Abstract
Background:
Prior research indicates rising methamphetamine use and harms in the U.S., potentially related to increases in methamphetamine injection. To date, research on trends and correlates of methamphetamine injection is limited.
Methods:
Analysis of trends and correlates of methamphetamine injection among treatment admissions among persons aged ≥ 12 whose primary substance of use at admission is methamphetamine. Data are from the Treatment Episode Data Set. Analyses includes descriptive statistics, trend analyses, and multilevel multivariable logistic regression.
Results:
Primary methamphetamine treatment admissions increased from 138,379 in 2010 to 201,021 in 2019. Among primary methamphetamine admissions, injection as the usual route of use increased from 24,821 (18.0% of admissions) in 2010 to 55,951 (28.2% of admissions) in 2019. Characteristics associated with increased adjusted odds of reporting methamphetamine injection included: males (aOR=1.13, 95% CI=1.10–1.15); admission age 25–34 years (aOR= 1.23, 95% CI=1.19–1.28) and 35–44 years (aOR=1.12, 95% CI=1.08–1.17) compared to age 18–24; dependent living (aOR=1.33, 95% CI=1.29–1.37) and homelessness (aOR=1.58, 95% CI=1.54–1.63) compared to independent living; part-time employment (aOR=1.08, 95% CI=1.02–1.14), unemployment (aOR=1.39, 95% CI=1.34–1.44) and not in labor force (aOR=1.43, 95% CI=1.37–1.49) compared to full-time employment; one to ≥four prior treatment admissions (aORs ranging from 1.19 to 1.94) compared to no prior admissions; also reporting use of cocaine (aOR=1.10, 95% CI=1.05–1.16), heroin (aOR=3.52, 95% CI=3.40–3.66), prescription opioids (aOR=1.61, 95% CI=1.54–1.67), or benzodiazepines (aOR=1.42, 95% CI=1.32–1.52) at treatment admission.
Conclusions:
Findings lend further evidence to a resurgence of methamphetamine use that is intertwined with the ongoing opioid crisis in the U.S. Efforts to expand evidence-based prevention, treatment, and response efforts, particularly to populations at highest risk, are urgently needed.
Keywords: methamphetamine, injection drug use, stimulant injection, opioid and methamphetamine
1. Introduction
Use of the addictive and potent stimulant, methamphetamine, is a global concern, including in the U.S. (United Office on Drug and Crime (UNODC), 2021). Reports in the U.S. confirm increases in methamphetamine availability across the country, along with increases to record levels of purity and potency (Drug Enforcement Administration (DEA), 2020, DEA, 2021a, DEA 2021b, UNODC, 2021). This increased availability of methamphetamine has corresponded with a rise in use and harms. The number of persons aged 12 or older in the U.S. reporting past-year methamphetamine use in 2019 was 2.0 million, up from 1.4 million in 2016, and the number of individuals with past-year methamphetamine use disorder increased from approximately 684,000 in 2016 to 1,048,000 in 2019 (Han, 2020). Substance use treatment admissions for methamphetamine also increased approximately 50% between 2010 and 2017 (Jones et al., 2020). In addition, rates of overdose deaths involving psychostimulants other than cocaine, primarily methamphetamine, increased more than four-fold between 2013 and 2019 (Mattson et al., 2021), and provisional estimates indicate a continued rise through February 2022 (Centers for Disease Control and Prevention, 2022).
Accumulating evidence demonstrates that increases in methamphetamine-related harms are intertwined with the ongoing opioid overdose crisis in the U.S. (Jones et al., 2021). Among primary heroin substance use treatment admissions, the percentage reporting methamphetamine use at admission increased from 2.1% of admissions in 2008 to 12.4% in 2017, an average annual increase of 23% per year (Jones et al., 2019). Similarly, among primary methamphetamine treatment admissions, heroin use reported at treatment admission increased nearly four-fold during the same time period (Jones et al., 2020). Additionally, psychostimulant-involved overdose deaths in which opioids were also involved increased by 34% per year from 2010 to 2019 (Hedegaard et al., 2021), in some instances these deaths were likely the result of the increasing adulteration of methamphetamine with highly potent synthetic opioids such as illicitly made fentanyl and fentanyl analogs (Jones et al., 2021). In addition to fatal overdoses, the rate of emergency department visits involving both opioids and psychostimulants increased 14.0% per year from 2011 to 2016 (Hoots et al., 2020) and polydrug overdoses (predominantly comprising opioids and amphetamines) treated in emergency departments increased by 37.3% from 2018–2019 (Liu et al., 2020).
Emerging research suggests the rise in methamphetamine-related harms is attributed, at least in part, to increases in methamphetamine injection, including among persons injecting both methamphetamine and opioids. National, as well as several smaller, U.S. studies in both the general population and in treatment samples have documented increases in methamphetamine injection (Al-Tayyib et al., 2017; Glick et al., 2018; Jones et al., 2020; Glick et al., 2021; Han et al., 2021a;). These trends are consistent with increases in methamphetamine injection seen in other countries, including Vancouver, British Columbia, and Australia (Degenhardt et al., 2017; Back et al., 2020).
Rising rates of methamphetamine injection pose several important public health challenges. Prior research shows that compared to other routes of use, persons who inject methamphetamine are more likely to engage in syringe sharing and reuse and are at greater risk for infectious disease transmission, including HIV, viral hepatitis, skin and soft tissue infections, and infective endocarditis (Binswanger, et al., 2000; Young et al., 2018; Rezaei et al., 2020; Wagner et al., 2021; Yen et al., 2021; Zhao et al., 2021). Increases in rates of viral hepatitis and outbreaks of HIV in the U.S. in recent years are linked to methamphetamine use (Cai et al., 2020; Lyss et al., 2020; Wagner et al., 2021), and a recent meta-analysis estimated that stimulant injection could contribute to 9–29% of new HIV infections and 7–20% of new hepatitis C virus (HCV) infections in the following year (Cepeda et al., 2020).
Methamphetamine injection has also been associated with increased risk for overdose (Yen et al., 2021). This risk may be particularly pronounced among persons injecting both methamphetamine and opioids (Jones et al., 2021). Compared with only injecting heroin (Al-Tayyib et al., 2017), injecting both substances is associated with a nearly 3-fold increase in the risk of having a nonfatal overdose in the past year, greater frequency of drug use, injecting daily, developing a dependence, sharing syringes and other injection equipment, and injecting in the femoral or jugular vein in the past three months (McKetin et al., 2008; Glick et al, 2021).
Although prior research has documented an overall increase in methamphetamine injection in recent years, little is known nationally about demographic groups that are contributing to the increase in methamphetamine injection, and limited research has examined the individual characteristics associated with methamphetamine injection compared to other routes of use. This study uses substance use treatment admissions data in the U.S. to examine trends and correlates of methamphetamine injection between 2010 and 2019. These findings can be used to inform prevention, treatment, and harm reduction efforts based on evolving substance use patterns.
2. Material and methods
2.1. Data source
Treatment admissions data are from the 18,393,313 treatment admissions reported in the 2010–2019 Treatment Episode Data Set (TEDS) public use files (Substance Abuse and Mental Health Services Administration (SAMHSA), 2021). TEDS, reported annually by the Substance Abuse and Mental Health Services Administration, provides information on substance use treatment admissions among persons aged 12 or older to state-licensed or certified substance use treatment facilities in the U.S. that receive federal public funding. TEDS represents a compilation of data collected through the individual data collection systems of the state agencies for substance use treatment (SAMHSA, 2021). Data from 46 states and the District of Columbia were included in the analysis. Data from South Carolina, Oregon, Washington, and Georgia were excluded due to missing data during at least one year of the study period.
2.2. Substance use measures
TEDS captures data on the primary, secondary, and tertiary substances of use at treatment admission, usual route of administration (i.e., injection, smoking, snorting, oral/other), age of first use for each reported substance, and number of prior treatment admissions, based on self-report by persons at treatment admission. TEDS may include multiple treatment admissions for the same patient. Thus, TEDS data represent admissions, not individual patients. This study focuses on admissions where methamphetamine was the primary substance of use at treatment admission.
2.3. Sociodemographic measures
Sociodemographic measures include: 1) sex; 2) age; 3) race and ethnicity; 4) U.S. census region (based on U.S. Census Bureau definition) of treatment facility; 5) living arrangement: independent living, dependent living (i.e., living in a supervised setting such as a residential institution, halfway house or group home, and children under age 18 living with parents, relatives, or guardians or in foster care), or homelessness (i.e., no fixed address, includes shelters); and 6) employment status: full-time (working ≥35 hours per week), part-time (working <35 hours per week), unemployed (looking for work in past 30 days or on layoff from job), or not in labor force.
2.4. Statistical analyses
First, we calculated the annual number of drug-related treatment admissions, the number of primary methamphetamine treatment admissions, and the percentage of drug-related treatment admissions that were primary methamphetamine admissions for each year from 2010 to 2019. Second, the percentage of primary methamphetamine treatment admissions by usual route of use were estimated for each year from 2010 to 2019. Third, the annual number of primary methamphetamine treatment admissions reporting methamphetamine injection as the usual route of use were calculated by sex, age group, race/ethnicity, U.S. census region, number of prior treatment admissions, and whether opioid use (illicit use and/or prescription opioid misuse) were reported at treatment admission as a secondary or tertiary substance of use. In addition, we calculated the percentage of primary methamphetamine treatment admissions within each of these sociodemographic groups who reported methamphetamine injection as the usual route of use.
The Joinpoint regression program (v 4.9.0.0, NCI, 2019) using a log-linear model assessed changes in trends by incorporating point estimates and their standard errors and testing a regression model using a Monte Carlo permutation method with no joinpoints (i.e., no changes in trends occurring during the assessed time period) against alternative models to determine whether and where more joinpoints (i.e., significant changes in trend) should be added (Kim et al., 2000). We used the Joinpoint calculated average annual percentage change (AAPC) to reflect the overall trend (annual percentage change, on average) during the study period (i.e., 2010–2019).
Finally, using 2019 data, a multilevel multivariable logistic regression model was used to examine characteristics associated with methamphetamine injection compared to non-injection routes of use among primary methamphetamine admissions. Variables included in the multivariable model were sex, age group, race and ethnicity, U.S. census region, living arrangement, employment status, age of first methamphetamine use, number of prior treatment admissions, and other substances reported at treatment admission. In the model, the state of an admitting treatment facility was included as a level two random intercepts parameter to control for the similarity of admissions within the same state. Multicollinearity was assessed using variance inflation factors and was not identified in the final models. Data analyses were conducted with STATA version 15.0 (Stata Corp. College Station, TX). For all analyses, P< .05 (2-tailed) was considered statistically significant.
3. Results
3.1. Trends in number of drug-related treatment admissions, primary methamphetamine admissions, and percentage of drug-related admissions that were primary methamphetamine admissions.
Drug-related treatment admissions where methamphetamine was not the primary substance of use remained stable during the study period with 1,361,233 admissions in 2010 and 1,146,234 admissions in 2019. The Average Annual Percentage Change (AAPC) was −1.1 (95% CI: −2.4–0.2) per year. In contrast, primary methamphetamine treatment admissions increased from 138,379 admissions in 2010 to 201,021 admissions in 2019; AAPC=5.0 (95% CI: 2.1–8.1). The percentage of drug-related treatment admissions where methamphetamine was the primary substance of use increased from 9.2% of admissions in 2010 to 14.9% of admissions in 2019; AAPC=5.9 (95% CI: 4.1–7.6).
3.1. Trends in number and percentage of primary methamphetamine treatment admissions reporting methamphetamine injection
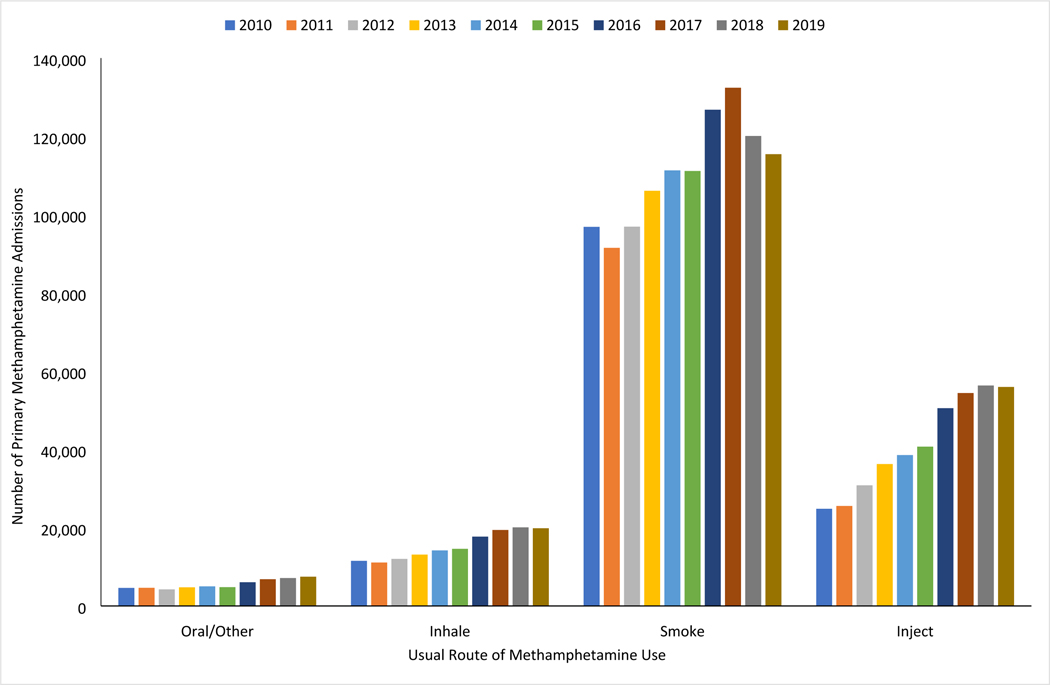
Among primary methamphetamine treatment admissions, admissions reporting injection as the usual route of use increased from 24,821 admissions in 2010 to 55,951 in 2019; admissions reporting smoking methamphetamine as their usual route of use increased from 96,866 admissions in 2010 to a peak of 132,426 admissions in 2017 before declining to 115,439 admissions in 2019 (Figure 1). Between 2010–2019, the Average Annual Percentage Change (AAPC) for number of primary methamphetamine treatment admissions reporting methamphetamine injection was 8.9 (95% CI: 6.7–13.1) per year (Table 1).
Figure 1.
Number of Primary Methamphetamine Treatment Admissions by Route of Use, 2010–2019
Table 1.
Trends in Number and Percentage of Primary Methamphetamine Treatment Admissions Reporting Methamphetamine Injection Overall and by Demographic Group, 2010–2019
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Average Annual Percent Change, 2010–2019 % (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Number | 24,821 | 25,534 | 30,800 | 36,263 | 38,562 | 40,703 | 50,542 | 54,392 | 56,330 | 55,951 | 9.8 (6.7–13.1) |
| Percentage | 18.0 | 19.2 | 21.4 | 22.6 | 22.8 | 23.8 | 25.1 | 25.5 | 27.7 | 28.2 | 5.2 (3.5–6.9) | |
| Sex | ||||||||||||
| Female | Number | 11,293 | 11,818 | 13,887 | 16,496 | 17,305 | 17,724 | 21,927 | 23,554 | 24,574 | 23,906 | 9.0 (5.6–12.4) |
| Percentage | 17.8 | 18.9 | 20.8 | 22.5 | 22.6 | 22.9 | 24.5 | 25.1 | 27.1 | 27.7 | 4.6 (3.9–5.4) | |
| Male | Number | 13,522 | 13,704 | 16,898 | 19,761 | 21,234 | 22,962 | 28,601 | 30,813 | 31,720 | 31,996 | 10.5 (7.4–13.7) |
| Percentage | 18.2 | 19.6 | 21.9 | 22.8 | 23.0 | 24.5 | 25.7 | 25.9 | 28.2 | 28.5 | 5.2 (3.4–7.1) | |
| Age | ||||||||||||
| 12–17 | Number | 148 | 183 | 255 | 311 | 286 | 288 | 303 | 308 | 238 | 171 | 5.1 (−4.3–15.4) |
| Percentage | 5.8 | 6.9 | 8.9 | 9.2 | 9.8 | 10.5 | 10.3 | 12.0 | 13.8 | 12.0 | 9.7(3.7–16.0) | |
| 18–24 | Number | 3,929 | 4,296 | 5,355 | 6,474 | 6,924 | 7,067 | 8,203 | 8,482 | 8,028 | 7,085 | 6.8 (3.2–10.6) |
| Percentage | 16.7 | 19.9 | 22.5 | 24.2 | 25.7 | 26.4 | 27.1 | 28.2 | 29.8 | 29.3 | 6.4 (5.1–7.7) | |
| 25–34 | Number | 10,494 | 10,757 | 13,072 | 15,474 | 16,722 | 17,655 | 22,422 | 24,445 | 25,542 | 25,263 | 10.9 (7.6–14.3) |
| Percentage | 19.1 | 20.0 | 22.3 | 24.0 | 24.4 | 25.1 | 27.1 | 27.7 | 30.6 | 31.3 | 5.4 (4.7–6.1) | |
| 35–44 | Number | 6,968 | 6,868 | 8,052 | 9,187 | 9,615 | 10,377 | 13,374 | 14,616 | 15,863 | 16,697 | 11.5 (9.9–13.1) |
| Percentage | 19.0 | 20.1 | 22.2 | 23.1 | 22.3 | 23.7 | 25.1 | 25.3 | 27.4 | 28.2 | 4.1 (3.4–4.9) | |
| 45–54 | Number | 2,907 | 3,030 | 3,626 | 4,186 | 4,330 | 4,523 | 5,229 | 5,370 | 5,392 | 5,388 | 7.1 (4.6–9.7) |
| Percentage | 16.5 | 17.2 | 18.7 | 19.2 | 19.2 | 20.0 | 20.4 | 20.1 | 21.2 | 21.6 | 3.1 (1.7–4.5) | |
| 55 or older | Number | 375 | 400 | 440 | 631 | 685 | 793 | 1,011 | 1,171 | 1,267 | 1,347 | 16.3 (12.3–20.4) |
| Percentage | 15.7 | 15.3 | 14.1 | 16.1 | 14.2 | 15.9 | 16.1 | 15.7 | 15.9 | 16.3 | 0.9 (−0.2–2.0) | |
| Race/Ethnicity | ||||||||||||
| White, NH | Number | 20,291 | 20,555 | 24,661 | 28,703 | 29,601 | 31,268 | 38,266 | 41,536 | 43,550 | 43,426 | 9.7 (8.0–11.5) |
| Percentage | 24.8 | 25.9 | 28.5 | 30.1 | 30.2 | 31.0 | 32.2 | 32.3 | 32.6 | 32.8 | 3.4 (2.4–4.3) | |
| Black, NH | Number | 361 | 497 | 560 | 813 | 938 | 1,081 | 1,302 | 1,568 | 1,544 | 1,629 | 16.4 (12.3–20.8) |
| Percentage | 7.3 | 9.8 | 9.9 | 11.7 | 11.7 | 12.7 | 12.8 | 13.4 | 15.8 | 16.0 | 7.1 (5.4–8.9) | |
| AI/AN, NH | Number | 611 | 657 | 855 | 996 | 1,189 | 1,423 | 1,941 | 2,065 | 2,360 | 2,154 | 16.4 (12.9–20.0) |
| Percentage | 23.5 | 25.0 | 28.9 | 29.2 | 30.6 | 34.0 | 36.1 | 35.0 | 34.6 | 34.8 | 4.1 (2.8–5.5) | |
| API, NH | Number | 200 | 169 | 205 | 293 | 312 | 313 | 409 | 398 | 356 | 396 | 9.0 (2.5–15.9) |
| Percentage | 4.7 | 4.0 | 4.7 | 6.5 | 6.5 | 6.5 | 8.1 | 8.3 | 10.5 | 12.4 | 12.3 (9.5–15.2) | |
| Other, NH | Number | 634 | 648 | 735 | 928 | 1,152 | 1,130 | 1,427 | 1,447 | 1,331 | 1,431 | 10.0 (5.7–14.4) |
| Percentage | 14.6 | 15.5 | 16.6 | 18.8 | 20.9 | 20.6 | 22.3 | 22.0 | 22.8 | 24.4 | 5.9 (4.3–7.5) | |
| Hispanic | Number | 2,324 | 2,569 | 3,304 | 3,979 | 4,749 | 4,690 | 6,078 | 6,196 | 5,550 | 5,231 | 9.6 (5.7–13.6) |
| Percentage | 6.6 | 7.7 | 9.3 | 9.9 | 10.8 | 11.1 | 12.4 | 12.6 | 15.2 | 15.0 | 8.4(6.1–10.7) | |
| U.S. Census Region | ||||||||||||
| Northeast | Number | 198 | 239 | 308 | 413 | 538 | 606 | 891 | 1,386 | 1,980 | 3,107 | 35.3 (32.8–37.9) |
| Percentage | 21.1 | 21.9 | 25.8 | 27.5 | 29.7 | 29.5 | 31.1 | 34.6 | 35.2 | 37.3 | 5.8 (4.9–6.7) | |
| Midwest | Number | 5,898 | 5,704 | 7,688 | 9,326 | 10,237 | 11,728 | 15,806 | 17,941 | 21,661 | 22,745 | 17.9 (15.9–20.0) |
| Percentage | 30.1 | 29.5 | 32.5 | 32.9 | 32.8 | 33.6 | 34.9 | 34.6 | 34.4 | 34.3 | 1.5 (0.5–2.5) | |
| South | Number | 3,728 | 4,401 | 4,934 | 6,337 | 6,194 | 7,982 | 10,517 | 12,440 | 13,993 | 14,570 | 17.5 (15.0–20.0) |
| Percentage | 32.7 | 33.2 | 36.9 | 38.8 | 36.9 | 38.0 | 38.6 | 37.7 | 36.1 | 34.3 | 0.2 (−1.5–1.9) | |
| West | Number | 14,997 | 15,190 | 17,870 | 20,187 | 21,593 | 20,387 | 23,328 | 22,625 | 18,696 | 15,529 | 0.9 (−2.6–4.4) |
| Percentage | 14.2 | 15.3 | 16.9 | 17.7 | 18.1 | 18.0 | 18.6 | 18.2 | 19.4 | 19.0 | 3.3 (2.2–4.4) | |
| Prior Treatment Admissions | ||||||||||||
| None | Number | 7,661 | 7,921 | 9,401 | 11,190 | 12,133 | 12,842 | 16,608 | 17,543 | 21,593 | 21,212 | 13.2 (11.4–15.0) |
| Percentage | 13.7 | 14.7 | 16.5 | 17.7 | 18.1 | 19.2 | 21.2 | 21.3 | 21.7 | 21.3 | 4.9 (3.6–6.2) | |
| One | Number | 5,877 | 6,130 | 7,384 | 8,554 | 8,955 | 9,364 | 11,507 | 12,349 | 10,658 | 9,644 | 5.6 (2.3–9.0) |
| Percentage | 16.7 | 17.7 | 20.0 | 21.2 | 21.3 | 22.4 | 24.1 | 24.1 | 28.9 | 30.5 | 6.4 (5.1–7.7) | |
| Two | Number | 3,983 | 3,834 | 4,659 | 5,488 | 5,571 | 5,710 | 6,926 | 7,320 | 6,790 | 6,310 | 5.6 (1.5–9.9) |
| Percentage | 20.7 | 21.1 | 23.6 | 24.9 | 24.7 | 24.9 | 25.7 | 26.6 | 31.3 | 32.2 | 4.6 (3.2–6.1) | |
| Three | Number | 2,321 | 2,595 | 3,020 | 3,423 | 3,719 | 3,813 | 4,516 | 5,005 | 4,322 | 4,290 | 6.4 (3.8–9.0) |
| Percentage | 23.3 | 26.6 | 26.7 | 27.7 | 27.9 | 28.1 | 28.5 | 30.3 | 34.7 | 36.5 | 4.3 (2.4–6.2) | |
| Four or more | Number | 4,604 | 4,855 | 6,099 | 7,329 | 7,867 | 8,570 | 10,229 | 10,942 | 10,710 | 11,969 | 11.0 (8.0–14.1) |
| Percentage | 31.1 | 32.0 | 34.1 | 35.0 | 34.5 | 35.0 | 34.8 | 35.2 | 40.8 | 41.1 | 2.8 (1.6–4.1) | |
| Opioid Use At Admission | ||||||||||||
| No | Number | 21,086 | 21,081 | 24,863 | 28,689 | 30,328 | 31,577 | 38,614 | 40,863 | 41,351 | 40,637 | 8.1 (5.0–11.3) |
| Percentage | 16.3 | 17.1 | 18.8 | 19.7 | 19.9 | 20.6 | 21.7 | 21.9 | 23.7 | 24.1 | 4.3 (3.3–5.3) | |
| Yes | Number | 3,735 | 4,453 | 5,937 | 7,574 | 8,234 | 9,126 | 11,928 | 13,529 | 14,979 | 15,314 | 16.2 (12.1–20.5) |
| Percentage | 46.1 | 47.6 | 49.8 | 51.1 | 50.0 | 50.0 | 51.9 | 51.7 | 51.0 | 51.1 | 1.2 (0.1–2.3) | |
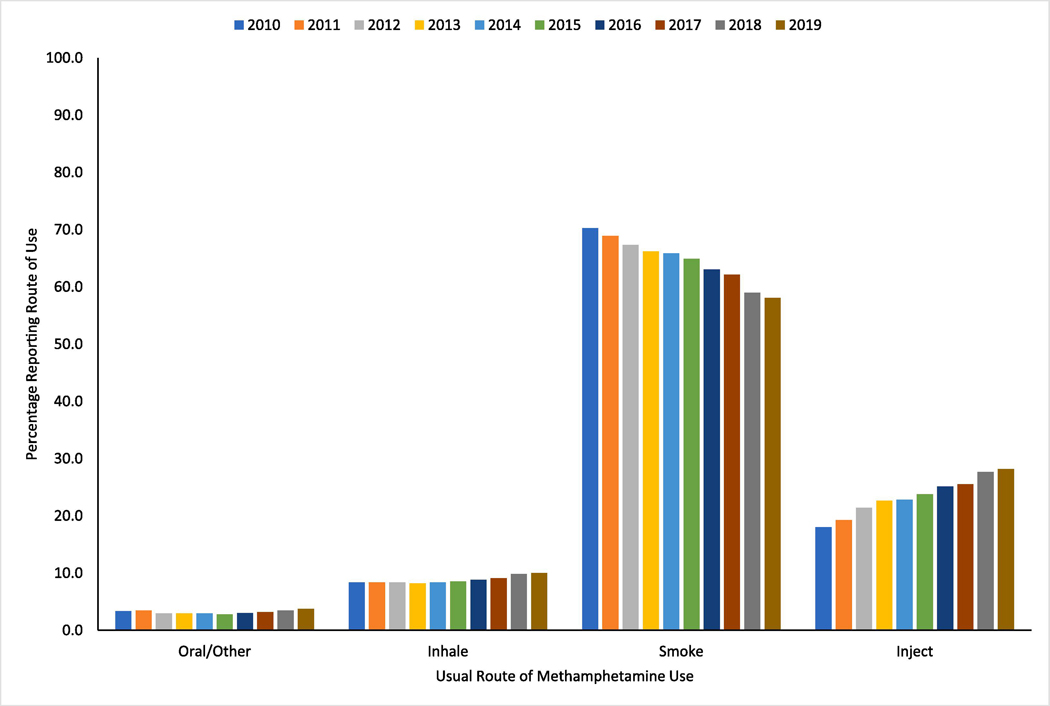
The percentage of primary methamphetamine treatment admissions reporting injection as the usual route of use increased from 18.0% of admissions in 2010 to 28.2% in 2019; the percentage of admissions reporting smoking methamphetamine as their usual route of use declined from 70.3% of admissions in 2010 to 59.0% in 2019 (Figure 2). Between 2010 to 2019, the AAPC for the percentage of primary methamphetamine admissions reporting injection was 5.2 (95% CI: 3.5–6.9) per year (Table 1).
Figure 2.
Percentage of Primary Methamphetamine Treatment Admissions by Route of Use, 2010–2019
Methamphetamine injection among primary methamphetamine treatment admissions increased among almost all demographic groups (Table 1). Among females, the number reporting methamphetamine injection increased from 11,293 in 2010 to 23,906 in 2019 (AAPC=9.0; 95% CI: 5.6–12.4), and the percentage of primary methamphetamine treatment admissions reporting injection also increased, from 17.8% in 2010 to 27.7% in 2019 (AAPC=4.6; 95% CI: 3.9–5.4). Among males, methamphetamine injection admissions increased from 13,522 to 31,996 (AAPC=10.5; 95% CI: 7.4–13.7), and the percentage reporting methamphetamine injection increased from 18.2% to 28.5% (AAPC=5.2; 95% CI:3.4–7.1). Among age groups, persons aged 25–34 had the largest number (25,263) and percentage (31.3%) of primary methamphetamine treatment admissions reporting methamphetamine injection in 2019, followed by persons aged 35–44 (16,697 and 28.2%) and 18–24 (7,085 and 29.3%).
Among racial and ethnic groups, admissions of non-Hispanic White persons accounted for the largest number of admissions reporting methamphetamine injection in 2019 (43,426), with 32.8% of primary methamphetamine treatment admissions reporting methamphetamine injection (Table 1). Admissions of non-Hispanic American Indian/Alaska Native persons had the highest percentage reporting methamphetamine injection (34.8%). The largest AAPCs for number of primary methamphetamine admissions reporting methamphetamine injection were found among admissions of non-Hispanic Black (AAPC=16.4; 95% CI: 12.3–20.8) and non-Hispanic American Indian/Alaska Native (AAPC=16.4; 95% CI: 12.9–20.0) persons during 2010–2019.
The number and percentage of primary methamphetamine treatment admissions reporting methamphetamine injection increased among those who were entering substance use treatment for the first time as well as those that had prior treatment admissions (Table 1). Among admissions with no prior treatment, the number reporting methamphetamine injection increased from 7,661 in 2010 to 21,212 in 2019 (AAPC=13.2; 95% CI:11.4–15.0). The percentage of admissions reporting methamphetamine injection increased in an incremental stepped manner as the number of prior treatment admissions increased. For example, in 2019, it increased from 21.3% for those with no prior treatment admissions to 41.1% for those with four or more prior admissions.
Among primary methamphetamine treatment admissions not reporting opioid use, the number of admissions reporting methamphetamine injection increased from 21,086 in 2010 to 40,637 in 2019 (AAPC=8.1; 95% CI: 5.0–11.3). Among those reporting opioid use at treatment admission, the number reporting methamphetamine injection increased from 3,735 in 2010 to 15,314 in 2019 (AAPC=16.2; 95% CI: 12.1–20.5). In 2019, the percentage of primary methamphetamine treatment admissions reporting methamphetamine injection was higher (51.1%) among those who also reported opioid use at treatment admissions compared to those who did not report opioid use (24.1%).
3.2. Multilevel multivariable logistic regression analysis
Among primary methamphetamine treatment admission in 2019, prevalence estimates and treatment admission characteristics associated with methamphetamine injection are found in Table 2. Characteristics associated with increased adjusted odds of reporting methamphetamine injection at treatment admission among primary methamphetamine treatment admissions included: males compared to females [adjusted odds ratio (aOR), 1.13, 95% CI, 1.10–1.15]; persons aged 25–34 (aOR, 1.23, 95% CI, 1.19–1.28) and 35–44 (aOR, 1.12, 95% CI, 1.08–1.17) compared to those aged 18–24; dependent living (aOR, 1.33, 95% CI, 1.29–1.37) and homelessness (aOR, 1.58, 95% CI, 1.1.54–1.63) compared to independent living; part-time employment (aOR, 1.08, 95% CI, 1.02–1.14) and unemployed (aOR, 1.39, 95% CI, 1.34–1.44) and not in labor force (aOR, 1.43, 95% CI, 1.37–1.49) compared to full-time employment; one to four or more prior treatment admissions (aORs ranging from 1.19 to 1.94) compared to no prior treatment admissions; and reporting the use of the following substances at treatment admission: cocaine (aOR, 1.10, 95% CI, 1.05–1.16), heroin (aOR, 3.52, 95% CI, 3.40–3.66), prescription opioids (aOR, 1.61, 95% CI, 1.54–1.67), or benzodiazepines (aOR, 1.42, 95% CI, 1.32–1.52).
Table 2.
Characteristics Associated with Reporting Methamphetamine Injection at Treatment Admission among Primary Methamphetamine Treatment Admissions in 2019
| Unadjusted Prevalence of Methamphetamine Injection* | Adjusted Odds Ratio aOR (95% CI) | |
|---|---|---|
| Sex | ||
| Female | 27.7% | Ref |
| Male | 28.5% | 1.13 (1.10–1.15) |
| Age | ||
| 12–17 | 12.0% | 0.32 (0.27–0.38) |
| 18–24 | 29.3% | Ref |
| 25–34 | 31.3% | 1.23 (1.19–1.28) |
| 35–44 | 28.2% | 1.12 (1.08–1.17) |
| 45–54 | 21.6% | 0.88 (0.84–0.93) |
| 55 or older | 16.3% | 0.69 (0.64–0.74) |
| Race/Ethnicity | ||
| White, NH | 32.8% | Ref |
| Black, NH | 16.0% | 0.49 (0.46–0.52) |
| American Indian/Alaska Native, NH | 34.8% | 1.00 (0.93–1.06) |
| Asian/Pacific Islander, NH | 12.4% | 0.38 (0.34–0.43) |
| Other, NH | 24.4% | 0.79 (0.74–0.85) |
| Hispanic | 15.0% | 0.53 (0.51–0.55) |
| Census Region | ||
| Northeast | 37.3% | Ref |
| Midwest | 34.3% | 1.03 (0.73–1.46) |
| South | 34.3% | 1.19 (0.85–1.66) |
| West | 19.0% | 0.92 (0.65–1.32) |
| Living Status | ||
| Independent | 26.5% | Ref |
| Dependent | 31.0% | 1.33 (1.29–1.37) |
| Homeless | 30.8% | 1.58 (1.54–1.63) |
| Employment Status | ||
| Full-time | 22.7% | Ref |
| Part-time | 22.5% | 1.08 (1.02–1.14) |
| Unemployed | 31.9% | 1.39 (1.34–1.44) |
| Not in Labor Force | 26.6% | 1.43 (1.37–1.49) |
| Age First Use of Methamphetamine | ||
| 14 or younger | 31.8% | Ref |
| 15–17 | 30.7% | 0.84 (0.81–0.87) |
| 18–20 | 28.8% | 0.72 (0.70–0.76) |
| 21–24 | 28.0% | 0.68 (0.65–0.71) |
| 25 or older | 23.9% | 0.55 (0.53–0.57) |
| Prior treatment admissions | ||
| None | 21.3% | Ref |
| One | 30.5% | 1.19 (1.15–1.23) |
| Two | 32.2% | 1.34 (1.29–1.40) |
| Three | 36.5% | 1.61 (1.53–1.69) |
| Four or more | 41.1% | 1.94 (1.87–2.01) |
| Other Substances Reported At Admission | ||
| Alcohol | 27.5% | 1.00 (0.97–1.03) |
| Marijuana | 28.6% | 0.97 (0.95–0.99) |
| Cocaine | 31.2% | 1.10 (1.05–1.16) |
| Heroin | 56.0% | 3.52 (3.40–3.66) |
| Prescription Opioids | 44.8% | 1.61 (1.54–1.67) |
| Benzodiazepines | 43.7% | 1.42 (1.32–1.52) |
among primary methamphetamine admissions
NH=Non-Hispanic
Bold text indicates statistically significant result
4. Discussion
Among primary methamphetamine treatment admissions across 46 states in the U.S., we found the number of admissions reporting methamphetamine injection more than doubled over the past decade, resulting in more than 1 in 4 admissions reporting methamphetamine injection as their usual route of use by 2019. This shift towards injection of methamphetamine was accompanied by a decline in smoking methamphetamine during 2010–2019. Increases in methamphetamine injection were quite widespread and impacted diverse populations, in that they were found among both men and women, nearly all age groups, all racial and ethnic groups, and across all regions of the U.S. In addition, increases in methamphetamine injection were seen among persons entering treatment for the first time as well as those who had prior substance use treatment admissions. Indeed, the largest increase was found among persons entering treatment for the first time, increasing 13% per year on average during 2010–2019. These findings are consistent with a recent study of community-dwelling adults showing an increase in the number and diversity of populations using methamphetamine as well as higher risk patterns of methamphetamine use in the U.S. between 2015 and 2019 (Han et al., 2021a). Trends in overdoses involving psychostimulants with abuse potential other than cocaine – largely methamphetamine – also mirror those observed with methamphetamine injection treatment admissions after 2010 (Hedegaard et al., 2021; Hoots et al., 2020; Mattson et al., 2021). Notably, non-fatal and fatal overdoses involving psychostimulants have increased markedly during this time period with significant increases seen among multiple demographic groups (Hedegaard et al., 2021; Hoots et al., 2020; Kariisa et al., 2021; Liu et al., 2020; Mattson et al., 2021; O’Donnell et al., 2019; Vivolo-Kantor et al., 2020). In addition, increases in psychostimulant-involved overdose deaths have been documented across geographic regions in the U.S. with the Northeast, Midwest, and South seeing the largest increases since 2013 (Cano et al., 2021; Mattson et al., 2021), consistent with the geographic trends for rising methamphetamine injection found in this study and drug supply data showing increased methamphetamine availability across the U.S. (DEA, 2020, DEA, 2021a, DEA 2021b).
Our results also add to the growing research documenting the relationship between rising methamphetamine use and the ongoing opioid crisis. Among primary methamphetamine treatment admissions, those also reporting opioid use at treatment admissions had higher rates of methamphetamine injection (51% in 2019) compared to those not reporting opioid use (24.1%); however, both groups experienced significant increases in the number of admissions and percentage of admissions reporting methamphetamine injection during 2010–2019. These findings are consistent with increases in fatal overdoses involving psychostimulants with and without opioid co-involvement, including among both sexes, in all racial and ethnic groups, and most age groups with males, non-Hispanic Black persons, American Indian and Alaskan Native persons, and persons aged 25–54 years old particularly impacted since 2011 (Han et al., 2021b; Kariisa et al., 2021; O’Donnell et al., 2019). Furthermore, overdose deaths co-involving psychostimulants and opioids began occurring at a greater rate than overdoses without co-involvement after 2017 with illicitly manufactured fentanyl and fentanyl analogs being a primary driver of these increases (Hedegaard et al., 2021; O’Donnell et al., 2019). Taken together, these findings suggest that while the resurgence of methamphetamine is intertwined with the opioid crisis, it is also occurring among persons who are not using opioids.
Our study carries important implications for public health and clinical practice. The rise in injection as the usual route of use underscores the need for strategies to address both overdose and infectious disease prevention. Expansion of interventions to identify and link persons using methamphetamine to evidence-based treatment and support services along with community-based harm reduction interventions are urgently needed. This should include strategies aimed at reducing drug use-related harms among PWID such as comprehensive syringe services programs (SSPs) that provide sterile syringes, needles, and injection equipment, screening for and linkage to substance use and infectious disease prevention and treatment services, naloxone, fentanyl test strips, and overdose prevention education (Broz et al., 2021).
The increases in methamphetamine injection also foreshadow challenges with methamphetamine treatment and recovery efforts moving forward. Prior research suggests treatment outcomes for methamphetamine use are suboptimal for persons who inject compared to those who smoke or snort (Rawson et al., 2007). Given the lack of medication-based treatment for methamphetamine use disorder, scaling up the provision of multiple treatment modalities, such as combining contingency management, which uses incentives for behavior change, and community reinforcement approach or cognitive behavioral therapy (De Crescenzo et al., 2018) is essential for achieving optimal outcomes. These efforts should be done in tandem with the expansion of recovery support services such as stable housing, food, and transportation. Given the large annual average increases seen among certain racial and ethnic minority groups such as non-Hispanic black persons and non-Hispanic American Indian and Alaska Native persons, it will be critical that efforts to expand access to prevention, treatment, harm reduction, and support services are implemented in a manner that reduces historical inequities in access to these services.
Although adolescents aged 12–17 in our study accounted for a small proportion of primary methamphetamine admissions reporting injection, the percentage of admissions injecting methamphetamine in this age group doubled over the study period. Coupled with the finding of a strong dose-response relationship showing increased risk of methamphetamine injection among individuals who initiated methamphetamine use at earlier ages highlights the importance of substance use prevention programs as a key long-run strategy for reducing methamphetamine use and its related health and social consequences. Universal substance use prevention programs that focus on youth social-emotional learning skills and strengthening other protective factors and reducing risk factors have demonstrated lasting protective effects in reducing substance use, including both methamphetamine and opioid use (Spoth et al., 2006; Spoth et al., 2007; Spoth et al., 2017). These evidence-based programs can be a central component of efforts to prevent substance use during youth and adulthood in communities.
Given the marked increases in overall treatment admissions as well as the proportion of persons admitted who report methamphetamine injection, several major areas of research are needed. The first and most acute need is for the development of more effective treatments for methamphetamine use disorder (Paulus et al., 2020). While recent work suggests that combinations of bupropion and naltrexone may be useful in methamphetamine use disorder treatment (Trivedi et al., 2021), work is needed to confirm these initial findings and develop other medications. In addition, research and policy development is needed in the U.S. to allow widespread implementation of contingency management approaches which have shown consistent positive impacts but have not been widely used and have known implementation and sustainability challenges (Higgins et al., 2019; Murphy et al., 2015; Petry et al., 2017). Given the particular increases in injection methamphetamine use, research is urgently needed on its impact on HIV and other infectious disease transmission along with testing of approaches to reducing the spread of infectious diseases (Grov et al., 2020).
The study is subject to several limitations. First, TEDS comprises a significant proportion of all admissions to substance use treatment in the U.S.; however, it does not capture every admission. TEDS includes admissions at facilities licensed or certified by the state substance abuse agency (SSAs) or administratively tracked for other reasons. States may include or exclude reporting by certain treatment sectors such as detoxification facilities and programs in the criminal justice system, and this may change over time. Some agencies regulate private facilities, methadone clinics, and/or individual practitioners and require them to report TEDS data. Second, the primary, secondary, and tertiary substances of use reported to TEDS are those that led to the treatment episode, not necessarily a complete enumeration of all drugs used. Third, TEDS is based on self-report data and thus may be subject to social desirability and recall bias. Fourth, these data should not be interpreted as prevalence estimates of drug use as TEDS captures admissions to treatment, not the general population using substances; the characteristics and patterns of methamphetamine use among treatment admissions may differ from those using methamphetamine but not engaging in substance use treatment. Fourth, TEDS admissions data do not include treatment outcomes or length of stay information; thus, we were not able to examine differences in these outcomes by route of use. Fifth, TEDS does not capture information on sexual orientation or identity. Sixth, TEDS may include multiple treatment admissions for the same patient. Thus, TEDS data represent admissions not individual patients. Finally, data from TEDS after 2019 are not yet available; thus, we are not able to explore the impact of the COVID-19 pandemic on treatment admissions, methamphetamine use, or methamphetamine injection. The currently available mortality data indicate that deaths involving psychostimulants (e.g., methamphetamine) both with and without opioid co-involvement increased during the pandemic and have continued to increase through at least February 2022 (CDC, 2022; Hedegaard et al., 2022). Future research should examine the impact of the COVID-19 pandemic on methamphetamine-related treatment and use patterns.
5. Conclusions
Over the past decade, reporting methamphetamine injection as the usual route of use among persons entering treatment for methamphetamine use has more than doubled. Importantly, increases were seen among virtually all demographic groups examined and across all regions in the U.S. These findings lend further evidence to a resurgence of methamphetamine use in the U.S. that is impacting more diverse populations, intertwined with the ongoing opioid crisis, and characterized by riskier patterns of use. Efforts are urgently needed to rapidly expand evidenced-based prevention, treatment, and response efforts, particularly to populations at highest risk.
Highlights.
Treatment admissions reporting methamphetamine injection doubled over past decade
Over 1 in 4 methamphetamine treatment admissions reported injection as usual route in 2019
Increases in methamphetamine injection were found among nearly all demographic groups
Efforts to expand prevention, treatment, and response efforts are urgently needed
Author Disclosures
Role of Funding Source: The opinions expressed in this article are those of the authors and do not necessarily represent the opinions of the Centers for Disease Control and Prevention, the National Institutes of Health, or the U.S. Department of Health and Human Services.
Footnotes
Conflicts of Interest: Unrelated to the submitted work, Compton reports ownership of stock in General Electric Co., 3M Co., and Pfizer Inc. All other authors have no conflicts to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Al-Tayyib A, Koester S, Langegger S, Raville L. 2017. Heroin and methamphetamine injection: an emerging drug use pattern. Subst Use Misuse. 52:1051–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bach P, Hayashi K, Milloy MJ, Nosova E, Kerr T, Wood E, Fairbairn N. 2020. Characterising the increasing prevalence of crystal methamphetamine use in Vancouver, Canada, from 2006–2017: a gender-based analysis. Drug Alcohol Rev. 39(7):932–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA., Kral AH., Bluthenthal RN., Rybold DJ., Edlin BR. 2000. High prevalence of abscesses and cellulitis among community-recruited injection drug users in San Francisco. Clin Infect Dis. 30(3):579–581. [DOI] [PubMed] [Google Scholar]
- Broz D. Carnes N, Chapin-Bardales J, Des Jarlais DC, et al. Syringe services programs’ role in ending the HIV epidemic in the U.S.: why we cannot do it without them. 2021. Am J Prev Med. 61(5 Suppl 1):S118–S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Y, Dai Z, Wen S, Bhandari R. 2020. Risk factors associated with infection of blood-borne virus among people who used methamphetamine. BMC Infect Dis. 20(1):742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano M, Huang Y. Overdose deaths involving psychostimulants with abuse potential, excluding cocaine: state-level differences and the role of opioids. 2021. Drug Alcohol Depend. 218:108384. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics. Provisional drug overdose death counts. 2022. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- Cepeda JA, Vickerman P, Bruneau J, et al. 2020. Estimating the contribution of stimulant injection to HIV and HCV epidemics among people who inject drugs and implications for harm reduction: a modeling analysis. Drug Alcohol Depend. 213:108135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Crescenzo F, Ciabattini M, D’Alo GL, et al. 2018. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: a systematic review and network meta-analysis. PLoS Med. 15(12):e1002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Grant S, McKetin R, Roxburgh A. et al. 2017. Crystalline methamphetamine use and methamphetamine-related harms in Australia. Drug Alcohol Rev. 36:160–170. [DOI] [PubMed] [Google Scholar]
- Drug Enforcement Administration, Diversion Control Division. 2020. National Forensic Laboratory Information System: NFLIS-drug annual report 2019. Available at: https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/NFLIS-Drug-AR2019.pdf
- Drug Enforcement Administration. 2021a. 2020 National Drug Threat Assessment. Available at: https://www.dea.gov/sites/default/files/2021-02/DIR-008-21%202020%20National%20Drug%20Threat%20Assessment_WEB.pdf
- Drug Enforcement Administration, Diversion Control Division . 2021b. National Forensic Laboratory Information System: NFLIS-drug annual report 2020.
- Glick SN, Klein KS, Tinsley J, Golden MR. 2021. Increasing heroin-methamphetamine (Goofball) use and related morbidity among Seattle area people who inject drugs. Am J Addict. 30:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick SN, Burt R, Kummer K, et al. 2018. Increasing methamphetamine injection among non-MSM who inject drugs in King County, Washington. Drug Alcohol Depend. 182:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Westmoreland D, Morrison C, Carrico AW, Nash D. 2020. The crisis we are not talking about: one-in-three annual HIV seroconversions among sexual and gender minorities were persistent methamphetamine users. J Acquir Immune Defic Syndr. 85:272–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B. 2020. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20–07-01–001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Han B, Compton WM, Jones CM, Einstein EB, Volkow ND. 2021a. Methamphetamine use, methamphetamine use disorder, and associated overdose deaths among U.S. adults. JAMA Psychiatry. Sep22:e212588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Cotto J, Etz K, Einstein EB, Compton WM, Volkow ND. 2021b. Methamphetamine overdose deaths in the U.S. by sex and race and ethnicity. JAMA Psychiatry. 78(5):564–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Minino AM, Warner M. 2021. Co-involvement of opioids in drug overdose deaths involving cocaine and psychostimulants. NCHS Data Brief, no 406. Available at: https://www.cdc.gov/nchs/products/databriefs/db406.htm [PubMed] [Google Scholar]
- Higgins ST, Kurti AN, Davis DR. 2019. Voucher-based contingency management is efficacious but underutilized in treating addictions. Perspect Behav Sci. 42(3):501–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoots B, Vivolo-Kantor A, Seth P. 2020. The rise in non-fatal and fatal overdoses involving stimulants with and without opioids in the United States. Addiction. 115:946–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Olsen EO, O’Donnell J, Mustaquim D. 2020. Resurgent methamphetamine use at treatment admission in the United States, 2008–2017. Am J Public Health. 110:509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Houry D, Han B, Baldwin G, Vivolo-Kantor A, Compton WM. 2021. Methamphetamine use in the United States: epidemiological updates and implications for prevention, treatment, and harm reduction. Ann NY Acad Sci. Sep 24 doi: 10.1111/nyas.14688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Underwood N, Compton WM. 2019. Increases in methamphetamine use among heroin treatment admissions in the United States, 2008–2017. Addiction. Sep10. Doi: 10.1111/add.14812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariisa M, Seth P, Scholl L, Wilson N, Davis NL. 2021. Drug overdose deaths involving cocaine and psychostimulants with abuse potential among racial and ethnic groups–United States, 2004–2019. Drug Alcohol Depend. 227:109001. [DOI] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. 2000. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 19(3):335–351. [DOI] [PubMed] [Google Scholar]
- Liu S, Scholl L, Hoots B, Seth P. 2020. Nonfatal drug and polydrug overdoses treated in emergency departments – 29 states, 2018–2109. Morb Mortal Wkly Rep. 69(34):1149–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyss SB, Buchacz K, McClung RP, Oster AM. 2020. Responding to outbreaks of human immunodeficiency virus among persons who inject drugs – United States, 2016–2019: perspectives on recent experience and lessons learned. J Infect Dis. 222(Suppl 5):S239–S249. [DOI] [PubMed] [Google Scholar]
- Mattson CL, Tanz LJ, Quinn K, et al. 2021. Trends and geographic patterns in drug and synthetic opioid overdose deaths – United States, 2013–2019. Morbid Mortal Wkly Rep. 70: 202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKetin R, Ross J, Kelly E, Backer A, et al. 2008. Characteristics and harms associated with injecting versus smoking methamphetamine among methamphetamine treatment entrants. Drug Alcohol Rev. 27(3):277–285. [DOI] [PubMed] [Google Scholar]
- Murphy SM, McDonell MG, McPherson S, Srebnik D, et al. 2015. An economic evaluation of a contingency-management intervention for stimulant use among community mental health patients with serious mental illness. Drug Alcohol Depend. 153:293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. 2020. Vital Signs: characteristics of drug overdose deaths involving opioids and stimulants – 24 states and the District of Columbia, January-June 2019. MMWR Morb Mortal Wkly Rep. 69(35):1189–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Olmstead TA, Rash CJ, Zajac K. 2017. Contingency management treatment for substance use disorders: how far has it come, and where does it need to go? Psychol Addict Behav. 31(8):897–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus MP, Stewart JL. 2020. Neurobiology, Clinical Presentation, and Treatment of Methamphetamine Use Disorder: A Review. JAMA Psychiatry. 77(9):959–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson RA, Gonzales R, Marinelli-Casey P, Ang A. 2007. Methamphetamine dependence: a closer look at treatment response and clinical characteristics associated with route of administration in outpatient treatment. Am J Addict. 16(4):291–299. [DOI] [PubMed] [Google Scholar]
- Rezaei O, Ghiasvand H, Higgs P, et al. 2020. Factors associated with injecting-related risk behaviors among people who inject drugs: a systematic review and meta-analysis study. J Addict Dis. 38(4):420–437. [DOI] [PubMed] [Google Scholar]
- Spoth RL, Clair S, Shin CS, Redmond C. 2006. Long-term effects of universal preventive interventions on methamphetamine use among adolescents. Arch Pediatr Adolesc Med. 160(9):876–882. [DOI] [PubMed] [Google Scholar]
- Spoth R. Redmond C, Shin C, Greenberg M, et al. 2007. Substance-use outcomes at 18 months past baseline: The PROSPER community-university partnership trial. Am J Prev Med. 32(5):395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Feinberg M, Trudeau L. 2017. PROSPER delivery of universal preventive interventions with young adolescents: long-term effects on emerging adult substance misuse and associated risk behaviors. Psyhcol Med. 47(13):2246–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS) public use files. 2021. Available at: https://www.samhsa.gov/data/data-we-collect/teds-treatment-episode-data-set
- Trivedi MH, Walker R, Ling W, Dela Cruz A, et al. 2021. Bupropion and naltrexone in methamphetamine use disorder. N Engl J Med. 384(2):140–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. World Drug Report Booklet 4: Drug Market Trends: Cocaine, Amphetamine-type Stimulants. 2021. Available at: https://www.unodc.org/unodc/en/data-and-analysis/wdr-2021_booklet-4.html
- Vivolo-Kantor AM, Hoots BE, Seth P, Jones CM. 2020. Recent trends and associated factors of amphetamine-type stimulant overdoses in emergency departments. Drug Alcohol Depend. 216:108323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner K, Zhong Y, Teshale E, et al. 2021. Hepatitis C virus infection and polysubstance use among young adult people who inject drugs in a rural county of New Mexico. Drug Alcohol Depend. Mar 1;220:108527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen Li M, Alba GA, Mitton J, Bearnot B. 2021. Care-engaged individuals with polysubstance use in Northeastern US are undertreated for methamphetamine use disorder: a retrospective cohort study. Addict Sci Clin Pract. Sep 26;16(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S. Wood E, Milloy MJ, et al. 2018. Hepatitis C cascade of care among people who inject drugs in Vancouver, Canada. Subst. Abuse 39(4):461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Kral AH, Simpson KA, et al. 2021. Factors associated with methamphetamine withdrawal symptoms among people who inject drugs. Drug Alcohol Depend. 223:108702. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States, 1999–2020. NCHS Data Brief, no 428. Hyattsville, MD: National Center for Health Statistics. 2021. DOI: 10.15620/cdc:112340 [DOI] [Google Scholar]