Abstract
Background
Polycystic ovary syndrome (PCOS) is a complex, chronic condition characterized by anovulation, polycystic ovarian morphology and hyperandrogenism that requires lifelong management. To reduce the risk of comorbidity and to manage symptoms, lifestyle management and pharmaceuticals such as oral contraceptives are the most common forms of treatment and should be tailored to the individual patient. The literature to date has shown PCOS patients to experience widespread dissatisfaction with the amount and quality of information they receive from providers, along with lower levels of trust in physicians. Little is known about the lived experiences of women managing PCOS in Canada, across age groups.
Methods
In-depth remote interviews explored women's lived experiences managing PCOS and the barriers and facilitators they encountered in their management journeys. Data were analyzed using thematic analysis and interpretive description methodology.
Results
Twenty-five in-depth, telephone interviews conducted with participants (aged 18–63 y) across Canada revealed participants lacking sufficient information and guidance from physicians, especially in primary care. Areas in need of more guidance included lifestyle management and mental health. Lack of empathy and weight bias among physicians were also perceived by participants. Older participants received little guidance on treatment options postmenopause. Loss of trust and withdrawal from seeking medical care were prominent themes, along with greater self-reliance on self-management, including self-educating and self-experimenting with treatments.
Conclusions
Most women in this study were frustrated with the level of involvement and information provision from their doctors. Key recommendations are identified for the provision of care to younger and older patients with PCOS. Improved education for physicians may be needed to improve the quality of healthcare provision for PCOS.
Keywords: facilitators, interviews, lived experiences, management, polycystic ovary syndrome
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders, affecting 8–13% of reproductive-aged women.1 Historically seen as a gynecological and reproductive disorder, PCOS's spectrum of health consequences are increasingly recognized.2 Many patients with PCOS develop insulin resistance, central obesity and dyslipidemia, which places them at a higher risk of developing diabetes and other long-term complications.3–5 An additional, often-overlooked dimension of PCOS impacts mental health: PCOS patients are likely to develop anxiety, depression, eating disorders and body image issues.6–9
Some patients with PCOS manage many symptoms at once, such as insulin resistance, weight, hirsutism, acne and infertility, and thus may require access to a multidisciplinary healthcare team and a variety of treatments.10–13 Symptoms and concerns are dependent on the age and needs of the patient: PCOS presentation varies across the life cycle.14,15 Access to an involved and present healthcare team who can monitor the long-term health of a patient is paramount to the success of PCOS management in the long term.16
Lifestyle management, involving weight loss or healthy weight maintenance, remains the most effective first-line therapeutic intervention.17,18 It can be helpful to refer to a dietitian for guidance on lifestyle management.18,19 Pharmaceuticals such as metformin, lipid-lowering agents and oral contraceptives should be tailored to the individual patient's risk profile and treatment goals.10,13,19,20
The literature to date shows that many women feel that they do not receive sufficient information about their condition and are frustrated by the limited knowledge of PCOS they find in professionals and their inconsistent approaches to diagnosis and management of PCOS.2,21–24 Studies of healthcare providers found that many may need more knowledge on PCOS and have a limited amount of information available for patients about PCOS and its management.24–27 Little is known about patients’ firsthand experiences accessing care for the management of PCOS and navigating the healthcare system in Canada.
This qualitative study explores the lived experiences of women with PCOS in Canada to better understand the meaning of that experience for them and identifies the barriers and facilitators in women's journeys to manage their condition. The study provides insight into patient perspectives on care and well-being, with the goal to inform healthcare providers in their attempts to provide care to this patient population. The experiences and needs of women with PCOS are explored with consideration to age.
Methods
Study design
In-depth, semistructured telephone interviews with participants explored their experiences in being diagnosed and subsequently managing PCOS. As described in a prior paper,28 interview participants were sourced from a larger, multi-methods study that involved an online questionnaire about PCOS diagnosis experience hosted on SurveyMonkey (Momentive Inc., San Mateo, California, USA). Respondents who indicated interest in being interviewed at the end of their questionnaires were subsequently interviewed remotely, via telephone, on a first-come, first-served basis. Interviews explored women's perceptions and experiences with the diagnosis and management of PCOS and perceptions on how to improve PCOS healthcare, but only the themes relating to their management experience are explored in this paper.
Research setting
Participants were reached across Canada. Canada is a country with 38 005 238 people (as of July 2020), with the four most populous provinces being Ontario, Quebec, British Columbia and Alberta.29 The three most populous provinces after Ontario (14 734 010) are Quebec (8 574 571), British Columbia (5 147 712) and Alberta (4 421 876).29
Participants and recruitment
A purposive convenience sample was gathered online with participants who met the inclusion criteria: age ≥18 y, reporting a medical diagnosis of PCOS, having lived in Canada since their diagnosis and able to speak and understand English. No upper age limit was established to promote participation from older patients living with PCOS in the perimenopausal and postmenopausal stages of life. Participants were recruited through posts on PCOS groups on Facebook, Reddit and online PCOS forums. Social media was used as a recruitment strategy to reach a wider sample from across all Canadian provinces. (Note that the recruitment posts included gendered, women-specific language. However, not all people with PCOS may identify as women. Due to our recruitment, we will continue to use gendered language in this publication to reflect our sample.) The survey was advertized entirely online by the first author posting a short paragraph about the purpose of the study along with a recruitment poster and a link to the survey on SurveyMonkey. The PCOS Awareness Association also helped with recruitment by carrying out a one-time re-post on their Facebook page with the study's recruitment poster and the survey link. Participants who filled out questionnaires were invited to submit their contact information for follow-up interviews. Participants were interviewed in the order in which their affirmative responses and consent forms were received. Recruitment continued until preliminary analysis during data collection suggested thematic consistency across age groups and no more perimenopausal and postmenopausal women were available to interview. Recruitment took place during April–December 2018.
Data collection
Twenty-five in-depth interviews were conducted remotely via telephone by first author from October to December 2018, averaging 1 h in length and conducted in one uninterrupted meeting. The interviewer conducted all interviews by telephone in a private residential office with no one else present. All interviews were audio-recorded (with participant consent) and transcribed verbatim by the first author. One interview was held over Skype due to participant preference. The participants were encouraged to share their experiences through a semistructured interview process. The semistructured interview guide was developed by first author based on themes and gaps identified in previous literature (Supplemental File 1).
Data analysis
The first author coded all qualitative interview data, including field notes made during and after interviews, and managed and analyzed all data in NVivo 12 (version 12, 2018; QSR International Pty Ltd). In accordance with Thorne et al.’s30 interpretive description methodology, an inductive analysis technique was used to analyze data. Themes were derived entirely from the data. Thorne et al.’s interpretive description approach is widely used in nursing research and does not generate new truths or theories but rather describes thematic patterns and commonalities while also accounting for individual variations and provides a product that clinicians can use as a backdrop for clinical decision-making.30 Braun and Clarke's six key stages in the thematic analysis of qualitative data were also followed in this study: (1) Familiarize, (2) Generate initial codes, (3) Search for themes, (4) Review themes, (5) Define themes and (6) Write up the data analysis.31 Codes and subsequent subcategories were generated directly from topics raised in the data. The overarching code categories (barriers and facilitators) were developed from the research questions.
Trustworthiness
This study was reported based on the consolidated criteria for reporting qualitative research (COREQ; Supplemental File 2).32 At the time of the study, first author was a MSc student conducting in-depth interviews for the first time after training in graduate classes and workshops. First author identifies as female, and participants were made aware of the reason for the author to be conducting this research, their personal interest in the research topic and PCOS status, but otherwise no significant relationship existed or was established between the author and participants. To ensure reliability and validity, first author considered researcher bias, used the strategies of thick description, development of a coding system, checking and agreement on themes and analysis by members of the team, transparency when reporting research (as per COREQ) and demonstrating the author's interpretive lens throughout the report.30,32
Results
Recruitment resulted in 25 participants ranging in age from 18 to 63 y (Table 1). Participants were mostly of white/Caucasian background, aged 25–30 y, resided in Ontario and employed full-time. Seven participants had children, and nine participants were looking to conceive at the time of the interview. The mean length of time since the diagnosis of PCOS was 5.5 y at the time of enrollment in the study (Table 2). All participant names below are pseudonyms.
Table 1.
Demographic characteristics of interview participants (n=25)*
| Demographic characteristic | Number of women (%) |
|---|---|
| Age group, y | |
| 18–24 | 5 (20) |
| 25–30 | 10 (40) |
| 31–36 | 4 (16) |
| 37–40 | 2 (8) |
| 41–50 | 2 (8) |
| 51–66 | 1 (4) |
| Province | |
| Alberta | 4 (16) |
| British Columbia | 4 (16) |
| Ontario | 13 (52) |
| Quebec | 1 (4) |
| Ethnicity | |
| Black | 1 (4) |
| East Asian | 2 (8) |
| Middle Eastern | 2 (8) |
| South Asian | 2 (8) |
| White/Caucasian | 18 (72) |
| Marital status | |
| Single | 11 (44) |
| Common-law/live-in partner | 5 (2 0) |
| Married | 9 (36) |
| Education | |
| Bachelor's degree | 12 (48) |
| Master's degree | 3 (12) |
| Trade/technical/vocational training | 2 (8) |
| Employment | |
| No paid work | 3 (12) |
| Student | 7 (28) |
| Employed full-time | 12 (48) |
| Employed part-time | 1 (4) |
| Parental status | |
| No children | 18 (72) |
| Has children | 7 (28) |
| Looking to conceive | 9 (36) |
| Pregnant | 2 (8) |
*Note: based on information participants were comfortable divulging; not all participants are captured.
Table 2.
Diagnostic characteristics of interview participants
| Participant (pseudonym) | Age (y) | Length of time since diagnosis | Diagnosing physician | Number of physicians seen before attaining diagnosis | Length of time seeking diagnosis |
|---|---|---|---|---|---|
| Sally | 30 | 1 mo | Gynecologist | 2 | 2 y |
| Melissa | 34 | 1 y | RE | 3 | 3 mo |
| Mei | 18 | 1 y | Pediatric gynecologist | 3 | 2.5 y |
| Melanie | 25 | 2 mo | GP | 2 | 3 mo |
| Lily | 18 | 1 y | Gynecologist | 2 | 3 mo |
| Lizzie | 27 | 10 y | Pediatrician | 2 | 4 y |
| Pam | 28 | 6 mo | Gynecologist | 2 | 2 wk |
| Josie | 27 | 2 y | Gynecologist | 2 | 10 y |
| Zara | 24 | 2 y | Ob-Gyn | 2 | 4 mo |
| Abigail | 31 | 2 y | Ob-Gyn | 2 | 1 y |
| Brianna | 21 | 5 y | Pediatric gynecologist | 2 | 1 y |
| Fiona | 31 | 5 y | Endocrinologist | 2 | 4 y |
| Eileen | 47 | 21 y | GP | 1 | 6 mo |
| Divya | 22 | 2 mo | Gynecologist | 2 | 4 y |
| Mary | 27 | 5 mo | Endocrinologist | 2 | 9 mo |
| Bianca | 36 | 5 y | GP | 1 | 3 mo |
| Jamila | 26 | 1 y | GP | 3 | 10 y |
| Holly | 29 | 7 y | GP | 1 | 1.25 y |
| Margaret | 33 | 9 mo | GP | 4 | 10 y |
| Vanessa | 63 | 43 y | GP | 1 | 2 wk |
| Rita | 38 | 2 mo | Fertility specialist | 5 | 5 y |
| Patricia | 29 | 8 y | GP | 2 | 2 y |
| Lucy | 47 | 14 y | Endocrinologist | 6 | 10 y |
| Emma | 29 | 5 y | GP | 1 | 4.5 y |
| Josephine | 32 | 3 y | Fertility specialist | 2 | 3 mo |
Abbreviations: GP, general practitioner; Ob-Gyn, obstetrician gynecologist; RE, reproductive endocrinologist.
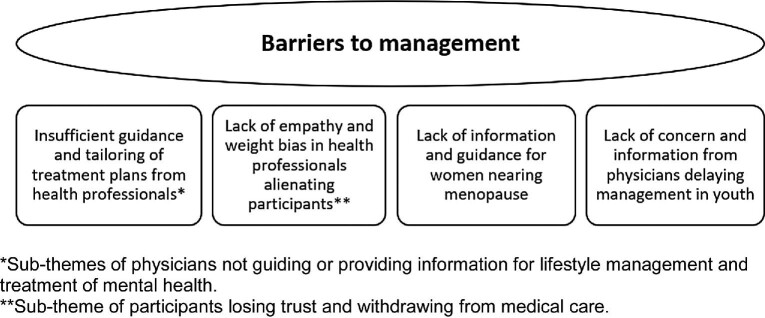
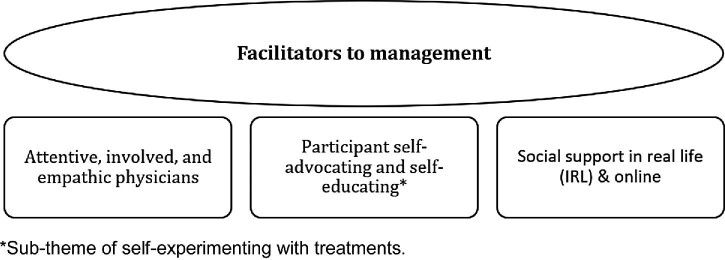
Barriers were identified as factors external or internal to participants that affected participant experience of their PCOS management negatively (e.g. by delaying management). Facilitators were identified as factors external or internal to participants that affected participant experience of their PCOS management positively (e.g. by making them feel supported or helping them meet treatment goals). Figures 1 and 2 outline the major themes found.
Figure 1.
Barriers to PCOS management.
Figure 2.
Facilitators to PCOS management.
Barriers
Insufficient guidance and tailoring of treatment plans from health professionals
A major barrier to management occurred for 68% of participants (17/25) who were not given enough information on treatment options or guidance from physicians in devising an individualized treatment plan. Primary care physicians (PCPs) were cited in 36% of experiences as particularly uninvolved with PCOS management, often not offering referrals to specialists to enable access to a multidisciplinary care team. Many participants felt unsupported by healthcare providers and gathered relevant information and made health decisions (short- and long-term) on their own.
Josie (age 27 y) expressed that her family doctor offered little guidance with Josie's management of PCOS. Josie felt as though she was unable to rely on her family doctor for guidance and resources like referrals:
It's very frustrating because I usually have to basically tell her ‘you need to refer me to this’ or ‘I need to be referred to this’ or ‘I need to see this person’. I don't know why, I haven't really figured out. It seems to be like I'm usually the one googling how to deal with this. I'm usually being my own doctor.
Holly (age 29 y) expressed how she felt unsupported and left to her own devices in her management of PCOS, not knowing the status of her own health:
I think with her understanding and knowing that I had it, I think it would have been nice to have them take a bit more interest. If that makes sense. Because I don't necessarily know what I should be watching for, or something that could be detrimental to me, that sort of thing. Whereas I would think that they do, which would have been nice. Because I mean like I don't know to check for insulin resistance. I don't know to check for my fasting glucose or whatever. But they do. Or they're supposed to.
1.2 Insufficient support for mental health-related symptoms
Several participants shared that they experienced mental health challenges because of PCOS but lacked acknowledgment of mental health from their doctors. Very few participants (8%) had general practitioners (GPs) who followed up on their mental health or discussed the mental health impacts of PCOS. Divya (age 22 y) shared an experience where she felt her doctor avoided the topic of her mental health:
But with my family doctor has always dismissed not just the PCOS but I've gone to him with other issues. I know PCOS is potentially linked to mental health issues too. I've read it. And I remember bringing these types of things up and he would just kind of shy away from it like he didn't want to deal with it. So I feel like they try to look for the path of least resistance if they can. Unless I was physically dying or something like diabetes. It's easier or maybe more of a concern to him than if there was mental health issues, or like the period issue where it's like ‘Oh, she's not trying to get pregnant or whatever, so who cares’.
1.2 Insufficient guidance with lifestyle management
Lifestyle management is the first-line recommendation for management of PCOS. Many participants (11/25 or 44%) were often told to lose weight but expressed frustration when their doctors did not offer any guidance or referrals to dietitians or nutritionists. Participants shared about keto diets, intermittent fasting and low-carb diets to manage their symptoms (e.g. menstrual irregularity, insulin resistance), but those diets were supervised by health professionals or the care team.
Lucy (age 47 y), who had struggled with her weight, explained her frustration with the minimal guidance from her doctors on lifestyle management:
They just said ‘Lose weight’, which is really useless. You don't need to tell people to lose weight. None of my doctors have ever offered valuable advice. Not only with PCOS but with lifestyle or nutrition or anything, ever.
2. Lack of empathy and weight bias in physicians alienating participants
Some participants’ (24%) interactions with their healthcare providers were marred by a feeling of not being heard, or in the case of overweight/obese participants, perceiving bias from doctors because of their weight. A lack of empathy, poor listening skills and dismissiveness in doctors were other barriers that led to participants feeling unsupported in their management journeys.
Holly (age 29 y) spoke about how a lot of doctors she encountered did not know much about PCOS, but she felt more frustrated at their lack of concern and empathy:
So I should preface this. My mom is a nurse. I've grown up around the healthcare profession. I mean I don't necessarily blame them for not knowing, like there's a myriad of disease and syndromes, like I can't expect every doctor to know off the top of their head and be able to pinpoint. I think I was just frustrated at the lack of follow-up, not even follow-up, but the lack of resources for me to go to. And I didn't feel like my doctor gave a hoot, which was frustrating and it felt like what was the point?
Some participants who were overweight or obese felt a bias in some of their doctors that alienated them. Zara (age 24 y) spoke about how frustrated she felt when her doctor had assumed she was sedentary due to her weight, when in fact Zara had been incorporating physical activity into her daily routine:
Totally negative. Kind of like without necessarily asking. Like I walk an hour and a half twice a day, every day. I'm not sedentary. But you just assuming is just very frustrating, especially when you're told that it's very hard for you to lose weight when you have PCOS. It's just like, oh my god, you need to talk about this better.
1.2 Loss of trust in physicians after adverse experiences
When encountering a lack of empathy and/or weight bias in physicians, some participants lost trust with their doctors and stopped reaching out for help. Many participants also began to opt out from seeking care from their physicians after finding that their doctors could not offer any useful information.
Mary (age 27 y) expressed that she wanted to be able to trust and rely on her doctor, but when she was not finding the information she needed, it was hard for her to do so:
Because it's not that I wouldn't trust my doctor if they gave me that information but they don't. So it kind of instills a lack of confidence, you know? So it's not even ‘Who do I trust the most?’, it's like ‘Who is the only one giving me information?’, because I would trust – like if my doctor handed me a pamphlet and was like ‘This is PCOS, if you have any questions ask me’ then I would 100 percent trust that. But then it's like they're not doing that.
3. Age considerations: lack of concern and information from doctors delaying management in youth
Some participants who were diagnosed early in life, such as during adolescence, reflected that their diagnosis and early visits with their doctors did not enable them to fully understand the long-term implications of PCOS or the importance of management. When doctors were unconcerned over younger patients’ symptoms, or when they did not take the time to explain the impacts and long-term nature of PCOS, it led participants to normalize their symptoms and delay management of symptoms until much later in life.
Margaret (age 33 y) detailed how her unconcerned GP, who initially diagnosed her in her early 20s, affected her attitude towards her health:
It's kind of really funny because even I discounted it because everybody was so casual about it, you know what I mean for so long that it really wasn't until I started seeing my GP now and she actually took it seriously and kind of treated it like it was something that actually needed to be dealt with, you know? Then I kind of clued in to like ‘Hey somebody should have been doing something about this like 10 years ago’.
4. Age considerations: need for more information and guidance for women nearing menopause
For older participants nearing menopause, a unique barrier to management arose when they had to terminate their medications due to advanced age risks. Older women with PCOS had to learn how to manage their symptoms anew, often without any medical guidance.
At the time of the interview, Vanessa (age 63 y) was postmenopausal and was facing health challenges and had many unanswered questions around how PCOS would affect her postmenopause. Ten years prior, at the age of 53 y, she had been assessed by an endocrinologist, who had to take her off the medications she was on:
Metformin, spironolactone and birth control of some sort, a variety. And so she had me come off of all those pills. And these last 10 years I haven't been on any medication and I'm in the process of going to see a specialist next week to see if I can find somebody that has some medication I can go back on because things have gotten quite a bit worse.
Vanessa's symptoms gradually worsened, and she had no follow-up for another check-up on how she was doing without the medication:
But then there was no follow-up. Like I went to see the endocrinologist and then there's no follow-up. They just took me off those meds and then there was no follow-up to see what's going on or if I should be on anything or whatever. It's always up to you to figure out what you should be doing and who you should be seeing.
Facilitators
Attentive, involved and empathic doctors who helped even with little knowledge
Many participants (40%) had doctors who had little knowledge of PCOS; however, these participants’ experiences accessing care were still positive because they felt that their doctors were nevertheless able to support them by researching and addressing concerns. Participants felt supported because their doctors would listen and act on their behalf by researching PCOS treatment options, offering information, providing reassurance and displaying empathy.
Vanessa (age 63 y) felt supported by one of her previous doctors who did not know much about PCOS at that point, but who listened to Vanessa's concerns and was proactive about researching and offering information:
The first doctor I had when I came to BC [British Columbia], I felt supported. At that point I didn't really understand terribly much. And she also didn't, looking back. But she cared enough that she sent me on these tests and she would listen to me when I'd come in and say ‘Okay I think I should be on this drug’. She would research it obviously or look it up in the drug book. But she listened to me.
Lizzie (age 27 y) has a very communicative, back-and-forth relationship with her new GP, which aided in her ability to access care and feel supported. She explained her experiences:
But I know even just going into her [office] and saying ‘You know this is what I've heard and this is what I'm thinking for this, what lines are you coming in on?’ She's open to discussing, she doesn't always like my ideas, I think she thinks I just sit on Google to make her life complicated. But she's pretty involved and ‘Ok, well let's think about it’ or ‘Ok, we'll try it, I'll give you 2 weeks and you'll have to come back and we're evaluating this’. But yeah, she's pretty good.
2. Participants self-advocating and self-educating
A significant facilitator to participants’ management of PCOS included their efforts to stay involved in self-management, especially in situations where participants lacked access to knowledgeable and/or involved doctors. Self-education aided 22/25 participants (88%) in the quest of understanding their condition better and finding treatment options to manage their symptoms. Self-advocating helped 44% of participants when they encountered physicians who had minimal informational resources to provide and/or seemed hesitant to offer referrals or become involved.
Although Emma (age 29 y) had symptoms from early in her life, such as significant and unexplained weight gain, facial hair and irregular periods, she was not diagnosed until an accidental finding on an ultrasound scan for an intrauterine device. After the diagnosis, Emma found that her doctors had little information and guidance to offer her. Emma reflected on the importance of self-advocating:
But I find that you really do have to advocate and that I think is the most frustrating part is that there just aren't enough doctors to give you that quality and that level of care. So you have to fill in the gaps yourself.
Mary (age 27 y) described how, through self-education on PCOS, she was able to self-advocate and get the referrals and guidance she needed:
So even though I wasn't really given a lot of resources, I feel like once I knew what was going on I was kind of able to advocate for myself enough to get those resources.
1.2 Self-experimenting with treatments
A lot of participants experienced a lack of information from their doctors about treatment options and plans for PCOS. In those instances, self-education aided them: learning to understand their condition better and researching therapeutic options on their own, often via the internet. Often a last resort, self-experimentation was a prominent theme for 48% of participants who were not supported by health professionals in their management efforts.
Holly (age 29 y) turned to self-experimentation with treatments after not being able to find the guidance she needed from her GP. She explained:
If it was coming from a GP, I would definitely trust that. In my experience, the information that I've been looking for hasn't come from a GP. When I was diagnosed, I wasn't given anything. Like in that experience that kind of leaves me with my GP knows nothing about it so I have to go and figure it out myself. So then I trust the information in all of these books and looking at kind of what the popular opinion is on certain things. Like testing out all these different supplements and then trial and error myself.
3. Social support in real life and online
Social support came up as a common facilitator in 72% of participants’ management journeys, usually in the form of participants reaching out to friends and family or online groups for support when dealing with health challenges. In cases where participants did not have social support in real life, online PCOS groups served as sources of support and anecdotal information.
When some participants struggled with hirsutism and other outwardly manifesting PCOS symptoms that can have a stigma associated with them, connecting with their loved ones helped them to cope with their feelings. Bianca (age 36 y) explained:
But with my mother and my girlfriends I'm like ‘Oh my gosh’ if anybody so much is complaining a little bit about an odd hair I'm like ‘Guys I have to shave’. Like you know it's not something pretty or feminine but I definitely have friends and family in a support sense, that I can be open and honest and reveal on those less flattering aspects.
Jamila (aged 26 y) benefited from the social connection and support in online platforms. She was unable to find the support in her friends, who could not fully understand and relate to her experiences. She explained:
In the group that I'm reading now, people have the same issues which I know and it's so nice, the group is actually what I find support in now. I really enjoy reading it and being able to connect with the people. Before that I did not have any support. I'm actually feeling much better now. I was actually really depressed about it. I didn't have a way out to speak to anyone. No one would actually understand it. So now with that group, it's definitely much better.
Discussion
Many participants in this study were frustrated by how little information they were able to receive from their physicians, which adds to the growing body of evidence of frustration in women with PCOS with the quality of information they receive.16,21–23,33–39 Participants described learning about common PCOS implications on their own, such as the increased risk of insulin resistance. The lack of clear information about PCOS led many participants to lose trust in their medical professionals and to opt out of consulting their doctors for medical advice in the future. A study by Lin et al. found that women with PCOS were more likely to have greater distrust in their PCP's opinion, have more arguments with their healthcare providers and feel that their doctors spent less effort to treat PCOS concerns.33
Most participants, across age groups, self-educated to understand PCOS and what treatments are available to manage their symptoms. Participants spoke of the need for credible information to be made available to patients with PCOS, such as pamphlets at the doctor's office or links to websites verified by medical professionals. Information giving is important, increased knowledge of PCOS empowers patients and is associated with better lifestyle practices and improved healthcare satisfaction.40
Key areas where more information and guidance were needed included lifestyle management, treatment options/plans in the short- and long-term and PCOS implications and risks (e.g. the risk of type 2 diabetes or mental illness). Consistent follow-up and involvement from health professionals were lacking, leading many women to largely rely on their own efforts to navigate management. Previous studies reported similar findings of participants lacking guidance and long-term support on the management of fertility and needing a comprehensive treatment plan from doctors.35,39,39,41–43
Many participants were told to lose weight but not given guidance as to how to go about it or offered referrals to dietitians and other allied health professionals. Several other studies similarly report women with PCOS not being given information on lifestyle management.33,39,44 There is wide variation across studies of physicians regarding how frequently lifestyle management is recommended by doctors for PCOS,2,24 and previous studies found low referral rates from PCPs to dietitians.19,45 Recommendations exist for doctors to provide information on lifestyle management and/or referrals to dietitians as necessary to patients,13,18,25 yet most attempts to modify lifestyle appear to be self-initiated and maintained.19,44,46
Some participants felt that their physicians were not aware of the links between PCOS and mental health. Women with PCOS are a high-risk population for anxiety, depression, eating disorders and poor body image.37,4–49 Screening for these conditions is recommended by numerous guidelines to improve well-being, ability to successfully implement and sustain lifestyle changes and manage PCOS.13,20,49
Participants also described finding a lack of empathy and concern in doctors when explaining symptoms or seeking care, similar to other studies.36,39,41,42,50 A lack of concern in doctors particularly affected younger patients, who grew to lose concern themselves and delayed managing their symptoms for several years. Adolescents with PCOS can struggle to cope with their condition and may require additional guidance from physicians in the management of PCOS.42,50,51
Some participants who were overweight or obese perceived weight bias in physicians. Participants felt that their physicians investigated symptoms less, pinning the cause of symptoms on weight instead of exploring patients’ concerns, and assumed the state of the participant's lifestyle modification. Curiously, many participants who struggled to lose weight and perceived a weight bias described their doctors as not offering any guidance on lifestyle management. Weight bias is common and can have adverse health consequences, especially for patients struggling with eating disorders, as many with PCOS do.52,53
Special consideration is needed from doctors to follow up with and guide women with PCOS in perimenopause and postmenopause. Perimenopausal and postmenopausal participants managing PCOS were frustrated with how little information and guidance they received from doctors after being taken off their prescriptions, and largely self-educated and self-experimented with treatments. Women with PCOS in their 40s and older have a higher prevalence of hypertension and triglycerides54 and are more likely to have insulin resistance compared with women without PCOS.55 More research is needed with this population of women with PCOS to better understand their needs and the practices of PCPs and specialists.
Limitations and strengths
The limitations of the study include self-reported diagnoses of PCOS, small sample size and uneven distribution of age groups. Selection bias is possible due to all participants being recruited from websites and online groups, eliminating the potential to reach women with PCOS who are not as active online. Only three participants aged >40 y were recruited. Most participants identified as Caucasian; few participants from diverse ethnic backgrounds were captured. Limited conclusions can be drawn regarding other world regions. Member checking, where participants are given an opportunity to review findings and provide feedback, was not performed, because participant contact information was not recorded and permission was not sought to contact the interviewees. A strength of this study included the involvement of perimenopausal and postmenopausal women whose experiences and beliefs may not be transferable from the experiences of women of reproductive age. Previous qualitative studies largely involved women aged <50 y.35–37,41
Conclusion
Lived experiences in this study point to a need to better support women with PCOS in Canada. Further awareness about PCOS may be needed in the medical community. Healthcare providers in Canada are encouraged to provide ample information about PCOS (e.g. pamphlets, acknowledged websites) and understand its biopsychosocial implications. Guidance is needed in lifestyle management, including referrals to allied health professionals to aid patients in reaching their health goals.
Policy recommendations
Education for healthcare professionals, especially PCPs, on evidence-based management of PCOS may be needed. Several international evidence-based guidelines and reviews13,20,56 have been established for the diagnosis and management of PCOS, which can be consulted by clinicians in practice. The guidelines inform regarding the necessary information to provide and the importance of screening and long-term follow-up, accounting for the individual needs and risk profiles of the patients. PCOS awareness may need greater integration in Canadian medical curriculums.
Future research
Future research is needed to explore the experiences of immigrant women and women from diverse ethnic backgrounds accessing care for PCOS in Canada, who may experience barriers to care not captured in this study. Immigrant populations with PCOS in Canada and patients in low- and middle-income countries may face additional barriers to PCOS management, such as poorer health-related quality of life due to infertility57,58 and a greater cardiometabolic risk.59 Social support was an important facilitator to participants in this study; women with PCOS living in countries with greater stigma towards infertility may face additional barriers in finding support.58,60 Further research is necessary to identify the unique barriers and facilitators that women coming from diverse cultural and economic backgrounds may experience in Canada and other countries.
PCOS has a high healthcare-related economic burden; comprehensive screening and counseling from physicians and greater public awareness can curtail morbidity and reduce the economic burden on both the patient and the healthcare system.61,62 Little is known about public awareness of PCOS in Canada and internationally. Recent studies conducted in South and Central Asia have found a need for greater PCOS awareness in girls and women,34,63,64 as well as physicians.65 More international studies are needed to examine cultural and environmental barriers and facilitators to patients seeking care for PCOS.
Individuals with PCOS who may not identify as women may also have unique needs in management that were not captured by this study. Studies on physician populations are needed to gauge PCOS awareness and to inform education efforts. Further studies are needed with perimenopausal and postmenopausal women with PCOS, whose needs and experiences seeking care are not fully understood. Women with conditions other than PCOS, such as fibroids or endometriosis, may have similar experiences managing those conditions; future research is needed to understand those experiences better.
Supplementary Material
Acknowledgements
We thank all the women who participated in this research. Thanks also to the PCOS Awareness Association for assistance with participant recruitment and to Dr. Angel Foster for help in developing the interview guide.
Contributor Information
Miya Ismayilova, Interdisciplinary School of Health sciences, University of Ottawa, 25 University Private, Ottawa, ON K1N 7K4, Canada.
Sanni Yaya, University of Parakou, Faculty of Medicine, Parakou, Benin; School of International Development and Global Studies, University of Ottawa, 120 University Private, Ottawa, ON K1N 6N5, Canada.
Authors’ contributions
MI and SY contributed to the study design and conceptualization. MI coordinated and directed the data collection phase. Coding and analysis for quantitative and qualitative data were carried out by MI and overseen by SY. MI drafted the manuscript with input from SY. Both authors read and approved the final draft version of the manuscript.
Funding
There was no funding for this study.
Competing interests
The authors declare no conflicts of interest.
Ethical approval
Ethical approval for the study was received from the University of Ottawa Research Ethics Board on 13 April 2018. Participants were voluntarily enrolled in the study with free and informed consent. Participants were informed that once they chose to participate, they could withdraw their consent and data at any time and/or refuse to answer any questions, without experiencing any negative consequences. Permission to audio-record the remote interviews was sought and obtained before data collection. All personal identifiers were removed from the transcripts and from the quotations provided throughout the paper. Written or oral informed consent was obtained from all participants prior to their participation. This study was performed in accordance with the relevant guidelines and regulations of the Declaration of Helsinki. No consent to publish was needed for this study as we did not use any details, images or videos related to individual participants.
Data availability
The interview guide is publicly available; other data are available from the corresponding author upon reasonable request.
References
- 1. Bozdag G, Mumusoglu S, Zengin Det al. The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-analysis. Hum Reprod. 2016;31:2841–55. [DOI] [PubMed] [Google Scholar]
- 2. Gibson-Helm M, Tassone EC, Teede HJet al. The needs of women and healthcare providers regarding polycystic ovary syndrome information, resources, and education: A systematic search and narrative review. Semin Reprod Med. 2018;36:35–41. [DOI] [PubMed] [Google Scholar]
- 3. Al-Jefout M, Alnawaiseh N, Al-Qtaitat A. Insulin resistance and obesity among infertile women with different polycystic ovary syndrome phenotypes. Sci Rep. 2017;7:5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jeanes YM, Reeves S.. Metabolic consequences of obesity and insulin resistance in polycystic ovary syndrome: Diagnostic and methodological challenges. Nutr Res Rev. 2017;30:97–105. [DOI] [PubMed] [Google Scholar]
- 5. Lim SS, Davies MJ, Norman RJet al. Overweight, obesity and central obesity in women with polycystic ovary syndrome: A systematic review and meta-analysis. Hum Reprod Update. 2012;18:618–37. [DOI] [PubMed] [Google Scholar]
- 6. Cooney LG, Lee I, Sammel MDet al. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: A systematic review and meta-analysis. Hum Reprod. 2017;32:1075–91. [DOI] [PubMed] [Google Scholar]
- 7. Açmaz G, Albayrak E, Acmaz Bet al. Level of anxiety, depression, self-esteem, social anxiety, and quality of life among the women with polycystic ovary syndrome. Sci World J. 2013;2013:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Damone AL, Joham AE, Loxton Det al. Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychol Med. 2019;49:1510–20. [DOI] [PubMed] [Google Scholar]
- 9. Himelein MJ, Thatcher SS.. Depression and body image among women with polycystic ovary syndrome. J Health Psychol. 2006;11:613–25. [DOI] [PubMed] [Google Scholar]
- 10. Bates GW, Legro RS.. Longterm management of polycystic ovarian syndrome (PCOS). Mol Cell Endocrinol. 2013;373:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ruan X, Li M, Mueck AO.. Why does polycystic ovary syndrome (PCOS) need long-term management? Curr Pharm Des. 2019;24:4685–92. [DOI] [PubMed] [Google Scholar]
- 12. Wolf WM, Wattick RA, Kinkade ONet al. The current description and future need for multidisciplinary PCOS clinics. J Clin Med. 2018;7:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Teede HJ, Misso ML, Costello MFet al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018;110:364–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sanchez N. A life course perspective on polycystic ovary syndrome. IJWH. 2014;22:115–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Welt CK, Carmina E. Lifecycle of polycystic ovary syndrome (PCOS): from in utero to menopause. J Clin Endocrinol Metab. 2013;98:4629–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dokras A, Witchel SF.. Are young adult women with polycystic ovary syndrome slipping through the healthcare cracks? J Clin Endocrinol Metab. 2014;99:1583–5. [DOI] [PubMed] [Google Scholar]
- 17. Moran LJ, Ranasinha S, Zoungas Set al. The contribution of diet, physical activity and sedentary behaviour to body mass index in women with and without polycystic ovary syndrome. Hum Reprod. 2013;28:2276–83. [DOI] [PubMed] [Google Scholar]
- 18. Balen AH. Polycystic ovary syndrome (PCOS). Obstet Gynecol. 2017;19:119–29. [Google Scholar]
- 19. Jeanes YM, Barr S, Smith Ket al. Dietary management of women with polycystic ovary syndrome in the United Kingdom: the role of dietitians. J Hum Nutr Diet. 2009;22:551–8. [DOI] [PubMed] [Google Scholar]
- 20. Hoeger KM, Dokras A, Piltonen T.. Update on PCOS: consequences, challenges, and guiding treatment. J Clin Endocrinol Metab. 2020;106:e1071–83. [DOI] [PubMed] [Google Scholar]
- 21. Ching HL, Burke V, Stuckey BGA.. Quality of life and psychological morbidity in women with polycystic ovary syndrome: body mass index, age and the provision of patient information are significant modifiers. Clin Endocrinol. 2007;66:373–9. [DOI] [PubMed] [Google Scholar]
- 22. Avery JC, Braunack-Mayer AJ.. The information needs of women diagnosed with polycystic ovarian syndrome – implications for treatment and health outcomes. BMC Women's Health. 2007;7:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gibson-Helm M, Teede H, Dunaif Aet al. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2017;102:604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dokras A, Saini S, Gibson-Helm Met al. Gaps in knowledge among physicians regarding diagnostic criteria and management of polycystic ovary syndrome. Fertil Steril. 2017;107:1380–6. [DOI] [PubMed] [Google Scholar]
- 25. Gibson-Helm M, Dokras A, Karro Het al. Knowledge and practices regarding polycystic ovary syndrome among physicians in Europe, North America, and internationally: An online questionnaire-based study. Semin Reprod Med. 2018;36:19–27. [DOI] [PubMed] [Google Scholar]
- 26. Chemerinski A, Cooney L, Shah Det al. Knowledge of PCOS in physicians-in-training: identifying gaps and educational opportunities. Gynecol Endocrinol. 2020;36:854–9. [DOI] [PubMed] [Google Scholar]
- 27. Tomlinson J, Letherby G, Pinkney Jet al. Raising awareness of polycystic ovary syndrome. Nursing Standard. 2013;27:35–9. [DOI] [PubMed] [Google Scholar]
- 28. Ismayilova M, Yaya S . “I felt like she didn’t take me seriously”: a multi-methods study examining patient satisfaction and experiences with polycystic ovary syndrome (PCOS) in Canada. BMC Womens Health. 2022;22:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Statistics Canada . Analysis : Population by age and sex. Annual Demographic Estimates: Canada, Provinces and Territories, 2018; 2018. [Google Scholar]
- 30. Thorne S, Kirkham SR, O'Flynn-Magee K.. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3:1–11. [Google Scholar]
- 31. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 32. Tong A, Sainsbury P, Craig J.. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. [DOI] [PubMed] [Google Scholar]
- 33. Lin AW, Bergomi EJ, Dollahite JSet al. Trust in physicians and medical experience beliefs differ between women with and without polycystic ovary syndrome. J Endocrine Soc. 2018;2:1001–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wasata R, Chertok IRA, Kingori Cet al. Exploratory study of knowledge and experience of polycystic ovary syndrome (PCOS) among PCOS-diagnosed Bangladeshi women. JWHCI. 2020;3:1–9. [Google Scholar]
- 35. Ee C, Smith C, Moran Let al. “the whole package deal”: Experiences of overweight/obese women living with polycystic ovary syndrome. BMC Women's Health. 2020;20:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Soucie K, Samardzic T, Schramer Ket al. The diagnostic experiences of women with polycystic ovary syndrome (PCOS) in Ontario, Canada. Qual Health Res. 2021;31:523–34. [DOI] [PubMed] [Google Scholar]
- 37. Williams S, Sheffield D, Knibb RC.. ‘Everything's from the inside out with PCOS’: Exploring women's experiences of living with polycystic ovary syndrome and co-morbidities through SkypeTM interviews. Health Psychol Open. 2015;2:2055102915603051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sterling EW, Vincent T, DeZarn Cet al. A study of perceptions, experiences, and satisfaction with healthcare among women with polycystic ovary syndrome (PCOS). Fertil Steril. 2010;94:S7. [Google Scholar]
- 39. Crete J, Adamshick P.. Managing polycystic ovary syndrome: What our patients are telling us. J Holist Nurs. 2011;29:256–66. [DOI] [PubMed] [Google Scholar]
- 40. Colwell K, Lujan ME, Lawson KLet al. Women's perceptions of polycystic ovary syndrome following participation in a clinical research study: implications for knowledge, feelings, and daily health practices. J Obstet Gynaecol Can. 2010;32:453–9. [DOI] [PubMed] [Google Scholar]
- 41. Tomlinson J, Pinkney J, Adams Let al. The diagnosis and lived experience of polycystic ovary syndrome: A qualitative study. J Adv Nurs. 2017;73:2318–26. [DOI] [PubMed] [Google Scholar]
- 42. Weiss TR, Bulmer SM.. Young women's experiences living with polycystic ovary syndrome. J Obst Gynecol Neonat Nursing. 2011;40:709–18. [DOI] [PubMed] [Google Scholar]
- 43. Bazarganipour F, Taghavi SA, Allan Het al. Facilitating and inhibiting factors related to treatment adherence in women with polycystic ovary syndrome: A qualitative study. Int J Reprod Biomed. 2017;15:553–60. [PMC free article] [PubMed] [Google Scholar]
- 44. Humphreys L, Costarelli V.. Implementation of dietary and general lifestyle advice among women with polycystic ovarian syndrome. J Royal Soc Promot Health. 2008;128:190–5. [DOI] [PubMed] [Google Scholar]
- 45. Mulquiney KJ, Tapley A, van Driel MLet al. Referrals to dietitians/nutritionists: A cross-sectional analysis of Australian GP registrars’ clinical practice. Nutrition Dietetics. 2018;75:98–105. [DOI] [PubMed] [Google Scholar]
- 46. Lim S, Smith CA, Costello MFet al. Barriers and facilitators to weight management in overweight and obese women living in Australia with PCOS: a qualitative study. BMC Endocr Disord. 2019;19:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cipkala-Gaffin J, Talbott EO, Song MKet al. Associations between psychologic symptoms and life satisfaction in women with polycystic ovary syndrome. J Women's Health. 2012;21:179–87. [DOI] [PubMed] [Google Scholar]
- 48. Sirmans SM, Parish RC, Blake Set al. Epidemiology and comorbidities of polycystic ovary syndrome in an indigent population. J Investig Med. 2014;62:868–74. [DOI] [PubMed] [Google Scholar]
- 49. Lee I, Dokras A. Mental health and body image in polycystic ovary syndrome. Curr Opin Endocr Metab Res. 2020;12:85–90. [Google Scholar]
- 50. Jones GL, Hall JM, Lashen HLet al. Health-related quality of life among adolescents with polycystic ovary syndrome. J Obst Gynecol Neonat Nursing. 2011;40:577–88. [DOI] [PubMed] [Google Scholar]
- 51. Hopkins CS, Kimble LP, Hodges HFet al. A mixed-methods study of coping and depression in adolescent girls with polycystic ovary syndrome. J Am Assoc Nurse Pract. 2019;31:189–97. [DOI] [PubMed] [Google Scholar]
- 52. Alberga AS, Russell-Mayhew S, von Ranson KMet al. Weight bias: a call to action. J Eating Disord. 2016;4:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Tay CT, Teede HJ, Hill Bet al. Increased prevalence of eating disorders, low self-esteem, and psychological distress in women with polycystic ovary syndrome: a community-based cohort study. Fertil Steril. 2019;112:353–61. [DOI] [PubMed] [Google Scholar]
- 54. Schmidt J, Brännström M, Landin-Wilhelmsen Ket al. Reproductive hormone levels and anthropometry in postmenopausal women with polycystic ovary syndrome (PCOS): A 21-year follow-up study of women diagnosed with PCOS around 50 years ago and their age-matched controls. J Clin Endocrinol Metab. 2011;96:2178–85. [DOI] [PubMed] [Google Scholar]
- 55. Puurunen J, Piltonen T, Morin-Papunen Let al. Unfavorable hormonal, metabolic, and inflammatory alterations persist after menopause in women with PCOS. J Clin Endocrinol Metab. 2011;96:1827–34. [DOI] [PubMed] [Google Scholar]
- 56. Teede HJ, Misso ML, Boyle JAet al. Translation and implementation of the Australian-led PCOS guideline: clinical summary and translation resources from the International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. Med J Aust. 2018;209:S3–8. [DOI] [PubMed] [Google Scholar]
- 57. Schmid J, Kirchengast S, Vytiska-Binstorfer Eet al. Infertility caused by PCOS—health-related quality of life among Austrian and Moslem immigrant women in Austria. Hum Reprod. 2004;19:2251–7. [DOI] [PubMed] [Google Scholar]
- 58. Sharma S, Mishra AJ.. Tabooed disease in alienated bodies: A study of women suffering from polycystic ovary syndrome (PCOS). Clin Epidemiol Global Health. 2018;6:130–6. [Google Scholar]
- 59. Kudesia R, Illions EH, Lieman HJ.. Elevated prevalence of polycystic ovary syndrome and cardiometabolic disease in South Asian infertility patients. J Immigrant Minority Health. 2017;19:1338–42. [DOI] [PubMed] [Google Scholar]
- 60. Hadjiconstantinou M, Mani H, Patel Net al. Understanding and supporting women with polycystic ovary syndrome: a qualitative study in an ethnically diverse UK sample. Endocr Connect. 2017;6:323–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Azziz R, Marin C, Hoq Let al. Health care-related economic burden of the polycystic ovary syndrome during the reproductive life Span. J Clin Endocrinol Metab. 2005;90:4650–8. [DOI] [PubMed] [Google Scholar]
- 62. Riestenberg C, Jagasia A, Markovic Det al. Health care-related economic burden of polycystic ovary syndrome in the United States: pregnancy-related and long-term health consequences. J Clin Endocrinol Metab. 2022;107:575–85. [DOI] [PubMed] [Google Scholar]
- 63. Pitchai P, Sreeraj SR, Anil PR. Awareness of lifestyle modification in females diagnosed with polycystic ovarian syndrome in India: explorative study. Int J Reprod Contracept Obstet Gynecol. 2016;5:470–6. [Google Scholar]
- 64. Rajkumari P, Sahoo J, Sujata Pet al. Awareness about PCOS and the likelihood of its symptoms in adolescent girls in a semi-urban set-up: a cross sectional study. J Med Sci Clin Res. 2016;4:14264–9. [Google Scholar]
- 65.Rostami Dovom M, Ahmady S, Amirshekari Get al. Awareness and performance of Iranian general practitioners in diagnosis and clinical management of polycystic ovary syndrome. Iran J Endocrinol Metabol. 2021;22:445. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The interview guide is publicly available; other data are available from the corresponding author upon reasonable request.