Abstract
Proximal interphalangeal joint (PIPJ) arthrodesis is a salvage option in the management of end-stage PIPJ arthropathy. Numerous techniques have been described, including screws, Kirschner wires, tension band wiring, intramedullary devices, and plate fixation. There remains no consensus as to the optimum method, and no recent summary of the literature exists. A literature search was conducted using the MEDLINE, EMBASE, and PubMed databases. English-language articles reporting PIPJ arthrodesis outcomes were included and presented in a systematic review. Pearson χ2 and 2-sample proportion tests were used to compare fusion time, nonunion rate, and complication rate between arthrodesis techniques. The mean fusion time ranged from 5.1 to 12.9 weeks. There were no statistically significant differences in fusion time between arthrodesis techniques. Nonunion rates ranged from 0.0% to 33.3%. Screw arthrodesis demonstrated a lower nonunion rate than wire fusion (3.0% and 8.5% respectively; P = .01). Complication rates ranged from 0.0% to 22.1%. Aside from nonunions, there were no statistically significant differences in complication rates between arthrodesis techniques. The available PIPJ arthrodesis techniques have similar fusion time, nonunion rate, and complication rate outcomes. The existing data have significant limitations, and further research would be beneficial to elucidate any differences between techniques.
Keywords: proximal interphalangeal joint, arthrodesis, systematic review
Introduction
The proximal interphalangeal joint (PIPJ) plays an important role in facilitating optimal finger dexterity, grip strength, and overall hand functionality. Proximal interphalangeal joint arthritis (often secondary to degenerative, inflammatory, or traumatic pathology) therefore may result in significant pain and functional impairment. Arthrodesis remains the main salvage option for end-stage PIPJ arthritis and is particularly useful in cases of joint instability, deformity, or deficient bone stock, which are generally not amenable to arthroplasty, and in younger patients where PIPJ arthroplasty may be inappropriate. 1 Although arthrodesis sacrifices joint mobility to achieve stability, this is often a necessary compromise to optimize hand function. 2 Other less common indications for PIPJ arthrodesis include Dupuytren disease and contractures secondary to pathologies such as cerebral palsy. 3
Several PIPJ arthrodesis techniques have been described and can be broadly categorized into screws, plates, and wires. Each technique has inherent advantages and disadvantages. A compression screw, for example, has a relatively simple insertion technique and may achieve a strong compressive force. 4 However, screws may provide inadequate purchase on the distal fragment particularly with fusion angles less than 30°. Plates achieve excellent fixation and are increasingly low-profile and unobtrusive; however, their use may result in extensor tendon adhesion, limiting distal interphalangeal joint (DIPJ) mobility. 5 Although tension band wiring is reliable, cost-effective, and allows early hand mobilization, this technique may require subsequent hardware removal due to pin protrusion. 6
A number of studies have described these techniques and the associated outcomes; however, there remains no summary of the reported results and comparison of the relative approaches, nor a consensus regarding the optimal method of fusion. This systematic review aims to summarize and compare the differing techniques for PIPJ arthrodesis, focusing primarily on union and complication rates.
Methods
Search Strategy and Study Selection
This systematic review was performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. The literature search was conducted using the MEDLINE, EMBASE, and PubMed databases from their inception through to February 2020, with search terms including “proximal interphalangeal joint,” “PIPJ,” “fusion,” and “arthrodesis.” A bibliographic review was also performed to identify additional articles.
Included studies were English-language papers reporting fusion times and/or complication rates for PIPJ arthrodesis by any technique. Studies were excluded if they did not report relevant outcomes, did not report isolated PIPJ outcomes, contained nonhuman subjects, or assessed a pediatric (<18 years) population. Conference abstracts and case reports were also excluded.
Data Extraction
Title and abstract screening, full-text screening, and data extraction were performed by 2 independent authors, with conflicts resolved via discussion and senior review. Extracted variables included demographic data (number of patients, number of joints, age, sex distribution, indication for surgery, length of follow-up), operative details (arthrodesis technique), and outcomes (fusion time, complication rate). Functional and biomechanical outcomes were not reported frequently or consistently, and so were not extracted.
The arthrodesis techniques were categorized as screws (including compression screws, interlocking screws, and a tenon method), plates, or wires (including tension band wiring).
Study quality was assessed using the methodological index for nonrandomized studies critical appraisal system, 7 which scores noncomparative studies out of 16 based on 8 criteria and scores comparative studies out of 26 with an additional 5 criteria.
Data Analysis
An independent statistician performed all statistical analyses using version 16 of the Software for Statistics and Data Science (Stata) program. 8 Weighted means were calculated, and comparison of fusion times (using Pearson χ2) and nonunion and complication rates (using 2-sample proportion tests) was performed to calculate z-statistics.
Results
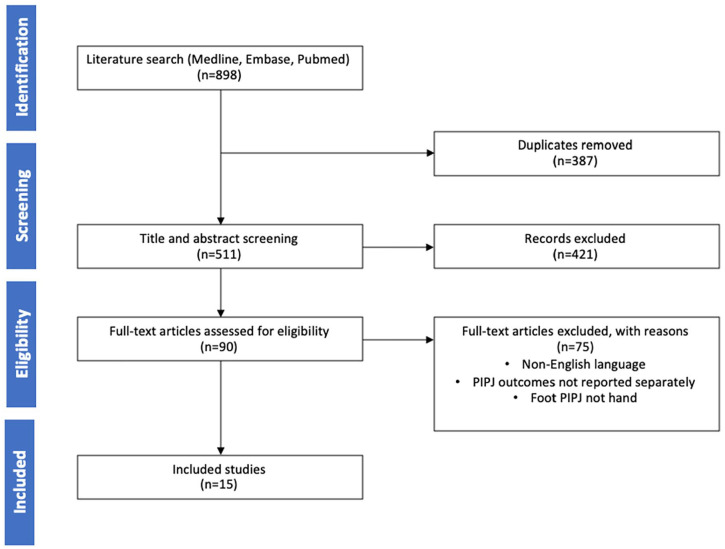
The literature search identified 806 articles. After title and abstract screening and removal of duplicates, 90 studies underwent full-text screening. A total of 154,9-22 studies were ultimately included in the systematic review (Figure 1), comprising 149-22 case series and 14 comparative studies. Common reasons for exclusion were non–English-language papers and studies reporting grouped PIPJ, DIPJ, and metacarpophalangeal joint outcomes.
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses flow diagram for systematic review identifying articles included in this study.
Note. PIPJ = proximal interphalangeal joint.
The 15 included studies contained 286 patients and 608 PIPJ fusions. The weighted mean age was 47.18 years. When reported, men accounted for 40% of patients. The indications for PIPJ arthrodesis included rheumatoid arthritis (n = 253), osteoarthritis (n = 20), trauma (n = 129), psoriatic arthropathy (16), Dupuytren contracture (11), scleroderma (n = 4), and systemic lupus erythematosus (n = 1), and for the remaining cases were not reported. The weighted mean duration of follow-up was 37 months (range, 6-72 months). The mean study quality for the case series was 7 (range, 2-11), and the study quality of the comparative study was 17 (Table 1).
Table 1.
Demographic Characteristics of Included Studies.
| Authors | Study design | Mean age | Male % | Mean follow-up, mo | Study quality |
|---|---|---|---|---|---|
| Ayres et al 9 | Retrospective case series | 52 | Not reported | 14 | 7 |
| Büchler and Aiken 10 | Retrospective case series | 37 | 94 | 15 | 8 |
| Burton et al 11 | Retrospective case series | Not reported | Not reported | Not reported | 10 |
| Granowitz and Vainio 12 | Retrospective case series | 41 | 17 | 50 | 9 |
| Khuri 13 | Retrospective case series | 52 | 50 | 8 | 6 |
| Leibovic and Strickland 4 | Retrospective comparative series | 49 | Not reported | Not reported | 17 |
| Leonard and Capen 14 | Retrospective case series | Not reported | 62 | Not reported | 4 |
| McGlynn et al 15 | Retrospective case series | Not reported | Not reported | Not reported | 6 |
| Novoa-Parra et al 16 | Retrospective case series | 60 | 100 | 20 | 10 |
| Sabbagh et al 17 | Retrospective case series | 54 | Not reported | 72 | 7 |
| Seitz et al 18 | Retrospective case series | 54 | 71 | Not reported | 5 |
| Tan et al 19 | Retrospective case series | 48 | Not reported | 8 | 11 |
| Wright and McMurtry 20 | Retrospective case series | 49 | Not reported | 48 | 9 |
| Lewis et al 21 | Retrospective case series | 51 | Not reported | 6 | 4 |
| Potenza 22 | Retrospective case series | Not reported | Not reported | Not reported | 2 |
Note. Study quality was assessed using the methodological index for nonrandomized studies scoring system.
Fusion Time
The reported fusion times are presented in Tables 2 and 3. Nine studies reported mean fusion time, which ranged from 5.1 to 12.9 weeks. The studies reporting mean fusion time were grouped according to arthrodesis technique, and the median for each group was used for comparison. Screw arthrodesis (2 studies, 41 procedures) had a median fusion time of 8.5 weeks (95% confidence interval [CI], 8-9 weeks), plate arthrodesis (1 study, 4 procedures) had a median fusion time of 12.0 weeks (95% CI, 12-12 weeks), and wire arthrodesis (8 studies, 273 procedures) had a median fusion time of 9.6 weeks (95% CI, 7-12 weeks). Comparison between groups demonstrated no statistically significant difference (P = .08, .11, and .24 for screw vs plate, screw vs wire, and plate vs wire, respectively).
Table 2.
Arthrodesis Outcomes for All Included Papers.
| Authors | Arthrodesis technique | No. of joints | Mean fusion time, wk | Fusion time (other) | Nonunion, % | Complications, % |
|---|---|---|---|---|---|---|
| Ayres et al 9 | Compression screw | 51 | Not reported | 98% at 6 wk | 2.0 | 11.8 |
| Büchler and Aiken 10 | Plate | 25 | Not reported | 92% at 12 wk | 8.0 | 4.0 |
| Burton et al 11 | K-wire | 35 | 9.2 | Not reported | 0.0 | 2.9 |
| Granowitz and Vainio 12 | K-wire | 122 | Not reported | 94% at 6 wk | 6.6 | 22.1 |
| Khuri 13 | Tension band wire | 10 | 7.3 | 20% at 6 wk | 0.0 | 20.0 |
| Leibovic and Strickland 4 | K-wire | 99 | 10 | Not reported | 21.2 | 7.1 |
| Compression screw | 35 | 9 | Not reported | 0.0 | 2.9 | |
| Tension band wire | 66 | 11 | Not reported | 4.5 | 7.6 | |
| Plate | 4 | 12 | Not reported | 0.0 | 0.0 | |
| Other | 7 | 12 | Not reported | 0.0 | 14.3 | |
| Leonard and Capen 14 | Compression | 22 | 7.1 | 40% at 6 wk | 13.6 | Not reported |
| McGlynn et al 15 | K-wire | 28 | 8.1 | 50% at 6 wk | 0.0 | Not reported |
| Novoa-Parra et al 16 | Screw | 6 | 8 | Not reported | 0.0 | 0.0 |
| Sabbagh et al 17 | Harrison-Nicolle peg | 20 | Not reported | Not reported | 5.0 | 10.0 |
| Seitz et al 18 | Compression | 7 | 5.1 | 100% at 6 wk | 0.0 | 0.0 |
| Tan et al 19 | K-wire | 3 | 12.9 | Not reported | 33.3 | 0.0 |
| Wright and McMurtry 20 | Plate | 37 | Not reported | 100% at 6 wk | 0.0 | Not reported |
| Lewis et al 21 | Tenon | 6 | Not reported | 100% at 8 wk | 0.0 | 0.0 |
| Potenza 22 | K-wire | 25 | 6.8 | 88% at 6 wk | 0.0 | Not reported |
Note. K-wire = Kirschner wire.
Table 3.
Arthrodesis Outcomes for Grouped Studies According to Arthrodesis Technique.
| Arthrodesis technique | No. of joints | Median fusion time, wk | Nonunion rate, % | Complication rate, % |
|---|---|---|---|---|
| Screw | 113 | 8.5 | 1.8 | 8.5 |
| Plate | 66 | 12 | 3.0 | 4.0 |
| Wire | 395 | 9.6 | 8.4 | 12.7 |
Nonunion
The reported nonunion rates are presented in Tables 2 and 3. The nonunion rate for screw arthrodesis (113 procedures) was 1.8%, for plate arthrodesis (66 patients) was 3.0%, and for wire arthrodesis (395 procedures) was 8.4%. When compared, the difference in nonunion rate between screw and wire arthrodesis was statistically significant (z-statistic = 2.44, P = .01). The other differences between groups were not statistically significant (z-statistic = 0.55 and P = .58 for screw vs plate, and z-statistic = 1.51 and P = .13 for plate vs wire).
Nine studies reported nonunion rates grouped by underlying diagnosis. The nonunion rate for rheumatoid arthritis was 9.5% (253 procedures), for trauma was 10.9% (129 procedures), for psoriatic arthritis was 25% (20 procedures), and for osteoarthritis and Dupuytren contractures was 0.0% (20 and 11 procedures, respectively).
Complications
The reported complication rates are presented in Tables 2 and 3. For those studies reporting complications, screw arthrodesis (106 procedures) had a complication rate of 8.5%, with 4 dorsal cortex fractures, 3 infections, and 2 cases of long-term pain. Plate arthrodesis (25 procedures) had a complication rate of 4.0%, with 1 infection. Wire arthrodesis (339 procedures) had a complication rate of 12.7%, with 5 infections, 4 cases of malunion, 9 cases of delayed union, 24 cases of hyperextension deformity, and 1 case of intraoperative arterial spasm. Comparisons between groups demonstrated no statistical significance (z-statistic = 0.76 and P = .45 for screw vs plate, z-statistic = 1.17 and P = .24 for screw vs wire, and z-statistic = 1.29 and P = .20 for plate vs wire).
Discussion
This systematic review presents the reported outcomes of common PIPJ arthrodesis techniques and demonstrated a lower nonunion rate for screw arthrodesis than for wire arthrodesis. All other comparisons, including fusion time and complication rates, demonstrated no statistically significant difference between arthrodesis techniques.
The reported outcomes for PIPJ arthrodesis are aligned with those for similar procedures, such as DIPJ arthrodesis—a more common operation with a larger body of existing literature. The reported mean fusion time for DIPJ arthrodesis ranges from 6 to 12 weeks,23-27 and in a large systematic review, Dickson et al 28 reported nonunion rates of 8.4% and 4.0% for Kirschner wire (K-wire) and compression screw arthrodesis, respectively. This difference was statistically significant (P < .01), mirroring the relatively high nonunion rate observed with K-wire arthrodesis in our review. As in our study, Dickson et al found no statistically significant differences in complication rates (namely, infection) between arthrodesis techniques.
The ultimate goal of PIPJ arthrodesis is to optimize hand function, and the clinical outcomes reported in this review are only able to assess part of that objective. Functional outcomes and patient-reported outcome measures have been poorly reported in the literature (not lending to inclusion in this review), but would add valuable information. Although biomechanical parameters are relevant only to the extent that they reflect clinical outcomes, with an absence of long-term patient data laboratory studies may contribute to the comprehensive comparison of arthrodesis techniques. In 1 cadaveric study, Capo et al 29 demonstrated significantly greater stiffness for intramedullary screws and dorsal plates than for all forms of wiring, including K-wires and tension band wiring. In load-to-failure testing (a measure of construct strength and durability), intramedullary screws were significantly stronger than wire and plate arthrodesis. In a similar study of different wire techniques, Kovach et al 30 found superior strength for figure-of-8 tension band wiring than for crossed K-wires or intraosseous wires.
Individual patient factors must also be considered and have implications for the relative advantages and disadvantages of each technique. Importantly, the integrity of the surrounding soft tissue and the bone stock and quality may vary significantly among the common indications for arthrodesis. Although osteoarthritis and traumatic injury often spare the soft tissue structures surrounding the joints, rheumatoid arthritis may involve significant destruction of the joint capsule, ligaments, and tendons, thereby necessitating high-stability constructs. 31 Conversely, in cases of poor bone stock and quality, it has been suggested that K-wires provide superior fixation, given the difficulty of achieving adequate purchase with screws. 28
The heterogeneity of reported data was a significant limitation of this review. In particular, inconsistent reporting of measures of fusion time (eg, mean fusion time vs percentage fused at 6 weeks) prevented direct comparison between many studies and resulted in small sample sizes for statistical analysis. No studies reported standard deviation or similar statistics, precluding meta-analysis or more robust statistical comparison. Complication rates were often reported without further stratification or detail, which raises the possibility of differences in definitions between studies. Many of the studies reporting PIPJ outcomes and included in this review were published before the year 2000, and more recent data may be useful in identifying the impact, if any, of changes in operative and postoperative practice in recent decades. Improvements in material engineering, construct design, and imaging modalities may all be relevant to the comparison of arthrodesis techniques. A lack of comparative studies is another important limiting factor in this review, and differences between study populations may confound the results. Importantly, arthrodesis outcomes likely differ based on the indication for surgery, and potential confounding factors such as these have not been controlled in any studies to date. Further research is necessary to elucidate the relative advantages and disadvantages of PIPJ arthrodesis techniques, ideally with matched comparative studies, comparison of techniques for each underlying diagnosis, and the inclusion of additional outcomes such as functional scores.
Conclusions
Common techniques used for arthrodesis of the PIPJ, including compression screws, K-wires, tension bands, and dorsal plates, appear to achieve similar fusion times, nonunion rates, and complication rates. In this analysis, arthrodesis with screws produced a significantly lower nonunion rate than with fusion wires; however, all other comparisons demonstrated no statistically significant difference. The quality of existing data is low, and further research is required to better compare available PIPJ arthrodesis techniques.
Footnotes
Ethical Approval: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This is a review article and informed consent was not required.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Harrison Faulkner  https://orcid.org/0000-0001-9937-7278
https://orcid.org/0000-0001-9937-7278
David J. Graham  https://orcid.org/0000-0003-3421-822X
https://orcid.org/0000-0003-3421-822X
Brahman S. Sivakumar  https://orcid.org/0000-0003-0890-2132
https://orcid.org/0000-0003-0890-2132
References
- 1. Jung J, Haghverdian B, Gupta R. Proximal interphalangeal joint fusion: indications and techniques. Hand Clin. 2018; 34(2):177-184. [DOI] [PubMed] [Google Scholar]
- 2. Newman EA, Orbay MC, Nunez FA, Jr, et al. Minimally invasive proximal interphalangeal joint arthrodesis using headless screw: surgical technique. Tech Hand Up Extrem Surg. 2018;22(2):39-42. [DOI] [PubMed] [Google Scholar]
- 3. Mortens J. Surgery of the hand in cerebral palsy. Acta Orthop Scand. 1965;36(4):441-452. [DOI] [PubMed] [Google Scholar]
- 4. Leibovic SJ, Strickland JW. Arthrodesis of the proximal interphalangeal joint of the finger: comparison of the use of the Herbert screw with other fixation methods. J Hand Surg Am. 1994;19(2):181-188. [DOI] [PubMed] [Google Scholar]
- 5. Herren D. The proximal interphalangeal joint: arthritis and deformity. EFORT Open Rev. 2019;4(6):254-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Uhl RL. Proximal interphalangeal joint arthrodesis using the tension band technique. J Hand Surg Am. 2007;32(6):914-917. [DOI] [PubMed] [Google Scholar]
- 7. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 8. StataCorp. Stata Statistical Software: Release 16 [Computer program]. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 9. Ayres JR, Goldstrohm GL, Miller GJ, et al. Proximal interphalangeal joint arthrodesis with the Herbert screw. J Hand Surg. 1988;13(4):600-603. [DOI] [PubMed] [Google Scholar]
- 10. Büchler U, Aiken MA. Arthrodesis of the proximal interphalangeal joint by solid bone grafting and plate fixation in extensive injuries to the dorsal aspect of the finger. J Hand Surg Am. 1988;13(4):589-594. [DOI] [PubMed] [Google Scholar]
- 11. Burton RI, Margles SW, Lunseth PA. Small-joint arthrodesis in the hand. J Hand Surg. 1986;11(5):678-682. [DOI] [PubMed] [Google Scholar]
- 12. Granowitz S, Vainio K. Proximal interphalangeal joint arthrodesis in rheumatoid arthritis: a follow-up study of 122 operations. Acta Orthop Scand. 1966;37(3):301-310. [DOI] [PubMed] [Google Scholar]
- 13. Khuri SM. Tension band arthrodesis in the hand. J Hand Surg Am. 1986;11(1):41-45. [DOI] [PubMed] [Google Scholar]
- 14. Leonard MH, Capen DA. Compression arthrodesis of finger joints. Clin Orthop Relat Res. 1979(145):193-198. [PubMed] [Google Scholar]
- 15. McGlynn JT, Smith RA, Bogumill GP. Arthrodesis of small joint of the hand: a rapid and effective technique. J Hand Surg Am. 1988;13(4):595-599. [DOI] [PubMed] [Google Scholar]
- 16. Novoa-Parra C, Montaner-Alonso D, Pérez-Correa JI, et al. Arthrodesis of the proximal interphalangeal joint of the 4th and 5th finger using an interlocking screw device to treat severe recurrence of Dupuytren’s disease. Rev Esp Cir Ortop Traumatol. 2018;62(3):216-221. [DOI] [PubMed] [Google Scholar]
- 17. Sabbagh W, Grobbelaar A, Clarke C, et al. Long-term results of digital arthrodesis with the Harrison-Nicolle peg. J Hand Surg Br. 2001;26(6):568-571. [DOI] [PubMed] [Google Scholar]
- 18. Seitz WH, Jr, Sellman DC, Scarcella JB, et al. Compression arthrodesis of the small joints of the hand. Clin Orthop Relat Res. 1994(304):116-121. [PubMed] [Google Scholar]
- 19. Tan M, Ho SWL, Sechachalam S. Acute arthrodesis of interphalangeal joints of the hand in traumatic injuries. J Hand Microsurg. 2018;10(1):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wright C, McMurtry R. AO arthrodesis in the hand. J Hand Surg Am. 1983;8(6):932-935. [DOI] [PubMed] [Google Scholar]
- 21. Lewis RC, Nordyke MD, Tenny JR. The tenon method of small joint arthrodesis in the hand. J Hand Surg Am. 1986; 11(4):567-569. [DOI] [PubMed] [Google Scholar]
- 22. Potenza AD. A technique for arthrodesis of finger joints. J Bone Joint Surg Am. 1973;55(7):1534-1536. [PubMed] [Google Scholar]
- 23. Konan S, Das A, Taylor E, et al. Distal interphalangeal joint arthrodesis in extension using a headless compressive screw. Acta Orthop Belg. 2013;79(2):154-158. [PubMed] [Google Scholar]
- 24. Kocak E, Carruthers KH, Kobus RJ. Distal Interphalangeal Joint Arthrodesis With the Herbert Headless Compression Screw: Outcomes and Complications in 64 Consecutively Treated Joints. Los Angeles, CA: Sage; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. El-Hadidi S, Al-Kdah H. Distal interphalangeal joint arthrodesis with Herbert screw. Hand Surg. 2003;8(1):21-24. [DOI] [PubMed] [Google Scholar]
- 26. Han SH, Cha YS, Song WT. Arthrodesis of distal interphalangeal joints in the hand with interosseous wiring and intramedullary K-wire fixation. Clin Orthop Surg. 2014;6(4):401-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Iwamoto T, Matsumura N, Sato K, et al. An obliquely placed headless compression screw for distal interphalangeal joint arthrodesis. J Hand Surg Am. 2013;38(12):2360-2364. [DOI] [PubMed] [Google Scholar]
- 28. Dickson D, Mehta S, Nuttall D, et al. A systematic review of distal interphalangeal joint arthrodesis. J Hand Microsurg. 2014;6(2):74-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Capo JT, Melamed E, Shamian B, et al. Biomechanical evaluation of 5 fixation devices for proximal interphalangeal joint arthrodesis. J Hand Surg Am. 2014;39(10):1971-1977. [DOI] [PubMed] [Google Scholar]
- 30. Kovach JC, Werner FW, Palmer AK, et al. Biomechanical analysis of internal fixation techniques for proximal interphalangeal joint arthrodesis. J Hand Surg Am. 1986;11(4):562-566. [DOI] [PubMed] [Google Scholar]
- 31. Parker AJR, Wessely S, Cleare AJ. The neuroendocrinology of chronic fatigue syndrome and fibromyalgia. Psychol Med. 2001;31(8):1331-1345. [DOI] [PubMed] [Google Scholar]