Abstract
Objectives
Differences in National Institutes of Health (NIH) funding between specialties may affect research and patient outcomes in specialties that are less well funded. The aim of this study is to evaluate how NIH funding has been awarded by medical specialty. This study assesses differences and trends in the amount of funding, by medical specialty, for the years 2011–2020, via a retrospective analysis of data from the NIH RePORTER (Research Portfolio Online Reporting Tools Expenditures and Results).
Study design
Longitudinal cross-sectional study
Setting
NIH RePORTER data from 2011 to 2020 for awarded NIH grants (F32, T32, K01, K08, K23, R01, R03, R21, U01, P30) in the following medical specialties: anaesthesiology, dermatology, emergency medicine, family medicine, internal medicine, neurology, neurosurgery, obstetrics and gynaecology, ophthalmology, orthopaedic surgery, otolaryngology, pathology, paediatrics, physical medicine and rehabilitation, plastic surgery, psychiatry, radiation-diagnostic/oncology, surgery, and urology.
Participants
NIH grant awardees for the years 2011-2020
Intervention
None
Primary and secondary outcome measures
The following measures were studied: (1) number of grants by specialty, (2) number of grants per active physician in each specialty, (3) total dollar amount of grants by specialty, (4) total dollar amount of grants per active physician in each specialty and (5) mean dollar amount awarded by specialty for each grant type. We investigated whether any of these measures varied between medical specialties.
Results
In general, internal medicine/medicine, psychiatry, paediatrics, pathology and neurology received the most grants per year, had the highest number of grants per active physician, had the highest total amount of funding and had the highest amount of funding per active physician, whereas fields like emergency medicine, plastic surgery, orthopaedics, and obstetrics and gynaecology had the lowest. The mean dollar amount awarded by grant type differed significantly between specialties (p value less than the Bonferroni-corrected alpha=0.00029).
Conclusions
NIH funding varies significantly between medical specialties. This may affect research progress and the careers of scientists and may affect patient outcomes in less well funded specialties.
Keywords: statistics & research methods, public health, education & training (see medical education & training)
Strengths and limitations of this study.
This study compares National Institutes of Health (NIH) funding across all medical specialties in the publicly available NIH database and evaluates an important clinical question: whether there are differences in funding between specialties.
We compare several funding measures by specialty, including (1) number of grants awarded, (2) number of grants per active physician, (3) total dollar amount of grants awarded, (4) total dollar amount of grants awarded per active physician and (5) mean dollar amount of each grant.
This study was limited because there were no data on the success rate of grant applications by specialty.
NIH data did not state whether the principal investigator was a physician or not, which limits the ability to evaluate if the funding of physician researchers varied by specialty.
Introduction
The US National Institutes of Health (NIH) is part of the US Department of Health and Human Services and is the primary agency responsible for public health and biomedical research.1 The NIH comprised over 27 separate institutes and centres covering several biomedical disciplines and specialties in medicine (online supplemental appendix I).1 Approximately 80% of NIH funding goes towards funding extramural research in the form of research grants.1
bmjopen-2021-058191supp001.pdf (231.6KB, pdf)
NIH funding is used for advancement of research across many fields of basic science and clinical medicine.2 In fiscal year 2020, the total NIH funding was $40.3 billion.2 NIH funding is spread across many medical specialties, and the number of physicians in these medical specialties varies. Assuming that the number of active physicians can be viewed as a rough approximation of the demand for a specialty and a proxy for the disease burden (diseases treated by that specialty) in the society, we hypothesised that the amount of funding for each specialty would be proportional to the number of active physicians in the specialty.
We investigated whether NIH funding metrics (number of grants, number of active physicians per grant in that specialty, total dollar amount of grants, total dollar amount of grants per active physician in that specialty and mean dollar amount of each grant type) vary between specialties and evaluated the trends in these NIH funding metrics from 2011 to 2020.
Methods
Patient and public involvement statement
Neither patients nor members of the public were involved in any way in this research. It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting or dissemination plans of our research.
Study design and data source
We carried out a retrospective analysis of the NIH’s RePORTER (Research Portfolio Online Reporting Tools Expenditures and Results) database (https://reporter.nih.gov/), which has data on grants that were awarded by the NIH.3 Unlike the federal Query/View/Report database, the RePORTER database shows data only for grants that were awarded and therefore does not allow for analysis of data involving grant applications that did not result in the awarding of a grant. As a result, we could not evaluate the success rates of grant applications by specialty.
The RePORTER database was searched for grants awarded between 2011 and 2020, which were classified, based on the department name on the grant application, into one of the following 19 specialties: anaesthesiology, dermatology, emergency medicine, family medicine, internal medicine, neurology, neurosurgery, obstetrics and gynaecology, ophthalmology, orthopaedic surgery, otolaryngology, pathology, paediatrics, physical medicine and rehabilitation, plastic surgery, psychiatry, radiation-diagnostic/oncology, surgery, and urology.3 4 These specialties were chosen because they were the medical specialties in clinical medicine available in the RePORTER database. Grants that were not classified as one of these specialties were excluded. We included all grants for each specialty from the RePORTER database. The grant types appearing in the data set are listed in online supplemental appendix II.
Number of active physicians
The number of active physicians was obtained from the Physician Specialty Data Report by the American Association of Medical Colleges.5 The number of active physicians included those from all training pathways, including doctor of (allopathic) medicine (MD), doctor of osteopathic medicine (DO) and international medical graduates.5 Because the number of active physicians per specialty was only available for certain years, during the time period of 2010–2020, linear interpolation was used to estimate the number of active physicians in the unlisted years (2011, 2012, 2014, 2016, 2018 and 2020).5 These data are shown in online supplemental appendix III.
Number of NIH grants by specialty
We evaluated all grants awarded over the 10-year period to identify the most frequently awarded grant types. The 10 most frequently awarded grant types were R01, R03, R21, F32, T32, K01, K08, K23, U01 and P30. The titles and descriptions of these grant types appear in online supplemental appendix IV. Plots of the number of grants by specialty and the per cent change in the number of grants from 2011 by specialty were created. We systematically evaluated NIH grants awarded at critical periods in the academic career pipeline, including training grants (predoctoral T32, and postdoctoral F32), career development grants (K01, K08 and K23), and grants typically awarded in the later/advanced career stages, including the R01, R03, R21, P30 and U01 grants.
Number of active physicians in each specialty per grant
To evaluate how many active physicians existed per grant type, the total number of active physicians was divided by the total number of each grant type for each year for each specialty. This metric gauges how rare it is for a physician of each specialty to have any grant type.
Total dollar amount of NIH grants awarded in each specialty
To evaluate whether differences in the number of grants resulted in differences in the dollar amount of funding for each specialty, we calculated the total dollar amount of funding by specialty from 2011 to 2020 after adjusting for inflation.6 The total dollar amount of funding was calculated for each specialty for each grant type during the study period. The annual funding each year from 2012 through 2020 was converted to year 2011 dollars, using the gross domestic product price index for the relevant years.6 To evaluate changes in funding over the time period studied, for each year after 2011, we calculated the per cent change in the dollar amount of funding after adjusting for inflation (compared with 2011) by specialty.
Dollar amount of grants per active physician
Because the total dollar amount of grants may be affected by the number of researchers in that specialty and therefore the number of active physicians, we calculated the number of dollars of funding per active physician to adjust for the differing sizes of the medical specialties. We divided the dollar amount of funding for each specialty by the number of active physicians in that specialty to calculate the dollar amount of grants per active physician.
Mean dollar amount per grant for each specialty by grant type
The dollar amounts vary by grant type, with smaller grants typically awarded to early-stage investigators and larger grants awarded to more seasoned investigators. We hypothesised that there should be no differences between specialties when the mean dollar amount per grant for a given grant type was evaluated. To test this hypothesis, we calculated the mean and SD of the inflation-adjusted dollar amount per grant by specialty for each grant type for 2011–2020.
All analyses were performed in Excel V.2107 (Microsoft, Redmond, Washington, USA) and R V.4.1.2 (R Foundation for Statistical Computing, Vienna, Austria). Qualitative variables were compared between specialties using χ2 tests, while quantitative variables were compared between specialties using t-tests with unequal variances. All test statistics were two-sided. To control for false-positive findings due to multiple comparisons between specialties, we used the Bonferroni-adjusted type I error rate of , so that p values less than this Bonferroni-adjusted type I error rate were considered statistically significant.
Results
Number of grants
From 2011 through 2020, there were 184 382 grants awarded by the NIH in the specialties considered. Internal medicine/medicine (72 205, 37.2%), psychiatry (19 029, 10.3%), paediatrics (17 422, 9.4%) and pathology (14 946, 8.1%) were the specialties that received the most NIH grants (table 1). In comparison, plastic surgery (16, 0.009%), physical medicine and rehabilitation (1124, 0.6%), urology (1474, 0.8%), and emergency medicine (1258, 0.7%) were the specialties that received the fewest NIH grants (table 1).
Table 1.
NIH funding per active physician by specialty, 2011–2020
| Specialty | Rank (based on average dollars of funding per active physician per year) | Grants (n) | Total grants awarded (%) | Average number of grants per active physician per year | Dollars of funding over the entire study period (millions) | % of total | Average number of active physicians, 2011–2020 | Average dollars of funding per active physician per year (K) |
| Pathology | 1 | 14 946 | 8.1 | 0.112 | 6366.7 | 7.6 | 13 311 | 47.8 |
| Neurology | 2 | 12 448 | 6.8 | 0.092 | 6001.6 | 7.2 | 13 539 | 44.3 |
| Internal medicine/medicine | 3 | 72 205 | 39.2 | 0.063 | 36 022.6 | 43.2 | 114 639 | 31.4 |
| Psychiatry | 4 | 19 029 | 10.3 | 0.050 | 8267.6 | 9.9 | 38 089 | 21.7 |
| Neurosurgery | 5 | 2956 | 1.6 | 0.055 | 1111.6 | 1.3 | 5410 | 20.5 |
| Paediatrics | 6 | 17 422 | 9.4 | 0.030 | 7896.5 | 9.5 | 57 967 | 13.6 |
| Ophthalmology | 7 | 5957 | 3.2 | 0.032 | 2380.8 | 2.9 | 18 684 | 12.7 |
| Surgery | 8 | 8171 | 4.4 | 0.032 | 3212.5 | 3.9 | 25 378 | 12.7 |
| Otolaryngology | 9 | 3198 | 1.7 | 0.034 | 1102.3 | 1.3 | 9485 | 11.6 |
| Radiation-diagnostic/oncology | 10 | 9562 | 5.2 | 0.025 | 3999.4 | 4.8 | 38 702 | 10.3 |
| Dermatology | 11 | 2270 | 1.2 | 0.019 | 764.5 | 0.9 | 11 803 | 6.5 |
| Urology | 12 | 1474 | 0.8 | 0.015 | 572.7 | 0.7 | 9922 | 5.8 |
| Obstetrics and gynaecology | 13 | 4343 | 2.4 | 0.010 | 1697.8 | 2 | 41 552 | 4.1 |
| Physical medicine and rehabilitation | 14 | 1124 | 0.6 | 0.012 | 357.9 | 0.4 | 9220 | 3.9 |
| Orthopaedics | 15 | 2218 | 1.2 | 0.012 | 750.2 | 0.9 | 19 222 | 3.9 |
| Anaesthesiology | 16 | 3770 | 2 | 0.0091 | 1434.7 | 1.7 | 41 391 | 3.5 |
| Emergency medicine | 17 | 1258 | 0.7 | 0.0031 | 550.2 | 0.7 | 40 395 | 1.4 |
| Family medicine | 18 | 2015 | 1.1 | 0.0018 | 848.5 | 1.0 | 112 396 | 0.8 |
| Plastic surgery | 19 | 16 | 0.0 | 0.00023 | 4.6 | 0.0 | 7079 | 0.1 |
| Total | – | 184 382 | 100 | – | 83 342.9 | 100 | 627 782 | 133 |
K, thousands; MM, millions; NIH, National Institutes of Health.
Internal medicine/medicine received the greatest number of grants, in aggregate over the period from 2011 through 2020, followed by psychiatry, paediatrics, pathology and neurology (online supplemental figure 1a, b). Internal medicine/medicine consistently received the greatest number of grants during the study.
bmjopen-2021-058191supp002.pdf (111.4KB, pdf)
The average percentage change in the number of grants by specialty from 2012 to 2020 compared with the initial year (2011) was highest for emergency medicine (40.8%), neurosurgery (34.2%) and orthopaedics (32.2%) (online supplemental figure 2). The average percentage change was lowest for plastic surgery (−51.9%), and otolaryngology (−36.8%) (online supplemental figure 2).
bmjopen-2021-058191supp003.pdf (60.7KB, pdf)
Table 2 shows the number of the most commonly awarded grant types for each specialty and shows R01 and R21 were the most awarded grant types. The number of the most awarded NIH training grants (F32 and T32) (online supplemental table 1), NIH career development grants (K01, K08 and K23) (online supplemental table 2) and NIH advanced career grants (R01, R03, R21, P30 and U01) (online supplemental table 3) is shown for each year.
Table 2.
Total number of NIH grants awarded by specialty and grant type aggregated from 2011 through 2020
| Training grants | Career development grants | Advanced career grants | ||||||||
| Specialty | F32 | T32 | K01 | K08 | K23 | R01 | R03 | R21 | P30 | U01 |
| Anaesthesiology | 43 | 178 | 53 | 167 | 126 | 2258 | 63 | 289 | 1 | 111 |
| Dermatology | 32 | 105 | 73 | 146 | 49 | 1169 | 54 | 182 | 82 | 65 |
| Emergency medicine | 4 | 9 | 9 | 58 | 171 | 415 | 27 | 58 | 0 | 89 |
| Family medicine | 2 | 51 | 97 | 27 | 59 | 787 | 56 | 174 | 30 | 131 |
| Internal medicine/medicine | 1161 | 3691 | 1462 | 2535 | 2791 | 30 801 | 1147 | 3829 | 3122 | 4512 |
| Neurology | 235 | 340 | 175 | 352 | 529 | 5769 | 129 | 791 | 181 | 577 |
| Neurosurgery | 96 | 46 | 16 | 101 | 44 | 1669 | 47 | 272 | 18 | 129 |
| Obstetrics and gynaecology | 46 | 107 | 48 | 55 | 103 | 1620 | 119 | 286 | 41 | 137 |
| Ophthalmology | 83 | 204 | 7 | 268 | 166 | 3823 | 15 | 327 | 303 | 67 |
| Orthopaedics | 60 | 76 | 62 | 48 | 26 | 1349 | 83 | 215 | 49 | 7 |
| Otolaryngology | 86 | 157 | 9 | 112 | 100 | 1642 | 118 | 225 | 118 | 38 |
| Pathology | 201 | 718 | 148 | 306 | 21 | 8110 | 197 | 1282 | 206 | 390 |
| Paediatrics | 194 | 865 | 208 | 1007 | 924 | 7467 | 362 | 1146 | 186 | 1161 |
| Physical medicine and rehabilitation | 17 | 46 | 80 | 6 | 68 | 443 | 58 | 89 | 0 | 51 |
| Plastic surgery | 1 | 0 | 0 | 0 | 0 | 7 | 2 | 0 | 0 | 3 |
| Psychiatry | 293 | 772 | 743 | 250 | 1060 | 9066 | 236 | 1580 | 133 | 825 |
| Radiation-diagnostic/oncology | 65 | 266 | 147 | 66 | 36 | 5424 | 145 | 1062 | 81 | 342 |
| Surgery | 172 | 532 | 92 | 464 | 106 | 3975 | 174 | 540 | 300 | 536 |
| Urology | 22 | 55 | 33 | 63 | 22 | 686 | 27 | 83 | 39 | 160 |
NIH, National Institutes of Health.
bmjopen-2021-058191supp014.pdf (263.6KB, pdf)
Number of active physicians per grant
More F32 grants were awarded in neurology, internal medicine/medicine and pathology than in emergency medicine. An F32 training grant was awarded for every 428–1304 neurologists, for every 875–1113 internal medicine/medicine physicians and for every 523–973 pathologists during the study period (online supplemental table 4). However, an F32 training grant was only awarded for every 33 984–45 202 emergency medicine physicians. T32 grants were also more commonly awarded in neurology, internal medicine/medicine and pathology than in emergency medicine. A T32 grant was awarded for every 349–462 neurologists, every 256–337 internal medicine/medicine physicians, every 144–230 pathologists and every 21 174–40 974 emergency medicine physicians during the years 2011-2020(online supplemental table 4).
Career development grants (K01, K08 and K23) were more frequently awarded in internal medicine/medicine, neurology and pathology as these specialties consistently had the lowest numbers of physicians per awarded grant (online supplemental table 5), while emergency medicine, family medicine and radiation-diagnostic/oncology had the highest numbers of physicians per career development grant.
For the advanced career researcher grants (R01, R03, R21, P30 and U01), internal medicine/medicine, neurology and pathology consistently had the lowest numbers of physicians per awarded grant (online supplemental table 6). There was an R01 grant awarded for every 34–41 internal medicine/medicine physicians, for every 20–25 neurologists and for every 15–17 pathologists, while there was an R01 grant awarded for every 2274–7317 plastic surgeons and for every 1194–1622 family medicine physicians. U01 grants were more commonly awarded in internal medicine/medicine and neurology and least commonly awarded in orthopaedics and family medicine. A U01 grant was awarded for every 204–295 internal medicine/medicine physicians, for every 174–391 neurologists, for every 9629–19 374 orthopaedists, and for every 7420–11 820 family medicine physicians during the study period 2011 to 2020.
Dollar amount of grants
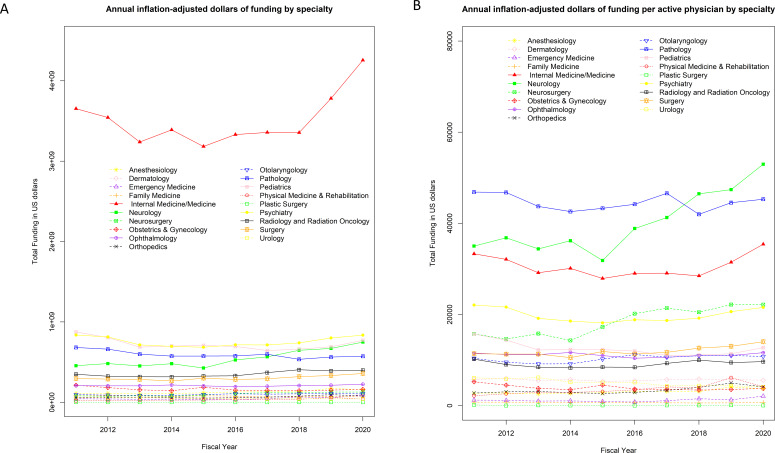
The total dollar amount of funding awarded from 2011 to 2020 was US$83 342 MM (US$1 MM is US$1 million). Of this total, the specialties receiving the largest total amount of funding were internal medicine/medicine (US$36 023 MM, 43.2%), psychiatry (US$8268 MM, 9.9%) and paediatrics (US$7897 MM, 9.5%). The specialties receiving the least funding were plastic surgery (US$4.6 MM, <0.1%), physical medicine and rehabilitation (US$358 MM, 0.4%), and emergency medicine (US$550 MM, 0.7%) (table 1). Internal medicine/medicine was the most funded specialty after adjusting for inflation (figure 1A); however, pathology and neurology were better funded after adjusting for number of active physicians (figure 1B). Of the specialties considered, emergency medicine had the largest average per cent increase in the amount of funding compared with the baseline year of 2011 (online supplemental figure 2).
Figure 1.
(A) Annual inflation-adjusted dollars of funding by specialty and (B) annual inflation-adjusted dollar amount of grant funding adjusted by the number of active physicians.
The dollar amount of funding for each specialty for the NIH training grants (F32 and T32) from 2011 to 2020 is shown in online supplemental table 7. Emergency medicine, family medicine and plastic surgery had the least amount of funding for these NIH training grants. For the NIH career development grants, we found that emergency medicine and family medicine were also among the least funded (online supplemental table 8). Finally, we found that most of the more advanced career NIH grants were in internal medicine/medicine (online supplemental table 9).
Dollar amount of grants per active physician
Pathology ($47.8 K/year) and neurology ($44.3 K/year) had the highest amounts of funding per physician over 2011–2020 (table 1) and in each of the 10 years studied (figure 1B). Both internal medicine/medicine and neurology were among the highest funded per active physician for many of the grant types studied. For instance, for NIH T32 training grants, internal medicine/medicine, neurology, pathology and psychiatry had the highest amounts of funding per physician (online supplemental table 10). Likewise, internal medicine/medicine, neurology, neurosurgery and pathology had the highest amounts of F32 funding per physician (online supplemental table 10). Internal medicine/medicine, neurology, pathology and psychiatry had the highest amounts of K01 and K08 funding per physician (online supplemental table 11). Internal medicine/medicine, neurology, paediatrics and psychiatry had the highest amounts of K23 funding per active physician (online supplemental table 11). Internal medicine/medicine, neurology, neurosurgery and psychiatry had the highest amounts of R01 and U01 funding per physician (online supplemental table 12).
Mean dollar amount per grant for each specialty by grant type
We compared the mean dollar amount of each grant for each grant type between specialties to assess whether the amount of funding varies between specialties. Online supplemental figures 3–12 show the p values from these comparisons. We found that the mean dollar amount of the NIH training grants (online supplemental table 13) varied between specialties (online supplemental figures 3 and 4). Pathology, psychiatry and neurology had significantly different F32 funding from physical medicine and rehabilitation (p<0.0002924), and urology, ophthalmology, dermatology, surgery, orthopaedics and otolaryngology had significantly different T32 funding from pathology (p<0.0002924). The mean dollar amount of the NIH career development grants (online supplemental table 14) varied between specialties. A significant variation in mean K01 funding (online supplemental figure 5), mean K08 funding (online supplemental figure 6) and K23 funding (online supplemental figure 7) was noted. For example, the mean K01 funding for dermatology was statistically significantly different from that for physical medicine and rehabilitation, psychiatry, neurology, urology, anaesthesiology, obstetrics and gynaecology, radiology, family medicine, pathology, paediatrics, otolaryngology, and internal medicine/medicine. The mean dollar amount of the NIH advanced career grants (online supplemental table 15) varied between specialties (online supplemental figures 8–12). Psychiatry had significantly different R01 funding from all other specialties, except plastic surgery, family medicine and emergency medicine (p<0.0002924).
bmjopen-2021-058191supp004.pdf (44.2KB, pdf)
bmjopen-2021-058191supp005.pdf (48.7KB, pdf)
bmjopen-2021-058191supp006.pdf (48.1KB, pdf)
bmjopen-2021-058191supp007.pdf (48.4KB, pdf)
bmjopen-2021-058191supp008.pdf (49.3KB, pdf)
bmjopen-2021-058191supp009.pdf (47.7KB, pdf)
bmjopen-2021-058191supp010.pdf (48.2KB, pdf)
bmjopen-2021-058191supp011.pdf (49.5KB, pdf)
bmjopen-2021-058191supp012.pdf (47.3KB, pdf)
bmjopen-2021-058191supp013.pdf (48.2KB, pdf)
Discussion
The data show that the number of NIH grants awarded over the investigated period varied substantially across specialties. Internal medicine/medicine consistently received the greatest number of grants, followed by psychiatry, paediatrics, pathology and neurology. After adjusting for the number of active physicians in each specialty, we found that neurology, internal medicine/medicine and pathology were the specialties with the greatest number of grants per active physician, while emergency medicine, family medicine and plastic surgery were the fields with the fewest number of grants per active physician, and this pattern was consistent across training grants, career development grants and advanced career grants. We found that internal medicine/medicine had the greatest dollar amount of funding of all medical specialties. After adjusting the dollar amount of funding by the number of active physicians in each specialty, we found that pathology, neurology, internal medicine/medicine and psychiatry were the specialties with the highest levels of funding per active physician, while plastic surgery, family medicine, emergency medicine and anaesthesiology were the specialties with the lowest levels of funding per active physician. When we analysed the mean amount of funding for each grant type, we found significant differences in funding amount between specialties.
Our results have tremendous clinical and biomedical ramifications. We show that there are differences in the amount of funding, amount of funding adjusted for number of physicians, dollar amount of NIH funding adjusted for number of physicians and funding amount for each grant type between specialties. It is unclear why these differences exist.
One speculation is that some of the better funded specialties (internal medicine/medicine, neurology, pathology) are more closely aligned with the NIH mission than other specialties; however, the NIH’s mission is ‘To seek fundamental knowledge about the nature and behavior of living systems and the application of that knowledge to enhance health, lengthen life, and reduce illness and disability’ (https://www.nih.gov/about-nih/what-we-do/nih-almanac/about-nih), which is largely applicable to all medical specialties. One consideration is the number of physicians in each specialty, or alternatively the number or amount of grants awarded to each specialty does not reflect patients’ needs for the specialty in the society. Another speculation is that the better funded specialties are intrinsically better than the less funded specialties at doing research, and in having a pipeline of training grants and career development grants, and this has resulted in the discrepancies that we have noted. One may speculate that a better funded specialty at the training and career development levels may result in that specialty having better funded status at the more advanced research career levels.
The differences in research funding between specialties have likely already had significant consequences for future progress in research. It has been shown that the proportion of individuals with MDs/PhDs who spend at least 50% of their time on research differs markedly by specialty.7 We note that the three specialties that were most highly funded on a per-physician basis (pathology, neurology and internal medicine/medicine) in our study were noted to have higher proportions of individuals spending at least 50% of their time on research, while family medicine and emergency medicine (which were among the lowest funded in our study) had much lower proportions of faculty with more than 50% time dedicated to research.8 9
Whether specialty choice is a driver of subsequent research focus in physicians’ careers is unknown; however, it is easy to speculate that greater availability of NIH funding in certain specialties may facilitate research-focused careers in those specialties. The specialties of internal medicine, pathology, paediatrics and neurology together accounted for approximately 60% of the specialties in which Medical Scientist Training Program (MSTP) MD/PhD graduates attended residency programmes.8 9 Three of these specialties were the three specialties with the highest amount of NIH funding per active physician. The temporal trend is difficult to assess, and it is unclear which is the cause and which is the effect. MD/PhD programme graduates were more likely to choose specialties like pathology and less likely to choose emergency medicine or family medicine.10 MSTP graduates may be more attracted to these better funded specialties due to increased NIH funding per active physician, or alternatively MSTP graduates in these better funded specialties were able to acquire more NIH funding per active physician.
However, the distribution of specialties pursued by MSTP graduates has changed over time and many specialties now have substantial representation,7 which means a larger proportion of these MSTP graduates are in specialties that are less well funded. The presence of substantial numbers of MDs/PhDs in specialties with lower levels of funding (eg, 12.9% of MDs/PhDs in paediatrics, 7.0% in surgical specialties and 4.2% in radiation-diagnostic/oncology) leaves the possibility of a mismatch between the supply of such well-trained physician scientists and the amount of funding available to them, which could lead to increased competition for research grants in these specialties and increased attrition, ultimately further exacerbating the relatively lower levels of research in these specialties.7 This problem is not unique to MDs/PhDs and physicians, and may also occur for nurses, nurse practitioners, public health scientists, social workers, engineers, pharmacists, PhDs and other biomedical research professionals who do research in one of the less funded specialties.
The importance of having a diverse biomedical workforce has been stressed. Diversity in race/ethnicity and gender has been at the forefront of these discussions due to the tremendous health disparities that exist across races/ethnicities and genders. However, this research shows that there are disparities in funding based on physician specialty. The current status quo makes some specialties (better NIH-funded specialties) more attractive to physician researchers. However, the inequity in NIH funding may create significant societal problems. For example, one of the worst instances of healthcare inequalities in the USA is the inequality seen in the difference between black and white maternal mortality.11 The mortality rate for non-Hispanic black women was 3.55 times that of non-Hispanic white women.11 Here, our data show that obstetrics and gynaecology was one of the worst NIH-funded specialties. Further research is required to understand the aetiology of this disparity so that the NIH research dollars are appropriately distributed among all specialties.
This study has a few limitations. We assumed that the size of the active physician workforce was a proxy for the relative amount of clinical/public health need for a given medical specialty. However, deviations from proportionality may arise if the diseases treated by certain specialties result in greater morbidity/mortality or cost to the society, and if the NIH funding depends on morbidity/mortality or cost to the society. There are several non-physician researchers, including PhDs and individuals with degrees in public health, nursing, social work, pharmacy or engineering, who are funded by the NIH. These non-MD researchers may be more likely to be hired in some specialties, and as a result change the funding landscape of those specialties. The categorisation of grants into specialties was done by the NIH. The NIH did not provide the training backgrounds of the principal investigators (PIs) and also did not provide information on whether the PIs were clinicians, and therefore we could not determine whether the categorisation was based on the specialty in which these PIs were clinically practising, or if categorisation was based on the clinical department that the PI was affiliated with. The analyses in this study were based only on grants that were awarded and did not include any data for grant applications which were rejected to assess differences in funding rates. Grant application data are not included in the RePORTER database and can only be accessed through an internal database at the NIH and were unavailable for this study. Finally, the study was limited to the PI only and did not investigate the specialties of the coinvestigators since these data were not available in the RePORTER database.
In conclusion, the number of NIH grants, total dollar amount of funding, dollar amount of funding per active physician and mean funding amount per grant (by grant type) vary by specialty. This may affect research progress and the careers of scientists and may affect patient outcomes in specialties that are less well funded. Further research is required to understand why this discrepancy exists.
Supplementary Material
Footnotes
AS and RS contributed equally.
Contributors: AS and RS analysed the data and drafted and revised the paper. RS conceived of the idea. RS is the author responsible for the overall content as the guarantor of the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was evaluated by the Mayo Clinic Institutional Review Board (IRB). The study involves freely available, public data and was determined to be exempt.
References
- 1.National Institutes of Health (NIH) . Budget, 2021. Available: https://www.nih.gov/about-nih/what-we-do/budget [Accessed 25 Aug 2021].
- 2.Atkinson RD. Healthy funding: the critical role of investing in NIH to boost health and lower costs. Information Technology & Innovation Foundation, 2019. https://itif.org/publications/2019/03/25/healthy-funding-critical-role-investing-nih-boost-health-and-lower-costs [Google Scholar]
- 3.RePORT . RePORTER [Internet]. Reporter.nih.gov, 2021. Available: https://reporter.nih.gov/advanced-search [Accessed 29 Mar 2021].
- 4.AAMC . 2020 Key Definitions, Commonly Used Acronyms, and Practice Specialties [Internet], 2021. Available: https://www.aamc.org/data-reports/workforce/interactive-data/2020-key-definitions-commonly-used-acronyms-and-practice-specialties [Accessed 17 May 2021].
- 5.AAMC . Number of People per Active Physician by Specialty, 2019 [Internet], 2021. Available: https://www.aamc.org/what-we-do/mission-areas/health-care/workforce-studies/interactive-data/number-people-active-physician-specialty-2019 [Accessed 10 May 2021].
- 6.NIH Office of Budget . Gross Domestic Product Price Index, 2022 [Internet], 2022. Available: https://officeofbudget.od.nih.gov/gbipriceindexes.html [Accessed 16 Jun 2022].
- 7.Brass LF, Akabas MH. The National MD-PhD program outcomes study: relationships between medical specialty, training duration, research effort, and career paths. JCI Insight 2019;4:133009. 10.1172/jci.insight.133009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akabas MH, Brass LF. The National MD-PhD program outcomes study: outcomes variation by sex, race, and ethnicity. JCI Insight 2019;4:133010. 10.1172/jci.insight.133010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brass LF, Akabas MH, Burnley LD, et al. Are MD-PhD programs meeting their goals? an analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med 2010;85:1–701. 10.1097/ACM.0b013e3181d3ca17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andriole DA, Whelan AJ, Jeffe DB. Characteristics and career intentions of the emerging MD/PhD workforce. JAMA 2008;300:1165–73. 10.1001/jama.300.10.1165 [DOI] [PubMed] [Google Scholar]
- 11.MacDorman MF, Thoma M, Declcerq E, et al. Racial and ethnic disparities in maternal mortality in the United States using enhanced vital records, 2016‒2017. Am J Public Health 2021;111:1673–81. 10.2105/AJPH.2021.306375 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058191supp001.pdf (231.6KB, pdf)
bmjopen-2021-058191supp002.pdf (111.4KB, pdf)
bmjopen-2021-058191supp003.pdf (60.7KB, pdf)
bmjopen-2021-058191supp014.pdf (263.6KB, pdf)
bmjopen-2021-058191supp004.pdf (44.2KB, pdf)
bmjopen-2021-058191supp005.pdf (48.7KB, pdf)
bmjopen-2021-058191supp006.pdf (48.1KB, pdf)
bmjopen-2021-058191supp007.pdf (48.4KB, pdf)
bmjopen-2021-058191supp008.pdf (49.3KB, pdf)
bmjopen-2021-058191supp009.pdf (47.7KB, pdf)
bmjopen-2021-058191supp010.pdf (48.2KB, pdf)
bmjopen-2021-058191supp011.pdf (49.5KB, pdf)
bmjopen-2021-058191supp012.pdf (47.3KB, pdf)
bmjopen-2021-058191supp013.pdf (48.2KB, pdf)
Data Availability Statement
No data are available.