Abstract
Study Objectives:
Physician-patient interactions influence the immediate encounter and leave lasting impressions for future health care encounters. We aimed to understand patient experiences and decision-making for considering sleep surgery, in terms of barriers and communication behaviors that facilitate or hinder referral for consideration of sleep surgery management of obstructive sleep apnea (OSA) when continuous positive airway pressure (CPAP) therapy has failed.
Methods:
We employed qualitative methods, using semistructured interviews of adults with OSA who presented for sleep surgery consultation after unsatisfactory therapy with CPAP. Open-ended questions traced symptoms and progression of sleep apnea burden, trials of noninvasive OSA therapies, outcomes, and patient expectations and concerns. The interviews were audio-recorded, transcribed, and analyzed using content analysis to identify themes.
Results:
Ten adult patients with OSA were enrolled March through April 2021 and reached predominant thematic saturation. Barriers to sleep surgery consultation included: (1) delays in OSA diagnosis due to limited OSA awareness among patients or primary providers and patients’ perceived inconvenience of sleep testing, (2) patients faulted for slow progress, (3) patient-reported lack of urgency by providers in troubleshooting noninvasive management options, (4) scheduling delays and waitlists, and (5) cost. Patients were receptive to noninvasive treatment options, but inadequate improvement led to frustration after multiple encounters. Patients appreciated empathetic providers who shared information through transparent and understandable explanations and who presented multiple treatment options.
Conclusions:
Experiences of patients with OSA highlight the need for shared decision-making through improved communication of unresolved concerns and alternative management options, including timely referral for sleep surgery consultation when indicated.
Citation:
Ikeda AK, McShay C, Marsh R, et al. Barriers and communication behaviors impacting referral to sleep surgery: qualitative patient perspectives. J Clin Sleep Med. 2023;19(1):111–117.
Keywords: qualitative methods, obstructive sleep apnea, patient perspectives, communication behaviors, barriers
BRIEF SUMMARY
Current Knowledge/Study Rationale: Qualitative methods provide rich information about patient experiences, which provides deeper understanding of current barriers or limitations in health care management. Management of patients with obstructive sleep apnea is complex, with multidisciplinary care and multiple therapy options, which together present unique challenges and nuances that may impact timely referral for sleep surgery consultation when indicated.
Study Impact: Patients with obstructive sleep apnea who have difficulty with continuous positive airway pressure perceive delays and barriers in ultimately reaching sleep surgery consultation. Each health care encounter—with primary care provider, sleep specialist, and sleep surgeon—matters, and patients are most responsive to empathetic providers who provide transparent information with understandable explanations.
INTRODUCTION
Patients with obstructive sleep apnea (OSA) are confronted with difficult decisions regarding optimal management of this condition since multiple treatment options exist. First-line nonsurgical treatment options for OSA, including continuous positive airway pressure therapy (CPAP), are often untenable and prompt consideration for sleep surgery.1 There is often a stepwise approach to management of OSA, from trialing and troubleshooting noninvasive therapy, before the transition to more involved or invasive treatment options, like sleep surgery. Considering the recent clinical guidelines on referral of adults with OSA for surgical consultation,2 there is a need for deeper understanding of current barriers faced by patients with OSA who are considering and seeking referral for sleep surgery, as these barriers can lead to costly delays or missed opportunities.
Sleep surgery can open and stabilize the upper airway during sleep, but it carries perioperative risks, often followed by painful recovery (lasting weeks to months) and is associated with variable outcomes. Risks and benefits vary by type of sleep surgery. Additionally, patients and providers assess the sleep apnea burden and desired treatment outcomes differently, including by physiological parameters (eg, apnea-hypopnea index), symptom severity (eg, sleepiness, snoring), quality of life, function, and long-term health risks. These differing characterizations of the disease burden add variation to reported outcomes and satisfaction. Patients considering sleep surgery must weigh the severity of their OSA burden against the risks and potential benefits they may receive following various forms of sleep surgery, which is a complex decision.
A recent study found patients with OSA considering sleep surgery demonstrated high decisional conflict, as measured by a validated 4-item decisional conflict screening scale (SURE).3 Among the 100 patients with OSA enrolled, over half of the patient sample reported uncertainty in optimal treatment choice and lack of knowledge of treatment-option risks and benefits.3 This self-reported lack of knowledge is anticipated to negatively impact patients’ decision-making. Additionally, misinformation about sleep surgery, which can be difficult to discern, can be found in information resources used by patients, including internet searches, social media, and family/friend interactions. Thus, sleep specialists at each patient encounter are in the unique position to offer effective counseling and recommendations that are tailored to patient needs, address potential falsehoods, and filter patient interpretations.
Qualitative methods provide an exploratory and in-depth approach to understanding the patient experience and patient factors that influence decision-making, which is crucial to improving the longitudinal physician-patient relationship surrounding OSA management. Prior qualitative work reported that adult patients with OSA who were considering sleep surgery (specifically a modified or traditional uvulopalatopharyngoplasty) had significant OSA burden impacting personal and professional life and motivations for undergoing surgery.4 However, the health care encounters and duration of decision-making to choose sleep surgery was not elicited and represent important aspects in this process, as delayed decision-making or barriers to surgical consultations could negatively influence a clinically meaningful improvement. In another cohort of patients with OSA who underwent sleep surgery, the decision to elect sleep surgery was reported to be up to 2 years after the sleep surgery consultation, due to information gathering and weighing of options.5 This emphasizes the need to introduce the role of sleep surgery early in discussions of management and optimization of care. Avoiding sleep surgery consideration in these early management discussions may further delay beneficial OSA treatment if CPAP does not succeed.
We aimed to understand the experiences of patients with OSA from initial presentation of sleep symptoms to surgical consultation, in terms of barriers and communication behaviors that either hindered or facilitated referral for consideration of sleep surgery when CPAP therapy had failed. Our approach intended to identify potential delays in management that could be targeted to improve patient experiences, facilitate effective decision-making, and minimize barriers to care at all levels (primary care, sleep specialist, sleep surgeon, and staff). The goal was to improve clinical outcomes by optimizing communication with patients and enabling timely and informed decisions regarding sleep surgery.
METHODS
Study design
Patients (aged ≥ 18 years old) with OSA (defined as preoperative apnea-hypopnea index ≥ 5 events/h of sleep, scored by American Academy of Sleep Medicine-accredited standards) who had been evaluated for and offered sleep surgery treatment at Harborview Medical Center were eligible. Sleep surgery treatments included nasal surgery, pharyngeal surgery, or staged surgery (a combination of nasal and pharyngeal surgeries to be performed separately). Referrals of patients who were evaluated at the sleep surgery clinic stemmed from both internal and external referral networks, given the limited number of sleep surgeons in the region. Inclusion criteria included English fluency, willingness to provide consent, and access to video interview. Exclusion criteria included patients who had undergone prior sleep surgery at this facility, though a history of adenotonsillectomy or sinus surgery at another facility (often during childhood) was not an excluding criterion. This ensured eligible patients would not have established relationship with our clinic, which could have influenced findings. The selection process provided a representative sampling of patients, in terms of age, sex, range of OSA severity and symptoms, as well as other clinical variables.
Recruitment and enrollment
We contacted eligible patients electronically after scheduled sleep surgery consultation. Video meetings for introduction, informed consent, and the subsequent recorded interview were arranged within 2 weeks of sleep surgery consultation or postoperative visit. These study procedures were in line with the University of Washington’s COVID restrictions on clinical research, and Institutional Review Board approval was obtained (STUDY00011521). The Standards for Reporting Qualitative Research were followed for this qualitative study.6 Informed consent was obtained from all patients at enrollment.
Data collection and interviewing
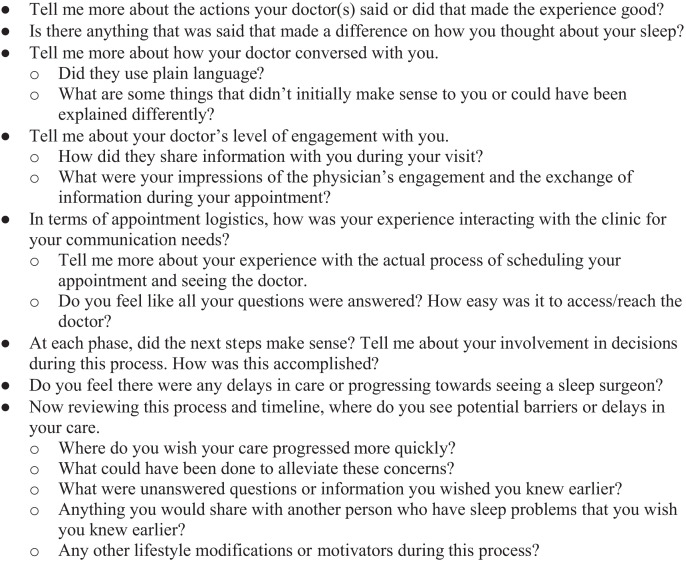
After informed consent was obtained, recordings followed the semistructured interview guide created by the research team. This guide consisted of open-ended questions, with a subset of questions focusing on physician behaviors and barriers in reaching sleep surgery referral. The interview guide was based on prior qualitative studies examining decision-making and sleep surgery among adults and children.3–5,7,8 An abbreviated interview guide is shown in Figure 1. All interviews were audio-recorded, transcribed, and de-identified prior to analysis.
Figure 1. Abbreviated interview guide.
A subset of questions from the semistructured interview guide that correspond with evidence included in analysis.
Data analysis and thematic content approach
Transcripts were analyzed using conventional thematic content analysis.9 Analysis consisted of: (1) identifying key concepts and overarching themes and associated subtheme clusters, (2) coding response segments to correspond to identified subthemes, and (3) creating summaries of themes. The goal of analysis was to identify emergent themes within an established a priori framework.
The initial stage of coding was performed immediately following conduct of each interview by 2 independent research team members, and recruitment continued until predominant thematic saturation was reached within a convenience sample. We used a broad definition of predominant thematic saturation to mean when data collection and analysis were identifying little or no new information related to the study questions. At this stage, all transcripts were reviewed again for additional theme identification as an iterative process. All discrepancies in coding were discussed by the research team in order to change consensus. Representative de-identified quotes were compiled and summarized to support each theme. Following each quote is the type of surgery recommended in brackets to provide context (see Results). Based on the literature, we anticipated thematic saturation between 10 and 18 interviews.4 All de-identified transcripts were stored on a secure, Health Insurance Portability and Accountability Act–compliant, firewall-protected network. Consent documentation was hosted on the Research Electronic Data Capture (REDCap) database.
RESULTS
We approached and enrolled 10 consecutive eligible adult patients with OSA, who were evaluated and recommended sleep surgery, between March 8, 2021 and April 21, 2021. The sample was representative of patients with OSA, composed of (on average) middle-aged, predominantly male, and overweight patients (mean age 41 ± 14 years old, 80% male, and mean body mass index 29 ± 6, respectively). Eighty percent were married, half had commercial health insurance at time of consultation (and half had government insurance), and 30% reported a history of airway surgery (history of adenotonsillectomy or sinus surgery at other facility, often during childhood). On average, patients had moderate OSA (mean apnea-hypopnea index 27 ± 15 events/h). Sleep apnea burden varied by measure (severity, symptoms, and quality of life) (Table 1).
Table 1.
Characteristics of interviewed patients with OSA.
| Characteristic | |
|---|---|
| Age (years) | 41 ± 14 |
| Sex (M/F) | 8/2 |
| Body mass index | 29 ± 6 |
| Preoperative apnea-hypopnea index (events/h) | 27 ± 15 |
| History of prior airway surgery (yes) | 30% |
| Marital status (married) | 80% |
| Insurance status (commercial) | 50% |
| Epworth Sleepiness Scale | 9.4 ± 5.9 |
| SNORE-25 | 2.2 ± 1.0 |
Mean ± SD displayed for continuous variables with normal distribution. Categorical variables are reported in prevalence (%). Symptoms of nocturnal obstruction ad related events-25 (SNORE-25) is a validated OSA specific quality of life measure.
Mean interview session duration was 62 ± 11 minutes. Barriers to the sleep surgery consultation included: (1) delays in OSA diagnosis due to limited OSA awareness among patients or primary providers and patient perceived inconvenience of sleep testing, (2) patients faulted for slow progress, (3) patient-reported lack of urgency by providers in troubleshooting noninvasive management options, (4) scheduling delays and waitlists, and (5) cost. Patients were open to noninvasive treatment options, though opportunities for reevaluation and shared decision-making may address unmet needs, as inadequate improvements led to frustration after multiple encounters. Patients appreciated empathetic providers who shared information through transparent and understandable explanations and who presented multiple treatment options.
Barriers to sleep surgery consultation
Patients reported several barriers to reaching a sleep surgery consultation. One patient reported a 2-year delay in OSA diagnosis, possibly due to limited sleep apnea awareness (“It’s unfortunate it took so long to get the initial diagnosis. Symptoms started at end of 2017, and I finally got a diagnosis in January 2020. I feel that was a big delay because there isn’t a lot of sleep apnea awareness.” [nasal adjunctive surgery]). Others reported a perceived inconvenience of the sleep test, delaying diagnosis (“[The sleep test] sounded like a big pain to get done. Is it bad enough that I need to go have people watch me sleep?” [nasal adjunctive surgery]). Another patient reported feeling frustrated by feeling at fault for sleep symptoms and associated weight (“Sometimes I’d be [criticized for] my weight. It was frustrating because they made it sound like it was my fault.” [nasal adjunctive surgery]).
Frustration was a common feeling, due to the perceived lack of urgency by providers and scheduling. One patient reported feeling ashamed, frustrated, and distraught (“I felt ashamed I have a problem….I ended the [visit] incredibly frustrated and distraught because I didn’t feel there was any urgency to these really bad [sleep test] results.” [pharyngeal surgery]). Another patient reported the burden of the symptoms (“I was frustrated. I was disheartened. These feelings of being tired all the time and dealing with all the symptoms.” [nasal adjunctive surgery]). Another reported concern about the quality of the sleep test data, due to limited sleep time, and potential delays in care, which led them to seek referral from another provider (“I was concerned [the sleep test] didn’t have enough data. I reached out immediately to see if we needed to schedule another sleep [test] and to do it right away…. They never responded to my query, so I was sitting in limbo. [Then] I saw my [primary care provider] and [they] gave me a recommendation for [sleep surgery].” [nasal adjunctive surgery]). Another patient reported desire to understand the underlying cause of symptoms and to know potential options (“I knew I wanted to move forward with whatever resolution, so I had hoped that [the provider] would break down any potential options I have and tell me exactly what the issue was.” [nasal adjunctive surgery]).
Additionally, other patients reported long delays in waiting for a referral to a sleep surgeon (“[Referral to sleep surgery] took the longest amount of time, though I had to do [CPAP], a treatment that everyone knew wasn’t going to work [for me].” [nasal adjunctive surgery]). Patients also expressed frustration with multiple visits to sleep medicine providers and unaddressed issues with CPAP intolerance (mask fit, removing during sleep) (“There wasn’t a lot of information given to me. My main takeaways were that I wasn’t going to talk to [sleep provider] for a long time until after a sleep [test] with CPAP.” [nasal adjunctive surgery]). This encounter left the patient unclear about what to expect, despite the patient’s motivation to know what else to consider in the meantime. Another patient reported no solutions to the CPAP mask coming off with movements while sleeping (“The problem is I move too much when I sleep, so after one hour I realized my CPAP is on the other side of the bed or on the floor.” [staged surgery]). Improved communication on what information is needed for further recommendations would be helpful for the bigger picture management plan.
Last, the financial cost of the sleep medicine visit and potential sleep testing sometimes delay seeking evaluation (“I had to pay for those appointments, so I decided to wait to go to the sleep clinic. I was waiting until last year, when I got a permanent job and I have medical insurance.” [staged surgery]). Another patient reported inconsistencies in health care insurance coverage and other differential diagnosis workups distracting from sleep medicine evaluation; however, the sleep medicine evaluation led to improvements in other aspects of their health.
Communication between providers and patients
Conversations with primary care providers or sleep providers about sleep test results and management options are important. One patient recalled good communication (“I talked to the [primary care provider] about the symptoms, and they told me that this is a common problem in the United States because of the food and the way we live.” [staged surgery]). However, initial patient reactions to sleep test results varied, including validation, shock, or concern, which can impact subsequent progress. Patients learning about their sleep study results may need to time to process this new information, while others may not. One patient reported after hearing sleep test results, thinking “Wow, this sucks and, hopefully, I can get something done,” while another patient reported the sleep test results were consistent with their “hunch.” Assessing what information the patient is ready to receive is important, as well as arranging follow-up for continued discussions that may be necessary to review options.
Some patients appreciated trialing different options and the empathy their sleep providers shared (“[The sleep provider] verified everything I thought. [They] said try a wedge pillow, try this sensor that goes on your neck, and I thought those are great ideas. I liked the empathy.” [nasal adjunctive surgery]). Other patients expressed mixed feeling about CPAP and other noninvasive treatment options (“The CPAP was given as a solution and was really disheartening because it seemed like a band aid. I was very hopeful that there would be better alternatives.” [nasal adjunctive surgery]). Another patient shared similar sentiment about CPAP (“I did not feel good about the current treatment plan that I had with my doctor—a no win scenario, with no options on the horizon, as to what I can do, except hopefully sleep surgery.” [nasal adjunctive surgery]). Other patients face significant difficulty tolerating CPAP and reported, “Believe it or not, I get better rest, if I sleep less time [without CPAP]… than when I sleep my eight hours with CPAP” [staged surgery].
If the management option did not adequately improve sleep symptoms, these feelings often transition to frustration after multiple encounters with providers (“[The sleep provider] is a nice [person] but they didn’t seem very proactive. When [CPAP] didn’t work they didn’t seem to ‘take the bull by the horns’ and say, ‘Okay, that’s not working. Let’s try this.’” [pharyngeal surgery]). Another patient reported, “[The sleep provider] that I had at the time, I did not have very good communication with them at all. It didn’t seem like [the sleep provider] had any other suggestions, so it seemed like a dead end” [pharyngeal surgery]. In some cases, frustrated patients sought out information from online resources and family/friends, and then self-advocated for sleep surgery referral.
Effective communication included information sharing and empathy
Ineffective information sharing included limited discussion regarding alternative options to CPAP. One patient reported, “CPAP was the only thing that I was instructed to do, and I was struggling to use it….There wasn’t much time, probably a solid 2 and a half or three weeks, when I was using it well, or using it often, and then the last week or 2 not well at all. I couldn’t fall asleep or kept waking up….It’s the friction on my nose or breaking the seal or both” [nasal adjunctive surgery]. Another patient: “I thought CPAP was the better option from what [the provider] had said and from what we discussed CPAP seemed like the only real option. That’s why I wanted to give it another shot again, though it was frustrating” [nasal adjunctive surgery].
Patients responded well to providers who shared information (“I didn’t have to ask [them] very much at all, because [they] were so thorough and explained each of the possibilities.” [pharyngeal surgery]). Similarly, the sleep surgeon was reported to be validating and well received (“I felt the ENT [sleep surgeon] at least matched the severity and urgency of what was happening to me: ‘You must feel awful not being able to get any sleep. People have trouble with CPAP and stop using it, and then go back into the same cycle, so it’s good that you’re looking for more alternatives.’ I felt better that someone validated how I was feeling about everything.” [nasal adjunctive surgery]). Another patient reported effective communication with understandable explanations and eye contact (“Taking time to explain things in a very understandable manner. I have had a lot of doctors that don’t explain things very well and go very fast, but I was able to comprehend and understand everything. [They] looked me in the eye when talking.” [pharyngeal surgery]). Another patient reported detailed discussions about the surgeries and use of visual aids (“[The sleep surgeon] recommended three separate surgeries and went through them in very good detail and even had diagrams on the walls.” [nasal adjunctive surgery]), while another patient highlighted the impact of details about recovery and pain (“[The sleep surgeon] went into detail about recovery time and pain, so I feel that between all of that I was informed and ready to make a decision.” [nasal adjunctive surgery]). Last, patients appreciated understanding and being involved in the thought process for management considerations (“It was the thought process—how [they] systematically whittle things out and communicating that. Being transparent in terms of how [they are] coming to these conclusions. ‘It may be this and I am looking at that’ and ‘That eliminates it down to this.’ That type of logic definitely helps.” [staged surgery]).
DISCUSSION
Patients with OSA encounter with the health care system on multiple levels, including primary care, sleep medicine, sleep surgery, sleep dentistry, and others. Often there are several visits to establish a diagnosis and then several more visits with sleep medicine to discuss management options and to optimize and troubleshoot options. Each encounter is meaningful and impacts how patients understand and choose future management options for OSA.
Unfortunately, there is a subset of patients with OSA for whom noninvasive options are inadequate in managing OSA burden. In a retrospective chart review of 1,174 patients with OSA, about half of patients were adherent to positive airway pressure therapy after 3 years, and roughly a third of the remaining untreated patients with OSA were referred for other management options, including sleep surgery or oral appliance.10 In particular, 12.4% of untreated patients with OSA were referred to an otolaryngologist.10 We recognize the perspectives included in our sample represent a subpopulation of patients with OSA and thus cannot be generalizable to represent the experiences of all patients with OSA. However, cases when sleep surgery can be considered represent a crucial subset of patients whose care could be optimized.2 In our study, we focused on patients with OSA who were offered sleep surgery; our goal was to understand their experiences from symptom onset through reaching surgical consultation. This project was timely with the recent American Academy of Sleep Medicine’s “Referral of adults with obstructive sleep apnea for surgical consultation: an American Academy of Sleep Medicine clinical practice guideline.”2 The guideline and accompanying evidence review2 highlight the role and timing of referral to sleep surgery, and our study complements this work by focusing on the patient experiences that impact referral to sleep surgery. Barriers and communication behaviors were the main focus, and qualitative methods were employed to best describe the in-depth patient experiences and to uncover themes that may not otherwise be appreciated through broad surveys or other measures. Additionally, the patient perspectives and reflections from initial sleep symptoms to surgical consultation examined the impact of patients’ multidisciplinary teams and highlighted the need for improved counseling to minimize delays and optimize treatment.
Patients with OSA who present to clinics are motivated to improve their sleep, in addition to their overall health, and providers’ empathy facilitates those outcomes. Often patients have waited weeks or months to be evaluated and are hopeful for relief from their OSA burden. Listening to their concerns and providing a clear and transparent exchange of information will provide context for information from outside resources or resolution of conflicting information. Additionally, these conversations can lay the foundation for ongoing troubleshooting and expectations for timing of transitions to other options. All providers know these fundamental approaches to patient care, but they are time-consuming and can fade in the context of a repetitive, routine, systematic approach to evaluating OSA and initiating CPAP therapy. Above all, OSA is best managed with a multidisciplinary approach, which provides opportunities for ongoing discussions and reassessment of clinical progress. Patients with OSA who present for evaluation are interested in improving their health, and their visits can be optimized by providing accurate information and expectations.
Study limitations include generalizability and team positionality. Our enrollment was from a single tertiary sleep surgery practice, but it drew from both community and academic referral sources. The patients typically had failed conservative medical management (CPAP and lifestyle modifications) prior to evaluation for sleep surgery, which is often the situation in community sleep surgery practices too. They may have failed medical management for a variety of reasons, and their frustration may have motivated the pursuit of surgical consultation, as there were frequent reports of frustration throughout the whole process of OSA management. Additionally, we understand that our patient sample is biased to patients who may be highly motivated to pursue sleep surgery (or at least to consider it) as a means of OSA treatment, especially given their willingness to wait 1 or more months for consultation. We speculate that patients who never reach a sleep surgery consultation after CPAP failure may just have given up on treating their OSA and may be even more frustrated, which is grounds for studying other populations of patients who are still in the midst of the whole process (ie, before surgery consultation). We also recognize other factors may impact timing and expectations, including: (1) relationship status, as bed partners often report symptoms or are impacted by sleep symptoms, (2) health insurance status, as any surgical procedure carries financial burden and depends on insurance status, and (3) history of prior airway surgery, as prior experience and outcome may influence future decision-making. Our sample offers a mix of real-world patient perspectives.
The research team included members from both clinical and research backgrounds and from different departments and institutions; however, the research team did not include sleep medicine or primary care providers. Future research will benefit from studying different cohorts of patients at various stages of OSA care who are still working directly with other providers. The multiple interview moderators (A.K.I., C.M., R.M., S.S.) offered diverse training and backgrounds, which provided greater insight into new and possible themes, which is a strength of this study. Last, we are confident we reached predominant thematic saturation with our enrollment, given the duration of each interview, depth each patient was willing to share, and lack of new emergent themes in the later interviews; however, remaining untapped themes still may exist. Prior qualitative methodological studies have reported that a majority (70%) of new information is identified in the first 5 or 6 interviews, and that 92% of identified themes typically are identified within the first 12 interviews.11 We believe the underlying referral pattern and specifics relative to the sleep surgery practice contribute to reaching thematic saturation efficiently in this sample. In our sleep surgery practice, the sample represents roughly 10% of new sleep surgery consultations annually. This highlights the benefit of expanding future studies to include different clinical sites and consideration of different phases of the treatment journey (Ikeda AK, McShay C, Marsh R, et al. Understanding patient experience leading to sleep surgery consultation through journey mapping. JAMA Otolaryngol Head Neck Surg. [submitted]).
Future related directions include development of interventions to minimize these barriers to surgical consultation, when indicated2; for example informational modules that lay out common pathways of care and options to consider, along with evidence-based information about each. Similarly, development of surveys that assess and reassess patient goals and preferences in specific treatment options could tailor conversations during patient visits and potentially include introductory conversations about alternative therapies earlier when trialing primary management options, if appropriate. Qualitative research methods offer depth and richness to understand the patient experience, which is crucial in providing high quality care. Future work includes assessing patient experiences in other sleep medicine and sleep surgery settings, including community practices, assessing during different phases of management, and assessing impacts of other prior experiences or factors (prior care, health insurance status, etc.) on interpretation of encounter and information sharing. The application of qualitative methods in sleep medicine and sleep surgery remains limited and its use holds promise for improved decision-making and quality of care.
CONCLUSIONS
Patients with OSA face multiple treatment options. They benefit from ongoing conversations to optimize their care. These conversations involve sleep medicine and primary care providers, and in some cases, sleep surgeons. As the timing of when to consider a sleep surgery referral becomes clearer with the recent guideline, this qualitative study identifies barriers and communication behaviors that hinder or facilitate appropriate referral for consideration of sleep surgery management. Experiences of patients with OSA and barriers faced highlight the need for improved communication structures to discuss unresolved concerns and remaining management options, thus setting the foundation for shared decision-making for the optimal treatment of patients with OSA.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Funding provided by American Academy of Otolaryngology–Head and Neck Surgery Resident Research Grant and NIH T32 DC000018. Dr. Weaver’s effort was supported, in part, by the Seattle Veteran Affairs Medical Center; the contents do not represent the views of the United States Government. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: A.K.I. had substantial contribution to funding, conception, study design, data collection and analysis, data interpretation, and drafting of manuscript for final submission. C.M. had substantial contribution to data collection and analysis, data interpretation, and drafting of manuscript. R.M. had substantial contribution to data collection and analysis, data interpretation, and drafting of manuscript with revisions. S.S. had substantial contribution to data collection and analysis, data interpretation, and drafting of manuscript. M.S. had contribution to conception, study design, data interpretation, and revisions of manuscript. E.F.B. had contribution to conception, study design, data interpretation, and revisions of manuscript. E.M.W. had substantial contribution to funding, conception, study design, participant enrollment, data interpretation, and revisions of manuscript.
ABBREVIATIONS
- CPAP
continuous positive airway pressure
- OSA
obstructive sleep apnea
REFERENCES
- 1. Weaver TE , Grunstein RR . Adherence to continuous positive airway pressure therapy: the challenge to effective treatment . Proc Am Thorac Soc. 2008. ; 5 ( 2 ): 173 – 178 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kent D , Stanley J , Aurora RN , et al . Referral of adults with obstructive sleep apnea for surgical consultation: an American Academy of Sleep Medicine clinical practice guideline . J Clin Sleep Med. 2021. ; 17 ( 12 ): 2499 – 2505 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gulati A , Stephens EM , Cai Y , Chang JL . Characterizing decisional conflict in patients presenting to sleep surgery clinic and an exploration of resource limitations . Laryngoscope. 2021. ; 131 ( 10 ): 2384 – 2390 . [DOI] [PubMed] [Google Scholar]
- 4. Rudolph MA , Rotsides JM , Zapanta PE . The patient’s perioperative perspective during the treatment of obstructive sleep apnea: a pilot study . Sleep Breath. 2018. ; 22 ( 4 ): 997 – 1003 . [DOI] [PubMed] [Google Scholar]
- 5. Ikeda AK , McShay C , Marsh R , et al . Patient factors and preferences in choosing sleep surgery for obstructive sleep apnea: a qualitative study . Otolaryngol Head Neck Surg. 2022. . [DOI] [PubMed] [Google Scholar]
- 6. O’Brien BC , Harris IB , Beckman TJ , Reed DA , Cook DA . Standards for reporting qualitative research: a synthesis of recommendations . Acad Med. 2014. ; 89 ( 9 ): 1245 – 1251 . [DOI] [PubMed] [Google Scholar]
- 7. Boss EF , Links AR , Saxton R , Cheng TL , Beach MC . Parent experience of care and decision making for children who snore . JAMA Otolaryngol Head Neck Surg. 2017. ; 143 ( 3 ): 218 – 225 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Links AR , Callon W , Wasserman C , et al . Parental role in decision-making for pediatric surgery: perceptions of involvement in consultations for tonsillectomy . Patient Educ Couns. 2020. ; 103 ( 5 ): 944 – 951 . [DOI] [PubMed] [Google Scholar]
- 9. Hsieh HF , Shannon SE . Three approaches to qualitative content analysis . Qual Health Res. 2005. ; 15 ( 9 ): 1277 – 1288 . [DOI] [PubMed] [Google Scholar]
- 10. Russell JO , Gales J , Bae C , Kominsky A . Referral patterns and positive airway pressure adherence upon diagnosis of obstructive sleep apnea . Otolaryngol Head Neck Surg. 2015. ; 153 ( 5 ): 881 – 887 . [DOI] [PubMed] [Google Scholar]
- 11. Guest G , Namey E , McKenna K . How many focus groups are enough? Building an evidence base for nonprobability sample sizes . Field Methods. 2017. ; 29 ( 1 ): 3 – 22 . [Google Scholar]