Abstract
Purpose
To determine the predictors for visual outcome after silicone oil removal (SOR) in eyes with complicated retinal detachment.
Patients and Methods
A total of 182 eyes with complicated retinal detachment that had undergone SOR were retrospectively reviewed. Snellen best-corrected visual acuity (BCVA), intraocular pressure (IOP) and complications were recorded at baseline, 1 day, 1 month and 3 months postoperatively. Good visual outcome was defined as best-corrected visual acuity of ≥20/200 at 3 months visit. Factors predicting visual outcome were evaluated using univariate and multivariate analysis.
Results
After SOR, anatomical retinal reattachment was noted in 165 eyes (90.66%). Good visual outcome (VA ≥ 20/200) was achieved in 104 eyes (57.14%) at 3 months after SOR. For the eyes that remained attached after SOR, the percentage of good visual outcome was 63.03%. With univariate and multivariate analysis, visual acuity before SOR (p<0.001), circumferential peripheral retinopexy (p=0.037), additional endolaser during SOR (p=0.004), and pseudophakia status at the last follow up (p=0.021) were associated with visual outcome. Complications after SOR included redetachment (9.4%), hypotony (6.6%) and bullous keratopathy (1.7%).
Conclusion
While anatomically attached retina was achieved in most of the patients, the functional outcomes were still much lower. Good BCVA before SOR and pseudophakia status at the last follow up were predictors for good visual outcomes, whereas circumferential peripheral retinopexy and additional endolaser during SOR were predictors for poor visual outcomes after SOR in eyes with complicated retinal detachment.
Keywords: complicated retinal detachment, silicone oil removal, visual outcome
Introduction
Numerous studies have demonstrated that silicone oil (SO) tamponade is effective in reattaching the retina following severe proliferative vitreoretinopathy (PVR).1–3 Pars plana vitrectomy (PPV) with SO tamponade has become a standard technique in complicated retinal detachment surgery. Retained SO in the eye, however, leads to emulsification and consequent complications such as cataract, glaucoma, keratopathy, and retinopathy.4–7 Therefore, SO is considered a temporary tamponade agent and needs to be removed after a period of stable anatomical attachment. A matched-pair cohort analysis has revealed significantly better visual acuity after oil removal than with oil tamponade.3 Therefore, following a period of successful retinal reattachment, silicone oil removal (SOR) is recommended to avoid potential sight-threatening complications.3–10
Although impressive anatomical success rates (72–96%) after SOR have been reported, only 35–76% of patients achieved visual acuity of ≥20/200.11–18 Functional success rates are not similar to anatomical success rates due to a variety of factors. Previous studies have identified factors associated with anatomical success and predictors for re-detachment after SOR, but data on predictors of visual outcomes are inconclusive.11–18 This study aims to address this knowledge gap by investigating the functional success rate of SOR after successful primary procedure with SO tamponade, and the predictive factors associated with functional outcomes.
Patients and Methods
This study was carried out in accordance with the tenets of the Declaration of Helsinki and was approved by the Khon Kaen University (KKU) Ethics Committee for Human Research. We reviewed medical records of patients who had undergone primary PPV with SO injection followed by SOR at the KKU Eye Center between January 2012 and October 2021. Although patient consent to review their medical records was not required by the ethics committee, data were de-identified and patient data confidentiality was protected. Patients who had undergone complete reattachment of the retina over a period of 3–6 months and/or had developed complications of SO were eligible for SOR. Patients with at least 3 months post-operative follow up were eligible to be included in this study. Cases of endophthalmitis, heavy silicone oil, and post trauma were excluded. In participants with history of multiple retinal procedures, the timing data from only the most recent procedure were used in analysis. Five surgeons (SS, TS, CB, TR and WL) were involved using the same standard surgical technique during the entire study period.
Data collected before the primary retinal detachment repair with SO tamponade included age, gender, laterality, type and causes of retinal detachment, number and location of retinal breaks, presence of giant tear, macular holes, preoperative visual acuity, time to initial PPV, and number of previous retinal surgeries. Data on the types of primary retinal detachment repair procedure were SO viscosity, scleral buckle placement, combined cataract surgery, and circumferential endolaser photocoagulation. Data collected for the SOR procedure included visual acuity and lens status before SOR, complications of SO, additional endolaser photocoagulation, and concomitant cataract surgery. Lens status at the final follow up was also recorded.
The primary outcomes were predictors for visual acuity after SOR. Best-corrected visual acuity (BCVA) after SOR was grouped as good or poor visual outcome. Good visual outcome at a 3-month follow up visit was defined as BCVA of 20/200 and better; poor visual outcome as BCVA poorer than 20/200. Visual acuity was recorded in Snellen notation and converted to ETDRS letters score for analysis. Counting fingers was recorded as 20/1000, hand movements as 20/2000 and light perception as 20/4000 Snellen visual acuity, following Steinberg et al.19 Visual acuity was examined in each patient at 1 day, 1 month and 3 months after SOR.
Statistical Analysis
Data were analyzed using R software version 4.0.5 (The R Foundation for Statistical Computing, Vienna, Austria). Data were presented as mean and standard deviation (SD) unless otherwise noted and descriptive analysis was performed on all variables. Pearson’s Chi square test or Fisher’s exact test was used for comparison between two categorical variables, as appropriate. Student’s t-test was used to compare two sets of numerical data. Numerical data that were not normally distributed are reported as median with interquartile range and analyzed using the Mann–Whitney U-test. The univariate and multivariate relationship between factors and functional outcomes were evaluated using logistic regression analysis. Multilevel mixed-effects linear regression was performed for repeated measurement variables. A p-value of <0.05 was considered statistically significant.
Results
A total of 182 eyes from 174 patients were included in this study. The mean age at presentation was 50.7±11.8 years (50.2±12.4 years in the good visual outcome group and 51.3±11.1 years in the poor visual outcome group, p=0.51). One hundred and nine patients (62.6%) were male. Eight patients (4.6%) had complicated retinal detachment requiring SO tamponade in both eyes. The three most common underlying systemic diseases in the study population were hypertension (51 patients, 29.3%), diabetes mellitus (49 patients, 28.2%) and dyslipidemia (12 patients, 6.9%). Retinal detachments were classified as rhegmatogenous (RRD, 140 eyes, 76.9%), tractional (TRD, 29 eyes, 15.9%) and combined (13 eyes, 7.1%). Demographic data of patients with good (VA ≥20/200) and poor (VA <20/200) visual outcomes were not significantly different (Table 1).
Table 1.
Clinical Findings Before Primary PPV with SO Tamponade
| Patient Characteristics | Total (182 Eyes) | Eyes with Good Visual Outcome (102 Eyes) | Eyes with Poor Visual Outcome (80 Eyes) | P value |
|---|---|---|---|---|
| Types of complicated RD N (%) | 0.099 | |||
| Rhegmatogenous RD | 140 (76.9%) | 83 (81.4%) | 57 (71.3%) | |
| Tractional RD | 29 (15.9%) | 11 (10.8%) | 18 (22.5%) | |
| Combined | 13 (7.2%) | 8 (7.8%) | 5 (6.2%) | |
| Causes of complicated RD N (%) | 0.051 | |||
| Pseudophakic | 56 (30.8%) | 33 (32.4%) | 23 (28.7%) | |
| Macular hole | 19 (10.4%) | 12 (11.8%) | 7 (8.8%) | |
| Proliferative diabetic retinopathy | 19 (10.4%) | 9 (8.8%) | 10 (12.5%) | |
| Choroidal detachment | 13 (7.1%) | 8 (7.8%) | 5 (6.2%) | |
| Uveitis | 4 (2.2%) | 2 (2%) | 2 (2.5%) | |
| Cytomegalovirus retinitis | 5 (2.7%) | 2 (2%) | 3 (3.8%) | |
| Combined causes | 15 (8.2%) | 8 (7.8%) | 7 (8.8%) |
Abbreviations: RD, retinal detachment; PPV, pars plana vitrectomy; SO, silicone oil.
The primary outcome of good visual acuity (VA ≥20/200) at 3 months after SOR was achieved in 104 of 182 eyes (57.14%) whereas anatomical retinal reattachment was achieved in 165 of 182 eyes (90.66%). For the eyes that remained attached after SOR, the percentage of good visual acuity increased to 104 of 165 eyes (63.03%). Table 2 shows clinical details pertaining to primary procedure with SO tamponade. The visual acuity before primary PPV with SO tamponade was significantly associated with good visual outcomes (p=0.001) after SOR. However, history of multiple retinal surgeries was significantly associated with poor visual outcomes (p=0.001). Macular attachment before primary PPV was also associated with good visual outcomes (p=0.047) after SOR. No significant difference between the two groups was found in time to primary procedure, number and location of retinal breaks, presence of giant retinal tear, total retinal detachment, combined scleral buckling, circumferential peripheral retinopexy or SO viscosity (Table 2).
Table 2.
Clinical Findings Before Primary PPV and SOR as Well as Surgical Approaches
| Clinical Findings | Total (182 Eyes) | Eyes with Good Visual Outcome (102 eyes) | Eyes with Poor Visual Outcome (80 Eyes) | P value |
|---|---|---|---|---|
| Primary PPV with SO tamponade | ||||
| Preop BCVA (ETDRS letter score) Median (Q1, Q3) | −3.90 (−15.0, 2.18) | 0.05 (−15.0, 19.95) | −15 (−15.0, 0.05) | <0.001 |
| Time to primary procedure (months) Median (Q1, Q3) | 2 (1.0, 6.0) | 2 (0.8, 5.0) | 3 (1.0, 6.0) | 0.051 |
| No. of retinal surgery N (%) | 0.001 | |||
| Single | 139 (76.4) | 87 (85.3) | 52 (65) | |
| Multiple | 43 (23.6) | 15 (14.7) | 28 (35) | |
| Superior retinal break location N (%) | 47 (26.4) | 31 (31.3) | 16 (20.3) | 0.098 |
| No. of retinal breaks N (%) | 0.157 | |||
| Not seen | 21 (11.8) | 9 (9.1) | 12 (15.2) | |
| Single | 46 (25.8) | 29 (29.3) | 17 (21.5) | |
| Multiple | 111 (58.6) | 61 (61.6) | 50 (63.3) | |
| Presence of giant tear N (%) | 28 (16.4) | 5 (15.6) | 13 (17.6) | 0.662 |
| Presence of PVR N (%) | 0.091 | |||
| Grade A | 13 (7.1) | 8 (7.8) | 5 (6.2) | |
| Grade B | 19 (10.4) | 9 (8.8) | 10 (12.5) | |
| Grade C | 63 (37.9) | 38 (37.3) | 31 (38.8) | |
| Total retinal detachment N (%) | 62 (34.3) | 34 (33.7) | 28 (35) | 0.851 |
| Macula on status N (%) | 12 (6.7) | 10(10) | 2 (2.5) | 0.047 |
| Combined scleral buckling N (%) | 26 (14.5) | 10(10) | 16 (20.3) | 0.053 |
| Combined cataract surgery N (%) | 50 (27.9) | 23(23) | 27 (34.2) | 0.096 |
| Circumferential peripheral retinopexy N (%) | 60 (34.09) | 28 (28.57) | 32 (41.03) | 0.097 |
| Viscosity of SO N (%) | 0.978 | |||
| 1300 cSt. | 137 (75.3) | 76 (74.5) | 61 (76.2) | |
| 5700 cSt. | 20 (10.9) | 12 (11.8) | 8(10) | |
| Silicone Oil Removal | ||||
| BCVA before SOR (ETDRS letter score) Median (Q1, Q3) | 0.05 (−3.9, 35.0) | 35 (0.05, 46.09) | 0.05 (−15.0, 0.05) | <0.001 |
| Time to removal (months) Median (Q1, Q3) | 9.4 (6.2, 13.5) | 9.1 (5.6, 12.8) | 9.8 (6.3, 14.3) | 0.50 |
| Cataract surgery during SOR N (%) | 53 (29.1) | 36 (35.3) | 17 (21.2) | 0.038 |
| Lens status before SOR N (%) | 0.067 | |||
| Phakic | 76 (41.8) | 48 (47.1) | 28 (35) | |
| Pseudophakic | 88 (48.4) | 48 (47.1) | 40 (50) | |
| Aphakia | 18 (9.9) | 6 (5.9) | 12(15) | |
| Additional Endolaser N (%) | 10 (5.5) | 1(1) | 9 (11.2) | 0.005 |
| Pseudophakia at last follow up | 158 (86.81) | 96 (94.12) | 62 (77.50) | 0.002 |
Abbreviations: BCVA, best-corrected visual acuity; cSt, centistokes; ETDRS, Early Treatment Diabetic Retinopathy Study; PVR, proliferative vitreoretinopathy; SO, silicone oil; SOR, silicone oil removal.
Table 2 also shows the clinical details related to the SOR procedure. Best-corrected visual acuity before SOR (p<0.001), combined cataract surgery during SOR (p=0.038), and pseudophakia status after SOR (p=0.002) were significantly associated with good visual outcomes. Endolaser during SOR, however, was associated with poor visual outcomes. Visual outcomes were statistically independent of time to removal or duration of SO tamponade and did not vary significantly (p>0.05) in lens status at time of SOR.
Table 3 shows that eyes with visual acuity in the LP-HM group decreased from 52.2%, at initial presentation, to 21.98%. Moreover, eyes with visual acuity in the ≥20/200 group increased from 17.58% to 57.14% after SOR.
Table 3.
Initial BCVA Before Primary PPV and After SOR
| Final BCVA After SOR (at 3 Mo) | Initial BCVA (Before PPV) | |||
|---|---|---|---|---|
| LP-HM | CF to 20/200 | ≥ 20/200 | Total (%) | |
| ≥ 20/200 | 43 | 37 | 24 | 104 (57.14%) |
| CF to 20/200 | 23 | 12 | 3 | 38 (20.88%) |
| LP-HM | 29 | 6 | 5 | 40 (21.98%) |
| Total (%) | 95 (52.2%) | 55 (30.22%) | 32 (17.58%) | 182 (100%) |
Abbreviations: BCVA, best-corrected visual acuity; PPV, pars plana vitrectomy; SOR, silicone oil removal; CF, counting fingers; HM, hand movement; LP, light perception.
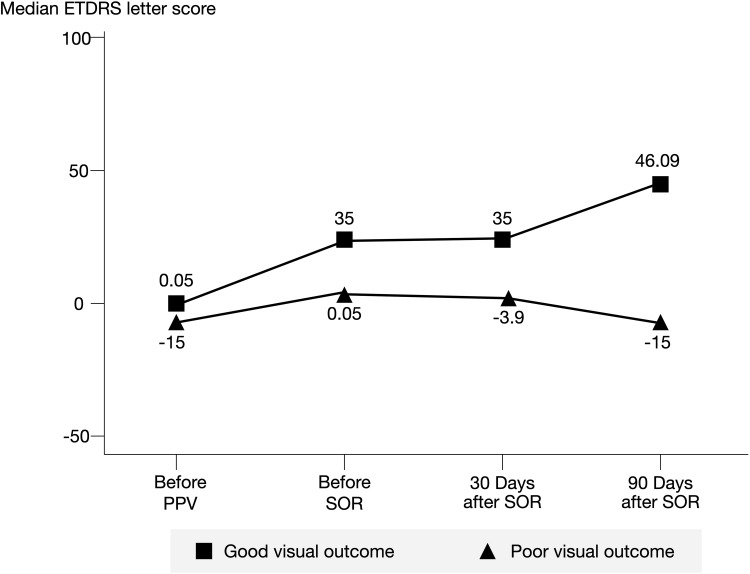
The primary PPV procedure improved median ETDRS letter score from −3.9 (−15.0, 2.18) to 0.05 (−3.9, 35.0) (p<0.001) and SOR further improved it to 35.0 (−3.90, 46.09) (p<0.001). Figure 1 demonstrates change in visual acuity over time in the good and poor visual outcome groups. Before SOR, the median ETDRS letters score in eyes with good visual outcome was 35.0 (0.05, 46.09) and improved to 46.09 (35.0, 54.9) at 3 months, whereas those in eyes with poor visual outcome was 0.05 (−15.0, 0.05) and decreased to −15.0 (−15.0, 0.05) at the last visit, despite attached retinas being observed in 79.78% of patients of this group.
Figure 1.
VA (ETDRS letters) before PPV, SOR and after SOR at 1- and 3-month visits.
Abbreviations: ETDRS, Early Treatment Diabetic Retinopathy Study; PPV, pars plana vitrectomy; SOR, silicone oil removal.
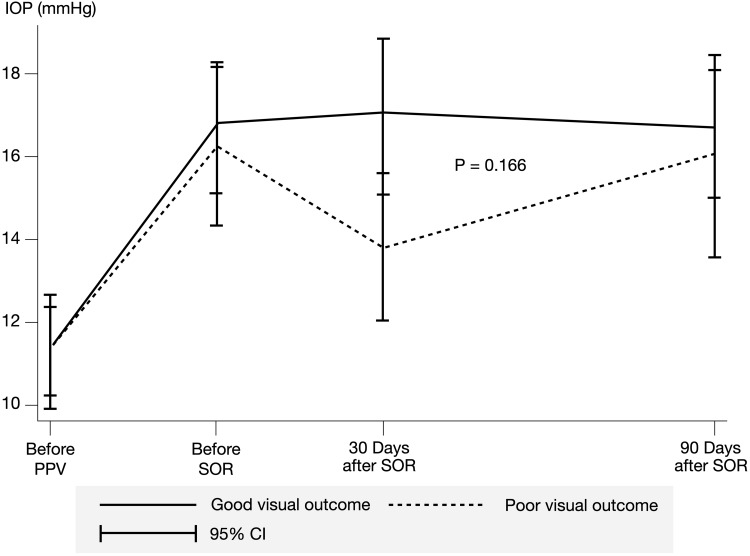
Ocular hypertension was the most common SO-related complication in our study. Mean intraocular pressure (IOP) increased from 11.30 ± 5.58 mmHg before primary procedure to 16.51 ± 8.12 mmHg before SOR and remained stable over 3 months after SOR. During SO tamponade, elevated IOP occurred in 84 eyes (46.2%). Elevated IOP was defined as IOP > 21 mmHg and required topical anti-glaucoma medical treatment. Postoperative ocular hypertension persisted in a total of 57 eyes (31.7%) and 65 eyes (36.1%), at 1 month and 3 months, respectively. However, elevated IOP was well controlled with one or more anti-glaucomatous drugs. Figure 2 shows IOP changes. The mean IOP in eyes with good visual outcome was 16.70 ± 7.90 mmHg before SOR and 16.59 ± 7.62 mmHg at 3 months after SOR. In eyes with poor visual outcome IOP was 16.27 ± 8.43 and 16.05 ± 10.79 mmHg before and after SOR, respectively. These differences were not statistically significant on mixed-effects regression analysis (p=0.166). Other complications after SOR included retinal re-detachment (17 eyes, 9.07%), hypotony (12 eyes, 6.6%) and bullous keratopathy (3 eyes, 1.7%).
Figure 2.
IOP (mmHg) before PPV, SOR and after SOR at 1- and 3-month visits.
Abbreviations: CI, confidence interval; IOP, intraocular pressure; PPV, pars plana vitrectomy; SOR, silicone oil removal.
To determine possible predictors for visual outcomes after SOR, univariate and multivariate relationships between relevant factors and functional outcomes were evaluated using logistic regression analysis (Table 4). On univariate analysis, the factors that could significantly predict the functional outcome were BCVA before primary procedure with SO tamponade (p=0.001), single primary procedure (p=0.002), macula-on status (p=0.047), BCVA before SOR (p<0.001), combined cataract surgery and SOR (p=0.038), additional endolaser during SOR (p=0.005) and pseudophakia at last follow up (p=0.002). Factors insignificantly associated with functional outcomes were time to initial surgery (p=0.051), scleral buckling procedure (p=0.053) and circumferential endolaser retinopexy (p=0.097). After multivariate analysis, BCVA before SOR (p<0.001), additional endolaser (p=0.004) and pseudophakia at last follow up (p=0.021) were predictive of visual outcomes after SOR.
Table 4.
Predictors for Visual Outcomes by Univariate and Multivariate Analysis
| Predictors for Visual Outcomes | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Crude OR (95% CI) | P value | Adjusted OR (95% CI) | P value | |
| BCVA before primary procedure | 0.29 (0.13, 0.63) | 0.001 | 0.67 (0.19, 2.34) | 0.530 |
| Total retinal detachment | 0.93 (0.50, 1.73) | 0.851 | 1.24 (0.50, 3.06) | 0.642 |
| Single primary procedure | 3.12 (1.53, 6.38) | 0.002 | 2.59 (0.89, 7.58) | 0.082 |
| Macula on status | 4.28 (1.09, 28.38) | 0.047 | 1.28 (0.07, 22.78) | 0.866 |
| Combined scleral buckling | 0.44 (0.18, 1.01) | 0.053 | 0.96 (0.27, 3.32) | 0.943 |
| Combined lens surgery | 0.58 (0.30, 1.11) | 0.098 | 0.56 (0.19, 1.69) | 0.306 |
| Circumferential peripheral retinopexy | 0.59 (0.31, 1.10) | 0.097 | 0.39 (0.16, 0.94) | 0.037 |
| BCVA before SOR | 0.06 (0.02, 0.15) | <0.001 | 0.03 (0.01, 0.10) | <0.001 |
| Lens operation during SOR | 2.02 (1.04, 4.03) | 0.038 | 2.59 (0.82, 8.20) | 0.105 |
| Additional endolaser during SOR | 0.08 (0.01, 0.43) | 0.005 | 0.01 (0.00, 0.26) | 0.004 |
| Pseudophakia at last follow up | 4.65 (1.75, 12.35) | 0.002 | 5.48 (1.29, 23.29) | 0.021 |
Abbreviations: OR, odds ratio; CI, confidence interval; BCVA, best-corrected visual acuity; PPV, pars plana vitrectomy; SO, silicone oil; SOR, silicone oil removal.
Discussion
In this study, the anatomical retinal reattachment rate was 90.66% and functional success rate was 57.14% which was in the range of previous reports (35–76%).8,11–17 Previous studies have reported factors associated with anatomical success and predictors for re-detachment after SOR.11–18 Information about predictors for visual outcome, however, have been limited and inconclusive. Al-Wadani et al demonstrated that younger age (<16 years), pars plana lensectomy at primary procedure, and presence of pseudophakia at last follow up were factors associated with final visual acuity of ≥ 20/200 after SOR in patients with complicated retinal detachment.15 In our study, predictors of visual outcomes were BCVA before SOR, circumferential peripheral retinopexy, additional endolaser retinopexy during SOR and pseudophakia at the last follow up.
Compared with a previous study by Al-Wadani, the present study included older patients (35.8 ± 8.7 vs 50.7 ± 11.8 years) and none under the age of 16 years, preventing age-related analysis. In addition, our study failed to show a statistically significant association between combined cataract surgery during primary PPV and visual outcomes. However, our findings agree with those of Al-Wadani in that pseudophakia at the last follow up was associated with good visual outcome after SOR.
The present study identified BCVA before SOR as a predictor of good visual outcome after SOR. Although Tsui et al found the same association in patients with proliferative diabetic retinopathy, this predictor has never been reported in patients with complicated retinal detachment.20 Visual improvement during the repair of complicated retinal detachment using SO tamponade occurs in two steps corresponding with the two-stage procedure. Visual impairment due to retinal detachment is alleviated to a certain degree after the primary PPV procedure as the retina reattaches with SO tamponade, depending on the presence of macula on or off. Optical properties of SO in the vitreous result in high refractive errors which preclude good visual results. The SOR procedure improves visual acuity via SO removal and subsequent cataract surgery with intraocular lens (IOL) placement further improves visual outcomes. Therefore, visual acuity before SOR and pseudophakia status may be predictors for good visual outcome after SOR.
Previous studies have reported that functional vision is restored following combined SOR and cataract surgery with IOL implantation.21,22 Using univariate analysis, our study also revealed that combined cataract surgery and SOR was associated with good visual outcomes. Cataract progression as a result of SO tamponade is the main reversible cause of visual impairment. Previous studies have reported that cataract occurred in 49–100% of eyes with prolonged SO tamponade.1,15 The potential disadvantage of conducting cataract surgery concurrent with SOR is that IOL calculations before primary PPV may be inaccurate due to retinal detachment. A prospective non-randomized study by Krepler et al showed that visual outcomes and complication rates were similar when cataract surgery and SOR were combined in one procedure or conducted separately in two procedures.23 In the present study, however, after adjusting for the factors included in multivariate analysis, cataract surgery during SOR was not significantly associated with final visual outcome.
In our study, circumferential peripheral retinopexy (p=0.037) and additional endolaser during SOR (p=0.004) were associated with poor visual outcomes after SOR. Avitabile et al revealed that circumferential laser treatment prevented re-detachment after SOR.24 However, these two procedures were not routinely conducted during SOR in the present study. Only 60 eyes (34.09%) underwent circumferential peripheral retinopexy and only 10 eyes (5.5%) had additional endolaser during SOR. The reason why both procedures were significantly associated with poor visual outcomes can be explained by the fact that these procedures are usually performed in difficult cases with potential for re-detachment, for example, TRD and severe proliferative vitreoretinopathy. These eyes usually have poor initial visual acuity and poor visual outcome. In our study, among 60 eyes with circumferential peripheral retinopexy, RRD, TRD and combined were noted in 36, 18 and 6 eyes, respectively. The result showed that 17 eyes (47.2%) with RRD, 11 eyes (61.1%) with TRD, and 4 eyes (66.7%) with combined TRD-RRD had poor visual outcomes. Among 10 eyes with additional laser during SOR, there were 8 eyes with RRD, one eye with TRD, and one eye with combined type. In TRD, additional endolaser was performed in cases of neovascularization and large area of ischemic retina. In RRD, it was selectively performed in eyes with severe proliferative vitreoretinopathy. The result showed that seven eyes (87.5%) with RRD, all eyes with TRD and combined type had poor visual outcomes.
A previous study reported that poor visual outcome was associated with having undergone multiple primary procedures,16 and univariate analysis in our study also showed that undergoing a single primary procedure was associated with good visual outcome (odds ratio 3.12, p=0.002). However, after multivariate analysis, this factor is not significantly associated with visual outcome.
BCVA before the primary procedure, total extent of retinal detachment, macular status, combined scleral buckling, and combined lens surgery are reportedly associated with anatomical success and may be predictors for visual outcome.11–18,25 In our study, good BCVA before primary procedure and macular on status were significantly associated with good visual outcome in univariate analysis, but not significantly after multivariate analysis. The other factors did not reach a significant level in both univariate and multivariate analysis. These results may be explained by the fact that improved visual function may not occur, despite anatomical reattachment. Therefore, factors reportedly associated with anatomical reattachment may not be the same as those with good visual outcome.
Complications after SOR were also analyzed in this study. Ocular hypertension was the most common complication of SO tamponade, and SOR did not reduce this complication, given the sustained IOP shown in our data. The removal of SO does not completely remove droplets in the trabecular meshwork. The IOP may be lower on the first postoperative day and gradually return to the preoperative level. Issa et al also reported ocular hypertension and cataract progression as common complication.26 Consistent with previous findings, our study showed that redetachment, hypotony and bullous keratopathy were complications after SOR.26 However, we did not find a statistically significant difference between the mean IOPs of the good and poor visual outcome groups. Theoretically, early SO removal would reduce the chance of SO complications and improve visual outcome, but in the present study time to SO removal did not have a significant effect on the final visual outcome. This may be due to most patients having had SO removal later than 6 months after SO tamponade, with only 44 out of 182 eyes (24%) having earlier removal.
In our study, BCVA before SOR, circumferential peripheral retinopexy, additional endolaser during SOR and pseudophakia status at the last follow up were predictors for visual outcome after SOR. Pseudophakia has been reported previously as a predictor, but the other three factors have not been reported in patients with complicated retinal detachment. However, there were some limitations in the present study. Firstly, it is retrospective, and some patients may be excluded due to incomplete data. Secondly, our center is a tertiary eye center receiving referrals from primary hospitals and referring patients back after successful surgery and in stable condition. This may result in underestimation of the number of patients with good visual outcomes. Another limitation is lacking information on choroidal and macular thickness which might have some effect on the visual outcome.
Conclusion
Our study demonstrates anatomical success of 90.66% and functional success of 57.14% after SOR. Good BCVA before SOR and pseudophakia status at the last follow up were predictors for good visual outcomes, whereas circumferential peripheral retinopexy and additional endolaser during SOR were predictors for poor visual outcomes. Knowledge of these predictors may help to fully inform patients and to enhance clinical decision-making by ophthalmologists.
Acknowledgments
The authors would like to thank Dr. Kaewjai Thepsuthammarat, Clinical Epidemiology Unit, Faculty of Medicine, Khon Kaen University for helping in statistical analyses.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gonvers M. Temporary silicone oil tamponade in the management of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1985;100(2):239–245. doi: 10.1016/0002-9394(85)90788-3 [DOI] [PubMed] [Google Scholar]
- 2.Lean JS, Boone DC, Azen SP. Vitrectomy With Silicone Oil or Sulfur Hexafluoride Gas in Eyes With Severe Proliferative Vitreoretinopathy: results of a Randomized Clinical Trial: silicone Study Report 1. Arch Ophthalmol. 1992;110(6):770–779. doi: 10.1001/archopht.1992.01080180042027 [DOI] [PubMed] [Google Scholar]
- 3.Hutton WL, Azen SP, Blumenkranz MS, et al. The effects of silicone oil removal. Silicone Study Report 6. Arch Ophthalmol. 1994;112(6):778–785. doi: 10.1001/archopht.1994.01090180076038 [DOI] [PubMed] [Google Scholar]
- 4.Ichhpujani P, Jindal A, Jay Katz L. Jay Katz L Silicone oil induced glaucoma: a review. Graefes Arch Clin Exp Ophthalmol. 2009;247(12):1585–1593. doi: 10.1007/s00417-009-1155-x [DOI] [PubMed] [Google Scholar]
- 5.Lai W, Wong D, Li K, Leow P. Emulsification and inverted hypopyon formation of oxane HD in the anterior chamber. Graefes Arch Clin Exp Ophthalmol. 2008;246(11):1633–1635. doi: 10.1007/s00417-008-0851-2 [DOI] [PubMed] [Google Scholar]
- 6.Miller JB, Papakostas TD, Vavvas DG. Complications of emulsified silicone oil after retinal detachment repair. Semin Ophthalmol. 2014;29(5–6):312–318. doi: 10.3109/08820538.2014.962181 [DOI] [PubMed] [Google Scholar]
- 7.Ferrara M, Coco G, Sorrentino T, et al. Retinal and corneal changes associated with intraocular silicone oil tamponade. J Clin Med. 2022;11(17):5234. doi: 10.3390/jcm11175234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zilis JD, McCuen BW, De Juan E, Stefansson E, Machemer R. Results of silicone oil removal in advanced proliferative vitreoretinopathy. Am J Ophthalmol. 1989;108(1):15–21. doi: 10.1016/S0002-9394(14)73254-4 [DOI] [PubMed] [Google Scholar]
- 9.Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988;95(7):860–867. doi: 10.1016/S0161-6420(88)33080-0 [DOI] [PubMed] [Google Scholar]
- 10.Lucke KH, Foerster MH, Laqua H. Long-term results of vitrectomy and silicone oil in 500 cases of complicated retinal detachments. Am J Ophthalmol. 1987;104(6):624–633. doi: 10.1016/0002-9394(87)90176-0 [DOI] [PubMed] [Google Scholar]
- 11.Teke MY, Balikoglu-Yilmaz M, Yuksekkaya P, et al. Surgical outcomes and incidence of retinal redetachment in cases with complicated retinal detachment after silicone oil removal: univariate and multiple risk factors analysis. Retina. 2014;34(10):1926–1938. doi: 10.1097/IAE.0000000000000204 [DOI] [PubMed] [Google Scholar]
- 12.Jonas JB, Knorr HL, Rank RM, Budde WM. Retinal redetachment after removal of intraocular silicone oil tamponade. Br J Ophthalmol. 2001;85(10):1203–1207. doi: 10.1136/bjo.85.10.1203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falkner CI, Binder S, Kruger A. Outcome after silicone oil removal. Br J Ophthalmol. 2001;85(11):1324–1327. doi: 10.1136/bjo.85.11.1324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Velikay-Parel M, Kiss CG, Ivastinovic D, Richter-Mueksch S. Encircling band, laser retinopexy and lens removal as standard procedure in complicated retinal detachment shows a good clinical outcome. Acta Ophthalmol. 2011;89(7):629–633. doi: 10.1111/j.1755-3768.2009.01763.x [DOI] [PubMed] [Google Scholar]
- 15.Al-Wadani SF, Abouammoh MA, Abu El-Asrar AM. Visual and anatomical outcomes after silicone oil removal in patients with complex retinal detachment. Int Ophthalmol. 2014;34(3):549–556. doi: 10.1007/s10792-013-9857-9 [DOI] [PubMed] [Google Scholar]
- 16.Dhalla K, Kapesa I, Odouard C. Incidence and risk factors associated with retinal redetachment after silicone oil removal in the African population. Int Ophthalmol. 2017;37(3):583–589. doi: 10.1007/s10792-016-0309-1 [DOI] [PubMed] [Google Scholar]
- 17.Ratanapakorn T, Thongmee W, Meethongkam K, et al. Emulsification of different viscosity silicone oil in complicated retinal detachment surgery: a randomized double-blinded clinical trial. Clin Ophthalmol. 2020;14:359–367. doi: 10.2147/OPTH.S242804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choudhary MM, Choudhary MM, Saeed MU, Ali A. Removal of silicone oil: prognostic factors and incidence of retinal redetachment. Retina. 2012;32(10):2034–2038. doi: 10.1097/IAE.0b013e3182562045 [DOI] [PubMed] [Google Scholar]
- 19.Steinberg EP, Tielsch JM, Schein OD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–638. doi: 10.1001/archopht.1994.01090170074026 [DOI] [PubMed] [Google Scholar]
- 20.Tsui MC, Hsieh YT, Yang CM. Silicone oil removal after extended tamponade in proliferative diabetic retinopathy-a long range of follow-up. Eye. 2020;34:2307–2314. doi: 10.1038/s41433-020-0815-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Habboubi HF, Al-Zamil W, Al-Habboubi AA, Khandekar R. Visual outcomes and refractive status after combined silicone oil removal/cataract surgery with intraocular lens implantation. J Ophthalmic Vis Res. 2018;13(1):17–22. doi: 10.4103/jovr.jovr_252_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karimi S, Nikkhah H, Farzanbakhsh S, Karjou Z, Safi S. Outcome of combined phacoemulsification/intraocular lens implantation and silicone oil removal. Int Ophthalmol. 2022;42(7):2267–2272. doi: 10.1007/s10792-022-02227-3 [DOI] [PubMed] [Google Scholar]
- 23.Krepler K, Mozaffarieh M, Biowski R, Nepp J, Wedrich A. Cataract surgery and silicone oil removal: visual outcome and complications in a combined vs two step surgical approach. Retina. 2003;23(5):647–653. doi: 10.1097/00006982-200310000-00007 [DOI] [PubMed] [Google Scholar]
- 24.Avitabile T, Longo A, Lentini G, Reibaldi A. Retinal detachment after silicone oil removal is prevented by 360 degrees laser treatment. Br J Ophthalmol. 2008;92(11):1479–1482. doi: 10.1136/bjo.2008.140087 [DOI] [PubMed] [Google Scholar]
- 25.Lam RF, Cheung BT, Yuen CY, Wong D, Lam DS, Lai WW. Retinal redetachment after silicone oil removal in proliferative vitreoretinopathy: a prognostic factor analysis. Am J Ophthalmol. 2008;145(3):527–533. doi: 10.1016/j.ajo.2007.10.015 [DOI] [PubMed] [Google Scholar]
- 26.Issa R, Xia T, Zarbin MA, Bhagat N. Silicone oil removal: post-operative complications. Eye. 2020;34(3):537–543. doi: 10.1038/s41433-019-0551-7 [DOI] [PMC free article] [PubMed] [Google Scholar]