Abstract
Ovarian hyperstimulation syndrome is a rare condition in pregnant women. Most cases are associated with the use of ovulation induction and stimulation medications. Some studies have reported cases of this condition in non-pregnant women or women undergoing ovulation therapy. In this case report, we report the case of a 27-year-old pregnant Saudi woman presenting with a picture of severe spontaneous ovarian hyperstimulation syndrome secondary to severe undiagnosed hypothyroidism. Treatment with Eltroxin (thyroxine) led to complete improvement and regression of ovarian enlargement after empirical titrating thyroxin replacement therapy, which proved the presence of this causation. The diagnosis was confirmed by laboratory and imaging findings, which helped prompt management and prevented complications of unneeded surgical intervention.
Keywords: primary hypothyroidism, hypothyrodism, thyroxine, thyroid-stimulating hormone, spontaneous ovarian hyperstimulation syndrome
Introduction
Spontaneous ovarian hyperstimulation syndrome is an uncommon condition in pregnancies conceived naturally. Ovarian hyperstimulation syndrome rarely occurs in the absence of exogenous gonadotropins. Few reported cases have been documented in the literature [1-8]. Ovarian hyperstimulation syndrome is common in patients undergoing ovulation induction therapy with a rate of 0.2%-1%. Spontaneous occurrence is rare in patients do not who use ovulation induction therapies [9]. Symptoms associated with this condition include bilateral symmetric enlargement of ovaries with cysts of varying sizes, associated with pericardial effusion, pleural effusion, or ascites in severe cases. Van Wyk and Grumbach gave the first description of combined multicystic ovaries, precocious puberty, and juvenile hypothyroidism in 1960, and since then, several cases of this condition have been reported in adolescents or prepubertal girls [10-13]. Very few cases have been observed in adults, both gestational and non-gestational [1-8]. Studies have shown a likelihood of spontaneous ovarian hyperstimulation syndrome occurring at 3-8 weeks of gestation [14,15]. In this case report, we describe the occurrence of spontaneous ovarian hyperstimulation syndrome in a 27-year-old pregnant Saudi woman with a history of normal pregnancy without the use of induction of ovulation medication of exogenous herbal medication, which ended with spontaneous vaginal delivery of a normal baby at term gestation and without complications. Very few cases have been reported in the literature [16]. This case illustrates the role and effectiveness of levothyroxine empirically with gradual dose reduction in the treatment of a patient with spontaneous ovarian hyperstimulation with hypothyroidism.
Case presentation
The patient is a 27-year-old Saudi woman who presented to our facility referred case from a private hospital for possible surgical intervention as an ovarian tumor with abdominal distention and nausea. She is gravida 2, Para 1 (G2P1+0) at 10 weeks gestation and has no abdominal pain, vomiting, or per vaginal bleeding. Not known to have any chronic medical diseases and is not on regular medications with no previous history of any surgical intervention. The patient also had no history of medications or herbal use for induction of ovulation. She was admitted for further investigation and management. Blood investigations were within normal ranges except for high thyroid-stimulating hormone (TSH) of 123 µIU/ml (normal value is 0.35 - 4.0 µIU/ml) and low level of free thyroxine (T4), at 0.21 (normal value is 0.8 - 1.8 ng/dl), indicating hypothyroidism which was undiagnosed previously in her case. Her pregnancy was confirmed biochemically by hormonal assay and radiologically by ultrasound examination.
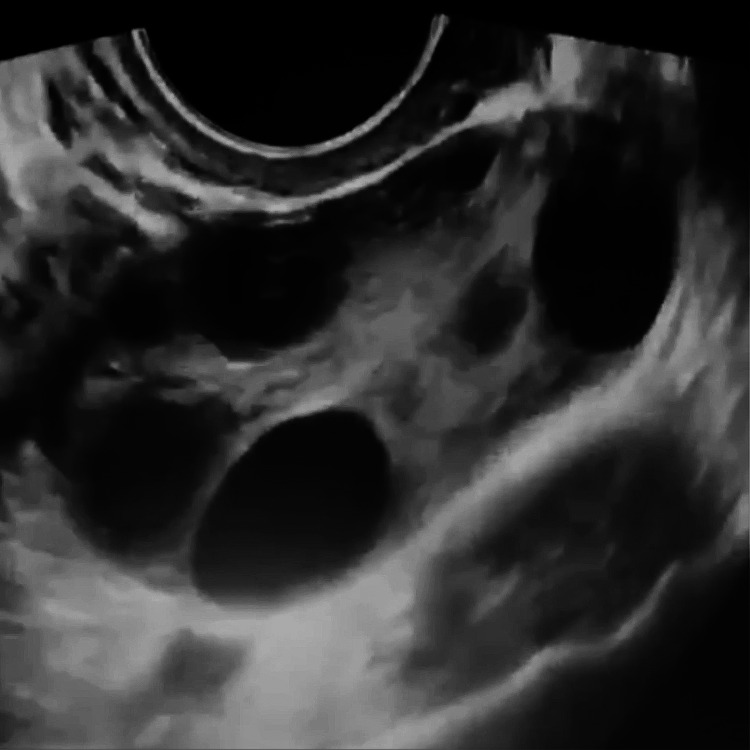
The transvaginal ultrasound showed large bilateral ovarian cysts with mild fluid collection (ascites) and thin septations (Video 1).
Video 1. Transvaginal ultrasound shows multiple ovarian cysts.
The right ovary measures 10 x 9.7 x 11.7 cm (anteroposterior plane (AP) x transverse plane (TRANS) x craniocaudal plane (CC)) and has a volume of 323.6 ccs. Measurement of the left ovary was at 7.5 x 10.5 x 10.3 cms (AP) x (TRANS) x (CC), with a volume of 395.4 ccs. Picture suggestive of ovarian hyperstimulation syndrome (Figure 1).
Figure 1. Transvaginal ultrasound shows an ovary with multiple cysts.
The patient was given the possibility of ovarian malignancies in another facility. Therefore, CA-125 was done, and the results were normal. Additional hormonal investigations due to abnormal thyroid function tests were performed. The test results (Table 1) showed high estradiol (E2) at a value of 758.93 Picogram per milliliter (Pg/ml) (normal, < 56 pg/ml). The follicle-stimulating hormone (FSH) was slightly raised at a level of 11.92 milli-international units per ml (mIU/ml) (normal 2.5-10.2 mIU/ml). The luteinizing hormone (LH) was normal, with a value of less than 3.0 International Units per liter (IU/L) (normal < 5.0).
Table 1. Blood investigations of the case.
FSH: Follicle-stimulating hormone, LH: Luteinizing hormone, E2: Estradiol, HCG: Human chorionic gonadotropin
TSH: Thyroid-stimulating hormone, T4: Free thyroxin, CA-125: Cancer antigen 125
| BLOOD INVESTIGATION | RESULT | NORMAL RANGE |
| FSH | 11.92 | 2.5 - 10.2 mIU/ml |
| LH | <3 | <5 IU/l |
| E2 | 758.93 | <56 pg/ml |
| HCG | 23150 | < 6.4 mIU/ml |
| TSH | 123 | 0.35-4.0 mIU/ml |
| T4 | 0.21 | 0.8-1.8 ng/dl |
| CA-125 | 11 | <35 IU/ml |
A spontaneous ovarian hyperstimulation syndrome diagnosis was made based on radiological and clinical findings. The patient started on levothyroxine at a daily dose of 300 micrograms (mcg) for two days. The dose was gradually reduced to 100 mcg and continued until delivery. This regimen leads to a complete reduction of ovarian enlargement and elimination of ascites, abdominal distention, and respiratory symptoms by three months duration postpartum.
Discussion
De Leener et al. reported spontaneous ovarian hyperstimulation syndrome could occur in both pregnant and non-pregnant women [17]. Ovarian hyperstimulation syndrome could be classified into three types based on FSH receptor mutation and clinical presentation. Type 1 is due to mutation of the FSH receptor and may result in recurrent hyperstimulation syndrome. Type II occurs secondary to high levels of human chorionic gonadotropin (hCG) as in multiple gestation and hydatiform mole and is common. Type III is associated with hypothyroidism which is rare [17].
Controlled ovarian stimulation is a risk factor for ovarian hyperstimulation syndrome. In rare cases, it may occur as a spontaneous event in pregnancy.
Risks for developing ovarian hyperstimulation syndrome include asthenic habitus, polycystic ovarian syndrome, luteal supplementation of hCG, multiple follicles, high levels of estradiol in the serum, and GnRH agonist protocols [18].
Some studies have reported spontaneous ovarian hyperstimulation syndrome between the 8th and 14th weeks of pregnancy as a rare occurrence. Cases have also been reported with follicle-stimulating (FSH) producing pituitary adenoma. There have also been reports of this syndrome in rare cases of increased hCG production, which is typical in multiple pregnancies, hydatidiform mole, polycystic ovary disease, and increased thyroid-stimulating hormone levels in hypothyroidism [19].
More studies are needed to know the etiology of spontaneous ovarian hyperstimulation syndrome. However, very few cases of ovarian hyperstimulation syndrome have been documented with pregnancy.
The pathophysiology of ovarian hyperstimulation syndrome in hypothyroid conditions is still unclear and needs further studies. Rotmensch and Scommegna explained the estriol formation via the 16-hydroxylation pathway rather than the 2-hydroxylation pathway typical of hypothyroid patients [20]. Due to a reduction in feedback regulation, a high release of gonadotropin caused by substituting estradiol with estriol would cause high ovarian stimulation [2].
Cardoso illustrated large bilateral ovarian cyst regression in a patient with the hypothyroid condition after thyroid hormone replacement therapy, indicating a relationship between spontaneous ovarian hyperstimulation syndrome and primary hypothyroidism [2]. A case report by Nappi et al. showed the effectiveness of thyroid replacement therapy and fluid administration in a previously untreated hypothyroid patient with spontaneous ovarian hyperstimulation syndrome [20].
The patient, in our case, had very high TSH levels with low levels of free thyroxine, which indicate hypothyroidism.
Ovarian hyperstimulation syndrome (OHSS) has varying clinical symptoms, which depend on its severity. Symptoms may be classified as mild, moderate, severe, and critical. In mild OHSS, ovarian enlargement is ‘uncomplicated,’ and with multiple cysts, ascites characterizes moderate conditions, while severe forms are associated with pericardial or pleural effusion, thrombosis, hemoconcentration, and oliguria [21]. The critical form required intensive care unit (ICU) admission with possible termination of pregnancy.
Symptoms are mostly due to fluid accumulation in the extravascular space as well as in the third space due to the high permeability of the membranes. The resulting complications may be electrolyte imbalance, hypo-albuminemia, oliguria, decreased renal perfusion, and pericardial and pleural effusions, leading to respiratory failure, liver, and renal failure, as well as hemoconcentration and thrombosis formation [22].
Imaging in MRI, CT, and US may be similar. Findings may include pleural effusion, ascites, and cysts alongside bilateral enlarged ovaries. OHSS may be complicated by ovarian torsion [23]. Our patient has moderate ovarian hyperstimulation syndrome.
The radiological finding can give the wrong impression of an ovarian tumor which might lead to unnecessary intervention for the patient, so careful assessment and a high index of suspicions of other differential diagnoses should be considered.
Mild or moderate OHSS may be treated with conservative management. Severe conditions are usually characterized by the depletion of body fluids which may be replaced with normal saline or ringer lactate. It is important that the clinician determines the underlying cause and treat it accordingly. In our case, the patient had OHSS with hypothyroidism and was treated with thyroxine.
Conclusions
This case study has illustrated the occurrence of spontaneous ovarian hyperstimulation. Patients with similar conditions should be tested for hypothyroidism, as this has the potential to cause spontaneous OHSS. Early diagnosis can help in prompt management and prevent unnecessary surgical intervention and complications.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Spontaneous ovarian hyperstimuation syndrome in a naturally conceived singleton pregnancy. Ahmed Kamel RM. Fertil Steril. 2010;94:351–354. doi: 10.1016/j.fertnstert.2009.12.076. [DOI] [PubMed] [Google Scholar]
- 2.Spontaneous ovarian hyperstimulation and primary hypothyroidism with a naturally conceived pregnancy. Cardoso CG, Graça LM, Dias T, et al. Obstet Gynecol. 1999;93:809–811. doi: 10.1016/s0029-7844(98)00435-9. [DOI] [PubMed] [Google Scholar]
- 3.Spontaneous ovarian hyperstimulation in a naturally conceived pregnancy with uncontrolled hypothyroidism. Edwards-Silva RN, Han CS, Hoang Y, Kao LC. Obstet Gynecol. 2008;111:498–501. doi: 10.1097/01.AOG.0000279139.12412.90. [DOI] [PubMed] [Google Scholar]
- 4.Regression of both pituitary and ovarian cysts after administration of thyroid hormone in a case of primary hypothyroidism. Yamashita Y, Kawamura T, Fujikawa R, Mochizuki H, Okubo M, Arita K. Intern Med. 2001;40:751–755. doi: 10.2169/internalmedicine.40.751. [DOI] [PubMed] [Google Scholar]
- 5.Spontaneous ovarian hyperstimulation syndrome caused by hypothyroidism in an adult. Taher BM, Ghariabeh RA, Jarrah NS, et al. Eur J Obstet Gynecol Reprod Biol. 2004;112:107–109. doi: 10.1016/s0301-2115(03)00283-5. [DOI] [PubMed] [Google Scholar]
- 6.A case of ovarian enlargement in severe primary hypothyroidism and review of the literature. Bassam T, Ajlouni K. Ann Saudi Med. 2006;26:66–68. doi: 10.5144/0256-4947.2006.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Primary hypothyroidism presenting as multiple ovarian cysts in an adult woman: a case report. Kubota K, Itho M, Kishi H, Igarashi S, Minegishi T. Gynecol Endocrinol. 2008;24:586–589. doi: 10.1080/09513590802288192. [DOI] [PubMed] [Google Scholar]
- 8.Ignored adult primary hypothyroidism presenting chiefly with persistent ovarian cysts: a need for increased awareness. Shu J, Xing L, Zhang L, Fang S, Huang H. Reprod Biol Endocrinol. 2011;9:119. doi: 10.1186/1477-7827-9-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Recurrent spontaneous ovarian hyperstimulation syndrome with hypothyroidism: A case report. Akbay E, Uzunçakmak C, Sevdaİdil N, et al. https://cms.galenos.com.tr/Uploads/Article_23840/BTD-6-42-En.pdf Baki Sad Tra Res Hosp. 2010;2010:1. [Google Scholar]
- 10.Multiple ovarian cysts in a young girl with severe hypothyroidism. Panico A, Lupoli GA, Fonderico F, et al. Thyroid. 2007;17:1289–1293. doi: 10.1089/thy.2007.0056. [DOI] [PubMed] [Google Scholar]
- 11.Primary hypothyroidism presenting as severe vaginal bleeding in a prepubertal girl. Gordon CM, Austin DJ, Radovick S, et al. J Pediatr Adolesc Gynecol. 1997;10:35–38. doi: 10.1016/s1083-3188(97)70042-1. [DOI] [PubMed] [Google Scholar]
- 12.Evaluating the roles of follicle-stimulating hormone receptor polymorphisms in gonadal hyperstimulation associated with severe juvenile primary hypothyroidism. Ryan GL, Feng X, d'Alva CB, et al. J Clin Endocrinol Metab. 2007;92:2312–2317. doi: 10.1210/jc.2006-2086. [DOI] [PubMed] [Google Scholar]
- 13.Van Wyk and Grumbach syndrome revisited: imaging and clinical findings in pre- and postpubertal girls. Browne LP, Boswell HB, Crotty EJ, O'Hara SM, Birkemeier KL, Guillerman RP. Pediatr Radiol. 2008;38:538–542. doi: 10.1007/s00247-008-0777-1. [DOI] [PubMed] [Google Scholar]
- 14.Ovarian hyperstimulation syndrome due to a mutation in the follicle-stimulating hormone receptor. Smits G, Olatunbosun O, Delbaere A, Pierson R, Vassart G, Costagliola S. N Engl J Med. 2003;349:760–766. doi: 10.1056/NEJMoa030064. [DOI] [PubMed] [Google Scholar]
- 15.Spontaneous ovarian hyperstimulation syndrome concomitant with spontaneous pregnancy in a woman with polycystic ovary disease. Zalel Y, Katz Z, Caspi B, et al. Am J Obstet Gynecol. 1992;167:122–124. doi: 10.1016/s0002-9378(11)91642-1. [DOI] [PubMed] [Google Scholar]
- 16.Spontaneous ovarian hyperstimulation syndrome and pituitary hyperplasia mimicking macroadenoma associated with primary hypothyroidism. Kanza RE, Gagnon S, Villeneuve H, Laverdiere D, Rousseau I, Bordeleau E, Berube M. World J Radiol. 2013;5:20–24. doi: 10.4329/wjr.v5.i1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Presence and absence of follicle-stimulating hormone receptor mutations provide some insights into spontaneous ovarian hyperstimulation syndrome physiopathology. De Leener A, Montanelli L, Van Durme J, Chae H, Smits G, Vassart G, Costagliola S. J Clin Endocrinol Metab. 2006;91:555–562. doi: 10.1210/jc.2005-1580. [DOI] [PubMed] [Google Scholar]
- 18.Ovarian hyperstimulation syndrome complicating a spontaneous singleton pregnancy: a case report. Chae HD, Park EJ, Kim SH, et al. https://www.scielo.br/j/eins/a/6zP5SVNrNTKGw887bf5VMxg/abstract/?lang=en. J Assist Reprod Genet. 2001;18:120–123. doi: 10.1023/A:1026543027300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spontaneous ovarian hyperstimulation syndrome. Kasum M, Oreskovic S, Jezek D. https://hrcak.srce.hr/104769. Coll. Antropol. 2013;37:653–656. [PubMed] [Google Scholar]
- 20.Spontaneous ovarian hyperstimulation syndrome associated with hypothyroidism. Rotmensch S, Scommegna A. Am J Obstet Gynecol. 1989;160:1220–1222. doi: 10.1016/0002-9378(89)90196-8. [DOI] [PubMed] [Google Scholar]
- 21.Natural pregnancy in hypothyroid woman complicated by spontaneous ovarian hyperstimulation syndrome. Nappi RG, Di Naro E, D’Aries AP, et al. Am J Obstet Gynecol. 1998;178:610–611. doi: 10.1016/s0002-9378(98)70448-x. [DOI] [PubMed] [Google Scholar]
- 22.Ovarian hyperstimulation syndrome: classifications and critical analysis of preventive measures. Aboulghar MA, Mansour RT. Hum Reprod Update. 2003;9:275–289. doi: 10.1093/humupd/dmg018. [DOI] [PubMed] [Google Scholar]
- 23.Clinical Practice Guidelines: OHSS guidelines and management. April. [ Jan; 2023 ]. 2012. https://www.hse.ie/eng/about/who/acute-hospitals-division/woman-infants/clinical-guidelines/ovarian-hyperstimulation-syndrome-diagnosis-and-management.pdf https://www.hse.ie/eng/about/who/acute-hospitals-division/woman-infants/clinical-guidelines/ovarian-hyperstimulation-syndrome-diagnosis-and-management.pdf