Abstract
Microscopic colitis is a common cause of chronic diarrhea, particularly in patients with autoimmune disorders. Colonic mucosa appears normal and only shows inflammation on histological examination. There are two histological variations of microscopic colitis. It has been associated with several drug classes, and certain drugs are associated with one variation or another. In this case report, we discuss the case of a patient who is on a drug not previously associated with her variation of microscopic colitis and who has an autoimmune condition whose relationship to microscopic colitis is not well studied. We aim to outline the potential triggers for the disease and to call for further studies regarding how certain drugs and/or autoimmune disorders trigger it in order to further our understanding and improve management.
Keywords: Microscopic colitis, Selective serotonin reuptake inhibitor, Autoimmune disorder, Chronic diarrhea
Introduction
Microscopic colitis (MC) is defined as a chronic inflammatory bowel disease in which abnormal reactions of the immune system cause an inflammation of the inner lining of the colon. The symptoms of MC can be broad but include watery, nonbloody diarrhea, fecal urgency, and incontinence along with abdominal pain, weight loss, fatigue, and arthralgia. The colonic mucosa generally appears normal on endoscopic examination, and biopsy is required for diagnosis. The two main subtypes of MC are lymphocytic, which is characterized by a marked increase in intraepithelial lymphocytes, and collagenous, which is characterized by a thick subepithelial collagen band. The triggers of MC include any inflammatory precursor to the colon such as smoking as well as various types of medications, including NSAIDs and proton-pump inhibitors. A common drug class with previous association to MC is selective serotonin reuptake inhibitors (SSRIs). Sertraline in particular has been associated with the lymphocytic subtype of MC [1]. However, SSRIs are a very important and effective drug in treating many psychiatric diseases that patients face, and withdrawal of the drug could have many harms. Another documented association with MC is the presence of autoimmune conditions such as rheumatoid arthritis, celiac disease, and psoriasis. This case report discusses a patient with a personal and family history of vitiligo, an autoimmune condition, and who is on the SSRI escitalopram. We would like to discuss the relationship between autoimmune conditions and include a new SSRI in escitalopram as a potential trigger for lymphocytic MC, along with treatment options to allow patients to improve their quality of life.
Case Report
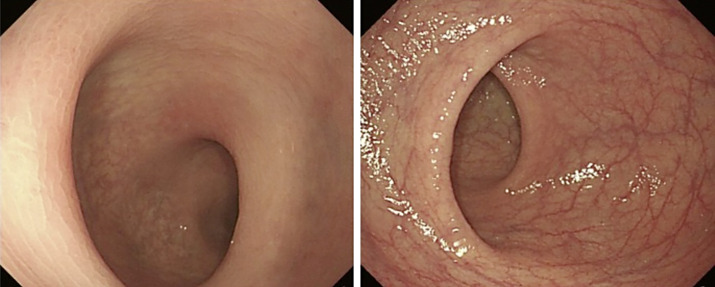
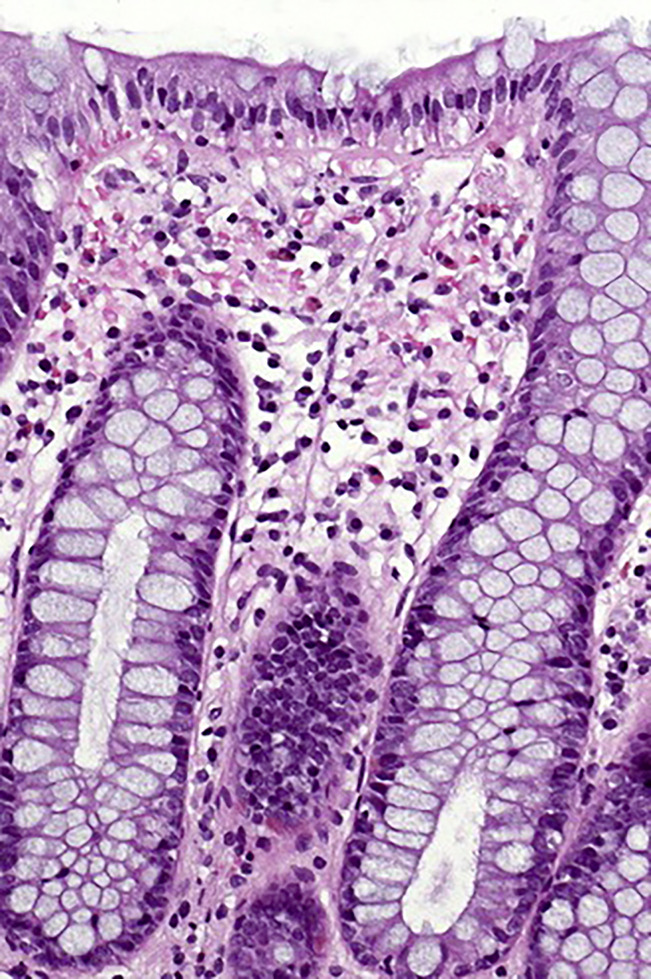
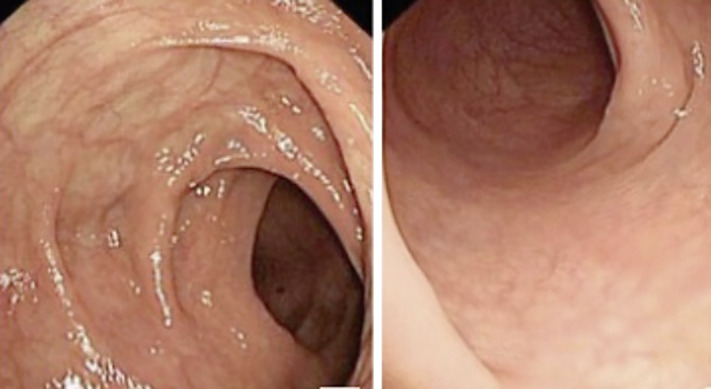
A 42-year-old woman with a past medical history significant for high-grade small bowel obstruction of unclear etiology was seen in an outpatient clinic for a follow-up visit. Previous history of the patient included longstanding depression and anxiety which led to the introduction of escitalopram about 6 months prior to her clinic visit. The patient was lost to follow-up until the recent visit and presented to clinic due to reported complaints of intermittent diarrhea and nausea with no triggers. She described her symptoms as experiencing 2–3 watery bowel movements per day along with 2 episodes of incontinence since her hospitalization for small bowel obstruction about 5 weeks prior. She reported random onset of symptoms with no identifiable pattern. The patient denied melena, hematochezia, emesis, and abdominal pain. The patient also reported having tried loperamide to help with her symptoms, but it did not work. On review of family history for colon disease or cancer, it was negative and was positive only for vitiligo in her father. She also reported new onset vitiligo in herself for the past 2 weeks, confirmed on physical exam as patches of hypopigmentation present in her upper extremities bilaterally. She denied history of any other autoimmune condition. On social history, the patient was a former smoker but quit 10 years ago. On flex colonoscopy, colonic mucosa appeared normal (Fig. 1) and showed no evidence of Crohn’s disease, ulcerative colitis, or other colon pathology. Random biopsies of the colon were taken which showed there was colonic mucosa with marked inflammation and an increase of intraepithelial lymphocytic infiltrate consistent with the diagnosis of lymphocytic MC (Fig. 2). The patient was started on budesonide oral 9 mg for 90 days and a recommendation to find an alternative to her current SSRI of escitalopram due to findings that SSRIs have an association with MC. The patient was told to follow up in 3 months following the completion of the budesonide course as this has been shown to be beneficial in treating MC. According to recent guidelines from the American Gastroenterological Association, budesonide is a first-line treatment [2]. After 3 months of treatment with budesonide, the patient showed significant improvement in her symptoms and was started on a tapered budesonide regimen. Repeat colonoscopy was performed which again showed normal mucosa endoscopically (Fig. 3) and a marked decrease in lymphocytic infiltrate and inflammation of the intraepithelial space on biopsy (Fig. 4).
Fig. 1.
Findings from colonoscopy prior to treatment showing normal mucosa on endoscopy with no evidence of inflammation or ulceration.
Fig. 2.
Evidence of lymphocytic colitis on biopsy with an increase in intraepithelial lymphocytes and marked inflammation.
Fig. 3.
Endoscopic findings on repeat colonoscopy after 12 weeks of oral budesonide consistent with normal colonic mucosa.
Fig. 4.
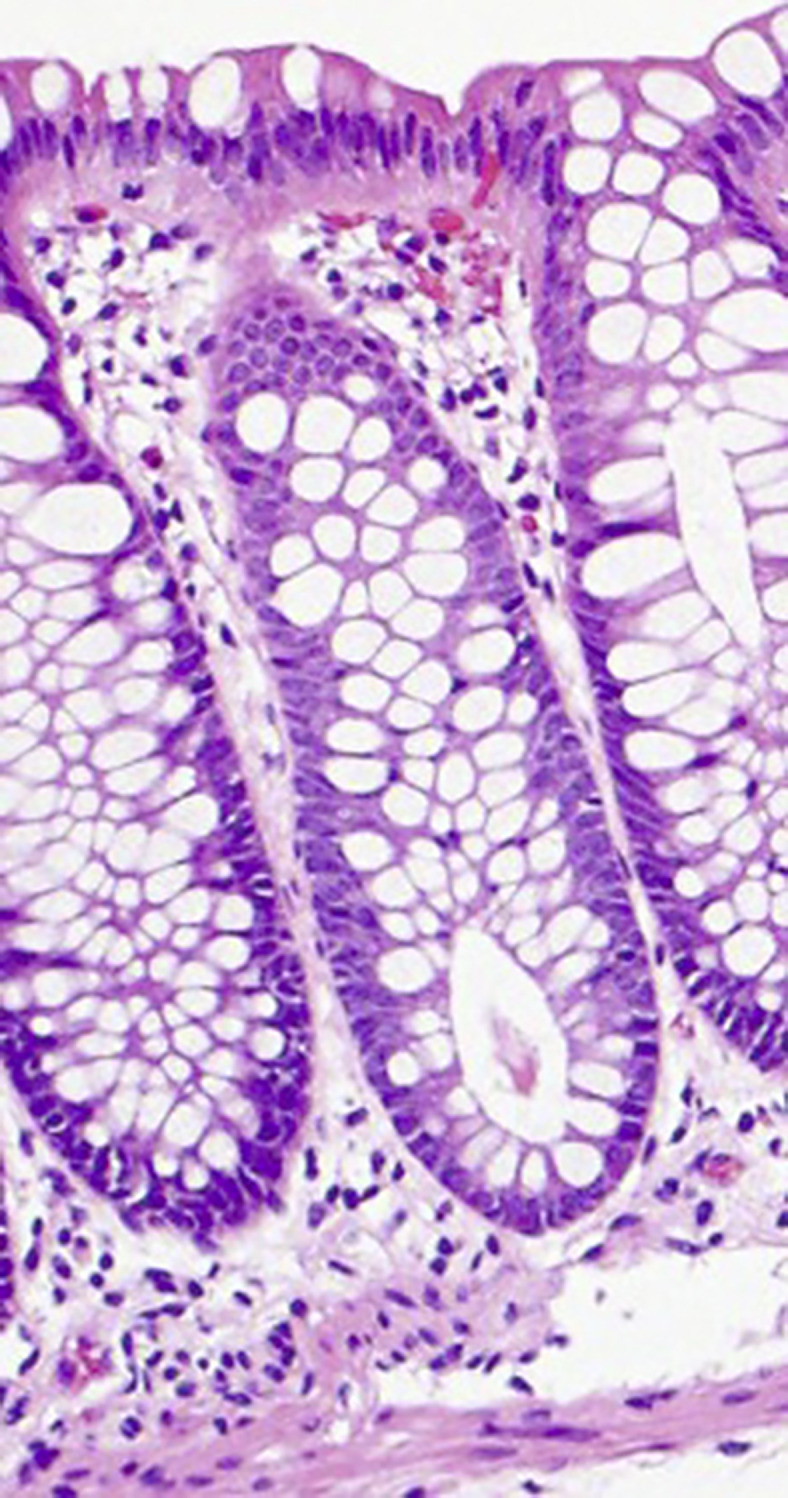
Repeat colon biopsy after 12 weeks of oral budesonide and improvement of symptoms showing a marked decrease in intraepithelial inflammation and lymphocytes.
Discussion
MC is a chronic and debilitating disease for the patients it affects. There are two main types of MC, collagenous and lymphocytic. MC has been an increasing complication in patients, reported as 103 cases per 100,000, and it is important to have a clear understanding of its causes and treatments in order to help lower the incidence and prevalence of the disease [3]. Certain drugs and tobacco use are common causes of MC. Our patient has been diagnosed with the lymphocytic subtype, which previously has only been associated with the usage of sertraline. Our patient, however, has never taken sertraline and has been taking a different SSRI, escitalopram. In a published case report, a 63-year-old man was diagnosed with MC confirmed by random biopsies taken from the terminal ileum and colon that showed increased intraepithelial lymphocytes giving the diagnosis of the lymphocytic subtype [1]. MC in this patient was found following sertraline treatment for 6 weeks for anxiety and depressive symptoms. The patient had no previous history of any gastrointestinal problems and upon cessation of sertraline for 2 weeks there was full resolution of the diarrhea; even after a 3-month follow-up, there was still no recurrence of the diarrhea. In another case study, a 50-year-old woman was stable on nortriptyline but experienced breakthrough depression and was then prescribed duloxetine after a series of prescription changes. Shortly thereafter, the patient had the onset of diarrhea, though she had no history of previous episodes of diarrhea despite being on antidepressant therapy before [4]. There is no clear etiology of how SSRIs can cause MC, but one proposed mechanism is that the gut houses one of the locations of serotonin storage, especially the enterochromaffin cells and enteric neurons, with the serotonin reuptake transporter having a role in the reuptake of serotonin into the enterochromaffin cells [5, 6]. Enteric serotonin is believed to have roles in cell signaling, intestinal inflammation, and gastrointestinal motility [5, 6]. Increasing the levels of serotonin, as is the primary mechanism of action of SSRIs, is then thought to trigger an increase in colonic inflammation and motility. A previous study had found significantly higher levels of serum serotonin in patients with MC versus healthy controls and found gene abnormalities in the MC patients involving a serotonin transporter polymorphism [7]. We would like to add our case report to the ongoing investigations supporting SSRIs triggering MC and add escitalopram as a proposed trigger to the lymphocytic subtype. With SSRIs being a widely used and highly efficacious medication given to treat a wide variety of psychiatric symptoms, we would like clinicians to be aware about all possible adverse effects. Additionally, the association between certain autoimmune conditions such as rheumatoid arthritis, celiac disease, and psoriasis has been studied in relation to MC. However, these conditions are often already present during the onset of MC and rarely the other way around. We would like to propose vitiligo, the autoimmune destruction of melanin-producing melanocytes, as another potential autoimmune condition associated with MC and call for further studies to be done involving the pathogenesis of the condition and how it relates to the gut. In this patient who developed vitiligo after her diagnosis of MC, a unique relationship between the manifestations of autoimmune disorders in the skin and in the gut may be occurring.
Statement of Ethics
This retrospective review of patient data did not require ethical approval in accordance with local/national guidelines. Written informed consent was acquired from the subject regarding publication of the details of their medical case and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
Humzah Iqbal conducted patient interviews, chart reviews, and contributed to writing the manuscript. Rakahn Haddadin conducted the literature review and contributed to writing the manuscript. All authors reviewed the final manuscript.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required. Further inquiries can be directed to the corresponding author.
References
- 1. Menon R, Ng C. Sertraline-induced microscopic colitis. Psychosomatics. 2015;56(3):316–7. 10.1016/j.psym.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 2. American Gastroenterological Association . Aga Institute guideline on the management of microscopic colitis: clinical decision support tool. Gastroenterology. 2015 Nov 22;150(1):276. 10.1053/j.gastro.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 3. Pardi DS, Loftus EV, Smyrk TC, Kammer PP, Tremaine WJ, Schleck CD, et al. The epidemiology of microscopic colitis: a population based study in Olmsted County, Minnesota. Gut. 2007;56(4):504–8. 10.1136/gut.2006.105890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salter TG, Williams MD. Antidepressant-associated microscopic colitis: a case report and literature review. Psychosomatics. 2017;58(3):307–12. 10.1016/j.psym.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 5. Ghia JE, Li N, Wang H, Collins M, Deng Y, El–Sharkawy RT, et al. Serotonin has a key role in pathogenesis of experimental colitis. Gastroenterology. 2009 Aug 23;137(5):1649–60. 10.1053/j.gastro.2009.08.041. [DOI] [PubMed] [Google Scholar]
- 6. Tyce GM, George HCS, Flock EV, Jesse LB. 5-hydroxytryptamine in the gastrointestinal tract after intestinal obstruction or hepatectomy. Exp Biol Med. 1964;115(4):1068–72. 10.3181/00379727-115-29118. [DOI] [PubMed] [Google Scholar]
- 7. Sikander A, Sinha SK, Prasad KK, Rana SV. Association of serotonin transporter promoter polymorphism (5-HTTLPR) with microscopic colitis and ulcerative colitis. Dig Dis Sci. 2014;60(4):887–94. 10.1007/s10620-014-3482-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required. Further inquiries can be directed to the corresponding author.