Abstract
The burden of asthma disproportionately affects minority and low-income communities, resulting in racial and socioeconomic disparities in asthma prevalence, exacerbations, and asthma-related death. Social determinants of health are increasingly implicated as root causes of disparities and healthy housing is perhaps the most critical social determinant in asthma health disparities. In many minority communities, poor housing conditions and value are a legacy of historical policies and practices imbued with structural racism, including redlining, displacement, and exclusionary zoning. As a result, poor quality, substandard housing is a characteristic feature of many underrepresented minority communities. Consequently, structurally deficient housing stock cultivates home environments rife with indoor asthma triggers. In this review we consider the historical context of urban housing policies and practices and how this contributed to the substandard housing conditions for many minority children in the present day. We describe the impact of poor housing quality on asthma and interventions that have attempted to mitigate its influence on asthma symptoms and healthcare utilization. We discuss the need to promote asthma health equity by reinvesting in these neighborhoods and communities to provide healthy housing.
Keywords: asthma, housing, disparities, structural racism, social determinants of health
Capsule Summary
This paper discusses the historical context and the current state of housing disparities, how that fosters asthma disparities, and ways to promote asthma health equity by improving housing conditions.
Introduction
In the US, there are 5.1 million children with asthma, making it the most common chronic physical condition of childhood.1 Although in recent decades advancements in medical therapy have contributed to an overall reduction in asthma morbidity and mortality, racial, ethnic, and socioeconomic disparities persist for asthma outcomes, including rates of asthma-related death, hospitalization, and emergency room visits.2 The burden of asthma symptoms – sleep disturbance, activity limitation, and missed days of school and work – is disproportionately represented in underrepresented minority communities.3, 4, 5 To better understand and address asthma disparities, researchers, clinicians, and policymakers have increasingly turned to the role of social determinants of health. Although healthcare access remains important, other factors account for a substantial portion of health outcomes.6
For asthma disparities, perhaps none of these social determinants are as critical as housing. A landmark Institute of Medicine report established that exposure to indoor allergens such as mold, cockroach, mouse, and dust mite allergens is common in substandard housing.7 The overall level of disrepair in the home, particularly in low-income, urban communities is an important determinant of the presence of environmental asthma allergens.8 In this paper, we will highlight studies linking indoor aeroallergens, housing conditions, and asthma outcomes, as well as interventions aimed at modifying allergen exposure and the structural housing components that give rise to these exposures, including early results of a major structural repairs intervention we conducted. First, however, we highlight the critical historical context that gave rise to racial and ethnic inequities in housing quality and neighborhood investment, as expectations for solutions to housing-mediated asthma disparities must be bound by a candid understanding of their complex causes.
The Critical Context of History and Structural Racism
Racial disparities in housing value and quality are downstream results of systemic and structural racism. There are several detailed accounts of how structural racism became a feature of US housing practices and policy.9, 10 An in-depth discussion of this complex history is beyond the scope of this article, however, several key practices and policies are germane to understanding current racial disparities in housing value and quality in the US. These include “redlining”, a real estate practice of ranking non-White neighborhoods as credit-unworthy, which became codified in the federal housing policy in the 1930–1960s through the Home Owner’s Loan Corporation and Federal Housing Authority (FHA).11 These federal organizations were designed to promote home-ownership to low income individuals by providing refinancing assistance and underwriting mortgage risk, but because of the explicit use of race and ethnicity data, only 2% of FHA mortgage insurance was available to non-white families.12Another practice, exclusionary landuse zoning based on race and ethnicity was determined unconstitutional in 1917, but continued through the practice of zoning white, wealthy neighborhoods as exclusively single-family and low-density preventing the inclusion of multi-unit buildings with affordable rent for low-income communities of color. 13 Though the Fair Housing Act of 1968 rendered these practices illegal, they created segregated neighborhoods in which residents were systematically denied mortgages on the basis of race. As a result, entire neighborhoods predominantly occupied by minorities were denied access to home ownership, a key component of multigenerational wealth building.11
The ongoing effects of exclusionary housing practices and their long-term economic consequences for residents are still felt in neighborhoods characterized by poor quality, substandard, unhealthy housing. Greater housing deprivation leads to poor health and sustained housing deprivation increases the probability of poor health as adults.14 Historical oppressive housing practices have further resulted in limited housing choices for Black and Hispanic families.11 Homeowners in these neighborhoods often have lower-paying jobs or less opportunity for better-paying jobs, resulting in limited income which impairs their ability to maintain homes.15 Blacks are twice as likely to experience the burden of housing hardship- the ability of households to afford basic living needs and housing expenses.11, 16 The hardship of maintaining older homes results in defects in the building envelope leading to conditions in the home which promote problems with pests, leaking roof or ceiling, plumbing problems, holes or cracks in the walls or ceiling and large dangerous holes in the floor.17 Caregivers in low-income, struggle to provide healthy housing. Healthy housing, a basic necessity, is a dream for the poor and yet essential in promoting equitable asthma outcomes.
Impact of Poor Housing Quality on Asthma
In-home asthma triggers
Exposure to indoor allergens is the direct pathway by which poor housing quality may affect asthma.18 Early childhood exposure and sensitization to allergens found in substandard housing results in increased risk of incident asthma among those who are genetically predisposed.19 Continued exposure to allergens may exacerbate asthma symptoms and increase ongoing risk of asthma morbidity even after adjusting for age, sex, race, and ethnicity.20, 21In inner city children, exposure and sensitization to multiple asthma triggers has been associated with asthma severity. 21, 22 By one estimate, elimination of all identified residential risk factors for asthma would result in a 39% decrease in asthma in the United States.23
Pests such as cockroaches and rodents, more likely to be found in substandard housing, present a risk for children with asthma.24 Children with asthma who had been sensitized to mouse allergen are at increased risk of unscheduled physician visits, ED visits, and hospitalizations when exposed to mouse allergens in the home.25 Similarly, there is a dose response between exposure to cockroach antigen and asthma exacerbations.22, 26 Dust mites present in house dust can exacerbate asthma symptoms. 27, 28 Finally, mold is a common in-home allergen associated with asthma exacerbations. Infants exposed to high concentrations of mold species common among water-damaged buildings were more likely to have asthma when they reached school age.23
Housing conditions and asthma triggers
A pooled analysis of nine studies examined the relationship between housing conditions and the presence of asthma allergens.29 In homes that had not been actively maintained, common structural issues facilitate allergen exposure. Water intrusion, which can stem from plumbing leaks, roof leaks, and unventilated or damp basements, may lead to mold development and attract pests. Cracks and holes in the walls, below average housekeeping, and water leaks were positively associated with cockroach allergen. Housing built prior to 1951 was associated with elevated dust mite levels. Additionally, homes with basements or crawl spaces predicted increased allergens in the home. Carpet in older homes carry a large load of house dust which can lead to exposures to dust mite, pet dander and pests.30
Low-income households may face differing challenges in eliminating asthma allergens from the home. While homeowners have autonomy in maintaining their home, the cost burden of improvements may make it difficult for low-income homeowners to conduct repairs to address structural deficiencies that facilitate asthma triggers. Renters are less able to control the repairs in their homes and landlords may not be aware of the impact of housing conditions on residents’ asthma control.31, 32 Finally, when public housing is occupied by transient residents, it is more likely to have poorer-quality management and upkeep, resulting in conditions that facilitate the presence of asthma triggers.33
Levels of Intervention
Interventions aimed at reducing exposures to asthma triggers occur at three levels of intensiveness and investment: (1) multi-trigger, multicomponent interventions, (2) single, targeted structural repairs, and (3) major structural repairs.
Multi-trigger, multicomponent interventions
The CDC task force on Community Preventive Services recommends home-based, multicomponent, multi-trigger reduction interventions as an effective way to improve quality of life for children and adolescents with asthma.34 Except for pests such as cockroach and mice, targeting a single asthma trigger with environmental mitigation does not appear to be effective in improving asthma outcomes.35 Therefore, interventions for reducing common triggers such as dust, cockroach, mice, and mold require a multipronged approach. House dust mite can be reduced through multicomponent intervention including removal of carpet, mattress and pillow covers, and targeted cleaning strategies. Cockroach and mice allergens can be reduced through integrated pest management which includes cleaning, exclusion practices (filling holes), traps and non-toxic pest bait. 36 Mold allergen presence requires better ventilation, dehumidifiers and repair of leaks. Studies which use skin testing to target areas of intervention and a more general approach of reducing common asthma triggers in the home with community health workers have been shown to be both efficacious in reducing asthma exacerbations and overall effective. 37–39
Single, targeted structural repairs
Single intervention home repairs aimed at root causes of moisture damage, poor heating and poor ventilation for children with asthma show some promise in reducing the presence of asthma triggers, though generally do not address all asthma triggers in the home. In a pilot study of 72 children with asthma who lived in damp housing, interventions included gas central heating units in 47%, electric heaters in 37% and solid fuel central heating in 12%. All respiratory symptoms improved but nocturnal cough improved significantly from 3 to 1 night each month.40 In another study insulating homes led to self-reported improvement in symptoms, and reduced sick visits and missed work and schooldays.41, 42 In a tailored package which combined both ventilation and heating, self-reported physical functioning improved amongst children with moderate to severe asthma.43 Moisture reduction through targeted home repairs in addition to behavior interventions has also been associated with modestly improved asthma outcomes.44
Major structural repairs
Few studies have addressed comprehensive structural interventions aimed at root causes of a compromised building envelope and internal structural deficiencies, likely due to the expense of such an approach.44–46 However, it is the logical next step, given the linkage between poor housing conditions and asthma outcomes. In the Breathe Easy Homes intervention, Takaro and colleagues moved 34 renter families into new homes with added asthma-friendly elements including moisture proof exteriors, heat-exchange ventilation systems with filtration and continuous fresh air supply, and low emission, low dust accumulation interior finishes, in addition to being built with both energy efficient and sustainable products. In comparing the asthma outcomes of children who lived in those homes to children who did not, they found that nighttime symptoms improvement was similar to outcomes from 1 year of inhaled corticosteroid use in improving symptom free days. 45 Gruber and colleagues enrolled 42 families who were a combination of homeowners and renters.47 The HUD healthy home assessment (adapted for asthma triggers) was used at baseline to determine need for home structural and behavioral interventions. The repairs were prioritized to address mold and pest issues first, then heating, ventilation and dust next, which included the repair of heaters and ventilation and creation of vapor barriers and carpet removal. Findings included reduced symptoms, improved quality of life and reduced costs for hospitalizations. 46
A New Program Model: Linking Multi-trigger Interventions with Major Structural Repairs in Philadelphia
Philadelphia is characterized by older rowhomes built at the turn of the 20th century. Our program, the Community Asthma Prevention Program (CAPP) utilizes a community-based approach to implement asthma education and asthma trigger remediation interventions in homes. In the past twenty years, we have conducted over 20,000 home asthma education and trigger remediation visits for children with asthma. Unfortunately, due to the age of the homes and the consequences of historical redlining in Philadelphia, homeowners cannot always maintain their homes, limiting their ability to reduce asthma trigger exposure. Community Health Workers (CHW) are often struck by gaping holes in walls and ceilings, improper ventilation, old and worn carpeting and visible mold, all not addressed by our original interventions (see Box 1). For this reason, CAPP sought partners to expand in-home interventions to include structural repairs. With funding provided by our health system and the BUILD initiative, we partnered with two home repair agencies, Rebuilding Together Philadelphia (RTP) and Habitat for Humanity Philadelphia (H4H), to implement major structural repairs for homes in order to reduce the presence of in-home asthma allergens.
Box 1. Patient Vignette.
Sarah, a single mom and homeowner living in West Philadelphia balances work, parenting, and homeownership, all in addition to managing the health of a child with a chronic disease—asthma. In the year prior to enrollment in the Community Asthma Prevention Program (CAPP) home visiting program, her four-year-old daughter visited urgent care once and the emergency room three times, all for severe asthma exacerbations. As part of CAPP, she received in-home asthma education from her daughter’s home visitor, along with trigger-mitigating supplies including mattress/pillow covers, asthma-friendly cleaning materials, roach bait and mouse traps, and a new spacer and mask. Still she had structural issues that the home visitor could not address. Fortunately, since she is a homeowner, she was eligible for the Children’s Hospital of Philadelphia’s CAPP+ Home Repairs program, where substantial structural home repairs were completed to further reduce asthma triggers caused by mold/mildew, pests, and dust. Sarah was thrilled by the opportunity to make an even bigger impact on her child’s health by having long-overdue repairs completed in her home: “As a homeowner in West Philadelphia, repairs on a home are very, very hard, especially being a single mother.”
Despite several months of delays due to the pandemic, since construction’s completion, her daughter’s asthma has remained under control and exacerbation-free, not requiring a single emergency room visit or hospitalization. Repairs to Sarah’s home included a new roof, an exhaust fan over the cooktop to remove nitrous oxide, new vinyl-plank flooring replacing wall-to-wall carpeting in several rooms including her daughter’s bedroom, and a bathroom fan, clothes dryer vent to outside, and dehumidifier to reduce moisture throughout the house. Sarah is extremely grateful that her daughter’s health has so significantly benefited from both the asthma education and the home repairs — “I’m just really excited and really happy about my repairs and am so, so happy about my new house now.”
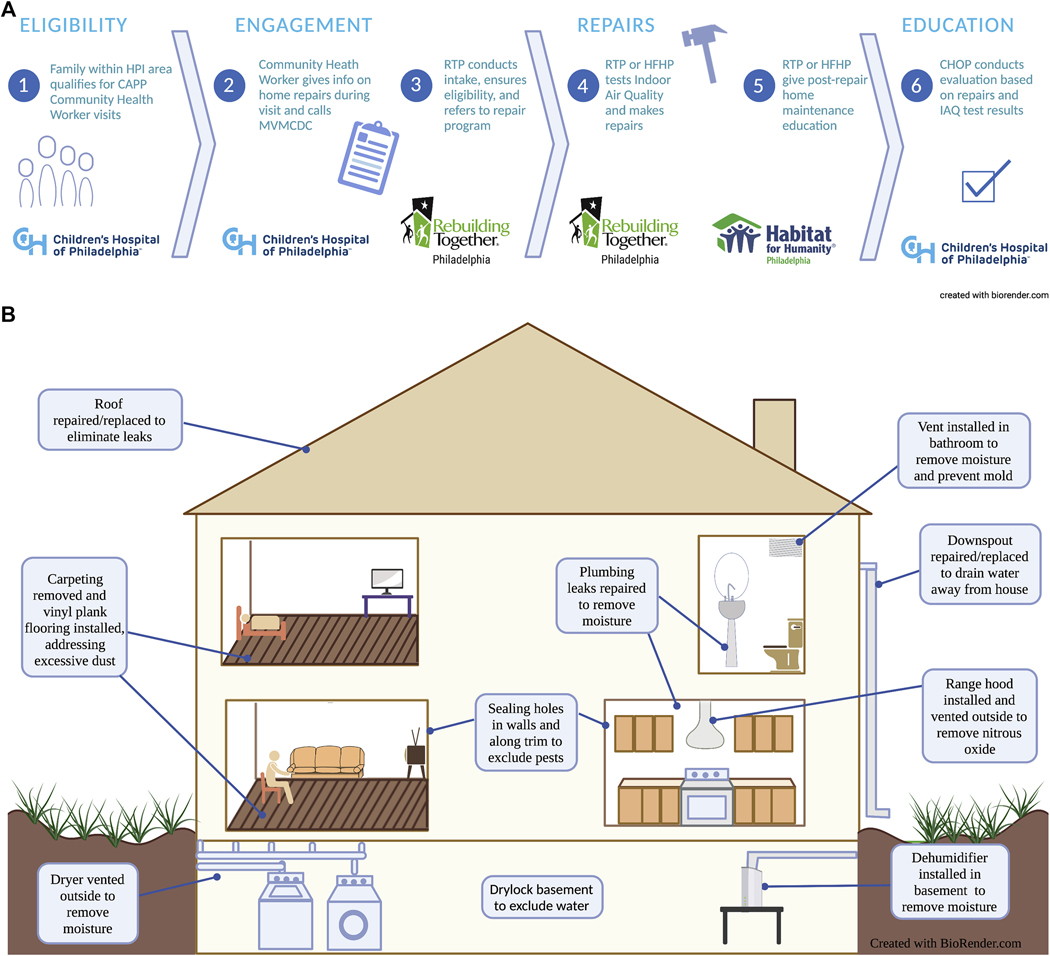
Families meeting the eligibility requirements of being a homeowner living in West Philadelphia and child enrolled in CAPP (eligible if child has 1 asthma-related hospital visit or 2 emergency visits in past year) were offered CAPP+ home repairs by RTP or H4H. Once identified, the housing repair agency conducted the initial inspection, created a work scope, reviewed that work scope with the homeowner and assigned contractors to the job. Figure 1 illustrates how all partners were connected in implementing home repairs for children with asthma (Figure 1). The repairs focused on dust, mold, and pests (Figure 2) and outcomes were number of repairs completed and number of repairs needed, reduction in number of triggers, and reduction in asthma symptoms and healthcare utilization.
Figure 1.
Collaboration of partner organizations to support a home repair program for children with asthma
Figure 2.
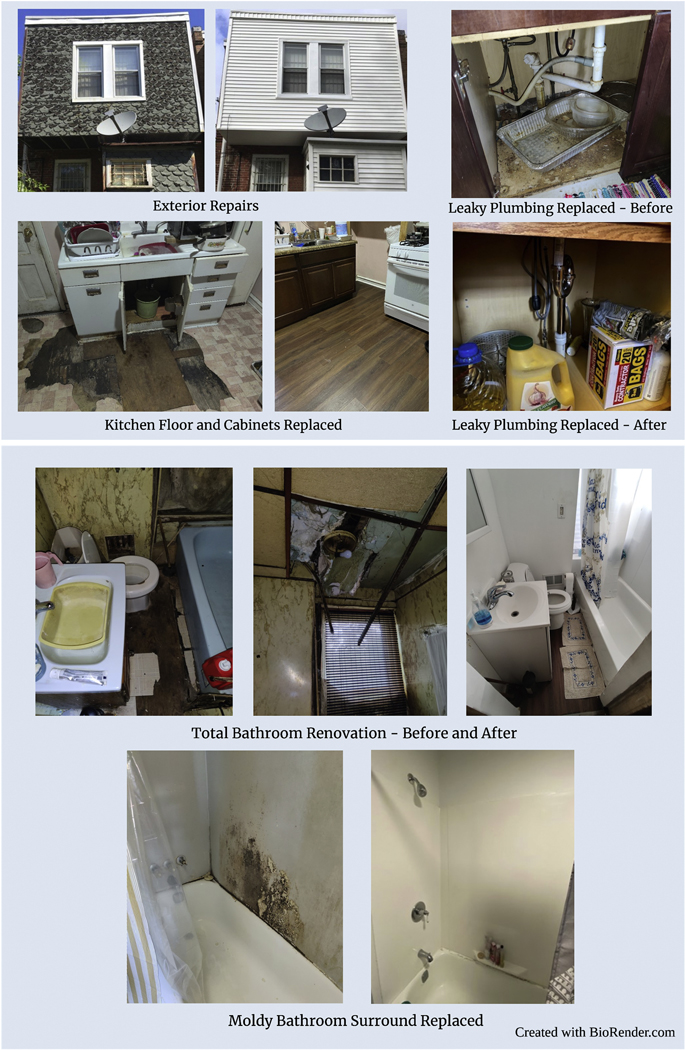
Image of structural repairs done in homes
Demographics and living conditions
We enrolled 30 homeowners with the first cohort. Homeowners were primarily African American living with children who were between 2– 17 years of age (table I). According to CHWs observation at the initial home visit, only 25% of the child’s bedrooms were in good condition and less than 20% of the general living conditions were rated as good.
Table I -.
Characteristics of the children and households at time of enrollment in CAPP
| Child characteristics | N | % |
|---|---|---|
| Age | ||
| 1–4 | 8 | 27% |
| 5–9 | 14 | 46% |
| 10–17 | 8 | 27% |
| Race | ||
| Black | 27 | 90% |
| Sex | ||
| Male | 15 | 50% |
| Female | 15 | 50% |
| ED visit for asthma in the past 12 months (%) | - | 90% |
| Hospitalization for asthma in the last 12 months (%) | - | 86% |
| Household characteristics* | N | % |
| General condition of child’s bedroom | ||
| Poor | 4 | 14% |
| Fair | 17 | 61% |
| Good | 7 | 25% |
| General assessment of home’s condition | ||
| Poor | 8 | 26% |
| Fair | 17 | 57% |
| Good | 5 | 17% |
Household characteristics were assessed by CAPP community health workers at the time of enrollment in the program
Home Repairs for Asthma Triggers
Most repairs identified at baseline were targeted to reduce pests, moisture and dust (Table II). Repairs made to eliminate pests were primarily exclusionary in focus. For mold, repairs were made to eliminate sources of water intrusion and provide adequate ventilation.— For dust, removing sources of dust in living area and child’s bedroomwere the most common repairs (Figure 1, 2). Parents reported a reduction in cockroaches, mice and evidence of mold (Table III) at the 12– 18 month post-repair survey.
TABLE II.
Need for and completion of asthma-related structural repairs in the homes of children with asthma
| Homes eligible for repair at initial walkthrough | Homes with repairs completed at final walkthrough | |||
|---|---|---|---|---|
|
|
|
|||
| Structural home repairs | No. | Percentage of all homes | No. | Percentage of eligible homes that received the repair |
|
| ||||
| Pest-related repairs | ||||
| Seal all accessible plumbing penetrations to exclude mice | 22 | 81% | 19 | 86% |
| Eliminate pests during demonstratoin: vacuum cockroaches, clean rodent sebum (rub marks), etc, cockroach frass (feces), and grease buildup, etc | 19 | 70% | 18 | 95% |
| Fill rodent holes with copper mesh and finish with spackle or patching cement | 17 | 63% | 15 | 88% |
| Repair subfloor and seal along walls to exclude rodents. Ensure that there are no gaps behind cabinets, etc | 14 | 52% | 12 | 86% |
| Seal cabinets to walls, floor, etc, with silicone caulk to deny pest access. Apply boric acid dust (cockroach prevention) into voids before sealing | 14 | 52% | 11 | 79% |
| Seal gaps and open joints in accessible HVAC ducts to reduce pest entry | 13 | 48% | 10 | 77% |
| Install wall or base cabinets in kitchen when they are badly damaged or missing, leading to insufficient storage for food | 9 | 33% | 7 | 78% |
| Mold-related repairs | ||||
| Ensure that the roof and building shell are watertight and properly shed water away from the home | 23 | 85% | 23 | 100% |
| Repair plumbing leaks in sinks, showers/tubs, toilets, supply lines, and/or drain lines | 19 | 70% | 18 | 95% |
| Correct improperly vented exhaust fan to exhaust outside | 11 | 41% | 10 | 91% |
| Install dehumidifier if humidity in the home is higher than 60% and homeowner understands the maintenance requirements and electricity costs | 9 | 33% | 7 | 78% |
| Dust-related repairs | ||||
| Paint with low–volatile organic compouind paint areas of the home where interior paint covering is chipped or peeling | 16 | 59% | 11 | 69% |
| Remove carpeting in living areas such as living rooms, dining rooms, and hallways and install smooth, cleanable flooring | 13 | 48% | 13 | 100% |
| Vacuum and clean grates and termination points in duct systems | 12 | 44% | 10 | 83% |
| Remove carpeting in the bedroom of the person with asthma and install smooth, cleanable flooring | 11 | 41% | 11 | 100% |
| Replace air filters on the heating/cooling system; install filter seals if the slot for the furnace filter allows air to bypass the filter | 10 | 37% | 8 | 80% |
HVAC, Heating, ventilation, and air conditioning.
Homes were assessed for structural deficiencies at the time of enrollment in the home repair program and then again at the final walkthrough to ascertain whether each repair had been completed.
Table III.
Parental report of in-home asthma triggers pre and post repair*
| Environmental asthma trigger | Pre-Repair | Post-Repair | p-value** |
|---|---|---|---|
| Cockroaches | 43% | 13% | <0.01 |
| Rodents | 57% | 26% | <0.01 |
| Evidence of mold | 53% | 43% | 0.41 |
Prior to repair, the presence of environmental triggers was indicated if either the parent of the community health worker reported evidence of the trigger. Following repairs, all triggers were assessed by parental self-report.
McNemar’s Test was used to examine changes in the number of households with each outcome between the pre- and post-repair periods
Asthma Symptoms and Health care utilization (Table IIIa–b)
Self-reported symptoms were used as a proxy for asthma control. The 12-month post repair questionnaire reveals a nearly 50% reduction in nighttime symptoms, 40% reduction in rescue medication use and a 60% reduction in missed school days, all of which indicate improved asthma control. Approximately 90% had an inpatient and/or emergency visit in the year prior to enrolling in CAPP home visits. At 12 months, emergency and hospital room visits decreased by approximately 90%.
Homeowner Feedback
In general, homeowners were grateful for the repairs offered (see Box 2), although some were disappointed that other major home repairs (not asthma-trigger related) could not be completed due to budget restraints
Box 2. Qualitative feedback from homeowners.
“Everything is really goad. They just completed the basement steps. One person has to come out and change address sign on the front. A lot of back and forth towards the end. But everybody was friendly, in and out, kept areas clean. Other than that, totally happy with the bathroom. Likes to just sit in the bathroom. I thank you for referring to the program, can focus on other little things. (She can focus on smaller repairs since the biggest repairs were taken care of). We love Courtney (CHW). ”
“ No more wheezing now. Everything is feeling good. Every month I’d go to the hospital. But now, everything is perfect. No more. They are taking their medications. They are doing good. Not like before. They helped me a lot for my kids.”
“A lot of things on the list they did not get to because of the cost of other repairs. My expectations were high and I was excited for things to get done but my home is a fixer upper. I am greatly appreciative, but I wish the homeowner had a say in what repairs were prioritized.”
“Some contractors did not seem to be on the same page. The gentleman who did the work seemed to have a different vision than the project manager and some things did not get done that the contractor said because the project manager did not agree.”
“ Best advice I would give is to be paitent with the process and definitely use your voice even though ultimately the decision is not yours on what repairs are completed. I think this is a great opportunity. Thank you”
“I felt like my brothers and my father were working in my house. Let me tell you, everybody you sent to my house was so respectable, so down to earth, friendly and did nothing but their job. To the point that I trust them, To the point where I could walk out my house and leave them.”
Pilot program summary
This pilot feasibility study combined an evidence-based CHW-led intervention with major structural housing repairs. We demonstrated the feasibility of health care organizations partnering with home repair agencies, with a signal for improved asthma control. Lessons learned include setting expectations for homeowners at the beginning of the repair process; when possible, allowing homeowners to prioritize which repairs are made; and the importance of having the CHW serve as the liaison between the homeowner and the contractor. Although we showed a decrease in symptoms and healthcare utilization, this was a pilot feasibility study in which follow-up data was collected during the COVID-19 pandemic. Early evidence shows that hospitalizations and ED visits for asthma decreased for all children with asthma during the pandemic, so future evaluations including a control group will be necessary to expand on our findings.48
This demonstration of feasibility and signal for improved outcomes prompted an expansion of this program (CAPP Plus) funded by the Children’s Hospital of Philadelphia, which is now approaching 100 completed homes. Our hope is to serve as a model for other health care organizations to leverage expertise across different sectors to improve children’s lives.
Discussion/Future Directions
While we highlight the results of several interventions with at least a signal of effectiveness, there is currently a paucity of rigorous research or evaluation of programs that complete targeted or major structural repairs to improve asthma morbidity. As stated earlier, this is likely due to the large financial investment necessary to complete such repairs at the scale necessary to show impacts on health outcomes. Other barriers beyond cost include the cross-sector collaboration and time-intensiveness of intervention planning and repairs, both of which require committed stakeholders, relationship-building, and a shared vision of the goals. Given these barriers, a common critique of this intensive and expensive approach is the concern about return on investment, especially if funding for such interventions comes solely from the health sector. This critique may be appropriate if the only goal is improving narrow asthma-specific metrics such as symptom control or ED visits. But if the goal is to decrease or eliminate broader health disparities by investing time and effort to address their fundamental causes, such as inhumane housing conditions and wealth inequality from centuries of policies imbued with varying degrees of structural racist practices such as redlining and exclusion, perhaps the return on investment critique is shortsighted, both in time horizon and its underlying motivation. If we are to achieve health equity, we first must correct the wrongs of disinvestment in these communities by achieving adequate housing for all children, especially children who suffer from asthma.
Table IVa –
Parental report of asthma symptoms pre- and post-home repairs*
| Asthma Symptoms | Pre-Repairs | Post-Repairs | ||
|---|---|---|---|---|
| Mean | % reporting any | Mean | % reporting any | |
| During the last four weeks, how many days did [child’s name] have any daytime asthma symptoms (like wheezing, shortness of breath, tightness in the chest, or cough)? | 1.9 | 70% | 1.2 | 61% |
| During the last four weeks, how many nights did [child’s name] wake up during the night because of asthma? | 1.9 | 43% | 0.5 | 22% |
| During the past 14 days, how many days did [ child’s name] use [his/her] quick-relief or rescue medicine (by pump or machine) to help stop asthma symptoms like wheezing, shortness of breath, tightness in the chest, or cough? | 1.7 | 62% | 0.8 | 39% |
| In the last four weeks, on how many days did [child’s name] have to slow down or stop [his/her] play or activities because of asthma symptoms: shortness of breath, wheezing, tightness in chest, or cough? | 1.7 | 60% | 1.2 | 39% |
| There are many reasons children sometimes stay home from school. During the past twelve (12) months, how many days did [child’s name] miss school due to asthma? | 4.6 | 71% | 0.8 | 30% |
| In the past 12 months, on how many days did you [or other caregivers] have to miss work to care for [child’s name]’s asthma? | 4.3 | 46% | 0.4 | 17% |
Asthma symptoms were assessed by parental self-report at time of enrollment in CAPP, as well as at 12 months following completion of home repair
Table IVb.
Parental report of healthcare utilization pre- and post-repairs*
| Healthcare utilization | Pre-Repairs | Post-Repairs | ||
|---|---|---|---|---|
| In the past twelve (12) months, how many times has [child’s name] made unscheduled visits to the doctor’s office or clinic for urgent asthma care? | 1.3 | 57% | 0.5 | 22% |
| In the past twelve (12) months, how many times has [child’s name] been treated in Emergency Department or ER for asthma? | 1.3 | 90% | 0.2 | 17% |
| In the past twelve (12) months, how many times has [child’s name] had to stay overnight for one or more nights in a hospital for asthma? | 1.0 | 86% | 0.1 | 4% |
Asthma morbidity was assessed by parental self-report at time of enrollment in CAPP, as well as at 12 months following completion of home repairs.
Acknowledgements-
The authors would like to acknowledge the homeowners and their children; Rebuilding Together Philadelphia-Brandon Alcorn, Stefanie Seldin and Habitat for Humanity Philadelphia-Emily Lucas, Carrie Rathmann; CAPP community health workers-Catherine Brown, Charmane Braxton, Carmen Perez, and Jasmine Dean; the Home Preservation Initiative partners and Carina Flaherty.
Sources of funding
This work was supported by the BUILD Health Challenge 2.0, Children’s Hospital of Philadelphia (CHOP) matching funds, CHOP PolicyLab and National Institutes of Health (grant no. K23HL136842 to C.C.K.)
Tyra C Bryant-Stephens-receives funding from the National Institutes of Health (Grant No. U01HL138687) and Pennsylvania Department of Health (Grant No. 9239140621)
Chen Kenyon-receives funding from National Institutes of Health (grant no. K23HL136842)
List of abbreviations
- CHOP
Children’s Hospital of Philadelphia
- BUILD
Build Health Challenge Grant
- CAPP
Community Asthma Prevention Program
- CHW
Community Health Worker
- ED
Emergency Department
- CDC
Centers for Disease Control and Prevention
- HUD
U.S. Department of Housing and Urban Development
- RTP
Rebuilding Together Philadelphia
- H4H
Habitat for Humanity Philadelphia
- HVAC
Heating, ventilation and air conditioning
Footnotes
Declaration-
The authors have no financial relationship with a biotechnology and/or pharmaceutical manufacturer that has an interest in the subject matter or materials discussed in the submitted manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tyra C Bryant-Stephens, Children’s Hospital of Philadelphia, University of Pennsylvania, Perelman School of Medicine.
Douglas Strane, Children’s Hospital of Philadelphia.
Elizabeth K. Robinson, Children’s Hospital of Philadelphia.
Sanya Bhambhani, Children’s Hospital of Philadelphia.
Chén C. Kenyon, Children’s Hospital of Philadelphia, University of Pennsylvania Perelman School of Medicine.
References
- 1.Most Recent National Asthma Data [Internet]. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2021. [cited 2021Jun29]. Available from: https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm [Google Scholar]
- 2.Akinbami L, Moorman J, Simon A, Schoendorf K. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. J Allergy Clin Immunol. 2014;134(3):547–553.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz J, Gold D, Dockery DW, Weiss ST, Speizer FE. Predictors of asthma and persistent wheeze in a national sample of children in the United States: association with social class, perinatal events, and race. Am Rev Respir Dis. 1990; 142 (1):555–62. [DOI] [PubMed] [Google Scholar]
- 4.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005; 26:89–113. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R. The widening Black/White gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117(1)351–8. [DOI] [PubMed] [Google Scholar]
- 6.McGovern L, Miller G, Hughes-Cromwick P. The Relative Contribution of Multiple Determinants to Health Outcomes. Bethesda MD: Health Affairs Health Policy Brief; 2014. Aug 21. 9 p. DOI: 10.1377/hpb20140821.404487 [DOI] [Google Scholar]
- 7.Institute of Medicine. Clearing the air: asthma and indoor exposures. Washington (DC): Institute of Medicine; 2000; p.105–221. [Google Scholar]
- 8.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann N Y Acad Sci. 2008;1136:276–288 [DOI] [PubMed] [Google Scholar]
- 9.Massey D, Denton N. American Apartheid. Cambridge: Harvard University Press; 1993 [Google Scholar]
- 10.Rothstein R. The color of law: A forgotten history of how our government segregated America. Liveright Publishing; 2017. May 2. [Google Scholar]
- 11.Swope CB, Hernández D. Housing as a determinant of health equity: A conceptual model. Soc Sci Med. 2019;243:112571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woods L, Shaw-Ridley M, & Woods C. Can Health Equity Coexist With Housing Inequalities? A Contemporary Issue in Historical Context. Health Promot Pract. Jul 2014;15(4), 476–482. [DOI] [PubMed] [Google Scholar]
- 13.Hirt S. The rules of residential segregation: US housing taxonomies and their precedents. PP. 2015. Mar; 30(3):367–395. [Google Scholar]
- 14.Desmond M. Heavy is the house: rent burden among the American urban poor. Int. J. Urban Reg. 2018. Jan 18; Res., 42: 160–170. https://doi-org.proxy.library.upenn.edu/10.1111/1468-2427.12529 [Google Scholar]
- 15.Carr JH, Kutty NK. Segregation: The Rising Costs for America. New York: Routledge; 2008. 372 p. [Google Scholar]
- 16.Rodems R, Shaefer HL. Many of the kids are not alright: Material hardship among children in the United States. Children and Youth Serv Rev. 2020. May;112:7. [Google Scholar]
- 17.Blake KS, Kellerson RL, Simic A. Measuring overcrowding in housing [Internet] Washington (DC): US Department of Housing and Urban Development, Office of Policy Development and Research; Sept 2007. 38p. Available from: https://www.huduser.gov/publications/pdf/Measuring_Overcrowding_in_Hsg.pdf [Google Scholar]
- 18.Institute of Medicine, Committee on the Assessment of Asthma and Indoor Air. Indoor biological exposures: cockroach. In: Clearing the Air: Asthma and Indoor Air Exposures. Washington, DC: National Academy Press; 2000. DOI: 10.17226/9610 [DOI] [Google Scholar]
- 19.Burrows B, Martinez FD, Halonen M, Barbee RA, Cline MG. Association of asthma with serum IgE levels and skin-test reactivity to allergens. N Engl J Med. 1989; 320:271–277. [DOI] [PubMed] [Google Scholar]
- 20.Poowuttikul P, Saini S, Seth D. Inner-city asthma in children. Clin Rev Allergy Immunol. 2019. Apr;56(2):248–268. DOI: 10.1007/s12016-019-08728-x [DOI] [PubMed] [Google Scholar]
- 21.Matsui EC. Environmental exposures and asthma morbidity in children living in urban neighborhoods. Allergy. 2014. May;69(5):553–8. doi: 10.1111/all.12361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997. May 8;336(19):1356–63. DOI: 10.1056/NEJM199705083361904 [DOI] [PubMed] [Google Scholar]
- 23.Reponen T, Lockey J, Bernstein DI, Vesper SJ, Levin L, Khurana Hershey GK, et al. Infant origins of childhood asthma associated with specific molds. J Allergy Clin Immunol. 2012. Sep;130(3):639–644.e5. DOI: 10.1016/j.jaci.2012.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Visness CM, Calatroni A, Gergen PJ, Mitchell HE, Sampson HA. Effect of environmental allergen sensitization on asthma morbidity in inner-city asthmatic children. Clin Exp Allergy. 2009. Sep;39(9):1381–9. DOI: 10.1111/j.1365- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matsui EC, Eggleston PA, Buckley TJ, Krishnan JA, Breysse PN, Rand CS, Diette GB. Household mouse allergen exposure and asthma morbidity in inner-city preschool children. Ann Allergy Asthma Immunol. 2006. Oct;97(4):514–20. DOI 10.1016/S1081-1206(10)60943-X. [DOI] [PubMed] [Google Scholar]
- 26.Matsui EC, Perzanowski M, Peng RD, Wise RA, Balcer-Whaley S, Newman M, Cunningham A, Divjan A, Bollinger ME, Zhai S, Chew G, Miller RL, Phipatanakul W. Effect of an Integrated Pest Management Intervention on Asthma Symptoms Among Mouse-Sensitized Children and Adolescents with Asthma: A Randomized Clinical Trial. JAMA. 2017. Mar 14;317(10):1027–1036. doi: 10.1001/jama.2016.21048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perzanowski MS, Chew GL, Divjan A, Jung KH, Ridder R, Tang D, et al. Early-life cockroach allergen and polycyclic aromatic hydrocarbon exposures predict cockroach sensitization among inner-city children. J Allergy Clin Immunol. 2013. 131(3):886–893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson JM, Platts-Mills TAE. Home Environmental Interventions for House Dust Mite. J Allergy Clin Immunol Pract. 2018. Jan-Feb;6(1):1–7. DOI: 10.1016/j.jaip.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R 3rd, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004. Sep 9;351(11):1068–80. doi: 10.1056/NEJMoa032097 [DOI] [PubMed] [Google Scholar]
- 30.Wilson J, Dixon SL, Breysse P, Jacobs D, Adamkiewicz G, Chew GL, et al. Housing and allergens: A pooled analysis of nine US studies. Environmental Research. 2010;110(2):189–98. [DOI] [PubMed] [Google Scholar]
- 31.Elliott L, Arbes SJ, Harvey ES, Lee RC, Salo PM, Cohn RD, London SJ, Zeldin DC. Dust weight and asthma prevalence in the National Survey of Lead and Allergens in Housing (NSLAH). Environ Health Perspect. 2007. Feb;115(2):215–20. DOI: 10.1289/ehp.9412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grineski SE, Hernández AA. Landlords, fear, and children’s respiratory health: an untold story of environmental injustice in the central city. Local Environ. 2010. Mar 21; 15(3): 199–216 [Google Scholar]
- 33.Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD Determinants of allergen concentrations in apartments of asthmatic children living in public housing. J Urban Health. 2007. Mar; 84(2):185–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. J Urban Health. 2010. Mar;87(2):211–24. DOI: 10.1007/s11524-009-9404-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crocker DD, Kinyota S, Dumitru GG, Ligon CB, Herman EJ, Ferdinands JM, et al. ; Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011. Aug;41(2 Suppl 1):S5–32. doi: 10.1016/j.amepre.2011.05.012 [DOI] [PubMed] [Google Scholar]
- 36.Cloutier MM, Baptist AP, Blake KV, Brooks EG, Bryant-Stephens T, DiMango, et al. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 2020. Dec;146(6):1217–1270. DOI: 10.1016/j.jaci.2020.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Phipatanakul W, Cronin B, Wood RA, Eggleston PA, Shih MC, Song L et al. Effect environmental intervention on mouse allergen levels in homes of inner-city Boston children with asthma. Annals of Allergy, Asthma and Immunology. 2004. Apr;92(4):420–425. 10.1016/S1081-1206(10)61777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leas BF, D’Anci KE, Apter AJ, Bryant-Stephens T, Lynch MP, Kaczmarek JL, Umscheid CA. Effectiveness of indoor allergen reduction in asthma management: A systematic review. J Allergy Clin Immunol. 2018. May;141(5):1854–1869. doi: 10.1016/j.jaci.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 39.Nurmagambetov TA, Barnett SB, Verughese J, Chattopadhyay SK, Hopkins DP, Crocker DD, et al. Economic value of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review, Am J Prev Med. 2011; 41(2):S33–S47. 10.1016/j.amepre.2011.05.011 [DOI] [PubMed] [Google Scholar]
- 40.Turcotte DA, Alker H, Chaves E, Gore R, Woskie S. Healthy homes: in-home environmental asthma intervention in a diverse urban community. Am J Public Health. 2014;104(4):665–671. DOI: 10.2105/AJPH.2013.301695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Somerville M, Mackenzie I, Owen P, Miles D. Housing and health: does installing heating in their homes improve the health of children with asthma? Public Health. 2000. Nov;114(6):434–9. [DOI] [PubMed] [Google Scholar]
- 42.Howden-Chapman P, Matheson A, Crane J, Viggers H, Cunningham M, Blakely T, Cunningham C, et al. Effect of insulating existing houses on health inequality: cluster randomized study in the community. BMJ. 2007. Mar 3; 334(7591):460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Howden-Chapman P, Pierse N, Nicholls S, Gillespie-Bennett J, Viggers H, Cunningham M, et al. BMJ. 2008. Sep 23; 337(7674):a1411. doi: 10.1136/bmj.a1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woodfine L, Neal RD, Bruce N, Edwards RT, Linck P, Mullock L, et al. Enhancing ventilation in homes of children with asthma: pragmatic randomised controlled trial. Br J Gen Pract. 2011. Nov;61(592):724–32. doi: 10.3399/bjgp11X606636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kercsmar CM, Dearborn DG, Schluchter M, et al. Reduction in asthma morbidity in children as a result of home remediation aimed at moisture sources. Environ Health Perspect. 2006;114(10):1574–1580. doi: 10.1289/ehp.87427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takaro TK, Krieger J, Song L, Sharify D, Beaudet N. The Breathe-Easy Home: the impact of asthma-friendly home construction on clinical outcomes and trigger exposure. Am J Public Health. 2011;101(1):55–62. doi: 10.2105/AJPH.2010.300008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gruber KJ, McKee-Huger B, Richard A, Byerly B, Raczkowski JL, Wall TC. Removing asthma triggers and improving children’s health: The Asthma Partnership Demonstration project. Ann Allergy Asthma Immunol. 2016. May;116(5):408–14. doi: 10.1016/j.anai.2016.03.025 [DOI] [PubMed] [Google Scholar]
- 48.Ulrich L, Macias C, George A, Bai S, Allen E. Unexpected decline in pediatric asthma morbidity during the coronavirus pandemic. Pediatr Pulmonol. 2021. Jul;56(7):1951–1956. doi: 10.1002/ppul.25406 [DOI] [PMC free article] [PubMed] [Google Scholar]