To the Editor:
The proportion of physicians who have a positive screening for depression increases by a factor of five to six times with the start of residency.1 The long work hours that are typical of residency are a potential driver of worsening depressive symptoms.2 We used an emulated trial design, a method that is suited to simulate a randomized trial when a trial is not feasible, to estimate the association between work-hour levels and change in depressive symptoms during the first year of residency.
We analyzed data from repeated cohorts of U.S. physicians who were recruited annually from April through June during the years 2009 to 2020 to participate in the Intern Health Study (17,082 participants), a national sample of interns (physicians in their first postgraduate year). We assessed depressive symptoms by means of the Patient Health Questionnaire 9-item version (PHQ-93) at baseline (1 to 2 months before the start of the internship) and then quarterly throughout the internship year. On the PHQ-9, depression is categorized as minimal by a score of 0 to 4, mild by a score of 5 to 9, moderate by a score of 10 to 14, moderately severe by a score of 15 to 19, and severe by a score of 20 to 27.3 At baseline, we also assessed participants’ demographic characteristics (i.e., age, sex, marital status, and parental status), surgical or non-surgical specialty, early family environment, personality trait of neuroticism, and history of depression. We gathered data on participant-reported work hours over the preceding week, stressful life events, and medical errors quarterly during the internship.
We emulated a target trial of the effect of weekly work hours on depression, categorizing weekly work hours into increasing levels, starting from 0 to 20 hours per week and going up to more than 90 hours per week (Table S1 in the Supplementary Appendix, available with the full text of this letter at NEJM.org). We used standardization to estimate the mean change in PHQ-9 scores from baseline associated with each work-hour level, with adjustment for covariates and modeling with post-stratification and attrition weights (see the Supplementary Methods section).
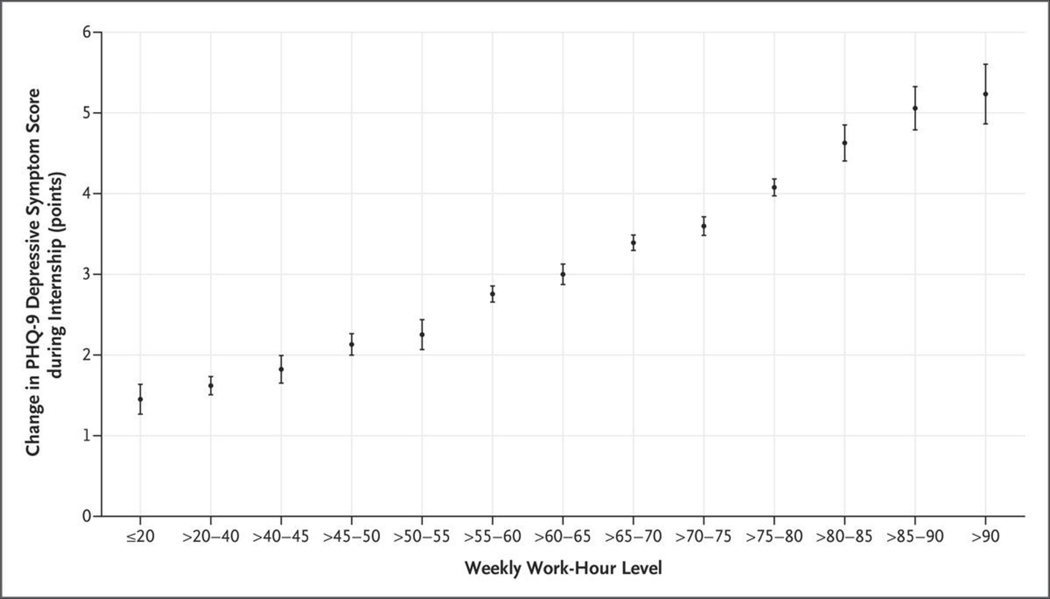
At baseline, the interns’ median PHQ-9 total score was 2.0 points and the mean (±SD) score was 2.7±3.1 points. The mean work hours, as assessed quarterly, were 63±19 per week (median, 67 hours per week; interquartile range, 50 to 76). At higher work-hour levels, interns’ PHQ-9 total scores more often fell within higher cate-gories of severity of depression, with 33.4% of the interns meeting PHQ-9 criteria for depression at a level of more than 90 work hours per week (Fig. S2). After standardization, the estimated change from baseline in the PHQ-9 score increased (indicating worsening depressive symptoms) with increasing work-hour levels, a pattern consistent with a dose–response relationship (Fig. 1). For the work-hour category of more than 40 and up to 45 hours per week, the estimated increase from baseline in the PHQ-9 score was 1.8 points (95% confidence interval [CI], 1.7 to 2.0). In contrast, in the work-hour category of more than 90 hours per week, the increase was 5.2 points (95% CI, 4.9 to 5.6). Sensitivity analyses, which included an analysis for clustering according to institution, provided results that were similar to those of the primary analysis.
Figure 1. Estimated Mean Change in the PHQ-9 Score for Depressive Symptoms during Physician Internship, According to Weekly Work-Hour Levels, among 17,082 Participants in the Intern Health Study, 2009–2020.
Scores on the Patient Health Questionnaire 9-item version (PHQ-9) were assessed at baseline (1 to 2 months before the start of the internship) and then quarterly throughout the internship year. On the PHQ-9, depression is categorized as minimal by a score of 0 to 4, mild by a score of 5 to 9, moderate by a score of 10 to 14, moderately severe by a score of 15 to 19, and severe by a score of 20 to 27. The widths of the 95% confidence intervals (I bars) have not been adjusted for multiplicity and may not be used in place of hypothesis testing. The analysis was adjusted for the baseline factors of sex, surgical or nonsurgical specialty, personality trait of neuroticism, history of depression before the internship, early family environment, age, cohort calendar year, marital status, parental status, and time-varying factors of stressful life events and medical errors (see the Supplementary Appendix for details of measures).
In this large, national cohort study involving U.S. medical interns, higher work hours were associated with progressively greater increases in depressive symptoms from baseline. Specifically, the increase in symptom scores was almost 3 times as high in the highest work-hour category (>90 hours per week) as in the work-hour category of more than 40 and up to 45 hours per week, which is the category closest to the hours typical of most nonmedical professions. Given that this was an observational study, it is possible that the results could be explained by residual confounding, even though the design and analytic approaches we used emulated those of a clinical trial.
Reduction in work hours has received only limited mention in the recent recommendations and policy statements addressing clinician well-being.4,5 Our findings suggest that limiting the number of hours worked per week by residents has the potential to reduce rates of depression among early-career trainees.
Supplementary Material
THIS WEEK’S LETTERS.
| 1522 | Work Hours and Depression in U.S. First-Year Physicians |
| 1524 | IL-1RA Antibodies in Myocarditis after SARS-CoV-2 Vaccination |
| 1527 | Brentuximab Vedotin in Advanced Hodgkin’s Lymphoma |
| 1528 | Anti-BDCA2 Antibody for Cutaneous Lupus Erythematosus |
| 1529 | Once-Weekly Dulaglutide for Treatment of Youths with Type 2 Diabetes |
| 1531 | A 49-Year-Old Man with Hypoglycemia |
Acknowledgments
Supported by a grant (R01MH101459, to Dr. Sen) from the National Institutes of Heath.
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Yu Fang, University of Michigan Medical School Ann Arbor, MI
Sara Lodi, Boston University School of Public Health Boston, MA
Tasha M. Hughes, University of Michigan Medical School Ann Arbor, MI
Elena Frank, University of Michigan Medical School Ann Arbor, MI
Srijan Sen, University of Michigan Medical School Ann Arbor, MI
Amy S.B. Bohnert, University of Michigan Medical School Ann Arbor, MI
References
- 1.Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015; 314:2373–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Philibert I. What is known: examining the empirical literature in resident work hours using 30 influential articles. J Grad Med Educ 2016; 8:7 95–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;1 6:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office of the Surgeon General. Addressing health worker burnout: the U.S. Surgeon General’s advisory on building a thriving health workforce. 2022. (https://wwwhhsgov/surgeongeneral/priorities/health-worker-burnout/index.html ). [PubMed]
- 5.National Academies of Sciences, Engineering, and Medicine. Taking action against clinician burnout: a systems approach to professional well-being. Washington, DC: National Academies Press, 2019. (https://www.nap.edu/catalog/25521). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.