Abstract
Introduction
In advanced cancer care, early communication about palliative care (PC) and end-of-life (EoL)-related issues is recommended, but is often impeded by physicians’ communication insecurities. We investigated the effect of a newly developed compact communication skills training ‘PALLI-COM’ on oncologists’ competencies to early address PC/EoL-related issues.
Materials and methods
We conducted a randomized, controlled trial (RCT) with an intervention group (IG; 2 × 90 min training) and a wait list control group (CG) at five sites. At two assessment points, participating oncologists led videotaped medical consultations with simulated patients (SPs) via a privacy compliant video conference platform. SPs were represented by trained actors. The taped conversations were rated for primary outcome (communication skills assessed by adapted COM-ON-checklist and COM-ON-coaching rating scales) by raters blinded for study group. Secondary outcomes included oncologists’ self-reported communication skills (Self-Efficacy in Palliative Care Scale, Thanatophobia-Scale, Communication about End of Life Survey, study-specific items) as well as external rating of the SPs. Univariate analyses of covariance with baseline adjustment were used to analyze intervention effects.
Results
A total of 141 oncologists [age: mean (standard deviation) = 32.7 (6.3) years, 60% female (nIG = 73, nCG = 68)] participated. Following intervention, the IG showed significantly more improvement in four out of five assessed communication skills: ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’, ‘addressing the EoL’ and ‘explaining the concept of PC’. IG participants also improved more than CG participants in almost all secondary outcomes assessed by participants and SPs: oncologists’ self-efficacy, attitudes towards caring for terminally ill patients, communication strategies and confidence in dealing with PC/EoL-related issues as well as communication quality from the SPs’ perspective.
Conclusion
Findings indicate that the compact communication skills training PALLI-COM increases oncologists’ competencies in early addressing PC/EoL-related issues from different perspectives. Implementation in routine oncology residency might improve advanced cancer care by strengthening these communication skills.
Key words: palliative care, supportive care, oncology, communication skills training, randomized, controlled trial
Introduction
Communication about palliative care (PC) and end-of-life (EoL)-related issues is recommended early after first diagnosis of incurable malignant diseases with limited life expectancy1, 2, 3 and should include advance care planning, addressing personal values, fears and concerns, preparing for the future or talking about death and dying.1,4 Several studies indicate that early communication of these issues is associated with a range of benefits for patients, family caregivers and the health care system. Among others, it is associated with increased quality of life, improved symptom control, more acceptance of an incurable illness leading to premature dying and a decrease of caregivers’ burden.5, 6, 7, 8 Further, early PC/EoL communication is associated with reduced health care costs, as it leads to less aggressive medical care, less admissions to the intensive care unit at the very EoL and earlier hospice referrals.6,9, 10, 11 In addition, patients themselves prefer early and clear communication about their prognosis and EoL issues12, 13, 14, 15 and consider this communication essential for their personal EoL care.16 A timely discussion also enables them to participate more actively in treatment decisions, to set their individual priorities and to prepare themselves for death.17
According to international guidelines, this early communication of PC/EoL-related issues should be provided by the primary care physicians; within cancer care these are medical and organ-specific oncologists (further called ‘oncologists’).1, 2, 3,18,19 Despite these international recommendations,1, 2, 3 in daily clinical practice, PC/EoL-related issues are often not addressed until no further cancer-specific treatment can be offered. Oncologists tend to avoid addressing the expectable EoL early after first diagnosis of advanced cancer, which might be caused by communication insecurities and personal issues.20, 21, 22 PC/EoL conversations are considered the most stressful part of cancer care23 and insecurities often relate to the fear of causing additional distress or destroying hope.23, 24, 25, 26 Further, lacking training in PC/EoL communication seems to be crucial for those rare conversations.27
There is strong evidence that communication skills trainings (CSTs) are effective to improve communication skills of oncologists in general.28,29 However, most CSTs in the field of PC and EoL care solely address one specific communication skill.30 Mainly, that is breaking bad news, which is often taught based on the six-step SPIKES protocol.30,31 The protocol includes (i) ‘Setting up the interview’, (ii) ‘assessing the patient’s Perception’, (iii) ‘making an Invitation to disclose the news’, (iv) ‘sharing the Knowledge about the news’, (v) ‘responding to patient’s Emotion’, (vi) ‘Summarize the plan’.31 Other CSTs teach, for example, intrapersonal empathy based on the NURSE-statement, a commonly used approach to teach empathic expressions (‘Naming’, ‘Understanding’, ‘Respecting’, ‘Supporting’, and ‘Exploring’).32 Existing interventions are often time-intensive, although time pressure in daily clinical practice calls for less time-intensive CSTs.28
Therefore, we developed a compact CST named ‘PALLI-COM’ to train oncologists in early communication of PC/EoL-related issues in advanced cancer patients and evaluated its effects within a multicenter randomized, controlled trial (RCT). We investigated if PALLI-COM can improve PC/EoL communication skills from two different external and the trained oncologists’ own perspectives. Further, we analyzed the effects of PALLI-COM on the oncologists’ perceived self-efficacy, confidence and attitudes as well as self-reported communication strategies.
Materials and methods
Study design
This two-arm RCT (allocation 1 : 1) evaluated the efficacy of the new compact PALLI-COM CST at five sites in Germany [Hamburg-Eppendorf (UKE; main study center), Berlin, Goettingen, Heidelberg, Kiel]. The study was funded by the German Cancer Aid (‘Deutsche Krebshilfe e.V.’) and registered at the German Clinical Trials Register (DRKS00017025). The study protocol (further details published elsewhere33) was approved by the local ethic committees of all sites. Due to the COVID 19-pandemic, the protocol had to be adjusted and training plus data collection had to be carried out online.
All participants provided written informed consent. They were randomly assigned to an intervention group (IG) and a wait list control group (CG). Data assessment was conducted at two time points (pre—T0 and post—T1), in-between which only the IG received the training. The CG received the training after data collection.
Intervention development
PALLI-COM was developed based on international literature, expert discussions (medical and organ-specific oncologists, PC specialists and psycho-oncologists) and four focus groups. Each focus group included six to eight physicians with different experience and specialization within cancer care (medical and organ-specific oncologists, PC specialists) discussing their perceptions, communication difficulties and training needs {N = 28, mean (M)age [standard deviation (SD)] = 39.5 [8.92]; details will be published elsewhere}. The focus groups were transcribed and analyzed via qualitative content analysis by Mayring.34 Results were merged with relevant literature30 including the ‘core competencies in palliative care’ (European Association for Palliative Care, EAPC)35 and discussed with specialists of PC, oncology, psychology and psycho-oncology. The PALLI-COM curriculum was manualized according to the CReDECI2 guidelines.36
Standardized simulated patient (SP) case vignettes and actor scripts were developed by oncologists and PC specialists for outcome evaluation and role plays within the training. In all vignettes, patients with metastatic cancer and a life expectancy of <2 years had already been informed about the incurability of their disease and now ask their oncologists for treatment options. Each case existed in both gender variants. A train-the trainer workshop for all facilitators was conducted.
PALLI-COM was originally designed as a face-to-face workshop, but had to be converted into a digital interactive workshop due to the pandemics.
PALLI-COM is provided in groups of 6-10 physicians and consists of two sessions of 90 minutes with 2 weeks in-between, jointly conducted by a senior physician specialized in medical oncology plus PC and a psycho-oncologist. According to the ‘knowledge, skills, attitudes’ (KSA)-framework,37 PALLI-COM addresses knowledge [e.g. on the integration of (specialist) PC, empathy and hope], skills (specific communication skills regarding PC/EoL, application and consolidation in simulated consultations) and attitudes (e.g. by introducing the concept of double awareness38). The training didactics comprise theoretical input, self-reflection and interactive discussions, an example video of a successful consultation and practical role plays with SPs. In order to support the transfer of training content into daily practice, participants received a take-home communication aid and written summaries.
Participants and study sites
Participants were medical oncologists or organ-specific oncologists during their residency or at specialist level. Physicians at PC specialist level or with PC residency of >3 months were excluded. Recruitment took place via email distribution lists, conferences and local oncology networks at the five University Medical Centers in Germany.
Sample size and randomization
For medium group differences (Cohen’s d = 0.5) in a two-tailed test with a power of 0.80 at a significance level of P < 0.05, a needed total sample size of 134 participants (67 per group) was calculated for primary outcome analysis.
Computer-generated randomization was carried out separately per site by an experienced independent statistics specialist of the Department of Medical Psychology (UKE). Participants were recruited consecutively and block randomization in blocks of 20 with an allocation ratio of 1 : 1 was conducted.
Data assessment
Assessments for both groups were scheduled 5-8 weeks before and 5-8 weeks after the IG received the intervention. Assessment at both times included a videotaped medical consultation with an SP and self-report questionnaires.
The videotaped simulated medical consultations were based on two different standardized case vignettes. Sixteen different actors experienced in patient simulation were trained on these roles in an online workshop. The participating physicians received a short medical file of the SP’s situation and were then asked to conduct a consultation including discussion of limits of cancer-directed treatment options, prognostic implications and handling of the following life-time. The cases and the patient’s gender varied between assessment time points and participants. The consultations were conducted and taped via a privacy compliant video conference platform and supposed to take 10-15 min. Afterwards, the oncologist and the SP completed questionnaires on their perceived quality of the consultation.
Primary outcome
Primary outcome parameters were different oncologists’ communication skills addressing PC/EoL-related issues based on the two videotaped medical conversations rated by study scientists (NH, HR, HB, KH, NR). A study-specific rating tool was developed based on the German version of the validated COM-ON-checklist39,40 and the COM-ON-coaching rating scales41—which were kindly provided to us by PD Dr Alexander Wuensch from the University Medical Center of Freiburg, Germany—as well as under consideration of the core competencies in palliative care.35 The empathy items of the COM-ON-coaching rating scales were developed based on the NURSE model.32 Our final rating tool is presented in Supplementary Material 1, available at https://doi.org/10.1016/j.esmoop.2022.100623. We also created an additional instruction manual with detailed criteria for all response options.
Based on exploratory factor analyses and theoretical considerations, our items were assigned to five scales: ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’, ‘discussing further cancer-specific treatment’, ‘addressing the EoL’ and ‘explaining the concept of PC’. After a comprehensive rater training in order to establish an acceptable interrater reliability, ∼20% of the videos were rated by two raters. Disagreements between the raters were solved by consensus after discussion. To avoid habituation or memory effects, the videos were rotated between the different sites, so that no physician was rated by researchers from the own site of the participant or by the same rater at both assessment time points´. The raters were blinded to the group membership of the respective oncologist.
Secondary outcomes
Secondary outcomes were assessed by questionnaires on physicians’ perceptions, communication strategies and attitudes at both assessment time points: self-efficacy regarding conversations about PC, attitudes towards caring for terminally ill patients, communication strategies in discussing EoL issues, confidence in dealing with specific PC/EoL-related issues as well as attitudes towards early communication of PC/EoL-related topics.
Further, after the videotaped medical consultations, the SPs rated their perception of communication quality. Those rating items were assigned to four scales: ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’, ‘addressing the EoL’ and ‘discussing further cancer-specific treatment’. The SPs were also blinded to group membership of the respective oncologist.
Above that, the physicians rated their own satisfaction with their consultation after the videotaped medical consultations. The respective items were assigned to the following four scales: ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’, ‘addressing the end of life’ and ‘self-confidence addressing PC/EoL-related issues’.
Finally, after completion of the PALLI-COM training, participants evaluated the training via an online survey.
Table 1 presents an overview on all outcome parameters and measurements.
Table 1.
Primary and secondary outcome parameters
| Study outcome | Data source | Assessment tool | Items and scales |
|---|---|---|---|
| Primary outcome | |||
| Communication skills addressing PC/EoL-related issues | External rating by study scientists | Study-specific rating manual (adapted version of COM-ON-checklist39,40 and COM-ON-coaching rating scales41) | 13 Items (Likert scale 0-4) on 5 scales:
|
| Secondary outcomes | |||
| Self-efficacy regarding conversations about PC | Physicians’ self-report | Scale ‘communication’ of the Self-Efficacy in Palliative Care Scale (SEPC; valid and reliable questionnaire59) | 8 Items [visual analogue scale from (0) very anxious to (10) very confident] |
| Attitudes towards caring for terminal ill patients | Physicians’ self-report | Thanatophobia-Scale,60 valid and reliable59,60 | 7 Items (Likert scale 1-7) |
| Communication strategies in discussing PC/EoL-related issues | Physicians’ self-report | Communication about End of Life Survey20; good internal reliability | 19 Items (Likert scale 1-5) on 2 scales:
|
| Confidence in dealing with specific PC/EoL-related issues | Physicians’ self-report | Study-specific items | 5 Items (Likert scale 0-4) |
| Attitudes towards early communication of PC/EoL-related issues | Physicians’ self-report | Study-specific items | 2 Items (Likert scale 0-4) |
| Communication quality from the physicians’ perspective | Physicians’ self-report | Study-specific items | 8 Items (Likert scale 0-4) on 4 scales:
|
| Communication quality from the SPs’ perspective | External rating by SPs | Study-specific items inspired by the German version of the questionnaire on the Quality of Physician-Patient-Interaction (QQPPI)61,62 | 15 Items (Likert scale 0-4) on 4 scales:
|
| Satisfaction with PALLI-COM training | Physicians’ self-report | Study-specific items | 5 Items (Likert scale 1-5) |
COM-ON, communication in oncology; EoL, end-of-life; PC, palliative care; SP, simulated patient.
Statistical analysis
Descriptive statistics analyzed group characteristics (IG/CG). Group differences in sociodemographic variables were analyzed via t-tests or comparable non-parametric tests.
Univariate analyses of covariance with baseline adjustment were carried out to measure intervention effects on primary and secondary outcome parameters. The group membership (IG or CG) represented the independent variable (fixed factor) and the differences from T0 to T1 the dependent variables. For baseline adjustment, the initial level of the outcome parameter was added as a covariate. To avoid a potential type I error inflation due to multiple testing, levels of significance were adjusted by the Bonferroni–Holm method.42 Effect sizes were determined by partial eta2 (ƞp2), which according to Cohen43 can be interpreted as small from the value of 0.01, as medium from the value of 0.06 and as strong from the value of 0.14.
Results
Participant characteristics
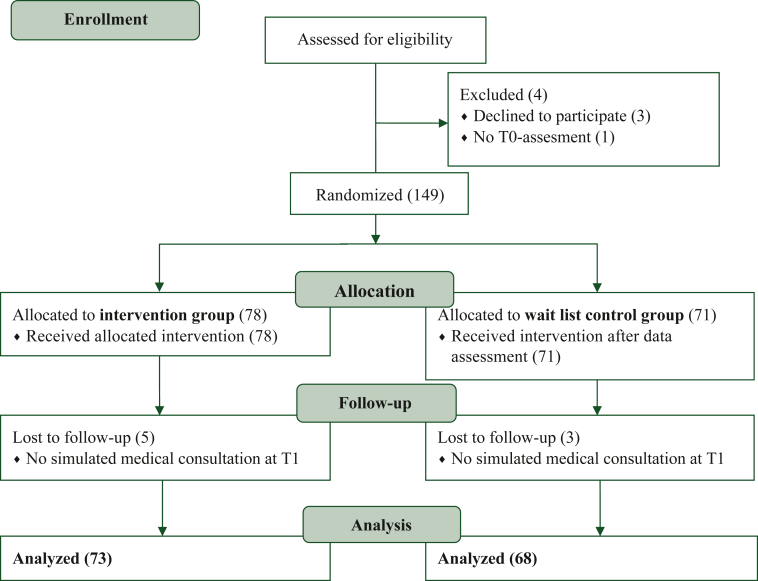
Within the 15 months recruitment period from September 2020 to November 2021, a total of 153 oncologists consented to participate, 4 of whom dropped out before randomization. Of 149 randomized, another 8 dropped out during the study process, resulting in 141 participants available for outcome analysis. Of those, 73 were randomized to IG and 68 to CG (required sample size: 134). A study flow chart including reasons for dropout is presented in Figure 1.
Figure 1.
Study enrollment according to the Consolidated Standards of Reporting Trials (CONSORT) 2010 flow diagram.
The mean age of the 141 participating physicians was 32.7 (SD = 6.3) years and the majority were female (58.9%). About 79% were residents and a majority worked in inpatient settings (70.2%). On average, they had 4.8 (SD = 5.4) years of professional experience as a physician. Most physicians underwent specialization in medical oncology (32.1%), followed by gastroenterology (23.4%) and gynecology (12.8%). An overview of participant characteristics is presented in Table 2.
Table 2.
Characteristics in total and per study group
| n | Total (N = 141) | n | IG (n = 73) | n | CG (n = 68) | χ2/t | P | |
|---|---|---|---|---|---|---|---|---|
| Age (M, SD) | 141 | 32.7 (6.3) | 73 | 32.5 (6.0) | 68 | 32.9 (6.6) | 0.434a | 0.665 |
| Gender (%) | 141 | 73 | 68 | |||||
| Female | 58.9 | 57.5 | 60.3 | 0.111b | 0.739 | |||
| Male | 41.1 | 42.5 | 39.7 | |||||
| Position (%) | 141 | 73 | 68 | |||||
| Residents | 78.7 | 79.5 | 77.9 | 2.946c | 0.399 | |||
| Specialists | 12.8 | 15.1 | 10.3 | |||||
| Senior physicians | 5.7 | 2.7 | 8.8 | |||||
| Before career entry | 2.8 | 2.7 | 2.9 | |||||
| Years in practice (M, SD) | 140 | 4.8 (5.4) | 73 | 4.3 (4.5) | 67 | 5.4 (6.2) | 1.104a | 0.271 |
| Main setting (%) | 141 | 73 | 68 | |||||
| Outpatient | 17.7 | 20.5 | 14.6 | 4.966c | 0.299 | |||
| Inpatient | 70.2 | 64.4 | 76.5 | |||||
| Inpatient and outpatient | 8.5 | 10.9 | 5.9 | |||||
| Other | 3.5 | 4.1 | 2.9 | |||||
| Specialty (%) | 141 | 73 | 68 | |||||
| Medical oncology | 31.2 | 37.0 | 25.0 | 8.535c | 0.704 | |||
| Gastroenterology | 23.4 | 21.9 | 25.0 | |||||
| Gynecology | 12.8 | 15.1 | 10.3 | |||||
| Internal medicine | 8.5 | 6.8 | 10.3 | |||||
| Surgery | 7.8 | 8.2 | 7.4 | |||||
| Dermatology | 2.8 | 2.7 | 2.9 | |||||
| Radiation therapy/radiooncology | 2.8 | 1.4 | 4.4 | |||||
| Other | 10.6 | 6.9 | 14.8 |
CG, control group; IG, intervention group; M, mean; SD, standard deviation.
t-test.
χ2 test.
Fisher’s exact test.
Communication skills
Externally rated PC/EoL communication skills revealed significantly higher improvement in the IG on the scales ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’, ‘addressing the EoL’ and ‘explaining the concept of PC’ with small to medium effect sizes. No significant effect was found on the sclae ‘discussing further cancer-specific treatment’. Table 3 presents the mean values of both groups at both assessment time points for all scales as well as the results of the analyses of covariance. A graphical illustration of the four significant primary outcome scales is displayed in Supplementary Material 2, available at https://doi.org/10.1016/j.esmoop.2022.100623.
Table 3.
Comparison of communication skill improvement from T0 to T1 between IG and CG after PALLI-COM training
| Pre (T0) |
Post (T1) |
Intervention effect |
||||||
|---|---|---|---|---|---|---|---|---|
| IG (n = 73) | CG (n = 68) | IG (n = 73) | CG (n = 68) | |||||
| Scales | M (SD) | M (SD) | M (SD) | M (SD) | df | F | Pa | part. η2 |
| Emotions and empathy | 2.04 (0.94) | 1.92 (0.75) | 2.49 (0.85) | 2.08 (0.94) | 1 | 6.47 | 0.012b | 0.045 |
| Opportunities and hope | 2.6 (0.73) | 2.52 (0.75) | 2.89 (0.61) | 2.57 (0.67) | 1 | 7.74 | 0.006b | 0.054 |
| Further cancer-specific treatment | 2.71 (0.61) | 2.64 (0.63) | 2.79 (0.58) | 2.8 (0.56) | 1 | 0.144 | 0.705 | 0.001 |
| Addressing end of life | 2.0 (0.92) | 1.95 (0.93) | 2.42 (0.77) | 2.06 (0.85) | 1 | 5.64 | 0.019b | 0.040 |
| Explaining concept of palliative care | 0.81 (1.11) | 0.88 (1.28) | 1.86 (1.32) | 1.04 (1.23) | 1 | 15.63 | <0.001b | 0.102 |
CG, control group; df, degrees of freedom; IG, intervention group; M, mean; part. η2, partial eta squared (effect size); SD, standard deviation.
Analyses of covariance considering the initial value as a covariate; dependent variable: mean difference from T0 to T1.
Significant intervention effect with Bonferroni–Holm corrected alpha level of 0.05.
The interrater reliability (ICC coefficient) ranged from 0.619 to 0.936, which can be interpreted as good to very good.44
Oncologists’ perceptions, communication strategies and attitudes
The intervention significantly improved oncologists’ self-efficacy and their confidence to address four of five PC/EoL-related issues: ‘PC structures’, ‘personal goals/values/wishes’, ‘feelings/thoughts regarding the EoL’ and ‘fears and concerns’. In each of those scales, the IG improved significantly more than the CG with medium to high effect sizes. No effect was found regarding their confidence in discussing oncologic treatment goals. Further, IG participants reported significantly more reduction of negative attitudes towards caring for terminally ill patients (high effect size) as well as less avoidant communication (medium effect size). Mean values and results of analyses of covariance regarding all secondary outcomes are displayed in Table 4.
Table 4.
Secondary outcome scores of IG and CG and effect of the factor ‘group’ in baseline-adjusted analyses of covariance
| Pre (T0) |
Post (T1) |
Intervention effect |
||||||
|---|---|---|---|---|---|---|---|---|
| IG (n = 73) | CG (n = 68) | IG (n = 73) | CG (n = 68) | |||||
| M (SD) | M (SD) | M (SD) | M (SD) | df | F | Pa | part. η2 | |
| Self-efficacyc | 5.11 (1.90) | 5.09 (1.91) | 6.63 (1.43) | 5.82 (1.74) | 1 | 12.51 | 0.001b | 0.088 |
| Attitudes towards caring for terminally ill patientsd | 20.36 (7.78) | 20.81 (8.34) | 18.24 (6.53) | 20.92 (8.27) | 1 | 35.27 | <0.001b | 0.211 |
| Communication strategiese | ||||||||
| Approach communication | 30.74 (3.74) | 30.65 (4.28) | 30.65 (4.28) | 32.58 (6.48) | 1 | 0.33 | 0.565 | 0.003 |
| Avoidant communication | 23.26 (4.25) | 22.54 (4.69) | 22.54 (4.69) | 22.34 (4.48) | 1 | 14.24 | <0.001b | 0.099 |
| Confidence in dealing with the following PC/EoL-related issues topicsf: | ||||||||
| Treatment goals | 2.54 (.96) | 2.37 (1.02) | 2.99 (0.67) | 2.67 (0.97) | 1 | 3.71 | 0.056 | 0.027 |
| Palliative care services | 1.76 (1.0) | 1.81 (1.04) | 1.70 (0.92) | 2.11 (0.99) | 1 | 22.11 | <0.001b | 0.144 |
| Personal goals/values/wishes | 2.42 (0.80) | 2.35 (0.84) | 2.93 (0.77) | 2.45 (0.75) | 1 | 14.65 | <0.001b | 0.101 |
| Feelings/thoughts regarding the end of life | 1.78 (0.92) | 1.82 (0.90) | 2.54 (0.75) | 2.03 (0.98) | 1 | 17.74 | <0.001b | 0.118 |
| Fears and concerns | 2.36 (0.74) | 2.35 (0.82) | 2.83 (0.63) | 2.43 (0.81) | 1 | 11.35 | 0.001b | 0.080 |
| Attitudes towards early communication of PC/EoL-related issuesg | ||||||||
| Knowing until where palliative care is own responsibility | 2.01 (0.93) | 1.87 (0.88) | 2.42 (0.77) | 2.28 (0.83) | 1 | 0.50 | 0.481 | 0.004 |
| Considering early communication as reasonable | 3.50 (0.69) | 3.51 (0.68) | 3.61 (0.60) | 3.56 (0.56) | 1 | 0.46 | 0.500 | 0.003 |
| Communication quality from the SPs’ perspectiveh | ||||||||
| Emotions and empathy | 3.04 (0.82) | 3.11 (0.81) | 3.47 (0.58) | 3.09 (0.82) | 1 | 9.87 | 0.002b | 0.71 |
| Opportunities and hope | 3.22 (0.59) | 3.23 (0.68) | 3.60 (0.50) | 3.39 (0.58) | 1 | 5.38 | 0.022b | 0.040 |
| Addressing end of life | 3.33 (0.76) | 3.23 (0.96) | 3.67 (0.61) | 3.22 (0.89) | 1 | 11.72 | 0.001b | 0.083 |
| Further cancer-directed treatment | 3.26 (0.61) | 3.24 (0.77) | 3.62 (0.51) | 3.43 (0.63) | 1 | 2.92 | 0.090 | 0.022 |
| Communication quality from the physicians’ perspectiveh | ||||||||
| Emotions and empathy | 2.49 (0.56) | 2.70 (0.53) | 2.85 (0.54) | 2.59 (0.69) | 1 | 11.59 | 0.001b | 0.091 |
| Opportunities and hope | 2.37 (0.63) | 2.49 (0.54) | 2.77 (0.58) | 2.52 (0.63) | 1 | 8.54 | 0.004b | 0.067 |
| Addressing end of life | 2.43 (0.82) | 2.75 (0.67) | 2.68 (0.89) | 2.83 (0.87) | 1 | 0.33 | 0.569 | 0.003 |
| Self-confidence addressing PC/EoL-related issues | 2.37 (0.86) | 2.50 (0.87) | 2.85 (0.75) | 2.45 (0.84) | 1 | 16.58 | <0.001b | 0.124 |
CG, control group; df, degrees of freedom; IG, intervention group; M, mean; part. η2, partial eta squared (effect size); SD, standard deviation.
Analyses of covariance considering the initial value as covariate; dependent variable: mean difference from T0 to T1.
Significant intervention effect with Bonferroni–Holm corrected alpha level of 0.05.
Visual analogue scale 0-10; the higher the value the higher the perceived self-efficacy.
Likert scale; 1-7; the higher the value the more negative attitudes towards caring for terminally ill patients; averaged total values displayed.
Likert scale 1-5; the higher the value the more approach or avoidance communication; averaged total values displayed.
Likert scale 0-4; the higher the value the higher the perceived confidence.
Likert scale 0-4; the higher the value the more positive the attitude.
Likert scale 0-4; the higher the value the higher the competence.
Communication quality from the SPs’ perspective
Regarding the SPs’ perspective, IG physicians improved more than CG physicians on three of four scales: ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’ and ‘addressing the EoL’, with medium and one small effect size. No effect was found on the scale ‘discussing further cancer specific treatment’ (Table 4).
Communication quality from the physicians’ perspective
Analyses of oncologists’ satisfaction with their communication revealed significantly more increase in IG than in CG on three of four scales: ‘reacting to emotions and showing empathy’, ‘pointing out opportunities and giving hope’ and ‘self-confidence addressing PC/EoL-related issues’ with medium effect sizes. No effect was found on the scale ‘addressing the end of life’ (Table 4).
Satisfaction
Oncologists’ satisfaction with the PALLI-COM CST was high in general (M = 4.6, SD = 0.53; scale 1-5) as well as with regard to specific aspects such as the helpfulness of trained skills (M = 4.58, SD = 0.69) or the trainers’ feedback (M = 4.60, SD = 0.64).
Discussion
To our knowledge, PALLI-COM is the first compact CST for oncologists without PC specialization on communicating different PC/EoL-related issues that was analyzed in an RCT including multi-perspective evaluation.
PALLI-COM training achieved significant improvements in participating oncologists’ competencies to address PC/EoL-related issues: reacting to patients’ emotions and showing empathy, pointing out opportunities, giving hope, addressing the EoL and explaining the concept of PC.
Effects of a CST on multiple communication skills of oncologists concerning PC/EoL-related issues observed within an RCT were previously only reported by Goelz et al.40 evaluating the ‘COM-ON-p’ CST using the questionnaire we adapted for primary outcome assessment, who reported significant improvements in global communication skills, communicating the transition to PC and involving significant others. Their training consisting of 1.5 total days plus coaching was, however, much more time intensive than the compact PALLI-COM intervention.
Two other RCTs with effects on multiple communication skills included not only physicians, but also patients45,46 and the few remaining RCTs addressed just one communication skill each: ‘breaking bad news’,47, 48, 49 ‘dealing with emotions’,50,51 ‘shared decision making’30,52 or ‘goals-of-care discussions’.53
PALLI-COM efficacy was evaluated not only from the scientists’ perspective, but also from the SPs’ and the oncologists’ own perspective, which allows comparison of different rating perspectives. Only ∼20% of previous studies (three RCTs) also considered the SPs’ perspective.30 Regarding the SPs’ perspective, PALLI-COM yielded significant improvements in oncologists’ competence in reacting to emotions and showing empathy, pointing out opportunities and giving hope as well as addressing the EoL. Oncologists’ own satisfaction with their consultation improved regarding reacting to emotions and showing empathy, pointing out opportunities and giving hope and their self-confidence addressing PC/EoL-related issues. Thus, our analyses revealed concordant results of communication skills improvement from three perspectives with regard to reacting to emotions and showing empathy as well as pointing out opportunities and giving hope. This indicates that PALLI-COM represents an effective training to reduce the frequent fear of destroying hope23, 24, 25, 26 and oncologists’ difficulties in meeting the emotional needs of advanced cancer patients.54,55
Addressing the EoL was improved from the external raters’ and SPs’ perspective, but not from the oncologists’ own perspective. This might suggest that talking about death and dying remains challenging, even if it was adequately addressed from an external perspective.
Further oncologists’ self-reports demonstrated significantly more self-efficacy, less negative attitudes towards caring for terminally ill patients, less avoidant communication strategies in discussing EoL issues and more confidence in dealing with most specific PC/EoL-related issues—all with medium to large effect sizes. To our knowledge, this is the first study evaluating the effect of a CST on personal attitudes, communication strategies and perceptions towards caring for terminal ill patients from the participants’ own perspective. Considering the high personal discomfort physicians experience with EoL conversations,56 this seems to be a crucial aspect of the PALLI-COM training.
PALLI-COM seemed to have no impact on discussing further cancer-specific treatment options, although this was only assessed by a limited number of items. This result, however, was consistently observable from both evaluating perspectives. This might indicate that communication about PC/EoL-related issues early after advanced life-limiting cancer diagnoses according to the PALLI-COM curriculum does not influence oncologists’ conversations about cancer treatment.
PALLI-COM was well accepted and participants reported high satisfaction and a significant benefit for their daily clinical practice. The low dropout rate during the study reflects the subjectively beneficial experience.
In addition, the conversion into an online format was considered practicable by both facilitators and participants. Given the accelerated digitalization process in health care since the beginning of the COVID-19 pandemic,57 PALLI-COM represents a contemporary CST that can be attended from everywhere. As we consider PALLI-COM CST easily transferable into other languages, an international use of the training is also realistic.
Further strengths of this RCT are the comparably large sample size30 and the multicenter approach enabling the inclusion of oncologists from different settings and regions. Rigorous blinding towards group membership of both SPs and external raters elevated the study evaluation quality. Selection bias due to structural and political changes over time is unlikely because of the short recruitment period. In contrast to prior studies,30 we also included organ-specific oncologists to address all physicians responsible for early communication of PC/EoL-related issues in cancer care.1 As communication difficulties in oncology are not resolved ‘over time’ or do not decrease with growing clinical experience,58 there was a need for training interventions for physicians of all ages and degrees of experience, which is why we included not only oncology or organ-specific oncology residents, but also senior oncologists to our study.
Some limitations, however, have to be noticed. Due to the lack of standardized measurements for some outcome parameters, study-specific items had to be developed and rating was carried out by an adapted pre-existing scale that had not been previously tested in this specific form. Yet, the extensive training of the raters resulted in a ‘good’ to ‘very good’ interrater reliability. Further, due to the short follow-up period, we cannot draw any conclusions on long-term training effects or if re-training will be necessary in future. Another limitation might be caused by self-selection bias: participating oncologists were already interested in communication and might therefore initially present with better communication skills than their colleagues. This might explain the only small to medium effect sizes in some outcomes with initially relatively high mean values and thus smaller potential for statistical improvement (ceiling effects). This assumption is substantiated by the item ‘considering early communication as reasonable’ displaying very high initial mean values and no intervention effect, as this notion might probably be the very reason for study participation. When implementing PALLI-COM in curricula obligatory for oncologists in general, this bias might be mitigated and the partly low to moderate effects in outcome parameters might improve.
Conclusion
In conclusion, the compact PALLI-COM CST improves different communication skills of early addressing PC/EoL-related issues in oncologists from different perspectives, including the oncologists’ own experience. We achieved remarkable multi-perspectively observed improvements in oncologists’ PC/EoL communication skills with only two sessions of 90 minutes. Respecting time pressure in daily practice, PALLI-COM is easily integrable into routine oncology education. The implementation of PALLI-COM as an integral part of oncology residency might improve timely communication of PC/EoL issues in advanced cancer care, as recommended by international guidelines.1, 2, 3 Regarding the several benefits of this early communication for patients and family caregivers,5, 6, 7, 8, 9, 10, 11 an implementation of PALLI-COM into routine education might be a promising approach to improve advanced cancer care.
Acknowledgements
The authors appreciate all participating colleagues making this study possible and the German Cancer Aid (‘Deutsche Krebshilfe e.V.’) for their funding. We thank PD Dr. Alexander Wuensch from the University Medical Center of Freiburg, Germany for providing us with study material.
Funding
This work was supported by the German Cancer Aid (‘Deutsche Krebshilfe e.V.’) [grant number 70113231].
Disclosure
The authors have declared no conflicts of interest.
Supplementary data
References
- 1.Ferrell B.R., Temel J.S., Temin S., et al. Integration of palliative care into standard oncology care: American Society of clinical oncology clinical practice guideline update. J Clin Oncol. 2017;35(1):96–112. doi: 10.1200/JCO.2016.70.1474. [DOI] [PubMed] [Google Scholar]
- 2.Jordan K., Aapro M., Kaasa S., et al. European Society for Medical Oncology (ESMO) position paper on supportive and palliative care. Ann Oncol. 2018;29(1):36–43. doi: 10.1093/annonc/mdx757. [DOI] [PubMed] [Google Scholar]
- 3.Kaasa S., Loge J.H., Aapro M., et al. Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol. 2018;19(11):e588–e653. doi: 10.1016/S1470-2045(18)30415-7. [DOI] [PubMed] [Google Scholar]
- 4.Back A.L. Patient-clinician communication issues in palliative care for patients with advanced cancer. J Clin Oncol. 2020;38(9):866–876. doi: 10.1200/JCO.19.00128. [DOI] [PubMed] [Google Scholar]
- 5.Zimmermann C., Swami N., Krzyzanowska M., et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–1730. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]
- 6.Rugno F.C., Paiva B.S., Paiva C.E. Early integration of palliative care facilitates the discontinuation of anticancer treatment in women with advanced breast or gynecologic cancers. Gynecol Oncol. 2014;135(2):249–254. doi: 10.1016/j.ygyno.2014.08.030. [DOI] [PubMed] [Google Scholar]
- 7.Vanbutsele G., Pardon K., Van Belle S., et al. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol. 2018;19(3):394–404. doi: 10.1016/S1470-2045(18)30060-3. [DOI] [PubMed] [Google Scholar]
- 8.Temel J.S., Greer J.A., El-Jawahri A., et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol. 2017;35(8):834–841. doi: 10.1200/JCO.2016.70.5046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright A.A., Zhang B., Ray A., et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Romano A.M., Gade K.E., Nielsen G., et al. Early palliative care reduces end-of-life intensive care unit (ICU) use but not ICU course in patients with advanced cancer. Oncologist. 2017;22(3):318–323. doi: 10.1634/theoncologist.2016-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sullivan D.R., Chan B., Lapidus J.A., et al. Association of early palliative care use with survival and place of death among patients with advanced lung cancer receiving care in the Veterans Health Administration. JAMA Oncol. 2019;5(12):1702–1709. doi: 10.1001/jamaoncol.2019.3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nyborn J.A., Olcese M., Nickerson T., Mack J.W. “Don’t Try to Cover the Sky with Your Hands”: Parents’ experiences with prognosis communication about their children with advanced cancer. J Palliat Med. 2016;19(6):626–631. doi: 10.1089/jpm.2015.0472. [DOI] [PubMed] [Google Scholar]
- 13.Hagerty R.G., Butow P.N., Ellis P.A., et al. Cancer patient preferences for communication of prognosis in the metastatic setting. J Clin Oncol. 2004;22(9):1721–1730. doi: 10.1200/JCO.2004.04.095. [DOI] [PubMed] [Google Scholar]
- 14.Collins A., McLachlan S.A., Philip J. Communication about palliative care: a phenomenological study exploring patient views and responses to its discussion. Palliat Med. 2018;32(1):133–142. doi: 10.1177/0269216317735247. [DOI] [PubMed] [Google Scholar]
- 15.Kirk P., Kirk I., Kristjanson L.J. What do patients receiving palliative care for cancer and their families want to be told? A Canadian and Australian qualitative study. BMJ. 2004;328(7452):1343. doi: 10.1136/bmj.38103.423576.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steinhauser K.E., Christakis N.A., Clipp E.C., McNeilly M., McIntyre L. Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284(19):2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 17.Clayton J.M., Hancock K.M., Butow P.N., et al. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust. 2007;186(S12):S77–S105. doi: 10.5694/j.1326-5377.2007.tb01100.x. [DOI] [PubMed] [Google Scholar]
- 18.Buss M.K., Rock L.K., McCarthy E.P. Understanding palliative care and hospice: a review for primary care providers. Mayo Clin Proc. 2017;92(2):280–286. doi: 10.1016/j.mayocp.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization WHO Definition of Palliative Care. 2002. https://www.dgpalliativmedizin.de/images/stories/WHO_Definition_2002_Palliative_Care_englisch-deutsch.pdf
- 20.Granek L., Nakash O., Cohen M., Ben-David M., Ariad S. Oncologists’ communication about end of life: the relationship among secondary traumatic stress, compassion satisfaction, and approach and avoidance communication. J Psychooncology. 2017;26(11):1980–1986. doi: 10.1002/pon.4289. [DOI] [PubMed] [Google Scholar]
- 21.Almack K., Cox K., Moghaddam N., Pollock K., Seymour J. After you: conversations between patients and healthcare professionals in planning for end of life care. BMC Palliat Care. 2012;11:15. doi: 10.1186/1472-684X-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daugherty C.K., Hlubocky F.J. What are terminally ill cancer patients told about their expected deaths? A study of cancer physicians’ self-reports of prognosis disclosure. J Clin Oncol. 2008;26(36):5988–5993. doi: 10.1200/JCO.2008.17.2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baile W.F., Lenzi R., Parker P.A., Buckman R., Cohen L. Oncologists’ attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol. 2002;20(8):2189–2196. doi: 10.1200/JCO.2002.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Granek L., Krzyzanowska M.K., Tozer R., Mazzotta P. Oncologists’ strategies and barriers to effective communication about the end of life. J Oncol Pract. 2013;9(4):e129–e135. doi: 10.1200/JOP.2012.000800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhi W.I., Smith T.J. Early integration of palliative care into oncology: evidence, challenges and barriers. Ann Palliat Med. 2015;4(3):122–131. doi: 10.3978/j.issn.2224-5820.2015.07.03. [DOI] [PubMed] [Google Scholar]
- 26.Brighton L.J., Bristowe K. Communication in palliative care: talking about the end of life, before the end of life. Postgrad Med J. 2016;92(1090):466–470. doi: 10.1136/postgradmedj-2015-133368. [DOI] [PubMed] [Google Scholar]
- 27.Buss M.K., Lessen D.S., Sullivan A.M., Von Roenn J., Arnold R.M., Block S.D. Hematology/oncology fellows’ training in palliative care: results of a national survey. Cancer. 2011;117(18):4304–4311. doi: 10.1002/cncr.25952. [DOI] [PubMed] [Google Scholar]
- 28.Moore P.M., Rivera S., Bravo-Soto G.A., Olivares C., Lawrie T.A. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. 2018;7:CD003751. doi: 10.1002/14651858.CD003751.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fischer F., Helmer S., Rogge A., et al. Outcomes and outcome measures used in evaluation of communication training in oncology - a systematic literature review, an expert workshop, and recommendations for future research. BMC Cancer. 2019;19(1):808. doi: 10.1186/s12885-019-6022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harnischfeger N., Rath H.M., Oechsle K., Bergelt C. Addressing palliative care and end-of-life issues in patients with advanced cancer: a systematic review of communication interventions for physicians not specialised in palliative care. BMJ Open. 2022;12(6) doi: 10.1136/bmjopen-2021-059652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baile W.F., Buckman R., Lenzi R., Glober G., Beale E.A., Kudelka A.P. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 32.Back A.L., Arnold R.M., Baile W.F., Tulsky J.A., Fryer-Edwards K. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55(3):164–177. doi: 10.3322/canjclin.55.3.164. [DOI] [PubMed] [Google Scholar]
- 33.Harnischfeger N., Rath H.M., Ullrich A., et al. Evaluation of a communication skills training to facilitate addressing palliative care related topics in advanced cancer patients: study protocol of a multicenter randomized controlled trial (PALLI-KOM) BMC Palliat Care. 2020;19(1):67. doi: 10.1186/s12904-020-00568-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayring P. Qualitative content analysis. A companion to qualitative research. 2004;1(2):159–176. [Google Scholar]
- 35.Gamondi C., Larkin P., Payne S.A. Core competencies in palliative care: an EAPC white paper on palliative care education: part 1. Eur J Cancer. 2013;20(2):86–91. [Google Scholar]
- 36.Möhler R., Köpke S., Meyer G. Criteria for reporting the development and evaluation of complex interventions in healthcare: revised guideline (CReDECI 2) Trials. 2015;16(1):204. doi: 10.1186/s13063-015-0709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stevens M.J., Campion M. The knowledge, skill, and ability requirements for teamwork: implications for human resource management. J Manage. 1994;20(2):503–530. [Google Scholar]
- 38.Rodin G., Zimmermann C. Psychoanalytic reflections on mortality: a reconsideration. J Am Acad Psychoanal Dyn Psychiatry. 2008;36(1):181–196. doi: 10.1521/jaap.2008.36.1.181. [DOI] [PubMed] [Google Scholar]
- 39.Stubenrauch S., Schneid E.M., Wünsch A., et al. Development and evaluation of a checklist assessing communication skills of oncologists: the COM-ON-Checklist. J Eval Clin Pract. 2012;18(2):225–230. doi: 10.1111/j.1365-2753.2010.01556.x. [DOI] [PubMed] [Google Scholar]
- 40.Goelz T., Wuensch A., Stubenrauch S., et al. Specific training program improves oncologists’ palliative care communication skills in a randomized controlled trial. J Clin Oncol. 2011;29(25):3402–3407. doi: 10.1200/JCO.2010.31.6372. [DOI] [PubMed] [Google Scholar]
- 41.de Figueiredo M.N., Krippeit L., Freund J., et al. Assessing communication skills in real medical encounters in oncology: development and validation of the ComOn-coaching rating scales. J Cancer Educ. 2019;34(1):73–81. doi: 10.1007/s13187-017-1269-5. [DOI] [PubMed] [Google Scholar]
- 42.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 43.Cohen J. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 44.Wirtz M., Caspar F. Hogrefe; Göttingen: 2002. Beurteilerübereinstimmung und Beurteilerreliabilität: Methoden zur Bestimmung und Verbesserung der Zuverlässigkeit von Einschätzungen mittels Kategoriensystemen und Ratingskalen. [Google Scholar]
- 45.Malhotra C., Rajasekaran T., Kanesvaran R., et al. Pilot trial of a combined oncologist-patient-caregiver communication intervention in Singapore. JCO Oncol Pract. 2020;16(2):e190–e200. doi: 10.1200/JOP.19.00412. [DOI] [PubMed] [Google Scholar]
- 46.Epstein R.M., Duberstein P.R., Fenton J.J., et al. Effect of a patient-centered communication intervention on oncologist-patient communication, quality of life, and health care utilization in advanced cancer: the VOICE Randomized Clinical Trial. JAMA Oncol. 2017;3(1):92–100. doi: 10.1001/jamaoncol.2016.4373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fujimori M., Shirai Y., Asai M., Kubota K., Katsumata N., Uchitomi Y. Effect of communication skills training program for oncologists based on patient preferences for communication when receiving bad news: a randomized controlled trial. J Clin Oncol. 2014;32(20):2166–2172. doi: 10.1200/JCO.2013.51.2756. [DOI] [PubMed] [Google Scholar]
- 48.Liénard A., Merckaert I., Libert Y., et al. Is it possible to improve residents breaking bad news skills? A randomised study assessing the efficacy of a communication skills training program. Br J Cancer. 2010;103(2):171–177. doi: 10.1038/sj.bjc.6605749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gorniewicz J., Floyd M., Krishnan K., Bishop T.W., Tudiver F., Lang F. Breaking bad news to patients with cancer: a randomized control trial of a brief communication skills training module incorporating the stories and preferences of actual patients. Patient Educ Couns. 2017;100(4):655–666. doi: 10.1016/j.pec.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tulsky J.A., Arnold R.M., Alexander S.C., et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593–601. doi: 10.1059/0003-4819-155-9-201111010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Butow P., Cockburn J., Girgis A., et al. Increasing oncologists’ skills in eliciting and responding to emotional cues: evaluation of a communication skills training program. Psychooncology. 2008;17(3):209–218. doi: 10.1002/pon.1217. [DOI] [PubMed] [Google Scholar]
- 52.Henselmans I., Smets E., de Haes J.C.J.M., Dijkgraaf M.G.W., de Vos F.Y., van Laarhoven H.W.M. A randomized controlled trial of a skills training for oncologists and a communication aid for patients to stimulate shared decision making about palliative systemic treatment (CHOICE): study protocol. BMC Cancer. 2018;18(1):55. doi: 10.1186/s12885-017-3838-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bickell N., Back A., Adelson K., et al. Effects of a communication intervention randomized controlled trial to enable goals-of-care discussions. JCO Oncol Pract. 2020;16:e1015–e1028. doi: 10.1200/OP.20.00040. [DOI] [PubMed] [Google Scholar]
- 54.Kelly B.J., Turner J. Depression in advanced physical illness: diagnostic and treatment issues. Med J Aust. 2009;190(S7):S90–S93. doi: 10.5694/j.1326-5377.2009.tb02478.x. [DOI] [PubMed] [Google Scholar]
- 55.Butow P.N., Brown R.F., Cogar S., Tattersall M.H.N., Dunn S.M. Oncologists’ reactions to cancer patients’ verbal cues. Psychooncology. 2002;11(1):47–58. doi: 10.1002/pon.556. [DOI] [PubMed] [Google Scholar]
- 56.Draper E.J., Hillen M.A., Moors M., Ket J.C.F., van Laarhoven H.W.M., Henselmans I. Relationship between physicians’ death anxiety and medical communication and decision-making: a systematic review. Patient Educ Couns. 2019;102:266–274. doi: 10.1016/j.pec.2018.09.019. [DOI] [PubMed] [Google Scholar]
- 57.Jnr B.A. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fallowfield L., Jenkins V., Farewell V., Saul J., Duffy A., Eves R. Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet. 2002;359(9307):650–656. doi: 10.1016/S0140-6736(02)07810-8. [DOI] [PubMed] [Google Scholar]
- 59.Mason S., Ellershaw J. Assessing undergraduate palliative care education: validity and reliability of two scales examining perceived efficacy and outcome expectancies in palliative care. Med Educ. 2004;38(10):1103–1110. doi: 10.1111/j.1365-2929.2004.01960.x. [DOI] [PubMed] [Google Scholar]
- 60.Merrill J., Lorimor R., Thornby J., Woods A. Caring for terminally ill persons: comparative analysis of attitudes (thanatophobia) of practicing physicians, student nurses, and medical students. Psychological Rep. 1998;83(1):123–128. doi: 10.2466/pr0.1998.83.1.123. [DOI] [PubMed] [Google Scholar]
- 61.Bieber C., Nicolai J., Mueller K., Eich W. Der Fragebogen zur Arzt-Patient-Interaktion (FAPI) – Validierung und psychometrische Optimierung anhand einer Stichprobe chronischer Schmerzpatienten. Klin. Diagnostik u. Evaluation. 2011;4:78–93. [Google Scholar]
- 62.Bieber C., Muller K.G., Nicolai J., Hartmann M., Eich W. How does your doctor talk with you? Preliminary validation of a brief patient self-report questionnaire on the quality of physician-patient interaction. J Clin Psychol Med Settings. 2010;17(2):125–136. doi: 10.1007/s10880-010-9189-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.