Abstract
Esophageal cancer is a familiar malignancy with high incidence and mortality, and the overall prognosis is poor. The numbers of cases of and deaths from esophageal cancer have risen rapidly in recent decades. It is one of the most malignant cancers, with more than 0.6 million new cases and 0.54 million deaths worldwide in 2020. Here, we present the global epidemiology of esophageal cancer in 2020 and projections to 2030 and 2040 at different geographical levels of continents, regions and countries, and analyze them by gender, race, geographic region and human development index. We summarize the prospects for the esophageal cancer burden and risk factors in different areas, which will be useful for global esophageal cancer clinical therapy and cancer control planning.
Keywords: esophageal cancer, incidence, mortality, projection
Esophageal cancer is one of the most malignant cancers, with more than 0.6 million new cases of esophageal cancer and 0.54 million deaths worldwide in 2020. In current review, we present the global epidemiology of esophageal cancer in 2020 and projections to two decades later at different levels of continents, regions and countries and analyze them in gender, race, geographic region, and human development index. Graph abstract showed global and top 3 countries with the highest incident cases of esophageal cancer in 2020 and projections to 2030 and 2040.
INTRODUCTION
Esophageal cancer is the eighth most commonly diagnosed cancer and is the sixth leading cause of cancer death worldwide. 1 , 2 The burden of this malignant tumor is significantly high in less developed regions, where almost 80% of all cases occur. Approximately 70% of cases occur in men, and there is a 2‐ to 5‐fold difference in incidence and mortality rates between the sexes. 2 In addition, esophageal cancer is higher in middle‐aged and elderly populations, and the chance of getting it increases with age. 3 The cancer burden of esophagus incidence and mortality is increasing rapidly worldwide, accompanied by global aging and population growth as well as the prevalence of associated risk factors such as tobacco and alcohol consumption, poor diet, lack of excise, and obesity. 1 , 4 Esophageal cancer is extremely malignant and prognosis is often poor.
In this review, we collect and analyze the cancer burden of esophagus incidence and mortality worldwide from GLOBOCAN 2020, produced by International Agency for Research on Cancer, and the esophageal cancer burden of the United States produced by the American Cancer Society (ACS). More specifically, we describe and compare the geographic variability of esophageal cancer incidence and mortality rate at different levels of countries, regions and continents. Furthermore, we assess associations of the four‐tier Human Development Index (HDI) (low, medium, high, very high, based on the United Nations Development Programme's 2020 Human Development Reports) with the incidence and mortality of esophageal cancer. Subsequently, predictions about the esophageal cancer burden in 2030 and 2040 are given. Follow‐up and understanding of the current and future epidemiology of esophageal cancer will be beneficial for the development of effective and timely prevention or treatment strategies. Finally, we summarize the prospects for the esophageal cancer burden and risk factors in different geographical areas.
PATHOLOGY OF ESOPHAGEAL CANCER
Cancer of the esophagus occur in several forms: squamous cell carcinoma (SCC), adenocarcinoma (AC), sarcomas, small cell carcinomas and rare types such as lymphomas and melanomas. 5 Most esophageal cancers are SCC or AC. 6 , 7 In patients with esophageal cancer, SCC accounts for the overwhelming majority of cases worldwide.
SCC and AC have important distinctions in tumorigenesis 5 , 8 that are based on the type of cell where the cancer originates. SCC starts in the squamous cells of the esophagus mucosa and mainly occurs in the cervical esophagus or upper and middle thoracic esophagus. AC starts in the gland cells, which are mainly found in the lower thoracic esophagus. Barrett's esophagus is a complication of gastroesophageal reflux disease characterized by mucosal dysplasia, may lead to esophageal adenocarcinoma. In addition, adenocarcinomas that occur in the gastroesophageal junction, the area where the esophagus joins the stomach, tend to be classified as esophageal cancer.
EPIDEMIOLOGY OF ESOPHAGEAL CANCER
Esophageal cancer is a type of malignant tumor in digestive system and is one of the leading causes of cancer‐related death, seriously affecting human health worldwide. In 2020, there were an estimated 0.6 million new cases of esophageal cancer and 0.54 million deaths occurred as a result of this disease based on GLOBOCAN 2020. The methods used to estimate the global cancer incidence and mortality in 2020 are based on the most recent data supplied by the population‐based International Agency for Research on Cancer (IARC) cancer registries for Cancer Incidence in Five Continents (CI5) Vol. XI. Esophageal cancer is known for its variation by lifestyle, gender, race, geographic region and HDI.
The predominant histological types of esophageal cancer are SCC and AC, with esophageal SCC being the most common histological type globally. The incidence of these two histologic subtypes differs by geographic region, race, lifestyle, etc.
Incidence
In 2020, the age‐standardized rate of esophageal cancer was 6.3 per 100 000 population. Between 1990 and 2020, the age‐standardized rate of incidence declined by 16.8%, but the global total incidence rose by 94.7%, from 310 236 to 604 100. 2 , 9 There is a significant statistical difference between males and females, with 418 350 cases among males and 185 750 cases among females (Figure 1b). As shown in Figure 1b, approximately 70% of newly diagnosed cases occur in men, and the incidence of esophageal cancer is 2‐ to 3‐fold different between the sexes globally.
FIGURE 1.
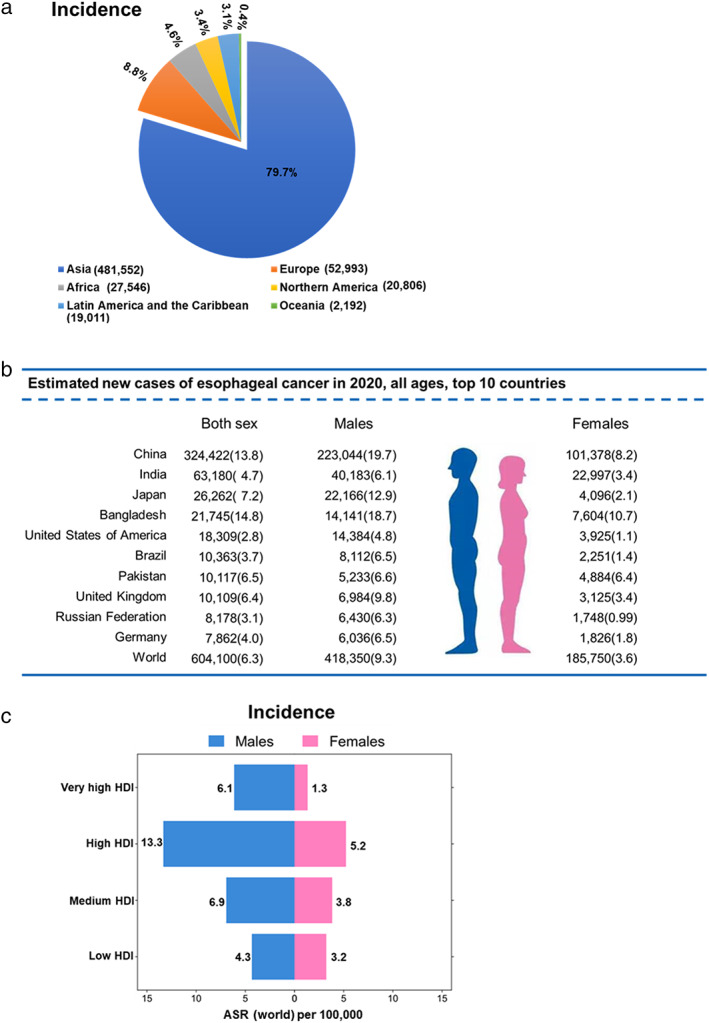
Incidence of esophageal cancer worldwide in 2020. (a) Distribution of new cases of esophageal cancer by continent, both sexes. (b) Top 10 countries for estimated new cases of esophageal cancer, both sexes, all ages. (c) Age‐standardized incidence rate of the four‐tier Human Development Index (HDI) for esophageal cancer worldwide in males and females. ASR, age‐standardized rate. GLOBOCAN 2020
For both sexes combined, in 2020, nearly 79.7% of new cases of esophageal cancer were detected in Asia (481 552 cases), which represents 59.5% of the global population. Europe (52 993 cases) accounted for 8.8%, followed by Africa (27 546 cases) at 4.6%, Northern America (20 806 cases) at 3.4%, Latin America and the Caribbean (19 011 cases) at 3.1%, and Oceania (2192 cases) at 0.4% (Figure 1a). Figure 1b shows the top 10 countries with the highest number of new esophageal cancer cases in 2020. Five of these countries are in Asia: China (324 422 cases, 223 044 cases in males and 101 378 cases in females), India (63 180 cases, 40 183 cases in males and 22 997 cases in females), Japan (26 262 cases, 22 166 cases in males and 4096 cases in females), Bangladesh (21 745 cases, 14 141 cases in males and 7604 cases in females), and Pakistan (10 117 cases, 5233 cases in males and 4884 cases in females). China had the highest incidence, comprising half of the new global cases. The incidence of esophageal cancer in China is almost five times higher than in America. Moreover, according to ACS analysis, the incidence of esophageal cancer in America has remained nearly constant in recent years, slightly increasing in men but decreasing in women over the past few decades.
Specifically, Eastern Asia has the highest regional age‐standardized incidence rates for both males and females, followed by Eastern Africa, Southern Africa, South‐Central Asia, and Northern Europe. In contrast, the lowest age‐standardized incidence rates are observed in Western Asia, Northern Africa, Western Africa, and Central America (Figure 2). Significant differences are shown in age‐standardized incidence rates of esophageal cancer between neighbouring regions, and the highest regional age‐standardized incidence rate was 13.2 times higher than the lowest (12.3 vs. 0.93 per 100 000 population). The highest estimated national‐level age‐standardized incidences in 2020 were observed in countries in Southern Africa (Malawi, Zimbabwe, Mozambique), Eastern Asia (Mongolia, China), and Eastern Africa (Kenya, Uganda, Tanzania) (Table S1). Malawi has the highest age‐standardized incidence (17.5 per 100 000 population), followed by Mongolia (17.1 per 100 000 population). Cabo Verde and Zimbabwe have the highest age‐standardized incidence rates globally in males and females, respectively. Furthermore, the esophageal “cancer belt” is found from northern Iran through Central Asia to Mongolia and north‐central China, where 90% of esophagus cancer cases are mainly SCC. 10 , 11 Meanwhile, AC occurs mainly in western countries, 12 such as America, the United Kingdom, France, Norway, and Australia.
FIGURE 2.
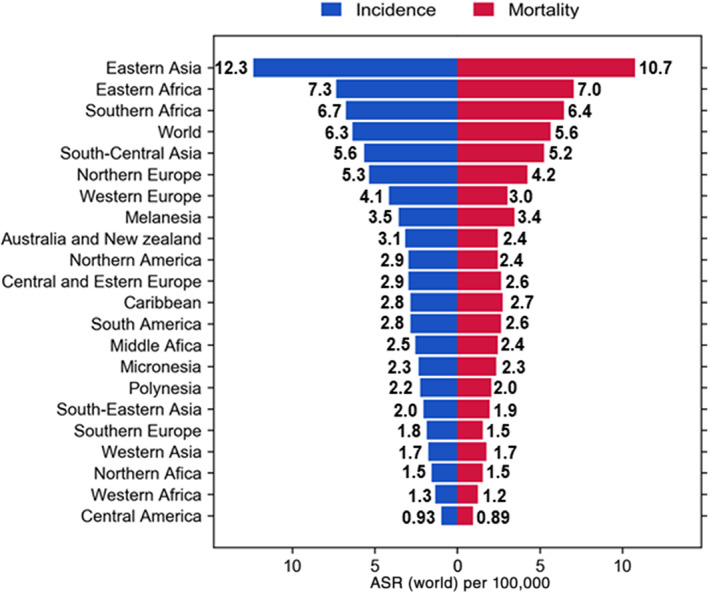
Region‐specific incidence and mortality age‐standardized rates for esophageal cancer worldwide in 2020. Rates are shown in descending order of the age‐standardized rates (ASR) among incidence. GLOBOCAN 2020
A racial difference in incidence is also noted for America (Esophageal cancer burden of the United States produced by the ACS (https://cancerstatisticscenter.cancer.org/). Esophageal cancer is most common in whites and Amerindians, African‐Americans, Alaskan Natives and Hispanics have a lower incident rate, followed by Asians and Pacific Islanders. AC is the predominant esophageal cancer type among whites, while SCC is major type in African‐Americans. In addition, there has been a decrease in the incidence of esophageal SCC and an increase in esophageal AC in recent decades. 13
The HDI, one of the most common measures of development, is a composite index of life expectancy, education, and gross national income. It has been reported that the overall incidence of cancer is positively correlated with HDI. 14 , 15 Figure 1c shows the incidence of esophageal cancer for the four‐tier HDI in 2020. Age‐standardized incidence of esophageal cancer increased with HDI, rising from a low to a high level (low HDI 3.7, medium HDI 5.3, high HDI 9.1 per 100 000), but the very high HDI countries exhibited the lowest incidence rate for both sexes (3.5 per 100 000). Moreover, the incidence ratio of males to females increased with HDI level, ranging from 1.34 to 4.69. The lowest rate in men was observed in low HDI countries, while that in women was found in very high HDI countries.
Mortality
In 2020, esophageal cancer was the sixth leading cause of cancer‐related death worldwide, with an estimated 0.54 million deaths. The age‐standardized rate of mortality was 5.6 deaths per 100 000 people (Figure 3b). Between 1990 and 2020, global age‐standardized mortality decreased by 27.5%, but the number increased by 74.8%, from 311 289 to 544 076. 2 , 9
FIGURE 3.
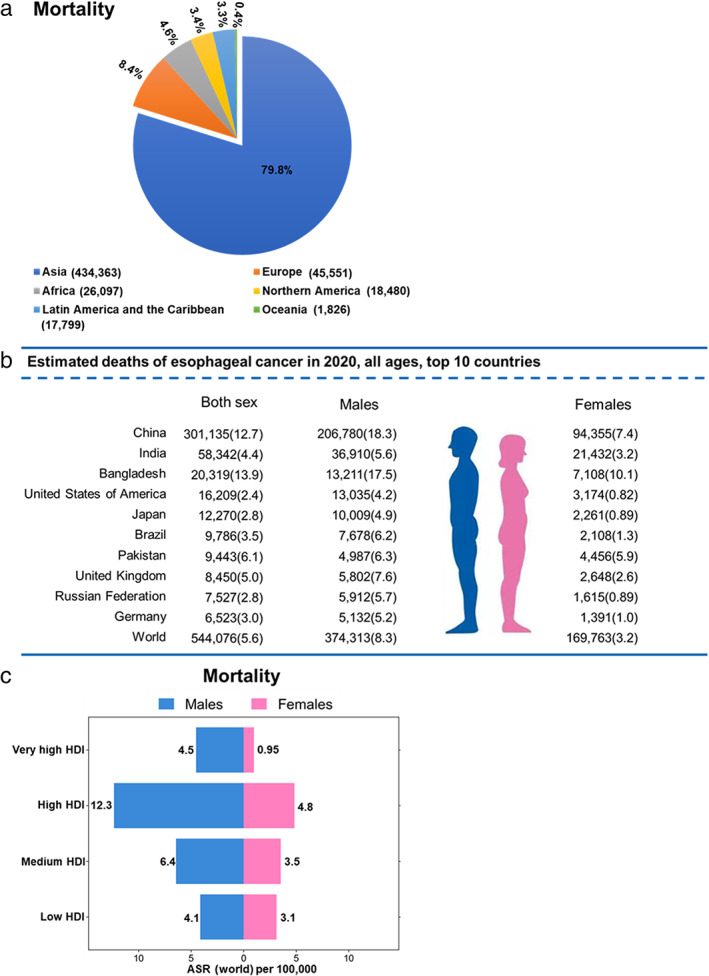
Mortality of esophageal cancer worldwide in 2020. (a) Distribution of deaths for esophageal cancer by continent, both sexes. (b) Top 10 countries for estimated deaths of esophageal cancer, both sexes, all ages. (c) Age‐standardized mortality rate of the four‐tier Human Development Index (HDI) for esophageal cancer worldwide in males and females. GLOBOCAN 2020
Esophageal cancer is a refractory disease that starts in the inner of the esophagus wall and grows outward through the other layers, such as mucosa, submucosa, muscularis propria and adventitia, therefore early esophageal carcinomas usually do not have obvious symptoms, leading to detection at a late stage and very poor prognosis. 16 , 17 , 18 Moreover, nearly half of patients develop distant metastasis within 5 years. 19 Because of its high malignancy and poor prognosis, esophageal cancer also has high mortality accompanied by high incidence. As show in Figure 3a, the distribution of esophageal cancer mortality in six continents is similar to that of its incidence. The 10 countries with the highest incidence are also the 10 countries with the most deaths (Figure 3b). Regions with high age‐standardized incidence rates also have the highest age‐standardized mortality, although there is a slight change in ranking (Figure 2). China has the largest number of deaths from esophageal cancer, more than half of the total deaths worldwide (Figure 3b), and Malawi (16.7 per 100 000) and Mongolia (16.2 per 100 000) have the highest mortality rate globally. Cabo Verde has the highest age‐standardized mortality rate in the world for men, and the highest mortality rate for women is observed in Malawi (Table S2).
There is also some correlation between esophageal cancer mortality and HDI. The mortality rate of esophageal cancer per HDI group (very high, high, medium, low) in 2020 is shown in Figure 3c. The death rates in low, medium, high and very high HDI countries are 3.6, 4.9, 8.3, and 2.6 per 100 000 population, respectively. Furthermore, the age‐standardized mortality rate for males and females also increases with HDI level, ranging from 1.32 to 4.74.
Future burden of esophageal cancer in 2030 and 2040
The prevalence of esophageal cancer has grown dramatically worldwide in recent years. If current trends continue, as shown in Figure 4. Based on GLOBOCAN 2020, the estimated numbers of esophageal cancer cases and deaths in 2030 and 2040 are calculated by multiplying the rates in 2020 by the expected population in 2030 and 2040. It is projected that 739 666 new cases of and 723 466 deaths from esophageal cancer will occur in 2030, and there will be 987 723 new cases and 914 304 deaths in 2040 around the world, with a 31.4% and 33.0%, 63.5% and 68.0% more than in 2020, respectively. The highest change in the number of new cases is projected to occur in Africa, rising from 27 546 in 2020 to 38 656 (increase of 40.3%) in 2030 and 54 279 (increase of 97.9%) in 2040. The lowest change is Europe, rising from 52 993 in 2020 to 59 626 (increase of 12.5%) in 2030 and 64 720 (increase of 22.1%) in 2040. In addition, the largest number of new cases will still occur in Asia, rising from 481 552 in 2020 to 642 148 (increase of 33.3%) in 2030 and 803 911 (increase of 66.9%) in 2040 (Figure 4a). The projected esophageal cancer deaths in 2030 and 2040 in six continents is similar to the new cases (Figure 4b).
FIGURE 4.
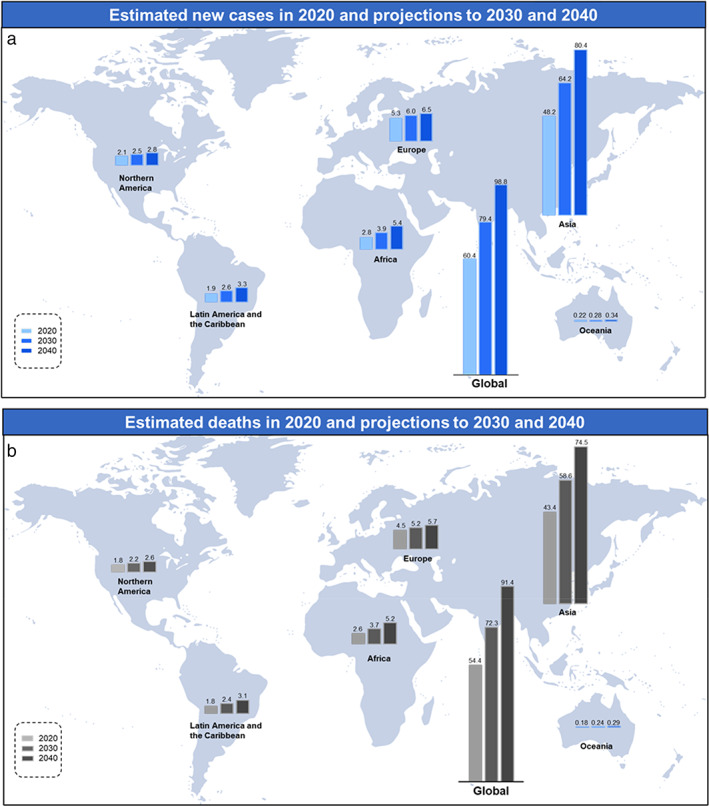
Estimated new cases (a) and deaths (b) of esophageal cancer worldwide in 2020 and projections to 2030 and 2040. GLOBOCAN 2020
The burden of esophageal cancer increases substantially at all HDI levels (Table S3). The striking magnitude of the increase can be seen in low HDI countries. High HDI countries would experience the greatest new cases and deaths in 2030 and 2040.
At the country level, estimates of esophageal cancer cases and deaths in the top three most populous countries, China, India, and the United States, in 2030 and 2040 are shown in Figure 5. The number of new cases in China is predicted to increase from 324 422 in 2020 to 435 958 in 2030 and to 529 621 in 2040. The number of deaths in China is predicted to increase from 301 135 in 2020 to 416 509 in 2030 and to 525 362 in 2040. In India, the number of new cases is projected to grow from 63 180 in 2020 to 83 332 in 2030 and to 105 640 in 2040, while the number of deaths is projected to grow from 58 342 in 2020 to 76 731 in 2030 and to 97 179 in 2040. The number of new cases in the United States is predicted to increase from 18 309 in 2020 to a projected 21 755 in 2030 and 24 590 in 2040. The number of deaths in the United States is predicted to increase from 16 209 in 2020 to a projected 19 611 in 2030 and 22 593 in 2040.
FIGURE 5.
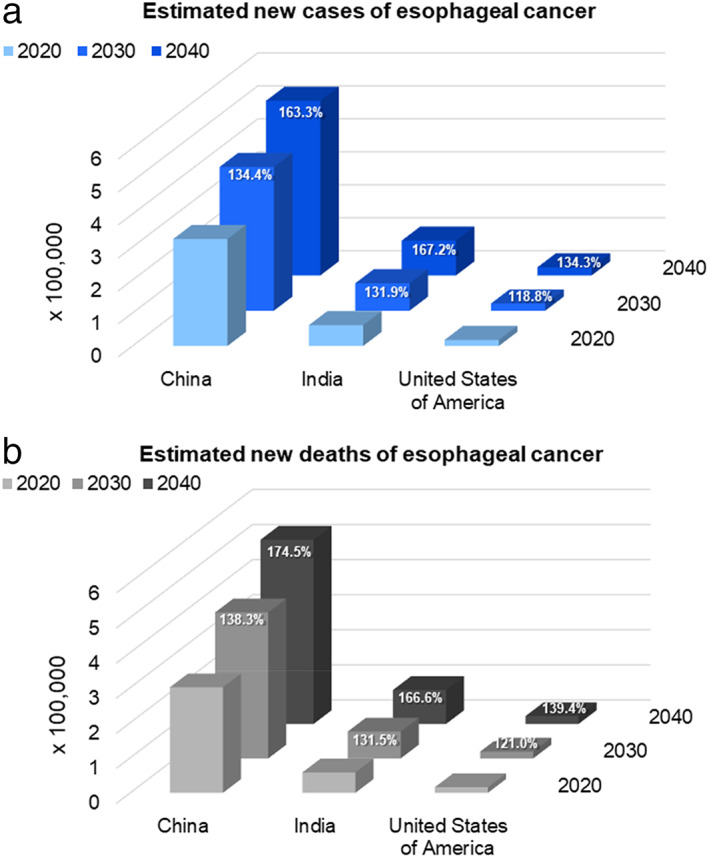
Estimated new cases (a) and deaths (b) of esophageal cancer in China, India, and the United States in 2020 and projections to 2030 and 2040. GLOBOCAN 2020
With increasing level and aging of the world population, as well as the prevalence of associated risk factors such as tobacco and alcohol assumption, poor diet, lack of exercise and obesity, it is very likely the predicted estimates for esophageal cancer will be reached in 2030 and 2040.
CONCLUSIONS
As one of the most common malignancies, esophageal cancer has become an urgent global health challenge and the growing trend of esophageal cancer cases is expected to continue for the next two decades and beyond. Based on GLOBOCAN 2020 analysis from 1990 to 2020, there was a decrease in the global age‐standardized rates of incidence and mortality, but an increase in new cases of and deaths from esophageal cancer. The incidence and mortality of esophageal cancer indicate variations for gender, race, and geographic region. Furthermore, there was a positive relationship between the incidence of esophageal cancer and mortality and HDI level. The age‐standardized incidence and mortality of esophageal cancer increase with HDI, rising from low level to high level, and are lowest in countries with very high HDI.
A high male predominance is found for esophageal cancer, with risk 2‐ to 3‐fold higher for men than for women worldwide in 2020. Cabo Verde has the highest age‐standardized incidence and mortality rates in males. In females, Zimbabwe has the highest age‐standardized incidence rate, and the highest mortality rate is observed in Malawi. The causes for this gender difference in esophageal cancer are still unclear. Different exposure to high‐risk factors such as alcohol and tobacco, 20 , 21 hormonal influences, 22 , 23 and abdominal obesity, particularly in men, 24 probably led to this male predominance.
In terms of geographical distribution, Eastern Asia has the highest regional standardized incidence and mortality, followed by Eastern Africa, Southern Africa, and South‐Central Asia. Approximately 80% of new cases and deaths take place in Asia. China has the heaviest burden of esophageal cancer, accounting for more than half of the world. Esophageal SCC is the predominant histological type in high‐risk regions of esophageal cancer. In most African countries, tobacco and alcohol consumption are the two main risk factors for esophageal cancer. 3 , 25 , 26 , 27 In addition, firewood cooking and the use of white maize flour had strong associations with SCC in Malawi. 28 In the Asian esophageal “cancer belt”, drinking hot liquids, high‐temperature cooking, poor oral hygiene, and low socio‐economic status were reported to increase the risk of SCC. 29 , 30 Smoking and heavy alcohol intake are the two main risk factors for SCC in western counties. 31 In addition, betel quid chewing is a suspected risk factor for SCC, 32 and risk for esophageal SCC increases by more than 41‐fold versus alcohol and tobacco in Taiwan Region. 33 Most esophageal cancers are SCC or AC, but these two types of cancer have very distinct risk factors and geographic distribution. The highest risk factor for AC is gastro‐esophageal efflux, especially Barrett's esophagus, 34 along with obesity 35 and decreased Helicobacter pylori. 36 AC occurs mainly in western countries, such as the United States, the United Kingdom, France, Norway and Australia, and probably represents two‐third of cases in high‐income countries. 37 Furthermore, the incidence of AC is rising due to the increase in the risk factors of obesity (especially waist circumference) and gastroesophageal efflux. 13 , 38 Special attention should be paid to the link between the prevalence of overweight individuals and increasing obesity and the incidence of AC in most countries, as this is likely to contribute greatly to the future burden of esophageal cancer.
Finally, with the increase in aging of the world population, and the prevalence of associated risk factors, it is strongly expected that the real incidence of esophageal cancer would reach the predicted one in 2030 and 2040. In recent years, the incidence of SCC, accounting for approximately 90% of all esophageal cancer cases worldwide, has decreased in most countries, probably because of dietary improvements, and less smoking and heavy drinking, etc., 39 , 40 but new cases of SCC are rising with the growth in and aging of the world population. Moreover, a rapid increase in the incidence of AC is occurring in high‐income countries, 13 and it is predicted that AC incidence will surpass that of SCC in the near future. Further actions are necessary to address this phenomenon to prevent an increase in new cases of SCC and AC. Furthermore, as AC and SCC have distinct outcomes, treatment strategies, and response profiles to therapy, 41 , 42 there is a need for different management strategies for them. Although the overall prognosis of patients with esophageal cancer is gradually improving due to surgical improvements, medical advances, and neoadjuvant therapy, overall survival is still poor. 43 , 44 , 45 , 46 A third to half of cancers are preventable 47 and earlier diagnosis, for example through endoscopic screening, has provided better outcomes by identifying the cancer at an early stage. In a community‐based study in rural China, considerable reductions in esophageal SCC incidence (−43%) and mortality (−45%) were observed after one‐time endoscopic screening followed by normative treatment for precancerous lesions among individuals aged 40–69 years. 48 Strategies for the prevention of esophageal cancer and methods for early detection are therefore urgently needed, and these require worldwide attention and effort from policymakers, researchers, and clinicians.
AUTHOR CONTRIBUTIONS
Chun‐Quan Liu and Yun‐Lei Ma contributed equally to this paper and should be considered as co‐first authors. Yong Cui, Peng‐Fei Xu, and Chun‐Quan Liu designed the manuscript, and Peng‐Fei Xu, Chun‐Quan Liu, and Yun‐Lei Ma collected relevant data. All authors contributed to manuscript writing, and read and approved the final manuscript.
CONFLICT OF INTEREST
There are no conflict of interest for this article.
Supporting information
TABLE S1. Supporting information
ACKNOWLEDGMENTS
Capital's Funds for Health Improvement and Research (No. 2022–2‐2024). Wu Jieping Medical Foundation for Clinical Research (No. 320.6750.2022‐16‐16).
Liu C‐Q, Ma Y‐L, Qin Q, Wang P‐H, Luo Y, Xu P‐F, et al. Epidemiology of esophageal cancer in 2020 and projections to 2030 and 2040. Thorac Cancer. 2023;14(1):3–11. 10.1111/1759-7714.14745
Funding information Capital Health Research and Development of Special Fund, Grant/Award Number: 2022‐2‐2024; Wu Jieping Medical Foundation, Grant/Award Number: 320.6750.2022‐16‐16
Contributor Information
Peng‐Fei Xu, Email: pex9@pitt.edu, Email: dyxufei@sina.com, Email: dyxufei@sina.com.
Yong Cui, Email: cywork1@sina.com.
REFERENCES
- 1. Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal cancer. Lancet. 2017;390(10110):2383–96. 10.1016/S0140-6736(17)31462-9 [DOI] [PubMed] [Google Scholar]
- 2. Collaborators GBDOC . The global, regional, and national burden of oesophageal cancer and its attributable risk factors in 195 countries and territories, 1990‐2017: a systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol. 2020;5(6):582–97. 10.1016/S2468-1253(20)30007-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Asombang AW, Chishinga N, Nkhoma A, Chipaila J, Nsokolo B, Manda‐Mapalo M, et al. Systematic review and meta‐analysis of esophageal cancer in Africa: epidemiology, risk factors, management and outcomes. World J Gastroenterol. 2019;25(31):4512–33. 10.3748/wjg.v25.i31.4512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–21. 10.1007/s12328-020-01237-x [DOI] [PubMed] [Google Scholar]
- 5. Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19(34):5598–606. 10.3748/wjg.v19.i34.5598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015;64(3):381–7. 10.1136/gutjnl-2014-308124 [DOI] [PubMed] [Google Scholar]
- 7. Rogers JE, Sewastjanow‐Silva M, Waters RE, Ajani JA. Esophageal cancer: emerging therapeutics. Expert Opin Ther Targets. 2022;26(2):107–17. 10.1080/14728222.2022.2036718 [DOI] [PubMed] [Google Scholar]
- 8. Sanchez‐Danes A, Blanpain C. Deciphering the cells of origin of squamous cell carcinomas. Nat Rev Cancer. 2018;18(9):549–61. 10.1038/s41568-018-0024-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yang S, Lin S, Li N, Deng Y, Wang M, Xiang D, et al. Burden, trends, and risk factors of esophageal cancer in China from 1990 to 2017: an up‐to‐date overview and comparison with those in Japan and South Korea. J Hematol Oncol. 2020;13(1):146. 10.1186/s13045-020-00981-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet‐Tieulent J, Jemal A. Global cancer statistics, 2012. Ca‐Cancer J Clin. 2015;65(2):87–108. 10.3322/caac.21262 [DOI] [PubMed] [Google Scholar]
- 11. Abnet CC, Arnold M, Wei WQ. Epidemiology of esophageal squamous cell carcinoma. Gastroenterology. 2018;154(2):360–73. 10.1053/j.gastro.2017.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Caspa Gokulan R, Garcia‐Buitrago MT, Zaika AI. From genetics to signaling pathways: molecular pathogenesis of esophageal adenocarcinoma. Biochim Biophys Acta Rev Cancer. 2019;1872(1):37–48. 10.1016/j.bbcan.2019.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Arnold M, Laversanne M, Brown LM, Devesa SS, Bray F. Predicting the future burden of esophageal cancer by histological subtype: international trends in incidence up to 2030. Am J Gastroenterol. 2017;112(8):1247–55. 10.1038/ajg.2017.155 [DOI] [PubMed] [Google Scholar]
- 14. Fidler MM, Soerjomataram I, Bray F. A global view on cancer incidence and national levels of the human development index. Int J Cancer. 2016;139(11):2436–46. 10.1002/ijc.30382 [DOI] [PubMed] [Google Scholar]
- 15. Wong MCS, Hamilton W, Whiteman DC, Jiang JY, Qiao Y, Fung FDH, et al. Global incidence and mortality of oesophageal cancer and their correlation with socioeconomic indicators temporal patterns and trends in 41 countries. Sci Rep. 2018;8(1):4522. 10.1038/s41598-018-19819-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Veugelers PJ, Porter GA, Guernsey DL, Casson AG. Obesity and lifestyle risk factors for gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma. Dis Esophagus. 2006;19(5):321–8. 10.1111/j.1442-2050.2006.00602.x [DOI] [PubMed] [Google Scholar]
- 17. Ilson DH, van Hillegersberg R. Management of patients with adenocarcinoma or squamous cancer of the esophagus. Gastroenterology. 2018;154(2):437–51. 10.1053/j.gastro.2017.09.048 [DOI] [PubMed] [Google Scholar]
- 18. Njei B, McCarty TR, Birk JW. Trends in esophageal cancer survival in United States adults from 1973 to 2009: a SEER database analysis. J Gastroenterol Hepatol. 2016;31(6):1141–6. 10.1111/jgh.13289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hoeppner J, Kulemann B. Circulating tumor cells in esophageal cancer. Oncol Res Treat. 2017;40(7–8):417–22. 10.1159/000478863 [DOI] [PubMed] [Google Scholar]
- 20. Huang F‐L, Yu S‐J. Esophageal cancer: risk factors, genetic association, and treatment. Asian J Surg. 2018;41(3):210–5. 10.1016/j.asjsur.2016.10.005 [DOI] [PubMed] [Google Scholar]
- 21. Choi YJ, Lee DH, Han KD, Kim HS, Yoon H, Shin CM, et al. The relationship between drinking alcohol and esophageal, gastric or colorectal cancer: a nationwide population‐based cohort study of South Korea. PLoS One. 2017;12(10):e0185778. 10.1371/journal.pone.0185778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang QM, Qi YJ, Jiang Q, Ma YF, Wang LD. Relevance of serum estradiol and estrogen receptor beta expression from a high‐incidence area for esophageal squamous cell carcinoma in China. Med Oncol. 2011;28(1):188–93. 10.1007/s12032-010-9457-8 [DOI] [PubMed] [Google Scholar]
- 23. Xie SH, Ness‐Jensen E, Langseth H, Gislefoss RE, Mattsson F, Lagergren J. Prediagnostic circulating levels of sex hormones and survival in esophageal adenocarcinoma. Int J Cancer. 2021;148(4):905–13. 10.1002/ijc.33285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chen Q, Zhuang H, Liu Y. The association between obesity factor and esophageal caner. J Gastrointest Oncol. 2012;3(3):226–31. 10.3978/j.issn.2078-6891.2012.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sewram V, Sitas F, O'Connell D, Myers J. Tobacco and alcohol as risk factors for oesophageal cancer in a high incidence area in South Africa. Cancer Epidemiol. 2016;41:113–21. 10.1016/j.canep.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 26. Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27(1):2–12. 10.3978/j.issn.1000-9604.2015.01.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kitagawa Y, Uno T, Oyama T, Kato K, Kato H, Kawakubo H, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 1. Esophagus. 2019;16(1):1–24. 10.1007/s10388-018-0641-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mlombe YB, Rosenberg NE, Wolf LL, Dzamalala CP, Chalulu K, Chisi J, et al. Environmental risk factors for oesophageal cancer in Malawi: a case‐control study. Malawi Med J. 2015;27(3):88–92. 10.4314/mmj.v27i3.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tran GD, Sun XD, Abnet CC, Fan JH, Dawsey SM, Dong ZW, et al. Prospective study of risk factors for esophageal and gastric cancers in the Linxian general population trial cohort in China. Int J Cancer. 2005;113(3):456–63. 10.1002/ijc.20616 [DOI] [PubMed] [Google Scholar]
- 30. Dar NA, Islami F, Bhat GA, Shah IA, Makhdoomi MA, Iqbal B, et al. Poor oral hygiene and risk of esophageal squamous cell carcinoma in Kashmir. Br J Cancer. 2013;109(5):1367–72. 10.1038/bjc.2013.437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pandeya N, Olsen CM, Whiteman DC. Sex differences in the proportion of esophageal squamous cell carcinoma cases attributable to tobacco smoking and alcohol consumption. Cancer Epidemiol. 2013;37(5):579–84. 10.1016/j.canep.2013.05.011 [DOI] [PubMed] [Google Scholar]
- 32. Das M, Saikia BJ, Sharma SK, Sekhon GS, Mahanta J, Phukan RK. p16 hypermethylation: a biomarker for increased esophageal cancer susceptibility in high incidence region of North East India. Tumour Biol. 2015;36(3):1627–42. 10.1007/s13277-014-2762-7 [DOI] [PubMed] [Google Scholar]
- 33. Lee CH, Lee JM, Wu DC, Hsu HK, Kao EL, Huang HL, et al. Independent and combined effects of alcohol intake, tobacco smoking and betel quid chewing on the risk of esophageal cancer in Taiwan. Int J Cancer. 2005;113(3):475–82. 10.1002/ijc.20619 [DOI] [PubMed] [Google Scholar]
- 34. Hvid‐Jensen F, Pedersen L, Drewes AM, Sorensen HT, Funch‐Jensen P. Incidence of adenocarcinoma among patients with Barrett's esophagus. N Engl J Med. 2011;365(15):1375–83. 10.1056/NEJMoa1103042 [DOI] [PubMed] [Google Scholar]
- 35. Arnold M, Pandeya N, Byrnes G, Renehan PAG, Stevens GA, Ezzati PM, et al. Global burden of cancer attributable to high body‐mass index in 2012: a population‐based study. Lancet Oncol. 2015;16(1):36–46. 10.1016/S1470-2045(14)71123-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gao H, Li L, Zhang C, Tu J, Geng X, Wang J, et al. Systematic review with meta‐analysis: association of Helicobacter pylori infection with esophageal cancer. Gastroenterol Res Pract. 2019;2019:1953497. 10.1155/2019/1953497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Blot WJ. Esophageal cancer. In: Thun M, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D, editors. Cancer Epidemiology and Prevention. 4th ed. Oxford University Press; 2018. p. 579–93. 10.1093/ije/dyy166 [DOI] [Google Scholar]
- 38. Fukuchi T, Hirasawa K, Sato C, Makazu M, Kaneko H, Kobayashi R, et al. Potential roles of gastroesophageal reflux in patients with superficial esophageal squamous cell carcinoma without major causative risk factors. J Gastroenterol. 2021;56(10):891–902. 10.1007/s00535-021-01815-x [DOI] [PubMed] [Google Scholar]
- 39. Giri S, Pathak R, Aryal MR, Karmacharya P, Bhatt VR, Martin MG. Incidence trend of esophageal squamous cell carcinoma: an analysis of surveillance epidemiology, and end results (SEER) database. Cancer Causes Control. 2015;26(1):159–61. 10.1007/s10552-014-0485-0 [DOI] [PubMed] [Google Scholar]
- 40. Brown LM, Devesa SS, Chow WH. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst. 2008;100(16):1184–7. 10.1093/jnci/djn211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gamboa AC, Meyer BI, Switchenko JM, Rupji M, Lee RM, Turgeon MK, et al. Should adenosquamous esophageal cancer be treated like adenocarcinoma or squamous cell carcinoma? J Surg Oncol. 2020;122(3):412–21. 10.1002/jso.25990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bollschweiler E, Metzger R, Drebber U, Baldus S, Vallbohmer D, Kocher M, et al. Histological type of esophageal cancer might affect response to neo‐adjuvant radiochemotherapy and subsequent prognosis. Ann Oncol. 2009;20(2):231–8. 10.1093/annonc/mdn622 [DOI] [PubMed] [Google Scholar]
- 43. Vendrely V, Launay V, Najah H, Smith D, Collet D, Gronnier C. Prognostic factors in esophageal cancer treated with curative intent. Dig Liver Dis. 2018;50(10):991–6. 10.1016/j.dld.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 44. Ando N, Kato H, Igaki H, Shinoda M, Ozawa S, Shimizu H, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5‐fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19(1):68–74. 10.1245/s10434-011-2049-9 [DOI] [PubMed] [Google Scholar]
- 45. Yamagata Y, Saito K, Hirano K, Oya M. Long‐term outcomes and safety of radical transmediastinal esophagectomy with preoperative docetaxel, cisplatin, and 5‐fluorouracil combination chemotherapy for locally advanced squamous cell carcinoma of the thoracic esophagus. World J Surg Oncol. 2020;18(1):252. 10.1186/s12957-020-02023-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fujiwara Y, Fukuda S, Tsujie M, Kitani K, Yukawa M, Inoue M, et al. Clinical significance of preoperative chemoradiotherapy for advanced esophageal cancer, evaluated by propensity score matching and weighting of inverse probability of treatment. Mol . Clin Oncol. 2019;10(6):575–82. 10.3892/mco.2019.1843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vineis P, Wild CP. Global cancer patterns: causes and prevention. Lancet. 2014;383(9916):549–57. 10.1016/S0140-6736(13)62224-2 [DOI] [PubMed] [Google Scholar]
- 48. Zhang N, Li Y, Chang X, Lei F, Ma H, Liu J, et al. Long‐term effectiveness of one‐time endoscopic screening for esophageal cancer: a community‐based study in rural China. Cancer. 2020;126(20):4511–20. 10.1002/cncr.33119 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TABLE S1. Supporting information


