Abstract
Background: Sedentary behavior (SB) is considered a risk factor for musculoskeletal pain. We aimed to explore the association of sedentary behavior indicators with neck pain among children and adolescents.
Methods: A comprehensive review was performed in different databases until the end of January 2022. Odds ratios (ORs) with 95% confidence intervals were used as desired effect sizes to evaluate the association between prolonged screen time or mobile phone (MP) usage and neck pain risk.
Results: Among 1651 records, 15 cross-sectional studies were included in the systematic review, and 7 reports were included in the meta-analysis. Our results suggested a significant relationship between prolonged MP use and neck pain (OR=1.36, 95% CI=1.001–1.85, I2=40.8%, P value for heterogeneity test=0.119). Furthermore, a marginally insignificant association was found between prolonged screen time and neck pain (OR=1.13, 95% CI=0.98–1.30, I2=60.3%, P value=0.01); however, after sensitivity analysis and removing one study, this association became significant (OR=1.30, 95% CI=1.03–1.64). Moreover, a significant association between prolonged sitting time and neck pain was reported in two studies.
Conclusion: Available good-quality evidence reveals a significant mild association between sedentary behavior and the risk of neck pain among children and adolescents. However, longitudinal studies with objective measurement tools are warranted. In particular, potential preventive educational programs are suggested for pediatrics to reduce sedentary behavior and neck pain.
Keywords: Neck pain, Sedentary behavior, Screen time, Cell phone use, Meta-analysis
Introduction
Musculoskeletal pain (MSP) is a worldwide problem affecting people of all ages in both sexes. It is one of the major reasons for disability-adjusted life years.1,2 Neck pain (NP) is one of the most common MSPs, with a 27 per 1000 people prevalence rate. The United States spent approximately $134.5 billion on low back and NP in 2016.3 NP could be due to various reasons, including the involvement of nerve roots, muscles, joints, ligaments, or intervertebral discs. Most of the time, there is no underlying systemic disorder; thus, it is included in MSPs.4 Based on the World Health Organization (WHO) reports, NP is the 8th-ranked reason for years lived with disability in adolescents.5 Moreover, evidence suggests that persistent MSPs during childhood increase the risk of developing chronic MSPs in adulthood.6-8 Nevertheless, MSPs in adolescents have not been as extensively focused on as in adults.
Sedentary behaviors (SBs) involve activities with very low energy expenditure that are mostly performed in sitting or lying down positions, such as mobile phone (MP) use, computer use, TV watching, video gaming, and prolonged sitting.9,10 There is confirmed data about the association between SB and non-communicable diseases like cardiovascular disease and cancer.11,12 Besides, SBs are one of the items previously correlated to NP in adults and adolescents and are suggested to be an essential factor for differences in NP prevalence in populations.13-15 However, some studies did not suggest any significant association between SB and NP. For instance, Dianat et al16 reported no remarkable association between computer use, playing video games, and watching TV with NP history in the past month. Similarly, Silva et al17 did not report a significant relationship between MP and computer use with NP history in the last six months.
With more innovations in technology, an increase in SBs is unavoidable. Thus, to summarize the available evidence and address the controversies, we aimed to assess the relationship between different types of sedentary behaviors and NP, among children and adolescents, through a systematic literature review and meta-analysis.
Methods
Search strategy
We carried out the current study based on PRISMA 2020 statement.18 The PROSPERO code for the protocol of this study is CRD42022313079. The systematic search was conducted in biomedical databases, including Web of Science, Scopus, PubMed, Embase, and Google Scholar, for available records until January 2022. Based on our research question, the search strings were made by combining equivalents of sedentary behavior (including screen time and sitting time) on the one hand and neck pain on the other in the biomedical databases. The search line for each mentioned database is shown in Supplementary file 1.
Eligibility criteria and study selection
After removing the duplicates, two independent reviewers (SMB and SM-T) reviewed and screened the records based on the title, abstract, and full text. Meanwhile, conference proceedings, books, letters, and reviews were deleted. Additionally, the references of related review articles were checked to find undetected appropriate studies. The third reviewer (RK) resolved any disagreement related to eligible records. Only English-language and full-text articles (on human subjects) were included. Figure 1 shows the process of eligibility assessment.
Figure 1.
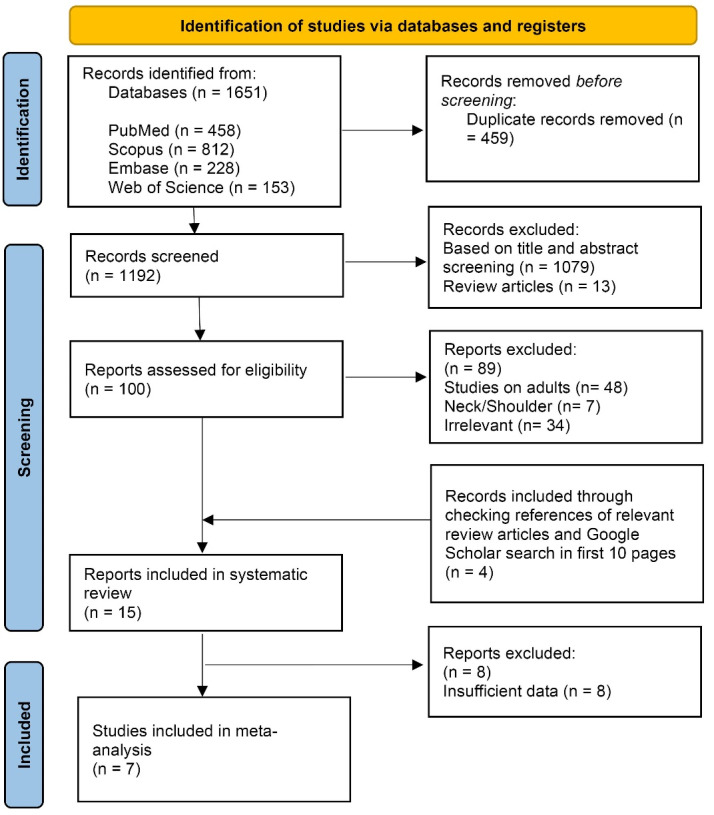
PRISMA flow diagram
Inclusion criteria
All observational research (cohort, case-control, and cross-sectional studies) on children or adolescents that assessed the relationship between different forms of SBs (screen time and sitting time) and NP were eligible to be included without the restriction of race, gender, and publication date.
Exclusion criteria
Studies with the following criteria were excluded: experimental research, studies on neck/shoulder pain, studies on cervical radicular pain, studies that assessed neck disability index, and studies with insufficient data.
Data extraction
Two independent reviewers (SBM, SM-T) performed data extraction from included articles. First author’s name, study design, publication date, study participants, sample size, gender, age range, type of SB, NP assessment tool, and a summary of main findings were extracted.
Quality assessment
The National Institute of Health (NIH) quality assessment tool was utilized to evaluate the quality of included records.19 The scale consists of 14 items for cross-sectional and cohort studies. Based on the mentioned tool, the quality of articles classifies as good, fair, and poor.
Data synthesis
For the meta-analysis, studies that investigated computer, tablet, and TV watching, as well as video gaming, were categorized as screen time. According to available data, the odds ratios (ORs) with 95% confidence intervals (CIs) were used as the effect sizes to evaluate the relationship between prolonged screen time or MP use and the risk of NP among children and adolescents. The random-effects model using DerSimonian and Laird was used for data analysis. Corresponding forest plots were made for both exposure factors. The heterogeneity of records was evaluated by Cochrane’s Q statistic and the inconsistency index (I2-statistic). The leave-one-out method was utilized for sensitivity analysis.
Moreover, the possible publication bias was assessed with funnel plots and was quantitatively examined by both Egger’s and Begg’s tests. We would use the trim-and-fill method to adjust the effect if there was publication bias. A two-sided P < 0.05 was considered significant in all cases. All analyses were conducted by STATA v12 (Stata Corporation, College Station, Texas, USA).
Results
Study selection
According to the initial search in the mentioned databases, 1651 records were recognized. After excluding duplications, 1192 papers were screened through the title and abstract. Then, 100 articles remained for further investigations via full text. Eventually, 15 articles were eligible for inclusion in the qualitative analysis, and 7 reports were included in the quantitative analysis. Figure 1shows the PRISMA flow diagram.
Study characteristics
All 15 included articles were in the cross-sectional design. The participants of all studies were school students (age range of 8- to 19-year-old), with nearly equal participants of both genders. These 15 studies explored 15512 participants from different years (from 2008 to 2022). The smallest sample size was 91 school students in Indonesia,20 and the largest one was 2750 from a study in Thailand.21 Included research was from different countries, including three in Brazil,14,15,22 two in Portugal,17,23 two in South Africa,24,25 and one study from Pakistan,13 Tunisia,26 Saudi Arabia,27 Thailand,21 Iran,16 Indonesia,20 Taiwan,28 and Bosnia and Herzegovina.29
MP usage, computer usage, watching TV, and playing video games are the most frequent SBs that have been assessed in six,13-15,17,20,23 seven,14,16,21,22,24-26 five,14,16,21,23,26 and four16,22,23,26 articles respectively. Other SBs like tablet usage, e-devices usage, sitting and doing homework, phone talking and texting, and sitting duration in school have also been assessed.
According to our search results, we divided the measured outcomes into screen time (computer usage, watching TV, and playing video games), MP usage, and sitting time (sitting duration in school and sitting time while doing homework). Based on the available data, we perform meta-analyses on studies evaluating the association between screen time or MP usage and NP.
Studies used different methods, including Questionnaires, interviews, and one-item questions for NP assessment. Each study investigated the history of NP in various timeframes, from the last week to the last 12 months. Table 1 presents the complete information of included studies.
Table 1. Included studies in the systematic review .
| Author, year | Country | Study design | Participants | Sample size | Gender (male%) | Age (year) | Sedentary behavior | Assessment of NP | Outcome | Main finding | QA |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mandhwani et al 2022 13 | Pakistan | Cross-sectional | School-going children | 385 | 50 | 11-15 | MP usage | One-item question | NP in the past 12 months | MP usage associated with NP | Fair |
| De Vitta et al 2021* 14 | Brazil | Cross-sectional | High school students | 1628 | 49 | 14-18 | Watching TV, computer use, MP usage, tablet usage | Interview | NP in the past 12 months | NP was associated with computer use ( > 3 h/day), MP usage in standing position, MP usage ( > 3 h/day), tablet usage in both standing and sitting positions, and tablet usage ( > 3 h/day) | Good |
| de Brito Nunes et al. 2021 15 | Brazil | Cross-sectional | High school students | 286 | 53.1 | 15-19 | MP addiction | One-item question | Cervical pain in the last 7 days | MP addiction was associated with cervical pain | Good |
| Minghelli 2019* 23 | Portugal | Cross-sectional | Elementary school students and high school students | 304 | 47.4 | 10-17 | MP usage, watching TV, console games | Interview | NP in the past 12 months | NP was associated with just MP usage | Good |
| Ben Ayed et al. 2019* 26 | Tunisia | Cross-sectional | Secondary school grade students | 1221 | 40.3 | 12-18 | Computer use, watching TV, playing videogames | Questionnaire | NP in the past 3 months | NP was associated with just computer use ( > 4 h/week) | Good |
| Alzaid et al. 2018 27 | Saudi Arabia | Cross-sectional | Children | 2435 | 58 | < 18 | e-devices usage | Questionnaire | NP | NP was associated with time spent on e-devices | Fair |
| Keeratisiroj and Siritaratiwat 2018 21 | Thailand | Cross-sectional | Primary and secondary school children | 2750 | 50 | 10-19 | Computer use, sitting and doing homework, watching TV | Questionnaire | NP in the past 12 months | NP was associated with computer use and sitting and doing homework | Good |
| Dianat et al 2017* 16 | Iran | Cross-sectional | School children | 1611 | 46.6 | 11-14 | Computer use, playing video games, watching TV | Questionnaire | NP in the past month | There is no association | Good |
| Silva et al. 2017* 17 | Portugal | Cross-sectional | High school students | 969 | 48.2 | 13-19 | MP usage, computer usage | Questionnaire | NP in the last 7 days | There is no association | Good |
| Widhiyanto et al 2017 20 | Indonesia | Cross-sectional | School students | 91 | 41.8 | NR | Duration of MP usage | Questionnaire | NP | Duration of MP usage was associated with NP | Fair |
| Yang et al 2016* 28 | Taiwan | Cross-sectional | Junior college students | 302 | 60.3 | NR | Phone talking, texting, | Questionnaire | NP in the past 6 months | There is no association | Good |
| Silva et al 2015 22 | Brazil | Cross-sectional | High school students | 961 | 38 | 14-19 | Computer use, playing video games, total time spent on e-devices | Questionnaire | Cervical pain in the past 6 months | Cervical pain was associated with computer usage ( > 3 h/day), video gaming ( > 1 h/day), and the total time of use ( > 4 h/day) | Good |
| Azabagic et al 2016 29 | Bosnia and Herzegovina | Cross-sectional | Primary school children | 1315 | 49.5 | 8-12 | Sitting duration in the school and during homework | Questionnaire | Acute NP | NP was associated with sitting duration in the school and during homework | Good |
| Mafanya and Rhoda 2011 25 | South Africa | Cross-sectional | High school students | 181 | 53.6 | 14-18 | Computer usage at school and elsewhere | Questionnaire | NP in the past month | NP was associated with computer usage elsewhere | Fair |
| Smith et al 2008* 24 | South Africa | Cross-sectional | High school students | 1073 | 35.1 | 14-18 | Computer usage ( > 8.5 h/week) | Questionnaire | NP in the past month | NP was associated with high hours of computer usage | Good |
Abbreviations; MP: mobile phone, NP: neck pain, QA: Quality assessment, e-devices: electronic devices, NR: not reported.
* Included articles in the meta-analysis.
According to the NIH quality assessment tool, among 15 included articles in the systematic review, 11 studies were qualified as good quality, and 4 studies as fair quality. All included papers in the meta-analysis had good quality. Table 2reveals the quality assessment of included studies in detail.
Table 2. Quality assessment of included studies in the systematic review .
| Study | Questions of NIH quality assessment tool for cohort and cross-sectional studies a | Summary quality | |||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | ||
| Mandhwani et al 2022 13 | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | Yes | NA | No | Fair |
| de Vitta et al 2021 14 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | NA | Yes | Good |
| de Brito Nunes et al 2021 15 | Yes | Yes | Yes | Yes | No | No | No | Na | Yes | No | Yes | Yes | NA | Yes | Good |
| Minghelli 2019 23 | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | Yes | NA | Yes | Good |
| Ben Ayed et al 2019 26 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | NA | Yes | Good |
| Alzaid et al 2018 27 | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | No | Yes | NA | Yes | Fair |
| Keeratisiroj and Siritaratiwat 2018 21 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | No | Yes | Yes | NA | Yes | Good |
| Dianat et al 2017 16 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | NA | Yes | Good |
| Silva et al 2017 17 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | NA | Yes | Good |
| Widhiyanto et al 2017 20 | Yes | No | No | Yes | Yes | No | No | Yes | No | No | No | Yes | NA | No | Fair |
| Yang et al 2016 28 | Yes | No | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | NA | No | Good |
| Azabagic et al 2016 29 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | NA | No | Good |
| Silva et al 2015 22 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | NA | Yes | Good |
| Mafanya and Rhoda 201125 | Yes | No | Yes | Yes | No | No | No | Yes | No | No | Yes | Yes | NA | Yes | Fair |
| Smith et al 2008 24 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | NA | Yes | Good |
aAvailable online at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
NA, Not applicable.
Main findings of meta-analysis for prolonged screen time
Results of the meta-analysis based on the crude odds ratio as desired effect size for the relationship between prolonged screen time and NP are shown in Figure 2. The pooled ORs by random effect model indicated no significant relationship between prolonged screen time and NP (OR = 1.13, 95% CI = 0.98–1.30), with significant heterogeneity (I2 = 60.3%, P value = 0.01).
Figure 2.
The pooled odds ratio for the association between prolonged screen time and neck pain among children and adolescents
Both Egger and Begg’s tests showed no evidence of publication bias (the P value of Egger’s test = 0.66, and the P value of Begg’s test = 0.60) (Figure 3).
Figure 3.

Funnel plot for publication bias of prolonged screen time and risk of neck pain
Main findings of meta-analysis for prolonged MP use
Results of the meta-analysis based on the adjusted odds ratio as desired effect size for the association between prolonged MP use and NP are summarized in Figure 4. The pooled ORs by random effect model showed that prolonged MP use was a significant risk factor for NP (OR = 1.36, 95% CI = 1.001–1.85), with non-significant heterogeneity (I2 = 40.8%, P value = 0.119).
Figure 4.

The pooled odds ratio for the association between prolonged MP use and neck pain among children and adolescents
Both Egger and Begg’s tests showed no publication bias (the P value of Egger’s test = 0.59, and the P value of Begg’s test = 0.45) (Figure 5).
Figure 5.

Funnel plot for publication bias of prolonged MP use and risk of neck pain
Sensitivity analysis
Sensitivity analyses revealed no significant differences between the before-after sensitivity pooled OR for the association between prolonged screen time and NP after excluding Silva et al,17 Ben Ayed et al,26 Minghelli et al,23 and Smith et al24 studies. However, results indicated a significant change between before-after sensitivity pooled OR for the association between prolonged screen time and NP after excluding Dianat et al study16 (OR = 1.30; 95% CI, 1.03–1.64).
Prolonged sitting time and NP
Two studies explored the association between prolonged sitting time and NP. Keeratisiroj and Siritaratiwat indicated that prolonged sitting and doing homework was associated with NP in the last 12 months among school children in Thailand.21 Another study on school children in Bosnia and Herzegovina demonstrated a significant relationship between sitting duration in school and during homework with acute NP.29 However, research on sitting time and neck pain in children is scarce and needs extra focus.
Discussion
This review investigated the relationship between different types of SBs and NP in adolescents and children. Results of the meta-analysis indicated a marginally insignificant association of screen time with NP. However, this association was significant after excluding one study in the sensitivity analysis (OR = 1.30). Moreover, we found a remarkable association between MP use and NP (OR = 1.36).
Some controversies exist in reviewing the literature. Dianat et al16 demonstrated no significant relationship between computer use, watching TV, and playing video games with NP in the last month. Alternatively, Silva et al17 suggested no significant relationship between MP and computer use with NP in the last seven days. These findings are in contrast with other studies,14,21-23,26 and that might be, on the one hand, because of the unknown level of the certainty of the information given about MSPs and the amount of time devoted to SBs, and on the other hand, differences in the time of neck pain history.
Nowadays, the time spent in SBs among adolescents and children has increased dramatically because of innovations in technology.30 Besides, during the current COVID-19 pandemic, SBs increased in all age groups, including adolescents and children.31 SBs in adolescents are demonstrated to have an association with an increased risk of a health crisis, including increased body mass index,32 higher blood pressure,33 and even psychosomatic health problems such as headaches, abdominal pains, irritability, difficulty falling asleep and feeling nervous.34
NP is a widespread and multifactorial public health crisis. Several neck structures, including discs, ligaments, joints, muscles, and nerves, might be the source of pain.35 Different pathologies could represent NP, such as tumors, congenital disorders, infections, and inflammatory diseases. However, most conditions have no systemic complications and are named MSPs.36 Recently, there has been a rise in adolescents complaining of NP.37 “Text Neck” syndrome is a newly emerged term used to describe the NP because leaning forward for prolonged periods, looking at the MP, tablet, and other e-devices while texting. Finally, prolonged neck flexion results in the “text neck”.38 Based on the text neck concept, higher weight is put on the spine with more flexion in the neck.39 The relation between text neck and NP is questionable. Some studies support the idea of an association of text neck with NP among adolescents5,40,41; however, some others did not find any relationship.42,43
Many researches have suggested obesity as a risk factor for NP in adolescents.44,45 Obesity is an important health problem with increasing rates among children and adolescents with a sedentary lifestyle.46 However, there is conflicting evidence on the association of obesity with NP. A retrospective cohort study on primary school children reported a significant association between obesity and NP,47 in line with a survey conducted by Martínez-Romero et al48 and Dianat et al16 However, some other studies did not report any association.49,50 On the other hand, a cohort research with two years of follow-up on 848 school children in Denmark demonstrated a higher incidence of overweight among children with pain in the spinal column. The relative risk for becoming overweight was reported (RR = 5.3, 95% CI = 3.98–7.58) for children with spinal pain and (RR = 1.6, 95% CI = 0.19–5.45) for children without.51
Physical activity is a possible protective factor against developing NP in adolescents.52,53 Lower physical activities are associated with higher SBs54; thus, they could be associated with NP. Enough physical activity diminishes spinal pain and NP by reducing muscle tension, decreasing pressure on vertebral discs, and increasing blood circulation.55 However, a systematic review demonstrated no significant relationship between physical activity and NP in children.56
One crucial factor that is associated with higher rates of MSPs in school-aged children is heavy-weight school bags. The average weight of a school bag should not exceed 10% of the body weight; otherwise, irreparable consequences on the spinal cord are unavoidable.57 Thus, according to their child, parents’ knowledge about a standard-weight backpack should increase.58
All SBs are approximately indoor activities, which reduce outdoor physical activity and, as a result, sun exposure. Thus, limited sunlight exposure causes lower serum vitamin D levels in a sedentary lifestyle.59,60 On the other hand, investigations demonstrated that vitamin D deficiency increases MSPs rates among children61 and also showed a significant decrease in MSPs of vitamin D deficient children prescribed vitamin D for six months.62 Given the information, vitamin D deficiency might be an underlying mechanism for NP in groups with higher SBs.63
Most children and adolescents are unaware of the long-term effect of MSPs because there are no severe short-term effects. On the other hand, adolescents are the greatest users of e-devices. Thus, paying attention to this group is essential to reduce their future disabilities and increasing life expectancy.5 Based on the latest WHO guideline on physical activity and sedentary behavior, children and adolescents is recommended for at least one hour of moderate-to-vigorous intensity physical activity per day. Moreover, a strong association was observed between lower SBs and a lower risk of future non-communicable diseases.64,65
Limitations of data synthesis
First, all the included studies used self-reported data; thus, various factors could affect the certainty level of collected data. Second, included studies assessed the associations among school children, and it might be questionable whether the pooled results could be generalized to the other groups of adolescents. Third, our results indicated a mild relationship between SBs and NP, possibly because of the limited number of included studies or the moderating effects of other factors related to children’s neck pain. Moreover, all included articles in this study were in a cross-sectional design. Further longitudinal studies will demonstrate the relationship and causality effect more accurately.
Strengths of the study
First, there is limited data on neck pain and sedentary behavior among children and adolescents, and the current work is the first review and meta-analysis in this field. Second, all included articles had acceptable quality and no publication bias.
Conclusion
Based on available good-quality evidence, MP use is associated with an increased risk of NP. Moreover, a marginally insignificant association between screen time with NP is observed. However, research on sitting time and neck pain in children is scarce and needs extra focus. It seemed necessary that the effect of sedentary behaviors such as screen time be assessed in different populations, especially after the COVID-19 pandemic, which increased the sedentary behaviors among adolescents, to determine the effect more accurately. Moreover, it is recommended that further studies aim to assess NP using unified objective tools validated across different cultures.
Author Contributions
Conceptualization: Roya Kelishadi, Sadegh Baradaran Mahdavi, Sadegh Mazaheri-Tehrani.
Data curation: Sadegh Mazaheri-Tehrani, Roya Riahi, Sadegh Baradaran Mahdavi.
Formal Analysis: Roya Riahi.
Investigation: Sadegh Baradaran Mahdavi, Sadegh Mazaheri-Tehrani.
Methodology: Roya Kelishadi, Sadegh Baradaran Mahdavi.
Project administration: Roya Kelishadi, Babak Vahdatpour.
Software: Roya Riahi, Sadegh Mazaheri-Tehrani.
Supervision: Roya Kelishadi, Babak Vahdatpour.
Writing – original draft: Sadegh Baradaran Mahdavi, Sadegh Mazaheri-Tehrani, Roya Riahi.
Writing – review & editing: Sadegh Baradaran Mahdavi, Sadegh Mazaheri-Tehrani, Roya Riahi, Roya Kelishadi, Babak Vahdatpour.
Funding
This research received no specific grant.
Ethical Approval
Not applicable.
Competing Interests
None to declare.
Supplementary Files
Supplementary file 1 containsthe search line for each mentioned database.
References
- 1.Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain-where to from here? Am J Public Health. 2019;109(1):35–40. doi: 10.2105/ajph.2018.304747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zitko P, Bilbeny N, Balmaceda C, Abbott T, Carcamo C, Espinoza M. Prevalence, burden of disease, and lost in health state utilities attributable to chronic musculoskeletal disorders and pain in Chile. BMC Public Health. 2021;21(1):937. doi: 10.1186/s12889-021-10953-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kazeminasab S, Nejadghaderi SA, Amiri P, Pourfathi H, Araj-Khodaei M, Sullman MJM, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. doi: 10.1186/s12891-021-04957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bogduk N. The anatomy and pathophysiology of neck pain. Phys Med Rehabil Clin N Am. 2011;22(3):367–82, vii. doi: 10.1016/j.pmr.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Fares J, Fares MY, Fares Y. Musculoskeletal neck pain in children and adolescents: risk factors and complications. Surg Neurol Int. 2017;8:72. doi: 10.4103/sni.sni_445_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamper SJ, Henschke N, Hestbaek L, Dunn KM, Williams CM. Musculoskeletal pain in children and adolescents. Braz J Phys Ther. 2016;20(3):275–84. doi: 10.1590/bjpt-rbf.2014.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones GT, Silman AJ, Power C, Macfarlane GJ. Are common symptoms in childhood associated with chronic widespread body pain in adulthood? Results from the 1958 British Birth Cohort Study. Arthritis Rheum. 2007;56(5):1669–75. doi: 10.1002/art.22587. [DOI] [PubMed] [Google Scholar]
- 8.Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. 2004;8(3):187–99. doi: 10.1016/j.ejpain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baradaran Mahdavi S, Riahi R, Vahdatpour B, Kelishadi R. Association between sedentary behavior and low back pain; a systematic review and meta-analysis. Health Promot Perspect. 2021;11(4):393–410. doi: 10.34172/hpp.2021.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katzmarzyk PT, Powell KE, Jakicic JM, Troiano RP, Piercy K, Tennant B. Sedentary behavior and health: update from the 2018 physical activity guidelines advisory committee. Med Sci Sports Exerc. 2019;51(6):1227–41. doi: 10.1249/mss.0000000000001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dempsey PC, Matthews CE, Dashti SG, Doherty AR, Bergouignan A, van Roekel EH, et al. Sedentary behavior and chronic disease: mechanisms and future directions. J Phys Act Health. 2020;17(1):52–61. doi: 10.1123/jpah.2019-0377. [DOI] [PubMed] [Google Scholar]
- 13.Mandhwani S, Zia S, Shaikh ES, Duarte D, Tanveer E. Association between cell phone usage and musculoskeletal disorders in school going children. J Musculoskelet Res. 2022;25(1):2250003. doi: 10.1142/s0218957722500038. [DOI] [Google Scholar]
- 14.de Vitta A, Bento TPF, de Oliveira Perrucini P, Felippe LA, Poli-Frederico RC, Borghi SM. Neck pain and associated factors in a sample of high school students in the city of Bauru, São Paulo, Brazil: cross-sectional study. Sao Paulo Med J. 2021;139(1):38–45. doi: 10.1590/1516-3180.2020.0168.r1.30102020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Brito Nunes PP, Abdon APV, de Brito CB, Silva FVM, Santos ICA, de Queiroz Martins D, et al. Factors related to smartphone addiction in adolescents from a region in Northeastern Brazil. Cien Saude Colet. 2021;26(7):2749–58. doi: 10.1590/1413-81232021267.08872021. [DOI] [PubMed] [Google Scholar]
- 16.Dianat I, Alipour A, Asgari Jafarabadi M. Risk factors for neck and shoulder pain among schoolchildren and adolescents. J Paediatr Child Health. 2018;54(1):20–7. doi: 10.1111/jpc.13657. [DOI] [PubMed] [Google Scholar]
- 17.Silva AG, Sa-Couto P, Queirós A, Neto M, Rocha NP. Pain, pain intensity and pain disability in high school students are differently associated with physical activity, screening hours and sleep. BMC Musculoskelet Disord. 2017;18(1):194. doi: 10.1186/s12891-017-1557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Study Quality Assessment Tools. NHLBI, NIH. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 20.Widhiyanto A, Munawir A, Prayitno H. The effect of duration of smartphone usage on neck pain. Dama International Journal of Researchers (DIJR) 2017;2(11):54–61. [Google Scholar]
- 21.Keeratisiroj O, Siritaratiwat W. Prevalence of self-reported musculoskeletal pain symptoms among school-age adolescents: age and sex differences. Scand J Pain. 2018;18(2):273–80. doi: 10.1515/sjpain-2017-0150. [DOI] [PubMed] [Google Scholar]
- 22.Silva GR, Pitangui AC, Xavier MK, Correia-Júnior MA, De Araújo RC. Prevalence of musculoskeletal pain in adolescents and association with computer and videogame use. J Pediatr (Rio J) 2016;92(2):188–96. doi: 10.1016/j.jped.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Minghelli B. Musculoskeletal spine pain in adolescents: Epidemiology of non-specific neck and low back pain and risk factors. J Orthop Sci. 2020;25(5):776–80. doi: 10.1016/j.jos.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Smith L, Louw Q, Crous L, Grimmer-Somers K. Prevalence of neck pain and headaches: impact of computer use and other associative factors. Cephalalgia. 2009;29(2):250–7. doi: 10.1111/j.1468-2982.2008.01714.x. [DOI] [PubMed] [Google Scholar]
- 25.Mafanya C, Rhoda A. Predictors of neck pain among South African youth: lifestyle and risk behaviour. Afr J Phys Health Educ Recreat Dance. 2011;17(Suppl-1):82–9. doi: 10.10520/ejc19771. [DOI] [Google Scholar]
- 26.Ben Ayed H, Yaich S, Trigui M, Ben Hmida M, Ben Jemaa M, Ammar A, et al. Prevalence, risk factors and outcomes of neck, shoulders and low-back pain in secondary-school children. J Res Health Sci. 2019;19(1):e00440. [PMC free article] [PubMed] [Google Scholar]
- 27.Alzaid AN, Alshadokhi OA, Alnasyan AY, AlTowairqi MY, Alotaibi TM, Aldossary FH. The prevalence of neck pain and the relationship between prolonged use of electronic devices and neck pain in: a Saudi Arabia, cross- sectional study in Saudi Arabia. Egypt J Hosp Med. 2018;70(11):1992–9. doi: 10.21608/ejhm.2018.9405. [DOI] [Google Scholar]
- 28.Yang SY, Chen MD, Huang YC, Lin CY, Chang JH. Association Between Smartphone Use and Musculoskeletal Discomfort in Adolescent Students. J Community Health. 2017;42(3):423–30. doi: 10.1007/s10900-016-0271-x. [DOI] [PubMed] [Google Scholar]
- 29.Azabagic S, Spahic R, Pranjic N, Mulic M. Epidemiology of musculoskeletal disorders in primary school children in Bosnia and Herzegovina. Mater Sociomed. 2016;28(3):164–7. doi: 10.5455/msm.2016.28.164-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hardy LM, Frisdal E, Le Goff W. Critical role of the human ATP-binding cassette G1 transporter in cardiometabolic diseases. Int J Mol Sci. 2017;18(9):1892. doi: 10.3390/ijms18091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Runacres A, Mackintosh KA, Knight RL, Sheeran L, Thatcher R, Shelley J, et al. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(21):11286. doi: 10.3390/ijerph182111286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mitchell JA, Pate RR, Beets MW, Nader PR. Time spent in sedentary behavior and changes in childhood BMI: a longitudinal study from ages 9 to 15 years. Int J Obes (Lond) 2013;37(1):54–60. doi: 10.1038/ijo.2012.41. [DOI] [PubMed] [Google Scholar]
- 33.Martinez-Gomez D, Tucker J, Heelan KA, Welk GJ, Eisenmann JC. Associations between sedentary behavior and blood pressure in young children. Arch Pediatr Adolesc Med. 2009;163(8):724–30. doi: 10.1001/archpediatrics.2009.90. [DOI] [PubMed] [Google Scholar]
- 34.Faridizad R, Ahadi Z, Heshmat R, Motlagh ME, Sheidaei A, Ziaodini H, et al. Association of screen time with subjective health complaints in Iranian school-aged children and adolescents: the CASPIAN-V study. J Public Health. 2020;28(1):31–40. doi: 10.1007/s10389-019-01014-2. [DOI] [Google Scholar]
- 35.David D, Giannini C, Chiarelli F, Mohn A. Text neck syndrome in children and adolescents. Int J Environ Res Public Health. 2021;18(4):1565. doi: 10.3390/ijerph18041565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bogduk N. Neck pain. Aust Fam Physician. 1984;13(1):26–30. [PubMed] [Google Scholar]
- 37.Cuéllar JM, Lanman TH. “Text neck”: an epidemic of the modern era of cell phones? Spine J. 2017;17(6):901–2. doi: 10.1016/j.spinee.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 38.Neupane S, Ifthikar Ali UT, Mathew A. Text neck syndrome-systematic review. Imp J Interdiscip Res. 2017;3(7):141–8. [Google Scholar]
- 39.Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277–9. [PubMed] [Google Scholar]
- 40.Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz J Phys Ther. 2014;18(4):364–71. doi: 10.1590/bjpt-rbf.2014.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nejati P, Lotfian S, Moezy A, Moezy A, Nejati M. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Med J Islam Repub Iran. 2014;28:26. [PMC free article] [PubMed] [Google Scholar]
- 42.Damasceno GM, Ferreira AS, Nogueira LAC, Reis FJJ, Andrade ICS, Meziat-Filho N. Text neck and neck pain in 18-21-year-old young adults. Eur Spine J. 2018;27(6):1249–54. doi: 10.1007/s00586-017-5444-5. [DOI] [PubMed] [Google Scholar]
- 43.Richards KV, Beales DJ, Smith AJ, O’Sullivan PB, Straker LM. Neck posture clusters and their association with biopsychosocial factors and neck pain in Australian adolescents. Phys Ther. 2016;96(10):1576–87. doi: 10.2522/ptj.20150660. [DOI] [PubMed] [Google Scholar]
- 44.Jahre H, Grotle M, Smedbråten K, Dunn KM, Øiestad BE. Risk factors for non-specific neck pain in young adults. A systematic review. BMC Musculoskelet Disord. 2020;21(1):366. doi: 10.1186/s12891-020-03379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Onan D, Ulger O. Investigating the relationship between body mass index and pain in the spine in children or adolescents: a systematic review. Child Obes. 2021;17(2):86–99. doi: 10.1089/chi.2020.0266. [DOI] [PubMed] [Google Scholar]
- 46.Lee EY, Yoon KH. Epidemic obesity in children and adolescents: risk factors and prevention. Front Med. 2018;12(6):658–66. doi: 10.1007/s11684-018-0640-1. [DOI] [PubMed] [Google Scholar]
- 47.Azabagic S, Pranjic N. The site of musculoskeletal pain in school children with excessive body weight and obesity in Bosnia and Herzegovina. Mater Sociomed. 2019;31(2):88–92. doi: 10.5455/msm.2019.31.88-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martínez-Romero MT, Cejudo A, Sainz de Baranda P. Prevalence and characteristics of back pain in children and adolescents from the Region of Murcia (Spain): ISQUIOS programme. Int J Environ Res Public Health. 2022;19(2):946. doi: 10.3390/ijerph19020946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gheysvandi E, Dianat I, Heidarimoghadam R, Tapak L, Karimi-Shahanjarini A, Rezapur-Shahkolai F. Neck and shoulder pain among elementary school students: prevalence and its risk factors. BMC Public Health. 2019;19(1):1299. doi: 10.1186/s12889-019-7706-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deere KC, Clinch J, Holliday K, McBeth J, Crawley EM, Sayers A, et al. Obesity is a risk factor for musculoskeletal pain in adolescents: findings from a population-based cohort. Pain. 2012;153(9):1932–8. doi: 10.1016/j.pain.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 51.Hestbaek L, Aartun E, Côté P, Hartvigsen J. Spinal pain increases the risk of becoming overweight in Danish schoolchildren. Sci Rep. 2021;11(1):10235. doi: 10.1038/s41598-021-89595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scarabottolo CC, Pinto RZ, Oliveira CB, Zanuto EF, Cardoso JR, Christofaro DGD. Back and neck pain prevalence and their association with physical inactivity domains in adolescents. Eur Spine J. 2017;26(9):2274–80. doi: 10.1007/s00586-017-5144-1. [DOI] [PubMed] [Google Scholar]
- 53.Guddal MH, Stensland S, Småstuen MC, Johnsen MB, Zwart JA, Storheim K. Physical activity level and sport participation in relation to musculoskeletal pain in a population-based study of adolescents: the young-HUNT study. Orthop J Sports Med. 2017;5(1):2325967116685543. doi: 10.1177/2325967116685543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Christofaro DG, De Andrade SM, Mesas AE, Fernandes RA, Farias Júnior JC. Higher screen time is associated with overweight, poor dietary habits and physical inactivity in Brazilian adolescents, mainly among girls. Eur J Sport Sci. 2016;16(4):498–506. doi: 10.1080/17461391.2015.1068868. [DOI] [PubMed] [Google Scholar]
- 55. Jackson CP, Brown MD. Is there a role for exercise in the treatment of patients with low back pain? Clin Orthop Relat Res. 1983(179):39-45. [PubMed]
- 56.Sitthipornvorakul E, Janwantanakul P, Purepong N, Pensri P, van der Beek AJ. The association between physical activity and neck and low back pain: a systematic review. Eur Spine J. 2011;20(5):677–89. doi: 10.1007/s00586-010-1630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dianat I, Javadivala Z, Allahverdipour H. School bag weight and the occurrence of shoulder, hand/wrist and low back symptoms among Iranian elementary schoolchildren. Health Promot Perspect. 2011;1(1):76–85. doi: 10.5681/hpp.2011.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Javadivala Z, Allahverdipour H, Dianat I, Bazargan M. Awareness of parents about characteristics of a healthy school backpack. Health Promot Perspect. 2012;2(2):166–72. doi: 10.5681/hpp.2012.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Milagres LC, Rocha NP, Albuquerque FM, Castro APP, Filgueiras MS, Pessoa MC, et al. Sedentary behavior is associated with lower serum concentrations of vitamin D in Brazilian children. Public Health. 2017;152:75–8. doi: 10.1016/j.puhe.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 60.da Silva ACM, Cureau FV, de Oliveira CL, Giannini DT, Bloch KV, Kuschnir MCC, et al. Physical activity but not sedentary time is associated with vitamin D status in adolescents: study of cardiovascular risk in adolescents (ERICA) Eur J Clin Nutr. 2019;73(3):432–40. doi: 10.1038/s41430-018-0192-0. [DOI] [PubMed] [Google Scholar]
- 61.Park MJ, Lee J, Lee JK, Joo SY. Prevalence of vitamin D deficiency in Korean children presenting with nonspecific lower-extremity pain. Yonsei Med J. 2015;56(5):1384–8. doi: 10.3349/ymj.2015.56.5.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Blagojevic Z, Nikolic V, Kisic-Tepavcevic D, Terzic Supic Z, Kovacevic R, Zivkovic Z, et al. Musculoskeletal pain and vitamin D deficiency in children: a pilot follow-up study of vitamin D therapy in musculoskeletal/orthopedic conditions. Acta Chir Orthop Traumatol Cech. 2016;83(1):21–6. [PubMed] [Google Scholar]
- 63.Baradaran Mahdavi S, Kelishadi R. Impact of sedentary behavior on bodily pain while staying at home in COVID-19 pandemic and potential preventive strategies. Asian J Sports Med. 2020;11(2):e103511. doi: 10.5812/asjsm.103511. [DOI] [Google Scholar]
- 64.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chaput JP, Willumsen J, Bull F, Chou R, Ekelund U, Firth J, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: summary of the evidence. Int J Behav Nutr Phys Act. 2020;17(1):141. doi: 10.1186/s12966-020-01037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file 1 containsthe search line for each mentioned database.



