To the editor,
Since December 7, 2022, China lifted the strict COVID-19 control policy. Here we quantitatively analyze its potential impacts on COVID-19 trend with the epidemiological model SUVQC using the population and parameter settings of Beijing as a case. Our results indicate that if non-pharmacological interventions are completely ceased, the ICU bed demand number will peak in 26 days at ∼23.88 thousand, which is 18 times the total number of ICU beds in Beijing. COVID-19 Omicron will cause 31,817 deaths in Beijing in the first year. We urge that the flattening curve strategy is necessary to slow down the infection and avoid overwhelming the healthcare system.
In the past three years, China had been implementing severe policy to control the COVID-19 epidemic. On December 7 2022, China National Health Commission lifted the control policy by announcing the Ten New Covid Rules. Most cities in China ceased strict local measures since then. In Beijing, the regular nucleic acid (RT-PCR) testing and the health code checking are not required anymore; and tested positive patients with mild symptoms can be self-quarantined at home. However, the current vaccination rate (proportion of booster doses administered) in China is only 56.9 % (https://ourworldindata.org/covid-vaccinations, Our World in Data),1 most of which are inactivated vaccines with lower protection efficacy. The pandemic trend is unclear under the drastic swing of containment policy, although Omicron causes much milder symptoms. Here we quantitatively assess the potential impact of the new measures. We analyze the level of healthcare system being overwhelmed after retracting the severe COVID-19 control policy, and compare the number of ICU beds demanded and available in Beijing.
We use the SUVQC model to estimate the number of ICU bed needs with the following parameter settings.2 , 3 The basic reproductive number (R0) of Omicron is set to be 9.5 following previous studies;4 the generations time is 2.2 days;5 hospitalizations and ICU admissions are 2.6% 6 and 0.27% (the number is chosen based on the estimation of risk of developing severe/critical disease in Shanghai,7 smaller than the estimation of 0.47% in the US6) for Omicron patients, respectively. The mean ICU bed occupation time is estimated to be 12 days per individual based on the daily ICU admissions for COVID-19 in the US (https://ourworldindata.org/covid-hospitalizations, Our World in Data), the proportion of patients who require ICU care, and the daily number of new cases in the US. Assume that the duration of immunity against COVID-19 is one year after the infection and with 100% protection efficacy. We set U0 (the number of initial infected individuals who are infectious and unquarantined) to be 200, identical to the number of infected from social screening reported by Beijing Municipal Health Commission in December 7, 2022. The number of C0 (the number of initial cumulative confirmed infected cases) to be 19,588 (https://voice.baidu.com/act/newpneumonia/newpneumonia/).
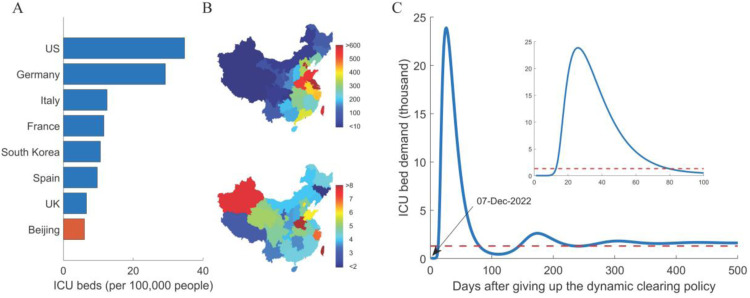
Our analysis indicates that the ICU bed demand will peak at ∼23.88 thousand, around 26 days after retracting the severe control policy, which is 18 times the total number of available ICU beds in Beijing. Considering we may underestimate the basic reproductive number and the initial unquarantined infected number, the peak time of ICU bed demand may be earlier than the estimation with higher peak value. After several waves of ups and downs, the number of active cases and ICU bed demand will reach an equilibrium state. At this state, the daily new confirmed cases will be around 50,000 and the ICU bed demand is around 1,617; even if all ICU beds are available for the treatment of COVID-19 patients, they still can only cover 81.76% of the demands (Before the end of 2021, the total number of ICU beds in Beijing is 1322, and the ICU per 100,000 people is 6.04,8 which is only 17.40% of that in the United States, https://ourworldindata.org/, Fig. 1 A).
Fig. 1.
Healthcare system overwhelmed by the shortage of medical resources after retracting the severe COVID-19 control policy.
(A) ICU beds per 100,000 people compared with the developed countries. (B) Uneven distribution of population and medical resources in China. The colors on the below map represent population density and the colors on the bottom map represent the number of ICU beds per 100,000 people. (C) Prediction of the ICU bed demand using SUVQC model after retracting the severe control policy. We used the hospitalizations rate of 2.6% and the ICU admissions rate of 0.27% for Omicron patients. The red line indicates the total number of ICU beds in Beijing.
The peak number of active cases and hospitalizations will reach 8.85 million and 0.23 million, respectively. The equilibrium values of these two numbers will be 0.5990 million and 0.0156 million. By assuming a fatality ratio of 0.09% under situations without overwhelming the healthcare system,7 it will cause 31,817 deaths in the first year, and ∼16,397 deaths annually in the following years. According to previous studies, the average number of hospitalization days due to influenza was 8.6199 days; the number of hospitalizations due to lower respiratory tract infection of influenza in China was 739,000;9 and the total hospitalization days were 6.37 million days. On average, 52,400 people occupy hospital resources every day during the flu season. For Beijing, the influenza burden for hospital is around 819 per day in proportion of population. The hospitalizations caused by Omicron infection will be 19.02 times that caused by influenza during flu season.
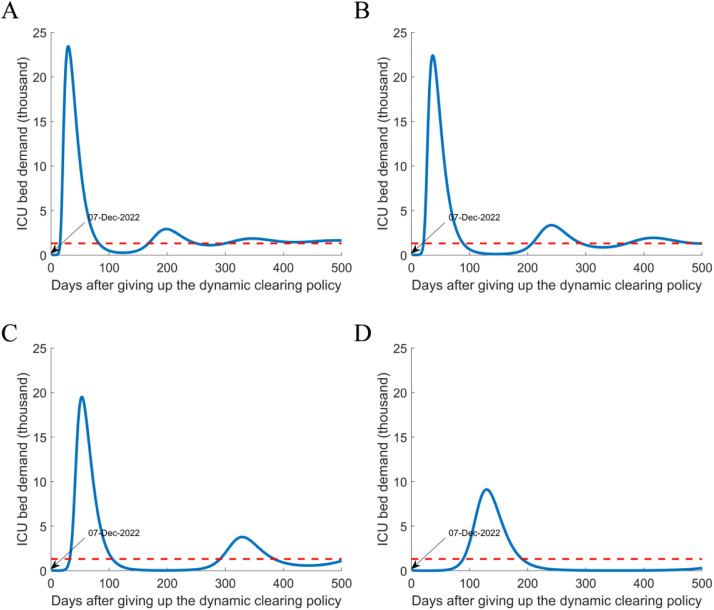
To avoid overwhelming the healthcare system at the equilibrium state in Beijing, we need ∼1617 ICU beds for SARS-CoV-2 patients, and more professional doctors and nurses. We have to flatten the curve of the first wave of the pandemic after relaxing the severe control policy (Fig. 2 ). The flattening curve strategy is different from the severe COVID-19 control policy, which aims to restrict the spread of the virus, and the herd immunity strategy of complete liberalization. Flattening curve strategy is to keep the rate of virus spreading low enough with some level of non-pharmacological interventions (NPI). The goal is to diminish the spread of the epidemic to avoid straining the health care system so that severely ill patients can receive medical treatment; and put medical resources at the maximum load of treating new coronary pneumonia patients such that the population can achieve herd immunity at the fastest speed while under the premise of the lowest number of deaths. For flattening curve strategy, Rt is still > 1, and the epidemic spreads exponentially but with a lower rate. In addition, the economic loss is smaller in the short term than the rigorous interventions under the severe COVID-19 control policy.
Fig. 2.
Estimation of ICU demand under different NPI intensities of the flattening curve strategy.
(A-D): 80%, 60%, 40%, and 20% of transmissions of the usual level. The peak values are 23444, 22414, 19511, and 9124, respectively.
Note that the distribution of medical resources in China is extremely uneven (Fig. 1B) and the bed utilization rate is generally higher than 60%. The situation in areas outside Beijing will be even worse. It is necessary to adopt the flattening curve strategy, and in the meanwhile, accelerate the development of drugs for hospitalized patients and vaccines with more protection efficacy.
To implement the flattening curve strategy, we urge increasing the vaccination rate of the elderly to reduce deaths and relieve medical pressure. Higher levels of NPI, including, social distancing, wearing masks, indoor ventilation and air filtering, regular rapid antigen tests (RAT) and self-examination, and restricted access to public space for those tested positive with RAT, are still very necessary to slow the spread of the virus.
CRediT authorship contribution statement
Shilei Zhao: Formal analysis, Writing – original draft. Tong Sha: Formal analysis. Yongbiao Xue: Supervision. Hua Chen: Writing – original draft, Supervision.
Declaration of Competing Interest
The authors declare no competing interests.
Acknowledgments
The work was supported by the National Key R&D Program of China (Grant No.2021YFC0863400).
References
- 1.Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5(7):947–953. doi: 10.1038/s41562-021-01122-8. JulPubMed PMID: 33972767. Epub 2021/05/12. [DOI] [PubMed] [Google Scholar]
- 2.Zhao S., Sha T., Wu C., Xue Y., Chen H. Will the large-scale vaccination succeed in containing the COVID-19 pandemic and how soon? Quant Biol. 2021;9(3):304–316. 2021-09-15. [Google Scholar]
- 3.Zhao S., Chen H. Modeling the epidemic dynamics and control of COVID-19 outbreak in China. Quant Biol. 2020;8(1):11–19. doi: 10.1007/s40484-020-0199-0. PubMed PMID: 32219006. Pubmed Central PMCID: PMC7095099. Epub 2020/03/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y., Rocklov J. The effective reproductive number of the Omicron variant of SARS-CoV-2 is several times relative to Delta. J Travel Med. 2022;29(3) doi: 10.1093/jtm/taac037. May 31PubMed PMID: 35262737. Pubmed Central PMCID: PMC8992231. Epub 2022/03/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim D., Ali S.T., Kim S., Jo J., Lim J.S., Lee S., et al. Estimation of serial interval and reproduction number to quantify the transmissibility of SARS-CoV-2 omicron variant in South Korea. Viruses. 2022;14(3) doi: 10.3390/v14030533. Mar 4PubMed PMID: 35336939. Pubmed Central PMCID: PMC8948735. Epub 2022/03/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang L., Berger N.A., Kaelber D.C., Davis P.B., Volkow N.D., Xu R. COVID infection rates, clinical outcomes, and racial/ethnic and gender disparities before and after Omicron emerged in the US. medRxiv. 2022 Feb 22PubMed PMID: 35233579. Pubmed Central PMCID: PMC8887070 to disclose. Epub 2022/03/03. [Google Scholar]
- 7.Chen X., Yan X., Sun K., Zheng N., Sun R., Zhou J., et al. Estimation of disease burden and clinical severity of COVID-19 caused by Omicron BA.2 in Shanghai, February-June 2022. Emerg Microbes Infect. 2022;11(1):2800–2807. doi: 10.1080/22221751.2022.2128435. DecPubMed PMID: 36205530. Pubmed Central PMCID: PMC9683067. Epub 2022/10/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.国家卫生健康委员会. 《中国卫生健康统计年鉴(2022)》: 中国协和医科大学出版社; 2022.
- 9.Collaborators GBDI Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: an analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. 2019;7(1):69–89. doi: 10.1016/S2213-2600(18)30496-X. JanPubMed PMID: 30553848. Pubmed Central PMCID: PMC6302221. Epub 2018/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]