Abstract
Objective.
Childhood cancer represents a potentially traumatic experience for both patients and caregivers. We examined trajectories of posttraumatic stress symptoms (PTSS) across a 5-year period in children with a history of cancer and their parents/caregivers. Medical, demographic, and dispositional variables were examined as predictors of PTSS trajectories.
Method.
Using a longitudinal design, children with cancer history (n = 254, age 8-17 years at baseline) and one parent/caregiver (n = 255) completed measures of PTSS at baseline, and 1-,3-, and 5-years post-study entry. Children and caregivers completed dispositional measures including optimism, positive/negative affect, and Five-Factor Inventories. Latent class growth analysis (LCGA) was used to identify latent trajectories of PTSS, and univariate logistic regression models were conducted to predict LCGA class membership from medical, demographic and disposition factors
Results.
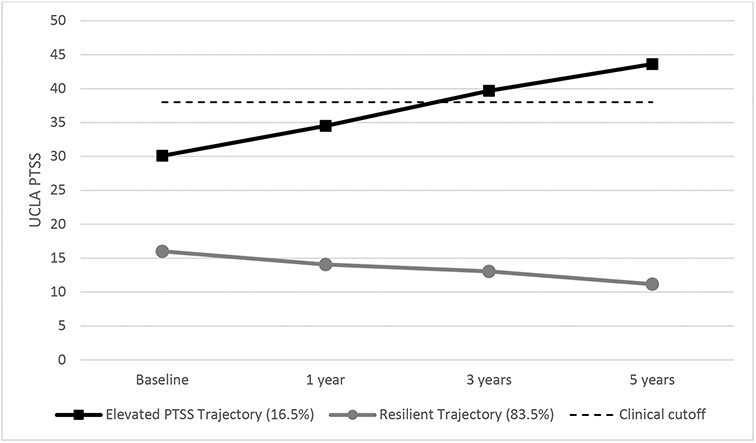
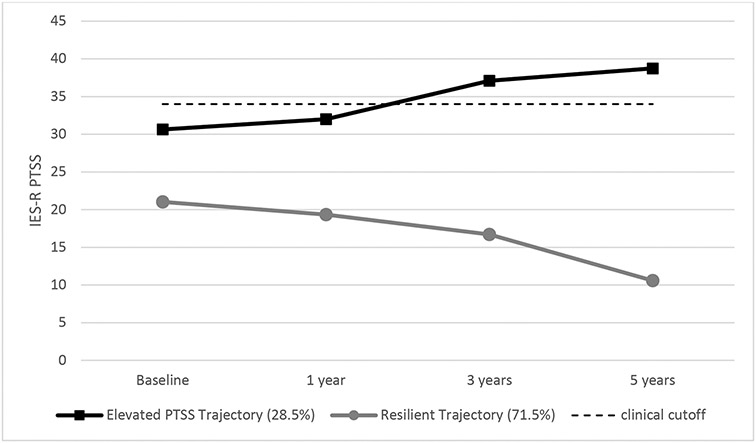
Very similar trajectories were observed in children and caregivers, with 2-class solutions providing the best fit: a ‘resilient’ class, with low PTSS at baseline, which declined significantly over time (83.5% in children; 71.5% in parents), and an ‘elevated PTSS’ class, which was moderately high at baseline and increased significantly over time. There was a small, but significant relationship between child and caregiver trajectories. Latent trajectories observed in children and parents were more strongly associated with dispositional variables than medical factors.
Conclusions:
Resilience, depicted by low PTSS, is by far the most common outcome observed in both children and caregivers. However, the smaller subset with elevated PTSS do not show recovery over time, and are identified as a group in need of targeted interventions.
Keywords: childhood cancer, posttraumatic stress, resilience, latent class growth analysis
The diagnosis and subsequent treatment demands associated with childhood cancer have long been considered a potentially traumatic event (PTE), with posttraumatic stress disorder and related symptoms (PTSD/PTSS) examined as a primary psychological outcome for patients (Bruce, 2006; Kazak et al., 2006). Similarly for parents, having a child with cancer has been examined not only as a PTE, but as one of the most severe stressors a parent can experience with PTSD/PTSS as the dominant psychosocial outcome in recent decades (Bruce, 2006; Kazak, et al., 2005; Ljungman et al., 2014). However, although trauma models continue to be applied in the childhood cancer setting, research has demonstrated that a relatively small minority of patients and parents meet full criteria for PTSD, and that most adjust well with only transient increases in distress or dysfunction (Dolgin et al., 2007; Husson et al., 2017; Noll & Kupst, 2007; Phipps et al., 2014; 2015). Thus, the setting of childhood cancer provides a unique opportunity to observe the human capacity to cope and adjust to highly stressful events, and much of the available data suggests considerable resilience in both patients and parents.
Research on the psychological responses of children with cancer have consistently demonstrated low levels of distress or dysfunction, whether focusing on internalizing outcomes such as depression (Noll et al., 1999; Phipps & Srivastava, 1997), or studies examining PTSD/PTSS outcomes (Brown et al., 2003; Kazak et al., 1997; Landolt et al., 2003; Phipps et al., 2009; Schwartz & Drotar, 2006). Studies of parental adjustment following the diagnosis of cancer in their child have been more mixed. Many studies show a mild to moderate increase in distress and depressive symptoms in the period following diagnosis, that decreases substantially over the following months, although a small subset continue to experience clinically elevated symptoms up to 5 years post-diagnosis (Compas et al., 2015; Dolgin et al., 2007; Howard Sharp et al., 2020; Katz et al., 2018; Pai et al., 2007). Studies of PTSD/PTSS have generally reported low levels of those meeting full criteria for PTSD, but with moderate elevations of PTSS (Brown et al., 2003; Dunn et al., 2012; Lindahl Norberg et al., 2012). Work from our laboratory has been the exception, with several studies demonstrating normative levels of both PTSD and PTSS (Jurbergs et al., 2009; Phipps et al., 2006; 2015). Thus, despite the somewhat higher levels of dysfunction observed in parents relative to the child patient, the great majority of parents also appear to adjust well, demonstrating considerable resilience.
There is some conceptual confusion in the literature regarding the construct of resilience, which has been operationalized in different ways as a trait, a process, or an outcome (Southwick et al., 2014). Researchers who conceptualize resilience as a trait may use a measure like the Connor-Davidson Resilience Scale (CD-RISC, Connor & Davidson, 2003) to predict responses to adversity. On the other hand, the same instrument has been used as an outcome to measure response to psychotherapeutic interventions, including in the pediatric cancer setting (Rosenberg et al., 2018). Although there is validity to all of these approaches, a recent American Psychological Association monograph concludes that resilience is not a trait, but is best operationalized in terms of positive outcomes in the face of adversity (APA, 2014). In such a framework, resilience may be demonstrated by the absence of distress/pathology following a PTE. Our approach reflects this thinking, and is modeled after the work of Bonanno (2004) who defines resilience as a stable trajectory of healthy psychological functioning following exposure to adversity or potentially traumatic events.
Examining resilience as a trajectory requires longitudinal study designs, which have been less frequent in childhood cancer, and have typically focused on change in mean levels of symptoms over time. Contemporary approaches to analysis of longitudinal data for examining resilience point towards the importance of person-centered techniques., These approaches assume variability in adjustment response (e.g., report of PTSS) within a given population and generate groupings (i.e., class or profile) based on similar response patterns (Berlin et al., 2014). In contrast, variable-centered approaches assume homogeneity across a population, and thus associations between variables and responses are assumend to be the same for all individuals within a sample. Person-centered approaches have been extensively researched by Bonanno and colleagues in the context of psychological resilience, and have demonstrated a resilience trajectory as the modal response in studies across numerous types of trauma (Bonanno et al., 2011; Galatzer-Levy et al., 2018). Other, less common trajectories have been also been consistently observed. In a recent review of 54 longitudinal studies that utilized approaches such as latent growth mixture modeling (LGMM) or latent class growth analysis (LCGA) to depict trajectories of response following PTE, Galatzer-Levy et al. (2018) found that the resilience trajectory (consistently low levels of distress/disruption) was by far the most commonly observed, occurring in nearly two thirds of cases. With a few recent exceptions (Howard Sharp et al., 2020; Katz et al., 2018) such approaches have not been applied in the childhood cancer setting.
Parental psychological functioning in response to stressful events has been shown to have a direct relationship to child adjustment in both the general population (Lambert et al., 2014) as well as in the childhood cancer setting (Bakula et al., 2019). This reflects the social-ecological model, and the influence of parent and family factors on child psychological functioning. A recent meta-analysis demonstrated moderate parent-child correlations in PTSS from 14 studies across the childhood cancer treatment continuum (mean r = .31, Bakula et al., 2019). Thus, some concordance in the trajectories of parent and child to the cancer experience would be expected.
The literature examining predictors of the resilience trajectory in adults has focused largely on individual differences, including dispositional variables such as self-enhancement, repressive coping, positive emotions, and optimism (Mancini & Bonanno, 2009). This is consistent with our earlier findings in the pediatric cancer setting, where dispositional variables, including optimism and neuroticism, accounted for the greatest variance in PTSS outcomes (Howard Sharp et al., 2015). Demographic variables, particularly socioeconomic status, have generally had a small, but significant effect on child psychosocial outcomes in the cancer setting (Howard Sharp et al., 2015; Wilson et al., 2016). Demographic factors have been inconsistently associated with parent/caregiver emotional responses to their child’s cancer, with some indicating a significant effect of employment and education (Sloper, 2000) but some more recent studies failing to show any impact (Barakat et al., 2021; Howard Sharp et al., 2020). Race/ethnicity has typically been examined only as a covariate in studies of both child and parent emotional response to cancer, and findings are inconsistent. Cancer-related variables such as diagnosis and treatment intensity have surprisingly been found to not have a significant impact on psychosocial outcomes either for patients or parents (Barakat et al., 2021; Howard Sharp et al., 2015), with a few exceptions, including chidren with brain tumors (Vannatta et al., 2007) and those who experience relapse (Phipps et al., 2009).
In the current paper we report 5-year longitudinal follow-up on a cohort of children with cancer and their parents, using measures of PTSS as the primary outcome. Findings from the baseline assessment of this cross-sectional cohort have been previously reported, and highlighted low levels of PTSD/PTSS and overall positive psychological adjustment in both patients (Phipps et al., 2014) and parents (Phipps et al., 2015). For the current study we obtained follow-up assessments of PTSS from children and parents at 1, 3, and 5 years post study entry, and utilized latent growth curve modeling to examine trajectories of PTSS over this 5-year time period. Based on the recent review of longitudinal response to PTE’s (Galatzer-Levy et al, 2018), as well as prior studies in pediatric cancer (Dolgin et al., 2007; Howard Sharp et al., 2020; Tillery et al., 2016; Katz et al., 2018), we predicted that 3 or 4 trajectories would emerge in both child and parent samples. We anticipated that a resilience trajectory of stable, low levels of PTSS across the 5-year period would be the largest trajectory observed, accounting for two thirds or more of participants in both samples, but with a somewhat higher prevalence of resilience in the children than in the parents. Any other latent classes that emerge were predicted to be much smaller and might include a stable trajectory of moderately elevated PTSS (i.e., a chronically distressed group) as well small groups showing increasing or declining PTSS over time. As a second aim, we examined the relationship of child and parent PTSS over the time frame, and the consistency of latent class membership across patient-parent dyads. We predicted that there would be small but significant parent-child correlations, and a moderate degree of concordance in their class assignments. Finally, we examined predictors of PTSS trajectories in both children and parents, including demographic and medical variables, life events history, and a number of dispositional variables. Based on our prior cross-sectional studies, we predicted that life events and dispositional variables would be more strongly related to PTSS outcomes than medical variables, and that a similar pattern of significant predictors would be found for both child and parent outcomes.
Method
Participants
Children and parents were recruited at St. Jude Children’s Research Hospital, and enrolled on a cross-sectional study, that was subsequently amended to include longitudinal assessments. The study was approved by the St. Jude Children’s Research Hospital Institutional Review Board (FWA4775) and informed consent/assent was obtained from all participants. Child eligibility at the baseline assessment included: age 8-17 years (this age was chosen to allow for valid child self-report and also to ensure that a parental respondent would be available for each patient); diagnosis of any malignancy; English-speaking; no significant cognitive or sensory impairments. Patients were recruited in 4 strata based on time since diagnosis: < 6 months; 6 months to 2 years; 2 to 5 years; > 5 years. At baseline, a total of 378 patients/parents were approached, and 258 (68%) agreed to participate. Ultimately, 254 were fully evaluable. Participants and those declining to participate did not differ significantly by age, sex, race/ethnicity, or cancer diagnosis. For each child, one parent/caregiver was enrolled, and utilized for all subsequent assessments. If that parent was not available at a particular timepoint, that data was considered missing and not substituted with data from another caregiver.
Participants who missed a subsequent observation were not considered off study unless they indicated their intention to drop out. Through the year 5 observation, overall retention was 78%. At the year 1 follow-up, a smaller number of dyads were assessed (60.4%, n = 154) due to a delay in IRB approval of the longitudinal component of the study. Participation at year 3 increased to 83.9% (n = 214), before declining slightly at year 5 (n = 199). Primary reasons for attrition at year 5 included death 7.8% (n = 20), declined further participation 4.7% (n = 12), and failure to respond or lost to follow-up 9.0% (n = 23). The demographic and medical backgrounds of the participating cohort at baseline are presented in Table 1.
Table 1.
Demographic and Medical Background of Participants
| Sex (% male) | 51.8 |
| Age at Baseline(Mean, SD) | 12.7 (2.9) |
| Child Race(%) | |
| White | 72.5 |
| Black | 22.7 |
| Other | 4.8 |
| SES (%) | |
| Group I & II | 27.5 |
| Group III | 31.8 |
| Group IV & V | 40.4 |
| Parent Participant (%) | |
| Mother | 82.4 |
| Father | 12.5 |
| Other | 4.7 |
| Parent Age (Mean, SD) | 41.7 (7.3) |
| Parent Race | |
| White | 78.3 |
| Black | 18.7 |
| Other | 3.0 |
| Diagnostic Category (%) | |
| ALL | 23.9 |
| Other Leukemia | 6.3 |
| HD/NHL | 13.3 |
| Solid Tumor | 38.4 |
| Brain Tumor | 17.3 |
| Time Since Diagnosis (%) | |
| Strata 1: < 6 months | 25.1 |
| Strata 2: 6 mos to 1.99 years | 24.7 |
| Strata 3: 2 to 4.99 years | 25.1 |
| Strata 4: ≥ 5 years | 25.1 |
| On/Off Treatment | |
| On | 47.5 |
| Off | 52.5 |
| Relapse | |
| No | 86.7 |
| Yes | 13.3 |
| Treatment Intensity | |
| Least intensive | 7.3 |
| Moderately intensive | 36.3 |
| Very intensive | 31.1 |
| Most intensive | 25.3 |
SES = Socioeconomic status (I = highest; V = lowest); ALL = Acute Lymphocytic Leukemia, HD/NHL = Hodgkin’s Disease/Non-Hodgkin’s Lymphoma. Note all demographic variables as measured as baseline
Procedure
Participants were recruited from outpatient clinics and inpatient units at St. Jude. Following consent, children and parents were seen in the Psychology clinic for completion of measures. Children and parents completed measures separately and were asked not consult with each other on their responses. Research assistants were available to assist as needed. At baseline, all data were obtained in person. During subsequent assessments at years 1, 3 and 5, for patients who did not have return oncology appointments during their scheduled timeframe +/− 3 months, an option to complete data by mail was provided.
Measures
Primary outcome measures.
University of California, Los Angeles PTSD Reaction Index for DSM-IV (UCLA-PTSDI, Pynoos et al., 1998; Steinberg et al., 2004).
This 22-item instrument was completed by children as the primary measure of PTSS. It is a widely used and well validated instrument, that provides scores on the subscales of re-experiencing, avoidance, and hyperarousal, as well as a total score. Respondents describe their most traumatic event and respond to questions in relation to that event. In the current study, we utilized the total score. A total score of 38 or greater has been identified as the clinical cutoff for likely PTSD caseness. Reliability (Cronbach’s α) across timepoints was .88 - .91.
Impact of Events Scale-Revised (Weiss & Marmar, 1997).
The 22-item IES-R was used as the measure of PTSS in parents. It provides scores on the subscales of Intrusion, Avoidance, and Hyperarousal, as well as a total score. It is a widely used instrument in the study of PTSS in adults, and reliability and validity are well documented. Parents completed this in reference to the event they described as their most traumatic. For this study, only the total score was utilized. A clinical cutoff of 34 has been used to identify likely cases of PTSD. Reliability (α ) across timepoints was .90 - .94.
Predictive Measures: Demographic and Medical Variables
In addition to child age, sex, race/ethnicity, parental respondent, and marital status, family socioeconomic status was measured using the Barratt Simplified Measure of Social Status (Barratt, 2006), an approach that utilizes parental education and occupation. A single SES score can be computed for each family (range 8-66) which can be used as a continuous variable, or cutoffs can be applied to create categorical variables, i.e., classes I – V. Medical variables examined include cancer diagnostic category (leukemia/lymphoma, non-CNS solid tumor, brain tumor), time since diagnosis, relapse status, and treatment intensity, measured with the Intensity of Treatment Rating Scale 2.0 (ITR-2, Werba et al., 2007), an approach which uses diagnosis, stage/risk level and treatment modality. All predictive variables included in the analyses, both demographic, medical, and self-report were those obtained at baseline.
Predictive Measures: Child Report
Life Events Scale for Children (LESC, Johnston et al., 2003).
This measure includes a list of 30 stressful life events. For each event, children are asked to identify if they have ever experienced it. It has shown good test-retest reliability and parent-child consistency (Johnston et al., 2003). For the current study, a simple sum of cumulative life events (unweighted) was utilized.
Youth Life Orientation Test (YLOT, Ey et al., 2004).
This 16-item measure of dispositional optimism includes 7 optimism items, 7 pessimism items and two filler items with children rating their agreement on a 4-point Likert scale. The current analysis used the global optimism score (optimism + the inverse of pessimism), which demonstrated adequate internal reliability (α = .81).
Positive and Negative Affect Scale for Children (PANAS-C, Laurent et al., 1999).
On this 20-item measure, children rate how often that have recently (past week) felt positive and negative emotions on a 5-point Likert scale. Excellent reliability, convergent and divergent validity have been reported (Laurent et al., 1999). In the current study, reliability (α) was .90 for positive and .86 for negative affectivity.
Child and Adolescent Five-Factor Inventory (CAFFI, Howard Sharp et al., 2014).
This five-factor measure was developed in our laboratory. In the current study we used a revised 50-item instrument, with 10 items per subscale. Internal reliabilities across all subscales were adequate: Neuroticism (α = .87) Extraversion (α = .80), Openness (α = .77), Agreeableness (α = .78), and Conscientiousness (α = .87). The CAFFI was found to be highly predictive of measures of depression, anxiety, and PTSS at the baseline observation of this cohort (Howard Sharp et al., 2014).
Parent Bonding Instrument (PBI, Parker et al., 1979).
The PBI is a 25-item measure assessing children’s perception of parental behavior on two domains: overprotection and care. Considerable data regarding reliability and validity have been reported (Parker et al., 1979). In the current sample, internal consistency was adequate (Overprotection, α = .72; Care, α = .81).
Predictive Measures: Parent-Report
Life Events Scale (LES, Johnston et al., 2003).
This is identical to the measure completed by children, but parents completed it in reference to their own life history.
Life Orientation Test, Revised (LOT-R, Scheier et al., 1994).
This measure was used to assess parents’ dispositional optimism. The LOT-R includes 12 items, 4 assessing optimism, 4 pessimsim and 4 filler items. It is a widely used instrument with well developed reliability and validity. In the current study, the global optimism score was used, with good internal consistency (α = .83).
NEO Five Factor Inventory (NEO-FFI, Costa & McCrae, 1992).
This 60-item, self-report instrument is a widely used measure of Big Five personality domains in adults. It consists of 5, 12-item subscales corresponding to each of the five-factor domains. In the current study, internal reliabilities for Openness (α = .59), Agreeableness (α = .68) and Extraversion (α = .69) were sub-optimal, while Neuroticism (α = .85) and Conscientiousness (α = .86) were adequate.
Positive and Negative Affect Schedule (PANAS, Watson, et al., 1988).
The PANAS is a widely used measure containing 2, 10-item scales, measuring positive and negative affect. The instrument has excellent reliability and demonstrated validity. It can be used to refer to varying timeframes. Here it is used as a dispositional measure, as parents were asked to respond based on how they ‘generally feel’. Internal reliabilities (α) in the current study were .88 for positive affect and .86 for negative affect.
Statistical Analysis
The analyses consisted of (1) latent class growth analysis (LCGA) to identify distinct change patterns and classify patients into unobserved groupings with similar patterns and (2) logistic regressions on potential factors that might contribute to the class membership identified by the LCGA. Four latent class growth models were fit to the longitudinal PTSS scores with different numbers of classes (1-4 classes). Models were compared based on Bayesian information criteria (BIC, Schwartz, 1978), sample-size adjusted BIC, entropy, and three likelihood ratio tests: Vuong-Lo-Mendell-Rubin Likelihood Ratio Test (VLMR), Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (LMR, Lo et al., 2001), and Bootstrap Likelihood Ratio Difference Test (BLRT, McLachlan & Peel, 2000) to compare each model with the model containing one fewer class according to the likelihood ratio. The LCGA was performed using Mplus software, Version 8.2 (Muthen & Muthen, 1998-2017). Missing data was handled using Full Information Maximum Likelihood (FIML), which is the default in Mplus, and allows for inclusion of all participants who provided at least one observation. Univariate logistic regression models were conducted to predict child and parent LCGA class membership from demographic, clinical, and disposition factors. Logistic regression was conducted in SAS software, Version 9.4 (Copyright (c) 2016 by SAS Institute Inc., Cary, NC, USA).
Results
Preliminary Analyses
Across all time points, PTSS scores were on average below clinical cutoff scores for both children (time 1, M=18.3, SD =13.8; time 2, M=17.69, SD =14.97; time 3, M=17.49, SD =15.58; time 4, M=16.17, SD =15.31) and caregivers (time 1, M=23.75, SD =17.84; time 2, M=22.84, SD =17.79; time 3, M=22.26, SD =17.12; time 4, M=18.33, SD =16.14). For children, approximately 11% at time 1, 7% at time 2, 9% at time 3, and 10% at time 4 met clinical cutoff score criteria for likely PTSD. A slightly higher proportion of caregivers met clinical cutoff score criteria for PTSD across all time points (28% at time 1, 17% at time 2, 21% at time 3, and 14% at time 4). Small, but significant correlations between patient and caregiver PTSS scores were observed across all four time points (time 1, r=.21, p=.001; time 2, r=.18, p=.03; time 3, r=.16, p=.03; time 4, r=.19, p=.01).
Longitudinal Trajectories
Child PTSS
A two-class solution was supported by significant changes in VLMR, LMR, and BLRT between the one- and two-class solutions, without a significant change in VLMR and LMR between the two- and three-class solutions (Table 2). The two-class model also evidenced relatively high entopy >.81 and class assignment probabilities >.94, considered strong evidence for accuracy and certainty of assignment (Rost, 2006). Although the two-class solution did not present the lowest BIC, the difference in BIC for the two- and three-class solutions was <2 and thus was not strong support for a three- over a two-class solution (Kass & Raftery, 195; Raftery 1995).
Table 2.
Comparison of Model Fit for Latent Class Growth Analyses
| Number of Classes |
BIC | Sample-size Adjusted BIC |
Entropy | VLMR p-value |
LMR p-value |
BLRT p-value |
|---|---|---|---|---|---|---|
| Child PTSS | ||||||
| 1 | 6496.981 | 6468.449 | - | - | - | - |
| 2 | 6447.703 | 6409.661 | 0.852 | 0.0023 | 0.0031 | 0.0000 |
| 3 | 6445.878 | 6398.325 | 0.855 | 0.2909 | 0.3095 | 0.0000 |
| 4 | 6439.153 | 6382.089 | 0.814 | 0.0531 | 0.0584 | 0.0000 |
| Parent PTSS | ||||||
| 1 | 6525.316 | 6496.783 | - | - | - | - |
| 2 | 6506.307 | 6468.264 | 0.659 | 0.0164 | 0.0204 | 0.0000 |
| 3 | 6505.457 | 6457.904 | 0.703 | 0.1556 | 0.1711 | 0.0000 |
| 4 | 6522.081 | 6465.017 | 0.462 | 0.4712 | 0.4712 | 1.0000 |
Note. Bolding indicates the selected model. BIC =Bayesian information criteria; VLRM= Vuong-Lo-Mendell-Rubin Likelihood Ratio Test; LMR = Lo-Mendell-Rubin Adjusted Likelihood Ratio Test; BLRT = Bootstrap Likelihood Ratio Difference Test.
Most children were categorized into a “Resilient trajectory” (n = 217, 83.5%; Figure 1) characterized by very low levels of PTSS initially, with a significantly decreasing slope over time, B = −1.64, SE = 0.37, p < .001. A smaller subgroup of children were categorized into a trajectory labeled “Elevated PTS trajectory” (n = 37, 16.5%; Figure 1). This trajectory was characterized by increasing PTSS over time, B = 4.70, SE = 1.05, p < .001, with mean PTSS exceeding the clinical cutoff of 38 in the two latter timepoints. Of note, a Chi-Square test found no significant difference in trajectory membership by time since diagnosis strata (p = .398)
Figure 1.
Child PTSS Trajectories
Parent PTSS
A two-class solution was also supported for parents by significant changes in VLMR, LMR, and BLRT between the one- and two-class solutions, without a significant change in VLMR and LMR between the two- and three-class solutions (Table 2). Although the two-class solution did not present the lowest BIC, the difference in BIC for the two- versus three-class solutions was <1 and thus not strong support for a three-class solution (Kass & Raftery, 1995; Raftery 1995). The two-class solution was further supported by average class assignment probabilities > .87.
Similar to children, most parents were categorized into a “Resilient trajectory” (n = 194, 71.5%; Figure 2), which was characterized by low levels of PTSS across all timepoints, with a significantly decreasing slope, B = −3.42, SE = 0.48, p < .001. The remaining parents were categorized into a trajectory labeled “Elevated PTS trajectory” (n = 61, 28.5%; Figure 2). This trajectory was characterized by increasing PTSS over time, B = 2.86, SE = 1.20, p = .017, with mean PTSS exceeding the clinical cutoff of 34 in the two latter timepoints. Chi-Square demonstrated no significant difference in trajectory membership across time since cancer diagnosis strata (p = .681).
Figure 2.
Parent PTSS Trajectories
Concordance between parent and child trajectory membership
A contingency table (Table 3) and McNemar test demonstrates that in addition to the small, but significant parent-child correlations, parent and child membership in the LPA classes were significantly associated, χ2 = 7.4, p = ..005.
Table 3.
McNemar Test of Concordance in Parent and Child Trajectory Membership
| Child | Parent | |||
|---|---|---|---|---|
| Low | High | Total | ||
| Low | Frequency | 168 | 49 | 217 |
| Percent | 66.1 | 19.3 | ||
| Row Pct | 77.4 | 22.6 | ||
| Col Pct | 87.1 | 80.3 | ||
| High | Frequency | 25 | 12 | 37 |
| Percent | 9.8 | 4.7 | ||
| Row Pct | 67.6 | 32.4 | ||
| Col Pct | 12.9 | 19.7 | ||
| Total | 193 | 61 | 254 | |
McNemar Test, Chi-square (df = 1) = 7.74, p =.005
Predictors of Trajectory Membership
For child PTSS, odds ratios comparing baseline predictors of membership in resilient versus elevated PTS trajectories are presented in Table 4, with the elevated PTSS trajectory used as the reference group. Baseline SES, race, cancer type, experience of stressful life events, optimism, negative affect, neuroticism, and parental overprotection predicted children’s trajectory membership. Specifically, children with higher SES and optimism were more likely to be in the resilient trajectory, whereas children reporting more stressful life events, negative affect, neuroticism, and parental overprotection were less likely in the resilient trajectory as compared to the elevated PTS trajectory. With regard to race, children who are minorities were significantly less likely to be in the resilient trajectory. Children with solid tumors were more likely to be in the resilient group compared to those with leukemia/lymphoma.
Table 4.
Correlates of child trajectory membership with the Elevated PTS group as the reference group
| Odds Ratio | 95% Wald Confidence Limits |
||
|---|---|---|---|
| Socio-demographic and Medical Factors | |||
| Patient Age | 1.047 | 0.927 | 1.183 |
| Sex (Female vs. Male) | 0.511 | 0.250 | 1.045 |
| Socioeconomic Status | 1.031* | 1.005 | 1.058 |
| Race (White vs. Other) | 0.435* | 0.212 | 0.893 |
| Marital Status | |||
| Single vs. Married | 0.429 | 0.163 | 1.125 |
| Divorced vs. Married | 1.333 | 0.374 | 4.756 |
| Separated vs. Married | 0.429 | 0.127 | 1.447 |
| Medical Factors | |||
| Diagnosis | |||
| Solid Tumor vs. Leukemia | 2.556* | 1.121 | 5.826 |
| Brain Tumor vs. Leukemia | 1.891 | 0.668 | 5.351 |
| Brain Tumor vs. Solid Tumor | 0.740 | 0.232 | 2.357 |
| Time (years) since diagnosis | 1.107 | 0.997 | 1.229 |
| Treatment Intensity Rating | |||
| Moderate vs. Least Intenstive | 0.580 | 0.121 | 2.781 |
| Very vs. Least Intensive | 0.885 | 0.178 | 4.408 |
| Most vs. Least Intensive | 1.029 | 0.193 | 5.477 |
| Relapse (yes) | 1.889 | 0.547 | 6.528 |
| Patient Dispositional Factors | |||
| Global Optimism | 1.083* | 1.031 | 1.138 |
| Positive Affect | 1.024 | 0.986 | 1.063 |
| Negative Affect | 0.935* | 0.893 | 0.978 |
| Openness | 1.036 | 0.984 | 1.090 |
| Conscientiousness | 1.004 | 0.968 | 1.041 |
| Extroversion | 1.008 | 0.952 | 1.068 |
| Agreeableness | 0.996 | 0.943 | 1.052 |
| Neuroticism | 0.901* | 0.862 | 0.941 |
| Patient Life Events | |||
| Number of Stressful Life Events | 0.905* | 0.832 | 0.985 |
| Patient-reported Parenting Behaviors | |||
| Parental Care | 1.006 | 0.940 | 1.075 |
| Parental Overprotection | 0.915* | 0.865 | 0.967 |
Note.
p is significant at least p<.05.
Similarly for parental PTSS, baseline SES, marital status, number of stressful life events, optimism, negative affect, neuroticism, and agreeableness significantly predicted trajectory membership. Specifically, parents with higher SES and optimism were more likely to be in the resilient trajectory, whereas parents reporting more stressful life events, negative affect, neuroticism, and agreeableness were less likely to be in the resilient trajectory.
Discussion
In this longitudinal sample, with excellent retention over the 5 years of study, LCGA revealed very similar patterns of PTSS trajectories in both children with cancer and their parents. As predicted, a trajectory depicting considerable resilience was by far the most common in both groups, but with a somewhat higher prevalence in children. A resilience trajectory as the modal response is consistent with the general literature on response to PTE’s (Galatzer-Levy et al., 2018). However, the prevalence of the resilient trajectory was higher than is typically observed, particularly for children, where nearly 84% of the cohort were considered resilient. These findings provide further evidence of resilience as the predominant adjustment outcome in the pediatric cancer setting.
Why are the resilient trajectories so prominent in the pediatric oncology setting? Although childhood cancer certainly remains a highly stressful event, in the modern treatment era, many of the formerly demanding or invasive treatment procedures have been eliminated or modified to be less traumatic (e.g., the use of general anesthesia for bone marrow aspirates and lumbar punctures) while at the same time, the supportive care provided to the patient and family have been strengthened. Such a context may actually serve to foster greater resilience. As we have suggested elsewhere (Phipps et al., 2014), the cancer treatment experience presents the child with a series of challenges which are stressful, but generally manageable if experienced with sufficient support, and thus can lead to a type of stress inoculation (Meichenbaum, 1993) or ‘toughening’ (Dienstbier, 1992) that leaves survivors better equipped to handle future stressors. Frequent stressful events that are managed successfully create a sense of mastery that can then generalize to other life contexts. Parents may have a similar experience as they support their child through this process.
Other elements of the current findings are unique, and somewhat unexpected. First, only two distinct trajectories were identified for children and caregivers, when three or more are generally observed across prior studies (Bonnano et al., 2011; Galatzer-Levy et al., 2018; Howard Sharp et al., 2020). For both children and caregivers, the two trajectories observed are similar, but not identical to those most commonly reported in the literature. The trajectories that we have labeled ‘resilient’ differ from the typically reported resilience trajectory in that they have a significant slope, depicting continued improvement rather than stability over time. Because both the children and parents in this group have very low PTSS at baseline, it would not be appropriate to describe the observed change as a process of recovery. Despite the significant change, we characterize this group as ‘resilient’, given that they continue to evidence low psychological morbidity. The ‘elevated PTSS’ trajectories most closely resemble the chronic distress trajectory depicted in the literature, but again, differ due to the significant slope demonstrating that the distress of this group continues to increase over time. These trajectories differ from the ‘delayed response’ or ‘worsening’ trajectories described in the review of Galatzer et al. (2018) in that the PTSS trajectories identified in the current study were already significantly elevated at baseline.
The unique trajectories observed, and the absence of a recovery or delayed response trajectory for either caregivers or patients have important clinical implications. Screening of psychological functioning has been recommended as a standard of care in pediatric cancer, but the frequency at which screening or re-screening should occur has not been established (Kazak et al., 2015). While different screening approaches may examine a broad range of variables, when focused on psychological distress, the current findings suggest that when an assessment reveals low levels of distress in patients or parents, the frequency of repeat screenings can be reduced. Ocassional monitoring will still be indicated, but more intensive surveillance is not necessary, and can allow for resources to be targeted at those with higher risk. By the same token, an assessment at any point in the cancer continnum that reveals high levels of PTSS or other psychological distress for either caregivers or patients suggests both the need for intervention and increased frequency of monitoring. Although there has been some evidence for decline in parental distress in the first 6 months following diagnosis (Dolgin et al., 2007; Steele et al., 2004), the current findings suggest there is not a natural history of recovery beyond that point, and those that are distressed are likely to remain distressed without specific, targeted intervention.
Although the overall prevalence of the resilient trajectory was higher in the children relative to parents, the similarity of the trajectory patterns in the two groups is striking. Those in the elevated PTSS classes have mean scores at baseline indicative of moderate levels of distress, and at years 3 & 5, mean scores are above the clinical cutoffs for likely PTSD. In contrast, the resilient class in both groups have low scores at baseline that continue to decline significantly in a similar manner across the 5-year period. Parent-child correlations were relatively small but statistically significant, and the McNemar test also reveals that parent and child trajectories are also related, with resilient parents also more likely to have resilient children.
As predicted, the latent trajectories observed in both children and parents were more strongly associated with dispositional variables than medical factors. Of the medical factors examined, only diagnosis was a significant predictor, where leukemia/lymphoma patients were less likely to be in the resilient class than those with solid tumors. Neither time since diagnosis, treatment intensity or relapse status were significantly related to class membership for children, and for parents, no medical variables were associated with PTSS trajectories.
In regards to demographic variables, neither age nor sex (child or parent) were significantly related to trajectories, while SES was a significant predictor for both child and parent. Race significantly predicted child trajectories, while marital status was predictive of parent outcome (where married parents were more likely to be in the resilient class than those who were separated). SES has a well established role in child health and development more generally, and has shown a small but significant relationship with patient adjustment in the childhood cancer setting (Howard Sharp et al., 2014; Poulain et al., 2020). Race has less consistently been predictive of child adjustment in the pediatric oncology setting, despite well established racial/ethnic differences in pediatric cancer survival, where the lower survival among black and Hispanic patients has been shown to be mediated by SES (Kehm et al., 2018). Race has been more clearly associated with adjustment in the adult cancer setting, where white patients show better mental health (Fuller-Thompson & West, 2019). It is worth noting that very little attention has been given to racial/ethnic differences as a predictor of adjustment in the childhood cancer setting. Even systematic reviews that cover sociodemographic factors associated with PTSD have failed to examine race/ethnicity at all (van Warmerdam et al., 2019). Cumulative stressful life events were among the strongest predictors of trajectory class in both children and parents. This is consistent with prior research in the childhood cancer setting (Currier et al., 2009; Howard Sharp et al., 2014), and integrates with the other demographic findings given the well demonstrated inter-relationship of minority status, socioeconomic disadvantage, and increased likelihood of adverse life events (Hatch & Dohrenwend, 2007), all of which are associated with lower odds of assignment to the resilient trajectory.
Dispositional optimism, negative affect, and neuroticism were consistently predictive of PTSS trajectories in both children and parents. These findings are in line with the general trauma literature (Breslau & Schultz, 2013; Gallagher et al., 2020), health-related trauma (Chung et al., 2006), as well as research specifically in pediatric oncology (Howard Sharp et al., 2014; Phipps et al., 2009). The strength of the dispositional predictors in contrast to the minimal impact of medical factors highlights the importance of attention to premorbid personality variables in the identification of those at highest risk of adjustment difficulties in the pediatric cancer setting. Given the brevity of measures of optimism and negative affectivity, consideration should be given to including such measures in standard screening processes in this setting.
Some limitations of the present study should be considered. First, the sample was cross-sectional in terms of time since diagnosis at the baseline evaluation, thus precluding an assessment from the common starting point of diagnosis for all participants. However, there were no differences in trajectory membership across the 4 time since diagnosis strata, nor was time since diagnosis as a continuous variable at baseline associated with study outcomes. Because of our interest in obtaining patient self-report, our sample did not include younger patients, and thus may not be generalizable to the larger sample of children with cancer. It is possible that parents of younger children may experience greater difficulties in adjusting to the their child’s cancer, although age of the child has not emerged as a consistent predictor of parental PTSS in the childhood cancer setting (Bruce, 2006; Lindahl Norberg et al. 2012). We also focused on the individual outcomes of patients and caregivers and did not measure the impact on family adaptation. The repeated measures utilized the DSM-IV criteria for PTSD, as it was still in effect at the time our longitudinal study began. Newer measures consistent with the DSM-5 conceptualization of PTSD are now available, but we maintained the DSM-IV version in order to be better able to assess change. Finally, a limitation to generalizability is the single-site design of the study. However, a number of multi-site studies that included the present site have not found significant site differences using the same PTSS outcome measures (Dolgin et al., 2007; Lindwall et al., 2014, Phipps et al., 2020; Sahler et al., 2013).
Despite these limitations, the current findings clearly depict resilient functioning, maintained over time, in the great majority of children and parents. This adds to the literature on response to PTE’s demonstrating the human capacity to thrive even in the face of the most difficult life challenges (Bonanno et al., 2011). Nevertheless, a subset of children and parents continue to experience high levels of distress, and the current findings suggest that recovery over time is unlikely without active intervention. Interventions that promote optimism and belief in self-efficacy are likely to be particularly helpful in this setting, such as the evidence-based Bright IDEAS program (Phipps et al., 2020; Sahler et al., 2013), but development of additional evidence based interventions are also warranted.
Table 5.
Correlates of caregiver trajectory membership with the Elevated PTSt group as the reference group
| Odds Ratio | 95% Wald Confidence Limits |
||
|---|---|---|---|
| Socio-demographic Factors | |||
| Caregiver Age | 0.990 | 0.952 | 1.030 |
| Caregiver Sex | 0.508 | 0.188 | 1.376 |
| Caregiver Race | 0.724 | 0.342 | 1.529 |
| Socioeconomic Status | 1.032* | 1.009 | 1.055 |
| Patient Sex | 0.873 | 0.491 | 1.552 |
| Patient Age | 0.998 | 0.903 | 1.103 |
| Marital Status | |||
| Single vs. Married | 0.661 | 0.270 | 1.619 |
| Divorced vs. Married | 0.646 | 0.274 | 1.521 |
| Separated vs. Married | 0.340* | 0.119 | 0.973 |
| Medical Factors | |||
| Solid Tumor vs. Leukemia | 1.208 | 0.641 | 2.279 |
| Brain Tumor vs. Leukemia | 1.139 | 0.500 | 2.597 |
| Brain Tumor vs. Solid Tumor | 0.914 | 0.389 | 2.147 |
| Time (years) since diagnosis | 0.997 | 0.933 | 1.066 |
| Treatment Intensity Rating | 1.389 | 0.439 | 4.394 |
| Moderate vs. Least Intenstive | 1.270 | 0.401 | 4.026 |
| Very vs. Least Intensive | 1.539 | 0.459 | 5.159 |
| Most vs. Least Intensive | 0.855 | 0.375 | 1.946 |
| Caregiver Dispotional Factors | |||
| Global Optimism | 1.075* | 1.015 | 1.139 |
| Positive Affect | 1.000 | 0.956 | 1.045 |
| Negative Affect | 0.898* | 0.856 | 0.943 |
| Neuroticism | 0.950* | 0.903 | 0.999 |
| Extroversion | 1.003 | 0.961 | 1.046 |
| Openness | 0.960 | 0.916 | 1.006 |
| Agreeableness | 0.940* | 0.897 | 0.986 |
| Conscienentiousness | 1.022 | 0.970 | 1.076 |
| Caregiver Life Events | |||
| Number of Stressful Life Events | 0.833* | 0.771 | 0.900 |
REFERENCES
- American Psychological Association (2014). The Road to Resilience. http://www.apa.org/practice/programs/campaign/resilience.
- Bakula DM, Sharkey CM, Perez MN, Espeleta HC, Gamwell KL, Baudino M, Delozier A,M, Chaney JM, Matt Anderson R, & Mullins LL (2019). The relationship between parent and child distress in pediatric cancer. Journal of Pediatric Psychology, 44(10), 1121–1136. 10.1093/jpepsy/jsz051. [DOI] [PubMed] [Google Scholar]
- Barakat LP, Madden RE, Vega G, Askins M, & Kazak AE (2021). Longitudinal predictors of caregiver resilience outcomes at the end of childhood cancer treatment. Psychooncology, Jan 11. 10.1002/pon.5625. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Barratt W The Barratt Simplified Measure of Social Status (BSMSS) Measuring SES. (2006). Unpublished manuscript. Indiana State University, available at http://wbarratt.indstate.edu/socialclass/Barratt_Simplified_Measure_of_Social_Status.pdf.2006 [Google Scholar]
- Berlin KS, Parra GR, & Williams NA (2014). An introduction to latent variable mixture modeling (part 2): longitudinal latent class growth analysis and growth mixture models. Journal of Pediatric Psychology, 39(2), 188–203. 10.1093/jpepsy/jst084. [DOI] [PubMed] [Google Scholar]
- Bonnano GA (2004). Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59(1), 20–28. 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonnano GA, Westphal M, & Mancini AD (2011). Resilience to loss and potential trauma. Annual Review of Clinical Psychology, 7, 511–535. 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Breslau N, & Schultz L (2013). Neuroticism and post-traumatic stress disorder: a prospective investigation. Psychological Medicine, 43(8), 1697–1702. 10.1017/S0033291712002632. [DOI] [PubMed] [Google Scholar]
- Brown RT, Madan-Swain A, & Lambert R (2003). Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. Journal of Traumatic Stress, 16(4), 309–318. 10.1023/A:1024465415620. [DOI] [PubMed] [Google Scholar]
- Bruce M (2006). A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clinical Psychology Review, 26(3), 233–256. 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Chung MC, Berger Z, Jones R, & Rudd H (2006). Posttraumatic stress disorder and general health problems following myocardial infarction (Post-MI PTSD) among older patients: the role of personality. International Journal of Geriatric Psychiatry, 21(12), 1163–1174. 10.1002/gps.1624. [DOI] [PubMed] [Google Scholar]
- Compas BE, Bemis H, Gerhardt CA, Dunn MJ, Rodriguez EM, Desjardins L, Preacher KJ, Manning S, & Vannatta K (2015). Mothers and fathers coping with their children’s cancer: Individual and interpersonal processes. Health Psychology, 34(8), 783–793. 10.1037/hea0000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, & Davidson JRT (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI), Professional Manual. Odessa, FL., Psychological Assessment Resources. [Google Scholar]
- Currier JM, Jobe-Shields LE, & Phipps S (2009). Stressful life events and posttraumatic stress symptoms in children with cancer. Journal of Traumatic Stress, 22(1), 28–35. 10.1002/jts.20382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dienstbier RA (1992). Mutual impact of toughening on crises and losses. In Mondada L, Filipp SH, & Lerner MJ (Eds.), Life crises and experiences of loss in adulthood. (pp. 367–384), Hillsdale, NJ: Erlbaum. [Google Scholar]
- Dolgin MJ, Phipps S, Fairclough DL, Sahler OJ, Askins M, Noll RB, Butler RW, Varni JR, & Katz ER (2007). Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history investigation. Journal of Pediatric Psychology, 32(7), 771–782. 10.1093/jpepsy/jsm013. [DOI] [PubMed] [Google Scholar]
- Dunn MJ Rodriguez EM, Barnwell AS, Grossenbacher JC, Vannatta K, Gerhardt CA, & Compas BE (2012). Posttraumatic stress symptoms in parents of children with cancer withing six months of diagnosis. Health Psychology, 31(2), 176–185. 10.1037/a0025545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ey S, Hadley W, Allen DN, Palmer S, Klosky J, Deptula D, Thomas J, & Cohen R (2004). A new measure of children’s optimism and pessimism: the youth life orientation test. Journal of Child Psychology and Psychiatry, 46(5), 548–558. 10.1111/j.1469-7610.2004.00372.x. [DOI] [PubMed] [Google Scholar]
- Fuller-Thompson E & West KJ (2019). Flourishing despite a cancer diagnosis: factors associated with complete mental health in a nationally-representative sample of cancer patients aged 50 and older. Aging and Mental Health, 23(9), 1263–1274. 10.1080/13607863.2018.1481926. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Huang SH, & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clinical Psychology Review, 63, 41–55. 10.1016/j.cpr.2018.05.008 [DOI] [PubMed] [Google Scholar]
- Gallagher MW, Long LJ, & Phillips CA (2020). Hope, optimism, self-efficacy, and posttraumatic stress disorder: A meta-analytic review of the prospective effects of positive expectancies. Journal of Clinical Psychology, 76(3), 329–355. 10.1002/jclp.22882. [DOI] [PubMed] [Google Scholar]
- Hatch SL, & Dohrenwend BP (2007). Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. American Journal of Community Psychology, 40(3-4), 313–332. 10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- Howard Sharp KM, Fisher RS, Clark OE, Dunnells ZDO, Murphy LK, Prussien KV, Vannatta K, Compas BE, & Gerhardt CA (2020). Long-term trajectories of depression symptoms in mothers of children with cancer. Health Psychology, 39(2), 89–98. 10.1037/hea0000826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard Sharp KM, Rowe AE, Russell K, Long A, & Phipps S (2015). Predictors of psychological functioning in children with cancer: disposition and cumulative life stressors. Psychooncology, 24(7), 779–786. 10.1002/pon.3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husson O, Zebrack B, Block R, Embry L, Aguilar C, Hayes-Lattin B, & Cole S (2017). Posttraumatic growth and well-being among adolescents and young adults (AYAS) with cancer: a longitudinal study. Supportive Care in Cancer, 25(9), 2881–2890. 10.1007/s00520-017-3707-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston CA, Steele RG, Herrera EA, & Phipps S (2003). Parent and child reporting of negative life events: discrepancy and agreement across pediatric samples. Journal of Pediatric Psychology,28(8), 579–588. 10.1093/jpepsy/jsg048. [DOI] [PubMed] [Google Scholar]
- Jurbergs N, Long A, Ticona L, & Phipps S (2009). Symptoms of posttraumatic stress in parents of children with cancer: are they elevated relative to parents of healthy children? Journal of Pediatric Psychology, 34(1), 4–13. 10.1093/jpepsy/jsm119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kass RE, Raftery AE: Bayes factors. Journal of the American Statistical Association 90(430), 773–795, 1995. 10.1080/01621459.1995.10476572. [DOI] [Google Scholar]
- Katz LF, Fladeboe K, King K, Gurtovenk K, Kawamura J, Friedman D, Compas BE, Gruhn M, Breiger D, Lengua L, Lavi I, & Settler N (2018). Trajectories of psychological adjustment in families of children with cancer. Health Psychology, 37(8), 725–735. 10.1037/hea0000619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak AE, Abrams AN, Banks J, Christofferson J, DiDonato S, Grootenhuis MA, Kabour M, Madan-Swain A, Patel SK, Zadeh S, & Kupst MJ (2015). Psychosocial assessment as a standard of care in pediatric cancer. Pediatric Blood & Cancer, 62, S426–S459. 10.1002/pbc.25730. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R, Penati B, & Stuber ML (1997). Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. Journal of Consulting and Clinical Psychology, 65(1), 120–129. 10.1037//0022-006x.65.120. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Boeving CA, Alderfer MA, Hwang WT, & Reilly A (2005). Posttraumatic stress symptoms during treatment in parents of children with cancer. Journal of Clinical Oncology, 23(30), 7405–7410. 10.1200/JCO.2005.09.110. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer MA, Rourke M (2006). An integrative model of medical traumatic stress. Journal of Pediatric Psychology, 31(4), 343–355. 10.1093/jpepsy/jsj054 [DOI] [PubMed] [Google Scholar]
- Kehm RD, Spector LG, Poynter JN Vock DM, Altekruse SF, & Osypuk TL (2918). Does socioeconomic status account for racial and ethnic disparities in childhood cancer survival? Cancer, 124(20), 4090–4097. 10.1002/cncr.31560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, & Hasbun A (2104). Association between parents’ PTSD severity and children’s psychological distress: A meta-analysis. Journal of Traumatic Stress, 27(1), 9–17. 10.1002/jts.218991. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath M, Ribi K, Gnehm HE, & Sennhauser FH (2003). Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry, 44(8), 1199–1297, 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- Laurent J, Cantanzaro SJ, Joiner TE, Rudolph KD, Potter KI, Lambert S Osborne L, & Gathright T (1999). A measure of positive and negative affect for children: Scale development and preliminary validation. Psychological Assessment, 11(3), 326–388. 10.1037/1040-3590.11.3.326. [DOI] [Google Scholar]
- Lindahl Norberg A, Poder U, Ljungman G, & von Essen L (2012). Objective and subjective factors of posttraumatic stress symptoms in parents of children with cancer – a longitudinal study. PLoS One, 7, e36218. 10.1371/journal.pone.0036218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindwall JJ, Russell K, Huang Q, Zhang H, Vannatta K, Barrera M, Alderfer M, & Phipps S (2014). Adjustment in parents of children undergoing stem cell transplantation. Biology of Blood and Marrow Transplantation, 20(4), 543–548. 10.1016/j.bbmt.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljungman L, Cernvall M, Gronqvist H, Ljotsson B, Ljungman G, & von Essen L (2014) Long-term positive and negative psychological late effects for parents of childhood cancer survivors: a systematic review. PLoS ONE, 9(7), e103340. 10.1371/journal.pone.103340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- Mancini AD, & Bonanno GA (2009). Predictors and parameters of resilience to loss: toward an individual differences model. Journal of Personality, 77(6), 1805–1832. 10.11111/j.1467-6494.2009.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meichenbaum D (1993). Stress-innoculation training: A twenty year update. In Woolfolf RL & Lehrer PM (Eds.), Principles and practices of stress management. (2nd ed., pp. 373–406). New York, NY: Guilford Press. [Google Scholar]
- Muthén LK and Muthén BO (1998-2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Noll RB, Garstein MA, Vannatta K, Correll J, Bukowski WM, & Davies WH (1999). Social, emotional, and behavioral functioning of children with cancer. Pediatrics, 103(1), 71–78. 10.1542/peds.103.1.71. [DOI] [PubMed] [Google Scholar]
- Pai AL, Greenely RN, Lewandowski A, Drotar D, Youngstrom E, & Peterson CC (2007). A meta-analytic view of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology, 21(3), 407–415. 10.1037/0893-3200.21.3.407. [DOI] [PubMed] [Google Scholar]
- Parker G, Tupling H, & Brown LB (1979). A parental bonding instrument. British Journal of Medical Psychology, 52(1), 1–10. 10.1111/j.2044-8341.1979.tb02487.x. [DOI] [Google Scholar]
- Phipps S, Fairclough DL, Noll RB, Devine KA, Dolgin MJ, Schepers SA, Askins MA, Schneider NM, Ingman K, Voll M, Katz ER, McLaughlin J, & Sahler OJZ (2020). In-person vs. web-based administration of a problem-solving skills intervention for parents of children with cancer: Report of a randomized noninferiority trial. EClinicalMedicine, 24, 100428. 10.1016/j.eclinm.2020.100428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S, Jurbergs N, & Long A (2009). Symptoms of posttraumatic stress in children with cancer: Does personality trump health status? Psycho-Oncology 18(9), 992–1002. 10.1002/pon.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S, Klosky JL, Long A, Hudson MM, Huang Q, & Zhang H (2014). Posttraumatic stress and psychological growth in children with cancer: has the traumatic impact of cancer been overestimated? Journal of Clinical Oncology, 32(7), 641–646. 10.1200/JCO.2013.49.8212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S, Larson S Long A, & Rai SN (2006). Adaptive style and symptoms of posttraumatic stress in children with cancer and their parents. Journal of Pediatric Psychology, 31(3), 298–309. 10.1093/jpepsy/js033. [DOI] [PubMed] [Google Scholar]
- Phipps S, Long A, Willard VW, Okado Y, Hudson M, Huang Q, Zhang H, & Noll RB (2015). Parents of children with cancer: At-risk or resilient? Journal of Pediatric Psychology, 40(9), 914–925. 10.1093/jpepsy/jsv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S, & Srivastava DK (1997). Repressive adaptation in children with cancer. Health Psychology, 16(6), 521–528. 10.1037//0278-6133.16.6.521. [DOI] [PubMed] [Google Scholar]
- Poulain T, Vogel M, & Kiess W (2020). Review on the role of socioeconomic status in child health and development. Current Opinions in Pediatrics, 32(2), 308–314. 10.1097/MOP.00000000000876. [DOI] [PubMed] [Google Scholar]
- Pynoos R, Rodriguez N, Steinberg A, Stuber M, & Frederick C UCLA PTSD Index for DSMIV, unpublished manual, 1998, UCLA Trauma Psychiatry Service [Google Scholar]
- Raftery AE (1995). Bayesian model selection in social research. Sociological Methodology 25, 111–163, 1995. 10.2307/271063. [DOI] [Google Scholar]
- Rosenberg AR, Bradford MC, McCauley E, Curtis JR, Wolfe J, Baker KS, & Yi-Frazier JP (2018). Promoting resilience in adolescents and young adults with cancer: results form the PRISM randomized control trial. Cancer, 124(19), 3909–3917. 10.1002/cncr.31666. [DOI] [PubMed] [Google Scholar]
- Rost J (2006). Latent-Class-Analyse [Latent Class Analysis], in Petermann FE M (ed): Handbuch der Psychologischen Diagnostik [Handbook of Psychological Assessment]. Göttingen, Germany, Hogrefe, pp 275–287 [Google Scholar]
- Sahler OJZ, Dolgin MJ, Phipps S, Fairclough DL, Askins MA, Katz E,R, Noll RB, & Butler RW (2013). Specificity of problem-solving skills training in mothers of children with newly diagnosed cancer: Results of a multisite randomized trial. Journal of Consulting and Clinical Psychology, 31(10), 1329–1335. 10.1037/0022-006X.73.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, & Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery and self-esteem): a reevaluation of the life orientation test. Journal of Personality and Social Psychology, 67(6), 1063–1078. 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Schwartz G (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. 10.1214/aos/1176344136. [DOI] [Google Scholar]
- Schwartz L, Drotar D (2006). Posttraumatic stress and related impairment in survivors of childhood cancer in early adulthood compared to healthy peers. Journal of Pediatric Psychology, 31(4), 356–366. 10.1093/jpepsy/js018. [DOI] [PubMed] [Google Scholar]
- Sloper P (2000). Predictors of distress in parents of children with cancer: a prospective study. Journal of Pediatric Psychology, 25(2), 79–91. 10.1093/jpepsy/25.2.79. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, & Yehuda R (2014). Resilience definitions, theory, and challenges: interdisciplinary perspectives. European Journal of Psychotraumatology, Oct 1:5, 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele RG, Dreyer ML, & Phipps S (2004). Patterns of maternal distress among children with cancer and their association with child emotional and somatic distress. Journal of Pediatric Psychology, 29(7), 507–517. 10.1093/jpepsy/jsh053. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Currents Psychiatry Reports, 6(2), 96–100. 10.1007/s11920-00400048-2. [DOI] [PubMed] [Google Scholar]
- Tillery R, Howard Sharp KM, Okado Y, Long A, Phipps S (2016). Profiles of resilience and growth in youth with cancer and healthy comparisons. Journal of Pediatric Psychology, 41(3), 290–297. 10.1093/jpepsy/jsv091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannatta K, Gerhardt CA, Wells RJ, & Noll RB (2007). Intensity of CNS treatment for pediatric cancer: prediction of social outcomes in survivors. Pediatric Blood and Cancer, 49(5), 716–722. 10.1002/pbc.21062. [DOI] [PubMed] [Google Scholar]
- Van Warmerdam J, Zabih V, Kurdyak P, Sutradhar R, Nathan PC, & Gupta S (2019). Pediatric Blood & Cancer, 66(6), e27677. 10.1002/pbc.27677. [DOI] [PubMed] [Google Scholar]
- Vrijmoet-Wiersma CM, van Klink JMM, Kolk AM, Koopman HM, Ball LM, Maarten Egeler R (2008). Assessment of parental strss in pediatric cancer: a review. Journal of Pediatric Psychology, 33(7), 694–706. 10.1093/jpepsy/jsn007. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weiss DS & Marmar CR (1997). The impact of event scale-revised. In Wilson JP, & Keane TM (Eds.), Assessing Psychological Trauma and PTSD (pp. 399–411). New York: Guilford. [Google Scholar]
- Werba BE, Hobbie W, Kazak AE, Ittenbach RF, Reilly AF, & Meadows AT (2007). Classifying the intensity of pediatric cancer treatment protocols: the intensity of treatment scale 2.0(ITR-2). Pediatric Blood & Cancer, 48(7), 673–677. 10.1002/pbc.21184. [DOI] [PubMed] [Google Scholar]
- Wilson JZ, Marin D, Maxwell K, Cumming J, Berger R, Saini S, Ferguson W, & Chibnall JT (2016). Association of posttraumatic growth and illness-related burden with psychosocial factors of patient, family, and provider in pediatric cancer survivors. Journal of Traumatic Stress, 29(5), 448–346. 10.1002/jts.22123. [DOI] [PubMed] [Google Scholar]