Abstract
One of the most challenging esthetic concerns in dentistry is conservative replacement of the missing anterior teeth. Although implants are considered to be a better treatment option for rehabilitation of such patients, resin-bonded bridges (RBBs) can conservatively restore the missing teeth and have thus gained popularity over the years. It consists of an artificial tooth with a wing-like extension that is cemented to the adjacent teeth. There are various types of RBBs among which Maryland bridge is the simplest and the popular most due to its micromechanical retention enabled by acid etching of both tooth and metal retainer. It can be fabricated by various techniques and materials. In this case reports, we have discussed about two unique designs of Maryland bridge fabricated by two different materials (Porcelain-fused metal and Graphene) and utilizing two different techniques (conventional and digital).
Keywords: Computer-Aided Designing and Computer-Aided Manufacturing, Graphene, Maryland bridge, Resin cements, Resin-bonded bridge
INTRODUCTION
A conventional fixed partial denture is the most common method for replacement of missing anterior teeth. However, it often produces pulpal stress on abutment teeth and usually not indicated for young patients. Implants though considered to be the better treatment option, but they are not feasible in every clinical situation due to high cost. Thus, in such cases, resin-bonded bridges (RBBs) are considered to be a better treatment option. It can be used as a permanent as well as an intermediate prosthesis while planning for implants and fixed partial denture.[1]
RBBs have micromechanical bonding with the tooth surface and the metal alloy surface and it requires minimal or no tooth reduction. Various types of RBBs are Rochette bridge, Virginia bridge, and Maryland bridge, among which Maryland bridge is commonly used.[2]
The requirement for tooth preparation for RBBs is debatable. Previously, more comprehensive preparations were utilized to improve retention. However, most practitioners now recommend minimum preparation, within enamel, or no preparation at all.[3] The tooth preparation is usually intra enamel involving the lingual surface of the abutment teeth. It extends 1 mm before the contact area and the incisal edge of the tooth with a shoulder finish line. These bridges are fabricated by using nonprecious alloys, as these alloys allow electrochemical etching to provide micromechanical retention.[4,5]
Various techniques available for fabrication of Maryland bridge are conventional casting, computer-aided designing and computer-aided manufacturing (CAD-CAM) and 3D printing. The materials used are metal, porcelain-fused metal, ceramics, more recently zirconia and graphene. The present case reports discus the conventional and digital technique for the fabrication of Maryland bridge for the replacement of missing anterior maxillary teeth.
CASE REPORTS
Case examination1
A 25-year-old female patient reported with chief complaint of unesthetic smile due to missing tooth in upper front teeth region for 6 months. History revealed that the patient had grossly decayed maxillary left central incisor, for which she underwent root canal treatment in 2018. She got the same tooth extracted 6 months back due to fracture of the coronal structure that could not be restored. There was no relevant medical history was given by the patient. Extraoral examination revealed no abnormalities. Intraoral examination revealed missing maxillary left central incisor (21) with moderate generalized fluorosis (according to dean fluorosis index) [Figure 1a, c and e]. The edentulous site was 8 mm mesiodistally, 7 mm buccolingually and 12 mm gingivaocclusally. Class 1 occlusion with overjet and overbite of 1 mm was noted.
Figure 1.

(a, c and e) Case 1 (prerehabilitative view, inter-arch relation, maxillary intraoral view), (b, d, and f) Case 2 (prerehabilitative view, inter-arch relation, maxillary intraoral view.
Case examination 2
A 23-year-old female reported with a chief complaint of unpleasant smile due to missing teeth in upper front tooth region since a year. Patient gave a history of trauma 2 years back in which her maxillary left lateral incisor got fractured and she got the same tooth extracted after 6 months of trauma. No relevant medical history was given by the patient. No extraoral abnormalities were noted. Intraoral examination revealed maxillary left lateral incisor (22) with mild generalized fluorosis (according to dean fluorosis index) [Figure 1b, d and f]. The edentulous site was measured 7 mm mesiodistally, 9 mm buccolingually and 11 mm gingivaocclusally. Class 1 occlusion with overjet and overbite of 2 mm was noted.
Treatment plan
Various treatment options such as fixed dental prosthesis, implant retained prosthesis, and removable partial dentures, were explained to the patient but later excluded due to various reasons such as patient desire for fixed restoration, extensive tooth preparation, and high cost. Considering the patient's age and financial status, a RBB (Maryland bridge) was planned and explained to the patient. For Case 1, a porcelain-fused-to-metal hybrid Maryland bridge was planned and fabricated by conventional casting technique. For Case 2, a graphene Maryland bridge was fabricated by CAD/CAM technique.
Treatment progress
Case 1
Diagnostic impression was made using irreversible hydrocolloid (Algitex Alginate Impression Material-Dental Product of India) [Figure 2a and b]. The diagnostic cast was poured using Type III gypsum product (Ultrastone dental stone; Kalabhai Karson Pvt. Ltd.) [Figure 2c and d]. Maxillary and mandibular cast was mounted on a mean value articulator [Figure 2e and f]. The diagnostic wax-up was done for missing teeth after arbitrary preparation of abutment teeth on the cast. The putty index was made over the same for fabrication of provisional restoration [Figure 3a]. Since it is a hybrid Maryland bridge, full veneer preparation of maxillary left lateral incisor and lingual window preparation of maxillary right central incisor was carried out in patient's mouth [Figure 3b]. The final impression was made using addition silicone putty and light body (LB) elastomeric impression material (Avue Gum Putty and LB: Hydrophilic Vinyl Polysiloxane Impression Material) [Figure 3c]. The master cast was poured using Type IV gypsum product (Kalabhai Kalrock Diestone: Dental Stone Class IV). The provisional restoration was fabricated using the tooth colored cold cure resin (PYRAX® High Quality Cold Cure SC-10 Temporary Acrylic Crown and Bridge Material) using direct technique. After polymerization, adequate trimming and polishing was done and provisional restoration was cemented using temporary luting material (Ammdent Temp-Ting Temporary Luting Material) [Figure 3d].
Figure 2.
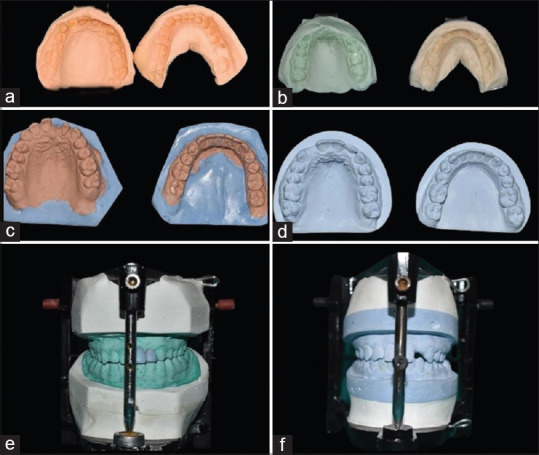
(a, c, and e) Case 1 (diagnostic impression and cast, maxillary and mandibular cast mounted in an articulator), (b, d, and f) Case 2 (diagnostic impression and cast, maxillary and mandibular cast mounted in an articulator).
Figure 3.

(a) Putty index, (b) Tooth preparation (full veneer preparation in 22 and lingual window preparation in 11), (c) Final impression, (d) Provisional restoration (e). Metal try in (f). Final prosthesis after porcelain firing and glazing.
The wax pattern was prepared using inlay wax over the die cast. It was removed carefully from the die, then sprue wax was attached followed by investing it in the casting ring. The conventional de-waxing and casting procedure was done in an induction casting machine followed by finishing of metal coping. The metal try in was carried out in the patient's mouth [Figure 3e] after which the conventional porcelain layering, firing, glazing, finishing, and polishing was done [Figure 3f]. The final prosthesis was evaluated for marginal fit and occlusion, initially on cast and then in patient's mouth [Figure 4a-c]. After necessary corrections were made, the tooth and prosthesis was acid etched using 37% phosphoric acid and hydrofluoric acid, respectively. The bonding agent was applied and the prosthesis was cemented using dual cure resin cement (Dental avenue Avue nano core dual) and cured using light curing unit [Figure 4d].
Figure 4.

(a) Final prosthesis in master cast (b) Final prosthesis in situ, (c) Final prosthesis in situ (occlusal view) (d) Postrehabilitative view.
Case 2
The diagnostic impression, cast, articulation, and wax-up were done same as Case 1. The lingual window preparation was done in maxillary left central incisor and canine, followed by final impression and fabrication of master cast same as in Case 1 [Figure 5d]. Provisional restoration was fabricated using flowable composite resin (Nexocomp Flow – Nano-Hybrid Flowable Composite resin). The putty index was made with clear heavy body elastomeric material (Poly Vinyl Silicone Clear LB – ChemiSil [Korean]) which allows blue curing light to pass through the material [Figure 5a]. An injecting tip was attached to the putty index for injecting the composite material [Figure 5b]. The putty index was placed in the patient's mouth and flowable composite was injected using the tip attached and was light cured [Figure 5c-f].
Figure 5.

(a) Putty index cut in the middle to replace with Chemi-sil, (b) Chemi-sil application (c) Provisional restoration composite material, (d) Tooth preparation (window preparation in 21 and 23), (e) Injecting the flowable composite after placing putty index in prepared tooth, (f) Provisional restoration.
In laboratory, the master cast was scanned using Dentsply Sirona – in Eos X5 scanner (Dentsply Sirona Global headquarters, Charlotte, NC 28277, USA) and after that designing was done using EXOCAD software (exocad GmbH, Darmstadt, Germany) [Figure 6a]. Utilizing CAD technology, the preparations were delineated and the pontic was designed [Figure 6b and c]. Thereafter, grapheme-based polymer disc (G-CAM Disc) was incorporated and the prosthesis was dry milled in Dentsply Sirona-inLab MC X5 milling machine (Dentsply Sirona Global headquarters, Charlotte, NC 28277, USA) [Figure 6d]. The prosthesis was then stained and glazed with light curing materials and cured and assessed initially on cast and then in patient's mouth, followed by cementation using resin cement similar to Case 1 [Figure 6e and f].
Figure 6.
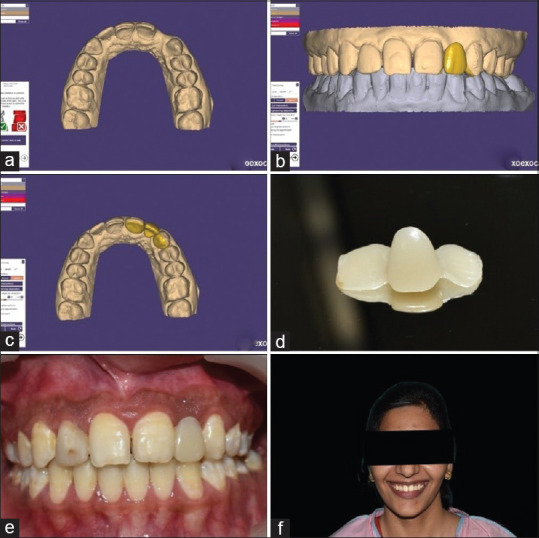
(a) After scanning of master cast, the maxillary scanned model in EXOCAD software, (b) CAD Designing of pontic, (c) Designing of two wings on prepared tooth, (d) Final prosthesis after Milling in CAM machine, (e) Final prosthesis in situ, (f) Postrehabilitative view. CAD: Computer-Aided Designing, CAM: Computer-Aided Manufacturing.
The post rehabilitative instructions were given to both the patients and they were recalled for periodic follow-up visit after a week, month, and 3 months.
DISCUSSION
There are several treatment options available for replacing missing anterior teeth, including removable partial dentures, fixed partial dentures, and implant retained prostheses. Removable partial dentures are the simplest and most cost-effective method of replacement, but they have several drawbacks, including underlying bone resorption, an unpleasant look, and a negative psychological impact in young patients. Fixed partial dentures are a useful treatment option, but it involves greater tooth reduction, which should be avoided in young patients as they have large pulp chambers in the abutments, predictable gingival transition, and patient age also limits the use of conventional fixed prostheses. Implants are the most acceptable treatment alternatives for long-term success, however owing to the bone development in young people, they are not recommended as well as they are more expensive, and failure rates are higher if not placed appropriately.[6,7]
A conventional cantilever bridge is another treatment option, but according to ante's law, lateral incisors cannot be used as abutment teeth for replacement of central incisor and also bridge cannot be cantilevered across the midline. Hence, resin-bonded Maryland bridges was planned because according to Prasanna et al. the success rate of resin-bonded cantilever bridges was more when compared to conventional cantilever bridges.[8]
The main advantage of a resin-bonded Maryland bridge is that it is a minimally invasive procedure that causes less damage to the abutment teeth, requires less chair time, and is less expensive.[9] It can be fabricated using various materials such as metal framed, fiber-reinforced, porcelain fused metal, and all-ceramic. However, the longevity of these restorations is still unclear because each material has its own disadvantages.[10] The systematic review conducted by Miettinen and Millar states that the failure rates of all ceramic restoration was more compared to fiber-reinforced and metal framed RBBs and concluded that resin-bonded restoration fabricated by any material can be used only for short period of time. Furthermore, it was mentioned that the most frequent complications are due to: debonding of metal-framed resin-bonded bridges (93% of all failures); delamination of the composite veneering material for the fiber-reinforced bridges (41%) and fracture of the framework for the all-ceramic bridges (57%).[11]
Therefore, graphene was used as a choice of material in Case 2. It is an allotropic carbon based material which will be nano-reinforced with polymethyl methacrylate acrylic resin as a biopolymer for dental use. They can be used as a material of choice for dental fillings, bridges and implants. The major advantage of this material is high mechanical strength, flexibility, low cost, nontoxicity, impermeability to liquid and gases, and transparency. Furthermore, CAD/CAM technology has the advantage of high quality, reproducibility, high efficiency, ability to store data from a standardized chain of production, industrial prefabrication and controlled materials, and increased popularity when compared to conventional techniques. However, it also has disadvantage of difficulty in fabrication and compromised esthetics in terms of color when compared to all-ceramic restoration. Hence, a long-term comparative studies has to be conducted to evaluate the success rate of graphene with other crown materials.[12,13]
CONCLUSION
RBBs can be highly effective in replacing missing anterior teeth, restoring oral function and esthetics, thereby increasing patient's satisfaction. In the following case reports two things were tried. A hybrid Maryland bridge was fabricated in first case which had a full veneer crown in maxillary left lateral incisor for adequate tooth coverage and not violating the ante's law and single wing on maxillary right central incisor of contralateral arch. The graphene was tried as a material of choice in second case and was fabricated by CAD/CAM technique which has an advantage of high strength and flexibility. Although the durability of RBBs is not much extended, a careful case selection, judicious designing of the preparation, and meticulous cementation regimen all can ensure the long-term success of Maryland Bridges.
Consent
As per international standard or university standard, patient's written consent has been collected and preserved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
REFERENCES
- 1.Gutmann JL. The origin of the Maryland bridge. J Hist Dent. 2019;67:110. [PubMed] [Google Scholar]
- 2.Livaditis GJ. Etched metal resin-bonded restorations: Principles in retainer design. Int J Periodontics Restorative Dent. 1983;3:34–47. [PubMed] [Google Scholar]
- 3.Durey KA, Nixon PJ, Robinson S, Chan MF. Resin bonded bridges: Techniques for success. Br Dent J. 2011;211:113–8. doi: 10.1038/sj.bdj.2011.619. [DOI] [PubMed] [Google Scholar]
- 4.Stolpa JB. An adhesive technique for small anterior fixed partial dentures. J Prosthet Dent. 1975;34:513–9. doi: 10.1016/0022-3913(75)90038-4. [DOI] [PubMed] [Google Scholar]
- 5.Malik P, Rathee M. From basics to beyond fabrication of resin-retained fixed partial dentures. Int J Curr Res. 2015;7(2):12889–12893. [Google Scholar]
- 6.Ahmad M, Naim H, Adawi AM, Siddiq A, Mayidi HM, Hakami YH. A conservative approach to replace missing teeth in the aesthetic zone with Maryland bridge – A case report. Dent Oral Craniofac Res. 2017;3:1–3. [Google Scholar]
- 7.Jenkins CB. The bond strength of new adhesive recommended for resin-bonded bridges. J Dent Res. 1985;64:664. [Google Scholar]
- 8.Prasanna BG, Reddy KK, Harsha TV, Ramesh GC. Clinical evaluation of conventional cantilever and resin bonded cantilever fixed partial dentures: A comparative study. J Contemp Dent Pract. 2012;13:793–8. doi: 10.5005/jp-journals-10024-1231. [DOI] [PubMed] [Google Scholar]
- 9.Valasingam S, Kumar M, Jyotsna P. Maryland bridge in children – A case report. Clin Dent. 2015;1:9. [Google Scholar]
- 10.Rathee M, Sikka N, Jindal S, Kaushik A. Prosthetic rehabilitation of severe Siebert's Class III defect with modified Andrews bridge system. Contemp Clin Dent. 2015;6:S114–6. doi: 10.4103/0976-237X.152965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miettinen M, Millar BJ. A review of the success and failure characteristics of resin-bonded bridges. Br Dent J. 2013;215:E3. doi: 10.1038/sj.bdj.2013.686. [DOI] [PubMed] [Google Scholar]
- 12.Holt LR, Drake B. The Procera Maryland Bridge: A case report. J Esthet Restor Dent. 2008;20:165–71. doi: 10.1111/j.1708-8240.2008.00172.x. [DOI] [PubMed] [Google Scholar]
- 13.Jaiswal PR, Godbole S. Replacement of missing anterior tooth with Maryland bridge. Sch J Dent Sci. 2017;4:38–42. [Google Scholar]


