Abstract
Introduction
To control the spread of COVID-19, mitigation strategies have been implemented globally, which may have unintended harmful effects on child and adolescent mental health. This study aims to synthesise the indirect mental health impacts on children and adolescents globally due to COVID-19 mitigation strategies.
Methods
We included relevant reviews from MEDLINE, Embase, PsycINFO, LILACS, CINAHL, The Cochrane Library and Web of Science until January 2022 that examined the impact of COVID-19-related lockdown and stay-at-home measures on the mental health of children and adolescents. Data extraction and quality assessments were completed independently and in duplicate by BC and LH. A Measurement Tool to Assess Systematic Reviews-2 was used to assess the methodological quality.
Results
Eighteen systematic reviews, comprising 366 primary studies, found a pooled prevalence of 32% for depression (95% CI: 27 to 38, n=161 673) and 32% for anxiety (95% CI: 27 to 37, n=143 928) in children and adolescents globally following COVID-19 mitigation measures. Subgroup analyses also uncovered important differences for both depression and anxiety by World Health Organization regions with few studies from Africa and relative high burden of anxiety and depression in the Eastern Mediterranean region.
Conclusions
Our findings reveal a high prevalence of depression and anxiety in children and adolescents during the COVID-19 pandemic, globally, compared with prepandemic estimates. These findings highlight the urgency for governments and policymakers to strengthen mental health systems in the COVID-19 recovery, especially in low-and middle-income countries where compounding psychological stress, access and affordability of care and discrepant reporting of mental health in this population remains a challenge. We also provide insight into how to alter mitigation strategies to reduce the unintended negative consequences for the health and well-being of children and adolescents in future pandemics.
PROSPERO registration number
CRD42022309348.
Keywords: COVID-19, mental health & psychiatry, child health
WHAT IS ALREADY KNOWN ON THIS TOPIC
Home confinement of children and adolescents is associated with fear, uncertainty and anxiety from disruptions to education, physical activities and opportunities for socialisation, and increased exposure to risky lifestyle behaviours. In March 2020, approximately 91% of the world’s student population were impacted by school closures due to the COVID-19 pandemic.
WHAT THIS STUDY ADDS
Meta-analyses revealed the overall pooled prevalence of depression and anxiety was 32% in children and adolescents without pre-existing mental health conditions, following the implementation of COVID-19 pandemic mitigation strategies.
Subgroup analyses revealed regional differences in anxiety and depression.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Governments and policymakers urgently need to strengthen their health systems to support children and adolescents in the development of internal and external resources for more adaptive ways of coping with stress.
Closures of schools during crises should be a last resort.
Introduction
Children and adolescents, aged 0–19 years, comprise over 1.9 billion of the world’s population, with the vast majority living in low-and middle-income countries (LMICs).1 This life stage is characterised by rapid biological, emotional and social development, often including risk-taking, emotional-influence and independence-seeking behaviours.2 3 To make a healthy transition to adulthood, children and adolescents must have access to health education, quality health services, including sexual and reproductive, and supportive environments—at home, in communities and countries.4 However, despite being inextricably linked, physical and mental health and well-being have not been promoted and protected in current discourse and investment agendas, leaving many children and adolescents behind.4 5 The number of disability-adjusted life-years (DALYs) in children and adolescents (0–19 years) diagnosed with mental disorders was 21.5 million (95% CI: 15.2 to 29.6 million) in 2019. From 1990 to 2019, the age-standardised rates of DALYs of mental disorders increased from 803.8 per 100 000 (95% CI: 567.7 to 1104.3 per 100 000) to 833.2 per 100 000 (95% CI: 589.0 to 1146.1 per 100 000) of children and adolescents.6
Across the world, countries have made significant efforts to control the spread of SARS-CoV-2 through a variety of interventions including social distancing, mobility restrictions and school closures. Evidence from previous pandemics such as Ebola have demonstrated that these interventions may have unintended and harmful effects on the health of children and adolescents.7 The nature and extent of impact on this age group depends on many vulnerability factors, including but not limited to developmental age, educational status, requiring special needs, pre-existing mental health conditions, family violence and child marriage, being economically underprivileged, bereavement and being quarantined due to infection or fear of infection.8–10 During the first wave of the pandemic in March 2020, approximately 91% of the world’s student population were impacted by school closures11 and in many countries, these closures continued well into the third and fourth quarters of 2021. The home confinement of children and adolescents is associated with uncertainty and anxiety, attributable to disruption in their education, physical activities and opportunities for socialisation.12 Furthermore, due to prolonged confinement at home, the increased use of the internet and social media exposes young people to risky lifestyle behaviours (i.e., through marketing and advertising of unhealthy food, beverage and alcohol consumption) through marketing and advertising, issues of ‘digital dependency’ or screen addiction, as well as risks of exposure to cyberbullying, age-inappropriate and violent content or sexual exploitation.13–16
To date, there have been several reviews that have synthesised the mental health impacts of COVID-19. However, these reviews included age groups beyond 0–19 years, as well as children and adolescents with pre-existing barriers and conditions. Moreover, very few reviews have generated quantitative estimates for mental health outcomes in this age group, disaggregated by gender, country income level and World Health Organization (WHO) region. As such, this overview of reviews synthesises the indirect mental health impacts of strategies which were implemented to mitigate the spread of COVID-19 in children and adolescents globally, thereby providing insight into how these strategies can be altered to reduce unintended negative impacts on the health and well-being of children and adolescents in future pandemics.
Methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (online supplemental appendix A). We undertook an overview of reviews, given this constitutes the highest level of evidence and there were a number of existing systematic reviews. Our protocol was prospectively registered with PROSPERO (CRD42022309348). To provide recommendations and a call-to-action for governments and policymakers, we collaborated with the International Pediatric Association. See box 1 for further details.
Box 1. Recommendations and call-to-action.
Mitigation strategies enacted to protect against the spread of the virus can potentially prevent associated morbidity and mortality of COVID-19, however it is essential that governments and policymakers consider the associated risks, in addition to the potential benefits, of these control measures to minimise the collateral impacts felt by this vulnerable group, in particular to their health and well-being.
There is urgent need to integrate mental health into COVID-19 recovery plans. A number of effective mental health interventions exist for adolescents, such as universally delivered psychosocial interventions.48 49 WHO and UNICEF have highlighted strategies to promote and protect adolescent mental health through guidelines48 and a toolkit.49 However, methods for delivery and access of these services need to be improved for scalability (i.e., telehealth), while focusing on prioritising equitable access for particularly vulnerable groups.
Governments, funding agencies and the broader research community should invest in improving mental health measurement tools and routine data collection for children and adolescents across varying contexts. For example, screening for mental health difficulties at a common contact point for children and adolescents (i.e., within schools).4 48–50
Awareness of the importance of mental health during future public health crises should be a focus for policymakers. Public health messaging should include the mental health impacts of COVID-19 and how to manage one’s mental health, as well as pathways to assessment and services if needed.8
Schools are an effective delivery platform for universal health promotion interventions which often include mental health strategies, as they reach the largest number of children and adolescents possible in both high-income countries and low-and middle-income countries (LMICs).48–50 WHO emphasises the ‘health-promoting school model’ as a global strategy to mitigate the long-term mental health consequences of the pandemic during postquarantine periods. As such, schools should be closed as a last resort.51 In the event that school closures are deemed necessary, it is imperative that educators and public health officials work together to determine the content and manner of effective online learning, while focusing on a safe return to school at the earliest possible date.28
Information on the pandemic should be controlled by caregivers, with limited but adequate exposure to the news. This should include accurate information, that is discussed with children in age-appropriate language or a way they can easily digest the information.
Children and adolescents should keep to a regular schedule. Caregivers should work with their child to establish a consistent routine around schoolwork, sleep, screen time, physical activity and healthy eating. In addition to regular daily activities, creating fixed dates to connect with friends or teachers can ease stress during social distancing. Establishing a routine to connect with others will help children and adolescents regulate their emotions and find normalcy in day-to-day life.
Additional support to vulnerable groups must be provided. For example, children and adolescents living in LMICs, and families with greater vulnerability that are unable to cope with new stressors. Parent support interventions should be universally available at both policy and service levels.4 WHO and UNICEF suggest making resources available for educational purposes and stress the importance of positive parenting, including kind and soft communication with children and adolescents during times of stress.52–54
To help facilitate a child’s or adolescent’s ability to overcome shocks and transitions, emphasis should be placed on developing protective factors, both internal and external resources for more adaptive ways of coping. For example, strengthening internal resources for coping through quality education, strong caregiver support or availability of external community resources.48 49
bmjgh-2022-010713supp001.pdf (1.2MB, pdf)
Search strategy and selection criteria
Searches were conducted in the following databases: MEDLINE, Embase, PsycINFO, LILACS, CINAHL, The Cochrane Library and Web of Science (online supplemental appendix B). There were no limitations on geographical settings or publication language. The original search was performed on 15 July 2021, with an updated search on 12 January 2022. Preprints and grey literature searches were also conducted (online supplemental appendix C).
Screening and selection process
Two reviewers screened and selected full-text articles for review. Data were extracted independently using a standardised form to characterise and meta-analyse the outcome data. Specific eligibility criteria were used to screen and select studies (online supplemental appendix D). Eligible study designs were systematic reviews that evaluated the research question. Studies were eligible if published after December 2019, where the primary exposure was SARS-CoV-2. Classification of high-income countries (HICs) and LMICs was conducted according to the World Bank’s 2019 fiscal year country income classification. We included studies where children and adolescents mean age was between 0 and 19 years. Studies were excluded if they observed the indirect mental health effects in age groups >19 years exclusively, indirect mental health effects in previous pandemics or exclusively included populations with compounding mental health effects (i.e., previous mental health conditions, chronic conditions, COVID-19-positive patients). We excluded populations with existing mental health effects because this group already faces many barriers that would bias the effects attributable to the pandemic. This defined a new need to understand the mental health impacts of the pandemic for those without existing barriers.
Data synthesis and statistical analysis
Overview of reviews meta-analyses
Pooled estimates (prevalence and the standardised mean difference) for all eligible mental health outcomes were extracted from each systematic review which included child and adolescent groups both with and without previously reported mental health or chronic conditions. Importantly, half of the systematic reviews (n=9) included in our overview, combined population groups of both healthy and children already involved in a disease process, such as cystic fibrosis, autism spectrum disorder, attention deficit hyperactivity disorder or who had received attention previously for mental health support. The systematic review authors extracted prevalence estimates from primary studies meeting their eligibility criteria and pooled estimates using random-effects meta-analyses, to account for variations in the methodology and measurement scales used between studies.
Determining overlap
To determine the overlap in primary studies included between the systematic reviews, we created a citation matrix and calculated the corrected covered area (CCA) using methods by Pieper et al 17.
Re-analysis of systematic reviews
Given that previous mental health or chronic conditions could confound the mental health effects being observed during the COVID-19 pandemic and the need to understand the mental health impacts of the pandemic for those without existing barriers, we screened primary studies captured in each systematic review, extracted prevalence estimates from eligible studies and re-analysed primary data in meta-analyses. Statistical analyses were conducted in STATA V.17 (StataCorp, College Station, Texas, USA). Where multiple measures were reported for an outcome in a single study, we used the most commonly reported measure across all included studies. For example, sleep disturbance was most often characterised by ‘any type of disturbance including insomnia’, compared with ‘insomnia alone’. To mitigate heterogeneity within included studies, a random-effects meta-analysis was used for all pooled outcomes of primary data and statistical heterogeneity was assessed by calculating the I2 statistic, χ2 test and reporting Tau2. Furthermore, sources of heterogeneity were explored through subgroup analyses of gender, country income level and WHO regions. Overall effect estimates were considered statistically significant if the associated p value was <0.05.
Quality assessment
Quality assessment for included systematic reviews was conducted according to A Measurement Tool to Assess Systematic Reviews-2 (AMSTAR 2) quality assessments. Specifically, systematic reviews were assessed using the AMSTAR 2 across the following domains: a priori review methods, comprehensive search strategy, study selection and data extraction in duplicate, reasoning for exclusion, provision of details for included studies, risk of bias assessment, appropriate statistical methods, disclosure of funding and conflicts of interest. Studies were assigned an overall quality judgement based on the overall confidence in the results of the review (ie, high, moderate, low, critically low) (online supplemental appendix E).
LH and BC independently assessed quality for each review using the criteria outlined above. These scores were compared and a final score decision was made. Any disagreements in the subjective quality ratings were resolved by consensus or a third reviewer. Additionally, we reviewed the focus, reported outcomes and characteristics of each study included within each review, retrieved the full text when relevant and extracted any summary outcome data related to indirect mental health outcomes in children and adolescents globally.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research; we used publicly available data for the analysis.
Results
Study selection
Our search generated 1672 records. After removal of duplicates, we screened 1347 records, of which 189 records were included for full-text review. Of these, 18 systematic reviews met the eligibility criteria and were included in our analyses. See figure 1 for study flow diagram.
Figure 1.
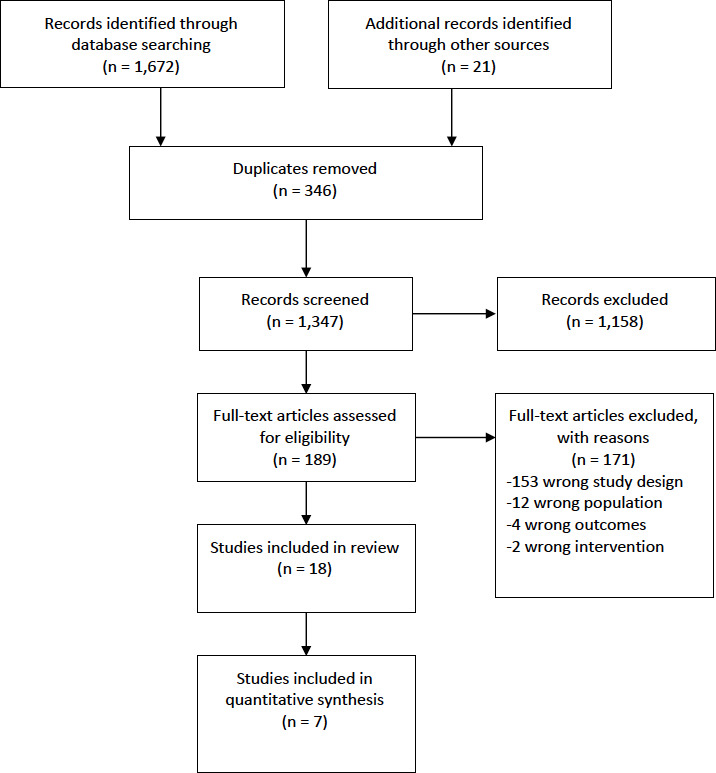
Preferred Reporting Items for Systematic Reviews and Meta-Analyses review flow diagram.
Study characteristics of included systematic reviews
We included 18 systematic reviews that synthesised data on the indirect impacts of COVID-19 on the mental health of children and adolescents from 366 unique primary studies. The primary studies of the included reviews took place in a mixture of HICs (n=21) and LMICs (n=16) across all six WHO regions (Africa, the Americas, Europe, South-East Asia, Eastern Mediterranean and Western Pacific). However, the majority of primary studies took place in China, where out of the seven reviews that reported quantitative analyses, 48.8% of included studies took place in China. Children ranged from 0 years to 24 years. The study designs of the included primary studies were broad and observational (i.e., mainly cross-sectional or cohort studies) and looked at indirect impacts of the COVID-19 pandemic, such as school closures, social distancing, quarantine, isolation or home confinement. Most systematic reviews assessed any mental health disorder or any psychological impact, followed by depression, anxiety, sleep disorders or post-traumatic stress symptoms. The majority of outcome measures were assessed using online questionnaire-based surveys. The systematic review search dates ranged from early 2020 to June 2021 (table 1).
Table 1.
Characteristics of included studies and author’s conclusions
| Study | Study designs included | HIC/LMIC | Countries | Number of studies | Age range | Mental health outcomes | Author’s conclusions | Impact on mental health |
| Octavius et al18 | Prospective cohort; cross-sectional | Both | USA, Turkey and China | 4 | 12–18 years | Adolescent’s mental health, such as depression, fear and anger | COVID-19 has been found to be associated with mental health changes in adolescents which meant management of COVID-19 should also focus on mental health as well. |
Negative |
| Racine et al19 | Empirical studies (case studies and qualitative analyses excluded) | Both | Jordan, Ecuador, China, USA, Italy, Brazil, Greece, Canada, Spain, Portugal and Germany | 29 | Mean age: 13 years (range: 4.1–17.6 years) | Prevalence of clinically elevated depressive or anxiety symptoms in youth during COVID-19 | Pooled estimates obtained in the first year of the COVID-19 pandemic suggest that one in four youth globally are experiencing clinically elevated depression symptoms, while one in five youth are experiencing clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double of prepandemic estimates. An influx of mental healthcare utilisation is expected, and allocation of resources to address child and adolescent mental health concerns are essential. | Negative |
| Sajid et al20 | Case-control, cross-sectional, cohort studies and case series (case reported >4), letters, perspectives and correspondences | Not reported | Not reported | 13 | 2–18 years | Mental health outcomes such as stress, anxiety, anger and depression | An analysis of available literature illustrates a clear correlation between increasing anxiety among children during the SARS-CoV-2 pandemic. Our systematic review encompasses school-going and early collegiate students who have shown to suffer from a deteriorating mental status due to the fear of being infected, a feeling of boredom and lack of productivity, which adds on to the stress level hindering their focused approach to learning. | Negative |
| Ma et al21 | Cross-sectional and longitudinal studies | Upper-middle income | Turkey and China | 23 | 0–18 years | Prevalence of depression, anxiety, sleep disorders and post-traumatic stress symptoms | Early evidence highlights the high prevalence of mental health problems among children and adolescents during the COVID-19 pandemic, especially among female and adolescents. Studies investigating the mental health of children and adolescents from countries other than China are urgently needed. |
Negative |
| Chawla et al22 | Cross-sectional and cohort studies | Both | The Netherlands, Turkey, Italy, USA, China, Bangladesh, France, Germany, Brazil, Hong Kong, Canada, Iran, Spain, Portugal, India, Indonesia, Australia, Chile, Croatia, Singapore, Switzerland, Israel, UK, Uruguay, Uganda and Norway | 102 | 0–24 years (6–18 years in majority of studies) | Any psychological impact | Psychological impact on children and adolescents is significant, either due to the fear of the illness or social isolation related to COVID-19. One may focus on improving sleep habits and physical activity and regulating internet use for maintaining psychological well-being. | Negative |
| Cachón-Zagalaz et al23 | Not reported | Both | USA, UK, Turkey, China, Italy, Spain | 9 | 0–12 years | Psychological and motor outcomes | There are very few studies on how confinement has affected children under 12 years psychologically and motorly. These articles agree on the consequences that confinement can have on minors and on the importance of psychological support from the family, and the establishment of routines can be effective. | Negative |
| Chaabane et al24 | All types of studies included: modelling study; quasi-experimental time series analysis; report; prepublication release; expert viewpoint; snapshot of strategies/challenges analysis; cross-sectional; descriptive study (n=2) and survey | Both | USA, Japan, France, Italy, Thailand and Turkey | 10 | Not reported | Mental or physical health-related issues | The impact of school closures during the COVID-19 pandemic includes loss of access to school-based and critical services and resources particularly for children with disabilities and those living in poorer families. COVID-19 school closures were also associated with increased stress among children and emotional reactions (eg, sadness, frustration, indiscipline) in addition to the breakdown in daily routines. | Negative |
| Sharma et al25 | Longitudinal and cross-sectional studies | Both | China, Italy, Israel, Canada, Spain, Brazil, Portugal and USA | 16 | 6 months to 18 years | Sleep disturbances: sleep quality, sleep duration and insomnia severity | The prevalence of sleep problems in children and adolescents during the COVID-19 pandemic is alarming. Preschool children had a trend towards relatively fewer sleep disturbances due to home confinement measures in comparison with prepandemic times. Sleep duration recommendations were not met in nearly half of healthy children. | Negative |
| Stavridou et al26 | Cross-sectional studies, qualitative analyses, longitudinal cohort and case-report studies | Both | China, Italy, USA, Singapore, UK and Kosovo | 21 | 3–18 years | Any mental health condition | A deterioration in mental health is highlighted, encompassing anxiety and mood symptoms and developmental, stressor-related and eating disorders among children, adolescents and young adults during the COVID-19 pandemic. | Negative |
| Nearchou et al27 | Cross-sectional studies | Both | China, Italy, Poland, Turkey and USA | 12 | 3–18 years | Any mental health disorder or outcome | The findings show that COVID-19 has an impact on youth mental health and is particularly associated with depression and anxiety in adolescent cohorts |
Negative |
| Panda et al28 | Prospective cohort and cross-sectional studies | Both | France, Italy, China, Spain, India, Hong Kong, Brazil, Turkey, Bangladesh and Korea | 15 | 18 years or younger | Various psychological and behavioural symptoms/disorders | Anxiety, depression, irritability, boredom, inattention and fear of COVID-19 are predominant new-onset psychological problems in children during the COVID-19 pandemic. | Negative |
| Jones et al29 | Quantitative studies | Both | USA, China, UK, Japan, Germany, Canada, Philippines and Denmark | 16 | 13–17 years | Any mental health issue | Globally, adolescents of varying backgrounds experience higher rates of anxiety, depression and stress due to the pandemic. Second, adolescents also have a higher frequency of using alcohol and cannabis during the COVID-19 pandemic. However, social support, positive coping skills, home quarantining and parent–child discussions seem to positively impact adolescent mental health during this period of crisis. |
Negative |
| Samji et al30 | Prospective/Retrospective cohort, case-control, chart review, cross-sectional and qualitative studies | Both | Europe (39/116), followed in diminishing order by East Asia (28/116), North America (21/116), South Asia (7/116), Australia (7/116), West Asia (6/116), South America (2/116), South-East Asia (2/116), sub-Saharan Africa (1/116) and North Africa (1/116). Two studies involved multiple countries or were international in focus |
116 | 0–18 years (24 studies also included populations ≥18 years) | COVID-19-related mental health changes | Mental health impacts of the COVID-19 pandemic on children and adolescents are significant and should be of tremendous concern to policymakers and practitioners globally. As the pandemic continues, innovative approaches that increase access to mental health services, as well as promote resilience and mental well-being such as maintaining social connection despite isolation and renewing social ties during the recovery phase may be explored. |
Negative |
| Panchal et al31 | Cross-sectional and longitudinal cohort studies | Both | Europe, Western Pacific, South-East Asia and the Americas | 61 | 0–19 years | Any mental health outcome | The COVID-19 lockdown has resulted in psychological distress and highlighted vulnerable groups such as those with mental health difficulties, and risk factors such as lack of routine and excessive COVID-19 media exposure. However, for some families being able to spend more quality time together has been positive. Supporting the mental health needs of children and adolescents at risk is key. Clinical guidelines to alleviate the negative effects of COVID-19 lockdown and public health strategies to support this population need to be developed. |
Negative |
| Marques de Miranda et al32 | Original data from surveys, cross-sectional and longitudinal studies, editorials, research letters and original papers | Both | Most articles were from China (n=11). Also, USA (n=2), Europe (n=1) and South America (n=1) | 51 | 6–21 years | Any mental health outcome | Children from all development phases had high rates of depression, anxiety and post-traumatic symptoms as expected in the aftermath of any disaster. | Negative |
| Bussières et al33 | Longitudinal, retrospective and cross-sectional studies | Both | Italy, UK, The Netherlands, Spain, Germany, Switzerland, China, Japan, South Korea, Singapore, Israel, Turkey, Canada, USA and Argentina | 71 | 5–13 years | Internalising problems, externalising problems and sleep disturbances | Studies included in this review suggest that children’s mental health was generally negatively impacted during the COVID-19 pandemic. More research is needed to understand the long-term effects of the COVID-19 pandemic on children’s mental health and the influence of specific risks factors as they evolve over time. | Negative |
| Chai et al.34 | Not reported | LMIC | China | 12 | 18 years or younger | Mental health-related problems including depression, anxiety, stress or other associated problems | Meta-regression analysis indicated that there was an increasing number of children and adolescents with mental problems during the home confinement. It suggested that we should pay more attention to this vulnerable population during a public health crisis in the future, especially for the girl groups, and more detailed implements for mental health management were needed and should be prepared. | Negative |
| Viner et al35 | Cohort, uncontrolled prepost, cross-sectional and modelling studies | Both | USA, Turkey, UK, China, Italy, Canada, Brazil, Japan, Spain, Ireland, India and Bangladesh | 36 | 0–19 years | Mental health outcomes (eg, anxiety, depression, psychological distress, sense of loneliness/isolation, suicide, psychiatric admission) | In this narrative synthesis of reports from the first wave of the COVID-19 pandemic, studies of short-term school closures as part of social lockdown measures reported adverse mental health symptoms and health behaviours among children and adolescents. | Negative |
HIC, high-income country; LMIC, low- and middle-income country.
In our sample, the CCA calculation revealed a 4.0% overlap, which is considered a slight overlap (online supplemental appendix F).
Methodological quality of included systematic reviews
AMSTAR 2 assessments were performed for the 18 included systematic reviews. Eleven reviews (61.1%) were rated as having critically low quality and seven reviews (38.9%) were rated as having low quality (see online supplemental appendix E for further detail).
Summary of main results
We included 18 systematic reviews that reported on a range of mental health outcomes.18–35 Seven reviews reported a quantitative synthesis through meta-analysis19–21 25 28 33 34 and 11 reviews reported qualitative narrative syntheses.18 22–24 26 27 29–32 35 Overall, all 18 systematic reviews reported a negative impact on children’s or adolescent’s mental health due to the impacts of COVID-19. See table 1 for further details.
For the seven systematic reviews that reported a quantitative synthesis, the mental health outcomes included were depression, anxiety, internalising symptoms, externalising symptoms, sleep outcomes, post-traumatic stress symptoms and overall psychological symptoms or mental health. Importantly, there was a diverse range of mental health-related scales and instruments used to assess outcomes, which needs to be considered when interpreting results. See tables 2–5 for a complete list of scales/instruments used. To assess the prevalence of depression and anxiety for children and adolescents without pre-existing conditions, we re-analysed primary data in meta-analyses. See table 6 for total and subgroup meta-analyses for the pooled prevalence (PP) of depression and anxiety in children and adolescents during the COVID-19 pandemic.
Table 2.
Study characteristics and pooled prevalence for depression
| Study | Diagnostic/Screening instrument used | Pooled effect estimates (95% CI) |
Heterogeneity (I2) | Total # of people | Total # of studies | AMSTAR 2 rating | Impact on MH |
| Racine et al19 | PHQ-9; MHI-5; DSRS-C; CBCL; DASS-21; CDI; CDI-SF; Preschool Feelings Checklist; HADS; Well-Being Index; SMFQ; SMFQ-P; CES-DC; MFQ and CESD | Pooled prevalence=25.2% (21 to 30) |
99.47% | 79 305 | 26 | Low | Negative |
| Ma et al21 | DSRS-C (n=2); PHQ-9 (n=3); CDI-SF; CES-D; CDI (n=2); PQSPHE; SDS; MMHI-60 | Pooled prevalence=28.6% (17.2 to 40.1) |
99.99% | 34 267 | 12 | Low | Negative |
| Panda et al28 | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=41.7% (40.8 to 42.3) |
36% | 21 330 | 11 | Critically low | Negative |
| Chai et al34 | DASS-21; SCL-90; SCARED; DSRS; MMHI-60; PHQ-9; CDI-SFF; CDI | Pooled prevalence=22% (26 to 30) | 99% | 26 012 | 9 | Low | Negative |
CBCL, Child Behaviour Checklist; CDI, Children’s Depression Inventory; CDI-SF, Short Form of CDI; CESD, Center for Epidemiological Studies Depression; CES-DC, CESD Scale for Children; DASS-21, Depression, Anxiety and Stress Scale; DSM-5, The Diagnostic and Statistical Manual of Mental Disorders-5; DSRS, Depression Self-Rating Scale; DSRS-C, DSRS for Children; GAD-7, General Anxiety Disorder-7; HADS, Hospital Anxiety and Depression Scale; IES-R, Impact of Event Scale-Revised; MFQ, Mood and Feelings Questionnaire; MHI-5, Mental Health Inventory-5; MMHI-60, Mental Health Inventory of Middle-school Students-60; PHQ-9, Patient Health Questionnaire-9; PQSPHE, Psychological Questionnaire for Sudden Public Health Events; SAS, Self-rating Anxiety Scale; SCARED, Screen for Child Anxiety-Related Disorders; SCAS, Spence Children’s Anxiety Scale; SCL-90, Symptom Checklist-90; SDS, Self-Rating Depression Scale; SMFQ, Short Mood and Feelings Questionnaire; SMFQ-P, The parent-report version of the SMFQ; STAI, State-Trait-Anxiety Inventory.
Table 3.
Study characteristics and pooled prevalence for anxiety
| Study | Diagnostic/Screening instrument used | Pooled effect estimates (95% CI) |
Heterogeneity (I2) | Total # of people | Total # of studies | AMSTAR 2 rating | Impact on MH |
| Racine et al19 | GAD-7; SCARED; CBCL; DASS-21; CAQ; HADS; Well-Being Index; SCAS-P-8; SAS and MHBQ | Pooled prevalence=20.5% (17 to 24) |
99.27% | 70 707 | 25 | Low | Negative |
| Sajid et al20 | SASC in Zheng et al; STAI in Senkalfa et al | SMD=1.1 (−1.43 to 3.63) | 98% | 1653 | 2 | Critically low | Negative |
| Ma et al21 | SCARED (n=5); GAD-7 (n=5); SAS; PQSPHE; MMHI-60 | Pooled prevalence=25.5% (16.0 to 35.1) |
99.9% | 42 435 | 13 | Low | Unclear |
| Panda et al28 | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=34.5% (33.8 to 35.1) |
45% | 21 330 | 11 | Critically low | Negative |
| Chai et al34 | DASS-21; SCL-90; SCARED; DSRS; MMHI-60; GAD-7; PSS-10; SCSQ; PHQ-9; CDI-SFF | Pooled prevalence=25% (20 to 32) |
99% | 22 809 | 9 | Low | Negative |
CAQ, Child Anxiety Questionnaire; CBCL, Child Behaviour Checklist; CDI, Children’s Depression Inventory; CDI-SF, Short Form of CDI; DASS-21, Depression, Anxiety and Stress Scale; DSM-5, The Diagnostic and Statistical Manual of Mental Disorders-5; DSRS, Depression Self-Rating Scale; GAD-7, General Anxiety Disorder-7; HADS, Hospital Anxiety and Depression Scale; IES-R, Impact of Event Scale-Revised; MHBQ, MacArthur Health and Behaviour Questionnaire; MMHI-60, Mental Health Inventory of Middle-school Students-60; PHQ-9, Patient Health Questionnaire-9; PQSPHE, Psychological Questionnaire for Sudden Public Health Events; PSS-10, Perceived Stress Scale-10; SAS, Self-rating Anxiety Scale; SASC, Social Anxiety Scale for Children; SCARED, Screen for Child Anxiety-Related Disorders; SCAS, Spence Children’s Anxiety Scale; SCAS-P-8, SCAS-Parent Version; SCL-90, Symptom Checklist-90; SCSQ, Simplified Coping Style Questionnaire; STAI, State-Trait-Anxiety Inventory.
Table 4.
Study characteristics and pooled prevalence for sleep outcomes
| Study | Sleep outcome | Diagnostic/Screening instrument used | Pooled effect estimates (95% CI) | Heterogeneity (I2) | Total # of people | Total # of studies | AMSTAR 2 rating | Impact on MH |
| Ma et al21 | Sleep disorders | ISI and CSHQ | Pooled prevalence=44.2% (20.7 to 67.7) | 94.8% | 1695 | 2 | Low | Negative |
| Sharma et al25 | Any sleep disturbance in children | Specific study questionnaire (n=5); SDSC; PSQI; CSHQ; Canadian Health Measures Survey and the Brief Infant/Child Sleep Questionnaire |
Pooled prevalence=54% (50 to 57) | 81% | 9600 | 3 | Critically low | Negative |
| Sharma et al25 | Any sleep disturbance in preschool children | Specific study questionnaire (n=5); SDSC; PSQI; CSHQ; Canadian Health Measures Survey and the Brief Infant/Child Sleep Questionnaire |
Pooled prevalence=87% (58 to 130) | 93% | 2545 | 2 | Critically low | Positive |
| Sharma et al25 | Sleep duration (proportion of children not meeting sleep duration recommendations) | Specific study questionnaire (n=5); SDSC; PSQI; CSHQ; Canadian Health Measures Survey and the Brief Infant/Child Sleep Questionnaire |
Pooled prevalence=49% (39 to 58) | 99% | 14 121 | 4 | Critically low | Negative |
| Panda et al28 | Sleep disturbance | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=21.3% (18.7 to 24.1) | 39% | 21 330 | 11 | Critically low | Unclear |
| Bussières et al33 | Sleep duration | SDQ; KCYWI and not reported | g=0.324 (0.10 to 0.55) | 98.02% | Not reported | 9 | Critically low | Negative |
CBCL, Child Behaviour Checklist; CDI, Children’s Depression Inventory; CSHQ, Children’s Sleep Habits Questionnaire; DSM-5, The Diagnostic and Statistical Manual of Mental Disorders-5; GAD-7, General Anxiety Disorder-7; IES-R, Impact of Event Scale- Revised; ISI, Insomnia Severity Index; KCYWI, Korean Children and Youth Well-being Index; PHQ-9, Patient Health Questionnaire-9; PSQI, Pittsburgh Sleep Quality Index; SAS, Self-rating Anxiety Scale; SCARED, Screen for Child Anxiety-Related Disorders; SCAS, Spence Children’s Anxiety Scale; SDQ, Sleep Disorders Questionnaire; SDSC, Sleep Disturbance Scale for Children; STAI, State-Trait-Anxiety Inventory.
Table 5.
Study characteristics and pooled prevalence for other mental health outcomes
| Study | Outcome | Diagnostic/Screening instrument used | Pooled effect estimates (95% CI) | Heterogeneity (I2) | Total # of people | Total # of studies | AMSTAR 2 rating | Impact on MH |
| Ma et al21 | Post-traumatic stress symptoms | PCL-C and IES-R | Pooled prevalence=48.0% (−25.4 to 121.4) | 100% | 5084 | 2 | Low | Unclear |
| Panda et al28 | Irritability | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=42.3% (39.4 to 45.7) | 31% | 21 330 | 11 | Critically low | Negative |
| Panda et al28 | Boredom | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=35.2% (32.9 to 39.1) | 35% | 21 330 | 11 | Critically low | Negative |
| Panda et al28 | Excessive fear | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=22.5% (19.3 to 25.4) | 41% | 21 330 | 11 | Critically low | Negative |
| Panda et al28 | Inattention | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=30.8% (27.9 to 32.8) | 29% | 21 330 | 11 | Critically low | Negative |
| Panda et al28 | Overall psychological symptoms | Specific study questionnaire (n=7); PHQ-9; GAD-7; IES-R; DSM-5; SCAS, CDI; STAI; CBCL; SCARED; Short Version of SAS; Coping Style Scale and Internet Addiction Scale | Pooled prevalence=79.4% (71.8 to 88.3) | 52% | 21 330 | 11 | Critically low | Negative |
| Bussières et al33 | Overall mental health | PedsQL; SDQ; SCARED; DASS-21; KCYWI; Kidscreen-27; SENA; CBCL; WHO-5-J; CY-BOCS; CDI-SF | g=0.3 (0.14 to 0.45) | 98.02% | 10 039 | 16 | Critically low | Negative |
| Bussières et al33 | Internalising symptoms | PedsQL; SDQ; SCARED; RCADS; DASS-21; KCYWI; SENA; CBCL; CDI-SF | g=0.215 (0.06 to 0.37) | 98.02% | 8916 | 19 | Critically low | Negative |
| Bussières et al33 | Externalising symptoms | SDQ; SCARED; SENA; CBCL | g=0.141 (0.08 to 0.21) | 98.02% | 5729 | 15 | Critically low | Negative |
| Chai et al34 | Overall mental problems | DASS-21; SCL-90; SCARED; DSRS; MMHI-60; GAD-7; PSS-10; SCSQ; PHQ-9; CDI-SF; CDI; SSS | Pooled prevalence=28% (22 to 34) | 99% | 26 821 | 11 | Low | Negative |
CBCL, Child Behavior Checklist.CDI, Children’s Depression Inventory; CDI-SF, Short version of CDI; CY-BOCS, Children’s Yale-Brown Obsessive Compulsive Scale; DASS-21, Depression, Anxiety and Stress Scale; DSM-5, The Diagnostic and Statistical Manual of Mental Disorders-5; DSRS, Depression Self-rating Scale for Children; GAD-7, General Anxiety Disorder-7; IES-R, Impact of Event Scale-Revised; KCYWI, Korean Children and Youth Wellbeing Index; MMHI-60, Mental Health Inventory of Middle-school Students-60; PCL-C, The PTSD Checklist-Civilian Version; PedsQL, Pediatric Quality of Life Inventory; PHQ-9, Patient Health Questionnaire-9; PSS-10, Perceived Stress Scale; RCADS, Revised Children’s Anxiety and Depression Scale; SAS, Self-rating Anxiety Scale; SCARED, Screen for Child Anxiety-Related Disorders; SCAS, Spence Children’s Anxiety Scale; SCL-90, Symptom Checklist; SCSQ, Simplified Coping Style Questionnaire; SDQ, Sleep Disorders Questionnaire; SENA, System of Evaluation of Children and Adolescent; SSS, Somatic Self-rating Scale; STAI, State-Trait-Anxiety Inventory; WHO-5-J, World Health Organization-Five Well-Being Index;
Table 6.
Total and subgroup meta-analyses for the pooled prevalence of depression and anxiety in children and adolescents during the COVID-19 pandemic
| Mental health outcome | Group | Number of studies | Prevalence (95% CI) | Heterogeneity | |||
| Tau2 | I2 | H2 | P value | ||||
| Depression | Total | 50 | 32% (27 to 38) | 0.04 | 99.89 | 929.19 | 0.00 |
| Depression | Male | 13 | 32% (24 to 40) | 0.02 | 99.57 | 231.55 | 0.00 |
| Female | 13 | 37% (28 to 47) | 0.03 | 99.72 | 352.11 | 0.00 | |
| Depression | Americas | 9 | 35% (20 to 50) | 0.05 | 99.78 | 444.98 | 0.00 |
| Eastern Mediterranean | 3 | 72% (43 to 101) | 0.07 | 99.56 | 227.23 | 0.00 | |
| Europe | 6 | 35% (19 to 50) | 0.04 | 99.24 | 131.40 | 0.00 | |
| South-East Asia | 2 | 23% (19 to 27) | 0.00 | 47.61 | 1.91 | 0.17 | |
| Western Pacific | 30 | 28% (22 to 34) | 0.03 | 99.89 | 872.57 | 0.00 | |
| Depression | HIC | 15 | 37% (26 to 47) | 0.04 | 99.70 | 330.43 | 0.00 |
| LMIC | 35 | 31% (23 to 38) | 0.05 | 99.91 | 1166.09 | 0.00 | |
| Anxiety | Total | 55 | 32% (27 to 37) | 0.04 | 99.85 | 662.78 | 0.00 |
| Anxiety | Male | 16 | 28% (21 to 36) | 0.02 | 99.55 | 222.82 | 0.00 |
| Female | 16 | 35% (26 to 44) | 0.03 | 99.68 | 317.34 | 0.00 | |
| Anxiety | Americas | 8 | 32% (16 to 49) | 0.06 | 99.76 | 414.91 | 0.00 |
| Eastern Mediterranean | 4 | 58% (29 to 88) | 0.09 | 99.81 | 536.75 | 0.00 | |
| Europe | 10 | 44% (32 to 56) | 0.04 | 99.30 | 143.66 | 0.00 | |
| South-East Asia | 3 | 22% (17 to 26) | 0.00 | 57.35 | 2.34 | 0.10 | |
| Western Pacific | 30 | 26% (21 to 30) | 0.01 | 99.73 | 368.00 | 0.00 | |
| Anxiety | HIC | 19 | 40% (30 to 50) | 0.05 | 99.73 | 374.54 | 0.00 |
| LMIC | 36 | 28% (23 to 33) | 0.03 | 99.83 | 599.22 | 0.00 | |
HIC, high-income country; LMIC, low- and middle-income country.
Prevalence of depression
Four systematic reviews reported on the PP of depression among children and adolescents during the COVID-19 pandemic.19 21 28 34 Racine et al reported a PP of 25.2% (95% CI: 0.21 to 0.30, I2=99.5%)19; Ma et al reported 28.6% (95% CI: 17.2 to 40.1; I2=99.9%),21 Panda et al reported 41.7% (95% CI: 40.8 to 42.3; I2=36%)28 and Chai et al reported 22% (95% CI: 26 to 30; I2=99%).34 All four systematic reviews highlight the high prevalence of depression among children and adolescents during the COVID-19 pandemic (see table 2).
Of the 18 included systematic reviews, 50 primary studies reported the prevalence of depression during the COVID-19 pandemic. Meta-analysis revealed the overall PP of depression was 0.32 (95% CI: 0.27 to 0.38; Tau2=0.04; I2=99.9%; H2=929.2) or 32% in children and adolescents without pre-existing conditions (see figure 2).
Figure 2.
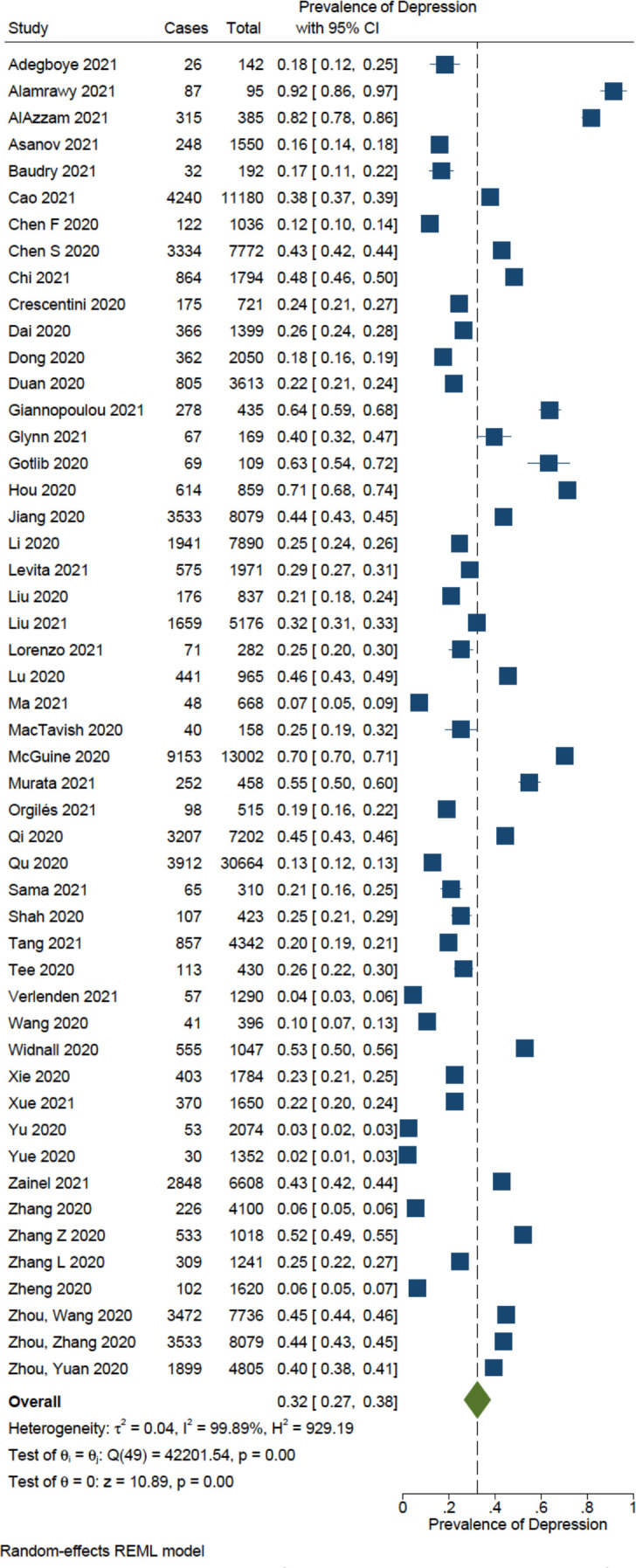
Forest plot of the pooled prevalence of depression in children and adolescents during the COVID-19 pandemic. REML, Restricted Maximum Likelihood.
Given the high heterogeneity observed, we conducted subgroup analyses for gender, WHO region and country income in children and adolescents without pre-existing conditions. The subgroup analysis by gender discovered that males have a 32% prevalence of depression (95% CI: 24 to 40; Tau2=0.02; I2=99.6%; H2=231.55) and females have a 37% prevalence of depression (95% CI: 28 to 47; Tau2=0.03; I2=99.7%; H2=352.11). The test for subgroup differences demonstrated a non-statistically significant difference in prevalence of depression between males and females (p=0.39) (online supplemental appendix G).
The subgroup analysis by WHO region found that children and adolescents living in the Americas have a 35% prevalence of depression (95% CI: 20 to 50; Tau2=0.05; I2=99.8%; H2=444.98); in Eastern Mediterranean have a 72% prevalence of depression (95% CI: 43 to 101; Tau2=0.07; I2=99.6%; H2=227.23); in Europe have a 35% prevalence of depression (95% CI: 19 to 50; Tau2=0.04; I2=99.2%; H2=131.40); in South-East Asia have a 23% prevalence of depression (95% CI: 19 to 27; Tau2=0.00; I2=47.6%; H2=1.91) and lastly in Western Pacific have a 28% prevalence of depression (95% CI: 22 to 34; Tau2=0.03; I2=99.9%; H2=872.57). The test for subgroup differences demonstrated a statistically significant difference in prevalence of depression between WHO regions (p=0.01) (online supplemental appendix H).
The subgroup analysis by country income discovered that children and adolescents living in HICs have a 37% prevalence of depression (95% CI: 26 to 47; Tau2=0.04; I2=99.7%; H2=330.43) compared with a 31% prevalence of depression for those living in LMICs (95% CI: 23 to 38; Tau2=0.05; I2=99.9%; H2=1166.09). The test for subgroup differences demonstrated a non-statistically significant difference in prevalence of depression between HICs and LMICs (p=0.33) (online supplemental appendix I).
Prevalence of anxiety
Four systematic reviews reported on the PP19 21 28 34 and one review reported the standardised mean difference (SMD) of anxiety20 among children and adolescents during the COVID-19 pandemic. Racine et al reported a PP of 20.5% (95% CI: 0.17 to 0.24; I2=99.3%)19; Ma et al reported 25.5% (95% CI: 16.0 to 35.1; I2=99.9%)21; Panda et al reported 34.5% (95% CI: 33.8 to 35.1; I2=45%)28 and Chai et al reported 25% (95% CI: 20 to 32; I2=99%).34 Sajid et al reported an SMD of 1.1 (95% CI: −1.43 to 3.63; p<0.00001; I2=98%).20 All five systematic reviews highlight the high prevalence of anxiety among children and adolescents during the COVID-19 pandemic (see table 3).
Of the 18 included systematic reviews, 55 primary studies reported the prevalence of anxiety during the COVID-19 pandemic. The meta-analysis revealed the overall PP of anxiety was 0.32 (95% CI: 0.27 to 0.37; Tau2=0.04; I2=99.9%; H2=662.78) or 32% in children and adolescents without pre-existing conditions (see figure 3).
Figure 3.
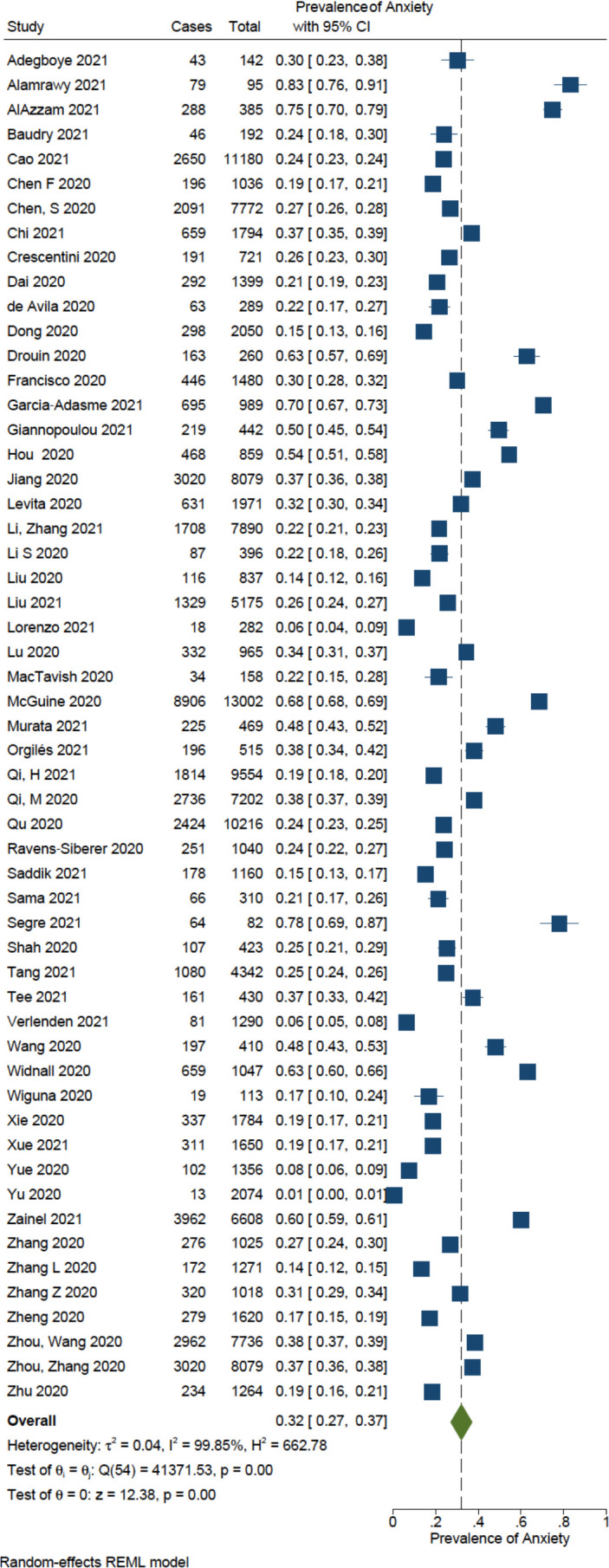
Forest plot of the pooled prevalence of anxiety in children and adolescents during the COVID-19 pandemic.
We conducted subgroup analyses for gender, WHO region and country income in children and adolescents without pre-existing conditions. The subgroup analysis by gender uncovered males have a 28% prevalence of anxiety (95% CI: 21 to 36; Tau2=0.02; I2=99.6%; H2=222.82) and females have a 35% prevalence of anxiety (95% CI: 26 to 44; Tau2=0.03; I2=99.7%; H2=317.34). The test for subgroup differences demonstrated a non-statistically significant difference in prevalence of anxiety between males and females (p=0.25) (online supplemental appendix J).
The subgroup analysis by WHO region uncovered that children and adolescents living in the Americas have a 32% prevalence of anxiety (95% CI: 16 to 49; Tau2=0.06; I2=99.7%; H2=414.91); in Eastern Mediterranean have a 58% prevalence of anxiety (95% CI: 29 to 88; Tau2=0.09; I2=99.8%; H2=536.75); in Europe have a 44% prevalence of anxiety (95% CI: 32 to 56; Tau2=0.04; I2=99.3%; H2=143.66); in South-East Asia have a 22% prevalence of anxiety (95% CI: 17 to 26; Tau2=0.00; I2=57.4%; H2=2.34) and lastly in Western Pacific have a 26% prevalence of anxiety (95% CI: 21 to 30; Tau2=0.01; I2=99.7%; H2=368.00). The test for subgroup differences demonstrated a statistically significant difference in prevalence of anxiety between WHO regions (p=0.00) (online supplemental appendix K).
The subgroup analysis by country income uncovered that children and adolescents living in HICs have a 40% prevalence of anxiety (95% CI: 30 to 50; Tau2=0.05; I2=99.7%; H2=374.54) compared with a 28% prevalence of anxiety for those living in LMICs (95% CI: 23 to 33; Tau2=0.03; I2=99.8%; H2=599.22). The test for subgroup differences demonstrated a borderline non-statistically significant difference in prevalence of anxiety between HICs and LMIC s(p=0.05) (online supplemental appendix L).
Prevalence of sleep outcomes
Three systematic reviews reported on the PP21 25 28 and one review reported an overall effect size (Hedges’s g) for sleep-related outcomes33 among children and adolescents during the COVID-19 pandemic. For example, Ma et al reported a PP of 44.2% (95% CI: 20.7 to 67.7; I2=94.8%) for any sleep disorders,21 while Sharma et al reported a PP of 54% (95% CI: 50 to 57; I2=81%) and 87% (95% CI: 58 to 130; I2=93%) for any sleep disturbance in children and preschool children, respectively.25 Sharma et al also reported a PP of 49% (95% CI: 39 to 58; I2=99%) for the proportion of children not meeting sleep duration recommendations.25 Panda et al reported a PP of 21.3% (95% CI: 18.7 to 24.1; I2=39%) for any sleep disturbance.28 Lastly, Bussières et al reported significantly longer sleeping hours during lockdown compared with before (g=0.324; 95% CI: 0.10 to 0.55; p=0.004; I2=98.0%).33 All three systematic reviews highlight the high prevalence of sleep problems (any sleep disorder, disturbance or sleep duration) in children and adolescents during the COVID-19 pandemic (see table 4).
Prevalence of all other mental health outcomes
One systematic review reported on the prevalence of post-traumatic stress symptoms among children and adolescents (PP=48%; 95% CI: 25.4 to 121.4; I2=100%).21 Another systematic review reported on the PP of overall worsening of behaviour and any psychological symptoms among children and adolescents (PP=79.4%; 95% CI: 71.8 to 88.3; I2=52%).28 Two systematic reviews reported on overall mental health,33 34 where one review reported an overall effect size (Hedge’s g) for mental health of healthy school-aged children (g=0.3; 95% CI: 0.14 to 0.45; I2=98.0%),33 and the other review reported the PP of overall mental health problems (including depression, anxiety and stress) in children and adolescents (PP=28%; 95% CI: 22 to 34; I2=99%).34 Lastly, one systematic review reported an overall effect size (Hedge’s g) for internalising symptoms (g=0.215; 95% CI: 0.06 to 0.37; I2=98.0%) and externalising symptoms (g=0.141; 95% CI: 0.08 to 0.21; I2=98.0%).33 Findings from the four systematic reviews highlight the high prevalence of other mental health problems (post-traumatic stress symptoms, worsening of behaviour, internalising and externalising symptoms, any psychological symptoms or overall mental health) in children and adolescents during the COVID-19 pandemic (see table 5).
Discussion
To address child and adolescent mental health during COVID-19, we conducted an overview of 18 systematic reviews and meta-analysis of eligible studies from 366 unique primary studies. Reviews were included from any setting, although the majority included primary studies conducted in China (48.8% of included studies from quantitative syntheses). Most reviews focused on the prevalence of depression and anxiety across a range of child (5–9.9 years) and adolescent (10–19.9 years) populations. This unfortunately made it impossible to disaggregate and analyse data by younger versus older age groups. Other mental health disorders including post-traumatic stress disorder, sleep disturbances (i.e., insomnia), substance, eating and addictive disorders were less often explored. We rated the quality of the 18 included systematic reviews using the AMSTAR 2 tool and found 61.1% of reviews to be critically low quality and 38.9% to be low quality. Our rating of the quality of included reviews as low or critically low underscores the urgent need to invest in improving mental health measurement tools and systematic data collection for children and adolescents across varying contexts.
To ensure comprehensiveness, we reviewed all primary studies within included systematic reviews and calculated the CCA to avoid duplication of data, which was found to be only a slight overlap of 4.0%. Furthermore, to limit confounding that may arise from including children and adolescents with previous mental health or chronic conditions and to address the need to understand the mental health impacts for those without pre-existing conditions, we re-analysed primary data from eligible studies with strict exclusion criteria. From our re-analysis of primary data, the overall PP of depression was 32% (95% CI: 27 to 38) (n=161 673), while the PP of anxiety was 32% (95% CI: 27 to 37) (n=143 928) in children and adolescents globally without disclosed prior mental health conditions, or positive for SARS-CoV-2. In comparison, our reported prevalence for depression and anxiety during the pandemic is higher than prepandemic estimates, where WHO estimated 3.6% of adolescents aged 10–14 years and 4.6% of those aged 15–19 years experienced an anxiety disorder prior to the pandemic, globally.36 Depression was estimated to occur among 1.1% of adolescents aged 10–14 years and 2.8% in those aged 15–19 years.36 These findings add to the extant literature on the detrimental effects of COVID-19, the spread of the virus, lockdown stay-at-home orders, school closures and decreased social interactions, but are likely an underestimation. The global underestimation of mental health conditions is recognised widely in the literature and has been hypothesised to stem from sociocultural factors (i.e., stigma), access and affordability of care and current measurement approaches (i.e., overlap between psychiatric and neurological disorders, conflation of chronic pain, exclusion of personality disorders).37 Furthermore, discrepant reporting across the world, with fewer studies from LMICs, may contribute to a lack of representative information from the countries where mental health issues are underestimated. Given the heterogeneity of included studies, instruments used and populations samples, results should be interpreted with caution. However, prevalence data still provides critical population-level information for service planning.
Furthermore, our review found subgroup differences for both depression and anxiety by WHO region in children and adolescents without prior conditions, but not by country income level or by gender. However, subgroup analyses should be interpreted with caution, given the low number of studies contributing to some subgroups (i.e., only three studies contributed to the Eastern Mediterranean region subgroup analysis compared with 30 studies for the Western Pacific). In comparison, a study by the COVID-19 Mental Disorders Collaborators reported increased prevalence of depressive and anxiety disorders due to the pandemic, where the PP of anxiety (B: –0.003, 95% uncertainty level (UL): –0.005 to –0.0002; p=0.0001) and major depressive disorder (B: −0.007, 95% UL: 0.009 to –0.0006; p=0.0001) was greater in younger age groups as compared with older age groups.8 Their findings also suggest that females were affected more by the pandemic than males (B: 0.1, 95% UL: 0.1 to 0.2; p=0.0001) for major depressive disorder and (B: 0.1, 95% UL: 0.1 to 0.2; p=0.0001) for anxiety disorders, which is hypothesised to be a result of compounding social and economic inequities that females face, which have been further exacerbated by the pandemic.8 The report by the COVID-19 Mental Disorders Collaborators also included ages into adulthood, so differences in our results may be due to increased inequities that females face later in life, compared with in childhood and adolescence. Systematic reviews by Racine et al,19 Ma et al21 and Chai et al34 all reported differences in the prevalence of anxiety and/or depression by female sex. It is likely that our findings did not reach statistical significance as our sample was limited to studies that reported disaggregated prevalence of depression and/or anxiety, resulting in a smaller sample size, and thus results may not have been powered to detect a difference.
The severity of COVID-19, as well as economic status, and healthcare systems, vary greatly by country.38 39 Despite this, we did not find a difference in the prevalence of depression and/or anxiety between country income level. For example, large discrepancies exist between different contexts and access to mental health infrastructures, where some countries may have well-developed programming available, and others have limited and underfunded systems of care. Furthermore, the socioeconomic consequences of the pandemic have led to significant job losses globally.40 This is particularly problematic in LMICs where individuals are informally employed as daily wagers and weekly incomes are used to support family feeding.20 With poverty rates expected to soar due to the pandemic,41 this will further deteriorate the mental health of children and adolescents in LMICs. Our findings highlight a significant difference between anxiety and depression prevalence by WHO region. We report a significantly higher prevalence for anxiety and depression in the Eastern Mediterranean, compared with the Americas, Europe, South-East Asia and the Western Pacific. In addition to few studies contributing to these meta-analyses, the high prevalence reported for the Eastern Mediterranean, may represent an overlap with other factors such as conflict and displacement. There are inconsistent findings across the systematic reviews for subgroup analyses by region. For example, Racine et al19 and Brussières et al33 reported higher mental health problems in European countries compared with Asian countries. In contrast, Panda et al28 reported that most studies from Asia showed a higher prevalence of psychological morbidities, compared with HICs in Europe. The inconsistency in these results may be due to differences in when each primary study was conducted. Regardless of country region, studies conducted early in the pandemic may have higher self-reported mental health symptoms due to the uncertainty and fear experienced earlier on in the pandemic.
Experiences from past pandemics and crises indicate that population shocks (i.e., unexpected or unpredictable events that disrupt the environmental, health, economic or social circumstances within a population) can heighten stress responses. For children and adolescents, these shocks could have lifelong implications. For example, evidence from the Ebola epidemic of 2014–2016 in West Africa highlighted the prevailing fear and stigma of Ebola undermined the willingness of community members to help orphaned children, which ultimately had severe psychological repercussions for children orphaned by Ebola.42 Likewise, Maclean et al suggest that experiencing a natural disaster by age 5 has been shown to significantly increase the risk of mental health, particularly anxiety disorders in adults.43 This illustrates that the worsening of mental health seen in children and adolescents during the pandemic cannot be attributed to the indirect impacts alone, but is also related to the direct effects of the pandemic, such as fear of illness, family/caregiver death, loss of income or food insecurity. In addition to the direct experience of a crisis, a negative response to shocks is also likely due to changing parenting styles. Parenting styles during crises demonstrate increases in maltreatment behaviours and poor emotional support.44 45 Of note however, protective factors, (i.e., strengthening internal resources for coping, strong caregiver support, community resources) can help facilitate an adolescent’s ability to overcome difficult shocks or transitions. This highlights the importance of identifying families with higher vulnerability that are unable to cope with new stressors, as well as ensuring parent support interventions are universally available at policy and service levels.4 Furthermore, the consequences of poor mental health in young populations experienced during a crisis can also lead to emotional reactivity and engagement in health risk behaviours such as increased sedentariness and screen time, cyberbullying, substance abuse and self-harm.4 46 This highlights the need to support children and adolescents in developing both internal and external resources for more adaptive ways of coping.
Limitations
Our review is limited by the quality of the included studies, where the included reviews were rated as very low or low quality, underscoring a critical limitation. First, there was substantial heterogeneity between included studies in measurement and reporting of outcomes. Although many of the tools were validated, some studies developed their own questionnaires to measure outcomes of mental health which could lead to bias and inconsistent results. It should also be noted that although these tools allow for the quantification of symptoms, none provide a clinical diagnosis, thus estimates may be underestimated. Second, we relied on study disclosure of prior mental health conditions in children and adolescents, however many children with these conditions are underdiagnosed, thus it is likely that children with prior mental health conditions have been included in this sample. Third, as mitigation strategies were often bundled and implemented nationally or subnationally, it is challenging to disentangle individual strategies that may have led to worse mental health effects. Furthermore, evidence from the included studies did not allow us to disentangle the direct effects of the pandemic (i.e., fear of illness) on children’s and adolescent’s mental health. Much more refined research is necessary to determine what precisely about the pandemic is contributing to crises in children’s mental health in order to inform policies and interventions. Lastly, as most studies were cross-sectional in nature, compared with few studies that were longitudinal, differences in timing of measurement (i.e., beginning of the pandemic vs multiple years into the pandemic) could lead to inconsistent results. Almost all the included studies used surveys through online self-report, which increases the chance of bias and inaccurate reporting from subjectivity of caregiver perceptions about their child’s mental health state.
Conclusion
Today’s children and adolescents face enormous challenges and compounding psychological consequences from poverty, climate change, racism, discrimination, conflict, political instability, migration and displacement.4 Our meta-analyses reveal a high prevalence of depression and anxiety in children and adolescents during the COVID-19 pandemic, globally, when compared with prepandemic estimates. Developments since have compounded the impact of the pandemic and school closures by additional shocks due to the global economic crisis, the conflict in Ukraine and Tigray, the disastrous consequences of climate change with floods in Pakistan47 and the drought-induced famine in Somalia. All of these challenges disproportionately affect children. These findings highlight the urgency for governments and policymakers to strengthen their mental health systems and integrate a mental health response into COVID-19 recovery plans and emerging challenges, while considering contextual differences such as gender. Schools remain an optimal platform for the delivery of mental health prevention and management strategies and their closure should be considered a last resort. Future research should implement longitudinal designs and use standardised tools to assess the long-term adverse mental health effects of the pandemic on children and adolescents.
Footnotes
Handling editor: Seye Abimbola
Contributors: ZAB and JDK conceptualised and designed the study. BC screened the search results, screened the retrieved papers against the inclusion criteria, appraised the quality of the papers, extracted the data and drafted the initial manuscript. LH screened the search results, screened the retrieved papers against the inclusion criteria, appraised the quality of the papers, extracted the data, completed data tabulation, synthesis and analysed primary data in meta-analyses and drafted the initial manuscript. All authors reviewed, revised and approved the final manuscript as submitted. ZAB accepts full responsibility for the finished work, the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: Funding was provided by United Nations Children’s Fund through a Small-Scale Funding Agreement to the International Pediatric Association.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.United Nations Population Division . 2019 revision of World population prospects, 2021. Available: https://population.un.org/wpp/ [Accessed 27 Apr 2022].
- 2.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. The Lancet 2012;379:1630–40. 10.1016/S0140-6736(12)60072-5 [DOI] [PubMed] [Google Scholar]
- 3.Vaivada T, Lassi ZS, Irfan O, et al. What can work and how? an overview of evidence-based interventions and delivery strategies to support health and human development from before conception to 20 years. The Lancet 2022;399:1810–29. 10.1016/S0140-6736(21)02725-2 [DOI] [PubMed] [Google Scholar]
- 4.United Nations Children’s Fund . The State of the World’s Children 2021: On My Mind—promoting, protection and caring for children’s mental health. New York: UNICEF, 2021. [Google Scholar]
- 5.Lu C, Li Z, Patel V. Global child and adolescent mental health: the orphan of development assistance for health. PLoS Med 2018;15:e1002524. 10.1371/journal.pmed.1002524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piao J, Huang Y, Han C, et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: a systematic analysis for the global burden of disease study. Eur Child Adolesc Psychiatry 2022;31:1827–45. 10.1007/s00787-022-02040-4 [DOI] [PubMed] [Google Scholar]
- 7.The Lancet Child & Adolescent Health . Children’s needs in an Ebola virus disease outbreak. Lancet Child Adolesc Health 2019;3:55. 10.1016/S2352-4642(18)30409-7 [DOI] [PubMed] [Google Scholar]
- 8.Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet 2021;398:1700–12. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das-Munshi J, Chang CK, Bakolis I, et al. All-cause and cause-specific mortality in people with mental disorders and intellectual disabilities, before and during the COVID-19 pandemic: cohort study. The Lancet Regional Health - Europe 2021;11:100228. 10.1016/j.lanepe.2021.100228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh S, Roy D, Sinha K, et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res 2020;293:113429. 10.1016/j.psychres.2020.113429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health 2020;4:421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiao WY, Wang LN, Liu J, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr 2020;221:264–6. 10.1016/j.jpeds.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lapierre MA, Fleming-Milici F, Rozendaal E, et al. The effect of advertising on children and adolescents. Pediatrics 2017;140:S152–6. 10.1542/peds.2016-1758V [DOI] [PubMed] [Google Scholar]
- 14.Sadeghirad B, Duhaney T, Motaghipisheh S, et al. Influence of unhealthy food and beverage marketing on children's dietary intake and preference: a systematic review and meta-analysis of randomized trials. Obes Rev 2016;17:945–59. 10.1111/obr.12445 [DOI] [PubMed] [Google Scholar]
- 15.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open 2019;9:e023191. 10.1136/bmjopen-2018-023191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suchert V, Hanewinkel R, Isensee B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: a systematic review. Prev Med 2015;76:48–57. 10.1016/j.ypmed.2015.03.026 [DOI] [PubMed] [Google Scholar]
- 17.Pieper D, Antoine S-L, Mathes T, et al. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol 2014;67:368–75. 10.1016/j.jclinepi.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 18.Octavius GS, Silviani FR, Lesmandjaja A, et al. Impact of COVID-19 on adolescents’ mental health: a systematic review. Middle East Current Psychiatry 2020;27:72. 10.1186/s43045-020-00075-4 [DOI] [Google Scholar]
- 19.Racine N, McArthur BA, Cooke JE, et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19. JAMA Pediatr 2021;175:1142–50. 10.1001/jamapediatrics.2021.2482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sajid MI, Tariq J, Waheed AA, et al. SARS-CoV-2 & pediatric mental health: a review of recent evidence. medRxiv 2020. [Google Scholar]
- 21.Ma L, Mazidi M, Li K, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord 2021;293:78–89. 10.1016/j.jad.2021.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chawla N, Tom A, Sen MS, et al. Psychological impact of COVID-19 on children and adolescents: a systematic review. Indian J Psychol Med 2021;43:294–9. 10.1177/02537176211021789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cachón-Zagalaz J, Sánchez-Zafra M, Sanabrias-Moreno D, et al. Systematic review of the literature about the effects of the COVID-19 pandemic on the lives of school children. Front Psychol 2020;11:569348. 10.3389/fpsyg.2020.569348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaabane S, Doraiswamy S, Chaabna K, et al. The impact of COVID-19 school closure on child and adolescent health: a rapid systematic review. Children 2021;8:415. 10.3390/children8050415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharma M, Aggarwal S, Madaan P, et al. Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med 2021;84:259–67. 10.1016/j.sleep.2021.06.002 10.1016/j.sleep.2021.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stavridou A, Stergiopoulou Angeliki‐Argyroula, Panagouli E, et al. Psychosocial consequences of COVID ‐19 in children, adolescents and young adults: a systematic review. Psychiatry Clin Neurosci 2020;74:615–6. 10.1111/pcn.13134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nearchou F, Flinn C, Niland R, et al. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health 2020;17:8479. 10.3390/ijerph17228479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panda PK, Gupta J, Chowdhury SR, et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr 2021;67:fmaa122. 10.1093/tropej/fmaa122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health 2021;18:2470. 10.3390/ijerph18052470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Samji H, Wu J, Ladak A, et al. Review: mental health impacts of the COVID-19 pandemic on children and youth: a systematic review. Child Adolesc Ment Health 2022;27:173–89. 10.1111/camh.12501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Panchal U, Salazar de Pablo G, Franco M, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry 2021;18:1–27. 10.1007/s00787-021-01856-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, et al. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct 2020;51:101845. 10.1016/j.ijdrr.2020.101845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bussières E-L, Malboeuf-Hurtubise C, Meilleur A, et al. Consequences of the COVID-19 pandemic on children’s mental health: a meta-analysis. Frontiers in Psychiatry 2021;12:691659. 10.3389/fpsyt.2021.691659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chai J, Xu H, An N, et al. The prevalence of mental problems for Chinese children and adolescents during COVID-19 in China: a systematic review and meta-analysis. Front Pediatr 2021;9:661796. 10.3389/fped.2021.661796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Viner R, Russell S, Saulle R, et al. School closures during social Lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave. JAMA Pediatr 2022;176:400–9. 10.1001/jamapediatrics.2021.5840 [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization . Adolescent mental health, 2021. Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health [Accessed 31 Oct 2022].
- 37.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016;3:171–8. 10.1016/S2215-0366(15)00505-2 [DOI] [PubMed] [Google Scholar]
- 38.Arsenault C, Gage A, Kim MK, et al. COVID-19 and resilience of healthcare systems in ten countries. Nat Med 2022;28:1314–24. 10.1038/s41591-022-01750-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pasquale S, Gregorio GL, Caterina A, et al. COVID-19 in low- and middle-income countries (LMICs): a narrative review from prevention to vaccination strategy. Vaccines 2021;9:1477. 10.3390/vaccines9121477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.International Labour Organization . Employment impact of the pandemic worse than expected, 2022. Available: https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_824098/lang-en/index.htm [Accessed 27 Apr 2022].
- 41.World Bank . Chapter 4: Impact of COVID-19 on Global Income Inequality. Global Economic Prospects, 2022. Available: https://thedocs.worldbank.org/en/doc/cb15f6d7442eadedf75bb95c4fdec1b3-0350012022/related/Global-Economic-Prospects-January-2022-Topical-Issue-2.pdf [Accessed 27 Apr 2022].
- 42.Meherali S, Punjani N, Louie-Poon S, et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health 2021;18:3432. 10.3390/ijerph18073432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maclean JC, Popovici I, French MT. Are natural disasters in early childhood associated with mental health and substance use disorders as an adult? Soc Sci Med 2016;151:78–91. 10.1016/j.socscimed.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 44.Cuartas J. Heightened risk of child maltreatment amid the COVID-19 pandemic can exacerbate mental health problems for the next generation. Psychol Trauma 2020;12:S195–6. 10.1037/tra0000597 [DOI] [PubMed] [Google Scholar]
- 45.Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: a review of current perspectives and risk factors. Child Adolesc Psychiatry Ment Health 2020;14:40. 10.1186/s13034-020-00347-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murray CJS. A collaborative approach to meeting the psychosocial needs of children during an influenza pandemic. J Spec Pediatr Nurs 2010;15:135–43. 10.1111/j.1744-6155.2009.00229.x [DOI] [PubMed] [Google Scholar]
- 47.Bhutta ZA, Bhutta SZ, Raza S, et al. Addressing the human costs and consequences of the Pakistan flood disaster. Lancet 2022;400:1287–9. 10.1016/S0140-6736(22)01874-8 [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization . Guidelines on mental health promotive and preventive interventions for adolescents: helping adolescents thrive. Geneva, 2020. Available: https://www.who.int/publications/i/item/9789240011854 [Accessed 27 Apr 2022]. [PubMed]
- 49.World Health Organization and the United Nations Children’s Fund . Helping adolescents thrive toolkit: strategies to promote and protect adolescent mental health and reduce self-harm and other risk behaviours. Geneva, 2021. Available: https://www.who.int/publications/i/item/9789240025554 [Accessed 27 Apr 2022].
- 50.Harrison L, Sharma N, Irfan O, et al. Mental health and positive development prevention interventions: overview of systematic reviews. Pediatrics 2022;149:S568–606. 10.1542/peds.2021-053852G [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization and the United Nations Educational, Scientific and Cultural Organization . Making every school a health-promoting school: global standards and indicators for health-promoting schools and systems. Geneva: World Health Organization and the United Nations Educational, Scientific and Cultural Organization, 2021. [Google Scholar]
- 52.World Health Organization . Helping children cope with stress during the 2019-nCoV outbreak, 2020. Available: https://www.who.int/docs/default-source/coronaviruse/helping-children-cope-with-stress-print.pdf [Accessed 27 Apr 2022].
- 53.Williams TP, Pontalti K. Responding to the mental health and psychosocial impact of COVID-19 on children and families. UNICEF, Child Protection Section, 2020. Available: https://www.unicef.org/media/83951/file/MHPSS-UNICEF-Learning-brief.pdf [Accessed 27 Apr 2022].
- 54.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet 2020;395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-010713supp001.pdf (1.2MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


