. Health Soc Work 2018; 43(2): 109–176. [DOI] [PubMed] [Google Scholar]
- 75.McGough P, Chaudhari V, El-Attar S, et al. A health system’s journey toward better population health through empanelment and panel management. Healthcare 2018; 6(2): 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shaikh U, Lachman P, Padovani AJ, et al. The care and keeping of clinicians in quality improvement. Int J Qual Health Care 2020; 32(7): 480–485. [DOI] [PubMed] [Google Scholar]
- 77.Shukor AR, Edelman S, Brown D, et al. Developing community-based primary healthcare for complex and vulnerable populations in the Vancouver Coastal Health Region: healthConnection clinic. Perm J 2018; 22: 18–010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lordon RJ, Mikles SP, Kneale L, et al. How patient-generated health data and patient-reported outcomes affect patient-provider relationships: a systematic review. Health Informatics J 2020; 26(4): 2689–2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine (Baltimore) 2018; 97(38): e12319. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-2-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-3-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-4-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-5-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-6-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health
Supplemental material, sj-docx-7-dhj-10.1177_20552076221145420 for Advancing digital patient-centered measurement methods for team-based care by Marcy G Antonio, Selena Davis, Mindy Smith, Paul Burgener, Morgan Price, Danielle C Lavallee, Sarah Fletcher and Francis Lau in Digital Health