Abstract
Primary cardiac tumors are rare, as the most common cause of cardiac masses is from metastatic disease. In this article, a unique case of isolated cardiac Burkitt lymphoma causing right-sided heart failure in a 70-year-old man who presented to the emergency department with abdominal distension and lower-extremity swelling is described. The right ventricular mass was initially identified via computed tomographic scans of the abdomen and pelvis. Further workup included transthoracic echocardiogram and cardiac magnetic resonance imaging that showed extension of the mass into the right atrium and pericardium. Staging imaging and bone marrow biopsy revealed no evidence of metastatic disease. Cytology of the peritoneal fluid and biopsy of the right ventricular mass confirmed Burkitt lymphoma. The cardiac mass substantially decreased in size and the right-sided heart failure resolved after the initiation of chemotherapy, which highlights the importance of prompt diagnosis and treatment of Burkitt lymphoma.
Keywords: Cardiac tumor, Burkitt lymphoma, neoplasms, heart failure, multimodality imaging, echocardiography, computed tomography, magnetic resonance imaging
The differential diagnoses for a patient presenting with volume overload are broad and include congestive heart failure, the most common of which is left-sided heart failure.1 We report an unusual case of right-sided heart failure caused by an obstructing mass invading the right ventricle and pericardium that was found to be a primary cardiac Burkitt lymphoma. Cardiac malignancies are uncommon; however, primary cardiac tumors represent only a small fraction of these cases and are typically benign.2 Treatment for malignant cardiac tumors is individualized to each patient but generally involves chemotherapy and resection when appropriate.3 This case suggests that Burkitt lymphoma and other cardiac malignancies should be included in the differential for right-sided heart failure and that early chemotherapy can provide rapid symptom relief.
Case Report
A 70-year-old man presented to the emergency department with a subacute history of abdominal distention, generalized fatigue, and lower-extremity swelling. He reported a recent history of constipation, discomfort with eating, and an unintentional 20-pound weight loss. He denied experiencing fevers, chills, chest pain, orthopnea, shortness of breath, nausea, or vomiting. On examination, he was afebrile, with a heart rate of 85 beats/min, a blood pressure of 125/65 mm Hg, respirations at 22/min, and an oxygen saturation of 99% on room air. He had no jugular vein distention (JVD). Cardiac examination revealed a regular rate without murmurs or rubs. His breath sounds were clear, and his abdomen was noted to be distended with a fluid wave but without organomegaly. There was bilateral lower-extremity pitting edema. He had no palpable lymphadenopathy. Skin examination showed no signs of jaundice, spider angiomatas, or telangiectasias. The patient was alert and oriented and displayed no asterixis.
The patient had a medical history of hypertension, hyperlipidemia, iron-deficiency anemia, well-controlled type 2 diabetes mellitus, and alcohol use disorder. He had never smoked and had no family history of cancer.
His clinical presentation before investigation was concerning for right-sided heart failure, decompensated cirrhosis, or nephrotic syndrome. The differential diagnoses for right-sided heart failure include left-sided heart failure, primary and secondary pulmonary hypertension, and severe tricuspid valve disease. Given his history of alcohol use disorder, new decompensated cirrhosis with portal hypertension was also considered. Nephrotic syndrome was also considered owing to the history of diabetes mellitus and generalized edema.
Initial laboratory values were notable for the following: white blood cells, 5,700/μL; hemoglobin, 11.9 g/dL; platelets, 393,000/μL; creatinine, 1.4 mg/dL (baseline 1.0 mg/dL from 1 year prior); troponin I, 0.05 ng/mL; and brain-type natriuretic peptide, 172 pg/mL. Liver function test results were within normal limits. Human immunodeficiency virus test results were negative. Electrocardiogram showed sinus rhythm with moderate T-wave inversions in the anterior leads.
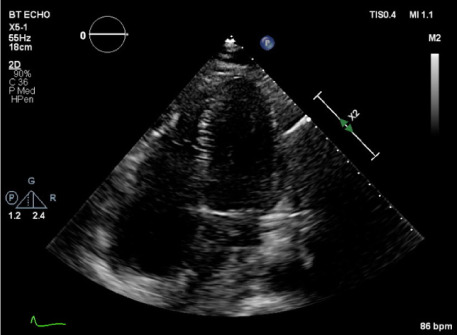
Computed tomography (CT) of the abdomen and pelvis with contrast revealed a multinodular mass along the anterior pericardium with extension to the right atrial and ventricular cavities, as well as generalized ascites (Fig. 1). Transthoracic echocardiogram (TTE) demonstrated a 2.5- × 1.8-cm fixed, hypodense mass attached at the base of the right ventricle (RV), which also had a filling effect in the pericardial space (Fig. 2). Chest CT with contrast revealed a large, homogenous soft tissue mass in the right atrial free wall that extended into the RV and was contiguous with multinodular thickening along the anterior pericardium. Subcarinal adenopathy was also identified. Cardiac magnetic resonance (CMR) imaging showed an ill-defined nodular infiltrative RV mass with extension into the right atrium and pericardium with a small complex pericardial effusion (Fig. 3). The RV ejection fraction on CMR was mildly reduced, at 45%.
Fig. 1.
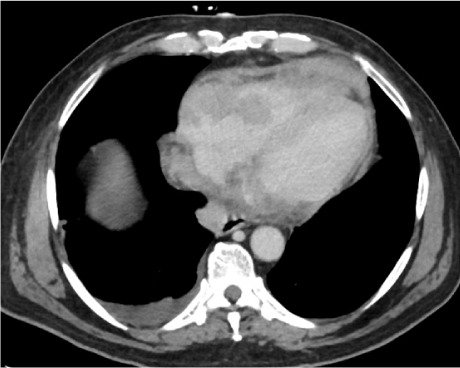
Computed tomography of abdomen and pelvis. A multinodular mass is seen along the anterior pericardium with extension into the right atrial and ventricular cavities.
Fig. 2.
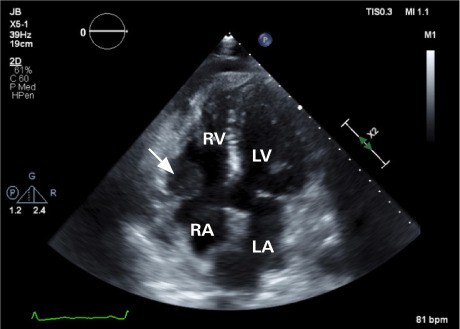
Transthoracic echocardiogram before chemotherapy. A 2.5- × 1.8-cm fixed, hypodense mass (arrow) is attached at the base of the right ventricle.
LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Supplemental motion image is available for Figure 2.
Fig. 3.
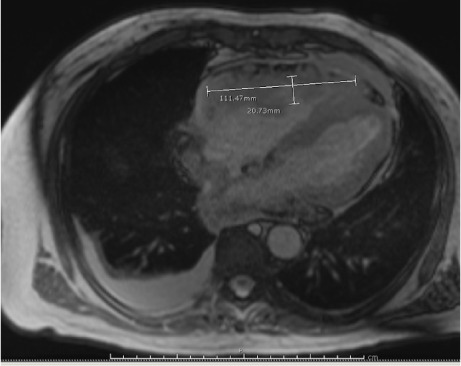
Cardiac magnetic resonance. An ill-defined nodular infiltrative right ventricular mass extends into the right atrium and pericardium associated with a small complex pericardial effusion.
The imaging findings of a multinodular mass were most concerning for malignancy. Because primary cardiac tumors are exceedingly uncommon, the mass was initially suspicious for metastatic spread of a malignancy of unknown primary origin.
The patient underwent transluminal biopsy of the RV mass via right internal jugular vein access using a 5.5F bioptome catheter under echocardiography and fluoroscopic guidance. Five samples were taken and sent to pathology. He also underwent paracentesis of the peritoneal fluid. Both the RV mass and ascites fluid showed a high-grade B-cell lymphoma that was positive for CD10 and CD20, negative for BCL2, and equivocal for BCL6 (Fig. 4). Fluorescence in situ hybridization analysis of the peritoneal fluid noted MYC/8q rearrangement, consistent with a diagnosis of Burkitt lymphoma. Bone marrow biopsy revealed no marrow involvement, and additional investigation did not show other evidence of disease, which is consistent with isolated primary cardiac Burkitt lymphoma.
Fig. 4.
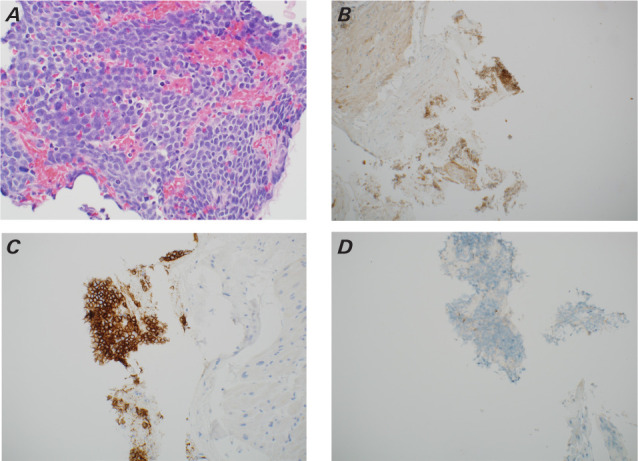
Pathologic samples of the right ventricular mass. A) Hematoxylin and eosin stain show monomorphic lymphocytes with apoptotic bodies that form a “starry sky” appearance that was B) CD10 +, C) CD20 +, D) BCL-2 negative, and E) BCL-6 equivocal. Panel A is at ×40 magnification, and panels B through E are at ×20 magnification. These findings are consistent with Burkitt lymphoma.
Fig. 4.
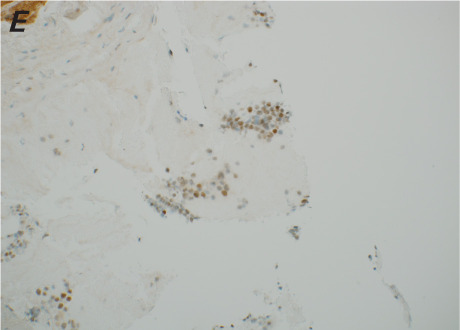
Pathologic samples of the right ventricular mass. A) Hematoxylin and eosin stain show monomorphic lymphocytes with apoptotic bodies that form a “starry sky” appearance that was B) CD10 +, C) CD20 +, D) BCL-2 negative, and E) BCL-6 equivocal. Panel A is at ×40 magnification, and panels B through E are at ×20 magnification. These findings are consistent with Burkitt lymphoma.
The patient had a complicated and protracted hospital course. Over the first few days, he developed profound JVD, worsening abdominal ascites, and scrotal swelling. Paracentesis revealed a serum ascites albumin gradient higher than 1.1, which is indicative of portal hypertension. Transthoracic echocardiogram at that time revealed an ejection fraction of 55% to 59% with a flattened interventricular septum in both systole and diastole, consistent with RV pressure and volume overload. Next, his urine output decreased and his creatinine level began to uptrend despite diuresis, ultimately peaking at 6.0 mg/dL from a baseline of 0.9 mg/dL. His acute renal failure was likely caused by uric acid nephropathy, with an elevated uric acid level of 20.5 mg/dL. He was evaluated by cardiothoracic surgery, and the mass was determined to be unresectable.
He was started on intravenous steroids when the biopsy results showed B-cell lymphoma, but before he could begin chemotherapy, he developed melena and hemodynamic instability with a hemoglobin nadir of 5.9 g/dL. He was intubated for airway protection and required continuous renal replacement therapy for oliguria for 3 days. Endoscopy revealed white plaques concerning for esophageal candidiasis, but no source of his gastrointestinal bleed was found.
Chemotherapy was initiated with vincristine, doxorubicin, dexamethasone, and rituximab while the patient was in the intensive care unit and produced encouraging results. He was extubated and came off dialysis. His JVD, ascites, and peripheral edema soon resolved. Repeat echocardiography 1 week after chemotherapy noted a substantial interval reduction in the size of the tumor, although the infiltration into the pericardial space was still present (Fig. 5).
Fig. 5.
Transthoracic echocardiogram 1 week after initiation of chemotherapy. The previous mass at the right atrial and right ventricular junction is no longer seen.
Supplemental motion image is available for Figure 5.
Despite receiving a dose-reduced cycle of chemotherapy owing to liver dysfunction, he developed pancytopenia that required multiple transfusions. When his counts recovered, he received an additional round of chemotherapy with intrathecal methotrexate and dose-reduced rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and hydroxydaunorubicin and was discharged home.
Following discharge, the patient was doing well and completed 2 additional cycles of dose-reduced rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and hydroxydaunorubicin and another cycle of intrathecal methotrexate without complication. Further imaging with CMR and positron emission tomography was planned to reassess the cardiac mass but unfortunately could not be completed because the patient was readmitted to the hospital with neutropenic fever and encephalopathy. He was found to have extended-spectrum β-lactamase Escherichia coli bacteremia as well as meningitis, and his condition rapidly worsened. After discussions with the patient's family regarding his wishes, he was transitioned to hospice and died several days later. There were 172 days from his initial presentation to his death.
Discussion
Cardiac involvement in cases of malignancy is uncommon and has a reported incidence of 0.02% based on 22 large autopsy series.4 Metastatic spread from distant tumors represents most cases. Primary cardiac tumors are even more rare, with approximately 75% of cases being benign and most often identified as myxomas.2 Various types of sarcomas and non-Hodgkin lymphomas comprise nearly all the primary malignant tumors of the heart, with lymphomas accounting for approximately 1% or 2% of cases. Diffuse large B-cell lymphomas make up more than half of reported cases of lymphoma.5 Interestingly and similar to our case, cardiac lymphomas appear to preferentially involve the pericardium and the right side of the heart.5,6 Like other types of lymphomas, primary cardiac lymphomas (PCLs) are more frequently found in patients with immunosuppression secondary to organ transplantation or HIV infection and should prompt suspicion for lymphoma when a cardiac mass is discovered.5,7 According to the largest systematic review of PCLs from 1949 to 2009, only 13 of 197 cases were found to be Burkitt lymphoma.6
The clinical presentation of PCL is varied, but the most common presenting symptoms are constitutional, such as fatigue, fevers, and weight loss. Symptoms of right-sided heart failure are often the first clue of cardiac involvement.8,9 The most common rhythm disturbances that accompany cardiac tumors are atrial fibrillation, ventricular tachycardia, and atrioventricular block, though these findings are nonspecific.5 Plain radiography is generally unrevealing beyond evidence of cardiomegaly, congestion, or pericardial effusion, whereas a multimodality imaging approach including TTE, CT, and CMR is the basis of investigation and diagnosis.3,10 Pathologic diagnosis can be obtained via endomyocardial biopsy, TTE-guided biopsy, percutaneous intracardiac biopsy, or pericardiocentesis and fluid analysis.10 Burkitt lymphoma is characterized by translocation between the C-MYC gene and IGH gene [t(8;14)] in 80% of cases, with translocation with light chain genes [t(2;8) or t(8;22)] making up the remainder.11
The mainstay PCL treatment is chemotherapy because surgical resection is often not possible owing to tumor infiltration into adjacent tissues.2 Therapies containing anthracyclines and anti-CD20 agents provide the foundation for most chemotherapy regimens.5,6 Overall prognosis appears poor, with a reported survival rate of 60% at 2 months.5 In a case series of 22 patients diagnosed with primary cardiac Burkitt lymphoma, there were no surviving patients at 3 years.5,6 Early chemotherapy is associated with better outcomes, yet the rare nature of the disease limits concrete conclusions.
Conclusion
Primary cardiac masses are exceedingly rare and should prompt further workup with multimodality imaging to evaluate for other primary malignancy-causing metastases to the heart. Most cases of Burkitt lymphoma that have cardiac involvement also have other organ involvement; however, our case was uniquely isolated to the heart. This case highlights the importance of prompt diagnosis and treatment of Burkitt lymphoma as patients can quickly deteriorate as a result of rapid tumor growth. Primary cardiac Burkitt lymphoma generally has a poor prognosis despite chemotherapy treatment.
Supplementary Material
Funding Statement
Funding/Support: None.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Konstam MA, Kiernan MS, Bernstein D et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation . 2018;137(20):578–622. doi: 10.1161/CIR.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 2.Hoffmeier A, Sindermann JR, Scheld HH, Martens S. Cardiac tumors--diagnosis and surgical treatment. Dtsch Arztebl Int . 2014;111(12):205–211. doi: 10.3238/arztebl.2014.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruce CJ. Cardiac tumours: diagnosis and management. Heart . 2011;97(2):151–160. doi: 10.1136/hrt.2009.186320. [DOI] [PubMed] [Google Scholar]
- 4.Reynen K. Frequency of primary tumors of the heart. Am J Cardiol . 1996;77(1):107. doi: 10.1016/s0002-9149(97)89149-7. [DOI] [PubMed] [Google Scholar]
- 5.Burazor I, Aviel-Ronen S, Imazio M et al. Primary malignancies of the heart and pericardium. Clin Cardiol . 2014;37(9):582–588. doi: 10.1002/clc.22295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petrich A, Cho SI, Billett H. Primary cardiac lymphoma. Cancer . 2011;117(3):581–589. doi: 10.1002/cncr.25444. [DOI] [PubMed] [Google Scholar]
- 7.Joshi M, Kumar S, Noshirwani A, Harky A. The current management of cardiac tumours: a comprehensive literature review. Braz J Cardiovasc Surg . 2020;35(5):770–780. doi: 10.21470/1678-9741-2019-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maleszewski JJ, Anavekar NS, Moynihan TJ, Klarich KW. Pathology, imaging, and treatment of cardiac tumours. Nat Rev Cardiol . 2017;14(9):536–549. doi: 10.1038/nrcardio.2017.47. [DOI] [PubMed] [Google Scholar]
- 9.Chan O, Igwe M, Breburda CS, Amar S. Burkitt lymphoma presenting as an intracardiac mass: case report and review of literature. Am J Case Rep . 2016;17:553–558. doi: 10.12659/AJCR.899022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Mahony D, Peikarz RL, Bandettini WP, Arai AE, Wilson WH, Bates SE. Cardiac involvement with lymphoma: a review of the literature. Clin Lymphoma Myeloma . 2008;8(4):249–252. doi: 10.3816/CLM.2008.n.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferry JA. Burkitt's lymphoma: clinicopathologic features and differential diagnosis. Oncologist . 2006;11(4):375–383. doi: 10.1634/theoncologist.11-4-375. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


