Abstract
Background
Intramedullary nail (IMN) fixation of metacarpal fractures is an alternative to Kirschner wire (K-wire) fixation. The goal of this study was to compare the biomechanical properties of K-wire fixation with a threaded IMN (InNate; ExsoMed, Aliso Viejo, California).
Methods
The study design was based on previously described biomechanical models for evaluating metacarpal fractures. Sixteen fresh frozen small finger–matched and ring finger–matched pairs were randomized to either IMN or 0.045 in K-wire fixation after receiving a standardized neck osteotomy. Proper implant placement was confirmed with plain radiographs. Specimens then underwent loading in a 3-point bend configuration. Load to failure (LTF), stiffness, and fracture displacement were recorded. Mechanical failure was defined by a sharp change in the load-displacement curve.
Results
Age, sex, sidedness (left or right), and digit (ring or small finger) were evenly distributed between groups. The IMN had a significantly higher LTF than K-wires (546 N vs 154 N, P < .001). The K-wire fixation demonstrated plastic deformation between 75 and 150 N. Intramedullary nail stiffness was higher than that of K-wires (155.89 N/mm vs 59.28 N/mm, P < .001).
Conclusions
When surgical fixation is indicated for metacarpal neck and shaft fractures, the threaded IMN is biomechanically superior to crossed K-wires with the application of 3-point bend.
Keywords: biomechanical study, metacarpal fractures, intramedullary fixation, K-wires
Introduction
Although many metacarpal neck and shaft fractures can be managed nonoperatively, surgical management is generally recommended in cases of multiple metacarpal fractures, open fractures, or fractures with significant angulation.1-3 Relative indications include the polytraumatized patient and patients who desire fixation for earlier return to activities. 1 In general, the clinical outcome of metacarpal fracture fixation is better when early mobilization is permitted.4,5
Surgical management options include Kirschner wire (K-wire) fixation, intramedullary fixation, or plate fixation. Kirschner wire fixation is a versatile, inexpensive option that requires less soft tissue dissection, but may be complicated by prolonged immobilization and requires a second procedure of pin removal. Plate fixation allows for excellent fracture stability and earlier mobility but involves substantial soft tissue dissection and a more expensive implant.6,7 Intramedullary fixation is not a new concept.4,8-10 Retrograde intramedullary compression screw fixation has been evaluated clinically and has allowed for early postoperative motion without compromising union.4,11 Previously evaluated intramedullary implants have included the 2.4-, 3.0-, and 3.5-mm cannulated headless compression screw (HCS) and an intramedullary nail (IMN).11-14 A new metacarpal-specific threaded IMN (InNate; ExsoMed, Aliso Viejo, California) may better fit metacarpal dimensions than other available options, but this implant has not yet been biomechanically evaluated.
Given that earlier mobility has been shown to improve patient outcomes, we sought to evaluate how the biomechanical characteristics of the threaded IMN compared with K-wire fixation. Our null hypothesis was that there would be no significant difference between the IMN and K-wire fixation biomechanically.
Materials and Methods
Randomization
A total of 16 fresh frozen cadaveric small finger or ring finger metacarpal specimens from 4 matched pair hands were used. Each of the 8 matched specimen pairs was randomized into either K-wire or IMN fixation, and the process was carried out to ensure that sidedness (left or right) and digit (ring or small) per fixation group were equal. Distal radius bone density data were available for all specimens. Specimens with preexisting fractures or gross bony defects were excluded.
Specimen Preparation and Implant Insertion
Specimens were skeletonized and kept frozen in a moist towel at −20°C and then slowly thawed to room temperature prior to fixation and experimentation. All specimens received the same linear osteotomy at the physeal scar, perpendicular to the long axis of the metacarpal using a 0.23-mm reciprocating saw as previously described by Avery et al. 13 In all cases, provisional reduction was obtained and held with pointed reduction clamps. Specimens were then either fixed with 0.045 in K-wires or an IMN. In 8 specimens, 2 K-wires were inserted in a retrograde manner through the metacarpal heads, past the osteotomy site into the proximal medullary canal. Care was taken to ensure the wires crossed proximal to the fracture site (Figure 1). The 8 specimens that received IMN fixation were first reduced with a guidewire centered in the dorsal third of the metacarpal head. The metacarpal medullary canals were reamed with a 2.7-mm cannulated drill bit, and the final implant length was measured with a depth gauge. Implants were inserted and tightened by hand (Figure 2).
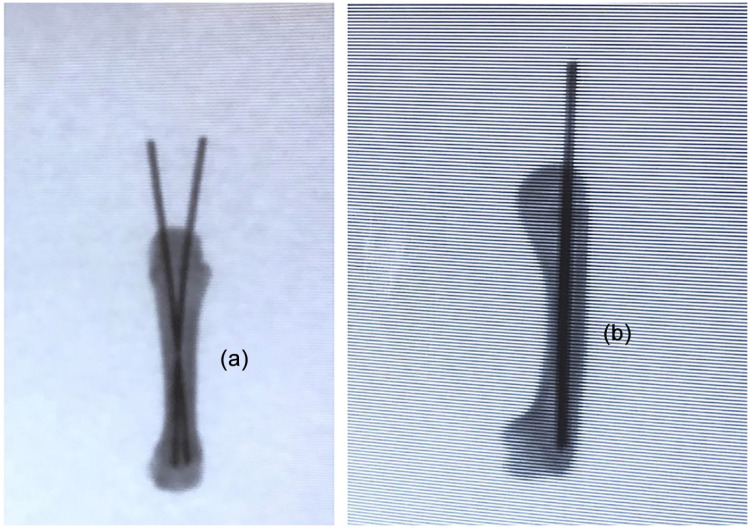
Figure 1.
(a) and (b) Anteroposterior and lateral radiographs demonstrating fixation of metacarpal neck fracture with cross Kirschner wires.
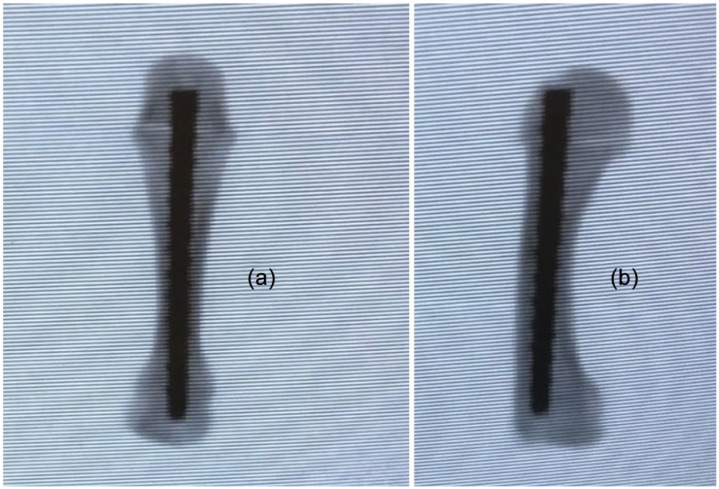
Figure 2.
(a) and (b) Anteroposterior and lateral radiographs demonstrating fixation of metacarpal neck fracture with InNate intramedullary nail.
Implant placement and fracture reduction were confirmed with plain radiographs. All measurements, osteotomies, and fixation were done by the same investigator in a random order to limit potential confounding variables.
Loading Protocols and Imaging
Three-point bending (3PB) was conducted using a TestResources, Inc. electromechanical testing machine (TestResources, Shakopee, Minnesota). Specimens were placed in a custom wooden base that was adjusted for each specimen to allow contact with the metacarpal base and head while the center section was unsupported. A dorsally directed force was applied at the midpoint of the volar cortex of each with a ½-in rounded wooden plunger (Figure 3). The specimens were not further stabilized or constrained. First, a 10-N preload was applied, and then each specimen was loaded from 0 to 100 N at 25 N intervals and 100 to 250 N at 50 N intervals. Subsequently, specimens were loaded from 10 to 1000 N (or catastrophic failure) at a rate of 10 N/s. Catastrophic failure was defined by either audible or visual failure of the construct at the implant-bone interface, with significant displacement.
Figure 3.
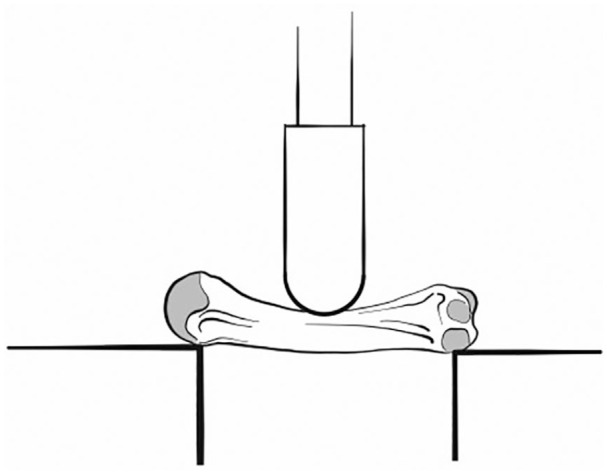
Illustration of loading configuration. Three-point bending at the midpoint of the metacarpal in a volar-to-dorsal direction. The osteotomy was kept 2 mm from the point of contact to allow free motion.
A load-displacement curve was recorded for each specimen. Mechanical load to failure (LTF) was defined as a sharp change in the load-displacement curve, as previously described in similar biomechanical studies.12,13
Statistical Analysis
A forward-selection multiple regression model was completed to evaluate the effect of fixation type (IMN or K-wires), bone mineral density (BMD), and digit (ring or small finger) on LTF and stiffness. Interaction plot analyses were completed to evaluate possible interactions. Across fixation types, BMD was compared with a paired t test, and the occurrence of failure <250 N was analyzed with the Fisher exact test. Due to matched pairing and balancing before specimen preparation, age, sex, laterality, and digit were not compared between groups. Statistical significance was defined as P = .05. With Bonferroni correction, this value was adjusted for multiple comparisons to P = .025 for stiffness and LTF.
Results
The average specimen age was 67 years (range: 51-83 years). Age, sex, sidedness, and digit were evenly distributed between groups. Bone mineral density was similar between groups (T score of −2.83 ± 2.20 and −3.02 ± 2.07 for K-wires and IMN, respectively; P = .1119).
Results are summarized in Table 1. The K-wire fixation demonstrated plastic deformation in 3PB between 75 and 150 N. Of the specimens loaded to failure, all 8 K-wire specimens failed below 250 N, whereas 1 of 8 IMN specimens failed at <250 N (P = .0014).
Table 1.
Comparison Between Fixation Methods.
| Group Characteristic | K-wires (mean ± SD) | IMS (mean ± SD) | P value (statistical test) |
|---|---|---|---|
| Number | n = 16 | n = 16 | n/a |
| Age, y | 67 ± 16 | 67 ± 16 | n/a |
| Sex (M or F) | 50% male | 50% male | n/a |
| BMD (T score) | −3.86 ± 2.62 | −4.14 ± 2.37 | .1806 (t test) |
| Side (L or R) | 50% left | 50% left | 1 (Fisher exact) |
| Metacarpal (4 or 5) | 50% 5th | 50% 5th | 1 (Fisher exact) |
| 3PB failure <250 N (count) | 8/8 | 1/8 | .0014* (Fisher exact) |
| LTF (N) | 164.18 ± 31.76 | 546.93 ± 268.95 | .0005* (t test) |
| Stiffness (N/mm) | 59.28 ± 27.93 | 155.89 ± 42.41 | .00001* (t test) |
Note. Specimens were paired; thus, there is no difference in age, sex, side, or tested metacarpal between groups. IMS = intramedullary screw; 3PB = 3-point bending; LTF = load to failure; BMD = bone mineral density; K-wires = Kirschner wires.
Statistical significance with Bonferroni correction.
The IMN had a significantly higher LTF than K-wires in 3PB (546 N vs 154 N, P = .0005) (Figure 4). The IMN stiffness was higher than K-wires in 3PB (155.89 N/mm vs 59.28 N/mm, P < .001).
Figure 4.
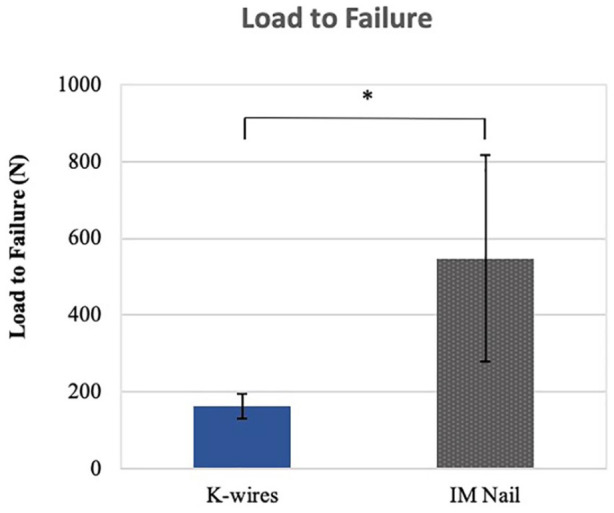
Load to failure of K-wires and IM nails in 3-point bending (*, 546 N vs 154 N, P = .0005).
Note. IM = intermedullary; K-wires = Kirschner wires.
Discussion
The goal of this study was to compare the biomechanical characteristics of an IMN for metacarpal fracture fixation with K-wires. With the application of a 3PB, the IMN had a significantly higher LTF than K-wires (546 N vs 154 N). The IMN was also stiffer than the K-wires in 3PB (155.89 N/mm vs 59.28 N/mm). Our results correlate with findings from Avery et al, 13 who demonstrated increased LTF in the intramedullary screw versus K-wires in both 3PB and axial loading and increased stiffness in the intramedullary screw in axial loading.
The K-wires are commonly used as a method of fixation for metacarpal fractures. 2 Benefits include minimally invasive technique, rapid insertion, and relative ease of use. 13 However, due to the relative weakness of K-wire constructs and to avoid pin-site complications, a period of immobilization is recommended after surgery. 2 This is associated with stiffness and loss of motion when compared with intramedullary implants. 1 In addition to stiffness, complications well described in the literature include pin-site infection, delayed wound healing, soft tissue irritation, and need for a secondary procedure to remove the wires.13,15
Retrograde intramedullary screw fixation is growing in popularity as a minimally invasive option for surgical treatment of metacarpal fractures, demonstrating improved clinical outcomes with early postoperative range of motion.4,10,12 One challenge noted by the authors when using standard 2.4, 3.0, and 3.5 mm HCS is the relative fit within the metacarpal head, neck, and shaft, which naturally taper from a relatively large-diameter space in the neck to a significantly narrower intramedullary space in the isthmus. The IMN evaluated in this study is a threaded intramedullary nail with a tapered diameter designed to optimize intramedullary fit within the metacarpal.
Concerns regarding intramedullary fixation include violation of the articular surface. However, ten Berg et al 10 have previously demonstrated that retrograde intermedullary screw insertion has minimal effects on articular motion and stability. The authors suggested that the defect in the articular surface represented a small percentage of the total articular surface, and if placed in the dorsal third of the metacarpal head, there was little contact with the proximal phalanx with physiologic range of motion. In addition, there were concerns that violating the extensor mechanism for retrograde screw insertion may result in complications, although this has not been shown to be clinically relevant.4,16-23 Further potential complications include hardware loosening with protrusion of the screw into the metacarpophalangeal joint and possible nonunion with hardware failure, both of which require subsequent surgery; however, these are reported to occur rarely. 24
With application of 3PB, peak load to failure for the IMN was significantly higher than K-wires (546 N vs 154 N). The K-wires demonstrated notable plastic deformation that began between 75 and 150 N with the 3PB force applied, whereas the IMN was significantly stiffer (Figure 5). These findings are similar to those by Avery et al and reinforce the protective nature of the IMN with early force application with activities of daily living and range of motion in the postoperative period, as the implant remains in place throughout the healing process.
Figure 5.
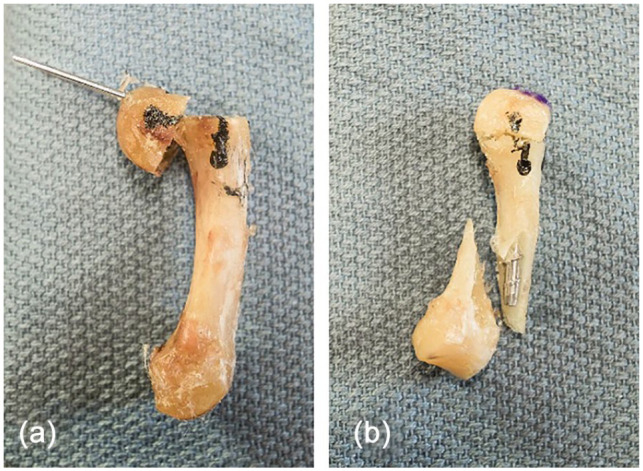
Posttest images demonstrating failure modes of 2 loading configurations: (a) Kirschner wires (K-wires) and (b) intramedullary nails (IMNs).
Note. (a) Three-point bending (3PB) of the K-wire construct where plastic deformation, as seen by K-wire bending at the osteotomy, occurred between 75 and 150 N. (b) 3PB of the IMN which demonstrates reduction at the osteotomy site, but subsequent failure around the implant/shaft interface.
There are several limitations to this study. The use of dissected isolated metacarpals means that stability from adjacent soft tissue structures cannot be assessed. Furthermore, the transverse metacarpal neck osteotomies simulate an axially stable fracture pattern, as described in previous biomechanical studies.12-14 This methodology does not account for other fracture patterns that may exhibit different responses to force application. Our testing simulated the force of the intrinsic and extrinsic flexor muscles with an apex-dorsal 3PB, as previously described.13,25,26
The purpose of this study was to demonstrate the biomechanical properties of a novel IMN as a minimally invasive alternative to commonly used K-wire fixation method. Cadaver metacarpals were used to better simulate native anatomy and in vivo biomechanical characteristics compared with synthetic bone substitutes. Dual-energy x-ray absorptiometry scan data and matched pairs were used to ensure a representative, similarly stratified sample for each respective group.
When surgical fixation is indicated for metacarpal neck and shaft fractures, the IMN provides a biomechanically superior option to crossed K-wires to maintain length and alignment with application of both 3PB axially stable fractures. Given their minimally invasive nature, they may allow for early, resisted motion and return to activity without complications such as loss of reduction or stiffness associated with other constructs. However, the authors recognize that there is not always a correlation between biomechanical stability and improved outcomes. Clinical studies are needed to further investigate their safety, efficacy, and appropriate indications.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: No humans or animals were involved in this biomechanical study.
Statement of Informed Consent: Informed consent was not required for this biomechanical study.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.M. reports royalties and consultant fees from Stryker, consultant fees from Bioventus, consultant fees from ITS, board member of Elsevier, and consultant fees and publishing royalties from Wolters-Kluwer, outside the submitted work. The remaining authors have no conflict of interest to report.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Midhat Patel  https://orcid.org/0000-0002-4282-9584
https://orcid.org/0000-0002-4282-9584
Jill G. Putnam  https://orcid.org/0000-0002-1520-1388
https://orcid.org/0000-0002-1520-1388
References
- 1. Friedrich JB, Vedder NB. An evidence-based approach to metacarpal fractures. Plast Reconstr Surg. 2010;126(6):2205-2209. doi: 10.1097/PRS.0b013e3181f830ad. [DOI] [PubMed] [Google Scholar]
- 2. Kollitz KM, Hammert WC, Vedder NB, et al. Metacarpal fractures: treatment and complications. Hand. 2014;9(1):16-23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Balfour GW. Minimally invasive intramedullary rod fixation of multiple metacarpal shaft fractures. Tech Hand Up Extrem Surg. 2008;12(1):43-45. doi: 10.1097/BTH.0b013e31815678ef. [DOI] [PubMed] [Google Scholar]
- 4. Ruchelsman DE, Puri S, Feinberg-Zadek N, et al. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am. 2014;39(12):2390-2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 5. Randall T, Portney L, Harris BA. Effects of joint mobilization on joint stiffness and active motion of the metacarpal-phalangeal joint. J Orthop Sports Phys Ther. 1992;16(1):30-36. doi: 10.2519/jospt.1992.16.1.30. [DOI] [PubMed] [Google Scholar]
- 6. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827-832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 7. Fusetti C, Meyer H, Borisch N, et al. Complications of plate fixation in metacarpal fractures. J Trauma. 2002;52(3):535-539. doi: 10.1097/00005373-200203000-00019. [DOI] [PubMed] [Google Scholar]
- 8. Geissler WB. Cannulated percutaneous fixation of intra-articular hand fractures. Hand Clin. 2006;22(3):297-305, vi. doi: 10.1016/j.hcl.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 9. Orbay JL, Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006;22(3):279-286. doi: 10.1016/j.hcl.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 10. ten Berg PW, Mudgal CS, Leibman MI, et al. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38(2):322-330.e2. doi: 10.1016/j.jhsa.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 11. Ozer K, Gillani S, Williams A, et al. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724-1731. doi: 10.1016/j.jhsa.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 12. Beutel BG, Ayalon O, Kennedy OD, et al. Crossed K-wires versus intramedullary headless screw fixation of unstable metacarpal neck fractures: a biomechanical study. Iowa Orthop J. 2018;38:153-157. [PMC free article] [PubMed] [Google Scholar]
- 13. Avery DM, 3rd, Klinge S, Dyrna F, et al. Headless compression screw versus Kirschner wire fixation for metacarpal neck fractures: a biomechanical study. J Hand Surg Am. 2017;42(5):392.e1-392.e6. doi: 10.1016/j.jhsa.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 14. Curtis BD, Fajolu O, Ruff ME, et al. Fixation of metacarpal shaft fractures: biomechanical comparison of intramedullary nail crossed K-wires and plate-screw constructs. Orthop Surg. 2015;7(3):256-260. doi: 10.1111/os.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hsu LP, Schwartz EG, Kalainov DM, et al. Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am. 2011;36(4):610-616. doi: 10.1016/j.jhsa.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 16. Beck CM, Horesh E, Taub PJ. Intramedullary screw fixation of metacarpal fractures results in excellent functional outcomes: a literature review. Plast Reconstr Surg. 2019;143(4):1111-1118. doi: 10.1097/PRS.0000000000005478. [DOI] [PubMed] [Google Scholar]
- 17. Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35(8):1260-1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 18. Couceiro J, Ayala H, Sanchez M, et al. Intramedullary screws versus Kirschner wires for metacarpal fixation, functional, and patient-related outcomes. Surg J. 2018;4(1):e29-e33. doi: 10.1055/s-0038-1637002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. del Piñal F, Moraleda E, Rúas JS, et al. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40(4):692-700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 20. Doarn MC, Nydick JA, Williams BD, et al. Retrograde headless intramedullary screw fixation for displaced fifth metacarpal neck and shaft fractures: short term results. Hand. 2015;10(2):314-318. doi: 10.1007/s11552-014-9620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Poggetti A, Nucci AM, Giesen T, et al. Percutaneous intramedullary headless screw fixation and wide-awake anesthesia to treat metacarpal fractures: early results in 25 patients. J Hand Microsurg. 2018;10(1):16-21. doi: 10.1055/s-0037-1618911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Romo-Rodríguez R, Arroyo-Berezowsky C. [Minimal invasive osteosynthesis with cannulated screws in metacarpal fractures]. Acta Ortop Mex. 2017;31(2):75-81. [PubMed] [Google Scholar]
- 23. Tobert DG, Klausmeyer M, Mudgal CS. Intramedullary fixation of metacarpal fractures using headless compression screws. J Hand Microsurg. 2016;8(3):134-139. doi: 10.1055/s-0036-1593390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guidi M, Frueh FS, Besmens I, et al. Intramedullary compression screw fixation of metacarpal and phalangeal fractures. EFORT Open Rev. 2020;5(10):624-629. doi: 10.1302/2058-5241.5.190068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dona E, Gillies RM, Gianoutsos MP, et al. Plating of metacarpal fractures: unicortical or bicortical screws? J Hand Surg Br Eur Vol. 2004;29(3):218-221. doi: 10.1016/j.jhsb.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 26. Prevel CD, Eppley BL, Jackson JR, et al. Mini and micro plating of phalangeal and metacarpal fractures: a biomechanical study. J Hand Surg Am. 1995;20(1):44-49. doi: 10.1016/s0363-5023(05)80057-7. [DOI] [PubMed] [Google Scholar]