Abstract
Background
The risk of sustaining a graft rupture after anterior cruciate ligament reconstruction (ACLR) is high. Contributing risk factors are, however, still not clearly identified.
Objective
The aim of this systematic review was to identify and quantify risk factors for graft rupture after ACLR.
Methods
A systematic review with meta-analysis (PROSPERO CRD42020140129) based on PRISMA guidelines was performed. MEDLINE, CINAHL and EMBASE were searched from inception to September 2021. Prospective and retrospective studies addressing risk factors for graft rupture after ACLR in males/females of all ages were considered. Meta-analyses using a random effect model (effect measure: odds ratio [OR] with 95% confidence interval [CI]) were performed. The GRADE tool was used to assess evidence quality.
Results
Following full-text screening of 310 relevant papers, 117 were eventually included, incorporating up to 133,000 individuals in each meta-analysis. Higher Tegner activity level (≥ 7 vs < 7) at primary injury (OR 3.91, 95% CI 1.69–9.04), increased tibial slope (degrees) (OR 2.21, 95% CI 1.26–3.86), lower psychological readiness to return to sport (RTS) (OR 2.18, 95% CI 1.32–3.61), early surgery (< 12 vs ≥ 12 months) (OR 1.87, 95% CI 1.58–2.22), RTS (pre-injury level) (OR 1.87, 95% CI 1.21–2.91) and family history of ACL injury (OR 1.76, 95% CI 1.34–2.31) were all associated with increased odds of graft rupture. Higher age (OR 0.47, 95% CI 0.39–0.59), female sex (OR 0.88, 95% CI 0.79–0.98), fewer self-reported knee symptoms pre-reconstruction (OR 0.81, 95% CI 0.69–0.95) and concomitant cartilage injuries (OR 0.70, 95% CI 0.62–0.79) instead decreased the odds. Meta-analysis revealed no association between body mass index, smoking, joint laxity, RTS time, knee kinematics, muscle strength or hop performance and graft rupture.
Conclusion
Conspicuous risk factors for graft rupture were mainly sports and hereditary related. Few studies investigated function-related modifiable factors or included sports exposure data.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40279-022-01747-3.
Key Points
| This systematic review with meta-analysis provides evidence that high activity level, young age, lower psychological readiness, and increased tibial slope are risk factors for graft ruptures following anterior cruciate ligament reconstruction. |
| Females seem to have lower risk of sustaining a graft rupture compared with males. |
| Having been little explored, future studies should focus on neuromuscular function and psychological aspects as potential risk factors, since these may be modifiable by training or other interventions. |
Background
Injury to the anterior cruciate ligament (ACL) is common among athletes [1, 2] and often leads to functional impairments, failure to return to sport (RTS) and terminated athletic careers [3, 4]. Surgical reconstruction of the ACL (ACLR) is an increasingly common treatment after injury with an increase in incidence in the US from 40.9 per 10,000 patients in 2004 to 47.8 in 2009 [5]. However, the risk of sustaining a graft rupture after ACLR remains high. Wiggins et al., reported in a systematic review and meta-analysis that approximately 10% of the individuals aged < 25 years who returned to their pre-injury activity level after primary ACLR suffered a secondary ACL injury to their ipsi-lateral knee [6]. A subsequent graft rupture may lead to further substantial decline in function and in quality of life, as well as to increased risk of early onset of knee osteoarthritis [7–10]. Still, risk factors associated with graft rupture remain largely unknown.
Prominent risk factors for primary ACL injury are female sex, increased joint laxity as well as aberrant neuromuscular and biomechanical movement patterns, such as deficits in neuromuscular control of the trunk and lower extremity and higher ground reaction forces during landing [11]. Further, as we reported in a recent systematic review, RTS is the risk factor with the strongest association with sustaining a secondary injury to the ACL of the contralateral leg (C-ACL). Notably, athletes who returned to a high activity level (International Knee Documentation Committee [IKDC] questionnaire, level 1–2) or sports including cutting and pivoting were more likely to sustain a C-ACL injury than those who did not return at all or returned to a lower activity level (odds ratio [OR] 3.3) [12]. Other risk factors for future C-ACL injuries included female sex, age 18 years or younger, family history of ACL injury, and early (≤ 3 months) primary ACL reconstruction. However, it is not known if and if so, to what extent, the factors that contribute to graft ruptures overlap with the risk factors for primary and C-ACL injury. Even when passing certain criteria for sensorimotor function following rehabilitation, there may still be an increased risk of C-ACL injury, while the risk for graft rupture is reduced [13]. Also, while females are reported to have a higher risk of primary and C-ACL injury compared with men [11, 12], they seem to have lower risk of graft rupture [14]. It is important to further disentangle specific risk factors for graft rupture after primary ACL injury in order to identify high-risk individuals. Such knowledge will further facilitate the design of training and rehabilitation protocols aiming at risk reduction for secondary injuries following ACL rupture. Previous narrative [15] and systematic reviews [6, 14, 16–18] on risk factors for graft rupture focus either on specific risk factors, such as sex [14, 17], or only include specific subgroups of studies, such as younger participants [16] or registry studies [18]. To our knowledge, there are no previous studies synthesizing all risk factors for graft rupture without population restrictions. Hence, the aim of this systematic review was to identify and quantify risk factors related to demographics/characteristics, injury, timing of surgery, activity, biomechanics, joint geometry/skeletal maturity, function and patient-reported outcomes that are associated with sustaining a future graft rupture.
Methods
Literature Search and Study Selection
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19, 20] and was pre-registered (PROSPERO: CRD42020140129).
Search Strategy
A systematic search was performed from inception to January 2020 (updated in September 2021) in the following databases: MEDLINE (PubMed), CINAHL and EMBASE with search terms incorporating different aspects of secondary ACL injuries and associated risk factors, previously published in full [12] (Online resource 1, see electronic supplementary material [ESM]). Reference lists of all relevant articles were subsequently manually searched for additional studies.
Eligibility Criteria
All studies meeting the following criteria were considered for inclusion: (1) prospective or retrospective studies with any follow-up duration; (2) inclusion of males and/or females of any age with primary ACLR (any graft/surgery technique); (3) assessment of any factor related to demographics/characteristics, injury, timing of surgery, activity/sport, biomechanics, joint geometry/skeletal maturity, function and patient-reported outcomes at baseline; and (4) recording of at least three graft ruptures, defined as clinically verified, MRI verified or self-reported graft rupture or as revision surgery during the study period. Exclusion criteria were (1) animal studies and in vitro studies; (2) case studies, conference abstracts, review papers and editorials; (3) external risk factors, such as weather, equipment, playing surface or possible risk factors related to type of graft and/or surgery technique; and (4) published in a language other than English or a Scandinavian language.
Data Extraction and Synthesis
All abstracts and full texts were independently screened according to the inclusion/exclusion criteria by two of the authors of this review (AC and ET) using the Covidence software (Veritas Health Innovation). Any disagreements were resolved by a consensus discussion between AC and ET, and if required with the third author (CH). The following data were extracted from the studies: authors, publication date, country, number of participants, sex, age, activity level, number of graft ruptures, time to graft rupture, graft type, follow-up period (years), assessed risk factor/s and effect measure/s. If there were not sufficient data to perform meta-analysis reported in a study, study authors were contacted with a request for additional information if the study was published within the last 10 years. A meta-analysis was performed if there were two or more studies that included the same risk factor for sustaining a graft rupture.
Comprehensive Meta-Analysis software, version 2.2.064 (Englewood, USA) was used for meta-analysis. The odds ratio (95% CI) for each risk factor for sustaining a graft rupture was chosen as the effect measure. The odds ratio was primarily calculated from the number of events and sample size in each group or from mean (SD) as appropriate. If not reported, the reported unadjusted univariable odds ratio was used if available. A random effect model was used because of expected heterogeneity between studies, regarding sex, age, graft types, physical activity level and time duration of follow-up. All meta-analyses and corresponding forest plots were weighted under the random effect model, taking both within-study variance and between-study variance (Tau2) into account [21]. The Q test and corresponding I2-statistics were used to calculate the between-study effect measure heterogeneity [22]. A 95% confidence interval excluding the null value of 1 was considered a statistically significant result. For studies reporting associated meniscal injuries/surgeries as risk factors for graft rupture, the results for any meniscal injury/surgery (medial or lateral injury) were included in the meta-analysis. If medial and lateral injury/surgery was reported separately, the result for the lateral side was included since the lateral meniscus is most frequently injured in conjunction with acute ACL injury [23]. In studies reporting data from more than one measuring technique for assessing tibial slope (i.e., anterior, posterior, central slope) in the same participants, the number of participants included in the primary analysis was divided by the number of measuring techniques reported, and each measuring technique was then treated as an independent study [24]. All the cut-off values applied for all the variables in this review (e.g., age ≥ 18 vs < 18 years) were based on those reported in the individual studies.
Subgroup analysis for children/adolescents (C&A) (aged ≤ 19 years) and adults (aged > 19 years) were performed if two or more studies investigated the same risk factor for graft rupture.
Risk of Bias, Publication Bias and Quality of Evidence Assessments
Two of the authors (AC and ET) independently assessed all included studies for risk of bias using the Quality In Prognosis Studies (QUIPS) tool [25, 26] (Online resource 2, see ESM). If consensus was not reached, further discussions with the third author (CH) were conducted to resolve any disagreements. If the meta-analysis included at least 10 studies and the corresponding I2 was ≤ 50%, funnel plots with trim and fill were used to evaluate any publication bias [27, 28]. The quality of evidence for each risk factor was likewise assessed by both AC and ET using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) for prognostic studies [29, 30] and discussed among all authors. The QUIPS and GRADE assessments were added after the PROSPERO protocol registration.
Results
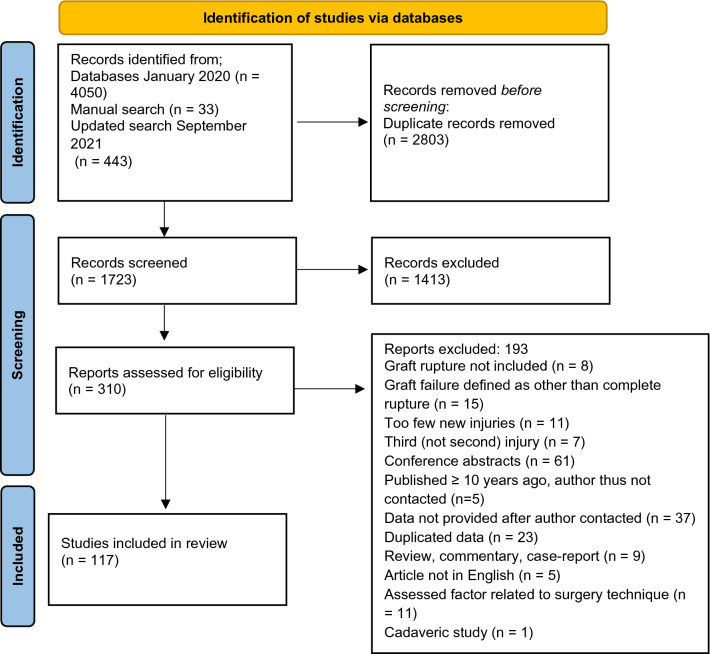
The systematic search yielded a total of 4493 articles, and another 33 articles were identified by manual search. Of these, 310 full-text papers were then screened according to the inclusion/exclusion criteria and 131 were further excluded. In addition, 52 studies pooled the results for graft rupture with C-ACL injury, or reported the results according to different surgery techniques instead of according to graft rupture/no graft rupture [10, 31–81]. Five of these studies [31–35] were published > 10 years ago and the authors were therefore not contacted. The authors of the remaining 47 studies were contacted by email and data for graft rupture, specifically, were provided for nine studies [36, 39, 41, 43, 46, 48, 49, 77, 79]. Twelve studies [82–93] reported partly on the same participants taken from the Nordic knee ligament registries. Of these, we included one study that included data from all registries (Sweden, Norway, Denmark) [88] and another two studies reporting on specific data not included in the first study (patient-reported outcomes, timing of surgery [82] and RTS [92]). Data from 15 other studies were also partly reported on in previous publications [94–105] [106–108]. Of those, the studies with the largest sample size, the most included risk factors and/or reporting statistics allowing calculation of ORs were included [94, 97, 101, 104, 106]. Altogether, 117 articles were included in this review [9, 36, 39, 41, 43, 46, 48, 49, 72, 73, 77, 79, 82, 88, 92, 94, 97, 101, 104, 106, 109–205] (Fig. 1).
Fig. 1.
Flow chart of the inclusion process
Study Characteristics
Twelve of the included articles [185–196] were not eligible for meta-analysis (e.g., only one study assessing the specific risk factor or reported statistics not possible to calculate as odds ratios). The characteristics and results of these studies are reported in Online resource 3 (see ESM). Consequently, 105 studies were included in the meta-analysis. Seventy-three studies reported on sex, 45 on age, 27 on activity level and/or sports participation, 21 on associated injuries, 14 on body mass index (BMI), 11 on family history, 12 on tibial slope, five on smoking status, four on timing of surgery, four on contact/non-contact injury mechanism, four on hop performance and two on general laxity, growth plate status, femoral condyle ratio, patient-reported outcomes, number of physiotherapy visits, kinematics, muscle strength and psychological readiness to RTS, respectively, (see Online resource 4, Table 1, in the ESM for characteristics of each individual study included in the meta-analyses). Thirty-one of these studies also included additional risk factors not eligible for meta-analysis (e.g., only one study assessing the specific risk factor). The results for these specific factors are also reported in Online resource 3 (see ESM).
Synthesis of Results
Meta-analyses consisting of between two and 73 studies (n = 108–133,128) were performed separately for 42 potential risk factors for graft rupture. Sixteen risk factors were rated as moderate quality, 12 as low and 14 as very low-quality evidence according to GRADE (Table 1).
Table 1.
Quality of evidence of the included risk factors according to Grading of Recommendations Assessment, Development and Evaluation (GRADE)
| Risk factor | GRADE criteria | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Phase of investigation | Risk of bias | Inconsistency | Indirectness | Impression | Publication bias | Upgrading factors | GRADE quality of evidence | Summary of findings | |
| Age ≥ 18 vs < 18 years | +++ | x | − | x | x | x | + | +++ | Age < 18 years associated with higher odds of graft rupture |
| Age ≥ 20 vs < 20 years | +++ | x | − | x | x | x | + | +++ | Age < 20 years associated with higher odds of graft rupture |
| Age ≥ 25 vs < 25 years | +++ | x | – | x | x | x | + | ++ | Age < 25 years associated with higher odds of graft rupture |
| Age ≥ 30 vs < 30 years | +++ | x | − | x | x | x | + | +++ | Age < 30 years associated with higher odds of graft rupture |
| Age continuous | +++ | x | – | x | x | x | + | +++ | Lower age associated with higher odds of graft rupture |
| Sex | +++ | x | x | x | − | x | x | ++ | Females had lower odds of graft rupture |
| Marx score at primary injury | +++ | x | – | x | − | x | x | − | No association |
| Tegner score at primary injury | +++ | x | x | x | − | x | x | ++ | Higher score associated with higher odds of graft rupture |
| Tegner score at primary injury ≥ 7 vs < 7 | +++ | x | x | x | − | x | + | +++ | Score ≥ 7 associated with higher odds of graft rupture |
| Lateral tibial slope | +++ | x | – | x | x | x | x | + | Increased tibial slope associated with higher odds of graft rupture |
| Medial tibial slope | +++ | x | − | x | − | x | x | + | No association |
| Femoral condyle ratio | +++ | x | x | x | − | x | x | ++ | No association |
| Duration between injury and surgery ≥ 12 vs < 12 months | +++ | x | x | x | x | x | x | +++ | Surgery < 12 months associated with higher odds of graft rupture |
| Duration between injury and surgery ≥ 6 vs < 6 months | +++ | − | x | x | − | x | x | + | No association |
| Duration between injury and surgery ≥ 3 vs < 3 months | +++ | x | − | x | x | x | x | ++ | No association |
| Return to pre-injury activity level (RTS) | +++ | x | x | x | x | x | x | +++ | RTS associated with higher risk of graft rupture |
| Family history of ACL injury | +++ | x | x | x | x | x | x | +++ | Family history associated with higher risk of graft rupture |
| KOOS ADL | +++ | x | x | x | x | x | x | +++ | No association |
| KOOS pain | +++ | x | x | x | x | x | x | +++ | No association |
| KOOS QoL | +++ | x | x | x | x | x | x | +++ | No association |
| KOOS sport/recreation | +++ | x | x | x | x | x | x | +++ | No association |
| KOOS symptom | +++ | x | x | x | − | x | x | ++ | Higher score associated with decreased odds of graft rupture |
| Psychological readiness to RTS | +++ | − | x | x | − | − | x | − | Lower readiness associated with higher odds of graft rupture |
| Concomitant cartilage injury | +++ | x | x | x | x | x | x | +++ | Cartilage injury associated with higher odds of graft rupture |
| Concomitant meniscal tear | +++ | x | x | x | x | x | x | +++ | No association |
| Concomitant meniscal repair | +++ | x | − | x | x | x | x | ++ | No association |
| Concomitant meniscectomy | +++ | x | x | x | x | x | x | +++ | No association |
| Concomitant MCL injury | +++ | x | x | x | x | x | x | +++ | No association |
| BMI ≥ 25 vs < 25 kg/m2 | +++ | − | – | x | x | x | x | − | No association |
| BMI | +++ | x | – | x | x | x | x | + | No association |
| Smoking status | +++ | x | − | x | x | x | x | ++ | No association |
| Contact vs non-contact mechanism of primary injury | +++ | x | − | x | − | x | x | + | No association |
| General joint laxity | +++ | − | – | x | − | x | x | − | No association |
| Growth plate status | +++ | x | − | x | − | x | x | + | No association |
| Number of physical therapy visits | +++ | x | x | x | − | x | x | ++ | No association |
| Timing of RTS ≥ 6 vs < 6 months | +++ | − | x | x | − | x | x | − | No association |
| Type of sport (soccer vs other sports) | +++ | x | − | x | x | x | x | ++ | No association |
| Hop performance (SLHD) | +++ | x | x | x | − | x | x | ++ | No association |
| Hop performance (THD) | +++ | − | x | x | − | x | x | + | No association |
| Knee abduction | +++ | x | x | x | − | x | x | ++ | No association |
| Q-ceps peak torque | +++ | − | x | x | − | x | x | + | No association |
| Hamstring peak torque | +++ | − | x | x | − | x | x | + | No association |
GRADE criteria: +++ = phase III studies, x = no serious limitations, – = moderate limitations, − = serious limitations, + = upgrade by one. GRADE quality: ++++ = high, +++ = moderate, ++ = low, ± = very low quality of evidence
ACL anterior cruciate ligament, ADL activities of daily living, BMI body mass index, KOOS Knee injury and Osteoarthritis Outcome Score, MCL medial collateral ligament, Q-ceps quadriceps, QoL quality of life, RTS return to sport, SLHD single-leg hop for distance, THD triple hop for distance
Seven key factors were identified to increase the odds of future graft rupture after ACLR: (1) high activity level with the odds being almost four times higher for those having a Tegner score of ≥ 7 compared with those scoring < 7 at the primary injury (OR 3.91, 95% CI 1.69–9.04, moderate quality evidence); (2) young age (dichotomous variable), with the odds being 2.6–3.5 times higher for those aged < 18–30 years compared with ≥ 18–30 years, respectively (OR 2.59–3.53, 95% CI 1.51–5.55, low to moderate quality evidence); (3) increased lateral tibial slope (degrees) (OR 2.21, 95% CI 1.26–3.86, very low quality evidence); (4) lower psychological readiness to RTS (OR 2.18, 95% CI 1.32–3.61, very low quality evidence); (5) surgery within 12 months compared with surgery ≥ 12 months post-injury (OR 1.87, 95% CI 1.58–2.22, moderate quality evidence); (6) returning to pre-injury activity level (OR 1.87, 95% CI 1.21–2.91, moderate quality evidence); and finally, (7) family history of ACL injury (OR 1.76, 95% CI 1.34–2.31, moderate quality evidence) (Online resource 5, Figs. 1–7, see ESM). In addition, higher age (continuous variable) (OR 0.47, 95% CI 0.38–0.59, moderate quality evidence), female sex (OR 0.88, 95% CI 0.79–0.98, low quality evidence), better pre-reconstruction score on the Knee injury and Osteoarthritis Outcome Score (KOOS) (symptom subscale) (OR 0.81, 95% CI 0.69–0.95, low quality evidence) and concomitant cartilage injury (OR 0.70, 95% CI 0.62–0.79, moderate quality evidence) decreased the odds of sustaining a graft rupture (Online resource 5, Figs. 2, 8–10, see ESM). The following factors were found not to be associated with future graft rupture: BMI, smoking status, contact versus non-contact injury mechanism, medial tibial slope, general joint laxity, pre-reconstruction KOOS score (subscales: pain, activities of daily living, quality of life, sport/recreation), timing of surgery (≥ 3 vs < 3 months or ≥ 6 vs < 6 months), number of physical therapy visits, timing of RTS (≥ 6 vs < 6 months), playing soccer compared with other sports, Marx activity score at primary injury, hop performance, quadriceps strength, hamstring strength, knee abduction after RTS, concomitant meniscal or medial collateral ligament injuries or femoral condyle ratio (Online resource 5, Fig. 7, 11–26, see ESM).
Subgroup Analysis
Sex was the sole variable eligible for meta-analysis for the adults. No difference in the odds of sustaining a graft rupture was observed between males and females if only adults were considered (Online resource 5, Fig. 27, see ESM).
Of the factors eligible for meta-analysis in the subgroup of C&A, a family history of ACL injury (OR 2.03, 95% CI 1.13–3.64) was associated with a higher odds of future graft rupture, whereas female sex decreased the odds (OR 0.71, 95% CI 0.57–0.89) (Online resource 5, Figs. 7 and 27, see ESM). On the other hand, the following factors were not associated with the odds of sustaining a future graft rupture in this population: age, BMI, return to pre-injury activity level, growth plate status and concomitant meniscal injury (Online resource 5, Figs. 7, 22–23, 28–30, see ESM).
Risk of Bias and Heterogeneity
Sex, family history, RTS and concomitant meniscal tear were the only variables eligible for assessment of publication bias. The funnel plots with trim and fill imputations showed no difference in effect measure, indicating no publication bias for either of the variables as risk factors for graft rupture [27] (Online resource 6, Figs. 1–4, see ESM).
Fifty-eight (50%) studies were rated as low risk of bias, 17 (14%) as moderate and 42 (36%) as high risk of bias (Online resource 6, Table 1, see ESM). After sensitivity analyses were performed, excluding articles with high risk of bias [206], a BMI ≥ 25 kg/m2 decreased the odds of sustaining a graft rupture. No other differences in the results were observed (Online resource 7, Table 1, see ESM).
I2 ranged between < 0.001% and 92% for all meta-analyses, indicating low to high heterogeneity between studies [22] (Online resource 5, Figs. 3–30, see ESM).
Discussion
This systematic review and meta-analysis identified the following factors as associated with graft rupture with moderate quality evidence: a higher pre-injury activity level, younger age (< 20 years), family history of ACL injury, surgery performed within 12 months and RTS. Increased lateral tibial slope and lower psychological readiness to RTS were also associated with sustaining a future graft rupture but with very low to low quality evidence. Female sex decreased the odds (low quality evidence). On the other hand, factors such as smoking status, joint laxity, timing of RTS, kinematics, knee muscle strength and hop performance were not associated with future graft rupture. Few studies investigated factors related to sensorimotor function and neuromuscular control.
A pre-primary injury Tegner score of ≥ 7 compared with a lower activity level was associated with the highest odds (OR 3.91) of sustaining a graft rupture. In addition, and in line with our previous review on risk factors for C-ACL injury [12], return to pre-injury activity level after ACLR was associated with almost twice the odds of future graft rupture, whereas the time point of RTS (< 6 vs ≥ 6 months), or playing soccer compared with other sports, were not related to graft rupture. A high activity level has previously been linked to an increased risk of ACL injury [37], and individuals who have a higher Tegner score prior to their primary injury are reported to be more likely to return to their pre-injury activity level compared with those initially active on a lower level [207]. Taken together, these results corroborate that participating in and returning to a high activity level that imposes substantial load on the knees leads to a higher risk of graft rupture, irrespective of time point of return and the sports involved. While the pre-injury Marx score was not significantly associated with graft rupture, the Marx score was reported in only two studies and has poorer psychometric properties [208], which may explain differences in the result between these two scales of activity level/participation.
Extending the result from a recent meta-analysis reporting younger age to be a risk factor for C-ACL injury [12], younger age was likewise associated with a higher odds of graft rupture in the current review. Those younger than 20 years had an odds ratio of 3.53 for sustaining a future graft rupture compared with those older than 20 years. The fact that the anatomical structures and neuromuscular system are still under development during adolescence may partly explain why young individuals have a greater risk [209, 210]. Secondly, athletes younger than 20 years are often involved in sport at a higher level [150] and also seem to return to sport to a greater extent [51, 104, 157] without having achieved proper knee function [211] compared with older athletes, which also likely contributes to an increased risk in these young individuals. This reasoning is further supported by the absence of any association between age and graft rupture in the analysis including only those aged 19 and younger, when most athletes may return to a more competitive and knee challenging sports level.
In accordance with research on risk factors for both primary [119, 169, 212] and C-ACL injury [12], the current data revealed that those with a parent and/or sibling who had suffered an ACL injury had higher odds (OR 1.76) of sustaining a graft rupture compared with those with no family history of ACL injury. This was true for both adults and those of younger age. Many factors that predispose individuals to knee injury may be hereditary. Suggested explanations may be related to specific gene polymorphisms [213] and/or inherited anatomical, biomechanical and neuromuscular factors [119, 214]. In line with research that reported increased MRI-verified lateral, but not medial tibial slope to be associated with primary ACL injury [215], the current meta-analysis showed that individuals with a greater lateral tibial slope had higher odds of sustaining a graft rupture, whereas there was no association for medial slope. Greater lateral compared with medial slope is suggested to increase anterior tibial translation as well as internal rotation during functional activity, which consequently may increase ACL strain [216–220]. Furthermore, while we found no relation between general joint laxity and graft rupture risk in the current review, Hewett et al. followed two fraternal female twins from baseline screening to when they both sustained an ACL injury and reported both twins to have increased joint laxity, altered joint biomechanics during movement, such as increased knee abduction and reduced knee flexion, and altered muscle activation pattern [214]. Another suggested explanation for the association between a positive family history and ACL injury may be a familial inclination for sport participation [119]. In-depth approaches are, however, warranted regarding which specific hereditary factors have the strongest links to increased primary and secondary ACL injury risk.
Performing ACLR within 12 months from injury increased the odds of sustaining a graft rupture by 87% compared with delayed surgery (≥ 12 months). In contrast to our previous review where a higher risk of sustaining a C-ACL injury was reported for those who received an ACLR within 3 months [12], no difference in graft rupture rate was observed for other surgery time point cut-offs (≥ 3 vs < 3 months or ≥ 6 vs < 6 months). An early reconstruction has previously been associated with a higher post-operative activity level [221] and it is plausible that the group that delayed reconstruction for 12 months or more represents a group of individuals that have a lower pre-injury activity level and/or may not return to their pre-injury activity level and, thus, are less likely to put their knee at risk. Individuals delaying surgery > 12 months may also represent a group of so called ‘copers’, that is, being able to RTS with excellent dynamic knee stability after ACLR [222]. A recent study has shown that copers have approximately three times the odds of rehabilitation success, including lower graft rupture rate, compared with non-copers [223], which may partly explain our result.
Similar to our previous review on C-ACL injury [12], the meta-analysis showed that concomitant cartilage injury at the time of primary injury decreased the odds of sustaining a future graft rupture, whereas no such association was observed for meniscal injuries. Given that individuals with concomitant cartilage injury are reported to have decreased self-reported knee function, worse knee symptoms, lower quadriceps muscle strength and reduced activity level post-surgery compared with those without cartilage damage [118, 224–226], these individuals may not return to sport and thereby decrease the risk of re-injury to either knee. The relationships between meniscal injury/other concomitant injuries, activity level and post-surgery function are not unscrambled [225, 226] and such complexities may underlie the lack of association between meniscal injuries and graft rupture in the current analysis. Further studies are needed to disentangle the possible association between concomitant injuries, related functional impairment, failure to RTS and second ACL injuries.
In contrast to previous research reporting female sex to be a risk factor for sustaining both a primary ACL injury [1, 227–230] and a C-ACL injury [12], females had lower odds of sustaining a graft rupture in the current review when both adults and C&A were included in the meta-analysis. This result is in accordance with a recent systematic review that reported females to have lower absolute risk of sustaining a graft rupture compared with males [14]. Hormonal sex differences as well as neuromuscular differences in muscle activation pattern and postural control have been suggested to contribute to the higher risk of ACL injuries in females [11, 231]. This indicates that such factors may play a role in primary injury and that a C-ACL injury may in fact be considered as a primary injury to the contra-lateral leg, whereas other factors may be important for graft rupture. The subgroup analyses further showed that when only adults were included in the analysis, there was no sex difference in the odds of sustaining a graft rupture but that the odds for sustaining a graft rupture for females decreased even more when only those age 19 and younger were considered, indicating that the apparent sex difference is mostly driven by young individuals. This is also supported by a recent systematic review that reported males to have a higher risk of graft rupture than females in individuals younger than 20 years of age [16]. It is known that young males return to sport both earlier, more often and to a higher level compared with their female counterparts [51], which may explain why young males had higher odds of graft rupture than young females. However, in the current review there was no effect of RTS on graft rupture in the subgroup for C&A, which may contradict this hypothesis. It should be noted though, that this particular subgroup analysis (i.e., RTS) included very few studies (n = 3), and that the OR (1.72) was quite similar to the OR (1.91) for the full analysis. Furthermore, young males seemed to undergo ACLR using a physeal-sparing technique due to skeletal immaturity and open growth plates to a higher extent than females, which has been suggested to influence graft rupture rate in young males [232]. Neither surgical technique [232] nor growth-plate status seemed, however, to be associated with graft rupture when males and females were pooled (Online resource 5, Fig. 30, see ESM) or stratified by sex [177].
In a previous systematic review, a BMI < 25 kg/m2 was associated with higher odds of sustaining a future C-ACL injury, whereas smoking status did not seem to be related to C-ACL injury [12]. Individuals with a high BMI and smokers have been reported to have lower activity levels and worse symptoms and self-reported function after ACLR compared with those with a lower BMI and non-smokers [221]. Notwithstanding, our results did not support any relationship between either BMI or smoking status and future graft rupture. However, when excluding one study with high risk of bias from the meta-analysis, a BMI ≥ 25 kg/m2 was associated with decreased odds of sustaining a graft rupture, indicating that any relation between BMI and graft rupture is still to be verified.
Knee kinematics, kinetics, knee muscle strength, hop performance and self-reported outcomes, such as knee confidence, have previously been linked to the risk of second ACL injuries (graft ruptures and C-ACL injuries combined) [31, 40, 50, 233]. In the current review, few articles on objective and self-reported function as risk factors for graft rupture as a separate entity were eligible for meta-analysis (too few studies on same factor assessed at same time point or pooling of graft rupture and C-ACL injury). Psychological factors, such as negative emotions, stress, lack of knee confidence and fear of re-injury are commonly reported after ACL injury [234–237] and may have a negative impact on both the rehabilitation process [235] and RTS rate [237]. Lower psychological readiness to RTS, as assessed with the ACL Return to Sport after Injury scale [238], 9–12 months post-reconstruction was associated with higher odds of sustaining a future graft rupture in the current meta-analysis. In addition, Paterno et al. [192] reported those with kinesiophobia to be more prone to rupture of the reconstructed ACL (Online resource 3, see ESM). This result further highlights the importance of incorporating psychological aspects into the rehabilitation process after knee injury.
Similar to the findings for primary ACL injury [239, 240], we found no association between peak knee abduction angle during drop landing and the odds of future graft rupture. Notably, the two studies included in this analysis used different measures to assess knee abduction (2D vs 3D) during slightly different tasks (one-leg vs double-leg drop landing). Although 2D and 3D measures of knee abduction seem closely related [241–243] and the knee abduction angle is proposed to be similar during the execution of single-leg and double-leg landings [244, 245], it is possible that these differences obscured the results of the separate studies. Given this and the few studies included in the analysis, the result for knee abduction angle should be interpreted with caution. Furthermore, the meta-analyses revealed no relation between the performance of the single and triple hop for distance or hamstring and quadriceps peak torque, respectively, and future graft rupture. On the other hand, Kyritsis et al., reported lower hamstring to quadriceps ratio when returning to sport to be associated with a higher risk of graft rupture [130] (Online resource 3, see ESM) and better KOOS score on the symptom subscale decreased the odds of graft rupture in our analysis (no associations for other subscales). The few studies included in these analyses (n = 2–4) highlight the lack of studies that include the same measures of sensorimotor function or psychological aspects as potential risk factors for graft rupture. Standardized objective and self-reported measures on function and psychological constructs that are responsive to training/intervention, in contrast to demographic factors that are non-modifiable by nature, should thus be considered in future studies on risk factors for secondary knee injuries. This is a prerequisite to fully understand the role of the neuromuscular and psychological factors in the risk of graft rupture after ACLR.
ACL injuries are most frequent in sports, and re-injury incidence is very high [6]. According to the results from this review, the aspects of being a highly active sport athlete, < 20 years, male, and having low psychological readiness to RTS were among the factors associated with higher odds of graft rupture. Clinicians should be prepared to meet the needs of young highly active sports athletes, incorporating psychological aspects into the rehabilitation after ACLR. Being able to RTS after injury is also closely related to the athletic and personal identity [246–248], as well as to regaining long-term quality of life [7, 249]. In light of this and of the International Olympic Committees’ “Athletes’ Rights and Responsibilities Declaration” (Right #7 of the Preamble) [250], athlete rehabilitation efforts post-ACLR as well as future research should focus on a safe return to sport to reduce the high risk of re-injury in athletes.
In this systematic review, we included all studies that assessed risk factors for graft rupture without any restrictions related to either participant demographics, sport exposure, graft type or year of publication, which also increases the generalizability of our findings. Other strengths of our review are the very high number of individuals in most of the meta-analyses (up to 133,000).
However, there are several limitations. Our review includes studies with different definitions of graft rupture, such as clinically or MRI verified ruptures as well as revision surgery identified from surgical records. It is possible that using only revision surgery as outcome may underestimate the graft rupture rate and consequently influence the result of the meta-analysis, since this approach will not capture those who chose to have non-surgical treatment of their second injury. We also pooled studies on males and females and different age groups, but have performed subgroup analysis to account for possible differences between C&A populations and adults. Since only seven of the 117 included articles reported solely on males (n = 4) or females (n = 3) and all other articles included both sexes, we do not believe that this had any major influence on our result. An additional limitation is that we pooled studies including different types of grafts and surgery techniques for ACLR. Since most of the included studies comprised a mixture of different graft types/surgery techniques or did not report graft type at all, we chose to not perform subgroup analysis for graft type. Although assessing graft type and surgery technique as possible risk factors was beyond the scope of this study, research indicates an advantage for autograft versus allograft and patella graft versus hamstring graft in the risk of graft failure [251, 252], which may be considered in future research. While most of our meta-analyses were associated with low to moderate heterogeneity, a few analyses—age (continuous, ≥ 25 vs < 25 years), BMI, Marx activity scale, lateral tibial slope and general joint laxity—had high heterogeneity measured with I2 statistics (≥ 75%) [22]. To account for expected heterogeneity, we performed all meta-analyses under the random effect model that incorporates both within-study and between-study variance in the analysis. It should also be noted that most analyses with high heterogeneity included a low number of studies, which may lead to bias of the I2 statistics [253]. Thus, the I2 statistics for these specific studies should be interpreted with caution. The mechanisms contributing to ACL injury and graft rupture are most likely multifactorial and incorporate a combination of both demographic factors, such as family history and age, as well as factors related to neuromuscular control and sensorimotor function [11] and cannot be entirely explained by single factors. Other important factors are RTS status and sports exposure. Since we included all studies assessing risk factors for graft rupture, regardless of sports exposure or RTS status, most studies did not provide such information. It has been suggested that, for example, the relation between young age and a higher risk of second ACL injury is more dependent on the higher RTS rate in young individuals than age [38]. Applying a multifactorial model for assessing risk factors for graft rupture was beyond the scope of the current review but it cannot be ruled out that the result for some factors would have been different if several possible risk factors, including RTS status and sports exposure, had been considered in the same model. We do, however, believe that this review could be a starting point for exploring more complex models incorporating all relevant factors for assessing graft rupture risk in future studies. Finally, we used OR as outcome measure in all analyses and the results should, thus, not be interpreted as equal to the risk of sustaining a future graft rupture [254].
Conclusion
This systematic review with meta-analysis provides evidence that high activity level, RTS, young age, low psychological readiness to RTS, family history of ACL injury, surgery performed within 12 months, and increased tibial slope are all factors related to increased odds of sustaining a future graft rupture. Females seem, however, to have lower odds of graft rupture compared with males. Studies including modifiable risk factors such as neuromotor control were rare. We recommend that future attention in research should be given to factors such as muscle strength and activation, sensorimotor control and movement quality as well as psychological factors, all of which may be responsive to training/intervention, and thus able to be incorporated into rehabilitation protocols aiming at reducing the risk of further knee injuries after ACL injury and facilitating a safe RTS for ACL-injured individuals.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
Open access funding provided by Umeå University. This work was supported by the Swedish Research Council for Sport Science (P2019-0011, D2019-0005), The Gyllenstierna Krapperup´s Foundation and Lennander’s Foundation.
Conflict of interest
Anna Cronström, Eva Tengman and Charlotte K. Häger declare that they have no conflicts of interest relevant to the content of this review.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
AC contributed to the conception and design of the study, performed the statistical analyses and was in charge of writing the manuscript. ET and CKH contributed to the conception and design of the study, helped in the interpretation of the statistical analyses and provided feedback on drafts of this paper. All authors read and approved the final manuscript.
References
- 1.Walden M, Hagglund M, Werner J, Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc. 2011;19(1):3–10. doi: 10.1007/s00167-010-1172-7. [DOI] [PubMed] [Google Scholar]
- 2.Beynnon BD, Vacek PM, Newell MK, Tourville TW, Smith HC, Shultz SJ, Slauterbeck JR, Johnson RJ. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806–1812. doi: 10.1177/0363546514540862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niederer D, Engeroff T, Wilke J, Vogt L, Banzer W. Return to play, performance, and career duration after anterior cruciate ligament rupture: a case–control study in the five biggest football nations in Europe. Scand J Med Sci Sports. 2018;28(10):2226–2233. doi: 10.1111/sms.13245. [DOI] [PubMed] [Google Scholar]
- 4.Ageberg E. Consequences of a ligament injury on neuromuscular function and relevance to rehabilitation—using the anterior cruciate ligament-injured knee as model. J Electromyogr Kinesiol. 2002;12(3):205–212. doi: 10.1016/S1050-6411(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 5.Leathers MP, Merz A, Wong J, Scott T, Wang JC, Hame SL. Trends and demographics in anterior cruciate ligament reconstruction in the United States. J Knee Surg. 2015;28(5):390–394. doi: 10.1055/s-0035-1544193. [DOI] [PubMed] [Google Scholar]
- 6.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Filbay SR, Ackerman IN, Russell TG, Crossley KM. Return to sport matters-longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand J Med Sci Sports. 2016;27:514–524. doi: 10.1111/sms.12698. [DOI] [PubMed] [Google Scholar]
- 8.Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1033–1041. doi: 10.1136/bjsports-2015-094864. [DOI] [PubMed] [Google Scholar]
- 9.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 10.Wasserstein D, Huston LJ, Nwosu S, Kaeding CC, Parker RD, Wright RW, Andrish JT, Marx RG, Amendola A, Wolf BR, et al. KOOS pain as a marker for significant knee pain two and six years after primary ACL reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) prospective longitudinal cohort study. Osteoarthritis Cartil. 2015;23(10):1674–1684. doi: 10.1016/j.joca.2015.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: cut risk with three sharpened and validated tools. J Orthop Res. 2016;34(11):1843–1855. doi: 10.1002/jor.23414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cronström A, Tengman E, Häger CK. Risk factors for contra-lateral secondary anterior cruciate ligament injury: a systematic review with meta-analysis. Sports Med. 2021;51(7):1419–1438. doi: 10.1007/s40279-020-01424-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med. 2019;49(6):917–929. doi: 10.1007/s40279-019-01093-x. [DOI] [PubMed] [Google Scholar]
- 14.Patel AD, Bullock GS, Wrigley J, Paterno MV, Sell TC, Losciale JM. Does sex affect second ACL injury risk? A systematic review with meta-analysis. Br J Sports Med. 2021;55(15):873–882. doi: 10.1136/bjsports-2020-103408. [DOI] [PubMed] [Google Scholar]
- 15.Costa GG, Perelli S, Grassi A, Russo A, Zaffagnini S, Monllau JC. Minimizing the risk of graft failure after anterior cruciate ligament reconstruction in athletes. A narrative review of the current evidence. J Exp Orthop. 2022;9(1):26. doi: 10.1186/s40634-022-00461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barber-Westin S, Noyes FR. One in 5 athletes sustain reinjury upon return to high-risk sports after ACL reconstruction: a systematic review in 1239 athletes younger than 20 years. Sports Health. 2020;12(6):587–597. doi: 10.1177/1941738120912846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mok AC, Fancher AJ, Vopat ML, Baker J, Tarakemeh A, Mullen S, Schroeppel JP, Templeton K, Mulcahey MK, Vopat BG. Sex-specific outcomes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Orthop J Sports Med. 2022;10(2):23259671221076883. doi: 10.1177/23259671221076883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW. Factors associated with revision following anterior cruciate ligament reconstruction: a systematic review of registry data. Knee. 2020;27(2):287–299. doi: 10.1016/j.knee.2019.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borenstein M, Hedges L, Higgins J, Hannah R. Introduction to meta-analysis. New York: Wiley; 2009. [Google Scholar]
- 22.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lento PH, Akuthota V. Meniscal injuries: a critical review. J Back Musculoskelet Rehabil. 2000;15(2):55–62. doi: 10.3233/BMR-2000-152-302. [DOI] [PubMed] [Google Scholar]
- 24.Cochrane handbook for systematic reviews of interventions. http://handbook.cochrane.org/chapter_16/16_5_4_how_to_include_multiple_groups_from_one_study.htm.
- 25.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 26.Grooten WJA, Tseli E, Äng BO, Boersma K, Stålnacke BM, Gerdle B, Enthoven P. Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS-aspects of interrater agreement. Diagn Progn Res. 2019;3:5. doi: 10.1186/s41512-019-0050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duval S, Tweedy R. A nonparametric "trim and fill method" of accounting for publication bias in meta-analyses. J Am Stat Assoc. 2000;95:89–98. [Google Scholar]
- 28.Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ. 2007;176(8):1091–1096. doi: 10.1503/cmaj.060410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.How to GRADE the quality of evidence. Cochrane Consumers and Evaluation Group. https://opal.latrobe.edu.au/articles/journal_contribution/How_to_GRADE/6818894.
- 30.Huguet A, Hayden JA, Stinson J, McGrath PJ, Chambers CT, Tougas ME, Wozney L. Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev. 2013;2:71. doi: 10.1186/2046-4053-2-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593–1601. doi: 10.1016/j.arthro.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 33.Gorschewsky O, Klakow A, Riechert K, Pitzl M, Becker R. Clinical comparison of the Tutoplast allograft and autologous patellar tendon (bone-patellar tendon-bone) for the reconstruction of the anterior cruciate ligament: 2- and 6-year results. Am J Sports Med. 2005;33(8):1202–1209. doi: 10.1177/0363546504271510. [DOI] [PubMed] [Google Scholar]
- 34.Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36(7):1275–1282. doi: 10.1177/0363546508314721. [DOI] [PubMed] [Google Scholar]
- 35.van Dijck RA, Saris DB, Willems JW, Fievez AW. Additional surgery after anterior cruciate ligament reconstruction: can we improve technical aspects of the initial procedure? Arthroscopy. 2008;24(1):88–95. doi: 10.1016/j.arthro.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 36.Fleming BC, Fadale PD, Hulstyn MJ, Shalvoy RM, Oksendahl HL, Badger GJ, Tung GA. The effect of initial graft tension after anterior cruciate ligament reconstruction: a randomized clinical trial with 36-month follow-up. Am J Sports Med. 2013;41(1):25–34. doi: 10.1177/0363546512464200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grindem H, Engebretsen L, Axe M, Snyder-Mackler L, Risberg MA. Activity and functional readiness, not age, are the critical factors for second anterior cruciate ligament injury—the Delaware-Oslo ACL cohort study. Br J Sports Med. 2020;54:1099–1102. doi: 10.1136/bjsports-2019-100623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tagesson S, Kvist J. Greater fear of re-injury and increased tibial translation in patients who later sustain an ACL graft rupture or a contralateral ACL rupture: a pilot study. J Sports Sci. 2016;34(2):125–132. doi: 10.1080/02640414.2015.1035668. [DOI] [PubMed] [Google Scholar]
- 40.Capin JJ, Khandha A, Zarzycki R, Manal K, Buchanan TS, Snyder-Mackler L. Gait mechanics and second ACL rupture: implications for delaying return-to-sport. J Orthop Res. 2016;35:1894–1901. doi: 10.1002/jor.23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beischer S, Gustavsson L, Senorski EH, Karlsson J, Thomeé C, Samuelsson K, Thomeé R. Young athletes who return to sport before 9 months after anterior cruciate ligament reconstruction have a rate of new injury 7 times that of those who delay return. J Orthop Sports Phys Ther. 2020;50(2):83–90. doi: 10.2519/jospt.2020.9071. [DOI] [PubMed] [Google Scholar]
- 42.Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Jt Surg Am. 2017;99(11):897–904. doi: 10.2106/JBJS.16.00758. [DOI] [PubMed] [Google Scholar]
- 43.Krosshaug T, Steffen K, Kristianslund E, Nilstad A, Mok KM, Myklebust G, Andersen TE, Holme I, Engebretsen L, Bahr R. The vertical drop jump is a poor screening test for ACL injuries in female elite soccer and handball players: a prospective cohort study of 710 athletes. Am J Sports Med. 2016;44(4):874–883. doi: 10.1177/0363546515625048. [DOI] [PubMed] [Google Scholar]
- 44.Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, Spang JT. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA division I cohort. Am J Sports Med. 2014;42(7):1638–1643. doi: 10.1177/0363546514524164. [DOI] [PubMed] [Google Scholar]
- 45.Schilaty ND, Nagelli C, Bates NA, Sanders TL, Krych AJ, Stuart MJ, Hewett TE. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. doi: 10.1177/2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J, Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med. 2017;51(22):1622–1629. doi: 10.1136/bjsports-2016-097124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.CarlLee T, Ries Z, Duchman K, Gao Y, Wolf B, Amendola A, Hettrich C, Bollier M. Outside-in vs. anteromedial portal drilling during primary ACL reconstruction: comparison at two years. Iowa Orthop J. 2017;37:117–122. [PMC free article] [PubMed] [Google Scholar]
- 48.McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857–862. doi: 10.1177/0363546518825258. [DOI] [PubMed] [Google Scholar]
- 49.Annear PT, Rohr EJ, Hille DM, Gohil S, Ebert JR. No clinical difference in 10-year outcomes between standard and minimal graft debridement techniques in patients undergoing anterior cruciate ligament reconstruction using autologous hamstrings: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):516–523. doi: 10.1007/s00167-018-5146-5. [DOI] [PubMed] [Google Scholar]
- 50.Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: preliminary development of a clinical decision algorithm. Orthop J Sports Med. 2017;5(12):2325967117745279. doi: 10.1177/2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brophy RH, Schmitz L, Wright RW, Dunn WR, Parker RD, Andrish JT, McCarty EC, Spindler KP. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. doi: 10.1177/0363546512459476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paterno MV, Kiefer AW, Bonnette S, Riley MA, Schmitt LC, Ford KR, Myer GD, Shockley K, Hewett TE. Prospectively identified deficits in sagittal plane hip-ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin Biomech (Bristol, Avon) 2015;30(10):1094–1101. doi: 10.1016/j.clinbiomech.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ateschrang A, Schreiner AJ, Ahmad SS, Schröter S, Hirschmann MT, Körner D, Kohl S, Stöckle U, Ahrend MD. Improved results of ACL primary repair in one-part tears with intact synovial coverage. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):37–43. doi: 10.1007/s00167-018-5199-5. [DOI] [PubMed] [Google Scholar]
- 55.Desai VS, Anderson GR, Wu IT, Levy BA, Dahm DL, Camp CL, Krych AJ, Stuart MJ. Anterior cruciate ligament reconstruction with hamstring autograft: a matched cohort comparison of the all-inside and complete tibial tunnel techniques. Orthop J Sports Med. 2019;7(1):2325967118820297. doi: 10.1177/2325967118820297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Helito CP, Camargo DB, Sobrado MF, Bonadio MB, Giglio PN, Pécora JR, Camanho GL, Demange MK. Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3652–3659. doi: 10.1007/s00167-018-4934-2. [DOI] [PubMed] [Google Scholar]
- 57.Hoogeslag RAG, Brouwer RW, Boer BC, de Vries AJ, Huis In ‘t Veld R. Acute anterior cruciate ligament rupture: repair or reconstruction? Two-year results of a randomized controlled clinical trial. Am J Sports Med. 2019;47(3):567–577. doi: 10.1177/0363546519825878. [DOI] [PubMed] [Google Scholar]
- 58.Leiter JR, Gourlay R, McRae S, de Korompay N, MacDonald PB. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1061–1069. doi: 10.1007/s00167-013-2466-3. [DOI] [PubMed] [Google Scholar]
- 59.Ouanezar H, Blakeney WG, Fernandes LR, Borade A, Latrobe C, Temponi EF, Sonnery-Cottet B. Clinical outcomes of single anteromedial bundle biologic augmentation technique for anterior cruciate ligament reconstruction with consideration of tibial remnant size. Arthroscopy. 2018;34(3):714–722. doi: 10.1016/j.arthro.2017.08.309. [DOI] [PubMed] [Google Scholar]
- 60.Parkinson B, Robb C, Thomas M, Thompson P, Spalding T. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(7):1529–1536. doi: 10.1177/0363546517691961. [DOI] [PubMed] [Google Scholar]
- 61.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013;29(1):98–105. doi: 10.1016/j.arthro.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 62.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish Registry of knee ligament reconstruction. Am J Sports Med. 2014;42(2):278–284. doi: 10.1177/0363546513509220. [DOI] [PubMed] [Google Scholar]
- 63.Rose MB, Domes C, Farooqi M, Crawford DC. A prospective randomized comparison of two distinct allogenic tissue constructs for anterior cruciate ligament reconstruction. Knee. 2016;23(6):1112–1120. doi: 10.1016/j.knee.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 64.Siebold R, Takada T, Feil S, Dietrich C, Stinton SK, Branch TP. Anatomical "C"-shaped double-bundle versus single-bundle anterior cruciate ligament reconstruction in pre-adolescent children with open growth plates. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):796–806. doi: 10.1007/s00167-016-4039-8. [DOI] [PubMed] [Google Scholar]
- 65.Suomalainen P, Järvelä T, Paakkala A, Kannus P, Järvinen M. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med. 2012;40(7):1511–1518. doi: 10.1177/0363546512448177. [DOI] [PubMed] [Google Scholar]
- 66.Calvo R, Figueroa D, Gili F, Vaisman A, Mocoçain P, Espinosa M, León A, Arellano S. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am J Sports Med. 2015;43(2):289–294. doi: 10.1177/0363546514557939. [DOI] [PubMed] [Google Scholar]
- 67.Leo BM, Krill M, Barksdale L, Alvarez-Pinzon AM. Failure rate and clinical outcomes of anterior cruciate ligament reconstruction using autograft hamstring versus a hybrid graft. Arthroscopy. 2016;32(11):2357–2363. doi: 10.1016/j.arthro.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 68.Söderman T, Wretling ML, Hänni M, Mikkelsen C, Johnson RJ, Werner S, Sundin A, Shalabi A. Higher frequency of osteoarthritis in patients with ACL graft rupture than in those with intact ACL grafts 30 years after reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2139–2146. doi: 10.1007/s00167-019-05726-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Evangelopoulos DS, Kohl S, Schwienbacher S, Gantenbein B, Exadaktylos A, Ahmad SS. Collagen application reduces complication rates of mid-substance ACL tears treated with dynamic intraligamentary stabilization. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2414–2419. doi: 10.1007/s00167-015-3838-7. [DOI] [PubMed] [Google Scholar]
- 70.Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ. Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Jt Surg Am. 2018;100(13):1087–1094. doi: 10.2106/JBJS.17.01327. [DOI] [PubMed] [Google Scholar]
- 71.Yang R, Deng H, Hou J, Ouyang Y, Chen Z, Song B, Zhou Y, Tan W, Li W, Shen H. Comparison of knee stability and synovial fluid alterations in anterior cruciate ligament reconstruction with a hamstring autograft or an allograft. Orthopedics. 2017;40(5):e892–e897. doi: 10.3928/01477447-20170824-02. [DOI] [PubMed] [Google Scholar]
- 72.Gupta R, Singhal A, Malhotra A, Soni A, Masih GD, Raghav M. Predictors for anterior cruciate ligament (ACL) re-injury after successful primary ACL reconstruction (ACLR) Malays Orthop J. 2020;14(3):50–56. doi: 10.5704/MOJ.2011.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–121. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hettrich CM, Dunn WR, Reinke EK, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41(7):1534–1540. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Reid D, Leigh W, Wilkins S, Willis R, Twaddle B, Walsh S. A 10-year retrospective review of functional outcomes of adolescent anterior cruciate ligament reconstruction. J Pediatr Orthop. 2017;37(2):133–137. doi: 10.1097/BPO.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 76.Gaj E, Monaco E, De Carli A, Wolf MR, Massafra C, Redler A, Mazza D, Ferretti A. Measurement technique for posterior tibial slope on radiographs can affect its relationship to the risk of anterior cruciate ligament rupture. Int Orthop. 2020. [DOI] [PubMed]
- 77.Fones L, Kostyun RO, Cohen AD, Pace JL. Patient-reported outcomes, return-to-sport status, and reinjury rates after anterior cruciate ligament reconstruction in adolescent athletes: minimum 2-year follow-up. Orthop J Sports Med. 2020;8(11):2325967120964471. doi: 10.1177/2325967120964471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chaker Jomaa M, Gultekin S, Orchard J, Driscoll T, Orchard J. Australian footballers returning from anterior cruciate ligament reconstruction later than 12 months have worse outcomes. Indian J Orthop. 2020;54(3):317–323. doi: 10.1007/s43465-020-00092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fältström A, Hägglund M, Hedevik H, Kvist J. Poor validity of functional performance tests to predict knee injury in female soccer players with or without anterior cruciate ligament reconstruction. Am J Sports Med. 2021;49(6):1441–1450. doi: 10.1177/03635465211002541. [DOI] [PubMed] [Google Scholar]
- 80.Law MA, Ko YA, Miller AL, Lauterbach KN, Hendley CL, Johnson JE, Tsai LC. Age, rehabilitation and surgery characteristics are re-injury risk factors for adolescents following anterior cruciate ligament reconstruction. Phys Ther Sport. 2021;49:196–203. doi: 10.1016/j.ptsp.2021.03.003. [DOI] [PubMed] [Google Scholar]
- 81.Gupta R, Singhal A, Kapoor A, Mehta R, Masih GD. Femoral tunnel length has no correlation with graft rupture: a retrospective cohort study. Knee. 2021;29:405–410. doi: 10.1016/j.knee.2021.02.023. [DOI] [PubMed] [Google Scholar]
- 82.Fältstrom A, Hagglund M, Magnusson H, Forssblad M, Kvist J. Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish National ACL Register. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):885–894. doi: 10.1007/s00167-014-3406-6. [DOI] [PubMed] [Google Scholar]
- 83.Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 84.Andernord D, Björnsson H, Petzold M, Eriksson BI, Forssblad M, Karlsson J, Samuelsson K. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42(7):1574–1582. doi: 10.1177/0363546514531396. [DOI] [PubMed] [Google Scholar]
- 85.Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. doi: 10.1177/0363546514552788. [DOI] [PubMed] [Google Scholar]
- 86.Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM, Fevang JM. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med. 2014;42(2):285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 87.Faunø P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the Danish Registry of knee ligament reconstruction. Orthop J Sports Med. 2014;2(10):2325967114552405. doi: 10.1177/2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42(10):2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 89.Snaebjornsson T, Svantesson E, Sundemo D, Westin O, Sansone M, Engebretsen L, Hamrin-Senorski E. Young age and high BMI are predictors of early revision surgery after primary anterior cruciate ligament reconstruction: a cohort study from the Swedish and Norwegian Knee Ligament Registries based on 30,747 patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3583–3591. doi: 10.1007/s00167-019-05487-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Svantesson E, Hamrin Senorski E, Alentorn-Geli E, Westin O, Sundemo D, Grassi A, Čustović S, Samuelsson K. Increased risk of ACL revision with non-surgical treatment of a concomitant medial collateral ligament injury: a study on 19,457 patients from the Swedish National Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2450–2459. doi: 10.1007/s00167-018-5237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Granan LP, Baste V, Engebretsen L, Inacio MC. Associations between inadequate knee function detected by KOOS and prospective graft failure in an anterior cruciate ligament-reconstructed knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1135–1140. doi: 10.1007/s00167-014-2925-5. [DOI] [PubMed] [Google Scholar]
- 92.Sandon A, Engström B, Forssblad M. High risk of further anterior cruciate ligament injury in a 10-year follow-up study of anterior cruciate ligament-reconstructed soccer players in the Swedish National Knee Ligament Registry. Arthroscopy. 2020;36(1):189–195. doi: 10.1016/j.arthro.2019.05.052. [DOI] [PubMed] [Google Scholar]
- 93.Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL Reconstruction Registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):117–124. doi: 10.1007/s00167-008-0654-3. [DOI] [PubMed] [Google Scholar]
- 94.Mardani-Kivi M, Mobarakeh MK, Keyhani S, Ebrahim-Zadeh MH, Azari Z. Contralateral and siblings' knees are at higher risk of ACL tear for patients with a positive history of ACL tear. Knee Surg Sports Traumatol Arthrosc. 2019;28:622–628. doi: 10.1007/s00167-019-05781-z. [DOI] [PubMed] [Google Scholar]
- 95.Mardani-Kivi M, Azari Z, Hasannejad F. Return to sport activity after anterior cruciate ligament reconstruction: a 6–10 years follow-up. J Clin Orthop Trauma. 2020;11(Suppl 3):S319–s325. doi: 10.1016/j.jcot.2019.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for "isolated" anterior cruciate ligament tear. Am J Sports Med. 2011;39(1):89–98. doi: 10.1177/0363546510379975. [DOI] [PubMed] [Google Scholar]
- 97.Thompson S, Salmon L, Waller A, Linklater J, Roe J, Pinczewski L. Twenty-year outcomes of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon autografts. Am J Sports Med. 2015;43(9):2164–2174. doi: 10.1177/0363546515591263. [DOI] [PubMed] [Google Scholar]
- 98.Thompson SM, Salmon LJ, Waller A, Linklater J, Roe JP, Pinczewski LA. Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med. 2016;44(12):3083–3094. doi: 10.1177/0363546516658041. [DOI] [PubMed] [Google Scholar]
- 99.Kaeding CC, Aros B, Pedroza A, Pifel E, Amendola A, Andrish JT, Dunn WR, Marx RG, McCarty EC, Parker RD, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Hewett TE, Flanigan DC, Spindler KP. Change in anterior cruciate ligament graft choice and outcomes over time. Arthroscopy. 2017;33(11):2007–2014. doi: 10.1016/j.arthro.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mariscalco MW, Flanigan DC, Mitchell J, Pedroza AD, Jones MH, Andrish JT, Parker RD, Kaeding CC, Magnussen RA. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29(12):1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case–control study. Am J Sports Med. 2009;37(12):2362–2367. doi: 10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 104.Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- 105.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. doi: 10.1177/0363546516651845. [DOI] [PubMed] [Google Scholar]
- 106.Maletis GB, Inacio MC, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR Registry. Am J Sports Med. 2015;43(3):641–647. doi: 10.1177/0363546514561745. [DOI] [PubMed] [Google Scholar]
- 107.Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry. Am J Sports Med. 2016;44(2):331–336. doi: 10.1177/0363546515614813. [DOI] [PubMed] [Google Scholar]
- 108.Maletis GB, Inacio MC, Funahashi TT. Analysis of 16,192 anterior cruciate ligament reconstructions from a community-based registry. Am J Sports Med. 2013;41(9):2090–2098. doi: 10.1177/0363546513493589. [DOI] [PubMed] [Google Scholar]
- 109.Akhtar MA, Bhattacharya R, Keating JF. Generalised ligamentous laxity and revision ACL surgery: is there a relation? Knee. 2016;23(6):1148–1153. doi: 10.1016/j.knee.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 110.Akada T, Yamaura I, Gupta A, Sakai H, Takahashi K, Tsuchiya A. Partial meniscectomy adversely affects return-to-sport outcome after anatomical double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):912–920. doi: 10.1007/s00167-018-5213-y. [DOI] [PubMed] [Google Scholar]
- 111.Allen MM, Pareek A, Krych AJ, Hewett TE, Levy BA, Stuart MJ, Dahm DL. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. doi: 10.1177/0363546516648439. [DOI] [PubMed] [Google Scholar]
- 112.Barrett AM, Craft JA, Replogle WH, Hydrick JM, Barrett GR. Anterior cruciate ligament graft failure: a comparison of graft type based on age and Tegner activity level. Am J Sports Med. 2011;39(10):2194–2198. doi: 10.1177/0363546511415655. [DOI] [PubMed] [Google Scholar]
- 113.Benner RW, Shelbourne KD, Gray T. The degree of knee extension does not affect postoperative stability or subsequent graft tear rate after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2016;44(4):844–849. doi: 10.1177/0363546515623507. [DOI] [PubMed] [Google Scholar]
- 114.Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. doi: 10.1177/0363546512454414. [DOI] [PubMed] [Google Scholar]
- 115.Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–2514. doi: 10.1177/0363546515597664. [DOI] [PubMed] [Google Scholar]
- 116.Cooper DE, Dunn WR, Huston LJ, Haas AK, Spindler KP, Allen CR, Anderson AF, DeBerardino TM, Lantz BBA, Mann B, et al. Physiologic preoperative knee hyperextension is a predictor of failure in an anterior cruciate ligament revision cohort: a report from the MARS Group. Am J Sports Med. 2018;46(12):2836–2841. doi: 10.1177/0363546518777732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Digiacomo JE, Palmieri-Smith RM, Redman JA, III, Lepley LK. Examination of knee morphology after secondary ipsilateral ACL injury compared with those that have not been reinjured: a preliminary study. J Sport Rehabil. 2018;27(1):73–82. doi: 10.1123/jsr.2016-0093. [DOI] [PubMed] [Google Scholar]
- 118.Everhart JS, DiBartola AC, Swank K, Pettit R, Hughes L, Lewis C, Flanigan DC. Cartilage damage at the time of anterior cruciate ligament reconstruction is associated with weaker quadriceps function and lower risk of future ACL injury. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):576–583. doi: 10.1007/s00167-019-05739-1. [DOI] [PubMed] [Google Scholar]
- 119.Goshima K, Kitaoka K, Nakase J, Tsuchiya H. Familial predisposition to anterior cruciate ligament injury. Asia-Pac J Sports Med Arthrosc Rehabil Technol. 2014;1(2):62–66. [Google Scholar]
- 120.Grassi A, Macchiarola L, Lucidi GA, Stefanelli F, Neri M, Silvestri A, Della Villa F, Zaffagnini S. More than a 2-fold risk of contralateral anterior cruciate ligament injuries compared with ipsilateral graft failure 10 years after primary reconstruction. Am J Sports Med. 2020;48(2):310–317. doi: 10.1177/0363546519893711. [DOI] [PubMed] [Google Scholar]
- 121.Grassi A, Signorelli C, Urrizola F, Macchiarola L, Raggi F, Mosca M, Samuelsson K, Zaffagnini S. Patients with failed anterior cruciate ligament reconstruction have an increased posterior lateral Tibial Plateau slope: a case–controlled study. Arthroscopy. 2019;35(4):1172–1182. doi: 10.1016/j.arthro.2018.11.049. [DOI] [PubMed] [Google Scholar]
- 122.Henle P, Bieri KS, Brand M, Aghayev E, Bettfuehr J, Haeberli J, Kess M, Eggli S. Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1182–1189. doi: 10.1007/s00167-017-4574-y. [DOI] [PubMed] [Google Scholar]
- 123.Henle P, Bieri KS, Haeberli J, Arnout N, Victor J, Herbort M, Koesters C, Eggli S. Surgeon experience with dynamic intraligamentary stabilization does not influence risk of failure. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):2978–2985. doi: 10.1007/s00167-018-4847-0. [DOI] [PubMed] [Google Scholar]
- 124.Ifran NN, Mok YR, Krishna L. Tear rates of the ipsilateral ACL graft and the contralateral native ACL are similar following ACL reconstruction. J Knee Surg. 2022;35(3):308–311. doi: 10.1055/s-0040-1713861. [DOI] [PubMed] [Google Scholar]
- 125.Kajetanek C, Rousseau R, Makridis K, Sanchez M, Dehlin C, Djian P. Influence of the tibial slope on recurrent ACL ruptures. Journal de Traumatologie du Sport. 2017;34(1):37–43. doi: 10.1016/j.jts.2016.10.002. [DOI] [Google Scholar]
- 126.Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41(8):1808–1812. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 127.Kim SH, Park YB, Kim DH, Pujol N, Lee HJ. Predictive factors for failure of anterior cruciate ligament reconstruction via the trans-tibial technique. Arch Orthop Trauma Surg. 2020;140(10):1445–1457. doi: 10.1007/s00402-020-03483-7. [DOI] [PubMed] [Google Scholar]
- 128.King E, Richter C, Jackson M, Franklyn-Miller A, Falvey E, Myer GD, Strike S, Withers D, Moran R. Factors influencing return to play and second anterior cruciate ligament injury rates in level 1 athletes after primary anterior cruciate ligament reconstruction: 2-year follow-up on 1432 reconstructions at a single center. Am J Sports Med. 2020;48(4):812–824. doi: 10.1177/0363546519900170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Krismer AM, Gousopoulos L, Kohl S, Ateschrang A, Kohlhof H, Ahmad SS. Factors influencing the success of anterior cruciate ligament repair with dynamic intraligamentary stabilisation. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3923–3928. doi: 10.1007/s00167-017-4445-6. [DOI] [PubMed] [Google Scholar]
- 130.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 131.Laboute E, Savalli L, Puig P, Trouve P, Sabot G, Monnier G, Dubroca B. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med. 2010;53(10):598–614. doi: 10.1016/j.rehab.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 132.Larson CM, Bedi A, Dietrich ME, Swaringen JC, Wulf CA, Rowley DM, Giveans MR. Generalized hypermobility, knee hyperextension, and outcomes after anterior cruciate ligament reconstruction: prospective, case–control study with mean 6 years follow-up. Arthroscopy. 2017;33(10):1852–1858. doi: 10.1016/j.arthro.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 133.Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595–605. doi: 10.1177/0363546511430375. [DOI] [PubMed] [Google Scholar]
- 134.Lord L, Cristiani R, Edman G, Forssblad M, Stålman A. One sixth of primary anterior cruciate ligament reconstructions may undergo reoperation due to complications or new injuries within 2 years. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2478–2485. doi: 10.1007/s00167-020-06127-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 136.Mohtadi N, Chan D, Barber R, Paolucci EO. Reruptures, reinjuries, and revisions at a minimum 2-year follow-up: a randomized clinical trial comparing 3 graft types for ACL reconstruction. Clin J Sport Med. 2016;26(2):96–107. doi: 10.1097/JSM.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 137.Okoroha KR, Fidai MS, Tramer JS, Elmenini J, Makhni EC, Verma NN, Bach BR, Moutzouros V. Length of time between anterior cruciate ligament reconstruction and return to sport does not predict need for revision surgery in National Football League players. Arthroscopy. 2019;35(1):158–162. doi: 10.1016/j.arthro.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 138.Pfeiffer TR, Burnham JM, Hughes JD, Kanakamedala AC, Herbst E, Popchak A, Shafizadeh S, Irrgang JJ, Debski RE, Musahl V. An increased lateral femoral condyle ratio is a risk factor for anterior cruciate ligament injury. J Bone Jt Surg Am. 2018;100(10):857–864. doi: 10.2106/JBJS.17.01011. [DOI] [PubMed] [Google Scholar]
- 139.Poston GR, Schmitt LC, Ithurburn MP, Hugentobler JA, Thomas S, Paterno MV. Reduced 2-D frontal plane motion during single-limb landing is associated with risk of future anterior cruciate ligament graft rupture after anterior cruciate ligament reconstruction and return to sport: a pilot study. J Orthop Sports Phys Ther. 2021;51(2):82–87. doi: 10.2519/jospt.2021.9302. [DOI] [PubMed] [Google Scholar]
- 140.Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW. Rates of revision and surgeon-reported graft rupture following ACL reconstruction: early results from the New Zealand ACL Registry. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2194–2202. doi: 10.1007/s00167-019-05773-z. [DOI] [PubMed] [Google Scholar]
- 141.Riff AJ, Luchetti TJ, Weber AE, Chahal J, Bach BR., Jr Thirty-year experience with ACL reconstruction using patellar tendon: a critical evaluation of revision and reoperation. Orthop J Sports Med. 2017;5(8):2325967117724345. doi: 10.1177/2325967117724345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rosenstiel N, Praz C, Ouanezar H, Saithna A, Fournier Y, Hager JP, Thaunat M, Sonnery-Cottet B. Combined anterior cruciate and anterolateral ligament reconstruction in the professional athlete: clinical outcomes from the Scientific Anterior Cruciate Ligament Network International Study Group in a series of 70 patients with a minimum follow-up of 2 years. Arthroscopy. 2019;35(3):885–892. doi: 10.1016/j.arthro.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 143.Runer A, Csapo R, Hepperger C, Herbort M, Hoser C, Fink C. Anterior cruciate ligament reconstructions with quadriceps tendon autograft result in lower graft rupture rates but similar patient-reported outcomes as compared with hamstring tendon autograft: a comparison of 875 patients. Am J Sports Med. 2020;48(9):2195–2204. doi: 10.1177/0363546520931829. [DOI] [PubMed] [Google Scholar]
- 144.Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46(3):531–543. doi: 10.1177/0363546517741497. [DOI] [PubMed] [Google Scholar]
- 145.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 146.Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34(5):721–732. doi: 10.1177/0363546505282626. [DOI] [PubMed] [Google Scholar]
- 147.Sanders TL, Pareek A, Hewett TE, Levy BA, Dahm DL, Stuart MJ, Krych AJ. Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):222–228. doi: 10.1007/s00167-016-4275-y. [DOI] [PubMed] [Google Scholar]
- 148.Sauer S, English R, Clatworthy M. The influence of tibial slope on anterior cruciate ligament graft failure risk is dependent on graft positioning. J Orthop Surg (Hong Kong) 2019;27(1):2309499019834674. doi: 10.1177/2309499019834674. [DOI] [PubMed] [Google Scholar]
- 149.Schlumberger M, Schuster P, Schulz M, Immendörfer M, Mayer P, Bartholomä J, Richter J. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1535–1541. doi: 10.1007/s00167-015-3699-0. [DOI] [PubMed] [Google Scholar]
- 150.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 151.Singhal MC, Gardiner JR, Johnson DL. Failure of primary anterior cruciate ligament surgery using anterior tibialis allograft. Arthroscopy. 2007;23(5):469–475. doi: 10.1016/j.arthro.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 152.Sousa PL, Krych AJ, Cates RA, Levy BA, Stuart MJ, Dahm DL. Return to sport: does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1356–1363. doi: 10.1007/s00167-015-3697-2. [DOI] [PubMed] [Google Scholar]
- 153.Su AW, Bogunovic L, Smith MV, Gortz S, Brophy RH, Wright RW, Matava MJ. Medial tibial slope determined by plain radiography is not associated with primary or recurrent anterior cruciate ligament tears. J Knee Surg. 2020;33(1):22–28. doi: 10.1055/s-0038-1676456. [DOI] [PubMed] [Google Scholar]
- 154.van Eck CF, Schkrohowsky JG, Working ZM, Irrgang JJ, Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40(4):800–807. doi: 10.1177/0363546511432545. [DOI] [PubMed] [Google Scholar]
- 155.Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N, Ogilvie-Harris D. Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med. 2013;41(9):2099–2107. doi: 10.1177/0363546513493580. [DOI] [PubMed] [Google Scholar]
- 156.Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. doi: 10.1177/0363546513503288. [DOI] [PubMed] [Google Scholar]
- 157.Welling W, Benjaminse A, Lemmink K, Gokeler A. Passing return to sports tests after ACL reconstruction is associated with greater likelihood for return to sport but fail to identify second injury risk. Knee. 2020;27(3):949–957. doi: 10.1016/j.knee.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 158.Webster KE, Feller JA. Clinical tests can be used to screen for second anterior cruciate ligament injury in younger patients who return to sport. Orthop J Sports Med. 2019;7(8):2325967119863003. doi: 10.1177/2325967119863003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 160.Yabroudi MA, Björnsson H, Lynch AD, Muller B, Samuelsson K, Tarabichi M, Karlsson J, Fu FH, Harner CD, Irrgang JJ. Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop J Sports Med. 2016;4(9):2325967116666039. doi: 10.1177/2325967116666039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vincent YP-H, Yiu-Chung W, Patrick YS-H. Role of physiotherapy in preventing failure of primary anterior cruciate ligament reconstruction. J Orthop Trauma Rehabil. 2017;22(1):6–12. [Google Scholar]
- 162.Borton ZM, Yasen SK, Mumith A, Wilson AJ. Mid-bundle positioning of the femoral socket increases graft rupture in anatomic single bundle anterior cruciate ligament reconstruction. Knee. 2018;25(6):1122–1128. doi: 10.1016/j.knee.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 163.Lee BH, Jangir R, Kim HY, Shin JM, Chang M, Kim K, Wang JH. Comparison of anterior cruciate ligament volume after anatomic double-bundle anterior cruciate ligament reconstruction. Knee. 2017;24(3):580–587. doi: 10.1016/j.knee.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 164.Lee CC, Youm YS, Cho SD, Jung SH, Bae MH, Park SJ, Kim HW. Does posterior tibial slope affect graft rupture following anterior cruciate ligament reconstruction? Arthroscopy. 2018;34(7):2152–2155. doi: 10.1016/j.arthro.2018.01.058. [DOI] [PubMed] [Google Scholar]
- 165.Pullen WM, Bryant B, Gaskill T, Sicignano N, Evans AM, DeMaio M. Predictors of revision surgery after anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(12):3140–3145. doi: 10.1177/0363546516660062. [DOI] [PubMed] [Google Scholar]
- 166.Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am J Sports Med. 1998;26(3):402–408. doi: 10.1177/03635465980260031001. [DOI] [PubMed] [Google Scholar]
- 167.Tulloch SJ, Devitt BM, Porter T, Hartwig T, Klemm H, Hookway S, Norsworthy CJ. Primary ACL reconstruction using the LARS device is associated with a high failure rate at minimum of 6-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3626–3632. doi: 10.1007/s00167-019-05478-3. [DOI] [PubMed] [Google Scholar]
- 168.Bayomy AF, Bompadre V, Schmale GA. The impact of transphyseal anterior cruciate ligament reconstruction on lower extremity growth and alignment. Arthroscopy. 2019;35(3):940–949. doi: 10.1016/j.arthro.2018.10.132. [DOI] [PubMed] [Google Scholar]
- 169.Bram JT, Pascual-Leone N, Patel NM, DeFrancesco CJ, Talathi NS, Ganley TJ. Do pediatric patients with anterior cruciate ligament tears have a higher rate of familial anterior cruciate ligament injury? Orthop J Sports Med. 2020;8(10):2325967120959665. doi: 10.1177/2325967120959665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Britt E, Ouillette R, Edmonds E, Chambers H, Johnson K, Bastrom T, Pennock A. The challenges of treating female soccer players with ACL injuries: hamstring versus bone-patellar tendon-bone autograft. Orthop J Sports Med. 2020;8(11):2325967120964884. doi: 10.1177/2325967120964884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cruz AI, Jr, Fabricant PD, McGraw M, Rozell JC, Ganley TJ, Wells L. All-epiphyseal ACL reconstruction in children: review of safety and early complications. J Pediatr Orthop. 2017;37(3):204–209. doi: 10.1097/BPO.0000000000000606. [DOI] [PubMed] [Google Scholar]
- 172.Ellis HB, Matheny LM, Briggs KK, Pennock AT, Steadman JR. Outcomes and revision rate after bone-patellar tendon-bone allograft versus autograft anterior cruciate ligament reconstruction in patients aged 18 years or younger with closed physes. Arthroscopy. 2012;28(12):1819–1825. doi: 10.1016/j.arthro.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 173.Engelman GH, Carry PM, Hitt KG, Polousky JD, Vidal AF. Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014;42(10):2311–2318. doi: 10.1177/0363546514541935. [DOI] [PubMed] [Google Scholar]
- 174.Ghosh K, Salmon LJ, Heath E, Pinczewski LA, Roe JP. Transphyseal anterior cruciate ligament reconstruction using living parental donor hamstring graft: excellent clinical results at 2 years in a cohort of 100 patients. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2511–2518. doi: 10.1007/s00167-019-05842-3. [DOI] [PubMed] [Google Scholar]
- 175.Grassi A, Pizza N, Zambon Bertoja J, Macchiarola L, Lucidi GA, Dal Fabbro G, Zaffagnini S. Higher risk of contralateral anterior cruciate ligament (ACL) injury within 2 years after ACL reconstruction in under-18-year-old patients with steep tibial plateau slope. Knee Surg Sports Traumatol Arthrosc. 2021;29(6):1690–1700. doi: 10.1007/s00167-020-06195-y. [DOI] [PubMed] [Google Scholar]
- 176.Graziano J, Chiaia T, de Mille P, Nawabi DH, Green DW, Cordasco FA. Return to sport for skeletally immature athletes after ACL reconstruction: preventing a second injury using a quality of movement assessment and quantitative measures to address modifiable risk factors. Orthop J Sports Med. 2017;5(4):2325967117700599. doi: 10.1177/2325967117700599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Heath EL, Salmon LJ, Cooper R, Pappas E, Roe JP, Pinczewski LA. 5-year survival of pediatric anterior cruciate ligament reconstruction with living donor hamstring tendon grafts. Am J Sports Med. 2019;47(1):41–51. doi: 10.1177/0363546518804502. [DOI] [PubMed] [Google Scholar]
- 178.Ho B, Edmonds EW, Chambers HG, Bastrom TP, Pennock AT. Risk factors for early ACL reconstruction failure in pediatric and adolescent patients: a review of 561 cases. J Pediatr Orthop. 2018;38(7):388–392. doi: 10.1097/BPO.0000000000000831. [DOI] [PubMed] [Google Scholar]
- 179.Larson CM, Heikes CS, Ellingson CI, Wulf CA, Giveans MR, Stone RM, Bedi A. Allograft and autograft transphyseal anterior cruciate ligament reconstruction in skeletally immature patients: outcomes and complications. Arthroscopy. 2016;32(5):860–867. doi: 10.1016/j.arthro.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 180.Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44(2):384–392. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- 181.Perkins CA, Busch MT, Christino M, Herzog MM, Willimon SC. Allograft augmentation of hamstring anterior cruciate ligament autografts is associated with increased graft failure in children and adolescents. Am J Sports Med. 2019;47(7):1576–1582. doi: 10.1177/0363546519849607. [DOI] [PubMed] [Google Scholar]
- 182.Ranade SC, Refakis CA, Cruz AI, Jr, Leddy KL, Wells L, Lawrence JT, Ganley TJ. Validated pediatric functional outcomes of all-epiphyseal ACL reconstructions: does reinjury affect outcomes? J Pediatr Orthop. 2020;40(4):157–161. doi: 10.1097/BPO.0000000000001217. [DOI] [PubMed] [Google Scholar]
- 183.Schmale GA, Kweon C, Larson RV, Bompadre V. High satisfaction yet decreased activity 4 years after transphyseal ACL reconstruction. Clin Orthop Relat Res. 2014;472(7):2168–2174. doi: 10.1007/s11999-014-3561-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Wall EJ, Ghattas PJ, Eismann EA, Myer GD, Carr P. Outcomes and complications after all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Orthop J Sports Med. 2017;5(3):2325967117693604. doi: 10.1177/2325967117693604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Gagliardi AG, Carry PM, Parikh HB, Traver JL, Howell DR, Albright JC. ACL repair with suture ligament augmentation is associated with a high failure rate among adolescent patients. Am J Sports Med. 2019;47(3):560–566. doi: 10.1177/0363546518825255. [DOI] [PubMed] [Google Scholar]
- 186.Gans I, Retzky JS, Jones LC, Tanaka MJ. Epidemiology of recurrent anterior cruciate ligament injuries in National Collegiate Athletic Association Sports: the Injury Surveillance Program, 2004–2014. Orthop J Sports Med. 2018;6(6):2325967118777823. doi: 10.1177/2325967118777823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Gonçalves H, Steltzlen C, Boisrenoult P, Beaufils P, Pujol N. High failure rate of anterior cruciate ligament reconstruction with bimeniscal repair: a case–control study. Orthop Traumatol Surg Res. 2017;103(6):943–946. doi: 10.1016/j.otsr.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 188.Lai CCH, Feller JA, Webster KE. Fifteen-year audit of anterior cruciate ligament reconstructions in the Australian Football League from 1999 to 2013: return to play and subsequent ACL injury. Am J Sports Med. 2018;46(14):3353–3360. doi: 10.1177/0363546518803932. [DOI] [PubMed] [Google Scholar]
- 189.Levins JG, Sturnick DR, Argentieri EC, Gardner-Morse M, Vacek PM, Desarno MJ, Tourville TW, Slauterbeck JR, Beynnon BD. Geometric risk factors associated with noncontact anterior cruciate ligament graft rupture. Am J Sports Med. 2016;44(10):2537–2545. doi: 10.1177/0363546516657525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP, Amendola A, Andrish JT, Brophy RH, Dunn WR, Flanigan DC, et al. Effect of high-grade preoperative knee laxity on 6-year anterior cruciate ligament reconstruction outcomes. Am J Sports Med. 2018;46(12):2865–2872. doi: 10.1177/0363546518793881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Patel NM, Talathi NS, Bram JT, DeFrancesco CJ, Ganley TJ. How does obesity impact pediatric anterior cruciate ligament reconstruction? Arthroscopy. 2019;35(1):130–135. doi: 10.1016/j.arthro.2018.07.044. [DOI] [PubMed] [Google Scholar]
- 192.Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2018;10(3):228–233. doi: 10.1177/1941738117745806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med. 2017;45(7):1547–1557. doi: 10.1177/0363546516686057. [DOI] [PubMed] [Google Scholar]
- 194.DeFrancesco CJ, Striano BM, Bram JT, Baldwin KD, Ganley TJ. An in-depth analysis of graft rupture and contralateral anterior cruciate ligament rupture rates after pediatric anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48(10):2395–2400. doi: 10.1177/0363546520935437. [DOI] [PubMed] [Google Scholar]
- 195.Kinsella SD, Rider SM, Fury MS, Tepolt FA, Ecklund K, Kocher MS. Concomitant posterolateral corner injuries in skeletally immature patients with acute anterior cruciate ligament injuries. J Pediatr Orthop. 2020;40(6):271–276. doi: 10.1097/BPO.0000000000001450. [DOI] [PubMed] [Google Scholar]
- 196.Della Villa F, Hägglund M, Della Villa S, Ekstrand J, Waldén M. High rate of second ACL injury following ACL reconstruction in male professional footballers: an updated longitudinal analysis from 118 players in the UEFA Elite Club Injury Study. Br J Sports Med. 2021;55:1379–1380. doi: 10.1136/bjsports-2021-104508. [DOI] [PubMed] [Google Scholar]
- 197.Lee DW, Lee JK, Kwon SH, Moon SG, Cho SI, Chung SH, Kim JG. Adolescents show a lower healing rate of anterolateral ligament injury and a higher rotational laxity than adults after anterior cruciate ligament reconstruction. Knee. 2021;30:113–124. doi: 10.1016/j.knee.2021.03.020. [DOI] [PubMed] [Google Scholar]
- 198.Webster KE, Murgier J, Feller JA, Klemm HJ, Devitt BM, Whitehead TS. Preservation of the tibial stump during anterior cruciate ligament reconstruction surgery did not increase the rate of surgery for symptomatic cyclops lesions. Orthop J Sports Med. 2021;9(4):2325967121992517. doi: 10.1177/2325967121992517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Webster KE, Feller JA, Klemm HJ. Second ACL injury rates in younger athletes who were advised to delay return to sport until 12 months after ACL reconstruction. Orthop J Sports Med. 2021;9(2):2325967120985636. doi: 10.1177/2325967120985636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Rauck RC, Apostolakos JM, Nwachukwu BU, Schneider BL, Williams RJ, 3rd, Dines JS, Altchek DW, Pearle A, Allen A, Stein BS, et al. Return to sport after bone-patellar tendon-bone autograft ACL reconstruction in high school-aged athletes. Orthop J Sports Med. 2021;9(6):23259671211011510. doi: 10.1177/23259671211011510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Csapo R, Runer A, Hoser C, Fink C. Contralateral ACL tears strongly contribute to high rates of secondary ACL injuries in professional ski racers. Knee Surg Sports Traumatol Arthrosc. 2021;29(6):1805–1812. doi: 10.1007/s00167-020-06234-8. [DOI] [PubMed] [Google Scholar]
- 202.Mitchell BC, Siow MY, Bastrom T, Bomar JD, Pennock AT, Parvaresh K, Edmonds EW. Predictive value of the magnetic resonance imaging-based coronal lateral collateral ligament sign on adolescent anterior cruciate ligament reconstruction graft failure. Am J Sports Med. 2021;49(4):935–940. doi: 10.1177/0363546521988939. [DOI] [PubMed] [Google Scholar]
- 203.King E, Richter C, Daniels KAJ, Franklyn-Miller A, Falvey E, Myer GD, Jackson M, Moran R, Strike S. Biomechanical but not strength or performance measures differentiate male athletes who experience ACL reinjury on return to level 1 sports. Am J Sports Med. 2021;49(4):918–927. doi: 10.1177/0363546520988018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bodkin SG, Hertel J, Diduch DR, Saliba SA, Novicoff WM, Brockmeier SF, Miller MD, Gwathmey FW, Werner BC, Hart JM. Predicting ACL reinjury from return to activity assessments at 6-months post-surgery: a prospective cohort study. J Athl Train. 2021 doi: 10.4085/1062-6050-0407.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Jaecker V, Drouven S, Naendrup JH, Kanakamedala AC, Pfeiffer T, Shafizadeh S. Increased medial and lateral tibial posterior slopes are independent risk factors for graft failure following ACL reconstruction. Arch Orthop Trauma Surg. 2018;138(10):1423–1431. doi: 10.1007/s00402-018-2968-z. [DOI] [PubMed] [Google Scholar]
- 206.Weir A, Rabia S, Ardern C. Trusting systematic reviews and meta-analyses: all that glitters is not gold! Br J Sports Med. 2016;50(18):1100–1101. doi: 10.1136/bjsports-2015-095896. [DOI] [PubMed] [Google Scholar]
- 207.Klasan A, Putnis SE, Grasso S, Kandhari V, Oshima T, Parker DA. Tegner level is predictive for successful return to sport 2 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020. [DOI] [PMC free article] [PubMed]
- 208.Letchford R, Button K, Sparkes V, van Deursen RWM. Assessing activity participation in the ACL injured population: a systematic review of activity rating scale measurement properties. Phys Therapy Rev. 2012;17(2):99–109. doi: 10.1179/1743288X11Y.0000000053. [DOI] [Google Scholar]
- 209.Quatman-Yates CC, Quatman CE, Meszaros AJ, Paterno MV, Hewett TE. A systematic review of sensorimotor function during adolescence: a developmental stage of increased motor awkwardness? Br J Sports Med. 2012;46(9):649–655. doi: 10.1136/bjsm.2010.079616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Shultz SJ, Nguyen AD, Schmitz RJ. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38(3):137–149. doi: 10.2519/jospt.2008.2645. [DOI] [PubMed] [Google Scholar]
- 211.Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1966–1974. doi: 10.1007/s00167-017-4747-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Hägglund M, Waldén M. Risk factors for acute knee injury in female youth football. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):737–746. doi: 10.1007/s00167-015-3922-z. [DOI] [PubMed] [Google Scholar]
- 213.John R, Dhillon MS, Sharma S, Prabhakar S, Bhandari M. Is there a genetic predisposition to anterior cruciate ligament tear? A systematic review. Am J Sports Med. 2016;44(12):3262–3269. doi: 10.1177/0363546515624467. [DOI] [PubMed] [Google Scholar]
- 214.Hewett TE, Lynch TR, Myer GD, Ford KR, Gwin RC, Heidt RS., Jr Multiple risk factors related to familial predisposition to anterior cruciate ligament injury: fraternal twin sisters with anterior cruciate ligament ruptures. Br J Sports Med. 2010;44(12):848–855. doi: 10.1136/bjsm.2008.055798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Wordeman SC, Quatman CE, Kaeding CC, Hewett TE. In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med. 2012;40(7):1673–1681. doi: 10.1177/0363546512442307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.McLean SG, Lucey SM, Rohrer S, Brandon C. Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech (Bristol, Avon) 2010;25(8):781–788. doi: 10.1016/j.clinbiomech.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 217.Shultz SJ, Schmitz RJ. Tibial plateau geometry influences lower extremity biomechanics during landing. Am J Sports Med. 2012;40(9):2029–2036. doi: 10.1177/0363546512453295. [DOI] [PubMed] [Google Scholar]
- 218.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case–control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. doi: 10.1016/j.jbiomech.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29(2):223–231. doi: 10.1002/jor.21242. [DOI] [PubMed] [Google Scholar]
- 220.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Jt Surg Br. 1994;76(5):745–749. doi: 10.1302/0301-620X.76B5.8083263. [DOI] [PubMed] [Google Scholar]
- 221.de Valk EJ, Moen MH, Winters M, Bakker EW, Tamminga R, van der Hoeven H. Preoperative patient and injury factors of successful rehabilitation after anterior cruciate ligament reconstruction with single-bundle techniques. Arthroscopy. 2013;29(11):1879–1895. doi: 10.1016/j.arthro.2013.07.273. [DOI] [PubMed] [Google Scholar]
- 222.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31(2):210–215. doi: 10.1097/00005768-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 223.Thoma LM, Grindem H, Logerstedt D, Axe M, Engebretsen L, Risberg MA, Snyder-Mackler L. Coper classification early after anterior cruciate ligament rupture changes with progressive neuromuscular and strength training and is associated with 2-year success: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2019;47(4):807–814. doi: 10.1177/0363546519825500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Filardo G, de Caro F, Andriolo L, Kon E, Zaffagnini S, Marcacci M. Do cartilage lesions affect the clinical outcome of anterior cruciate ligament reconstruction? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3061–3075. doi: 10.1007/s00167-016-4097-y. [DOI] [PubMed] [Google Scholar]
- 225.Cinque ME, Chahla J, Mitchell JJ, Moatshe G, Pogorzelski J, Murphy CP, Kennedy NI, Godin JA, LaPrade RF. Influence of meniscal and chondral lesions on patient-reported outcomes after primary anterior cruciate ligament reconstruction at 2-year follow-up. Orthop J Sports Med. 2018;6(2):2325967117754189. doi: 10.1177/2325967117754189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, Wright RW, Kaeding CC, Marx RG, Amendola A, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42(5):1058–1067. doi: 10.1177/0363546514525910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Deitch JR, Starkey C, Walters SL, Moseley JB. Injury risk in professional basketball players: a comparison of Women's National Basketball Association and National Basketball Association athletes. Am J Sports Med. 2006;34(7):1077–1083. doi: 10.1177/0363546505285383. [DOI] [PubMed] [Google Scholar]
- 228.Stanley LE, Kerr ZY, Dompier TP, Padua DA. Sex differences in the incidence of anterior cruciate ligament, medial collateral ligament, and meniscal injuries in Collegiate and High School sports: 2009–2010 through 2013–2014. Am J Sports Med. 2016;44(6):1565–1572. doi: 10.1177/0363546516630927. [DOI] [PubMed] [Google Scholar]
- 229.Montalvo AM, Schneider DK, Yut L, Webster KE, Beynnon B, Kocher MS, Myer GD. "What's my risk of sustaining an ACL injury while playing sports?" A systematic review with meta-analysis. Br J Sports Med. 2019;53(16):1003–1012. doi: 10.1136/bjsports-2016-096274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320–1325 e1326. doi: 10.1016/j.arthro.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 231.Herzberg SD, Motu'apuaka ML, Lambert W, Fu R, Brady J, Guise JM. The effect of menstrual cycle and contraceptives on ACL injuries and laxity: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5(7):2325967117718781. doi: 10.1177/2325967117718781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45(2):488–494. doi: 10.1177/0363546516638079. [DOI] [PubMed] [Google Scholar]
- 233.Ashigbi EYK, Banzer W, Niederer D. Return to sport tests' prognostic value for reinjury risk after anterior cruciate ligament reconstruction: a systematic review. Med Sci Sports Exerc. 2020;52(6):1263–1271. doi: 10.1249/MSS.0000000000002246. [DOI] [PubMed] [Google Scholar]
- 234.Brewer BW, Cornelius AE, Sklar JH, Van Raalte JL, Tennen H, Armeli S, Corsetti JR, Brickner JC. Pain and negative mood during rehabilitation after anterior cruciate ligament reconstruction: a daily process analysis. Scand J Med Sci Sports. 2007;17(5):520–529. doi: 10.1111/j.1600-0838.2006.00601.x. [DOI] [PubMed] [Google Scholar]
- 235.Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):752–762. doi: 10.1007/s00167-013-2699-1. [DOI] [PubMed] [Google Scholar]
- 236.Clement D, Arvinen-Barrow M, Fetty T. Psychosocial responses during different phases of sport-injury rehabilitation: a qualitative study. J Athl Train. 2015;50(1):95–104. doi: 10.4085/1062-6050-49.3.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Nwachukwu BU, Adjei J, Rauck RC, Chahla J, Okoroha KR, Verma NN, Allen AA, Williams RJ., 3rd How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sports Med. 2019;7(5):2325967119845313. doi: 10.1177/2325967119845313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 239.Cronström A, Creaby MW, Ageberg E. Do knee abduction kinematics and kinetics predict future anterior cruciate ligament injury risk? A systematic review and meta-analysis of prospective studies. BMC Musculoskelet Disord. 2020;21(1):563. doi: 10.1186/s12891-020-03552-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Nilstad A, Petushek E, Mok KM, Bahr R, Krosshaug T. Kiss goodbye to the 'kissing knees': no association between frontal plane inward knee motion and risk of future non-contact ACL injury in elite female athletes. Sports Biomech. 2021:1–15. [DOI] [PubMed]
- 241.Gwynne CR, Curran SA. Quantifying frontal plane knee motion during single limb squats: reliability and validity of 2-dimensional measures. Int J Sports Phys Ther. 2014;9(7):898–906. [PMC free article] [PubMed] [Google Scholar]
- 242.McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med. 2005;39(6):355–362. doi: 10.1136/bjsm.2005.018598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Sorenson B, Kernozek TW, Willson JD, Ragan R, Hove J. Two- and three-dimensional relationships between knee and hip kinematic motion analysis: single-leg drop-jump landings. J Sport Rehabil. 2015;24(4):363–372. doi: 10.1123/jsr.2014-0206. [DOI] [PubMed] [Google Scholar]
- 244.Atkin K. The relationship between 2D knee valgus angle during single leg squat (SLS), single leg landing (SLL), and forward running. Br J Sports Med. 2017;26:72–77. [Google Scholar]
- 245.Donohue MR, Ellis SM, Heinbaugh EM, Stephenson ML, Zhu Q, Dai B. Differences and correlations in knee and hip mechanics during single-leg landing, single-leg squat, double-leg landing, and double-leg squat tasks. Res Sports Med. 2015;23(4):394–411. doi: 10.1080/15438627.2015.1076413. [DOI] [PubMed] [Google Scholar]
- 246.Ohji S, Aizawa J, Hirohata K, Mitomo S, Ohmi T, Jinno T, Koga H, Yagishita K. Athletic identity and sport commitment in athletes after anterior cruciate ligament reconstruction who have returned to sports at their pre-injury level of competition. BMC Sports Sci Med Rehabil. 2021;13(1):37. doi: 10.1186/s13102-021-00264-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Brewer BW, Cornelius AE. Self-protective changes in athletic identity following anterior cruciate ligament reconstruction. Psychol Sport Exerc. 2010;11(1):1–5. doi: 10.1016/j.psychsport.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Scott SM, Perry MA, Sole G. "Not always a straight path": patients' perspectives following anterior cruciate ligament rupture and reconstruction. Disabil Rehabil. 2018;40(19):2311–2317. doi: 10.1080/09638288.2017.1335803. [DOI] [PubMed] [Google Scholar]
- 249.Filbay S, Pandya T, Thomas B, McKay C, Adams J, Arden N. Quality of life and life satisfaction in former athletes: a systematic review and meta-analysis. Sports Med. 2019;49(11):1723–1738. doi: 10.1007/s40279-019-01163-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Athletes’ Rights and Responsibilities Declaration. https://www.coe.int/en/web/sport/-/ioc-athletes-rights-and-responsibilities-declaration-2018.
- 251.Goetz G, de Villiers C, Sadoghi P, Geiger-Gritsch S. Allograft for anterior cruciate ligament reconstruction (ACLR): a systematic review and meta-analysis of long-term comparative effectiveness and safety results of a health technology assessment. Arthrosc Sports Med Rehabil. 2020;2(6):e873–e891. doi: 10.1016/j.asmr.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. doi: 10.1007/s11999-017-5278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:35. doi: 10.1186/s12874-015-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Montreuil B, Bendavid Y, Brophy J. What is so odd about odds? Can J Surg. 2005;48(5):400–408. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.