Abstract
Background
Anxiety is an unpleasant feeling of fear, apprehension, and nervousness without any apparent stimulus. Anxiety is one of the co-morbidities that are often overlooked in treating patients with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS). Anxiety is worse among people with HIV/AIDS than the general population. Few studies have been conducted on prevalence of anxiety in people receiving antiretroviral treatment and limited evidence is available on its associated factors. Therefore, the objective of this study was to investigate the magnitude and associated factors of anxiety among clients on highly active antiretroviral therapy in public hospitals of Southern Ethiopia.
Methods
An institution-based cross-sectional study was conducted in public hospitals of Southern Ethiopia. Simple random sampling method was used to recruit study participants. Data collection was done by using a structured questionnaire regarding medical data related to HIV/AIDS. Seven items of the Hospital Anxiety and Depression Scale (HADS) were also used to measure the anxiety level. Oslo social support scale and perceived stigma scale were used to measure social support and stigma respectively. Bivariate and multivariate logistic regression analyses were computed with 95% CI to identify different explanatory variables. Significance was declared at p<0.05. Multi-collinearity was checked by variance inflation factors and Hosmer-Lemeshow test was used to check model fitness.
Results
Prevalence of anxiety among clients on HAART in selected public hospitals of Southern Ethiopia was found to be 25.6%. Females (AOR=3.24, 95% CI [1.32, 7.97]), being widowed (AOR=5.47, 95% CI [1.08, 29.72], monthly income 1425–2280 Ethiopian birr (AOR=7.29, 95% CI [2.55, 20.88]), comorbid conditions (AOR=5.47, 95% CI [1.92, 15.62]), perceived stigma (AOR=8.34, 95% CI [3.49, 19.91]) were factors associated with anxiety.
Conclusion
Approximately one-fourth of participants living with HIV/AIDS had anxiety. Being female, widowed, medium income, comorbid conditions, and perceived stigma were significantly associated with anxiety. This finding highlights the importance of mental health assessment, early detection and treatment of anxiety as an integral component of HIV/AIDS care.
Keywords: anxiety, HAART, antiretroviral therapy, HIV/AIDS, Ethiopia
Introduction
Anxiety is a vague, subjective, non-specific feeling of uneasiness, apprehension, tension, and fear. In general, anxiety is a very unpleasant feeling of fear, nervousness, and apprehension without any apparent stimulus, associated with physiological change.1
Globally, about 264 million people are affected by different types of anxiety disorders and it is highly prevalent among individuals with chronic diseases such as HIV/AIDS compared with the general population.2–7 Anxiety disorders have high impact on the overall functioning of the population.8,9
Approximately 35 million people are affected by HIV/AIDS and nearly 2 million people died from AIDS related causes worldwide, a particularly large number of the population, 22 million, are living with HIV and 1.2 million people died from AIDS in sub-Saharan Africa.10,11
Antiretroviral therapy (ART) is a treatment option for people infected with human immune deficiency virus (HIV). Provision of ART is aimed at reduction of HIV related mortality and morbidity and to enhance quality of life.12 Poor ART adherence is strongly associated with anxiety.13 Anxiety was ranked as the sixth largest contributor to non-fatal health loss and globally affects an estimated 264 million.6 While people living with HIV/AIDS (PLWHA) might have anxiety as part of normal life experience when encountering stressful, novel or potentially dangerous situations, it could assume the dimension of an independent medical disorder.14 People with HIV/AIDS often suffer from anxiety as they adjust to the impact of the diagnosis of being infected and face the difficulties of living with a chronic life-threatening illness, for instance shortened life expectancy, complicated therapeutic regimens, different forms of stigma, and loss of family or friends’ support.11 People affected by HIV/AIDS are more prone to develop mental disorders such as anxiety, which, in turn, impair their immune function, reduce their quality of life and adherence to treatment and contribute significantly to their premature deaths.15,16 Anxiety may occur before HIV infection or it may be related to risk behaviors for HIV infection (ie, unsafe sex or drug use); in addition, patients may feel anxious at the time of or after HIV diagnosis because of the fear of the unknown, HIV-related death.17
Anxiety also has prominent impact on the overall functioning of a patient. Some of the impacts could be poor adherence to antiretroviral therapy (ART), stigma, poor quality of life and social functioning, finally leading to premature death.6 According to studies conducted around the world, the prevalence of anxiety ranges from 7% to 82.3%.6
Previously conducted studies indicated that educational status, gender, marital status, income level, behavior, psychosocial status, social status and HIV-related clinical variables were significantly associated factors for anxiety.17,18 Few studies have been conducted on prevalence of anxiety in people receiving antiretroviral treatment, and limited evidence is available on its associated factors. This study will fill the particular research gap by simultaneously assessing the prevalence of anxiety and factors associated with anxiety among patients receiving ART in Ethiopia.
Therefore, the aim of this study was to assess the prevalence and associated factors of anxiety among HIV/AIDS patients in Southern Ethiopia.
Materials and Methods
Study Design and Period
Institution-based cross-sectional study design was used among patients who attend ART clinic in selected public hospitals of Southern Ethiopia from June 1–30, 2021.
Study Setting
The study was conducted at three public hospitals, namely Wachemo University Nigist Elleni Mohammed Memorial Specialized Hospital (WUNEMMSH) located in Hadiya zone, Worabe comprehensive specialized hospital (WCSH) located in Silte zone and Butajira General Hospital (BGH) in Gurage zone. WUNEMMSH is a teaching hospital while WCSH and BGH are public hospitals.
Hadiya, Silte, and Gurage zonal administrations are among the zonal administrations of Southern Nations Nationalities and People (SNNPR) Ethiopia. Hosanna town is the capital city of Hadiya zonal administration and 230km from Addis Ababa. Worabe town is the capital city of Silte zonal administration and 170km from Addis Ababa. Wolkite Town is the capital city of Gurage zonal administration. Butajira town is a separate woreda located 130 km from Addis Ababa.
WUNEMMSH provides over 150 different services for around 830 inpatients per month within inpatient department. It provides services such as surgery, gynecology and obstetrics, medicine, pediatrics, outpatient department, diagnostic facilities, ART clinic, psychiatry and intensive care. The hospital provides services for clients at ART clinic.
WCSH provides services such as surgery, gynecology and obstetrics, medicine, pediatrics, outpatient department, diagnostic facilities, ART clinic, psychiatry and intensive care. It also provides services for clients at ART clinic. BGH is located in Butajira town. The hospital provides services such as surgery, gynecology and obstetrics, medicine, pediatrics, outpatient department, diagnostic facilities, psychiatry and intensive care. It also provides services for clients at ART clinic.
Study Participants
All people living with HIV/AIDS who were attending ART clinic in selected public hospitals of southern Ethiopia were the source population. Randomly selected people living with HIV/AIDS who were attending ART clinic in selected public hospitals during data collection period and those included in the sample were the study population. Clients on HAART aged 18 years and above attending ART clinic in the hospitals during the data collection period for ART services were included.
Patients who were seriously ill during the data collection period were excluded from the study.
Sample Size Determination and Sampling Procedure
The sample size required for the study was calculated using a single population proportion formula by considering the prevalence rate of anxiety among clients on HAART taken from the research conducted in Debre Tabor teaching hospital which was 22.2%,19 4% margin of error, 95% confidence interval and 10% non-response rate. The sample size was determined as follows:
 |
Where n=sample size
d= 4% margin of error
p=prevalence of anxiety of ART clients 22.2%
Zα/2 = 95% = 1.96 confidence interval.
 |
Taking 5% of non-respondent rate =21.
Therefore, the final calculated sample size of the study was 436.
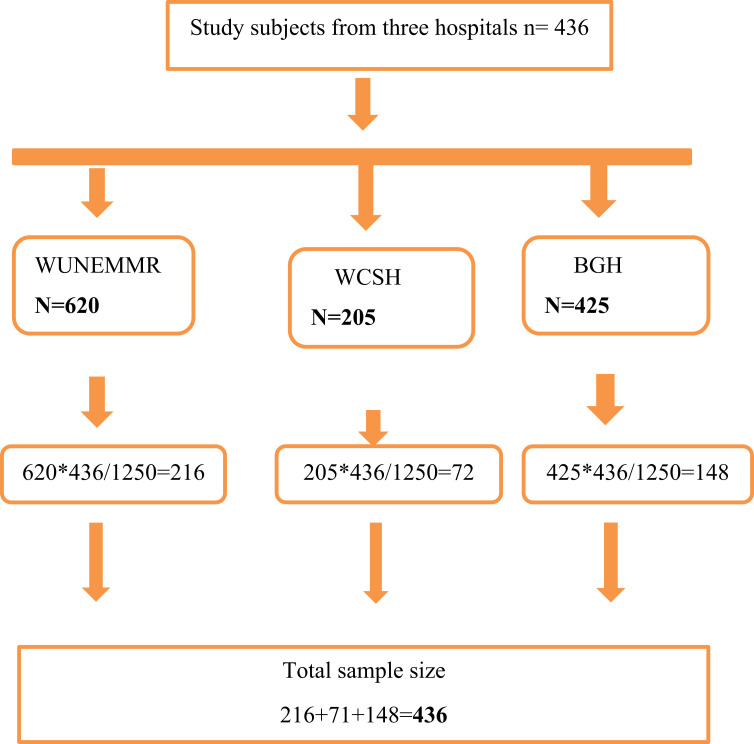
Three hospitals were selected from the public hospitals found in three zones of Southern Ethiopia. The study subjects were taken proportionally from these three hospitals (WUNEMMRH, WCSH and BGH) as shown in the figure below. Then, study participants were selected from each respected hospital by simple random sampling techniques (Figure 1).
Figure 1.
Schematic presentation of sampling procedure for assessing prevalence of anxiety and associated factors among clients on HAART in selected public hospitals of southern Ethiopia, 2021.
Data Collection Procedures and Tools
Data collection was performed by using the structured questionnaire regarding socio-demographic characteristics and medical data related to HIV/AIDS. Hospital anxiety and depression scale (HADS) was used to measure the anxiety level of HIV/AIDS. HADS has 14 items separated into two 7-item sub-scales for anxiety (HAD-A) and 7-item sub-scales for depression (HAD-D). Anxiety was measured by using seven items of (anxiety sub scale) HADS. HAD-A had Cronbach α = 0.89 in the current study.20 Oslo social support scale and HIV perceived stigma scale were used to measure social support and stigma in HIV patients respectively.21,22 The medical data related to HIV/AIDS such as co-morbidities, CD4 count, ART and infection duration were collected from medical records.
Before interviewing the clients, data collectors explained the aim of the study, risks and possible benefits, the right to refuse to participate in the study, and confidentiality issues. After that, those clients who were willing to sign the voluntary consent form were interviewed. At the end of each day, questionnaires were reviewed and cross-checked for completeness, accuracy and consistency by the supervisor and principal investigator. Six diploma and six BSc nurses were reqruited from Hossana, Worabe and Butajira towns for data collection. Three BSc nurses and three nurses with masters were also reqruited for supervision of data collectors.
Operational Definition
Social Support
The Oslo-3 Social Support Scale (OSS-3), which is a three-item scale exploring the number of close friends, perceived level of concern from others and perceived ease of getting help from neighbors, was used to assess the level of social support. A score 3–8, 9–11 and 12–14 was considered as low, medium and high level of social support respectively.22,23
Anxiety
Anxiety was considered when participants scored 11–21 on seven items of (anxiety sub scale) Hospital anxiety and depression scale (HADS).20
Perceived Stigma
Individuals who scored >26 on thirteen items of Perceived stigma scale.21
Substance Use
Current and ever substance use were considered when participants had used at least one of the specified substances in the last three months and used at least one of the specified substances in a lifetime, respectively, by using the adopted alcohol, smoking and substance involvement screening test (ASSIST).24
Income
Extreme poverty: <1.25 USD per day (38*1.25*30=1425 Ethiopian Birr (ETB) per month); poverty: <2 USD but >1.25 USD per day (38*2*30=2280 ETB per month); above poverty line: ≥ 2 USD per day (38*2*30=2280).
Data Quality Control
The questionnaire was prepared in English and then translated into Amharic for data collection and re-translated back into English by language experts. Two days’ training was provided to the data collectors and supervisors on the data collection tools and the data collection procedures. After that, the questionnaire was pre-tested on 5% of the sample size of the study area to ensure its validity. Data collectors were closely supervised by the supervisors and the principal investigator. Completeness of each questionnaire was checked on a daily basis. Double data entry was done by two data clerks and consistency of the entered data was cross-checked by comparing the two separately entered datasets.
Data Processing and Analysis
The collected data were checked for its completeness and cleaned before being entered into the computer. Then, data were coded, cleaned, edited, and entered into EpiData version 3.1 and exported to SPSS window version 22 for analysis. Descriptive statistics were presented in frequency, tables, texts and summary measures.
Bivariate and multivariate analyses were done to see the association between each independent variable and outcome variable by using binary logistic regression. The assumption for binary logistic regression was checked. The goodness of fit was checked by Hosmer-Lemeshow statistic at a p-value of greater than 0.05. All variables with p<0.25 in the bivariate analysis were included in the final model of multivariate analysis in order to control all possible confounders.25 The direction and statistical association were measured by odds ratio with 95% CI. Adjusted odds ratio along with 95% CI was estimated to identify factors associated with work related stress by using multivariate analysis in binary logistic regression. In this study, P-value<0.05 was considered statistically significant.
Patient and Public Involvement
No patients were involved during the development of the research questions, outcome measurement, reporting and study design. Results of this research could not be disseminated to the study participants.
Results
Socio-Demographic Characteristics
A total of 425 respondents were involved, resulting in a response rate of 97.7%. The mean age of the respondents was 35.7 (SD=8.68) years. The majority of participants, 183 (43.1%), were within the age group of 28–37 years. Out of the total 425 study respondents, 248 (58.4%) were females. Almost half of the study participants, 222 (52.2%), were married and about 92 (21.6%) were merchants. Concerning the educational status of the respondents, 106 (24.9%) were able to read and write. The mean estimated monthly household income was 2892.50 ETB. Over half of the respondents, 53.5%, had more than three children (Table 1).
Table 1.
Socio Demographic Characteristics of Respondents Among Clients on HAART in Selected Public Hospitals of Southern Ethiopia, 2021 (N=425)
| Characteristics | Category | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 177 | 41.6 |
| Female | 248 | 58.4 | |
| Age | 18–27 | 82 | 19.3 |
| 28–37 | 183 | 43.1 | |
| 38–47 | 114 | 26.8 | |
| >47 | 46 | 10.8 | |
| Marital status | Single | 149 | 35.1 |
| Married | 222 | 52.2 | |
| Divorced | 32 | 7.5 | |
| Widowed | 22 | 5.2 | |
| Educational status | Unable to read and write | 37 | 8.7 |
| Able to read and write | 106 | 24.9 | |
| Primary (1–8) | 83 | 19.5 | |
| Secondary (9–12) | 96 | 22.6 | |
| Tertiary (college and above) | 103 | 24.2 | |
| Occupation | Housewife | 79 | 18.6 |
| Gov’t employee | 90 | 21.2 | |
| Farmer | 65 | 15.3 | |
| Merchant | 92 | 21.6 | |
| Daily laborer | 58 | 13.6 | |
| Student | 41 | 9.6 | |
| Income | <1425 ETB | 63 | 21.3 |
| 1425–2280 ETB | 51 | 17.2 | |
| >2280 ETB | 182 | 61.5 | |
| Number of children | One | 35 | 12.8 |
| Two | 92 | 33.7 | |
| Three and above | 146 | 53.5 |
Clinical Characteristics of the Respondents
Majority of the respondents, 309 (72.7%), had diagnosed duration of HIV of 0–5 years. Regarding duration of ART treatment, 339 (79.8%) respondents were taking ART for 0–5 years. Most of the respondents, 249 (58.6%), had CD4 counts less than or equal to 500 cells/mL.
Majority of the respondents, 322 (75.8%), disclosed their HIV status to others and 111 (34.6%) disclosed it to their partners. Out of 425 respondents, 26.6% had comorbid conditions and from these 38 (33.6%) and 40 (35.4%) had hypertension and diabetes respectively (Table 2).
Table 2.
Clinical Characterstics of Respondents Among Clients on HAART in Selected Public Hospitals of Southern Ethiopia, 2021 (N=425)
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Diagnosis duration | 0–5 | 309 | 72.7 |
| 6–10 | 101 | 23.8 | |
| ≥11 | 15 | 3.5 | |
| Duration of treatment | 0–5 | 339 | 79.8 |
| 6–10 | 78 | 18.4 | |
| ≥11 | 8 | 1.9 | |
| CD4 count status | <=500 cells/mL | 249 | 58.6 |
| >500 cells/mL | 176 | 41.4 | |
| Stopping ART drug | Yes | 72 | 16.9 |
| No | 353 | 83.1 | |
| Taking ART drug as ordered | Yes | 414 | 97.4 |
| No | 11 | 2.6 | |
| Disclosing HIV status | Yes | 322 | 75.8 |
| No | 103 | 24.2 | |
| To whom disclosed | Partner | 111 | 34.6 |
| Family | 76 | 23.7 | |
| Brother and sisters | 10 | 3.1 | |
| Relatives | 53 | 16.5 | |
| Friends | 21 | 6.5 | |
| Community | 50 | 15.6 | |
| HIV status of the partner | Positive | 234 | 99.6 |
| Negative | 1 | 0.4 | |
| Is the partner on ART | Yes | 215 | 91.9 |
| No | 19 | 8.1 | |
| Comorbid condition | Yes | 113 | 26.6 |
| No | 312 | 73.4 | |
| Which comorbid condition | Hypertension | 38 | 33.6 |
| Diabetes | 40 | 35.4 | |
| Epilepsy | 4 | 3.5 | |
| Asthma | 24 | 21.2 | |
| Others | 7 | 6.2 |
Note: NB others: tuberculosis and hepatitis.
Psychosocial and Substance Use Related Characteristics
Regarding respondents’ social support, most of the respondents, 139 (32.7%), had poor social support and 66 (15.5%) had good social support. Out of 425 respondents, 99 (23.3%) of the respondents used substances in the last 3 months, of which 67 (67.7%) drank alcohol and 25 (25.3%) chew khat. Concerning perceived stigma, 147 (34.6%) of the respondents had perceived stigma (Table 3).
Table 3.
Psychosocial and Substance Use Related Characteristics of Respondents Among Clients on HAART in Selected Public Hospitals of Southern Ethiopia, 2021 (N=425)
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Social support | Low | 139 | 32.7 |
| Medium | 220 | 51.8 | |
| High | 66 | 15.5 | |
| Substance use in life | Yes | 157 | 36.9 |
| No | 268 | 63.1 | |
| Which substance | Tobacco | 10 | 6.4 |
| Alcohol | 113 | 72 | |
| Khat | 32 | 20.4 | |
| Others | 2 | 1.2 | |
| Substance use in last three months | Yes | 99 | 23.3 |
| No | 326 | 76.7 | |
| Which substance | Tobacco | 5 | 5.1 |
| Alcohol | 67 | 67.7 | |
| Chat | 25 | 25.3 | |
| Others | 2 | 2 | |
| Perceived stigma | Yes | 147 | 34.6 |
| No | 278 | 65.4 |
Note: NB others: cocaine and pethidine.
Prevalence of Anxiety
Prevalence of anxiety among clients on HAART in selected public hospitals of three zones of southern Ethiopia was found to be 25.6% (95% CI:21.4–29.6%).
Factors Associated with Anxiety Among Clients on HAART
In bivariate analysis the factors that fulfilled the the minimum requirements (P-value ≤0.25 in this study) were sex, age, marital status, educational status, income, diagnosis time, CD4 count, stopping ART, taking ART as ordered, disclosure, comorbidity, perceived stigma and social support, these factors were entered into multivariate logistic regression for further analysis in order to control confounding effects. The result of multivariate analysis showed that anxiety was significantly associated with sex, marital status, monthly income, comorbidity of HIV and perceived stigma.
According to the result of this study, females were 3.24 times more likely to have anxiety as compared to males (AOR=3.24, 95% CI [1.32, 7.97]). The result of this study showed those widowed were 5.5 times more likely to have anxiety when compared to unmarried (AOR=5.47, 95% CI [1.08, 29.72]. With respect to monthly income, those who had monthly income 1425–2280 ETB were 7.2 times more likely to have anxiety as compared to those who have monthly income >2280 ETB (AOR=7.29, 95% CI [2.55,20.88]). Those who have a comorbid illness were 5.5 times more likely to have anxiety when compared with those who did not have comorbid illness (AOR=5.47, 95% CI [1.92, 15.62]). Also, patients who reported perceived stigma were 8.3 times more likely to have anxiety as compared to patients who did not report perceived stigma (AOR=8.34, 95% CI [3.49, 19.91]) (Table 4).
Table 4.
Bivariate and Multivariate Logistic Regression Analysis of Factors Associated with Anxiety Among Clients on HAART in Selected Public Hospitals of Southern Ethiopia, 2021
| Characteristics | Anxiety | COR 95% CI | AOR 95% CI | |
|---|---|---|---|---|
| Yes | No | |||
| Sex | ||||
| Male | 23 | 154 | 1 | 1 |
| Female | 86 | 162 | 3.55(2.13,5.92) | 3.24 (1.32,7.97)* |
| Age | ||||
| 18–27 | 30 | 52 | 1 | 1 |
| 28–37 | 40 | 143 | 0.49(0.27,0.86) | 1.25(0.35, 4.56) |
| 38–47 | 29 | 85 | 0.59(0.32,1.10) | 0.65(0.13, 3.32) |
| >47 | 10 | 36 | 0.48(0.21,1.11) | 0.44(0.05,3.88) |
| Marital status | ||||
| Single | 44 | 105 | 1 | 1 |
| Married | 34 | 188 | 0.43(0.26,0.72) | 1.21(0.30,4.88) |
| Divorced | 20 | 12 | 3.98(1.79,8,83) | 1.69(0.27,10.52) |
| Widowed | 11 | 11 | 2.39(1.1,5.91) | 5.47 (1.08,29.72)* |
| Educational status | ||||
| Unable to read and write | 16 | 21 | 5.78(2.38,14.02) | 3.31(0.53,20.63) |
| Able to read and write | 40 | 66 | 4.60(2.24,9.43) | 2.70(0.79,9.23) |
| Primary (1–8) | 22 | 61 | 2.74(1.26,5.93) | 1.13(0.34,3.82) |
| Secondary (9–12) | 19 | 77 | 1.87(0.85,4.09 | 0.86(0.21,3.58) |
| Tertiary (college and above) | 12 | 91 | 1 | 1 |
| Monthly income | ||||
| <1425 | 19 | 34 | 4.69(2.27,9.72) | 2.71(0.93,7.95) |
| 1425–2280 | 23 | 32 | 6.04(2.97,12.26) | 7.29 (2.55,20.88)** |
| >2280 | 20 | 168 | 1 | 1 |
| Diagnosis duration | ||||
| 0–5 | 77 | 232 | 1 | 1 |
| 6–10 | 24 | 77 | 0.94(0.56,1.59) | 1.28 (0.48,3.41) |
| ≥11 | 8 | 7 | 3.44(1.21,9.81) | 0.79 (0.11,5.86) |
| CD4 count | ||||
| <=500 | 70 | 179 | 1.37(0.88,2.16) | 1.23 (0.55,2.72) |
| >500 | 39 | 137 | 1 | 1 |
| Have you ever stopped ART | ||||
| Yes | 14 | 58 | 1.53(0.81,2.86) | 0.34 (0.09,1.23) |
| No | 95 | 258 | 1 | 1 |
| Taking ART as ordered | ||||
| Yes | 104 | 310 | 1 | 1 |
| No | 5 | 6 | 2.48(0.74,8.31) | 1.35 (0.22,8.36) |
| Disclosure of HIV status | ||||
| Yes | 70 | 252 | 0.46(0.28,0.74) | 0.32 (0.09,1.13) |
| No | 39 | 64 | 1 | 1 |
| Comorbid condition | ||||
| Yes | 41 | 72 | 2.04(1.28,3.26) | 5.47 (1.92,15.62)* |
| No | 68 | 244 | 1 | 1 |
| Perceived stigma | ||||
| Yes | 71 | 76 | 5.9(3.68,9.45) | 8.34 (3.49,19.91)** |
| No | 38 | 240 | 1 | 1 |
| Social support | ||||
| Low | 54 | 85 | 4.61(2.04,10.39) | 2.30(0.54,9.76) |
| Medium | 47 | 173 | 1.97(0.88,4.41) | .97(0.23,4.09) |
| High | 8 | 58 | 1 | 1 |
Note: NB 1.00 –References, *P value less than 0.05 and **P value less than 0.01.
Discussion
This study aimed to assess the prevalence and associated factors of anxiety among clients on HAART in selected public hospitals of three zones of Southern Ethiopia. The overall prevalence of anxiety in this study was 25.6%. The current result was found to be higher than in studies conducted in Debre Tabor (22.2%) and Hawassa (17.4%).19,26 The current finding was also higher than in previous studies from South Africa,5 Kenya27 and Nigeria.14 The possible reason for the discrepancy might be differences in data collection instruments (tools) used, difference in sample size, study setting and social, economic and cultural differences.
However, it was found to be lower than the study done in Addis Ababa, 32.4%,16 China, 45.6%, and 53.3,28,29 Albania 82.3%,6 and Italy 47%.12 The possible reason for the discrepancy might be difference in outcome measurement instruments (tools), difference in sample size, and socio-cultural differences.1,6,28,29
Regarding associated factors, in this study, females were 3.24 times more likely to develop anxiety as compared to males, which was supported by previously conducted studies in Debre Tabor,19 Hawassa,26 Addis Ababa,16 and India.30 The possible reason might be social factors like burden of household responsibilities and low social network, exposure to acute life and other biological factors may contribute to the higher prevalence of anxiety among females than males. This finding revealed that female clients living with HIV/AIDS need early detection and screening, health education and counseling session and social support.28,31
When anxiety was in relation to being widowed, those who were widowed were more likely to have anxiety as compared to those who were unmarried. One of the effects of being widowed was lack of help from partners and financial/economic hardship. The possible reason might be current financial hardship, economic independence, low self-confidence, the responsibility of taking care of the children and family and fear of disclosing their status to family members due to concerns of losing social and economic support. This finding revealed that people living with HIV/AIDS need active social networks, getting help from others and economic and social support.18
The result of the present study revealed that the prevalence of anxiety was significantly associated with monthly income. Those who had monthly income 1425–2280 ETB were 7.2 times more likely to have anxiety as compared to those who have monthly income >2280 ETB. Low income or poverty has been shown to be directly related to psychological distress and mental health. The possible reason might be that low monthly income can cause multiple kinds of stress related to food and fuel poverty, debt, and restricted social opportunities affecting family relationships, harming physical and mental health.32,33
Perceived stigma was another significantly associated variable in which those participants with poor perceived stigma were more than eight times (AOR=8.34, 95% CI: (3.49, 19.91) more likely to have anxiety as compared to their counterparts. This finding is consistent with studies conducted in Debre Tabor,19 Hawassa26 and Albania 82.3%.6 Different previously conducted studies indicate that HIV/AIDS related perceived stigma has mental health impact such as feelings of helplessness and worthlessness, mental distress and poor attention and concentration. This can be explained as poor HIV/AIDS related knowledge.18,19
The result of the present study also revealed that the prevalence of anxiety was significantly associated with presence of comorbid condition. Anxiety was about 5.5 times higher among patients who reported having comorbid illness as compared with those who had no comorbid illness. The possible reason might be drug-drug interaction, increased adverse effects, co-infection and risk of hospitalization leading to high level of stigma and discrimination which may lead to high rate of anxiety. The implication of this finding indicates that people living with HIV/AIDS need strong adherence counseling, active social networks and early detection, and treatment so that they can cope better with the signs and symptoms of their illness as well as forthcoming complications.34,35
Limitations and Strengths of the Study
In this study we used a validated and standardized tool to assess variables. In addition, this study addressed potential confounding variables like comorbid condition, which has not been covered by other previous studies.
Since the study was conducted using face-to-face interviews, there may be a possibility of social desirability bias. Possibility of recall bias exists as some of the factors were assessed based on past history. Furthermore, some factors such as side effects of ART medications were not addressed in this study.
Conclusion
It was found that a significant number, one-fourth, of the study participants experienced considerable level of anxiety. There were multiple factors significantly associated with anxiety such as sex, marital status, income, comorbid illness and perceived stigma. Interventions that focus on reducing anxiety due to HIV/AIDS are recommended. Regular mental health assessment and identification of risk factors of anxiety among clients on HAART may help to address the problem.
Acknowledgments
We acknowledge the entire staff of the hospitals for their cooperation in making this study a success. We also appreciate the study participants for their cooperation in providing the necessary information.
Funding Statement
Funding for this study was provided by Haramaya University. The funder has no direct contribution to the study except funding the research work. Award/Grant numbers are not applicable.
Abbreviations
AOR, Adjusted Odds Ratio; COR, Crude Odds Ratio; CI, Confidence Interval; AIDS, Acquired Immune Deficiency Syndrome; APA, American Psychiatric Association; ART, Anti-Retroviral Treatment; BGH, Butajira General Hospital; GAD, Generalized Anxiety Disorder; HAART, Highly Active Anti-Retroviral Treatment; HADS, Hospital Anxiety and Depression Scale; HIV, Human Immune Deficiency Virus; MHS, Moderate to High Risk for Suicide; OR, Odds Ratio; OSSS, Oslo Social Support Scale; PLWHA, People Living With HIV/AIDS; SNNPR, Southern Nations Nationalities and People Ethiopia; WCSH, Worabe Comprehensive Specialized Hospital; WHO, World Health Organization; WUNEMMSH, Wachemo University Nigist Elleni Mohammed Memorial Specialized Hospital.
Data Sharing Statement
The datasets used and analyzed in the current study are included within the article.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) Haramaya University, College of Health and Medical Sciences with Ethics approval number of IHRERC/074/2021. In addition, support letter was written to the hospitals. The objective and purpose of the study were explained briefly to the study participants and confidentiality was assured. Finally, written informed consent was obtained from study participants before conducting the interview. This study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Shukla M, Agarwal M, Singh J, Srivastava A. Anxiety among people living with HIV/AIDS on antiretroviral treatment attending tertiary care hospitals in Lucknow, Uttar Pradesh, India. Int J Inn Res Med Sci. 2016;2897–2901. doi: 10.18203/2320-6012.ijrms20161973 [DOI] [Google Scholar]
- 2.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders, a systematic review and meta-regression. Psychol Med. 2013;43(5):897–910. doi: 10.1017/S003329171200147X [DOI] [PubMed] [Google Scholar]
- 3.Shacham E, Morgan JC, Önen NF, Taniguchi T, Overton ET. Screening Anxiety in the HIV Clinic. AIDS Behav. 2012;16(8):2407–2413. doi: 10.1007/s10461-012-0238-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Justice AC, McGinnis KA, Atkinson JH, et al. Psychiatric and neurocognitive disorders among HIV-positive and negative veterans in care, Veterans Aging Cohort Five-Site Study. Aids. 2004;18:49–59. doi: 10.1097/00002030-200401001-00008 [DOI] [PubMed] [Google Scholar]
- 5.Pappin M, Wouters E, Booysen FL. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa, a cross-sectional study. BMC Public Health. 2012;12(1):1–9. doi: 10.1186/1471-2458-12-244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrison SD, Banushi VH, Sarnquist C, et al. Levels of self-reported depression and anxiety among HIV-positive patients in Albania, a cross-sectional study. Croat Med J. 2011;52(5):622–628. doi: 10.3325/cmj.2011.52.622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brandt C, Zvolensky MJ, Woods SP, Gonzalez A, Safren SA, O’Cleirigh CM. Anxiety symptoms and disorders among adults living with HIV and AIDS: a critical review and integrative synthesis of the empirical literature. Clin Psychol Rev. 2017;51:164–184. doi: 10.1016/j.cpr.2016.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiltink J, Beutel ME, Till Y, et al. Prevalence of distress, comorbid conditions and well being in the general population. J Affect Disord. 2011;130(3):429–437. doi: 10.1016/j.jad.2010.10.041 [DOI] [PubMed] [Google Scholar]
- 9.Campbell-Sills L, Brown TA. Generalized Anxiety Disorder. The Guilford Press; 2010. [Google Scholar]
- 10.Granich R, Gupta S, Hersh B, et al. Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality burden; 1990–2013. PLoS One. 2015;10(7):e0131353. doi: 10.1371/journal.pone.0131353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UNAIDS P. HIV and AIDS Estimates. Lima, Peru: UNAIDS; 2009. [Google Scholar]
- 12.Celesia B, Coco C, Bisicchia F, et al. Anxiety disorders and adherence to HAART. XVIII International AIDS Conference; 2010. [Google Scholar]
- 13.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–839. doi: 10.1056/NEJMoa1600693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olagunju AT, Adeyemi JD, Erinfolami AR, Ogundipe OA. Factors associated with anxiety disorders among HIV-positive attendees of an HIV clinic in Lagos, Nigeria. Int J STD AIDS. 2012;23(6):389–393. doi: 10.1258/ijsa.2011.011200 [DOI] [PubMed] [Google Scholar]
- 15.Bitew H, Andargie G, Tadesse A, Belete A, Fekadu W, Mekonen T. Suicidal ideation, attempt, and determining factors among HIV/AIDS patients, Ethiopia. Depress Res Treat. 2016;2016:1–6. doi: 10.1155/2016/8913160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tesfaw G, Ayano G, Awoke T, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. 2016;16(1):368. doi: 10.1186/s12888-016-1037-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bravo P, Edwards A, Rollnick S, Elwyn G. Tough decisions faced by people living with HIV, a literature review of psychosocial problems. Aids Rev. 2010;12(2):76–88. [PubMed] [Google Scholar]
- 18.Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India - A community based cross sectional study. BMC Public Health. 2012;12:463. doi: 10.1186/1471-2458-12-463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amsalu B, Gashaw A, Minale T, Tigabu B, Telake A. Prevalence of anxiet y and associated factors among people living with HIV/AIDS at Debretabo r general hospital anti retro viral clinic Debretabor, Amhara, Ethiopia, 2014. J Psychiatry Neurosci. 2014;2(6):109–114. doi: 10.11648/j.ajpn.20140206.15 [DOI] [Google Scholar]
- 20.Lodhi FS, Elsous AM, Irum S, Khan AA, Rabbani U. Psychometric properties of the Urdu version of the Hospital Anxiety and Depression Scale (Hads) among pregnant women in Abbottabad, Pakistan. General Psychiatry. 2020;33:5. doi: 10.1136/gpsych-2020-100276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Emlet CA. Measuring stigma in older and younger adults with HIV/AIDS, an analysis of an HIV stigma scale and initial exploration of subscales. Res Soc Work Pract. 2016;15(4):291–300. doi: 10.1177/1049731504273250 [DOI] [Google Scholar]
- 22.Kocalevent RD, Berg L, Beutel ME, et al. Social support in the general population, standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018;6(1):31. doi: 10.1186/s40359-018-0249-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item Oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malaysia J Psychiatry. 2013;22(2):32–41. [Google Scholar]
- 24.Humeniuk R, Ali R, Babor TF, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x [DOI] [PubMed] [Google Scholar]
- 25.Bendel RB, Afifi AA. Comparison of stopping rules in forward “stepwise” regression. J Am Stat Assoc. 1977;72(357):46–53. [Google Scholar]
- 26.Bedaso A, Belagavi D, Bekele G, Mekonnen N. Factors associated with anxiety disorder among ART clients attending antiretroviral therapy clinic at Hawassa University referral hospital, Hawassa, SNNPR, Ethiopia. J Psychiatry. 2016;20(1):1–5. Page 2 of 5 J Psychiatry, an open access journal ISSN: 2378–5756 individuals and the effect of anxiety on adherence with antiretroviral therapy (ART) and engagement in high risk and health-compromising behaviors remains to be fully elucidated [14]. With increased understanding of this relationship, simple evidence-based interventions can be administered in clinical settings to reduce anxiety [15]. Globally 33 million people were living with HIV/AIDS and 2 million people died from AIDS related causes worldwide, particular in sub-Saharan Africa 22 million people living with HIV and 1.2 million people died from AIDS [16]. Ethiopia; 2016. doi: 10.4172/2378-5756.1000394 [DOI] [Google Scholar]
- 27.Ngssanga P. Prevalence of Anxiety and Depression Among HIV. AIDS Patients Attending the Comprehensive Care Centre (CCC), Kenyatta National Hospital (KNH). University of Nairobi, Kenya; 2013:20. [Google Scholar]
- 28.Liu L, Pang R, Sun W, et al. Functional social support, psychological capital, and depressive and anxiety symptoms among people living with HIV/AIDS employed full-time. BMC Psychiatry. 2013;13(1):324. doi: 10.1186/1471-244X-13-324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Mo PK, Kahler CW, et al. Prevalence and associated factors of depressive and anxiety symptoms among HIV-infected men who have sex with men in China. AIDS Care. 2016;28(4):465–470. doi: 10.1080/09540121.2015.1118430 [DOI] [PubMed] [Google Scholar]
- 30.Ghose T, Chowdhury A, Solomon P, Ali S. Depression and anxiety among HIV-positive sex workers in Kolkata, India, Testing and modifying the hospital anxiety depression scale. Int Soc Work. 2015;58(2):211–222. doi: 10.1177/0020872813497381 [DOI] [Google Scholar]
- 31.Ivanova EL, Hart TA, Wagner AC, Aljassem K, Loutfy MR. Correlates of anxiety in women living with HIV of reproductive age. AIDS Behav. 2012;16(8):2181–2191. doi: 10.1007/s10461-011-0133-6 [DOI] [PubMed] [Google Scholar]
- 32.Dijkstra-Kersten SM, Biesheuvel-Leliefeld KE, van der Wouden JC, Penninx BW, van Marwijk HW. Associations of financial strain and income with depressive and anxiety disorders. J Epidemiol Community Health. 2015;69(7):660–665. doi: 10.1136/jech-2014-205088 [DOI] [PubMed] [Google Scholar]
- 33.Mughal AY, Devadas J, Ardman E, Levis B, Go VF, Gaynes BN. A systematic review of validated screening tools for anxiety disorders and PTSD in low to middle income countries. BMC Psychiatry. 2020;20(1):1–18. doi: 10.1186/s12888-020-02753-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heron JE, Norman SM, Yoo J, et al. The prevalence and risk of non-infectious comorbidities in HIV-infected and non-HIV infected men attending general practice in Australia. PLoS One. 2019;14(10):e0223224. doi: 10.1371/journal.pone.0223224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guaraldi G, Zona S, Brothers TD, et al. Aging with HIV vs. HIV seroconversion at older age: a diverse population with distinct comorbidity profiles. PLoS One. 2015;10(4):e0118531. doi: 10.1371/journal.pone.0118531 [DOI] [PMC free article] [PubMed] [Google Scholar]