Abstract
Aim
Post-COVID-19 syndrome is defined as continuous symptoms related to SARS-CoV-2 infection, which can persist for several weeks or months. Previous studies identified risk factors associated with post-COVID-19 syndrome, including female sex, hypertension, and allergic respiratory diseases. This study aims to investigate the frequency of this syndrome among Arabic patients.
Subject and methods
A cross-sectional study was conducted from March to August 2022. The study included 520 Arabic patients with confirmed COVID-19 diagnosis, who were asked about possible symptoms persisting for ≥28 days.
Results
Twenty-five percent (25%) of the included patients developed post-COVID-19 syndrome. The most common recorded symptoms were cough (32%), anosmia (32%), fatigue (28%), headache (19%), muscle pain (19%), and shortness of breath (17%). It was found that female sex, hospitalization due to initial COVID-19 infection, and the presence of chronic diseases were significant risk factors for developing post-COVID-19 syndrome.
Conclusion
The study recorded post-COVID-19 syndrome among 25% of Arabic participants. Initial COVID-19 hospitalization, initial symptomatic COVID-19, and female sex were significant risk factors for developing post-COVID-19 syndrome.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10389-022-01802-3.
Keywords: Post-COVID-19 syndrome, SARS-CoV-2, Health issues, Risk factors, Chronic symptoms
Introduction
Post-COVID-19 syndrome is defined as continuous symptoms related to SARS-CoV-2 infection, which can persist for several weeks or months (Vehar et al. 2021). Patients with post-COVID-19 syndrome can experience multiple symptoms that may affect different tissues (Yong 2021). These symptoms may include fatigue, muscle pain, low-grade fever, cough, shortness of breath (SOB), chest pain, headache, and cognitive dysfunction (Raveendran et al. 2021; Greenhalgh et al. 2020; Kohale and Wajpeyi 2021). Numerous factors have been identified as risk factors for post-COVID-19 syndrome, including female sex, hypertension, and allergic respiratory diseases (Pazukhina et al. 2022; Kim et al. 2021).
The prevalence of this condition appears to vary considerably, with different symptoms and definitions arising. A previous study of over 4000 confirmed COVID-19 patients from the United Kingdom, the United States of America, and Sweden, reported that 12–16% of patients had symptoms lasting >28 days (Sudre et al. 2021). Other studies revealed that fatigue, shortness of breath, insomnia, and impaired cognitive skills were frequently reported 3-6 months after SARS-CoV-2 infection. In addition, other symptoms, including headache, anosmia, and cough, were reported 6 months after confirmation of COVID-19 (Alkodaymi et al. 2022).
In light of the variable symptoms associated with this syndrome, there may not be single pathogenesis to explain the condition (Gavrilova et al. 2022; Peluso and Deeks 2022). A comprehensive review of this syndrome is important to support these people with appropriate care and prevent further disease transmission. This study aims to investigate the frequency of this syndrome among Arabs with confirmed COVID-19 in Saudi Arabia and explore if it is possible to predict it early in the disease.
Methodology
Study design, sample size, and study participants
A cross-sectional study was conducted from March to August 2022 among Arabic COVID-19 patients. The minimum sample size was calculated using the Cochran formula (n = Z2 P*Q/ d2) (Bujang et al. 2018). Where n = minimum sample size required, Z = standard normal variable, which is 1.96 at a 95% confidence interval, P is the hypothesized proportion of post-COVID-19 syndrome in the population, which is taken as 15% (4), Q = 1-P, d = acceptable margin of error, which is considered as 0.05. Accordingly, we estimated a minimum sample size of 195. The inclusion criteria are Arabic COVID-19 patients aged ≥12 years after 28 days of confirmed infection with SARS-CoV-2.
Data collection
A questionnaire was used to collect data from eligible COVID-19 patients through a telephone call center provided by the Saudi Ministry of Health. The questionnaire was pretested and reviewed for validity (face validity). It consists of three parts related to the background variables of the studied subjects, present medical history, and post-COVID-19 syndrome, including the nature of symptoms and their severity (Additional file 1). Telephone calls were made for randomly selected people from a large electronic file of eligible individuals obtained from the Ministry of Health (MOH) database. People who accepted to participate were asked to answer the questionnaire and describe the existing symptoms to evaluate their severity. When the symptoms were tolerable and there was no need to visit a hospital or an emergency department, and daily activity was either only slightly affected or unaffected, they were recognized as mild/moderate. In contrast, intolerable symptoms requiring hospital or emergency department care and interfering with daily activity were classified as severe.
Statistical analysis
Data organization, management, and analysis were performed using SPSS version 24 software. Background and underlying conditions associated with the development and the severity of post-COVID-19 syndrome were studied using odds ratio (OR) and 95% confidence interval (CI). In addition, Chi-square, Fisher's exact, and logistic regression tests were performed. A P value <0.05 was considered statistically significant.
Results
The study included 520 Arabic people previously infected with COVID-19; 25% of them (N = 130) developed post-COVID-19 syndrome. The most common recorded symptoms were cough (N = 42 [32%]), anosmia (N = 41 [32%]), fatigue (N = 36 [28%]), headache (N = 25 [19%]), muscle pain (N = 25 [19%]), arthritis (N = 24 [18%]), and shortness of breath (N = 22 [17%]).
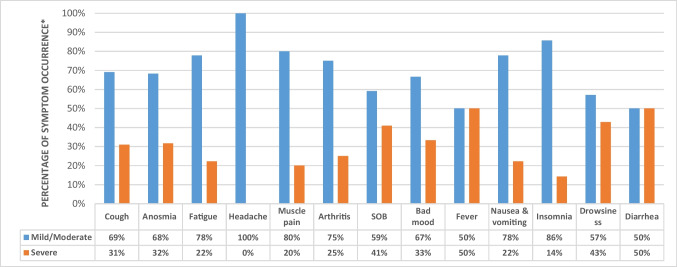
Figure 1 shows the severity of post-COVID-19 syndrome-related symptoms. Of 130 patients with post-COVID-19 syndrome, 50% complained of severe fever and diarrhea. In addition, severe symptoms of cough, anosmia, bad mood, shortness of breath, and drowsiness were presented among 30–40% of those with post-COVID-19 syndrome. Other symptoms, including headache, fatigue, muscle pain, arthritis, nausea, vomiting, and insomnia, were usually mild to moderate.
Fig. 1.
Severity of symptoms of post-COVID-19 syndrome among studied participants. SOB: shortness of breath. *The percentages of mild/moderate and severe events of each symptom were based on the frequencies of post-COVID-19 syndrome-related symptoms among included participants: cough (N = 42), anosmia (N = 41), fatigue (N = 36), headache (N = 25), muscle pain (N = 25), arthritis (N = 24), shortness of breath (N = 22), bad mood (N = 12), fever (N = 12), nausea & vomiting (N = 9), insomnia (N = 7), drowsiness (N = 7), and diarrhea (N = 2)
The possible risk factors for developing post-COVID-19 syndrome are summarized in Table 1. Age was not a significant risk factor (P > 0.05), while female sex showed an increased risk of post-COVID-19 syndrome (OR = 2.08, 95% CI = 1.39-3.11, P < 0.01). Regarding underlying factors, people hospitalized due to severe conditions of COVID-19 were at high risk of COVID-19 syndrome (OR = 6.60, 95% CI = 2.60-16.75, P < 0.01). In addition, the presence of chronic diseases and immunodeficiency also increased the risk of continuous symptoms by 2.3- to 4.4-fold (OR = 2.26, 95% CI = 1.43–3.58, P < 0.01 and OR = 4.38, 95% CI = 1.37–14.06, P < 0.01, respectively). All symptoms reported by the included patients during the initial COVID-19 infection were significant risk factors for developing post-COVID-19 syndrome (P < 0.05). However, logistic regression only showed initial hospitalization, initial symptomatic COVID-19, and female sex as significant risk factors (P < 0.01) (Table 2).
Table 1.
Background and underlying variables associated with post-COVID-19 syndrome among studied participants
| Background and underlying variables | Post-COVID-19 N = 130 |
Non-post-COVID-19 N = 390 |
Total N = 520 |
OR/Fisher's exact | 95% CI, P | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Age group: 12–27 years | 30 | 23.08 | 114 | 29.23 | 144 | 27.69 | 0.73 | 0.46–1.15, 0.18 |
| Age group: 28–50 years | 82 | 63.08 | 233 | 59.74 | 315 | 60.58 | 1.15 | 0.76–1.73, 0.25 |
| Age group: >50 years | 18 | 13.85 | 43 | 11.03 | 61 | 11.73 | 1.30 | 0.72–1.34, 0.19 |
| Females | 71 | 54.62 | 143 | 36.67 | 214 | 41.15 | 2.08 | 1.39–3.11, <0.01 |
| Chronic diseases | 40 | 30.77 | 64 | 16.41 | 104 | 20.00 | 2.26 | 1.43–3.58, <0.01 |
| Immunodeficiency | 7 | 5.38 | 5 | 1.28 | 12 | 2.31 | 4.38 | 1.37–14.06, <0.05 |
| Diabetes | 11 | 8.46 | 21 | 5.38 | 32 | 6.15 | 1.62 | 0.76–3.47, 0.10 |
| Hypertension | 11 | 8.46 | 16 | 4.10 | 27 | 5.19 | 2.16 | 1.0–4.78, <0.05 |
| Asthma | 7 | 5.38 | 13 | 3.33 | 20 | 3.85 | 1.65 | 0.64–4.23, 0.15 |
| Allergy | 7 | 5.38 | 10 | 2.56 | 17 | 3.27 | 2.16 | 0.81–5.80, 0.06 |
| Cardiovascular | 6 | 4.62 | 10 | 2.56 | 16 | 3.08 | 1.84 | 0.66–5.16, 0.12 |
| Others | 7 | 5.38 | 23 | 5.90 | 30 | 5.77 | 0.91 | 0.38–2.17, 0.41 |
| Asymptomatic COVID-19 | 3 | 2.31 | 71 | 18.21 | 74 | 14.23 | 0.11 | 0.03–0.34, <0.01 |
| Initial symptomatic COVID-19 | 127 | 97.69 | 319 | 81.79 | 446 | 85.77 | 9.42 | 2.91–30.46, <0.01 |
| Hospitalized | 14 | 10.77 | 7 | 1.79 | 21 | 4.04 | 6.60 | 2.60–16.75, <0.01 |
| Intensive care | 7 | 5.38 | 0 | 0 | 7 | 1.35 | – | < 0.01* |
*Fisher's exact performed
Table 2.
Logistic regression regarding incidence of post-COVID-19 syndrome in the presence of specific factors (sex, immunodeficiency, initial symptomatic COVID-19, chronic disease, and hospitalization)
| Dependent variable: Post-COVID-19 syndrome | ||
|---|---|---|
| Factor | Exp(B) | 95% CI for Exp(B), P value |
| Male | 0.490 | 0.321–0.748, <0.01 |
| Immunodeficiency | 1.977 | 0.521–7.500, 0.316 |
| Initial symptomatic COVID-19 | 7.729 | 2.373–25.172, <0.01 |
| Chronic disease | 1.606 | 0.974–2.648, 0.063 |
| Hospitalized | 4.370 | 1.596–11.966, <0.01 |
Table 3 shows the OR regarding the development of post-COVID-19 syndrome relative to the symptoms of the initial COVID-19 infection among studied groups (post-COVID-19 versus non-post-COVID-19 syndrome). Anosmia and shortness of breathing during initial COVID-19 infection increase the risk of developing post-COVID-19 syndrome by 2–3-fold (OR = 3.10, CI = 1.36–7.05, P < 0.01, OR = 2.16, CI = 1.00–4.81, P < 0.05, respectively). Other reported symptoms of the initial COVID-19 infection were not significant risk factors affecting the development of post-COVID-19 syndrome (P > 0.05).
Table 3.
Odds ratio regarding the development of post-COVID-19 syndrome relative to the symptoms of the initial COVID-19 infection among studied groups (post-COVID-19 vs. non-post-COVID-19 syndrome)
| Initial COVID symptoms | Post-COVID-19 N = 130 |
Non-post-COVID-19 N = 390 |
Total N = 520 |
OR | 95% CI, P | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Fever | 103 | 79.23 | 226 | 57.95 | 329 | 63.27 | 2.77 | 1.73–4.43, <0.01 |
| Headache | 82 | 63.08 | 161 | 41.28 | 243 | 46.73 | 2.43 | 1.161–3.66, <0.01 |
| Fatigue | 80 | 61.54 | 171 | 43.85 | 251 | 48.27 | 2.05 | 1.37–3.08, <0.01 |
| Cough | 77 | 59.23 | 153 | 39.23 | 230 | 44.23 | 2.25 | 1.50–3.37, <0.01 |
| Muscle pain | 76 | 58.46 | 126 | 32.31 | 202 | 38.85 | 2.95 | 1.96–4.44, <0.01 |
| Anosmia | 56 | 43.08 | 90 | 23.08 | 146 | 28.08 | 2.52 | 1.66–3.84, <0.01 |
| Arthritis | 66 | 50.77 | 109 | 27.95 | 175 | 33.65 | 2.66 | 1.77–4.00, <0.01 |
| Shortness of breath | 49 | 37.69 | 57 | 14.62 | 106 | 20.38 | 3.53 | 2.25–5.56, <0.01 |
| Diarrhea | 16 | 12.31 | 28 | 7.18 | 44 | 8.46 | 1.81 | 0.95–3.47, <0.05 |
| Nausea/vomiting | 18 | 13.85 | 32 | 8.21 | 50 | 9.62 | 1.80 | 0.97–3.33, <0.05 |
| Insomnia | 23 | 17.69 | 14 | 3.59 | 37 | 7.12 | 5.77 | 2.87–11.61, <0.01 |
| Bad mood | 14 | 10.77 | 21 | 5.38 | 35 | 6.73 | 2.12 | 1.05–4.30, <0.05 |
| Drowsiness | 13 | 10.00 | 8 | 2.05 | 21 | 4.04 | 5.31 | 2.15–13.11, <0.01 |
Discussion
The persistence of symptoms related to SARS-CoV-2 infection is a global public health issue. Most people recovered from COVID-19 completely within a few days (Catton and Gardner 2022). However, some patients experienced mild to severe symptoms lasting for ≥28 days after their initial recovery (Hull et al. 2022).
Although the UK National Institute for Health and Care Excellence (NICE) defines post-COVID-19 syndrome as a disease with symptoms lasting 12 weeks or more (Nguyen et al. 2022), Mayo Clinic, an American academic medical center, defines post-COVID-19 syndrome as ongoing or returning symptoms experienced for ≥4 weeks after confirmed infection with SARS-CoV-2 (Mayo Clinic 2022).
The current study aimed to estimate the prevalence of post-COVID-19 syndrome (based on the Mayo Clinic definition) and its associated risk factors among Arabic patients with COVID-19. It was found that 25% of the studied participants developed post-COVID-19 syndrome. Other studies conducted by Augustin et al. and AlRadini et al. found that 28% and 22.5% of COVID-19 patients in Germany and Saudi Arabia, respectively, had continuous symptoms for more than 4 weeks post-infection, which are more or less similar to the current study (Augustin et al. 2021; AlRadini et al. 2022). On the other hand, Fernández-de-las-Peñas et al. and Bell et al. showed that 63% and 69% of Spanish and American people, respectively, complained of post-COVID-19 symptoms 30 days after the infection (Fernández-de-Las-Peñas et al. 2021; Bell et al. 2021). The variation in the prevalence between those studies could be attributed to the difference in the sample size and genetic variation between different ethnic groups (Xu et al. 2022).
Although some researchers, including Almasri et al. (2022) and Sudre et al. (2021), found that increasing age is significantly correlated with the occurrence of post-COVID-19 syndrome, the current study did not find this association to be significant. Concerning sex, our study, along with several other studies, confirmed that female sex is a factor that increases the risk of long COVID-19 symptoms (Fernández-de-Las-Peñas et al. 2022a; Yong 2021; Fernández-de-Las-Peñas et al. 2022b).
More than four studies concluded that initial symptoms of COVID-19 infection are not significantly associated with post-COVID-19 syndrome (Townsend et al. 2021; Darawshy et al. 2022; Stengel et al. 2021; Townsend et al. 2020; Miyazato et al. 2020). However, the current study revealed that several symptoms, mainly insomnia, drowsiness, and shortness of breath, are risk factors for long COVID-19 symptoms, with odds ratios >3.
A recent study discussed six subtypes of post-COVID-19 syndrome, including non-severe COVID-19 multi-organ sequelae (NSC-MOS), pulmonary fibrosis sequelae (PFS), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), postural orthostatic tachycardia syndrome (POTS), post-intensive care syndrome (PICS), and medical or clinical sequelae (MCS) (Yong and Liu 2022). However, in the current study, the researchers could not categorize the included participants with post-COVID-19 syndrome into these six subtypes due to the lack of objective data and complete medical evaluation. In addition, this study did not assess the quality of life of patients with post-COVID-19 syndrome, while several other studies have discussed this issue.
Four studies evaluated and followed up on the quality of life of people with persistent COVID-19 symptoms using the EuroQol visual analog scale (EQ-VAS) and EuroQoL 5-dimensions 5-level scale (EQ-5D-5L) (Halpin et al. 2021; Taboada et al. 2021; Jacobs et al. 2020; Carfì et al. 2020). The prevalence of poor quality of life revealed by these studies ranged from 23% to 67%. Another four studies conducted by Mandal et al. (2021), Huang et al. (2021), Garrigues et al. (2020), and Moreno-Pérez et al. (2021) showed that the mean values for EQ-VAS among included participants with post-COVID-19 symptoms ranged from 70 to 90. Based on these eight studies, many people with persistent symptoms could have acceptable quality of life, and several minor symptoms might be tolerable and not affect the day’s activities. Nevertheless, Malik et al. (2022) revealed that long-lasting fatigue and intensive care admission after COVID-19 recovery were strongly associated with poor quality of life.
In summary, this study recorded post-COVID-19 syndrome in 25% of the studied Arabic participants. Initial COVID-19 hospitalization, initial symptomatic COVID-19, and female sex were significant risk factors for developing post-COVID-19 syndrome.
Limitations
The current study has several limitations, including the cross-sectional study design with the subjective assessment of symptoms, which could be associated with recall bias or underestimating symptoms. In addition, the correlation between the development of the syndrome and the history of COVID-19 vaccination and laboratory values relative to COVID-19 were not evaluated. Furthermore, several associated factors discussed in this study had small effect sizes.
Supplementary information
(DOCX 13 kb)
Authors’ contributions
NM, N.R, and AK contributed to the study conception and design. Data cleaning and data analysis were performed by AK, MH, EE, AQ, and AH. The first draft of the manuscript was written by AK, AF, and AF. NM, NR, and KA contributed in writing—review and editing. AK, SQ, and AH contributed in resources. All authors commented on previous versions of the manuscript. All authors read, reviewed, and approved the final manuscript.
Funding
This paper was not funded.
Data availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
Declarations
Ethical approval and consent to participate
The confidentially and anonymity of the participants’ data were preserved. The questionnaire includes a note explaining that answering and submitting the questionnaire are considered as acceptance to participate.
Ethical consideration
The study was reviewed and approved by the Central Institutional Review Board (IRB) at the Saudi Ministry of Health (IRB Log Number: 22-20 M). The confidentially and anonymity of the participants’ data were preserved. The electronic questionnaire includes a note explaining that answering and submitting the questionnaire are considered as acceptance to participate.
Consent for participation
Consent for participation was taken.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alkodaymi MS, Omrani OA, Fawzy NA, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022;28:657–666. doi: 10.1016/j.cmi.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almasri MS, Alqaisi R, Al-Shagahin M, Al-Kubaisy W, Aljarajreh A, Al-Shagahin H. Risk factors and characterization of post-COVID-19 syndrome in Jordan. Iproceedings. 2022;8:e36563. doi: 10.5281/zenodo.5208019. [DOI] [Google Scholar]
- AlRadini FA, Alamri F, Aljahany MS, Almuzaini Y, Alsofayan Y, Khan A, Albogami N, Abdulrahim M, Almogbil A, Alahmari A. Post-acute COVID-19 condition in Saudi Arabia: A national representative study. J Infect Public Health. 2022;15:526–532. doi: 10.1016/j.jiph.2022.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augustin M, Schommers P, Stecher M, et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Regional Health-Europe. 2021;6:100122. doi: 10.1016/j.lanepe.2021.100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Catalfamo CJ, Farland LV, Ernst KC, Jacobs ET, Klimentidis YC, Jehn M, Pogreba-Brown K. Post-acute sequelae of COVID-19 in a non-hospitalized cohort: results from the Arizona CoVHORT. PLoS One. 2021;16:e0254347. doi: 10.1371/journal.pone.0254347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujang MA, Omar ED, Baharum NA. A review on sample size determination for Cronbach's alpha test: a simple guide for researchers. Malaysian J Med Sci. 2018;25:85–99. doi: 10.21315/mjms2018.25.6.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catton G, Gardner A. Relationship between recovery from COVID-19-induced smell loss and general and Oral health factors. Medicina. 2022;58:283. doi: 10.3390/medicina58020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darawshy F, Abu Rmeileh A, Kuint R, Padawer D, Karim K, Fridlender Z, Laxer U, Goychman Cohen P, Berkman N. Residual symptoms, lung function, and imaging findings in patients recovering from SARS-CoV-2 infection. Intern Emerg Med. 2022;17:1491–1501. doi: 10.1007/s11739-022-02950-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, Navarro-Santana M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis. Eur J Internal Med. 2021;92:55–70. doi: 10.1016/j.ejim.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-de-Las-Peñas C, dela Llave-Rincón AI, Ortega-Santiago R, et al. Prevalence and risk factors of musculoskeletal pain symptoms as long-term post-COVID sequelae in hospitalized COVID-19 survivors: a multicenter study. Pain. 2022;163:e989–e996. doi: 10.1097/j.pain.0000000000002564. [DOI] [PubMed] [Google Scholar]
- Fernández-de-Las-Peñas C, Martín-Guerrero JD, Pellicer-Valero ÓJ, et al. Female sex is a risk factor associated with long-term post-COVID related-symptoms but not with COVID-19 symptoms: the LONG-COVID-EXP-CM multicenter study. J Clin Med. 2022;11:413. doi: 10.3390/jcm11020413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrigues E, Janvier P, Kherabi Y, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Inf Secur. 2020;81:e4–e6. doi: 10.1016/j.jinf.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavrilova N, Soprun L, Lukashenko M, Ryabkova V, Fedotkina TV, Churilov LP, Shoenfeld Y. New clinical phenotype of the post-Covid syndrome: fibromyalgia and joint hypermobility condition. Pathophysiology. 2022;29:24–29. doi: 10.3390/pathophysiology29010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, Walshaw C, Kemp S, Corrado J, Singh R, Collins T, O'Connor RJ, Sivan M. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2021;93:1013–1022. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull JH, Wootten M, Moghal M, Heron N, Martin R, Walsted ES, Biswas A, Loosemore M, Elliott N, Ranson C. Clinical patterns, recovery time and prolonged impact of COVID-19 illness in international athletes: the UK experience. Br J Sports Med. 2022;56:4–11. doi: 10.1136/bjsports-2021-104392. [DOI] [PubMed] [Google Scholar]
- Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, Nyirenda T, Friedman T, Gupta A, Rasouli L, Zetkulic M, Balani B, Ogedegbe C, Bawa H, Berrol L, Qureshi N, Aschner JL. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020;15:e0243882. doi: 10.1371/journal.pone.0243882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S, Jung CG, Lee JY, Kim G, Choi SW, Jin HJ, Park HK. Characterization of asthma and risk factors for delayed SARS-CoV-2 clearance in adult COVID-19 inpatients in Daegu. Allergy. 2021;76:918–921. doi: 10.1111/all.14609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohale SS, Wajpeyi SM. Management of Post Covid Symptoms through Ayurveda– a case study. Drugs and cell therapies. Hematology. 2021;10:3475–3482. [Google Scholar]
- Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, Patel U. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-a systematic review and meta-analysis. J Med Virol. 2022;94:253–262. doi: 10.1002/jmv.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal S, Barnett J, Brill SE, et al. 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021;76:396–398. doi: 10.1136/thoraxjnl-2020-215818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo Clinic (2022) COVID-19: Long-term effects (available at https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351). Accessed 23 Nov 2022
- Miyazato Y, Morioka S, Tsuzuki S, Akashi M, Osanai Y, Tanaka K, Terada M, Suzuki M, Kutsuna S, Saito S, Hayakawa K, Ohmagari N. Prolonged and late-onset symptoms of coronavirus disease 2019. Open Forum Infect Dis. 2020;7:ofaa507. doi: 10.1093/ofid/ofaa507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno-Pérez O, Merino E, Leon-Ramirez JM, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: a Mediterranean cohort study. J Inf Secur. 2021;82:378–383. doi: 10.1016/j.jinf.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen NN, Hoang VT, Dao TL, Dudouet P, Eldin C, Gautret P. Clinical patterns of somatic symptoms in patients suffering from post-acute long COVID: a systematic review. Eur J Clin Microbiol Infect Dis. 2022;41:515–545. doi: 10.1007/s10096-022-04417-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pazukhina E, Andreeva M, Spiridonova E, et al. Prevalence and risk factors of post-COVID-19 condition in adults and children at 6 and 12 months after hospital discharge: a prospective, cohort study in Moscow (stop COVID) BMC Med. 2022;20:244. doi: 10.1186/s12916-022-02448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peluso MJ, Deeks SG. Early clues regarding the pathogenesis of long-COVID. Trends Immunol. 2022;43:268–270. doi: 10.1016/j.it.2022.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndrome. 2021;15:869–875. doi: 10.1016/j.dsx.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stengel A, Malek N, Zipfel S, Goepel S. Long haulers-what is the evidence for post-COVID fatigue? Front Psychiat. 2021;12:677934. doi: 10.3389/fpsyt.2021.677934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taboada M, Moreno E, Cariñena A, Rey T, Pita-Romero R, Leal S, Sanduende Y, Rodríguez A, Nieto C, Vilas E, Ochoa M, Cid M, Seoane-Pillado T. Quality of life, functional status, and persistent symptoms after intensive care of COVID-19 patients. Br J Anaesth. 2021;126:e110–e113. doi: 10.1016/j.bja.2020.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Dyer AH, Jones K, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One. 2020;15:e0240784. doi: 10.1371/journal.pone.0240784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Dowds J, O'Brien K, et al. Persistent poor health after COVID-19 is not associated with respiratory complications or initial disease severity. Annals Am Thoracic Soc. 2021;18:997–1003. doi: 10.1513/AnnalsATS.202009-1175OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vehar S, Boushra M, Ntiamoah P, Biehl M. Post-acute sequelae of SARS-CoV-2 infection: caring for the 'long-haulers'. Cleve Clin J Med. 2021;88:267–272. doi: 10.3949/ccjm.88a.21010. [DOI] [PubMed] [Google Scholar]
- Xu Y, Gao R, Zhu G, Zhou S, Li H, Su W, Han G, Wang R. Genetic variation of allergic disease is associated with the susceptibility to COVID-19. J Inf Secur. 2022;84:e92–e93. doi: 10.1016/j.jinf.2022.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis Ther. 2021;53:737–754. doi: 10.1080/23744235.2021.1924397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong SJ, Liu S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev Med Virol. 2022;32:e2315. doi: 10.1002/rmv.2315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 13 kb)
Data Availability Statement
The data that support the findings of this study are available from the corresponding authors upon reasonable request.