Abstract
Background
Little is known about coronavirus disease 2019 (COVID-19) vaccination in Africa. We sought to understand Malawian healthcare workers’ (HCWs’) COVID-19 vaccination and its hypothesized determinants.
Methods
In March 2021, as the COVID-19 vaccine roll-out commenced in Malawi, we surveyed clinical and lay cadre HCWs (n=400) about their uptake of the vaccine and potential correlates (informed by the WHO Behavioral and Social Drivers of COVID-19 Vaccination framework). We analyzed uptake and used adjusted multivariable logistic regression models to explore how ‘what people think and feel’ constructs were associated with HCWs' motivation to be vaccinated.
Results
Of the surveyed HCWs, 82.5% had received the first COVID-19 vaccine dose. Motivation (eagerness to be vaccinated) was strongly associated with confidence in vaccine benefits (adjusted OR [aOR] 9.85, 95% CI 5.50 to 17.61) and with vaccine safety (aOR 4.60, 95% CI 2.92 to 7.23), but not with perceived COVID-19 infection risk (aOR 1.38, 95% CI 0.88 to 2.16). Of all the information sources about COVID-19 vaccination, 37.5% were reportedly negative in tone.
Conclusions
HCWs in Malawi have a high motivation to be vaccinated and a high COVID-19 vaccine uptake. Disseminating vaccine benefits and safety messages via social media and social networks may be persuasive for individuals who are unmotivated to be vaccinated and less likely to accept the COVID-19 vaccine.
Keywords: COVID-19, healthcare workers, vaccine hesitancy, vaccines
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused >5.9 million deaths worldwide at the time of writing, and its destruction is far from over.1 Countries in Southern Africa have experienced catastrophic recent increases in cases (‘waves’).2 The case fatality ratio appears to be highest in low-income countries, potentially reflecting weaker health systems with less capacity to manage COVID-19 complications, as well as a high prevalence of potentially exacerbating conditions including HIV, TB and chronic comorbidities.3
High COVID-19 vaccine coverage in low- and middle-income countries is likely to be extremely cost-effective and save millions of lives.4 There are however major global inequities in access to COVID-19 vaccines,5,6 and gaps in our knowledge of factors likely to be associated with COVID-19 vaccine uptake and acceptability, which has primarily come from high-income countries.7,8 The scant literature about COVID-19 vaccination from Africa to date has focused on COVID-19 vaccine acceptability and hesitancy rather than actual vaccination behaviors.9–12 A recent pooled analysis found that 80% of survey respondents from low- and middle-income countries expressed a willingness to be vaccinated,13 but data from Africa about COVID-19 vaccine uptake are still very limited. Although attitudes are an important precursor to vaccination behavior, stated acceptability may not correlate with actual uptake and different factors may influence acceptability vs uptake.14,15 It is therefore essential to study behavior (vaccine uptake) as well as the full range of potential drivers, including attitudes and their determinants.
The Ministry of Health (MOH) has reported >63 000 COVID-19 cases and 2311 deaths (a case fatality rate of 3.6%)16 in Malawi (as of 16 December 2021), although testing is limited and findings from elsewhere in Africa indicate that the actual seroprevalence may be much higher.17,18 Several factors have potentially exacerbated Malawi's COVID-19 situation, including proximity to very high-burden countries like South Africa,2 low knowledge and perceived risk of COVID-1919 and limited uptake of preventive measures like mask-wearing.20 On 5 March 2021, the first COVID-19 vaccine doses arrived in Malawi21; nearly 980 000 first doses, and 366 000 second doses, of the Serum Institute-AstraZeneca COVID-19 vaccine (COVISHIELD), had been distributed nationally as of 16 December 2021.16,21 As there are nearly 10 million adult Malawians, COVID-19 vaccine availability is relatively limited to date.
Given the scarcity of information from low-income countries about factors related to the uptake of, and attitudes toward, the COVID-19 vaccine, we undertook a survey of Malawian healthcare workers (HCWs) as the vaccine was being introduced, because these individuals were prioritized for vaccination.21 Achieving high COVID-19 vaccine coverage among HCWs is important because HCWs are at an elevated risk of infection, are essential to ensure continuity of safe medical service provision,22,23 and they strongly influence vaccine uptake among their patients.24–26
The objective of this analysis was to identify correlates of vaccine uptake and motivation among HCWs in Malawi, informed by the WHO behavioral and social drivers (BeSD) framework of COVID-19 vaccination.27
Materials and Methods
Study design
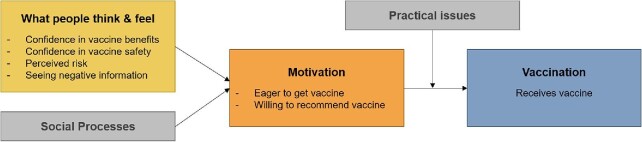
This was a cross-sectional survey of HCWs in Malawi, informed by the WHO BeSD framework, as it has been adapted for COVID-19 vaccination among HCWs (Figure 1).27
Figure 1.
Conceptual framework for this study, adapted from the WHO BeSD framework of COVID-19 vaccination.27 Boxes in gray are constructs unmeasured in this study.
Site and participant selection
We recruited and surveyed HCWs from 32 health facilities in Central and Southern Malawi. Sites were selected purposefully from among those supported by the Partners in Hope HIV Care and Treatment program to include government community hospitals (n=3, all rural) and district hospitals (n=6, all urban/peri-urban), faith-based hospitals run by the Christian Health Association of Malawi (n=7, three urban/peri-urban and four rural) and larger health centers (n=16, all rural except for one urban/peri-urban). Beginning on 15 March 2021, all HCWs at these sites were offered the Serum Institute-AstraZeneca COVISHIELD vaccine. Vaccination was optional and was offered on-site free of charge.
At each site, we identified eligible respondents: HCWs (stratified into clinical and non-clinical cadres, including Partners in Hope staff and government employees) aged ≥18 y who provided outpatient HIV care during the 3 mo preceding data collection and did not provide COVID-19 care. Clinical providers included physicians, clinical officers (who complete 3 y of training and a 1-y internship), medical assistants (who complete 2 y of training) and nurses. Non-clinical cadres included workers who support HIV treatment, counseling, health promotion and community-based care (i.e. HIV diagnostic assistants [HDAs], health surveillance assistants [HSAs] and patient supporters), as well as data clerks and antiretroviral therapy (ART) clerks, who are involved in data entry and reporting. At each facility, we generated a census of individuals and selected one at random per stratum to invite for participation; we repeated this process until up to 14 participants per facility were invited to participate.
Data collection
The survey tool incorporated modules from the OCEANS study, which surveyed British adults about their attitudes toward the COVID-19 vaccine28; and from the Vaccine Hesitancy Scale.29 We also asked respondents about their experiences with COVID-19, sources of information about COVID-19 vaccine and demographic information. The survey instrument was developed in English, translated to Chichewa, then back-translated to English; bilingual (English-Chichewa) members of the research team reviewed and revised the Chichewa-language tool to ensure correct meaning and intention. The survey was administered in private spaces by a trained research assistant using the SurveyCTO mobile data collection platform on an Android tablet. Research assistants read each survey question aloud to each respondent and logged all responses. All respondents gave oral informed consent before beginning the survey. Data were collected completely anonymously, with no names or identifying information that could be traced to the individual by Partners in Hope or their employer. Data were collected from 31 March to 5 May 2021.
Key variables and outcomes
The outcome of vaccine uptake (‘vaccination’ in the BeSD framework) was defined as a self-reported receipt of a COVID-19 vaccine dose. At the time of this survey, as vaccine distribution had recently commenced, no respondent was yet eligible for a second vaccine dose. People who reported an upcoming vaccine appointment, or being ineligible for the vaccine per Malawi MOH guidelines (pregnant and breastfeeding women, under the age of eligibility, or recent COVID-19 infection), were excluded from this analysis. People who had been offered but had not received the COVID-19 vaccine were therefore considered ‘decliners’ if they did not self-report ineligibility as per the guidelines.
The intermediate outcome of ‘motivation’ was operationalized based on survey responses as: (1) whether the respondent was eager or willing to receive the COVID-19 vaccine (vs not bothered about, unwilling to or extremely opposed to receiving it); and (2) whether the respondent would encourage family or friends who were thinking of getting the COVID-19 vaccine (vs would not say anything, would ask them to delay or would suggest they should not get the vaccine).
Respondents were classified as having ‘confidence in vaccine benefits’ if they reported: (1) the COVID-19 vaccine would save a lot of lives (vs save some lives or have no impact); and (2) the COVID-19 vaccine would strengthen their immune system (vs would weaken or have no effect on their immune system). ‘Confidence in vaccine safety’ was measured through survey questions about whether rapidly developed vaccines are unsafe and anticipated prevalence and severity of short- and long-term side effects from the COVID-19 vaccine. Respondents with ‘high perceived risk’ were those who thought they definitely, probably or possibly would be infected with COVID-19 in the next 12 mo (vs probably not or definitely not) and those who thought that they would get very ill from COVID-19 (vs have mild flu or symptoms that would hardly be noticeable).
Respondents were asked whether they had heard any information or opinions about any COVID-19 vaccine from each of a variety of sources (including family, media, religious leaders) and, if so, whether they would characterize the information/opinions from that source as overall positive, overall negative or neutral. No timeframe was specified for these questions. Each respondent was given a negative information exposure ‘score’ (1 point per negative information source) and a negative information ‘share’, that is, the percentage of all information sources seen/heard that was reportedly negative in tone. (As all respondents had been offered the vaccine and knew someone vaccinated, this analysis did not measure constructs related to ‘social processes’ or ‘practical issues’ from the WHO BeSD framework.)
Data analysis
We first estimated COVID-19 vaccine uptake for the full sample and by respondent characteristic (gender, age, job title/cadre, number of comorbidities [zero, one or more than one of high blood pressure, diabetes, lung or heart disease] and underlying vaccine hesitancy [proxied by whether the respondent expressed concern about the safety of routine childhood vaccines]). We then calculated the correlation between having high motivation (as defined above) and uptake of the vaccine. Based on multivariable logistic regression models that included respondent characteristics, we estimated the marginal probability that more or less motivated individuals had been vaccinated. Next, through a series of multivariable logistic regression models, we assessed whether ‘what people think and feel’ was correlated with motivation to be vaccinated (as described above). Lastly, we calculated the ‘prevalence’ of exposure to negative information about the COVID-19 vaccine by source. All the regression models included standard errors clustered at the sampling level (health facility).
Results
A total of 435 surveys were completed; 35 responses were excluded from this analysis as they were ineligible for COVID-19 vaccination or had an upcoming appointment to be vaccinated, resulting in an analytical sample of 400 respondents.
Description of the sample
The respondents’ median age was 32 (IQR: 28, 38) y and 77.8% reported no comorbidities (such as high blood pressure, diabetes, lung or heart disease) (Table 1). Approximately one-third of respondents were clinical staff (physicians, clinical officers, nurses and medical assistants) and the remainder were lay cadres involved in health promotion, counseling and community-based care (HDAs, HSAs, patient supporters, ART clerks and data clerks) (Table 1).
Table 1.
Description of the sample
| n (%) | |
|---|---|
| Gender | |
| Female | 179 (44.8%) |
| Male | 221 (55.3%) |
| Age, y | |
| Average (range) | 33.8 (20-60) |
| Median (IQR) | 32 (28, 38) |
| Cadre | |
| Physician or clinical officer | 34 (8.5%) |
| Medical assistant | 32 (8.0%) |
| Nurse | 71 (17.8%) |
| HDA/HSA1 | 104 (26.0%) |
| Patient supporter | 83 (20.8%) |
| Data clerk | 69 (17.3%) |
| ART clerk | 7 (1.8%) |
| Number of comorbidities2 | |
| 0 | 311 (77.8%) |
| 1 | 58 (14.5%) |
| ≥2 | 31 (7.8%) |
| Underlying attitudes towards childhood vaccines | |
| Agree (vs disagree or don't know) that: Childhood vaccines are effective | 397 (99.3%) |
| Agree (vs disagree or don't know) that: Having children vaccinated is important for the health of people in the community | 398 (99.5%) |
| Agree (vs disagree or don't know) that: Getting vaccines is a good way to protect children from disease | 398 (99.5%) |
| Agree (vs disagree or don't know) that: I am concerned about serious adverse effects of childhood vaccines | 21 (5.3%) |
| Total | 400 (100%) |
1HDA, HIV diagnostic assistant; HSA, health surveillance assistant.
2High blood pressure, diabetes, lung or heart disease.
Over two-thirds of respondents (n=284, 71.0%) knew someone who had died from COVID-19, most commonly a friend or acquaintance (n=199), a family member outside the household (n=52), a patient/client (n=52) or a coworker (n=48). Fifty respondents (12.5%) said they had been infected with COVID-19, but only 15 of these were reportedly laboratory-confirmed cases.
Uptake of the COVID-19 vaccine
Most respondents (82.5%, n=330) had received one dose of the COVID-19 vaccine by the time of the survey, and 17.5% (n=70) had declined the vaccine. No relationships between vaccine uptake and demographic or background characteristics were significant at the p<0.05 level, although some suggestive findings emerged (Supplementary Table 1). Uptake was lower among lay cadres (79.9% vs 87.6% of clinical staff), younger respondents (74.2% of those aged 20–29 y vs >85% among respondents aged >30 y), people without any comorbidities (81.4% vs 86.5% among people with one or more comorbidities) and people who were concerned about the safety of routine childhood vaccines (66.7% vs 83.4% among those who were not concerned).
Among respondents who had received one COVID-19 vaccine dose, nearly all (n=312, 94.5%) intended to receive a second dose (second doses had not commenced at the time of the survey). After receiving the first vaccine dose, 20.3% of respondents said they experienced no side effects (n=67), 29.1% experienced mild side effects (n=96), 42.1% experienced moderate side effects (n=139) and 8.5% experienced severe side effects (n=28).
The most common reasons for declining vaccination were a fear of side effects (n=36), challenges with vaccine supply/access (n=8), not feeling that the vaccine is necessary (n=7) and still feeling unsure/undecided (n=7).
Motivation towards the COVID-19 vaccine
Overall, 59.8% of respondents were eager or willing to be vaccinated and 85.8% said they would encourage friends or family to get the vaccine (Table 2, Supplementary Figure 1). Both types of motivation were strongly associated with the respondent's vaccination status.
Table 2.
Associations between motivation and vaccination behavior (n=400)
| n (%) expressing this | aOR vaccine uptake (vs decline), 95% CI | |
|---|---|---|
| Willing or eager to be vaccinated (vs not bothered, unwilling, opposed) | 239 (59.8%) | 12.22*** (5.48 to 27.22) |
| Would encourage friends/family to vaccinate (vs not say anything, ask them to delay) | 343 (85.8%) | 16.54*** (9.36 to 29.22) |
aOR includes: gender (male, female), age (continuous), cadre (MD/clinical officer, medical assistant, nurse, HDA/HSA, patient supporter, data clerk/monitor, ART clerk), presence of comorbidities (none, 1, 2 or more). Standard errors clustered by health facility.
***p<0.001.
Determinants of COVID-19 vaccine motivation
Most respondents expressed confidence in the benefits of the COVID-19 vaccine (Table 3): 74.0% felt that vaccination would save lives (no one said the vaccine would lead to more deaths); and 89.8% agreed that the vaccine would strengthen their immune system (only one person said the vaccine would weaken their immune system). In models that adjusted for respondent characteristics, agreeing with either of these statements was strongly and significantly associated with positive vaccination motivation, both willingness/eagerness to be vaccinated (adjusted OR [aOR] 9.85, 95% CI 5.50 to 17.62) and encouraging friends and family to be vaccinated (aOR 4.89, 95% CI 2.48 to 9.60). Having confidence in vaccine safety was also significantly associated with motivation (aOR for willingness/eagerness to be vaccinated 4.60, 95% CI 2.92 to 7.23; aOR for encouraging friends and family 23.37, 95% CI 2.94 to 185.51), although most respondents expressed that vaccines developed quickly are unsafe (n=241, 60.3%). A small minority of respondents thought that significant or life-threatening vaccine side effects would be relatively prevalent (short- and long-term side effects thought to affect at least some vaccinated people by 13.0% and 8.8% of respondents, respectively).
Table 3.
Correlates of motivation toward COVID-19 vaccination (n=400)
| Construct | Operationalization | n (%) expressing this | aOR willing or eager to be vaccinated (95% CI) | aOR would encourage friends/family to be vaccinated (95% CI) |
|---|---|---|---|---|
| Confidence in vaccine benefits | If individuals like me get the COVID-19 vaccine it will save a lot of lives (vs save some lives or have no impact) | 296 (74.0%) | 9.85*** (5.50 to 17.62) | 4.89*** (2.48 to 9.60) |
| The COVID-19 vaccine will strengthen my immune system (vs will neither strengthen nor weaken, or will weaken) | 359 (89.8%) | 17.39*** (5.92 to 51.08) | 9.61*** (4.79 to 19.26) | |
| Confidence in vaccine safety | Vaccines that are developed quickly will be safe or safety will be unaffected (vs will be unsafe or very unsafe) | 159 (39.8%) | 4.60*** (2.92 to 7.23) | 23.37** (2.94 to 185.51) |
| At least some people (vs a few or none) will have significant or life-threatening (vs none or mild/moderate) side effects in the short term | 52 (13.0%) | 0.49* (0.27 to 0.90) | 0.31** (0.15 to 0.66) | |
| At least some people (vs a few or none) will have significant or life-threatening (vs none or mild/moderate) side effects in the long term | 35 (8.8%) | 0.39** (0.20 to 0.76) | 0.26** (0.10 to 0.67) | |
| Perceived risk | I possibly, probably or definitely will get COVID-19 in the next 12 mo (vs probably not or definitely not) | 164 (41.0%) | 1.38 (0.88 to 2.16) | 1.07 (0.58 to 1.96) |
| If I got COVID-19, I would probably end up in hospital, would get quite ill or it would be like a mild flu (vs it would be hardly noticeable or I'd have no symptoms) | 253 (63.7%) | 1.18 (0.81 to 1.71) | 1.08 (0.56 to 2.08) | |
| Seeing negative information | Number of sources of negative information | Median: 4 | 0.93 (0.84 to 1.02) | 0.81** (0.69 to 0.95) |
| Percentage of all information sources negative in tone | Median: 35.7% | 0.33 (0.11 to 1.06) | 0.05** (0.01 to 0.38) |
aOR includes: gender (male, female), age (continuous), cadre (physician/clinical officer, medical assistant, nurse, HDA/HSA, patient supporter, data clerk/monitor, ART clerk), presence of comorbidities (none, 1, 2 or more). Standard errors clustered by health facility.
*p<0.05; **p<0.01; ***p<0.001.
Perceived risk of COVID-19 infection was not significantly associated with motivation to receive the vaccine. The 41.0% of respondents who thought it was possible (or likely) that they would be infected with COVID-19 in the next 12 mo were no more likely than those who thought it was unlikely to express willingness/eagerness to be vaccinated (aOR 1.38, 95% CI 0.88 to 2.16) or to encourage their loved ones to be vaccinated (aOR 1.07, 95% CI 0.58 to 1.96). Similarly, people who felt that contracting COVID-19 would result in serious or mild illness (63.7% of respondents) were no more likely to express a positive motivation to receive the vaccine than those who did not feel that a COVID-19 infection would be severe.
Exposure to negative information was common, with participants reporting exposure to a median of four negative sources of information about COVID-19 vaccination, and 35.7% of all information sources about COVID-19 vaccination were negative in tone. Greater exposure to negative information was significantly associated with being less likely to encourage loved ones to be vaccinated (number of negative sources: aOR 0.81, 95% CI 0.69 to 0.95; percentage of all information sources negative in tone: aOR 0.05, 95% CI 0.01 to 0.38), but was not associated with one's own willingness/motivation to be vaccinated (number of negative sources: aOR 0.93, 95% CI 0.84 to 1.02; percentage of all information sources negative in tone: aOR 0.33, 95% CI 0.11 to 1.06).
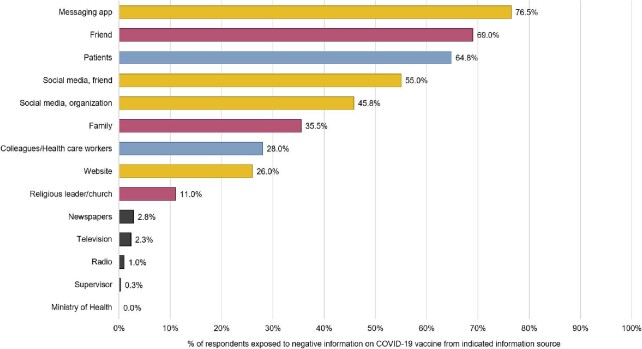
We assessed respondents’ exposure to specific sources of information (Figure 2). The most common sources of negative information were messaging apps (reported by 76.5% of respondents), friends (69.0%), patients (64.8%), social media posts by first-hand contacts such as friends and family (55.0%) and social media posts by others such as companies and organizations (45.8% of respondents).
Figure 2.
Sources of negative information about the COVID-19 vaccine. The figure shows the % of respondents reporting they heard information that was negative in tone from that source (vs heard no information, or heard information that was positive, neutral or indeterminate in tone). Participants could report multiple sources. Bar colors correspond to categories of information type: yellow: internet/virtual sources; purple: word-of-mouth from friends and family; blue: word-of-mouth at work; black: traditional media.
Discussion
This survey found a high uptake—>80%—of the COVID-19 vaccine among HCWs in Malawi at the time of the national vaccination program launch and following a surge in COVID-19 cases. However, results among HCWs should be generalized with caution (but do match other findings of high vaccine acceptability in low- and middle-income countries13), particularly because lay HCWs were less likely to accept the vaccine (just under 80% vs nearly 90% among clinical cadres), so the population-level average may be closer to this value. Similarly, studies from high-income countries have found that lower-cadre workers were more likely to decline the COVID-19 vaccine.30,31 How HCWs’ acceptance of vaccinations compares with the general public is an important area for future research.
We estimate a substantial difference in likelihood that a respondent had received the COVID-19 vaccine if they expressed a high vs low motivation to be vaccinated. Motivation to be vaccinated was strongly associated with confidence in vaccine benefits and safety, but not with perceived risks of COVID-19 infection or severe disease. This could be due to respondents’ attitudes about the AstraZeneca COVID-19 vaccine's efficacy against virus variants predominant in Malawi at the time, as per scientific publications32 and news reports to this effect. This suggests which specific determinants may be particularly important for influencing motivation and, consequently, uptake; emphasizing vaccine safety and general vaccine benefits may be more impactful in this context than communicating the risk of infection.
Many respondents reported hearing negative information about the COVID-19 vaccine from a variety of sources. Social relationships and social media were particularly common sources of negative information about the COVID-19 vaccine. Of particular note, over three-quarters of respondents had encountered negative information via messaging apps. This information about specific social media sources disseminating negative information can guide the targeted placement of factual vaccine information. This is particularly important given the association between exposure to negative information and vaccination motivation, in particular whether the respondent would encourage loved ones to be vaccinated. Interestingly, exposure to negative information was not associated with HCWs’ own willingness/motivation to be vaccinated, potentially suggesting that while HCWs’ occupation and education may ‘insulate’ them from the influence of negative information on their own vaccination attitudes, negative information may still shape how they feel about the importance of vaccination for others.
Some limitations of this study should be noted. First, this was a limited population—HCWs in Malawi—so results should be generalized with caution. By including lay cadres, however, we tried to include respondents who better represent the general population. Uptake of the COVID-19 vaccine in this sample was also very high, so further work is needed to understand attitudes and behaviors in different populations. Second, this was a cross-sectional study conducted as the vaccine was being introduced in Malawi and following a COVID-19 surge; attitudes and uptake may change over time as the pandemic continues and roll-out expands. We found no evidence of changing uptake over the study period, but a time trend could emerge over a longer period. This analysis could only examine correlations, and no causal relationships were explored given the cross-sectional study design. Third, we did not analyze the domains of ‘social processes’ and ‘practical issues’, both hypothesized to influence vaccine outcomes in the BeSD framework, as all respondents knew someone who had been vaccinated and had been offered the vaccine at their place of work, so there was no variation to explore. Our operationalization of who had declined the vaccine may also have been overly broad, as some eligible, unvaccinated respondents may have encountered logistical or other challenges to vaccination. Lastly, there are very few validated tools on this topic for use in low- and middle-income countries. There may also be social desirability and other biases in reporting vaccination attitudes and behaviors that are important to consider when creating tools for use in diverse settings. Our team tried to mitigate measurement error through careful selection of survey questions, and translation and back-translation of questions with review by multiple bilingual researchers. We encourage further research to develop culturally and contextually appropriate tools to improve the study of vaccine attitudes and behaviors in global contexts.
Conclusions
In this study of HCWs during the early weeks of COVID-19 vaccination in Malawi, a high proportion had accepted the offered vaccine. Vaccine uptake was likely associated with the perceived benefits and safety of the COVID-19 vaccine, and with exposure to negative vaccine information, which was very common in this sample, particularly from loved ones and via social media. Vaccine uptake in low- and middle-income countries, and its determinants, is relatively understudied, so these data offer important new insights about potentially modifiable factors. Future research should more robustly quantify differences across countries and settings, and qualitative research should seek to identify determinants and mechanisms, in order to inform intervention strategies for groups found to be less likely to be vaccinated. With information about what influences vaccine decisions and behaviors, the global health community can design effective implementation strategies and behavioral interventions to ensure high coverage of the COVID-19 vaccine.
Supplementary Material
Acknowledgements
We express deep gratitude to the field assistants who worked with diligence and excellence to collect these data, the participating health facilities and their management for allowing us to collect the data, Partners in Hope program leadership and the Science Department for supporting this study, and all respondents for so generously sharing their thoughts and experiences with us. We also thank Daniel Freeman and the OCEANS team for sharing their survey tool with us; and the Demand and Behavioural Sciences group at the Essential Programme on Immunization for sharing information about the BeSD COVID-19 tools with our team.
Contributor Information
Corrina Moucheraud, Departm ent of Health Policy and Management, Fielding School of Public Health, UCLA, 650 Charles E. Young Dr. South, Los Angeles, CA, 90095, USA.
Khumbo Phiri, Partners in Hope, PO Box 302, Area 36/Plot 8, M1 Road South, Lilongwe, Malawi.
Hannah S Whitehead, Division of Infectious Diseases, Department of Medicine, David Geffen School of Medicine at UCLA, 10833 Le Conte Ave, Los Angeles, CA, 90095, USA.
John Songo, Partners in Hope, PO Box 302, Area 36/Plot 8, M1 Road South, Lilongwe, Malawi.
Eric Lungu, Partners in Hope, PO Box 302, Area 36/Plot 8, M1 Road South, Lilongwe, Malawi.
Elijah Chikuse, Partners in Hope, PO Box 302, Area 36/Plot 8, M1 Road South, Lilongwe, Malawi.
Sam Phiri, Partners in Hope, PO Box 302, Area 36/Plot 8, M1 Road South, Lilongwe, Malawi.
Joep J van Oosterhout, Partners in Hope, PO Box 302, Area 36/Plot 8, M1 Road South, Lilongwe, Malawi; Division of Infectious Diseases, Department of Medicine, David Geffen School of Medicine at UCLA, 10833 Le Conte Ave, Los Angeles, CA, 90095, USA.
Risa M Hoffman, Division of Infectious Diseases, Department of Medicine, David Geffen School of Medicine at UCLA, 10833 Le Conte Ave, Los Angeles, CA, 90095, USA.
Authors’ contributions
CM, KP, SP and RMH conceived the study; KP, JS, EL and EC led data collection; CM, HSW and JS analyzed the data; CM led the drafting of the manuscript; all authors contributed to the interpretation of results, provided critical revisions to the manuscript, read and approved the final manuscript.
Funding
This study was supported by the United States Agency for International Development [Cooperative Agreement AID-OAA-A-15-00070]. The views in this publication do not necessarily reflect the views of the U. S. Agency for International Development (USAID), the U. S. President's Emergency Plan for AIDS Relief (PEPFAR) or the United States Government.
Competing interests
None declared.
Ethical approval
This study did not involve human patients. Oral consent was obtained from all survey respondents. The study was reviewed and approved by the National Health Sciences Research Committee in Malawi (#2338) and the University of California Los Angeles Institutional Review Board (#21-001278).
Data availability
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. Anonymized survey data are available upon request.
References
- 1. Center for Systems Science and Engineering at Johns Hopkins University . COVID-19 Dashboard. 2020Available at https://coronavirus.jhu.edu/map.html (accessed February 25, 2022). [Google Scholar]
- 2. Salyer SJ, Maeda J, Sembuche S, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. 2021;397(10281):1265–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schlüter JC, Sörensen L, Bossert A, et al. Anticipating the impact of COVID19 and comorbidities on the South African healthcare system by agent-based simulations. Sci Rep. 2021;11(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siedner MJ, Alba C, Fitzmaurice KP, et al. Cost-effectiveness of COVID-19 vaccination in low-and middle-income countries. medRxiv. 2021.04.28.21256237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Forman R, Shah S, Jeurissen P, et al. COVID-19 vaccine challenges: What have we learned so far and what remains to be done? Health Policy. 2021;125(5):553–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yamey G, Schäferhoff M, Hatchett R, et al. Ensuring global access to COVID-19 vaccines. Lancet. 2020;395(10234):1405–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang Q, Yang L, Jin H, et al. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prevent Med. 2021;150:106694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nachega JB, Sam-Agudu NA, Masekela R, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Global Health. 2021;9(6):e746–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dinga JN, Sinda LK, Titanji VP.. Assessment of vaccine hesitancy to a COVID-19 vaccine in Cameroonian adults and its global implication. Vaccines. 2021;9(2):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ditekemena JD, Nkamba DM, Mavoko AM, et al. COVID-19 vaccine acceptance in the Democratic Republic of Congo: a cross-sectional survey. Vaccines. 2021;9(2):153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bono SA, Faria de Moura, Villela E, Siau CS, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low-and middle-income countries. Vaccines. 2021;9(5):515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nzaji MK, Ngombe LK, Mwamba GN, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res. 2020;11:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Solís Arce JS, Warren SS, Meriggi NF, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries, and implications for messaging. Nat Med. 2021;27(8):1385–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brewer NT, Chapman GB, Rothman AJ, et al. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149–207. [DOI] [PubMed] [Google Scholar]
- 15. Roberts JR, Thompson D, Rogacki B, et al. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine. 2015;33(14):1748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Malawi Ministry of Health . Available at https://covid19.health.gov.mw/ (accessed August 4, 2021). [Google Scholar]
- 17. Nkuba AN, Makiala SM, Guichet E, et al. High prevalence of anti-SARS-CoV-2 antibodies after the first wave of COVID-19 in Kinshasa, Democratic Republic of the Congo: results of a cross-sectional household-based survey. Clin Infect Dis. 2021;ciab515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mulenga LB, Hines JZ, Fwoloshi S, et al. Prevalence of SARS-CoV-2 in six districts in Zambia in July, 2020: a cross-sectional cluster sample survey. Lancet Global Health. 2021;9(6):e773–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li Y, Liu G, Egolet RO, et al. Knowledge, attitudes, and practices related to COVID-19 among Malawi adults: a community-based survey. Int J Environ Res Public Health. 2021;18(8):4090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Banda J, Dube A, Brumfield S, et al. Knowledge, risk perceptions, and behaviors related to the COVID-19 pandemic in Malawi. Demogr Res. 2021;44:459–80. [Google Scholar]
- 21. GAVI. COVAX vaccine roll-out Malawi. Available at https://www.gavi.org/covax-vaccine-roll-out/malawi (accessed August 4, 2021). [Google Scholar]
- 22. Gómez-Ochoa SA, Franco OH, Rojas LZ, et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190(1):161–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Board on Health Sciences Policy; Committee on Equitable Allocation of Vaccine for the Novel Coronavirus . Framework for Equitable Allocation of COVID-19 Vaccine. Kahn B, Brown L, Foege W, Gayle H, editors. Washington (DC): National Academies Press (US); 2020. [PubMed] [Google Scholar]
- 24. Morales KF, Menning L, Lambach P.. The faces of influenza vaccine recommendation: A literature review of the determinants and barriers to health providers’ recommendation of influenza vaccine in pregnancy. Vaccine. 2020;38(31):4805–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Oh NL, Biddell CB, Rhodes BE, et al. Provider communication and HPV vaccine uptake: A meta-analysis and systematic review. Prevent Med. 2021;148:106554. [DOI] [PubMed] [Google Scholar]
- 26. Mergler MJ, Omer SB, Pan WK, et al. Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine. 2013;31(41):4591–5. [DOI] [PubMed] [Google Scholar]
- 27. World Health Organization . Data for action: Achieving high uptake of COVID-19 vaccines, Geneva: World Health Organization, 2021. [Google Scholar]
- 28. Freeman D, Loe BS, Chadwick A, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020. 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shapiro GK, Tatar O, Dube E, et al. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine. 2018;36(5):660–7. [DOI] [PubMed] [Google Scholar]
- 30. Azamgarhi T, Hodgkinson M, Shah A, et al. BNT162b2 vaccine uptake and effectiveness in UK healthcare workers–a single centre cohort study. Nat Commun. 2021;12(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Harrison J, Berry S, Mor V, et al. “Somebody Like Me”: understanding COVID-19 vaccine hesitancy among staff in skilled nursing facilities. J Am Med Dir Assoc. 2021;22(6):1133–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Madhi SA, Baillie V, Cutland CL, et al. Efficacy of the ChAdOx1 nCoV-19 Covid-19 vaccine against the B. 1.351 variant. New Engl J Med. 2021;384(20):1885–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. Anonymized survey data are available upon request.