Abstract
Background
This review discusses success, time to healing, and complications of bone morphogenic proteins (BMPs) 7 and 2 in treating upper extremity nonunions.
Methods
Systematic review identified 26 of 479 studies that met inclusion criteria. Publications described application of BMPs to acute and chronic upper extremity delayed unions/nonunions. Unions, complications, patient demographics, and fracture/healing patterns were pooled and analyzed.
Results
Nonunions treated with BMP-7 (n=302) involved the humerus (64%), forearm (22%), clavicle (11%), and hand/wrist (3%), with prior surgical correction attempted in 84%. Nonunions treated with BMP-2 (n=96) involved the humerus (58%), hand/wrist (27%), forearm (14%), and clavicle (1%), with prior surgical correction attempted in all. Most nonunions (80%) were present for over 12 months before BMP application. Union rates of BMP-7 varied according to site: hand/wrist (95%), humerus (74%), forearm (29%), and clavicle (6.2%) nonunions achieved union as defined by study authors in 232 days (confidence interval=96-369, Q<0.001) on average. While not significant across studies, BMP-2 union rates were 71% of hand/wrist and 75% of humerus nonunions. Comparison of the BMPs demonstrates different proportions of success in humerus and hand/wrist fractures (P<.001) but not forearm fractures (P<.77) and longer time to radiographic union with BMP-7 (P<.011).
Conclusions
Most hand/wrist and humerus nonunions treated with BMP-7 and BMP-2 achieved union, with significant similarity among BMP-7 studies not observed in BMP-2 studies. Nonunions treated with BMP-7 have longer healing times yet similar complication rates compared with BMP-2. Overall, BMPs are an effective adjunct to fracture healing with acceptable complication profile.
Keywords: allograft, basic science, distal radius, fracture/dislocation, diagnosis, forearm, hand, humerus, wrist
Introduction
In the United States, 10% of 6.2 million total fractures occurring annually experience nonunion or delayed healing.1-4 In the upper extremities specifically, there is variation among nonunion rates. Humeral fracture nonunions are reported in 2% to 10% of conservatively managed humeral shaft fractures 5 and 2% to 5% of humeral fractures surgically treated with plate fixation. 6 Among forearm fractures, 12% of open and 3% of closed fractures result in nonunion. 7 Among scaphoid fractures, 5% of operatively treated scaphoid fractures and up to 50% of operatively treated displaced scaphoid fractures result in nonunion. 8
Autologous bone grafting (ABG) is considered the criterion standard biological adjunct for stimulation of fracture healing; however, complications that arise from harvesting ABG include donor site morbidity, and the quantity and quality of the ABG vary between age groups and patient phenotypes. 9 Subsequently, the challenges posed by ABG have sparked research efforts to identify biologic and chemical alternatives for the treatment of delayed union and/or nonunion.
Bone morphogenic proteins (BMPs) are members of the transforming growth factor-β (TGF-β) family of growth factors that induce an osteogenic and embryogenic cascade by binding to specific cell membrane receptors.10,11 The US Food and Drug Administration (FDA) has approved 2 recombinant BMPs for clinical use: BMP-7, which was approved in 2001 for recalcitrant long bone nonunions, and BMP-2, which was approved in 2002 for spinal fusion and in 2004 for open tibial shaft fractures. 12 Four studies comparing ABG and BMP in tibial nonunions demonstrated no difference between the two in achieving radiographic union and cited the absence of donor site morbidity as a benefit of BMP. 13 In addition, BMP is associated with less blood loss during operation in tibial nonunions, likely due to the lack of autograft harvest and associated blood loss, 13 as well as the avoidance of ABG-associated donor site pain. 14 Reports of wound drainage and heterotopic ossification have all been described as adverse events (AEs) of using BMPs; in general, however, distinguishing complications arising from BMP can pose a challenge in nonunions that have high rates of complications at baseline. 14 The purpose of this systematic review is to compile and review the success, time to healing, and AEs of BMP-7 and BMP-2 growth factors in the treatment of upper extremity fractures. Our hypothesis is that nonunions treated with BMPs will predictably reach clinical and/or radiographic union with an acceptable AE profile.
Methods
Literature Search
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A search of articles published prior to June 1, 2019, in MEDLINE (PubMed) was performed using the keywords “BMP bone fracture.”
Study Selection
Abstracts were manually screened by investigators for inclusion. Eligible studies reported the application and outcome of BMP-7 and/or BMP-2 in upper extremity fractures in an original patient population and had full-text availability in English. Studies that were commentaries or letters to the editor were excluded. For each study that met the inclusion criteria, a full-text version of the publication was downloaded and reviewed by investigators. Studies referenced in full-text articles during review that were not found on PubMed search were screened to determine potential eligibility. A total of 479 articles were identified in the database search, 89 full-text publications were reviewed, and ultimately 26 were included in quantitative synthesis (Figure 1). Data on patient demographics, study characteristics, fracture patterns, healing patterns, and AEs were collected and recorded for analysis.
Figure 1.
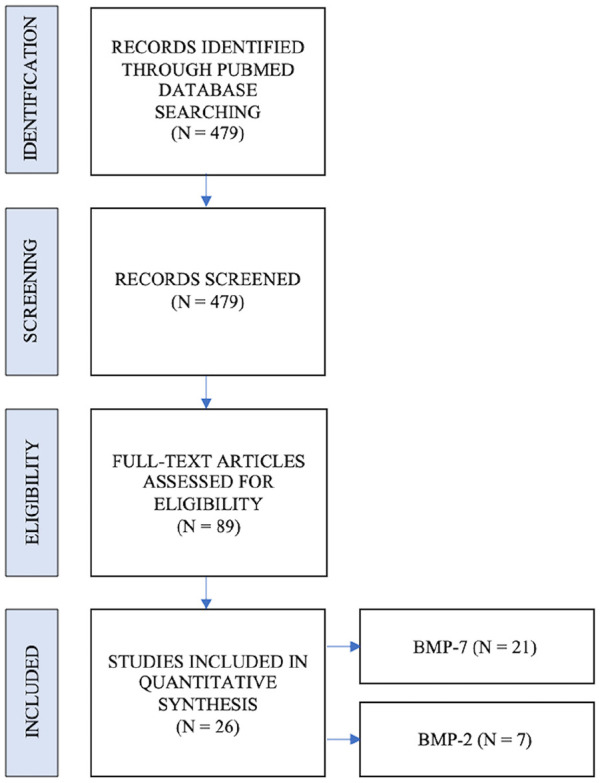
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Note. BMP = bone morphogenic protein.
Definitions
While the definition of nonunion remains disputed, 15 acute nonunion was differentiated from chronic nonunion based on duration: acute nonunion was defined as nonunion persisting 12 months or fewer, whereas chronic nonunion was defined as nonunion persisting more than 12 months. Index BMP application procedure was defined as the study’s focal application of BMP during treatment of the nonunion. Union was defined by individual authors, primarily by radiographic evaluation or computed tomography when applicable. Several authors separated union into radiological and clinical subtypes on analysis, with clinical union typically defined as the absence of pain with activity and functional recovery of extremity.
Adverse events were classified as perioperative and postoperative. Perioperative AEs included soft tissue reaction and early implant failure. Postoperative AEs included heterotopic ossification, neuromuscular symptoms, superficial tissue infection, deep tissue infection, late hardware failure, and delayed healing. Because few authors reported whether patients were hospitalized or discharged at the time of AE occurrence, AEs were stratified into either perioperative or postoperative based on the likeliness of AE to occur during hospitalization versus after discharge modeled after the classification used by Calori et al. 1 Persistence of nonunion alone was not considered an AE caused by BMP given the challenging nature of treating nonunions.
Statistical Analysis
Summary measures included estimate means with 95% confidence intervals (CIs). Statistical analysis was performed using a random model to account for both between-study and within-study variation. Between-study heterogeneity was evaluated with I 2 values and total variance with Cochran’s Q P values. Inferential statistics were used to compare contracture patterns and treatment success between and within complications and recurrence studies included.
Results
Bone Morphogenic Protein-7
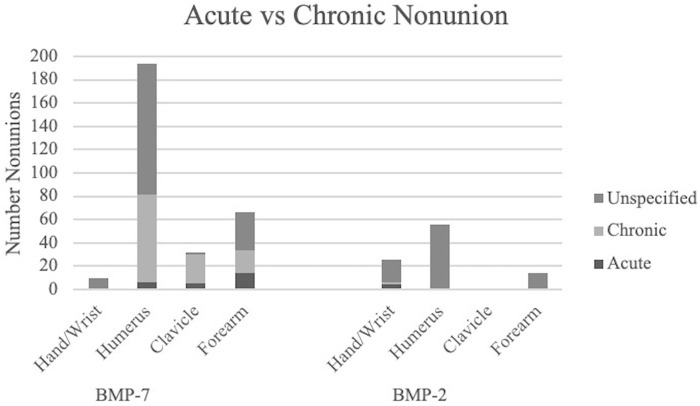
Overall, 302 upper extremity nonunions were included in BMP-7 analysis (Table 1). When reported, the average patient age was 51 years, and 58% (307 of 529) were men. Comorbidities included diabetes (15%, 44 of 303) and tobacco use (40%, 155 of 389). Unsuccessful prior surgical attempts at correction occurred in 82% of humerus (CI = 65%-92%, Q < 0.073), 77% of clavicle (CI = 34%-96%, Q < 0.520), and 89% of forearm (CI = 71%-96%, Q < 0.388) nonunions. No prior surgical correction attempts were reported in the 10 hand/wrist nonunions included in the study. On average, all nonunions reported in the studies (not limited to upper extremities) underwent 1.6 prior attempts at surgical correction (CI = 1.3-1.9, Q < 0.001). Most (83%) of the nonunions were chronic, with significantly more chronic humerus nonunions than acute humerus nonunions (Q < 0.001) (Table 2; Figure 2). Ratios of acute and chronic clavicle and forearm nonunions were not significantly different (Q < 0.484 and 0.395, respectively) (Table 2, Figure 2). All nonunions reported in the studies were present for an average of 17 months (CI = 12%-23%, Q < 0.001) before the index BMP procedure. Most patients (86%; 151 of 176) underwent an unsuccessful surgical attempt at correction of the nonunion before the index BMP-7 application procedure. Union was successfully reached in 95% of hand/wrist nonunions (CI = 55%-99%, Q n/a), 74% of humerus nonunions (CI = 46%-90%, Q < 0.001), 6% of clavicle nonunions (CI = 1.5%-23%, Q < 0.011), and 29% of forearm nonunions (Q < 0.001) (Table 3). Ultimately, 14% (CI = 3%-46%, Q < 0.0015) of treated fractures experienced perioperative AEs, and 23% (CI = 9%-47%, Q < 0.0027) experienced postoperative AEs following BMP-7 application (Table 4).
Table 1.
Studies Included in Analysis.
| Studies | Year | Type of study | Total patients | Upper extremity fractures | Acute nonunions | Chronic nonunions | Perioperative complications | Postoperative complications |
|---|---|---|---|---|---|---|---|---|
| BMP-7 | ||||||||
| Axelrad et al 16 | 2008 | Case study | 3 | 3 | 1 | 2 | 3 | |
| Bilic et al 17 | 2006 | Randomized controlled trial | 10 | 10 | 0 | 0 | ||
| Bong et al 18 | 2005 | Prospective cohort | 23 | 23 | 4 | 4 | ||
| Calori et al 1 | 2015 | Retrospective cohort | 44 | 12 | ||||
| Caterini et al 19 | 2016 | Retrospective case series | 12 | 12 | 12 | 6 | 2 | |
| Clark and McKinley 20 | 2010 | Case study | 1 | 1 | ||||
| Conway et al 2 | 2014 | Retrospective case series | 76 | 20 | ||||
| Dahabreh et al 21 | 2006 | Prospective cohort | 24 | 7 | ||||
| Giannoudis et al 3 | 2009 | Retrospective case series | 7 | 7 | ||||
| Giannoudis et al 22 | 2015 | Retrospective case series | 64 | 7 | 0 | |||
| Miska et al 23 | 2016 | Prospective cohort | 50 | 8 | ||||
| Moghaddam et al 24 | 2010 | Prospective cohort | 54 | 7 | 0 | |||
| Morision et al 25 | 2015 | Retrospective cohort | 65 | 65 | 65 | 2 | 5 | |
| Murena et al 5 | 2014 | Retrospective case series | 2 | 2 | 2 | 1 | ||
| O’hEireamhoin et al 11 | 2011 | Retrospective case series | 13 | 6 | 0 | 0 | ||
| Pantalone et al 26 | 2015 | Case study | 1 | 1 | 1 | 1 | ||
| Papanagiotou et al 27 | 2015 | Prospective cohort | 13 | 13 | 1 | 0 | ||
| Papanna et al 4 | 2012 | Retrospective case series | 17 | 17 | 8 | 9 | 1 | 1 |
| Ronga et al 28 | 2006 | Retrospective case series | 105 | 36 | ||||
| Singh et al 9 | 2016 | Prospective cohort | 42 | 42 | 15 | 27 | 2 | 2 |
| Van Houwelingen and McKee 29 | 2005 | Retrospective case series | 3 | 3 | 1 | 2 | 0 | 0 |
| Total | 629 | 302 | 25 | 120 | 17 | 18 | ||
| BMP-2 | ||||||||
| Ablove and Abrams 30 | 2015 | Retrospective case series | 4 | 4 | 0 | 0 | ||
| Axelrad et al 16 | 2008 | Case study | 1 | 1 | 1 | 1 | ||
| Brannan et al 31 | 2016 | Retrospective case series | 6 | 6 | 4 | 2 | 4 | |
| Conway et al 2 | 2014 | Retrospective case series | 138 | 50 | ||||
| Ritting et al 32 | 2012 | Case study | 1 | 1 | 1 | 0 | 1 | |
| Starman et al 33 | 2012 | Retrospective case series | 116 | 7 | ||||
| Rice and Lubahn 34 | 2013 | Retrospective case series | 27 | 27 | 0 | 8 | ||
| Total | 293 | 96 | 5 | 3 | 0 | 14 | ||
Note. BMP = bone morphogenic protein.
Table 2.
Nonunion Chronicity.
| Acute | Chronic | Unspecified | Total | ||||
|---|---|---|---|---|---|---|---|
| No. of studies | No. of nonunions (%) | No. of studies | No. of nonunions (%) | No. of studies | No. of nonunions (%) | N | |
| BMP-7 | 4 | 25 (8) | 8 | 120 (39) | 13 | 160 (52) | 305 |
| Hand/Wrist | — | — | — | — | 1 | 10 (100) | 10 |
| Humerus | 4 | 6 (3) | 8 | 75 (39) | 11 | 113 (58) | 194 |
| Clavicle | 2 | 5 (14) | 2 | 25 (71) | 3 | 5 (14) | 35 |
| Forearm | 2 | 12 (21) | 3 | 20 (30) | 8 | 32 (48) | 66 |
| BMP-2 | 2 | 5 (5) | 2 | 3 (3) | 4 | 89 (92) | 97 |
| Hand/Wrist | 1 | 4 (15) | 1 | 2 (8) | 2 | 20 (77) | 26 |
| Humerus | 1 | 1 (2) | 0 | 0 (0) | 2 | 55 (98) | 56 |
| Clavicle | 0 | 0 (0) | 0 | 0 (0) | 1 | 1 (100) | 1 |
| Forearm | 0 | 0 (0) | 1 | 1 (7) | 2 | 13 (93) | 14 |
Note. BMP = bone morphogenic protein.
Figure 2.
Nonunion chronicity distribution.
Note. BMP = bone morphogenic protein.
Table 3.
Union Rates.
| Fracture site | No. of studies | Fracture distribution by site, % | Union rates after BMP treatment, % | CI, % | Cochran’s Q |
|---|---|---|---|---|---|
| BMP-7 | 18 | 100 | 87 | 77-93 | 0.0287 |
| Clavicle | 4 | 11 | 6.2 | 1.5-23 | 0.0111 |
| Forearm | 6 | 22 | 29 | 7.8-65 | <0.001 |
| Hand/Wrist | 1 | 3 | 95 | 55-99 | — |
| Humerus | 13 | 64 | 74 | 46-90 | <0.001 |
| BMP-2 | 7 | 100 | 85 | 57-96 | 0.2670 |
| Clavicle | 1 | 1 | — | — | — |
| Forearm | 3 | 14 | — | — | — |
| Hand/Wrist | 3 | 27 | 71 | 41-90 | 0.2593 |
| Humerus | 3 | 58 | 75 | 11-99 | — |
Note. BMP = bone morphogenic protein; CI = confidence interval.
Table 4.
Adverse Events.
| Adverse event | BMP-7 | BMP-2 | BMP-7 vs BMP-2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Event occurrence, % | CI, % | Cochran’s Q | n | Event occurrence, % | CI, % | Cochran’s Q | P value | |
| Perioperative (subtotal) | 11 | 14 | 3-46 | 0.0015 | 0 | — | — | — | — |
| Soft tissue | 7 | 25 | 3-79 | 0.037 | 0 | — | — | — | — |
| Early hardware failure | 4 | 8 | 1.5-35 | 0.094 | 0 | — | — | — | — |
| Postoperative (subtotal) | 23 | 23 | 9-47 | 0.0027 | 14 | 49 | 24-75 | 0.213 | <.001 |
| Neuromuscular | 7 | 20 | 10-37 | 0.723 | 3 | 11 | 2-29 | — | — |
| Heterotopic ossification | 6 | 16 | 1-71 | 0.009 | 5 | 69 | 33-90 | 0.826 | <.001 |
| Superficial infection | 3 | 4 | 1.5-13 | 0.9394 | 0 | — | — | — | — |
| Deep tissue infection | 2 | 3 | 0.6-10 | 0.457 | 0 | — | — | — | — |
| Late hardware failure | 4 | 22 | 0.5-94 | 0.018 | 4 | 15 | 4-34 | — | .27 |
| Healing | 1 | 1.5 | 0.2-10 | — | 2 | 22 | 0.4-95 | 0.024 | <.001 |
| Total | 34 | — | — | — | 14 | — | — | — | — |
Note. BMP = bone morphogenic protein; CI = confidence interval.
Bone Morphogenic Protein-2
A total of 96 upper extremity nonunions were included in BMP-2 analysis (Table 1). When reported, the average patient age was 36 years, and 59% (156 of 255) were men. Comorbidities included diabetes (16%; 36 of 337) and tobacco use (30%; 75 of 261). Unsuccessful surgical attempts at correction occurred in 92% of hand/wrist (CI = 58%-99%, Q < 0.861), 75% of humerus (CI = 11%-99%, Q n/a), and 75% of forearm (CI = 11%-99%, Q n/a) nonunions before the index BMP-2 application procedure. No prior surgical correction attempts were reported in the single clavicle nonunion included in the study. Most (63%) of the nonunions were acute, with significantly more acute hand/wrist nonunions than chronic humerus nonunions (Q < 0.001) (Table 2; Figure 2). There were insufficient data reported between studies to calculate the average prior attempts at surgical correction and the duration of nonunion before the index BMP application procedure. All patients in studies that reported prior surgeries (n = 12) had undergone an unsuccessful surgical attempt to correct the nonunion before the index BMP-2 application procedure. Union was successfully reached in 71% of hand/wrist nonunions (CI = 41%-90%, Q < 0.259) and 75% of humerus nonunions (CI = 11%-99%, Q n/a) (Table 3). A total of 49% (CI = 24%-75%, Q < 0.001) of fractures treated with BMP-2 experienced postoperative AEs, with no reported perioperative AEs (Table 4).
BMP-7 Versus BMP-2
Comparison of BMP-7 versus BMP-2 treatment demonstrates significantly different proportions of success in humerus and hand/wrist fractures (P < .001), but not in forearm and clavicle fractures (P < .77 and P < .84, respectively) (Table 5), although comparison of clavicular nonunions is limited by sample size, with only 1 case of clavicular nonunion treated with BMP-2. Although no perioperative AEs were reported in fractures treated with BMP-2, rates of postoperative AEs overall were statistically greater in BMP-2 versus BMP-7 (P < .001) (Table 4). Heterotopic ossification and healing complications (P < 0.001 for both) were reported at higher rates in BMP-2 compared with BMP-7, whereas neuromuscular complications and late hardware failure were not observed at statistically different rates between the 2 (P < .12 and P < .27, respectively). Comparison of time to radiographic union demonstrates significantly longer healing times for fractures treated with BMP-7 compared with BMP-2 (196 [CI = 176-220] and 117 [CI = 170-223], respectively; P < .011).
Table 5.
Union Success: BMP-7 vs BMP-2.
| BMP-7 | BMP-2 | BMP-7 vs BMP-2 | |||||
|---|---|---|---|---|---|---|---|
| No. of studies | Treatment success, % | 95% CI, % | No. of studies | Treatment success, % | 95% CI, % | Test of equal proportions (P) | |
| Clavicle | 6 | 16 | 7.2-33 | 1 | 14 | 1-58 | .84 |
| Forearm | 10 | 34 | 19-52 | 3 | 37 | 18-62 | .77 |
| Hand/Wrist | 1 | 100 | 69-100 | 3 | 76 | 42-93 | <.001 |
| Humerus | 19 | 69 | 57-79 | 3 | 89 | 44-98 | <.001 |
Note. BMP = bone morphogenic protein; CI = confidence interval.
Discussion
The purpose of this systematic review is to compile and review the success, time to healing, and AEs of BMP-7 and BMP-2 growth factors in the treatment of upper extremity fractures. Key findings of our study include successful achievement of union following BMP application in a variety of fracture locations with longer time to union but fewer postoperative AEs observed following BMP-7 treatment compared with BMP-2. Ultimately, BMPs are a useful adjunct to fracture healing with acceptable complication rates.
Impaired or delayed union is a major barrier to treatment of fractures, with 5% to 10% of fractures in the United States experiencing delayed healing. 1 A number of risk factors predisposing patients to nonunion have been identified, notably age, smoking, diabetes, alcohol abuse, and medication use. 35 In our study, diabetes was noted at similar rates in patients treated with BMP-7 and BMP-2 (15% and 16%, respectively), with slightly higher tobacco use reported in patients treated with BMP-7 (40% as opposed to 30%). Smoking in particular has been reported to increase the likelihood of nonunion in both upper and lower extremities with effects independent of age, sex, and race. 35 Zura et al 35 reported increased risk of nonunion in type 1 and type 2 diabetes in both long and short bone fractures. Interestingly, a sampling of orthopedic surgeons revealed that 98% and 97% identify smoking and diabetes, respectively, as predictors of nonunion, whereas only 82% identify age as a similar predictor. 35
Bone morphogenic protein growth factors are being investigated as an alternative to ABG in treating nonunions. Urist first discovered BMPs in 1965, and the FDA approved BMP-7 for recalcitrant long bone nonunions in 2001 and BMP-2 for open tibial shaft fractures in 2004. 14 Subsequently, research surrounding BMPs and other engineered osteoinductive agents has been driven by efforts to prevent challenges posed by iliac crest bone grafting. 12 In addition, fracture rates in elderly patients are expected to triple in the upcoming years, which necessitates improving delayed fracture healing to prepare for the challenge of treating nonunion or delayed union in this population. 24
Humerus fractures were the most frequently reported upper extremity fracture among studies included in the analysis. In general, humeral nonunions are reported in 2% to 10% of conservatively managed fractures 5 and in 2% to 5% of fractures treated with plate fixation. 6 Our study found that humerus fracture healing rates were similar between BMP-7 and BMP-2 (74%, CI = 46%-90%, Q < 0.001 and 75%, CI = 11-99, Q n/a, respectively). Most of the humerus nonunions treated with BMP-7 were chronic (86%, CI = 74-93, Q < 0.001); of the 56 humerus nonunions treated with BMP-2, only 1 was specified as acute or chronic. Beyond humerus fractures, the dearth of hand/wrist fractures treated with BMP-7 (n = 10) coupled with the paucity of both forearm and clavicular fractures treated with BMP-2 (n = 26 and n = 1, respectively) created challenges in comparing outcomes of BMP-7 versus BMP-2. Despite the lack of comparable data, significant variation was seen among fracture sites, with 74% of humerus fractures (74%, CI = 46%-90%, Q < 0.001), 29% of forearm fractures (CI = 7.8%-65%, Q < .001), and 6.2% of clavicular fractures (CI = 1.5%-23%, Q = .0111) reaching clinical success following treatment. The significantly different proportions of success seen in BMP-7 versus BMP-2 for humerus and hand/wrist fractures (P < .001) and the absence of these differences in forearm fractures warrant further investigation to better understand how to best approach treatment by fracture site, although the absence of these differences in clavicular fractures is due to low sample size, with only 1 case of clavicular nonunion treated with BMP-2.
In general, fractures treated with BMP-7 reached radiographic union in 196 days (CI = 170- 223, Q = 0.248) on average, whereas those treated with BMP-2 reached radiographic union in 117 days (CI = 56-177, Q < .001) on average, with significantly less variation across studies included in analysis. Similarly, Conway et al 2 found that long bone fractures treated with BMP-2 reached radiographic union at a higher rate and faster than those treated with BMP-7. Haubruck et al 36 also found that surgically managed tibial nonunions treated once with BMPs had a significantly higher rate of union with BMP-2 versus BMP-7, regardless of the presence or absence of infection. Regardless, the high variation among union times in nonunions treated with BMP-7 coupled with the different distribution of nonunion sites and characteristics between studies requires further investigation to compare BMP-7 and BMP-2.
Complications in the treatment of upper extremity nonunion are not unique to BMP treatments. Reports of open reduction and internal fixation (ORIF) of humerus nonunions yield mechanical failure rates of 7% to 27%, heterotopic ossification rates of 0 to 49%, malunion rates of 30%, and substantial infection and wound-healing complications. 37 Our study’s estimations of both early and late hardware failure rates (8% for those treated with BMP-7; 22% and 15% for those treated with BMP-7 and BMP-2, respectively) are thus not appreciably discordant with existing ORIF rates. Similarly, our study’s estimation rates of heterotopic ossification of 16% for nonunions treated with BMP-7 and 69% for nonunions treated with BMP-2 are not unexpected given that heterotopic ossification has been raised as a concern for BMP treatment. Our review found that heterotopic ossification and healing complications were observed in different proportions between the 2 treatments (P < .001), whereas neuromuscular complications and late hardware failure were not. While nonunions treated with BMP-7 in our review had lower rates of heterotopic ossification and healing complications than those treated with BMP-2, Conway et al 2 report that long bone fractures treated with BMP-2 had lower complication rates than those treated with BMP-7.
Two notable reported AEs of BMPs include heterotopic ossification and the possibility of carcinogenesis. Heterotopic ossification following BMP treatment is described at a wide variety of treatment sites; while some cases are asymptomatic, others may warrant additional procedures.14,16 Barcak and Beebe 14 note that symptomatic heterotopic ossification tends to occur near joints, a trend that may impact reporting, and subsequently encourages consideration of BMP treatment location to prevent heterotopic ossification until the relationship between the 2 is better understood. The concern for carcinogenesis stems from the role of TGF-β in tumor progression. Although there is no clear evidence that BMP treatment induces novel carcinogenesis, studies have raised concern for increased cancer risk with increasing doses of BMPs. 14 Similarly, more evidence reporting on long-term outcomes is needed to elucidate whether carcinogenesis is a concern.
Fracture nonunion poses an economic burden due to health care expenses, compounded by increased infection rates and extended hospital stays and coupled with lost productivity. Dahabreh et al 21 cite estimated direct and indirect medical cost of a humeral nonunion as an equivalent of $24 438 compared with $27 004 and $26 638 for femoral and tibial nonunions, whereas the cost of a unit of BMP-7 was priced at $4710, less than 20% of the overall estimated cost. In a review of both upper and lower extremities, BMP treatment costs 47% less on average than the sum of previous unsuccessful treatments for nonunion. 38 Most of the existing literature on the cost-effectiveness of BMP focuses on open tibial fractures. A case review by Alt et al 39 found net savings in using BMP-2 for grade III open tibial fractures as opposed to standard-of-care treatment: specifically, the equivalent of $810 and $1295 costs per case in Germany and the United Kingdom, respectively, was offset by decreased time to healing, resulting in net savings of $6985 and $5275, respectively. A 2010 state of evidence review on BMP-2 for open tibial fractures concludes that the moderate evidence supporting enhanced healing and reduced need for secondary procedures results in higher quality-adjusted life years for BMP-2 priced at $1000 or $3000, with estimated mean incremental cost-effectiveness ratios per quality-adjusted life year of $7960 and $49 204, respectively. 40 Caterini et al 19 conclude that due to the high cost, BMP-7 should be reserved for fractures with recalcitrant nonunion that have failed surgical intervention. Furthermore, the economic implications of off-label BMP use in upper extremity fractures are not well documented, and the cost-effectiveness of BMPs warrants more investigation to determine whether the expense of the treatment is balanced by its efficacy.
Limitations
There is a paucity of literature available on the roles of BMP-7 and BMP-2 in treating upper extremity fractures, with appreciably fewer studies on BMP-2 compared with BMP-7. Different combinations of BMP treatments with and without autologous and allogenic grafts coupled with the lack of reporting results by both fracture location and materials used create challenges in isolating the effects of BMPs. Many studies reported the mean months from injury to the index BMP application procedure for all fracture sites included in the study, not necessarily limited to upper extremities, affecting estimates of mean nonunion duration. The absence of specification between acute and chronic for reported nonunion duration similarly limited comparison, especially in those treated with BMP-2. In addition, the lack of reported follow-up times also introduces bias in determining fracture healing rates and limits comparability between studies. Variability in dosing and limited reporting of dosing further complicated both efficacy and cost-effectiveness analyses. The lack of data on BMP for fractures specific to fracture location also poses a challenge in understanding the role of these treatments in upper extremities.
Conclusion
Most hand/wrist and humerus nonunions treated with BMP-7 and BMP-2 successfully achieved union, with longer times to healing but fewer postoperative AEs in patients treated with BMP-7. Systematic review of the success, time to healing, and AEs of BMP-7 and BMP-2 in treating upper extremity fractures demonstrates variable rates of success between fracture sites in studies of both BMP-7 and BMP-2, warranting further investigation in comparing the BMPs. Authors investigating this topic are encouraged to report treatment success rates, AEs, and costs specific to fracture site location to better discern the role of BMPs in upper extremity fractures. While continued investigation will help to elucidate the most effective application of BMPs in these sites, BMPs overall are an effective adjunct to fracture healing with acceptable AE profile and may offer a viable alternative for current ABG use in upper extremities.
Footnotes
Ethical Approval: This study did not require institutional review board approval.
Statement of Human and Animal Rights: This study does not involve any human or animal subjects.
Statement of Informed Consent: Informed consent was not indicated since this study did not involve subjects.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alexis B. Sandler  https://orcid.org/0000-0002-5784-9473
https://orcid.org/0000-0002-5784-9473
John C. Dunn  https://orcid.org/0000-0002-2292-8227
https://orcid.org/0000-0002-2292-8227
References
- 1. Calori GM, Colombo M, Bucci M, et al. Clinical effectiveness of Osigraft in long-bones non-unions. Injury. 2015;46:S55-S64. [DOI] [PubMed] [Google Scholar]
- 2. Conway JD, Shabtai L, Bauernschub A, et al. BMP-7 versus BMP-2 for the treatment of long bone nonunion. Orthopedics. 2014;37:e1049-e1057. [DOI] [PubMed] [Google Scholar]
- 3. Giannoudis PV, Kanakaris NK, Dimitriou R, et al. The synergistic effect of autograft and BMP-7 in the treatment of atrophic nonunions. Clin Orthop Relat Res. 2009;467:3239-3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Papanna MC, Al-Hadithy N, Somanchi BV, et al. The use of bone morphogenic protein-7 (OP-1) in the management of resistant non-unions in the upper and lower limb. Injury. 2012;43:1135-1140. [DOI] [PubMed] [Google Scholar]
- 5. Murena L, Canton G, Vulcano E, et al. Treatment of humeral shaft aseptic nonunions in elderly patients with opposite structural allograft, BMP-7, and mesenchymal stem cells. Orthopedics. 2014;37:e201-e206. [DOI] [PubMed] [Google Scholar]
- 6. Peters RM, Claessen FM, Doornberg JN, et al. Union rate after operative treatment of humeral shaft nonunion: a systematic review. Injury. 2015;46:2314-2324. [DOI] [PubMed] [Google Scholar]
- 7. Kujala S, Raatikainen T, Ryhanen J, et al. Composite implant of native bovine bone morphogenetic protein (BMP), collagen carrier and biocoral in the treatment of resistant ulnar nonunions: report of five preliminary cases. Arch Orthop Trauma Surg. 2004;124:26-30. [DOI] [PubMed] [Google Scholar]
- 8. Kujala S, Raatikainen T, Ryhanen J, et al. Composite implant of native bovine bone morphogenetic protein (BMP) and biocoral in the treatment of scaphoid nonunions: a preliminary study. Scand J Surg. 2002;91:186-190. [DOI] [PubMed] [Google Scholar]
- 9. Singh R, Bleibleh S, Kanakaris NK, et al. Upper limb non-unions treated with BMP-7: efficacy and clinical results. Injury. 2016;47:S33-S39. [DOI] [PubMed] [Google Scholar]
- 10. Dean DB, Watson JT, Jin W, et al. Distinct functionalities of bone morphogenetic protein antagonists during fracture healing in mice. J Anat. 2010;216:625-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O’hEireamhoin S, Quinlan JF, Rourke KO. The use of bone morphogenetic protein 7 in fracture non-unions. Orthop Surg. 2011;3:40-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bialy IE, Jiskoot W, Nejadnik MR. Formulation, delivery and stability of bone morphogenetic proteins for effective bone regeneration. Pharm Res. 2017;34:1152-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garrison KR, Donell S, Ryder J, et al. Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review. Health Technol Assess. 2007;11:1-150. [DOI] [PubMed] [Google Scholar]
- 14. Barcak EA, Beebe MJ. Bone morphogenetic protein: is there still a role in orthopedic trauma in 2017? Orthop Clin N Am. 2017;48:301-309. [DOI] [PubMed] [Google Scholar]
- 15. Bhandari M, Guyatt GH, Swiontkowski MF, et al. A lack of consensus in the assessment of fracture healing among orthopaedic surgeons. J Orthop Trauma. 2002;16:562-566. [DOI] [PubMed] [Google Scholar]
- 16. Axelrad TW, Steen B, Lowenberg DW, et al. Heterotopic ossification after the use of commercially available recombinant human bone morphogenetic proteins in four patients. J Bone Joint Surg Br. 2008;90:1617-1622. [DOI] [PubMed] [Google Scholar]
- 17. Bilic R, Simic P, Jelic M, et al. Osteogenic protein-1 (BMP-7) accelerates healing of scaphoid non-union with proximal pole sclerosis. Int Orthop. 2006;30:128-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bong MR, Capla EL, Egol KA, et al. Osteogenic protein-1 (bone morphogenetic protein-7) combined with various adjuncts in the treatment of humeral diaphyseal nonunions. Bull Hosp Jt Dis. 2005;63:20-23. [PubMed] [Google Scholar]
- 19. Caterini R, Potenza V, Ippolito E, et al. Treatment of recalcitrant atrophic non-union of the humeral shaft with BMP-7, autologous bone graft and hydroxyapatite pellets. Injury. 2016;47:S71-S77. [DOI] [PubMed] [Google Scholar]
- 20. Clark RR, McKinley TO. Bilateral olecranon epiphyseal fracture non-union in a competitive athlete. Iowa Orthop J. 2010;30:179-181. [PMC free article] [PubMed] [Google Scholar]
- 21. Dahabreh Z, Calori GM, Kanakaris NK, et al. A cost analysis of treatment of tibial fracture nonunion by bone grafting or bone morphogenetic protein-7. Int Orthop. 2009;33:1407-1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Giannoudis PV, Gudipati S, Harwood P, et al. Long bone non-unions treated with the diamond concept: a case series of 64 patients. Injury. 2015;46:S48-S54. [DOI] [PubMed] [Google Scholar]
- 23. Miska M, Findeisen S, Tanner M, et al. Treatment of nonunions in fractures of the humeral shaft according to the Diamond Concept. Bone Joint J. 2016;98:81-87. [DOI] [PubMed] [Google Scholar]
- 24. Moghaddam A, Elleser C, Biglari B, et al. Clinical application of BMP 7 in long bone non-unions. Arch Orthop Trauma Surg. 2010;130:71-76. [DOI] [PubMed] [Google Scholar]
- 25. Morison Z, Vicente M, Schemitsch EH, et al. The treatment of atrophic, recalcitrant long-bone nonunion in the upper extremity with human recombinant bone morphogenetic protein-7 (rhBMP-7) and plate fixation: a retrospective review. Injury. 2016;47:356-363. [DOI] [PubMed] [Google Scholar]
- 26. Pantalone A, Vanni D, Guelfi M, et al. From plate to nail: a case-report of proximal humerus non-union. Injury. 2015;46:S48-50. [DOI] [PubMed] [Google Scholar]
- 27. Papanagiotou M, Dailiana ZH, Karachalios T, et al. RhBMP-7 for the treatment of nonunion of fractures of long bones. Bone Joint J. 2015;97:997-1003. [DOI] [PubMed] [Google Scholar]
- 28. Ronga M, Baldo F, Zappala G, et al. Recombinant human bone morphogenetic protein-7 for treatment of long bone non-union: an observational, retrospective, non-randomized study of 105 patients. Injury. 2006;375:51-56. [DOI] [PubMed] [Google Scholar]
- 29. Van Houwelingen AP, McKee MD. Treatment of osteopenic humeral shaft nonunion with compression plating, humeral cortical allograft struts, and bone grafting. J Orthop Trauma. 2004;19:36-42. [DOI] [PubMed] [Google Scholar]
- 30. Ablove RH, Abrams SS. The use of BMP-2 and screw exchange in the treatment of scaphoid fracture non-union. Hand Surg. 2015;20:167-171. [DOI] [PubMed] [Google Scholar]
- 31. Brannan PS, Gaston RG, Loeffler BJ, et al. Complications with the use of BMP-2 in scaphoid nonunion surgery. J Hand Surg Am. 2016;41:602-608. [DOI] [PubMed] [Google Scholar]
- 32. Ritting AW, Weber EW, Lee MC. Exaggerated inflammatory response and bony resorption from BMP-2 use in a pediatric forearm nonunion. J Hand Surg Am. 2012;37:316-321. [DOI] [PubMed] [Google Scholar]
- 33. Starman JS, Bosse MJ, Cates CA, et al. Recombinant human bone morphogenetic protein-2 use in the off-label treatment of nonunions and acute fractures: a retrospective review. J Trauma. 2011;72:676-681. [DOI] [PubMed] [Google Scholar]
- 34. Rice I, Lubahn JD. Use of bone morphogenetic protein-2 (rh-BMP-2) in treatment of wrist and hand nonunion with comparison to historical control groups. J Surg Orthop Adv. 2013;22:256-262. [DOI] [PubMed] [Google Scholar]
- 35. Zura R, Mehta S, Della Roca GJ, et al. Biological risk factors for nonunion of bone fracture. Bone Joint J. 2016;4:1-12. [DOI] [PubMed] [Google Scholar]
- 36. Haubruck P, Tanner MC, Vlachopoulos W, et al. Comparison of the clinical effectiveness of Bone Morphogenic Protein (BMP) -2 and -7 in the adjunct treatment of lower limb nonunions. Orthop Traumatol Surg Res. 2018;104:1241-1248. [DOI] [PubMed] [Google Scholar]
- 37. Savvidou OD, Zampeli F, Koutsouradis P, et al. Complications of open reduction and internal fixation of distal humerus fractures. EFFORT Open Rev. 2018;3:558-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dahabreh Z, Dimitriou R, Giannoudis PV. Health economics: a cost analysis of treatment of persistent fracture non-unions using bone morphogenetic protein-7. Injury. 2007;38:371-377. [DOI] [PubMed] [Google Scholar]
- 39. Alt V, Borgman B, Eicher A, et al. Effects of recombinant human bone morphogenetic protein-2 (rhBMP-2) in grade III open tibia fractures treated with unreamed nails: a clinical and health-economic analysis. Injury. 2015;46:2267-2272. [DOI] [PubMed] [Google Scholar]
- 40. Ratko TA, Belinson SE, Samson DJ, et al. Bone Morphogenetic Protein: The State of the Evidence of on-Label and Off-Label Use. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [PubMed] [Google Scholar]