Abstract
Background
Female sex workers (FSWs) are at high risk of mental health problems and suicide risk. Few longitudinal studies have examined risk factors for poor mental health among FSWs.
Methods
Maisha Fiti is a longitudinal study among FSWs randomly selected from Sex Worker Outreach Programme clinics across Nairobi. Behavioural-biological survey data were collected at baseline (n = 1003, June–December 2019), midline (n = 366) (Jan–March 2020) and endline (n = 877) (June 2020–Jan 2021). Women reporting mental health problems were offered counselling services. Multivariable mixed logistic regression models were used to examine factors associated with mental health problems and suicidal behaviours.
Results
There was a decline in the proportion of women reporting any mental health problem (depression and/or anxiety and/or PTSD) (baseline: 29.9%, midline: 13.3%, endline: 11.8%). There was strong evidence that any mental health problem was associated with recent hunger (aOR 1.99; 95% CI 1.37–2.88) and recent violence from non-intimate partners (2.23; 95% CI 1.55–3.19). Recent suicidal behaviour prevalence was similar across survey rounds (baseline: 10.2%; midline: 10.2%; endline: 10.4%), and was associated with recent violence from non-intimate partners (aOR 1.96; 95% CI 1.31–2.95), recent hunger (aOR 1.69; 95% CI 1.15–2.47) and having an additional employment to sex work (aOR 1.50; 95% CI 1.00–2.23).
Conclusions
Our study found a decline in mental health problems but high levels of persistent suicidal behaviours among FSWs. Syndemic risk factors including food insecurity and violence were longitudinally associated with mental health problems and recent suicidal behaviours. There is a need for accessible mental health services for FSWs, alongside structural interventions addressing poverty and violence.
Key words: Female sex workers, mental health
Introduction
Mental health problems are a major contributor to the global burden of disease (Murray et al., 2020). There is a high burden of untreated common mental health problems with a treatment gap greater than 90% in low-income countries (Thornicroft et al., 2017). Women in low and middle-income countries (LMICs) are at greater risk than men according to the 2019 Global Burden of Disease study, with a higher prevalence of depression (4.5%; 95% CI 4.0–5.0 v. men: 3.0%; 95% CI 2.7–3.4) and anxiety disorders (4.3%; 95% CI 3.6–5.2% v. men: 2.8%; 95% CI 2.3–3.3%) (Murray et al., 2020). Risk factors for mental health problems include demographic and socio-economic factors such as age, gender, poverty and educational status, exposure to violence and harmful alcohol and substance use (Patel et al., 2016). Untreated mental health problems result in short- and long-term impacts on quality of life and increase the risk of mortality from suicide (Thornicroft et al., 2017).
Sex work [defined as the receipt of money or goods in exchange for sexual services (UNAIDS, 2002)] is criminalised in most parts of the world (Platt et al., 2018). Female sex workers (FSWs) face intersecting health and social risks, such as poverty, gender inequality, police arrest, harmful alcohol and substance use, violence from clients and intimate partners and a high prevalence of HIV and other sexually transmitted infections (STIs) (Shannon et al., 2015; Platt et al., 2018). These overlapping risk factors which often perpetuate each other are known as syndemic factors (Singer and Clair, 2003; Buttram et al., 2014). A recent systematic review and meta-analysis examining mental health problems among FSWs in LMICs found high levels of mental health problems including depression, anxiety and PTSD, compared to the general population (Beattie et al., 2020). The authors found strong evidence of associations between depression and recent violence experience (OR 2.3; 95% CI 1.3–4.2), alcohol use (OR 2.1; 95% CI 1.4–3.2), inconsistent condom use with clients (OR 1.6; 95% CI 1.2–2.1) and HIV (OR 1.4; 95% CI 1.1–1.8) (Beattie et al., 2020) as well as associations between recent suicide attempt with ever experiencing violence (OR 3.5; 95% CI 2.2–5.5), alcohol use (OR 1.6; 1.0–2.5) and HIV (OR 1.4; 95% CI 1.1–1.8).
Currently, there is an evidence gap both in (1) longitudinal studies examining the burden of mental health problems among FSWs over time, and (2) studies assessing the effect of interventions addressing mental health and associated risk factors such as violence among FSWs. The majority of research among FSWs has focussed on addressing HIV/STI risk through behavioural and biomedical interventions (Platt et al., 2018), although more recently some interventions have targeted key structural drivers such as violence (Beattie et al., 2015). Beattie et al. systematic review on mental health among FSWs reported both a lack of longitudinal and intervention studies among FSWs (Beattie et al., 2020). Longitudinal studies are crucial to understand pathways of causation between potential risk factors and mental health problems to identify targets for upstream interventions. In addition, there are limitations in interpreting the current evidence due to the varied use of measurement tools and cut-off scores (Beattie et al., 2020) to measure mental health problems and associated risk factors.
This paper aims to address this evidence gap by examining temporal trends in mental health problems and longitudinal relationships with risk factors such as violence, poverty and alcohol/substance use using data from the Maisha Fiti Study. Maisha Fiti is a mixed-methods longitudinal study among FSWs in Nairobi, Kenya which aims to examine associations between violence experience, mental health problems, harmful alcohol and substance use as well as biological changes to the immune system such as genital tract inflammation and HIV among FSWs. Previously reported findings from Maisha Fiti indicate a high baseline prevalence of depression, anxiety, PTSD and suicidal behaviours, measured using validated mental health tools, which were associated with syndemic risk factors including recent violence, poverty and harmful alcohol/substance use (Beksinska et al., 2021). Women were offered psychological counselling during the study and we report on the uptake and assess the effects of a brief psychological counselling service for FSWs. Our findings will be used to design and deliver much needed holistic mental health interventions tailored for FSWs.
Methods
Study design and sampling
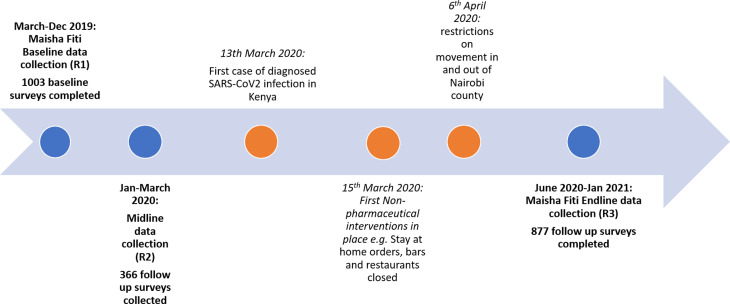
The Maisha Fiti study was designed in consultation with FSWs in Nairobi and with community mobilisers and staff working at seven SWOP clinics. These clinics are delivered with the support of Partners for Health and Development Africa (PHDA) to provide HIV/STI prevention and treatment services to FSWs across Nairobi. Women were randomly selected by the study team from the seven SWOP clinic attendance lists of all clinic attendees in the previous 12 months, and invited to enrol in the study. Sample size calculations and sampling methodology have been described previously (Beksinska et al., 2021). Initially follow-up data collection was planned one year after baseline and began in January 2020. Due to the onset of the COVID-19 epidemic in Kenya, data collection was paused in March 2020, resumed in June 2020 and was completed in January 2021. At the time, it was decided to re-survey all women (n = 877) due to the delay and the likely change in women's mental health experiences as a result of COVID-19. Data collected January–March 2020 (n = 366) were considered as midline data (Fig. 1).
Fig. 1.
Timeline of baseline and follow-up surveys in relation to COVID-19 and prevention measures in Kenya.
Eligibility criteria were women aged 18–45 years, who self-identified as sex workers (exchanged money for sex or accepted goods as payment), had attended one of the SWOP clinics in the past 12 months, were not pregnant or breast-feeding and did not have an underlying chronic illness (other than HIV) that was likely to alter host immunology. Selected women were telephoned, given information about the study and the opportunity to ask any questions and invited to attend the study clinic. Interested women were screened for eligibility and received detailed information about the study verbally and via the participant information leaflet (in English or Swahili). For women with low literacy, this information was read to them by study staff. Consenting participants completed a behavioural-biological survey. Those found to have mental health or alcohol/substance use problems were referred to a trained psychological counsellor based in the study clinic. All women who tested positive for HIV at any of the three study visits were counselled and encouraged to enrol in HIV care. All women who tested positive for STIs were offered appropriate treatment free of charge.
Behavioural-biological survey
Time-invariant measures collected at baseline include age, marital status, number of children, religion, literacy, socio-economic status (SES). Time-variant measures including mental health problems, recent physical and/or sexual violence experience, alcohol/substance use, sexual risk behaviours and recent indicators of financial stress (e.g. missed a meal in the past week due to financial difficulties) were collected at baseline, midline and endline. Validated tools with high reliability and validity [see baseline paper for more details (Beksinska et al., 2021)] were used for assessing depression – Patient Health Questionnaire (PHQ-9) (score ⩾15 = moderate/severe depressive disorder) (Kroenke et al., 2001); anxiety – Generalised Anxiety Disorder (GAD-7) (score ⩾10 = moderate/severe anxiety) (Spitzer et al., 2006) and PTSD – Harvard Trauma Questionnaire (HTQ-17) (Kleijn et al., 2001). Suicide risk was measured by a two-item questionnaire which included recent suicidal ideation (‘having thoughts about ending your life in the last 30 days’) and recent suicide attempt (‘having attempted to end your life in the last 30 days’). Due to the small number of women reporting a recent suicide attempt, and the significant overlap in women reporting a recent suicide attempt and recent suicidal ideation, we combined these measures into a dichotomous variable including women who reported recent suicidal thoughts and/or recent suicide attempt under the term ‘recent suicidal behaviours’. The term ‘suicidal behaviours’ encompasses a continuum of risk from suicidal thoughts to planning to attempts and is a recognised definition in the psychiatric literature (Posner et al., 2007; Nock et al., 2008; O'Connor and Nock, 2014).
The WHO ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) tool was used to measure harmful alcohol use (cut-off scores: moderate risk >11; high risk >27) and other substance use (cut-off scores: moderate risk >4; high risk >27) in the last 3 months including amphetamines, cannabis, cocaine, hallucinogens, sedatives and inhalants [World Health Organisation (WHO), 2010].
The WHO Violence Against Women 13-item questionnaire which measures frequency and severity of intimate partner violence (IPV) was adapted to also include violence perpetrated by non-IPs (e.g. police, strangers, clients, etc.) in the past 6 months (World Health Organisation, 2005).
Women were offered psychological counselling with a trained psychological counsellor if they reported moderate/severe depression, recent suicidal ideation/self-harm, recent violence or moderate/high risk alcohol use. As part of the study, training in an evidence-based brief psychological intervention for depression [Healthy Activity Program (HAP)] (Patel et al., 2017) and alcohol use disorders [Counselling for Alcohol Problems (CAP)] (Nadkarni et al., 2017) was delivered to lay counsellors (HIV testing and screening counsellors) and peer sex workers, working at existing SWOP clinics. Uptake of Maisha Fiti study counselling at baseline was self-reported at midline and endline.
Laboratory methods
Biological samples were collected at baseline, midline and endline. Urine samples were collected to test for pregnancy, Neisseria gonorrhoeae and Chlamydia trachomatis. Blood was collected for Treponema pallidum (syphilis) testing and HIV status. Self-collected vaginal swabs tested for Trichomonas vaginalis and bacterial vaginosis. Laboratory methods have been previously described in detail (Beksinska et al., 2021).
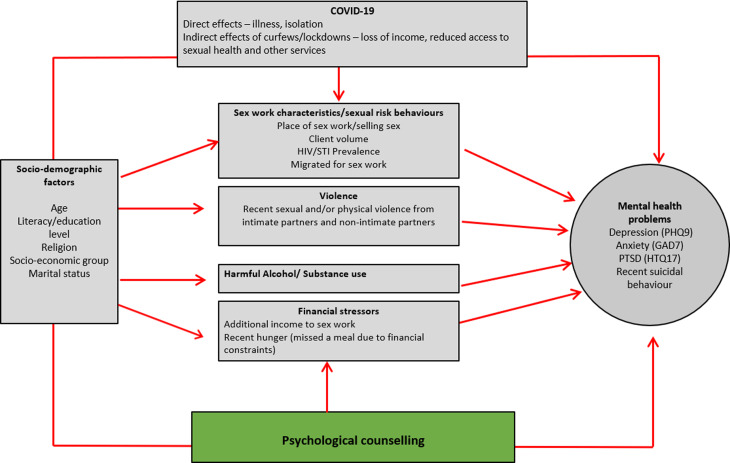
Conceptual framework
We developed a conceptual framework (Fig. 2) to explore correlates of mental health problems and recent suicidal behaviours using an eco-social life course theory approach (Krieger, 2012). This is based on the framework in our baseline analysis (Beksinska et al., 2021) and adapted to consider longitudinal associations, the impact of counselling and the potential effects of COVID-19 on mental health outcomes.
Fig. 2.
Conceptual framework exploring potential correlates of mental health problems and suicidal behaviours over time.
Statistical analyses
Data were double-entered and statistical analyses were conducted in STATA 16.1 (Stata Inc., College Station, TX, USA). As women aged <25 years old were over-sampled, analyses included weighting for age group using inverse probability weights. Key baseline socio-demographic characteristics were compared between those individuals participating at both baseline and endline (n = 877), with those seen at baseline only (n = 126) using Pearson's χ2 tests. Data from baseline, midline and endline surveys were used to describe changes in the prevalence of mental health problems and recent suicidal behaviours over time. Changes in mental health problems between survey rounds were calculated using mixed-effects logistic regression to adjust for repeated measures over time.
The two outcomes of interest were (1) any recent mental health problem (moderate/severe depression and/or moderate/severe anxiety and/or PTSD) and (2) suicidal behaviour (reported suicidal attempts and/or ideation). Analyses for each outcome were conducted using repeated measures mixed-effects logistic regression to allow for individual-level clustering, and adjusting for clinic-level clustering by including SWOP clinic as a fixed effect. Associations were estimated using odds ratios (OR), with p values obtained using the adjusted Wald test due to data being weighted. In this repeated measures model, the ORs are assumed constant for the association of outcomes at midline with exposures at baseline, and for outcomes at endline with exposures at midline. Initial ORs were estimated as crude, and a minimally-adjusted model which included the set of a priori defined potential confounders (age group at enrolment, religion, literacy, SES and marital status). Variables which were either associated with the outcome in the minimally-adjusted model (p < 0.10), or which were a priori defined potential confounders, were included in a multivariable model and were retained in the final model if they were independently associated with the outcome (p < 0.10). Uptake of counselling prior to endline was identified as an a priori effect-modifier to test the hypothesis that counselling could modify the association between baseline risk factors and endline mental health problems. Variables in the final multivariable model were assessed for effect-modification with uptake of counselling.
Results
Study population and sex work characteristics
Of the 1039 eligible FSWs, 1003 (96.5%) women participated in baseline surveys. Of these, 366 (36.5%) participated at midline and 877 (87.4%) at endline. Of the women that participated at midline 94.0% took part at endline. At baseline, the median age of participants was 32 years (range 18–45; IQR 26–39) and most were currently or previously married (81.2%). The majority of women reported their religion to be Protestant (54.4%) or Catholic (36.9%). The mean age at first sex was 16 years (IQR 15–18; s.d. 2.6). Almost half (43.7% at baseline, 45.7% at endline) of women reported additional employment to sex work, and there was an increase in the proportion of women reporting recent hunger due to financial difficulties during follow-up (33.0% at baseline; 54.3% at endline). Most women worked from a lodge/hotel/rented room (91.4% at baseline, 85.2% at endline). The median client volume per week (reported clients in last 7 days) declined from 3 at baseline to 2 at endline. HIV prevalence was 28.0% at baseline, with no new HIV diagnoses among those followed up. There was no change in the proportion of women reporting condom use at last sex (77.1% at baseline; 77.5% at endline). Reported harmful alcohol use declined between survey rounds (29.8% at baseline; 13.4% at endline), as did other harmful substance use (30.7% at baseline; 24.3% at endline), and reported sexual or physical violence from non-IPs (55.0% at baseline; 20.9% at endline) and from intimate partners (30.9% at baseline; 12.1% at endline).
Factors associated with loss-to-follow-up by endline were HIV status (higher follow-up among women living with HIV; p = 0.001) and reported recent violence from non-IPs (higher follow-up among those not reporting violence; p = 0.05) (online Supplementary Appendix A).
Temporal changes in mental health problems
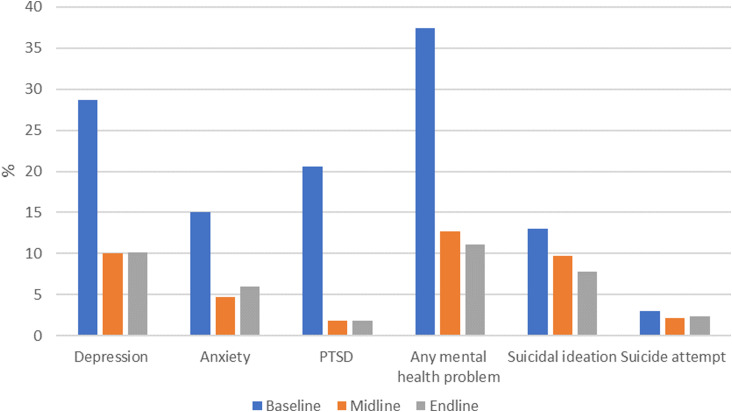
The prevalence of any mental health problem among participants declined over time (Table 1) from 29.9% at baseline to 13.3% at midline and 11.8% at endline (p value for trend <0.0001). The decline was seen for depression, anxiety and PTSD, respectively (Table 1). The prevalence of recent suicidal behaviour did not change over time (10.2% at baseline; 10.2% at midline; 10.4% at endline) (Table 1). Findings were similar among the 366 women who completed baseline, midline and endline surveys (Fig. 3).
Table 1.
Temporal changes in prevalence of mental health problems among FSWs at baseline, midline and endline surveys
| Baseline | Midline | Endline | p valuea | ||||
|---|---|---|---|---|---|---|---|
| (n = 1003) | % (95% CI) | (n = 366) | % (95% CI) | (n = 877) | % (95% CI) | <0.0001 | |
| Any mental health problem (depression/anxiety/PTSD) | 293 | 29.9 (27.2–32.8) | 47 | 13.3 (10.2–17.3) | 97 | 11.8 (9.9–14.2) | <0.0001 |
| Depression | 222 | 23.2 (20.7–25.9) | 40 | 11.6 (8.6–15.4) | 87 | 10.6 (8.7 −12.9) | <0.0001 |
| Anxiety | 109 | 11.0 (9.3–13.1) | 17 | 4.8 (3.0–7.5) | 39 | 4.8 (3.5–6.4) | <0.0001 |
| PTSD | 138 | 14.2 (12.2–16.5) | 7 | 1.8 (0.8–3.8) | 16 | 1.9 (1.1–3.0) | <0.0001 |
| Suicidal ideation (last 6 months) | 99 | 10.0 (8.3–12.0) | 36 | 10.2 (7.5–13.9) | 90 | 10.4 (8.5–12.6) | 0.9 |
| Suicide attempt (last 6 months) | 27 | 2.6 (1.8–3.8) | 7 | 1.9 (0.9–4.0) | 21 | 2.4 (1.5–3.6) | 0.7 |
| Suicidal behaviour (recent suicidal ideation and/or attempt) | 101 | 10.2 (8.5–12.2) | 36 | 10.2 (7.5–13.9) | 91 | 10.4 (8.4–12.6) | 0.9 |
Mixed-effects logistic regression.
Fig. 3.
Temporal changes in prevalence of mental health problems among FSWs in Nairobi who completed baseline, midline and endline surveys (n = 366).
We examined persistent and incident mental health problems among the 877 women who participated at baseline and endline (Table 2). Among 253 women who reported any mental health problems at baseline, 69 (27.3%) had a persistent mental health problem, and among 624 women without any mental health problems at baseline, 28 (4.5%) reported an incident mental health problem (Table 2). Approximately one-third of women with each condition at baseline had persistence of that condition at endline (depression: 31.7%, anxiety 29.8%, PTSD 29.8%). Co-morbid persistence of mental health problems was common. Among women with persistent depression nearly half (40.2%) reported persistent anxiety compared to women without persistent depression (4.1%) and 13.3% reported persistent PTSD (v. 0.8% amongst those without depression). The incidence of new mental health problems was low for each condition with 3.9% of women reporting incident depression, 1.4% anxiety and 0.5% PTSD.
Table 2.
Persistent and incident mental health problems/suicidal behaviours between baseline and endline surveys (n = 877)
| Persistenta n (%) | Incidentb n (%) | |
|---|---|---|
| Any MH problem (depression/anxiety/PTSD) | 69/253 (27.3%) | 28/624 (4.5%) |
| Depression | 60/189 (31.7%) | 27/685 (3.9%) |
| Anxiety | 28/94 (29.8%) | 11/783 (1.4%) |
| PTSD | 12/118 (10.2%) | 4/751 (0.5%) |
| Suicidal ideation | 57/85 (67.1%) | 33/792 (4.2%) |
| Suicide attempt | 14/21 (60%) | 7/856 (0.8%) |
| Suicidal behaviour | 57/86 (66.3%) | 34/791 (4.3%) |
Persistent, mental health problem at baseline and endline.
Incident, new mental health problem at endline.
Of the women with suicidal behaviour reported at baseline, two-thirds (66.3%) reported these at endline. Among women with a persistent mental health problem, one-third (33.6%) had persistent suicidal behaviours (v. 4.0% among women without persistent mental health problems).
Temporal associations between baseline exposures and mid/endline mental health and suicidal behaviour outcomes
To explore time-dependent associations, we assessed outcomes at midline and endline with exposures at baseline and midline respectively, adjusting for within-person correlation. The variables independently associated with any mental health problem or suicidal behaviours after adjusting for a priori confounders (Tables 3 and 4) were retained in the final multivariable model. In the final adjusted models, variables associated with increased odds of mental health problems include older age (age 25–34: aOR 2.68; 95% CI 1.40–5.12; age >35: aOR 2.29; 95% CI 1.19–4.42; p = 0.01), Muslim v. Catholic religion (aOR 2.74; 95% CI 1.43–5.24; p < 0.001), ever being married (aOR 2.07; 95% CI 1.20–3.56; p = 0.009), recent hunger (aOR 1.99; 95% CI 1.37–2.88; p < 0.001) and recent violence from non-IPs (2.23; 95% CI 1.55–3.19; p < 0.0001) (Table 5). There was some evidence that women with a higher client volume (>10 clients per week v. <5 clients) had lower odds of mental health problems (aOR 0.45; 95% CI 0.20–1.00; p 0.07). HIV/STIs were not associated with any mental health problems in univariate and adjusted analysis. Overall, 42.9% (n = 372) of women reported attending any Maisha Fiti counselling at mid/endline. There was no evidence that attending counselling modified the effect of any associations with mental health problems (Table 5).
Table 3.
Longitudinal associations between any mental health problems (moderate/severe depression and/or anxiety and /or PTSD) and key exposures including socio-demographic variables at baseline, financial stressors, sex work characteristics, recent violence experience and alcohol/substance
| % with mental health problems at baseline (n = 293/1003) | % with mental health problems at midline (n = 47/366) | % with mental health problems at endline (n = 97/877) | Crude OR (95% CI) | p value | Minimally adjusted ORa | p value | ||
|---|---|---|---|---|---|---|---|---|
| Age (years) | <25 | 9.2 | 4.4 | 4.3 | 1.0 | 1.0 | ||
| 25–34 | 37.0 | 35.6 | 46.3 | 3.05 (1.62–5.74) | 2.68 (1.40–5.12) | |||
| 35+ | 53.8 | 60.0 | 49.5 | 2.73 (1.47–5.08) | 0.002 | 2.29 (1.19–4.42) | 0.01 | |
| Literacy | Illiterate | 19.6 | 17.8 | 25.3 | 1.0 | 1.0 | ||
| Literate | 80.4 | 82.2 | 74.7 | 0.68 (0.45–1.03) | 0.07 | 0.85 (0.55–1.31) | 0.5 | |
| Religion | Catholic | 35.3 | 44.4 | 34.4 | 1.0 | 1.0 | ||
| Protestant | 54.2 | 43.4 | 46.3 | 0.81 (0.56–1.17) | 0.79 (0.54–1.15) | |||
| Muslim | 5.6 | 10.0 | 12.4 | 2.83 (1.54–5.20) | 2.74 (1.43–5.24) | |||
| Other/none | 4.9 | 2.2 | 7.0 | 1.69 (0.77–3.72) | <0.001 | 1.83 (0.83–4.00) | <0.001 | |
| Socio-economic status (SES) | Low/low-middle | 42.2 | 52.2 | 42.5 | 1.0 | 1.0 | ||
| Middle | 21.8 | 22.2 | 20.4 | 0.88 (0.56–1.37) | 0.87 (0.55–1.38) | |||
| Upper middle/upper | 36.0 | 25.6 | 37.1 | 0.68 (0.47–0.99) | 0.1 | 0.67 (0.44–1.04) | 0.2 | |
| Ever married | No | 15.8 | 6.7 | 11.3 | 1.0 | 1.0 | ||
| Yes | 84.2 | 93.3 | 88.7 | 2.33 (1.36–4.00) | 0.002 | 2.07 (1.20–3.56) | 0.009 | |
| Additional employment to sex work | No | 48.9 | 55.6 | 43.5 | 1.0 | 1.0 | ||
| Yes | 51.1 | 44.4 | 56.5 | 0.86 (0.61–1.20) | 0.4 | 0.84 (0.59–1.21) | 0.4 | |
| Recent hunger (missed a meal in the last 7 days due to financial constraints) | No | 52.6 | 50.0 | 26.9 | 1.0 | 1.0 | ||
| Yes | 47.4 | 50.0 | 73.1 | 2.41 (1.72–3.38) | <0.0001 | 2.19 (1.52–3.16) | <0.0001 | |
| Place of sex work | Lodge/hotel/rented room | 89.3 | 91.1 | 88.3 | 1.0 | 1.0 | ||
| Other public place | 3.4 | 4.5 | 2.13 | 1.86 (0.78–4.43) | 1.63 (0.67–3.96) | |||
| Home | 7.3 | 4.4 | 9.6 | 1.42 (0.72–2.78) | 0.2 | 1.39 (0.67–2.88) | 0.4 | |
| Client volume/week | <5 | 63.2 | 84.1 | 82.5 | 1.0 | 1.0 | ||
| 5–9 | 21.1 | 11.4 | 13.4 | 0.78 (0.52–1.18) | 0.77 (0.51–1.18) | |||
| 10+ | 15.7 | 4.6 | 4.2 | 0.50 (0.27–0.94) | 0.07 | 0.48 (0.25–0.92) | 0.06 | |
| Condom use last sex | No | 26.7 | 37.8 | 25.3 | 1.0 | 1.0 | ||
| Yes | 73.3 | 62.2 | 74.7 | 0.77 (0.53–1.13) | 0.2 | 0.83 (0.56–1.23) | 0.3 | |
| Any STI at baseline | No | 87.0 | 95.6 | 86.8 | 1.0 | 1.0 | ||
| Yes | 13.0 | 4.5 | 13.2 | 1.22 (0.72–2.05) | 0.5 | 1.16 (0.68–1.99) | 0.6 | |
| HIV status | Negative | 73.1 | 60.0 | 71.0 | 1.0 | 1.0 | ||
| Positive | 26.9 | 40.0 | 29.0 | 1.16 (0.81–1.66) | 0.8 | 1.06 (0.72–1.57) | 0.8 | |
| Migrated for sex work (sex work outside Nairobi last 6 months) | No | 72.7 | 65.4 | 59.7 | 1.0 | 1.0 | ||
| Yes | 27.4 | 34.6 | 40.3 | 1.09 (0.74–1.61) | 0.7 | 1.03 (0.69–1.54) | 0.9 | |
| Any recent sexual and/or physical non-IP violence | No | 32.8 | 54.5 | 59.2 | 1.0 | 1.0 | ||
| Yes | 67.2 | 45.5 | 40.8 | 2.26 (1.59–3.21) | <0.0001 | 2.23 (1.56–3.18) | <0.0001 | |
| Any recent sexual and/or physical IP violence | No | 60.6 | 67.8 | 80.1 | 1.0 | 1.0 | ||
| Yes | 39.4 | 32.2 | 19.9 | 1.29 (0.90–1.85) | 0.2 | 1.21 (0.83–1.78) | 0.3 | |
| Recent arrest | No | 63.1 | 75.6 | 81.7 | 1.0 | 1.0 | ||
| Yes | 36.9 | 24.4 | 18.3 | 1.18 (0.82–1.69) | 0.4 | 1.08 (0.74–1.58) | 0.7 | |
| Alcohol use problem (ASSIST moderate/high) | No | 49.7 | 54.6 | 65.9 | 1.0 | 1.0 | ||
| Yes | 50.3 | 45.5 | 34.1 | 1.15 (0.80–1.67) | 0.4 | 1.12 (0.76–1.65) | 0.6 | |
| Substance use problem (ASSIST moderate/high) | No | 56.6 | 73.4 | 62.4 | 1.0 | 1.0 | ||
| yes | 43.5 | 26.7 | 37.6 | 1.26 (0.89–1.79) | 0.2 | 1.16 (0.79–1.70) | 0.5 |
Adjusted for a priori defined potential confounders (age at baseline, literacy, religion, SES, ever married) and SWOP clinic.
Table 4.
Longitudinal associations between reported suicidal behaviour (recent suicide attempt and/or ideation) and key exposures including socio-demographic variables at baseline, financial stressors, sex work characteristics, recent violence experience and alcohol/substance
| % suicidal behaviour at baseline (n = 101/1003) | % suicidal behaviour at midline (n = 36/366) | % suicidal behaviour at endline (n = 91/877) | Crude OR (95% CI) | p valuea | Minimally adjusted OR | p valuea | ||
|---|---|---|---|---|---|---|---|---|
| Age (years) | <25 | 10.3 | 4.3 | 10.9 | 1.0 | 1.0 | ||
| 25–34 | 41.6 | 46.4 | 44.0 | 1.45 (0.86–2.44) | 1.26 (0.74–2.16) | |||
| 35+ | 48.1 | 49.3 | 45.2 | 1.07 (0.63–1.79) | 0.2 | 0.89 (0.51–1.55) | 0.2 | |
| Literacy | Illiterate | 27.4 | 20.3 | 26.9 | 1.0 | 1.0 | ||
| Literate | 72.7 | 79.7 | 73.1 | 0.60 (0.39–0.92) | 0.02 | 0.62 (0.39–0.99) | 0.04 | |
| Religion | Catholic | 36.1 | 31.9 | 34.7 | 1.0 | 1.0 | ||
| Protestant | 48.6 | 59.4 | 54.9 | 1.17 (0.79–1.71) | 1.25 (0.84–1.85) | |||
| Muslim | 8.7 | 2.9 | 6.7 | 1.27 (0.56–1.71) | 1.32 (0.56–3.09) | |||
| Other/none | 6.6 | 5.8 | 3.7 | 1.42 (0.57–3.50) | 0.8 | 1.45 (0.56–3.78) | 0.7 | |
| Socio-economic status (SES) | Low/low-middle | 56.4 | 56.5 | 44.5 | 1.0 | 1.0 | ||
| Middle | 19.9 | 34.8 | 29.9 | 1.32 (0.87–2.01) | 1.52 (0.98–2.35) | |||
| Upper middle/upper | 23.8 | 8.7 | 25.6 | 0.39 (0.24–0.62) | <0.0001 | 0.41 (0.25–0.68) | <0.0001 | |
| Ever married | No | 16.4 | 5.8 | 11.6 | 1.0 | 1.0 | ||
| Yes | 83.6 | 94.2 | 88.4 | 2.28 (1.29–4.02) | 0.005 | 2.31 (1.29–4.13) | 0.005 | |
| Additional employment to sex work | No | 48.1 | 52.2 | 50.0 | 1.0 | |||
| Yes | 51.9 | 47.8 | 50.0 | 1.27 (0.88–1.82) | 0.2 | 1.42 (0.98–2.07) | 0.06 | |
| Recent hunger (missed a meal in the last 7 days due to financial constraints) | No | 43.4 | 33.3 | 21.4 | 1.0 | |||
| Yes | 56.6 | 66.7 | 78.7 | 2.36 (1.65–3.38) | <0.0001 | 1.86 (1.29–2.68) | <0.001 | |
| Place of sex work | Lodge/hotel/rented room | 86.2 | 94.2 | 89.0 | 1.0 | 1.0 | ||
| Other public place | 6.1 | 0.0 | 4.3 | 1.54 (0.60–3.98) | 1.40 (0.51–3.84) | |||
| Home | 7.7 | 5.8 | 6.7 | 1.07 (0.50–2.29) | 0.7 | 1.08 (0.50–2.32) | 0.8 | |
| Client volume/week | <5 | 59.2 | 66.7 | 60.4 | 1.0 | 1.0 | ||
| 5–9 | 27.9 | 18.8 | 25.6 | 1.23 (0.82–1.85) | 1.19 (0.78–1.81) | |||
| 10+ | 12.9 | 14.5 | 14.0 | 0.86 (0.47–1.54) | 0.5 | 0.88 (0.47–1.64) | 0.6 | |
| Condom use last sex | No | 22.2 | 26.1 | 32.9 | ||||
| Yes | 77.8 | 73.9 | 67.1 | 0.73 (0.49–1.09) | 0.1 | 0.78 (0.52–1.22) | 0.3 | |
| Any STI at baseline | No | 86.9 | 97.1 | 88.7 | 1.0 | |||
| Yes | 13.1 | 2.9 | 11.3 | 1.11 (0.63–1.96) | 0.7 | 0.99 (0.55–1.80) | 1.0 | |
| HIV status | Negative | 72.1 | 52.2 | 70.7 | 1.0 | |||
| Positive | 27.9 | 47.8 | 29.3 | 1.29 (0.88–1.89) | 0.2 | 1.20 (0.79–1.81) | 0.4 | |
| Migrated for sex work Sex work outside Nairobi last 6 months | No | 70.7 | 65.3 | 58.7 | 1.0 | |||
| Yes | 29.3 | 34.7 | 41.3 | 1.03 (0.68–1.55) | 0.9 | 1.08 (0.70–1.67) | 0.7 | |
| Any recent sexual and/or physical non-IP violence | No | 23.5 | 31.9 | 53.7 | 1.0 | |||
| Yes | 76.5 | 68.1 | 46.3 | 2.28 (1.57–3.32) | <0.0001 | 2.03 (1.37–3.00) | <0.0001 | |
| Any recent sexual and/or physical IP violence | No | 55.8 | 66.7 | 86.6 | 1.0 | |||
| Yes | 44.3 | 33.3 | 13.4 | 2.28 (1.57–3.32) | <0.0001 | 1.37 (0.92–2.04) | 0.1 | |
| Recent arrest | No | 52.4 | 63.8 | 76.8 | 1.0 | |||
| Yes | 47.6 | 36.2 | 23.2 | 1.64 (1.13–2.38) | 0.009 | 1.49 (1.01–2.20) | 0.05 | |
| Alcohol use problem (ASSIST moderate/high) | No | 48.4 | 69.7 | 78.2 | 1.0 | |||
| Yes | 51.6 | 30.3 | 21.8 | 1.28 (0.85–1.94) | 0.3 | 1.28 (0.85–1.94) | 0.2 | |
| Substance use problem (ASSIST moderate/high) | No | 49.7 | 65.2 | 71.4 | 1.0 | |||
| Yes | 50.3 | 34.8 | 28.6 | 1.12 (0.74–1.70) | 0.2 | 1.16 (0.79–1.69) | 0.5 |
Adjusted Wald test.
Table 5.
Multivariable analysis to examine longitudinal associations with mental health outcomes and effect-modification with uptake of counselling
| Final adjusted OR (95% CI) | p valuea | Did not attend counselling | Attended counselling | p valuea | ||
|---|---|---|---|---|---|---|
| Baseline demographicsb | ||||||
| Age (years) at baselineb | <25 | 1.0 | 1.0 | 1.0 | ||
| 25–34 | 2.68 (1.40–5.12) | 2.13 (0.72–6.24) | 3.49 (1.19–10.2) | |||
| 35+ | 2.29 (1.19–4.42) | 0.01 | 1.46 (0.51–4.21 | 3.84 (1.33–11.06 | 0.2 | |
| Religion | Catholic | 1.0 | 1.0 | 1.0 | ||
| Protestant | 0.79 (0.54–1.15) | 0.81 (0.47–1.40) | 0.69 (0.40–1.19 | |||
| Muslim | 2.74 (1.43–5.24) | 3.22 (1.13–9.17) | 1.55 (0.54–4.41) | |||
| Other/none | 1.83 (0.83–4.00) | <0.001 | 1.35 (0.48–3.84 | 2.70 (0.95–7.68) | 0.5 | |
| Ever married | Yes | 2.07 (1.20–3.56) | 0.009 | 2.01 (0.84–4.79) | 2.65 (1.11–6.31) | 0.6 |
| Financial stressors, sex work characteristics, sexual risk behaviours, violence and alcohol/substance use (time variant exposures)c | ||||||
| Recent hunger – missed a meal in the last 7 days | Yes | 1.99 (1.37–2.88) | <0.001 | 1.77 (1.03–3.03) | 2.23 (1.40–3.82) | 0.5 |
| Clients per week | <5 | 1.0 | 1.0 | 1.0 | ||
| 5–9 | 0.68 (0.40–1.16) | 0.63 (0.28–1.44) | 0.76 (0.34–1.73) | |||
| 10+ | 0.45 (0.20–1.00) | 0.07 | 0.23 (0.09–0.8) | 0.78 (0.27–2.25) | 0.4 | |
| Any recent sexual and/or physical non-IP violence | Yes | 2.23 (1.55–3.19) | <0.0001 | 2.27 (1.36–3.80) | 2.26 (1.35–3.79) | 1.0 |
Adjusted Wald test.
Adjusted for all a priori potential confounders (age at baseline, religion, SES, literacy, ever married) and SWOP clinic.
Adjusted for all a priori potential confounders (age at baseline, religion, SES, literacy, ever married), clinic, violence from non-IPs, hunger and clients per week.
In adjusted analysis women with higher literacy (aOR 0.62; 95% CI 0.39–0.99) and higher SES (middle upper/upper v. lower middle/low aOR 0.41; 95% CI 0.25–0.68) had reduced odds of suicidal behaviour (Table 6). There was an increased odds of suicidal behaviour among women who had ever been married (aOR 2.31; 95% CI 1.29–4.13), reported an additional employment to sex work (aOR 1.50; 95% CI 1.00–2.23), experienced recent hunger (aOR 1.69; 95% CI 1.15–2.47) and among those who reported recent violence from non-IPs (aOR 1.96; 95% CI 1.31–2.95).
Table 6.
Multivariable analysis to examine longitudinal associations between exposures and suicidal behaviours (suicidal ideation and/or attempt) and effect-modification with uptake of counselling
| Adjusted OR (95% CI) | p valuea | Did not attend counselling | Attended counselling | p valuea | ||
|---|---|---|---|---|---|---|
| Baseline demographicsb | ||||||
| Literacy | Illiterate | 1.0 | 1.0 | 1.0 | ||
| Literate | 0.62 (0.39–0.99) | 0.04 | 1.14 (0.61–2.13) | 0.35 (0.18–0.65) | 0.01 | |
| Socio-economic status (SES) | Low/low-middle | 1.0 | 1.0 | 1.0 | ||
| Middle | 1.52 (0.98–2.35) | 2.43 (1.25–4.71) | 0.88 (0.45–1.70) | |||
| Upper middle/upper | 0.41 (0.25–0.68) | <0.0001 | 0.54 (0.26–1.07) | 0.33 (0.16–0.66) | 0.07 | |
| Ever married | No | 1.0 | 1.0 | 1.0 | ||
| Yes | 2.31 (1.29–4.13) | 0.005 | 2.05 (0.76–5.53) | 2.94 (1.09–7.95) | 0.6 | |
| Financial stressors, sex work characteristics, sexual risk behaviours, violence and alcohol/substance use (time variant exposures)c | ||||||
| Additional employment to sex work | No | 1.0 | 1.0 | 1.0 | ||
| Yes | 1.50 (1.00–2.23) | 0.05 | 1.81 (1.00–3.26) | 2.26 (0.70–2.28) | 0.4 | |
| Hunger – missed a meal in the last 7 days due to financial constraints | No | 1.0 | 1.0 | 1.0 | ||
| Yes | 1.69 (1.15–2.47) | 0.007 | 1.16 (0.65–2.06) | 2.44 (1.37–4.35) | 0.06 | |
| Any recent sexual and/or physical non-IP violence | No | 1.0 | 1.0 | 1.0 | ||
| Yes | 1.96 (1.31–2.95) | 0.001 | 1.44 (0.79–2.66) | 2.84 (1.54–5.23) | 0.1 | |
| Any recent sexual and/or physical IP violence | No | 1.0 | 1.0 | 1.0 | ||
| Yes | 1.25 (0.82–1.91) | 0.3 | 1.29 (0.67–2.50) | 1.20 (0.62–2.33) | 0.3 | |
| Recent arrest | No | 1.0 | 1.0 | 1.0 | ||
| Yes | 1.24 (0.81–1.88) | 0.3 | 1.15 (0.61–2.17) | 1.32 (0.69–2.50) | 0.7 | |
Adjusted Wald test
Adjusted for all a priori potential confounders (age at baseline, religion, SES, literacy, ever married) and clinic
Adjusted for all a priori potential confounders (age at baseline, religion, SES, literacy, ever married), clinic, violence from non-IPs, violence from IPs, hunger, additional employment to sex work and clients per week
When we examined for interaction with counselling, there was evidence that the association between higher literacy levels and reduced risk of suicidal behaviour was stronger amongst women who attended counselling (aOR 0.35; 95% CI 0.18–0.65; p 0.01) compared to women who did not attend counselling (aOR 1.14; 95% CI 0.61–2.13) (Table 6). There was some evidence that the association for the protective effect of higher SES on suicidal behaviour was stronger amongst women who attended counselling (aOR 0.33; 95% CI 0.16–0.66; p 0.07 v. those who did not attend counselling: aOR 0.54; 95% CI 0.26–1.07). Among women who attended counselling there was some evidence for a stronger association between recent hunger and suicidal behaviour (aOR 2.44; 95% CI 1.37–4.35; p 0.06) compared to those who did not attend counselling (aOR 1.16; 95% CI 0.65–2.06).
Discussion
Overall there was a decline in mental health problems but persistently high levels of suicidal behaviours during the study. To our knowledge this is the first study among FSWs to examine longitudinal associations between common risk factors and mental health problems and suicidal behaviours. We found that being married, recent violence from non-IPs and food insecurity were strongly associated with mental health problems and suicidal behaviours. Older women, women of Muslim religion and women with lower client volumes were more likely to have mental health problems. Indicators of poverty and financial insecurity including low SES, low literacy levels and additional employment to sex work were associated with increased risk of suicidal behaviours. Almost half of women in our study took up counselling sessions indicating a high demand for counselling services. Attending counselling modified the risk association between literacy, SES, hunger and suicidal behaviour.
There was a decline in the prevalence of all mental health problems during the study, with approximately one in three women reporting a mental health problem at baseline and just one in ten at endline. The greatest decline was seen between baseline and midline. Results from a recent systematic review examining mental health problems among FSWs in LMICs found that the pooled prevalence for depression was 41.8% (95% CI 35.8–48.0%), anxiety 21.0% (95% CI 4.8–58.4%), PTSD 19.7% (95% CI 3.2–64.6%), recent suicidal ideation 22.8% (95% CI 13.2–36.5%) and recent suicide attempt 6.3% (95% CI 3.4–11.4%) (Beattie et al., 2020). At baseline, these estimates are similar to the prevalences found in our study but at endline the prevalence of mental health problems among women in our study is closer to that of the general population in Kenya (World Health Organisation, 2017). In contrast, reported suicidal behaviours remained static throughout the study. There was a high proportion of persistent suicidal behaviours and mental health problems throughout the study. Longer duration of untreated mental health symptoms is associated with worse mental health outcomes (Amati et al., 2018) and a history of previous suicidal thoughts/behaviours significantly increases the lifetime risk of further suicide attempts and completed suicide (McHugh et al., 2019; World Health Organisation, 2014). There is a need for early interventions to address mental health problems and suicide risk among FSWs.
Reasons for a decline in mental health problems are likely to be multi-faceted including increased access to counselling as well as access to services addressing syndemic risks such as alcohol/substance use counselling and violence reduction programmes. In addition to counselling, the process of participating in the study may have had some therapeutic effect. In qualitative interviews women reported the benefits of having a safe space to talk about their experiences during study visits. Evidence-based brief psychological interventions such as the HAP have been shown to be beneficial at treating moderate to severe depressive symptoms as well as having an impact on secondary outcomes including a reduction in reported IPV (Patel et al., 2017) among primary care populations in India. Unfortunately, formal assessment of the effect of the counselling service on mental health problems in our study was limited due to women not being randomised to counselling and most only able to attend <3 in person sessions. However, the high uptake and successful delivery of a brief counselling intervention, based on the HAP, emphasises the need for these services to be embedded within existing sex worker services. The HAP has not previously been used in sub-Saharan Africa or with sex worker populations – future research should consider formally evaluating interventions such as the HAP among FSWs.
The COVID-19 epidemic in Kenya and globally forced many women out of sex work and into alternative employment or unemployment. Between midline (May 2020) and endline (June 2020–Jan 2021) surveys, a variety of measures to curb SARS-CoV-2 transmission including curfews, closure of sex work hot spots, restriction of movement and social distancing had major impacts on the sex work industry (Kimani et al., 2020). If sex work and its associated risk factors were driving poor mental health then this may have had positive effects on women's mental health. For example, the prevalence of violence from clients and harmful alcohol/substance use declined from baseline to endline, which may be due to women being less exposed to these risks. However, due to sex work being criminalised and stigmatised in Kenya, women reported difficulty accessing government financial support schemes during COVID-19 (Kimani et al., 2020). Globally sex worker organisations have reported exclusion from emergency financial protection schemes (Iversen et al., 2020). This was reflected in high levels of food insecurity (recent hunger) reported by women in our study which increased from a third to over 50% at endline, with a strong association between recent hunger and mental health problems and suicidal behaviours. In addition, low SES, requiring an additional employment to sex work and lower client volumes were associated with either mental health problems or increased suicide risk, emphasising the effects of economic insecurity on mental health. Among women who attended counselling there was an increased strength of association between hunger and suicidal behaviour compared to those who did not attend counselling indicating that women may have sought counselling due to the stresses of food insecurity. A recent commentary (Kimani et al., 2020) on the effects of COVID-19 on sex work in Nairobi found that one of the major causes of stress for FSWs was due to food insecurity. However, they also reported that pre-existing HIV programmes and sex worker organisations in Nairobi took steps to rapidly identify and respond to their community's needs, for example, SWOP clinics re-organised their counselling services to operate by phone and sex work leaders organised the distribution of food vouchers (Kimani et al., 2020). This highlights the resilience and adaptability of sex worker groups and local HIV programmes. In order to avoid inequalities being further exacerbated, governments and organisations working with FSWs need to ensure that women have access to financial support during public health emergencies such as COVID-19.
To our knowledge, this is the first study among FSWs in LMICs to find a longitudinal association between recent violence from non-IPs and subsequent mental health problems and suicidal behaviours. Previous cross-sectional data including from a recent systematic review among FSWs reported a pooled unadjusted OR between recent violence and depression of 2.3 (95% CI 1.3–4.2) (Beattie et al., 2020), and two studies among FSWs in South Africa (Coetzee et al., 2018) and Kenya (Roberts et al., 2018) have linked recent violence and PTSD. Overall violence from any perpetrator declined but the strong temporal association between violence and mental health problems/suicidal behaviours indicates that violence remains a major risk factor for FSWs mental health and overall health and wellbeing. There is now evidence that violence interventions can be effective in reducing violence against women in LMICs (Abramsky et al., 2014; Kapiga et al., 2019) as well as among FSWs (Beattie et al., 2015). Future mental health and violence interventions for FSWs should consider how these issues can be addressed in parallel, for example, ensuring women reporting violence are referred for mental health support.
There was no association found between HIV status or STIs and mental health or suicidal behaviour outcomes in our study. This contrasts to findings from Beattie et al.'s systematic review which found an association between depression and HIV (OR 1.4; 95% CI 1.1–1.8; n = 4 studies) and suicidal ideation and HIV (OR 1.4; 95% CI 1.1–1.8; n = 2 studies), however these represent a small number of cross-sectional studies which may not be generalisable to all settings (Beattie et al., 2020). Possible explanations are that FSWs living with HIV benefit from access to regular support delivered through HIV/STI services at SWOP clinics including peer support and violence prevention programmes (Bhattacharjee et al., 2019), which may have positive impacts on their mental health. In addition, most HIV-positive women in our study have known their status for a number of years, so the initial shock of diagnosis may have diminished and there have been efforts in recent years to destigmatise HIV by peer educators discussing their own HIV status.
Strengths and limitations
A major strength of our study is the use of validated tools to assess mental health and violence as well as the use of longitudinal data to assess the directionality of association between exposures and mental health problems. Approximately half of the estimated FSW population in Nairobi are in active follow-up at one of the seven SWOP clinics, from where we drew our sample. Due to the stigmatised nature of sex work it is possible that the most vulnerable women may have been under-represented because they were not registered at a SWOP clinic. There is potential for under-reporting of sensitive topics including mental health, alcohol/substance use and violence.
Conclusion
The mixed findings, of a decline in mental health problems but persistently high suicidal behaviours during the study, may reflect benefits of taking part in the study such as access to counselling services as well as the more complex effects of COVID-19 on sex work, with increased financial insecurity, but reduced risk factors associated with the sex work environment (i.e. violence, alcohol use). There was high uptake and acceptability of a brief counselling service among FSWs in our study. Future research should focus on evaluating the effectiveness of psychological interventions, tailored for FSWs. This is the first longitudinal study among FSWs to find that recent violence and financial insecurity are major longitudinal risk factors for poor mental health. There is an urgent need for interventions addressing up-stream drivers of poor mental health for FSWs, such as financial support and violence prevention programmes.
Acknowledgements
The authors would like to acknowledge the Maisha Fiti Study Champions, for their support in mobilising the FSW community, answering questions participants had about the study, and for supporting participants in accessing the study clinic during the follow-up survey rounds. The Maisha Fiti Study Champions were Celine Njeri, Evelyn Orobi, Ibrahim Lwingi, Demtilla Gwala, Daisy Oside, Ruth Kamene, Agnes Watata, Agnes Atieno and Faith Njau. The authors thank the women in Nairobi who participated in this study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/gmh.2022.44.
click here to view supplementary material
Financial support
Funding for this study was provided by the Medical Research Council and the UK Department of International Development (DFID) (MR/R023182/1) under the MRC/DFID Concordat agreement. No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
None.
Ethical standards
The Maisha Fiti study was approved by the Kenyatta National Hospital Ethics and Research Committee (KNH ERC P778/11/2018), the London School of Hygiene and Tropical Medicine (LSHTM) Ethics Committee (Approval number: 16229) and the University of Toronto ethics committee (Approval number: 37046). All methods were carried out in accordance with relevant local, national and international guidelines and regulations.
Informed consent statement
All participants gave informed consented to participate in the study. To ensure women agreed to participate in this study of their own free volition, a strict informed consent protocol was adhered to. Potential participants were given written and verbal information about the study in a language in which they were fluent. Participants who were literate gave written informed consent; for women who were illiterate, this consent process was witnessed by a person of their choice who was not part of the study team (i.e. legally authorised representatives of illiterate women provided written informed consent). If participants who needed a witness attended the study clinic alone, the witness could be one of two peer educators at the study clinic.
References
- Abramsky T, Devries K, Kiss L, Nakuti J, Kyegombe N, Starmann E, Cundill B, Francisco L, Kaye D, Musuya T, Michau L and Watts C (2014) Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Medicine 12, 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amati F, Banks C, Greenfield G and Green J (2018) Predictors of outcomes for patients with common mental health disorders receiving psychological therapies in community settings: a systematic review. Journal of Public Health 40, e375–e387. [DOI] [PubMed] [Google Scholar]
- Beattie TS, Bhattacharjee P, Isac S, Mohan HL, Simic-Lawson M, Ramesh BM, Blanchard JF, Moses S, Watts CH and Heise L (2015) Declines in violence and police arrest among female sex workers in Karnataka state, south India, following a comprehensive HIV prevention programme. Journal of the International Aids Society 18, 20079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie TS, Smilenova B, Krishnaratne S and Mazzuca A (2020) Mental health problems among female sex workers in low- and middle-income countries: a systematic review and meta-analysis. PLoS Medicine 17, e1003297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beksinska A, Jama Z, Kabuti R, Kungu M, Babu H, Nyariki E, Shah P, Gwala D, Oside D, Kamene R, Watata A, Atieno A, Njau F, Njeri E, Orobi E, Lwingi I, Nyabuto C, Okumu M, Mahero A, Ngurukiri P, Irungu E, Adhiambo W, Muthoga P, Kaul R, Seeley J, Beattie TS, Weiss HA, Kimani J and Maisha Fiti Study C (2021) Prevalence and correlates of common mental health problems and recent suicidal thoughts and behaviours among female sex workers in Nairobi, Kenya. BMC Psychiatry 21, 503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharjee P, Musyoki HK, Becker M, Musimbi J, Kaosa S, Kioko J, Mishra S, Isac SK, Moses S and Blanchard JF (2019) HIV prevention programme cascades: insights from HIV programme monitoring for female sex workers in Kenya. Journal of the International AIDS Society 22(Suppl Suppl 4), e25311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttram ME, Surratt HL and Kurtz SP (2014) Resilience and syndemic risk factors among African-American female sex workers. Psychology, Health & Medicine 19, 442–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coetzee J, Buckley J, Otwombe K, Milovanovic M, Gray GE and Jewkes R (2018) Depression and post traumatic stress amongst female sex workers in Soweto, South Africa: a cross sectional, respondent driven sample. PLoS ONE 13, e0196759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen J, Sabin K, Chang J, Morgan Thomas R, Prestage G, Strathdee SA and Maher L (2020) COVID-19, HIV and key populations: cross-cutting issues and the need for population-specific responses. Journal of the International AIDS Society 23, e25632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapiga S, Harvey S, Mshana G, Hansen CH, Mtolela GJ, Madaha F, Hashim R, Kapinga I, Mosha N, Abramsky T, Lees S and Watts C (2019) A social empowerment intervention to prevent intimate partner violence against women in a microfinance scheme in Tanzania: findings from the MAISHA cluster randomised controlled trial. The Lancet. Global Health 7, e1423–e1434. [DOI] [PubMed] [Google Scholar]
- Kimani J, Adhiambo J, Kasiba R, Mwangi P, Were V, Mathenge J, Macharia P, Cholette F, Moore S, Shaw S, Becker M, Musyoki H, Bhattacharjee P, Moses S, Fowke KR, McKinnon LR and Lorway R (2020) The effects of COVID-19 on the health and socio-economic security of sex workers in Nairobi, Kenya: emerging intersections with HIV. Global Public Health 15, 1073–1082. [DOI] [PubMed] [Google Scholar]
- Kleijn WC, Hovens JE and Rodenburg JJ (2001) Posttraumatic stress symptoms in refugees: assessments with the Harvard Trauma Questionnaire and the Hopkins symptom Checklist-25 in different languages. Psychological Reports 88, 527–532. [DOI] [PubMed] [Google Scholar]
- Krieger N (2012) Methods for the scientific study of discrimination and health: an ecosocial approach. American Journal of Public Health 102, 936–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL and Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh CM, Corderoy A, Ryan CJ, Hickie IB and Large MM (2019) Association between suicidal ideation and suicide: meta-analyses of odds ratios, sensitivity, specificity and positive predictive value. BJPsych Open 5, e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, Abegaz KH, Abolhassani H, Aboyans V, Abreu LG, Abrigo MRM, Abualhasan A, Abu-Raddad LJ, Abushouk AI, Adabi M, Adekanmbi V, Adeoye AM, Adetokunboh OO, Adham D, Advani SM, Agarwal G, Aghamir SMK, Agrawal A, Ahmad T, Ahmadi K, Ahmadi M, Ahmadieh H, Ahmed MB, Akalu TY, Akinyemi RO, Akinyemiju T, Akombi B, Akunna CJ, Alahdab F, Al-Aly Z, Alam K, Alam S, Alam T, Alanezi FM, Alanzi TM, Alemu BW, Alhabib KF, Ali M, Ali S, Alicandro G, Alinia C, Alipour V, Alizade H, Aljunid SM, Alla F, Allebeck P, Almasi-Hashiani A, Al-Mekhlafi HM, Alonso J, Altirkawi KA, Amini-Rarani M, Amiri F, Amugsi DA, Ancuceanu R, Anderlini D, Anderson JA, Andrei CL, Andrei T, Angus C, Anjomshoa M, Ansari F, Ansari-Moghaddam A, Antonazzo IC, Antonio CAT, Antony CM, Antriyandarti E, Anvari D, Anwer R, Appiah SCY, Arabloo J, Arab-Zozani M, Ariani F, Armoon B, Ärnlöv J, Arzani A, Asadi-Aliabadi M, Asadi-Pooya AA, Ashbaugh C, Assmus M, Atafar Z, Atnafu DD, Atout MMDW, Ausloos F, Ausloos M, Ayala Quintanilla BP, Ayano G, Ayanore MA, Azari S, Azarian G, Azene ZN, Badawi A, Badiye AD, Bahrami MA, Bakhshaei MH, Bakhtiari A, Bakkannavar SM, Baldasseroni A, Ball K, Ballew SH, Balzi D, Banach M, Banerjee SK, Bante AB, Baraki AG, Barker-Collo SL, Bärnighausen TW, Barrero LH, Barthelemy CM, Barua L, Basu S, Baune BT, Bayati M, Becker JS, Bedi N, Beghi E, Béjot Y, Bell ML, Bennitt FB, Bensenor IM, Berhe K, Berman AE, Bhagavathula AS, Bhageerathy R, Bhala N, Bhandari D, Bhattacharyya K, Bhutta ZA, Bijani A, Bikbov B, Bin Sayeed MS, Biondi A, Birihane BM, Bisignano C, Biswas RK, Bitew H, Bohlouli S, Bohluli M, Boon-Dooley AS, Borges G, Borzì AM, Borzouei S, Bosetti C, Boufous S, Braithwaite D, Breitborde NJK, Breitner S, Brenner H, Briant PS, Briko AN, Briko NI, Britton GB, Bryazka D, Bumgarner BR, Burkart K, Burnett RT, Burugina Nagaraja S, Butt ZA, Caetano dos Santos FL, Cahill LE, Cámera LLAA, Campos-Nonato IR, Cárdenas R, Carreras G, Carrero JJ, Carvalho F, Castaldelli-Maia JM, Castañeda-Orjuela CA, Castelpietra G, Castro F, Causey K, Cederroth CR, Cercy KM, Cerin E, Chandan JS, Chang K-L, Charlson FJ, Chattu VK, Chaturvedi S, Cherbuin N, Chimed-Ochir O, Cho DY, Choi J-YJ, Christensen H, Chu D-T, Chung MT, Chung S-C, Cicuttini FM, Ciobanu LG, Cirillo M, Classen TKD, Cohen AJ, Compton K, Cooper OR, Costa VM, Cousin E, Cowden RG, Cross DH, Cruz JA, Dahlawi SMA, Damasceno AAM, Damiani G, Dandona L, Dandona R, Dangel WJ, Danielsson A-K, Dargan PI, Darwesh AM, Daryani A, Das JK, Das Gupta R, das Neves J, Dávila-Cervantes CA, Davitoiu DV, De Leo D, Degenhardt L, DeLang M, Dellavalle RP, Demeke FM, Demoz GT, Demsie DG, Denova-Gutiérrez E, Dervenis N, Dhungana GP, Dianatinasab M, Dias da Silva D, Diaz D, Dibaji Forooshani ZS, Djalalinia S, Do HT, Dokova K, Dorostkar F, Doshmangir L, Driscoll TR, Duncan BB, Duraes AR, Eagan AW, Edvardsson D, El Nahas N, El Sayed I, El Tantawi M, Elbarazi I, Elgendy IY, El-Jaafary SI, Elyazar IRF, Emmons-Bell S, Erskine HE, Eskandarieh S, Esmaeilnejad S, Esteghamati A, Estep K, Etemadi A, Etisso AE, Fanzo J, Farahmand M, Fareed M, Faridnia R, Farioli A, Faro A, Faruque M, Farzadfar F, Fattahi N, Fazlzadeh M, Feigin VL, Feldman R, Fereshtehnejad S-M, Fernandes E, Ferrara G, Ferrari AJ, Ferreira ML, Filip I, Fischer F, Fisher JL, Flor LS, Foigt NA, Folayan MO, Fomenkov AA, Force LM, Foroutan M, Franklin RC, Freitas M, Fu W, Fukumoto T, Furtado JM, Gad MM, Gakidou E, Gallus S, Garcia-Basteiro AL, Gardner WM, Geberemariyam BS, Gebreslassie AAAA, Geremew A, Gershberg Hayoon A, Gething PW, Ghadimi M, Ghadiri K, Ghaffarifar F, Ghafourifard M, Ghamari F, Ghashghaee A, Ghiasvand H, Ghith N, Gholamian A, Ghosh R, Gill PS, Ginindza TGG, Giussani G, Gnedovskaya EV, Goharinezhad S, Gopalani SV, Gorini G, Goudarzi H, Goulart AC, Greaves F, Grivna M, Grosso G, Gubari MIM, Gugnani HC, Guimarães RA, Guled RA, Guo G, Guo Y, Gupta R, Gupta T, Haddock B, Hafezi-Nejad N, Hafiz A, Haj-Mirzaian A, Haj-Mirzaian A, Hall BJ, Halvaei I, Hamadeh RR, Hamidi S, Hammer MS, Hankey GJ, Haririan H, Haro JM, Hasaballah AI, Hasan MM, Hasanpoor E, Hashi A, Hassanipour S, Hassankhani H, Havmoeller RJ, Hay SI, Hayat K, Heidari G, Heidari-Soureshjani R, Henrikson HJ, Herbert ME, Herteliu C, Heydarpour F, Hird TR, Hoek HW, Holla R, Hoogar P, Hosgood HD, Hossain N, Hosseini M, Hosseinzadeh M, Hostiuc M, Hostiuc S, Househ M, Hsairi M, Hsieh VC-R, Hu G, Hu K, Huda TM, Humayun A, Huynh CK, Hwang B-F, Iannucci VC, Ibitoye SE, Ikeda N, Ikuta KS, Ilesanmi OS, Ilic IM, Ilic MD, Inbaraj LR, Ippolito H, Iqbal U, Irvani SSN, Irvine CMS, Islam MM, Islam SMS, Iso H, Ivers RQ, Iwu CCD, Iwu CJ, Iyamu IO, Jaafari J, Jacobsen KH, Jafari H, Jafarinia M, Jahani MA, Jakovljevic M, Jalilian F, James SL, Janjani H, Javaheri T, Javidnia J, Jeemon P, Jenabi E, Jha RP, Jha V, Ji JS, Johansson L, John O, John-Akinola YO, Johnson CO, Jonas JB, Joukar F, Jozwiak JJ, Jürisson M, Kabir A, Kabir Z, Kalani H, Kalani R, Kalankesh LR, Kalhor R, Kanchan T, Kapoor N, Karami Matin B, Karch A, Karim MA, Kassa GM, Katikireddi SV, Kayode GA, Kazemi Karyani A, Keiyoro PN, Keller C, Kemmer L, Kendrick PJ, Khalid N, Khammarnia M, Khan EA, Khan M, Khatab K, Khater MM, Khatib MN, Khayamzadeh M, Khazaei S, Kieling C, Kim YJ, Kimokoti RW, Kisa A, Kisa S, Kivimäki M, Knibbs LD, Knudsen AKS, Kocarnik JM, Kochhar S, Kopec JA, Korshunov VA, Koul PA, Koyanagi A, Kraemer MUG, Krishan K, Krohn KJ, Kromhout H, Kuate Defo B, Kumar GA, Kumar V, Kurmi OP, Kusuma D, La Vecchia C, Lacey B, Lal DK, Lalloo R, Lallukka T, Lami FH, Landires I, Lang JJ, Langan SM, Larsson AO, Lasrado S, Lauriola P, Lazarus JV, Lee PH, Lee SWH, LeGrand KE, Leigh J, Leonardi M, Lescinsky H, Leung J, Levi M, Li S, Lim L-L, Linn S, Liu S, Liu S, Liu Y, Lo J, Lopez AD, Lopez JCF, Lopukhov PD, Lorkowski S, Lotufo PA, Lu A, Lugo A, Maddison ER, Mahasha PW, Mahdavi MM, Mahmoudi M, Majeed A, Maleki A, Maleki S, Malekzadeh R, Malta DC, Mamun AA, Manda AL, Manguerra H, Mansour-Ghanaei F, Mansouri B, Mansournia MA, Mantilla Herrera AM, Maravilla JC, Marks A, Martin RV, Martini S, Martins-Melo FR, Masaka A, Masoumi SZ, Mathur MR, Matsushita K, Maulik PK, McAlinden C, McGrath JJ, McKee M, Mehndiratta MM, Mehri F, Mehta KM, Memish ZA, Mendoza W, Menezes RG, Mengesha EW, Mereke A, Mereta ST, Meretoja A, Meretoja TJ, Mestrovic T, Miazgowski B, Miazgowski T, Michalek IM, Miller TR, Mills EJ, Mini GK, Miri M, Mirica A, Mirrakhimov EM, Mirzaei H, Mirzaei M, Mirzaei R, Mirzaei-Alavijeh M, Misganaw AT, Mithra P, Moazen B, Mohammad DK, Mohammad Y, Mohammad Gholi Mezerji N, Mohammadian-Hafshejani A, Mohammadifard N, Mohammadpourhodki R, Mohammed AS, Mohammed H, Mohammed JA, Mohammed S, Mokdad AH, Molokhia M, Monasta L, Mooney MD, Moradi G, Moradi M, Moradi-Lakeh M, Moradzadeh R, Moraga P, Morawska L, Morgado-da-Costa J, Morrison SD, Mosapour A, Mosser JF, Mouodi S, Mousavi SM, Mousavi Khaneghah A, Mueller UO, Mukhopadhyay S, Mullany EC, Musa KI, Muthupandian S, Nabhan AF, Naderi M, Nagarajan AJ, Nagel G, Naghavi M, Naghshtabrizi B, Naimzada MD, Najafi F, Nangia V, Nansseu JR, Naserbakht M, Nayak VC, Negoi I, Ngunjiri JW, Nguyen CT, Nguyen HLT, Nguyen M, Nigatu YT, Nikbakhsh R, Nixon MR, Nnaji CA, Nomura S, Norrving B, Noubiap JJ, Nowak C, Nunez-Samudio V, Oţoiu A, Oancea B, Odell CM, Ogbo FA, Oh I-H, Okunga EW, Oladnabi M, Olagunju AT, Olusanya BO, Olusanya JO, Omer MO, Ong KL, Onwujekwe OE, Orpana HM, Ortiz A, Osarenotor O, Osei FB, Ostroff SM, Otstavnov N, Otstavnov SS, Øverland S, Owolabi MO, P A M, Padubidri JR, Palladino R, Panda-Jonas S, Pandey A, Parry CDH, Pasovic M, Pasupula DK, Patel SK, Pathak M, Patten SB, Patton GC, Pazoki Toroudi H, Peden AE, Pennini A, Pepito VCF, Peprah EK, Pereira DM, Pesudovs K, Pham HQ, Phillips MR, Piccinelli C, Pilz TM, Piradov MA, Pirsaheb M, Plass D, Polinder S, Polkinghorne KR, Pond CD, Postma MJ, Pourjafar H, Pourmalek F, Poznańska A, Prada SI, Prakash V, Pribadi DRA, Pupillo E, Quazi Syed Z, Rabiee M, Rabiee N, Radfar A, Rafiee A, Raggi A, Rahman MA, Rajabpour-Sanati A, Rajati F, Rakovac I, Ram P, Ramezanzadeh K, Ranabhat CL, Rao PC, Rao SJ, Rashedi V, Rathi P, Rawaf DL, Rawaf S, Rawal L, Rawassizadeh R, Rawat R, Razo C, Redford SB, Reiner RC Jr, Reitsma MB, Remuzzi G, Renjith V, Renzaho AMN, Resnikoff S, Rezaei N, Rezaei N, Rezapour A, Rhinehart P-A, Riahi SM, Ribeiro DC, Ribeiro D, Rickard J, Rivera JA, Roberts NLS, Rodríguez-Ramírez S, Roever L, Ronfani L, Room R, Roshandel G, Roth GA, Rothenbacher D, Rubagotti E, Rwegerera GM, Sabour S, Sachdev PS, Saddik B, Sadeghi E, Sadeghi M, Saeedi R, Saeedi Moghaddam S, Safari Y, Safi S, Safiri S, Sagar R, Sahebkar A, Sajadi SM, Salam N, Salamati P, Salem H, Salem MRR, Salimzadeh H, Salman OM, Salomon JA, Samad Z, Samadi Kafil H, Sambala EZ, Samy AM, Sanabria J, Sánchez-Pimienta TG, Santomauro DF, Santos IS, Santos JV, Santric-Milicevic MM, Saraswathy SYI, Sarmiento-Suárez R, Sarrafzadegan N, Sartorius B, Sarveazad A, Sathian B, Sathish T, Sattin D, Saxena S, Schaeffer LE, Schiavolin S, Schlaich MP, Schmidt MI, Schutte AE, Schwebel DC, Schwendicke F, Senbeta AM, Senthilkumaran S, Sepanlou SG, Serdar B, Serre ML, Shadid J, Shafaat O, Shahabi S, Shaheen AA, Shaikh MA, Shalash AS, Shams-Beyranvand M, Shamsizadeh M, Sharafi K, Sheikh A, Sheikhtaheri A, Shibuya K, Shield KD, Shigematsu M, Shin JI, Shin M-J, Shiri R, Shirkoohi R, Shuval K, Siabani S, Sierpinski R, Sigfusdottir ID, Sigurvinsdottir R, Silva JP, Simpson KE, Singh JA, Singh P, Skiadaresi E, Skou STS, Skryabin VY, Smith EUR, Soheili A, Soltani S, Soofi M, Sorensen RJD, Soriano JB, Sorrie MB, Soshnikov S, Soyiri IN, Spencer CN, Spotin A, Sreeramareddy CT, Srinivasan V, Stanaway JD, Stein C, Stein DJ, Steiner C, Stockfelt L, Stokes MA, Straif K, Stubbs JL, Sufiyan MAB, Suleria HAR, Suliankatchi Abdulkader R, Sulo G, Sultan I, Szumowski Ł, Tabarés-Seisdedos R, Tabb KM, Tabuchi T, Taherkhani A, Tajdini M, Takahashi K, Takala JS, Tamiru AT, Taveira N, Tehrani-Banihashemi A, Temsah M-H, Tesema GA, Tessema ZT, Thurston GD, Titova MV, Tohidinik HR, Tonelli M, Topor-Madry R, Topouzis F, Torre AE, Touvier M, Tovani-Palone MRR, Tran BX, Travillian R, Tsatsakis A, Tudor Car L, Tyrovolas S, Uddin R, Umeokonkwo CD, Unnikrishnan B, Upadhyay E, Vacante M, Valdez PR, van Donkelaar A, Vasankari TJ, Vasseghian Y, Veisani Y, Venketasubramanian N, Violante FS, Vlassov V, Vollset SE, Vos T, Vukovic R, Waheed Y, Wallin MT, Wang Y, Wang Y-P, Watson A, Wei J, Wei MYW, Weintraub RG, Weiss J, Werdecker A, West JJ, Westerman R, Whisnant JL, Whiteford HA, Wiens KE, Wolfe CDA, Wozniak SS, Wu A-M, Wu J, Wulf Hanson S, Xu G, Xu R, Yadgir S, Yahyazadeh Jabbari SH, Yamagishi K, Yaminfirooz M, Yano Y, Yaya S, Yazdi-Feyzabadi V, Yeheyis TY, Yilgwan CS, Yilma MT, Yip P, Yonemoto N, Younis MZ, Younker TP, Yousefi B, Yousefi Z, Yousefinezhadi T, Yousuf AY, Yu C, Yusefzadeh H, Zahirian Moghadam T, Zamani M, Zamanian M, Zandian H, Zastrozhin MS, Zhang Y, Zhang Z-J, Zhao JT, Zhao X-JG, Zhao Y, Zhou M, Ziapour A, Zimsen SRM, Brauer M, Afshin A and Lim SS (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396, 1223–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadkarni A, Weobong B, Weiss HA, McCambridge J, Bhat B, Katti B, Murthy P, King M, McDaid D, Park AL, Wilson GT, Kirkwood B, Fairburn CG, Velleman R and Patel V (2017) Counselling for Alcohol Problems (CAP), a lay counsellor-delivered brief psychological treatment for harmful drinking in men, in primary care in India: a randomised controlled trial. The Lancet 389, 186–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC and Lee S (2008) Suicide and suicidal behavior. Epidemiologic Reviews 30, 133–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor RC and Nock MK (2014) The psychology of suicidal behaviour. The Lancet Psychiatry 1, 73–85. [DOI] [PubMed] [Google Scholar]
- Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, Ferrari AJ, Hyman S, Laxminarayan R, Levin C, Lund C, Medina Mora ME, Petersen I, Scott J, Shidhaye R, Vijayakumar L, Thornicroft G, Whiteford H and Group DMA (2016) Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet 387, 1672–1685. [DOI] [PubMed] [Google Scholar]
- Patel V, Weobong B, Weiss HA, Anand A, Bhat B, Katti B, Dimidjian S, Araya R, Hollon SD, King M, Vijayakumar L, Park AL, McDaid D, Wilson T, Velleman R, Kirkwood BR and Fairburn CG (2017) The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. The Lancet 389, 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt L, Grenfell P, Meiksin R, Elmes J, Sherman SG, Sanders T, Mwangi P and Crago AL (2018) ‘Associations between sex work laws and sex workers’ health: a systematic review and meta-analysis of quantitative and qualitative studies’. PLoS Medicine 15, e1002680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Oquendo MA, Gould M, Stanley B and Davies M (2007) ‘Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants’. The American Journal of Psychiatry 164, 1035–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts ST, Flaherty BP, Deya R, Masese L, Ngina J, McClelland RS, Simoni J and Graham SM (2018) Patterns of gender-based violence and associations with mental health and HIV risk behavior among female sex workers in Mombasa, Kenya: a latent class analysis. AIDS and Behavior 22, 3273–3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M, Reza-Paul S, Lau J, Deering K, Pickles MR and Boily MC (2015) Global epidemiology of HIV among female sex workers: influence of structural determinants. The Lancet 385, 55–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M and Clair S (2003) Syndemics and public health: reconceptualizing disease in bio-social context. Medical Anthropology Quarterly 17, 423–441. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB and Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine 166, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade L, Borges G, Bruffaerts R, Bunting B, de Almeida JM, Florescu S, de Girolamo G, Gureje O, Haro JM, He Y, Hinkov H, Karam E, Kawakami N, Lee S, Navarro-Mateu F, Piazza M, Posada-Villa J, de Galvis YT and Kessler RC (2017) Undertreatment of people with major depressive disorder in 21 countries. British Journal of Psychiatry 210, 119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS (2002) Sex work and HIV/AIDS: Technical Update: Geneva. Available at https://data.unaids.org/publications/irc-pub02/jc705-sexwork-tu_en.pdf (Accessed).
- World Health Organisation (2005) WHO Multi-country Study on Women's Health and Domestic Violence Against Women: Initial Results on Prevalence, Health Outcomes and Women's Responses. Geneva. Available at: https://www.who.int/gender/violence/who_multicountry_study/Introduction-Chapter1-Chapter2.pdf (Accessed). [Google Scholar]
- World Health Organisation (2014) Preventing Suicide: A Global Imperative. Geneva, Switzerland. Available at https://apps.who.int/iris/bitstream/handle/10665/131056/9789241564779_eng.pdf (Accessed). [Google Scholar]
- World Health Organisation (2017) Depression and Other Common Mental Disorders: Global Health Estimates.
- World Health Organisation (WHO) (2010) The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for Use in Primary Care. Geneva: WHO. Available at https://www.who.int/publications/i/item/978924159938-2 (Accessed). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/gmh.2022.44.
click here to view supplementary material