INTRODUCTION
Resilience refers to the quality of being able to overcome adversity. [1] Studies conducted in the United States[2] and China[3] following the 2019 coronavirus disease (COVID-19) pandemic reported reduced resilience levels among medical residents. High resilience levels are associated with low burnout levels among residents.[4] Physician burnout affects patients’ safety and quality of care.[5] In particular, emergency physicians (EPs) are more prone to exhaustion or poor resilience, as their turnover intention tends to be higher.[6] Therefore, improving EPs’ resilience is imperative.
Common program requirements in medical residency emphasize the importance of residents’ mental, emotional, and physical wellbeing for their competency and resilience and that the responsibilities of managing themselves and supporting fellow medical staff are vital aspects of professionalism.[7] This warrants policies or programs to improve residents’ overall wellbeing. A survey of US residents revealed that resilience was higher among residents who received family support, support from the residency program, and guaranteed autonomy.[4] Among the common competencies required for residents’ training curriculum in Korea, self-management items under the professionalism category include residents’ wellbeing and self-control/stress management.[8] However, education or programs to improve doctors’ wellbeing and resilience in Korea are lacking.
Among the North American residency programs, various institutional and experimental methods of resilience management have been studied. These include the Wellness Committee run by residents,[9] workshops to improve pediatric residents’ emotional intelligence,[10] a mindfulness meditation program for family medicine residents,[11] an online wellbeing course for family medicine residents,[12] a wellness program for otolaryngology residents,[13] a mindfulness-based cognitive training program for surgical residents,[14] and an online resilience course for psychiatry residents.[15] These studies reported improvements in residents’ exhaustion and stress levels, resilience, wellness scores, emotional intelligence, and mindful awareness. Furthermore, residents’ wellbeing and their relationships with colleagues showed improvements.[16] In O’Connell et al[17] assessment of a resilience workshop that facilitated reflection, collaboration, and communication among emergency medicine residents, participants reported satisfaction with sharing their experiences of feeling resilient with their peers.
Although art therapy for doctors is limited, it can be used for doctors’ emotion improvement. A study of mindfulness-compassion art therapy for internal medicine residents reported a significant reduction in emotional exhaustion and depersonalization during burnout.[18] Furthermore, art therapy for healthcare workers has been shown to decrease burnout and enhance resilience.[19] Art therapy is used to improve cognitive and sensory-motor functions, promote self-esteem and self-awareness, develop emotional resilience, increase insight and improve social skills, resolve and mitigate conflict and pain, and grow social/ecological skills.[20]
Emotion-focused art therapy (EFAT) can help participants balance their experiences and emotions by encouraging them to appropriately express their emotions.[21] This can lead to emotional changes through the experience of negative and adaptive emotions. That is, emotions are reconstructed through the expression and regulation of negative emotions, wherein one becomes aware of, understands, and accepts their emotions.[21] Art therapy that focuses on emotion regulation may help one face situations, perceive oneself as a whole, and enable self-growth.[22]
As such, workshops to improve doctors’ resilience and wellbeing and to reduce burnout vary greatly in terms of their application. Except for a few programs that target specialists, these programs often target residents as they tend to be more exhausted and have lower resilience levels. Therefore, this study aimed to evaluate whether the EFAT could improve medical residents’ and specialists’ resilience levels and self-image. In addition, we sought recommendations for the implementation of art therapy for emotional recovery for not only EPs but also other specialists.
METHODS
Research design and study participants
This study compared the resilience and self-image of participants before and after the EFAT program. Between December 2021 and January 2022, EPs in three university teaching hospitals in South Korea were recruited. A researcher (KHP) explained the study’s purpose to the EPs of each hospital, and those willing to participate in the workshop on the scheduled were included. At the time of the study, there were 23 specialists and 27 residents from the three hospitals. This study was approved by the Institutional Review Board of Yonsei University Wonju Severance Christian Hospital (CR321108).
Emotion-focused art therapy
The EFAT was delivered by an accredited art therapist (ESK) with a PhD in art therapy. The EFAT was offered as a single, two-hour session. The following steps were performed.
Step 1: searching for emotions; identifying emotional images related to “me” in the emotion card.
Step 2: understanding emotions; sharing one’s feelings with others and making a “heart bandage” of comfort and giving it to each other.
Step 3: accepting emotions; drawing or writing down unwanted emotions on a balloon and blowing it away.
Step 4: emotional growth; expressing what gives me strength through drawings or in writing.
Step 5: creating acrylic mood light.
Resilience
Resilience was measured before and after the EFAT using the 25-item Connor-Davidson Resilience Scale (CD-RISC 25), which measures an individual’s ability to cope with stress and adversity.[1] The items are rated on a 5-point Likert scale from 0 (not true at all) to 4 (true nearly all of the time). The total score ranges from 0 to 100; higher scores indicate a higher level of resilience. The Korean version of the CD-RISC was used in this study, and Cronbach’s α was 0.91, indicateing adequate reliability.[23]
Tree drawing test
The tree drawing test is a qualitative tool to investigate changes in self-image before and after an art therapy program. It is a projection test that involves drawing a tree on a sheet of paper, according to given instructions, and reflects the participant’s psychological state based on the characteristics of the tree, such as its shape and spatial location.[24] In other words, tree drawing can reveal one’s subconscious self-image, adaptation to reality, maturity level, and harmony within the human.[25] An A4-size paper, a pencil, and an eraser were placed vertically on each participant’s respective desk, and they were told that they could use the paper as desired. Participants were instructed to draw a tree before and after the EFAT, and the shapes and different meanings of the tree drawings were compared. After the participants drew the trees, they were asked to write down the following: the type of tree, the age of the tree, the mood of the tree, the health of the tree, what is around the tree, the wish of the tree, what the tree will become in the future, and the person whom they thought of while drawing the tree.
Response to art therapy
After the EFAT, participants were asked to rate their satisfaction with the EFAT on a 5-point Likert scale from 1 (never satisfied) to 5 (very satisfied) at once. They were also asked to describe what they appreciated about the EFAT and what they thought could be improved.
Statistical analysis
Resilience scores before and after the EFAT were compared using a paired t-test. All continuous variables are presented as the mean ± standard deviation. SPSS version 23.0 (IBM Corp., USA) was used for the statistical analyses. The significance level was set at P<0.05.
The tree drawing was interpreted symbolically by considering the overall impression and examining the shape of each tree, followed by its size, location, the shape of branches, the shape of roots and fruits, and the presence or absence of knots. As elements of a morphological analysis of the entire figure, the tree columns, branches, crowns, roots, fruits, and positions were analyzed based on interpretations made in previous studies.[24-26] The three drawings were interpreted by the same art therapist (SKE) who conducted the EFAT. Qualitative content analysis of the narrative contents was performed by KHP.
RESULTS
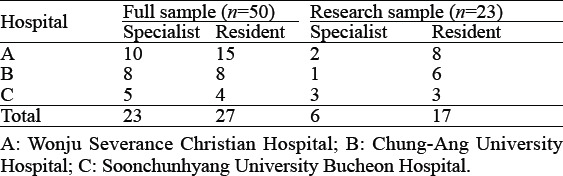
A total of 23 EPs (46.0%; 6 specialists and 17 residents) participated in this study. All participants underwent EFAT and art therapy for the first time. The number of residents in their first, second, third, and fourth years was 4, 3, 4, and 6, respectively. At Wonju Severance Christian Hospital, which had a relatively large number of participants, two EFAT workshops were held; meanwhile, Chung-Ang University Hospital and Soonchunhyang University Bucheon Hospital held one each (Table 1). In terms of sex, there was one female resident in Wonju Severance Christian Hospital, with the rest being male.
Table 1.
Number of participants in each hospital
Comparison of resilience levels before and after the EFAT
EPs’ CD-RISC scores increased significantly after the EFAT (60.61±8.97 vs. 68.48±10.25, P<0.001; Figure 1). The participant with the lowest score (41 points) before the EFAT also had the lowest score (42 points) after the EFAT. The participant with the highest score (92 points) after the EFAT obtained a score of 75 points before the EFAT, indicating an increase by 1.22 times. One participant’s score increased from 48 to 62, indicating an increase by a factor of 1.29. Meanwhile, two participants, both of whom were specialists, obtained the same, above-average scores before and after the EFAT (66 points and 76 points, respectively).
Figure 1.
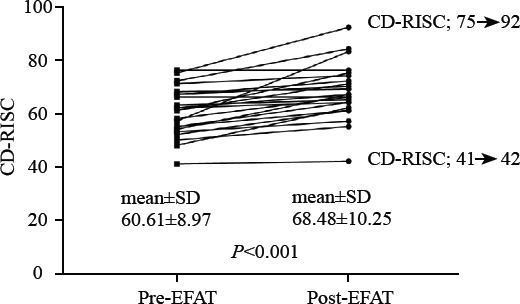
Paired comparison of resilience scores pre- and post-EFAT. CD-RISC: Connor-Davidson Resilience Scale; EFAT: emotion-focused art therapy.
Comparison of the tree drawings before and after the EFAT
Changes in different elements of the trees and their interpretations are presented in Table 2. There were significant changes in the trunks, branches, tree heads, roots, fruits, and locations. After EFAT, a tree whose shape had not been completed properly was completed appropriately. The analysis of the tree drawing test indicated that following the EFAT, participants perceived improvements in the strength of their inner self, the stability of their psychological states, and their energy and self-confidence levels. In addition, there was an improvement in communication with oneself and the environment and a greater desire for a sense of accomplishment (supplementary Table 1).
Table 2.
Summary of participants’ feedback regarding the EFAT
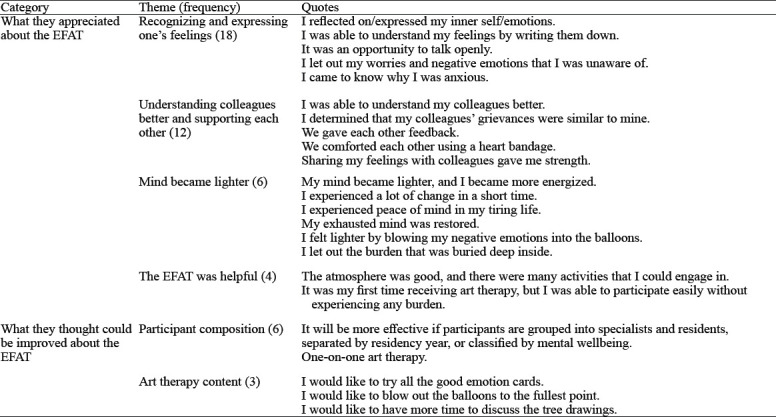
Response to the EFAT
The participants’ average satisfaction score was 4.52±0.51. The narrative contents regarding what participants apprecated about the EFAT were categorized into four themes: (1) recognizing and expressing one’s feelings; (2) understanding colleagues better and supporting each other; (3) making mind lighter and (4) the benefit of EFAT. Participants’ suggestions for improvements mostly pertained to the participant composition in the EFAT. They expressed wanting to use all the good emotion cards if they had more time. They also wanted to blow up the balloons to the fullest points, but due to COVID-19-related restrictions on the balloon-blowing task, they were unable to do so. Many participants expressed interest in learning more about the interpretation of the tree drawing (Table 2).
DISCUSSION
Our results suggest that EPs’ resilience scores and self-image improved after the EFAT. Participants were particularly satisfied with being able to recognize and express their emotions, as well as being able to understand and support their peers.
The average CD-RISC score of participants before the EFAT was similar to that (59.43±13.23) reported in a study on Korean EPs, but the average score after the EFAT in this study was significantly higher than that obtained in the aforementioned study.[27] The average CD-RISC scores of healthy adults and students in Korea are 66.8[28] and 67.2,[29] respectively, which are similar to the improved resilience scores after the EFAT in this study. Therefore, it can be interpreted that the temporary improvement in resilience is similar to the resilience levels of the general adult population in Korea. A US study using Visual Explorer for emergency medicine residents reported an average CD-RISC score of 76.5, which is lower than the average scores of healthy adults in the US.[17] While the CD-RISC scores of the general Korean population are lower than those of the general US population owing to cultural differences, the average post-EFAT score in this study was higher than that of the general Korean population. In addition, given that our study and Kim et al’s[27] study were conducted during the COVID-19 pandemic, whereas the aforementioned studies were conducted before the pandemic, it is necessary to follow up on the resilience levels of EPs after the pandemic ends.
Furthermore, changes in self-image after the EFAT were investigated using the tree drawing test. Although the duration of the EFAT was short, there was a noticeable change in participants’ tree drawings. The EFAT provided an opportunity for participants to explore and express their internal emotions and to accept, understand, and empathize with their colleagues’ feelings. These, in turn, made their emotions more stable. Changes in the shape of the trees after the EFAT may be attributed to an increase in positive emotions. Although the interpretation of the tree drawings may be subjective, the tree drawing test as an interpretive tool in art therapy can effectively assess one’s sense of self-identity or self-esteem. [30]
All participants in this study underwent EFAT, as well as art therapy, for the first time. Moreover, the workshop was conducted approximately two years after the COVID-19 outbreak, when the Omicron variant dominated most of the cases. In the event of severe stress and isolation, such as a pandemic, art therapy can be a healthy approach to care for and express oneself,[31] and participants’ responses to the EFAT in this study confirm this notion. In particular, most participants stated that they were able to recognize and express their emotions for the first time. These findings suggested that most participants experienced severe stress due to low resilience, and an art-based workshop provided an opportunity for deep reflection and expression without any negative effects.[32] Recognition and expression of feelings led to the perception of a temporary change in the state of mind. For example, although there were restrictions on the balloon-blowing activity as a precautionary measure against COVID-19, some participants stated wanting to blow up the balloons to the fullest point. This was interpreted as them wanting some relief from their negative emotions.
In addition, they stated that as residents and specialists belonging to the same hospital, they realized that their colleagues experienced the same concerns and, therefore, understood each other better. Given that opportunities to share feelings while working in the emergency department are limited and that the EFAT was conducted when social distancing was implemented, participants may have felt a great sense of isolation. A previous study of the Energy Leadership Program for surgical residents reported that participants felt connected with and supported by their colleagues and that trust was formed by getting to know each other well.[33]
Furthermore, in this study, various suggestions were made regarding the participant composition for EFAT. Participants may have been limited in expressing themselves in the EFAT due to workplace hierarchy. In another study, emergency medicine specialists, residents, physician assistants, and nurses underwent an emotional debriefing program together. The study showed that although the specialists found it easy to express themselves, the physician assistants and nurses found it uncomfortable.[16]
The EFAT in this study was offered as a single, two-hour session. While changes in participants’ resilience and self-image were measured immediately after the EFAT, there was no long-term follow-up of the outcomes. Although the interval between the pre- and post-EFAT assessments was not long, participants’ resilience scores increased, and their tree drawings (reflecting their self-image) changed; these results indicate that the EFAT had positive outcomes. In Ho et al’s[19] study, which examined an 18-hour art therapy program lasting 6 weeks, the decreases in burnout, resilience, and mental wellbeing were maintained at the 12-week follow-up.
The present study has a few limitations. First, the EFAT was a single session lasting for two hours, and the outcome variables were only measured immediately after the EFAT. Follow-up studies are needed to determine whether a short EFAT has long-term effects. Second, the effects of self-selection bias should be considered, as some participants identified themselves as in need of art therapy. If large-scale EFAT is included in the routine curriculum for residents, self-selection bias can be prevented.
CONCLUSION
The EFAT led to improvements in EPs’ resilience level and self-image. It also helped participants express their emotions and manage their negative emotions. Additionally, as these effects were achieved with a single EFAT session, we believe that medical staff, including residents, can participate in this program without finding it burdensome.
Footnotes
Funding: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1F1A1057947).
Ethics approval: This present study was approved by the Ethics Committee Board of Yonsei University Wonju Severance Christian Hospital.
Conflicts of interest: The authors report no conflicts of interest.
Contributors: conception and design- KHP, EKE; acquisition of data- KHP, SKE; analysis- KHP, SKE; interpretation of data-SKE, CK, KHP; drafting the article- SKE, KHP; revising it critically for important intellectual content/Final approval of the version to be published- all authors.
All the supplementary files in this paper are available at http://wjem.com.cn.
REFERENCES
- 1.Connor KM, Davidson JRT. Development of a new resilience scale:the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 2.Zoorob D, Shah S, La Saevig D, Murphy C, Aouthmany S, Brickman K. Insight into resident burnout, mental wellness, and coping mechanisms early in the COVID-19 pandemic. PLoS One. 2021;16(4):e0250104. doi: 10.1371/journal.pone.0250104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shen X, Li YT, Feng J, Lu ZX, Tian KM, Gan Y. Current status and associated factors of psychological resilience among the Chinese residents during the coronavirus disease 2019 pandemic. Int J Soc Psychiatry. 2022;68(1):34–43. doi: 10.1177/0020764020980779. [DOI] [PubMed] [Google Scholar]
- 4.Nituica C, Bota OA, Blebea J. Specialty differences in resident resilience and burnout - a national survey. Am J Surg. 2021;222(2):319–28. doi: 10.1016/j.amjsurg.2020.12.039. [DOI] [PubMed] [Google Scholar]
- 5.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability:a systematic review. BMJ Open. 2017;7(6):e015141. doi: 10.1136/bmjopen-2016-015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jyothindran R, d'Etienne JP, Marcum K, Tijerina A, Graca C, Knowles H, et al. Fulfillment, burnout and resilience in emergency medicine-Correlations and effects on patient and provider outcomes. PLoS One. 2020;15(10):e0240934. doi: 10.1371/journal.pone.0240934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements (Residency) 2021. [[Accessed August 2021]]. Available at: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2021.pdf .
- 8.Ministry of Health and Welfare (KR) Announcement of Training Curriculum of Medical Residents;2019. [[Accessed March 2022]]. Available at: http://www.mohw.go.kr/upload/viewer/skin/doc.html?fn=1551767423404_20190305153023.hwp&rs=/upload/viewer/result/202203/
- 9.Edmondson EK, Kumar AA, Smith SM. Creating a culture of wellness in residency. Acad Med. 2018;93(7):966–8. doi: 10.1097/ACM.0000000000002250. [DOI] [PubMed] [Google Scholar]
- 10.Shahid R, Stirling J, Adams W. Promoting wellness and stress management in residents through emotional intelligence training. Adv Med Educ Pract. 2018;9:681–6. doi: 10.2147/AMEP.S175299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minichiello V, Hayer S, Gillespie B, Goss M, Barrett B. Developing a mindfulness skills-based training program for resident physicians. Fam Med. 2020;52(1):48–52. doi: 10.22454/FamMed.2020.461348. [DOI] [PubMed] [Google Scholar]
- 12.Ricker M, Brooks AJ, Bodine S, Lebensohn P, Maizes V. Well-being in residency:impact of an online physician well-being course on resiliency and burnout in incoming residents. Fam Med. 2021;53(2):123–8. doi: 10.22454/FamMed.2021.314886. [DOI] [PubMed] [Google Scholar]
- 13.Acevedo JR, Schlacter JA, Chambers TN, Jacobson LK, Yalamanchili R, Clark B, et al. Targeted wellness initiatives are most effective for reducing otolaryngology resident burnout. Ear Nose Throat J. 2021:1455613211009139. doi: 10.1177/01455613211009139. [DOI] [PubMed] [Google Scholar]
- 14.Lebares CC, Coaston TN, Delucchi KL, Guvva EV, Shen WT, Staffaroni AM, et al. Enhanced stress resilience training in surgeons:iterative adaptation and biopsychosocial effects in 2 small randomized trials. Ann Surg. 2021;273(3):424–32. doi: 10.1097/SLA.0000000000004145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hategan A, Riddell T. Bridging the gap:responding to resident burnout and restoring well-being. Perspect Med Educ. 2020;9(2):117–22. doi: 10.1007/s40037-020-00567-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monette DL, Macias-Konstantopoulos WL, Brown DFM, Raja AS, Takayesu JK. A video-based debriefing program to support emergency medicine clinician well-being during the COVID-19 pandemic. West J Emerg Med. 2020;21(6):88–92. doi: 10.5811/westjem.2020.8.48579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Connell A, Siddiqui M, Sielicki A, Naples R, Papanagnou D. A workshop to reflect on personal resilience in emergency medicine residents:applying the Connor-Davidson resilience scale, visual explorer, and the critical incident questionnaire to support introspection. Cureus. 2020;12(6):e8597. doi: 10.7759/cureus.8597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orr AR, Moghbeli N, Swain A, Bassett B, Niepold S, Rizzo A, et al. The fostering resilience through art in medical education (FRAME) workshop:a partnership with the Philadelphia Museum of Art. Adv Med Educ Pract. 2019;10:361–9. doi: 10.2147/AMEP.S194575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ho AHY, Tan-Ho G, Ngo TA, Ong G, Chong PH, Dignadice D, et al. A novel mindful-compassion art-based therapy for reducing burnout and promoting resilience among healthcare workers:findings from a waitlist randomized control trial. Front Psychol. 2021;12:744443. doi: 10.3389/fpsyg.2021.744443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Art Therapy Association. Definition of art therapy. 2017. [[Accessed March 2022]]. Available at: https://www.arttherapy.org/upload/2017_DefinitionofProfession.pdf .
- 21.Greenberg LS. Emotion-focused therapy:coaching clients to work through their feelings. Washington: American Psychological Association; 2002. [Google Scholar]
- 22.Fletcher D, Sarkar M. Psychological resilience. Eur Psychol. 2013;18(1):12–23. [Google Scholar]
- 23.Baek HS, Lee KU, Joo EJ, Lee MY, Choi KS. Reliability and validity of the Korean version of the Connor-Davidson resilience scale. Psychiatry Investig. 2010;7(2):109–15. doi: 10.4306/pi.2010.7.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koch C. The Tree Test;the tree-drawing test as an aid in psychodiagnosis. Grune &Stratton. 1952 [Google Scholar]
- 25.Buck JN. The H-T-P technique;a qualitative and quantitative scoring manual. J Clin Psychol. 1949;5(1):37. doi: 10.1002/1097-4679(194901)5:1<37::aid-jclp2270050104>3.0.co;2-9. passim. [DOI] [PubMed] [Google Scholar]
- 26.Hammer EF. The clinical application of projective drawings. Charles C Thomas. 1958 [Google Scholar]
- 27.Kim C, Park KH, Eo EK, Kim YM, Eo SK, Han J. Burnout and resilience among emergency physicians at Korean university hospitals during the COVID-19 pandemic:a cross-sectional analysis. Yonsei Med J. 2022;63(4):372–9. doi: 10.3349/ymj.2022.63.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ha RY, Kang JI, An SK, Cho HS. Some psychological correlates affecting recognition of neutral facial emotion in young adults. Journal of Korean Neuropsychiatric Association. 2009;48(6):481–7. [Google Scholar]
- 29.Kang JI, Kim SJ, Song YY, Namkoong K, An SK. Genetic influence of COMT and BDNF gene polymorphisms on resilience in healthy college students. Neuropsychobiology. 2013;68(3):174–80. doi: 10.1159/000353257. [DOI] [PubMed] [Google Scholar]
- 30.Judith AR. Approaches to art therapy:theory and technique. Routledge. (3rd edition) 2016 [Google Scholar]
- 31.Braus M, Morton B. Art therapy in the time of COVID-19. Psychol Trauma. 2020;12(1):S267–S268. doi: 10.1037/tra0000746. [DOI] [PubMed] [Google Scholar]
- 32.Ceauşu F. The healing power of art-therapy. Review of Artistic Education. 2018:203–11. [Google Scholar]
- 33.Price ET, Coverley CR, Arrington AK, Nfonsam VN, Morris-Wiseman L, Riall TS. Are we making an impact?A qualitative program assessment of the resident leadership, well-being, and resiliency program for general surgery residents. J Surg Educ. 2020;77(3):508–19. doi: 10.1016/j.jsurg.2019.12.003. [DOI] [PubMed] [Google Scholar]


