Abstract
Hemolytic uremic syndrome (HUS) is associated with intestinal infection by enterohemorrhagic Escherichia coli strains that produce Shiga toxins. Globotriaosylceramide (Gb3) is the functional receptor for Shiga toxin, and tumor necrosis factor alpha (TNF-α) upregulates Gb3 in both human macrovascular umbilical vein endothelial cells and human microvascular brain endothelial cells. TNF-α treatment enhanced Shiga toxin binding and sensitivity to toxin. This upregulation was specific for Gb3 species containing normal fatty acids (NFA). Central nervous system (CNS) pathology in HUS could involve cytokine-stimulated elevation of endothelial NFA-Gb3 levels. Differential expression of Gb3 species may be a critical determinant of Shiga toxin toxicity and of CNS involvement in HUS.
Enteric infection by Shiga toxin-producing enterohemorrhagic Escherichia coli (EHEC) is associated with bloody diarrhea and, in some cases, systemic complications including hemolytic uremic syndrome (HUS). Although the triad of hemolytic anemia, acute renal failure, and thrombocytopenia define HUS, central nervous system (CNS) involvement is often a major complication (8, 32, 34). Signs of severe CNS involvement are associated with high mortality (41) and, because modern therapy compensates for renal failure, with the majority of deaths due to HUS (22).
During EHEC infection, Shiga toxin is thought to move into the blood through the inflamed intestinal mucosa. The thrombotic microangiopathic damage characteristic of HUS is thought to result from direct cytotoxic effects of circulating Shiga toxin on the vascular endothelium (17, 36). Shiga toxin, with one central A subunit surrounded by five B subunits, inhibits protein synthesis in eukaryotic cells through the action of the A subunit on the ribosome. The B subunits of the toxin bind specifically to the galactosyl-α1,4-galactose (Galα1, 4Gal) linkage found in a globotriaosylceramide (Gb3) located on the surface of endothelial cells. Thus, expression of Gb3, the receptor for Shiga toxin, in endothelial cells is thought to relate to their susceptibility to Shiga toxin.
EHEC infection may also result in absorption of lipopolysaccharide, an endotoxin known to stimulate production of tumor necrosis factor alpha (TNF-α) and other inflammatory cytokines. Shiga toxin itself may stimulate local production of cytokines in some tissues (35). TNF-α and Shiga toxin synergistically affect human umbilical vein endothelial cells (HUVEC) (21). In cultured HUVEC, TNF-α increases the concentration of Gb3 (26, 37) along with the cells' sensitivity to Shiga toxin (18).
Cultured human renal endothelial cells, which are microvascular in origin, were reported in 1993 to contain appreciably more glycolipid than macrovascular HUVEC and to be far more sensitive to Shiga toxin injury than were cultured HUVEC (26). However, a reexamination of this phenomenon with highly purified and characterized glomerular endothelial cells indicated that glomerular endothelial cells are closer to HUVEC in glycolipid content, sensitivity to toxin, and response to TNF-α than was originally reported (38). The earlier preparations may have included other renal cell populations with high Gb3 content and, therefore, elevated sensitivity to Shiga toxin (10, 11, 33).
The renal microangiopathy characteristic of HUS is thought to result directly from Shiga toxin damage to kidney cells and to be a direct consequence of high Gb3 levels. This microangiopathy is thought to lead to coagulation within the glomerulus and renal failure. Hemolytic anemia and thrombocytopenia are also thought to result from endothelial microangiopathy. In contrast, there is no consensus on the pathogenic mechanisms of brain involvement in HUS; CNS damage has not been linked directly to cerebral coagulopathy (27). We hypothesize that a common pathogenic event in both kidney and CNS is Shiga toxin damage to endothelial cells, magnified by upregulation of cell surface Gb3 in response to TNF-α.
Toxin binding can be affected by factors other than the total amount of Gb3, including the type of fatty acyl moieties contained within Gb3 (i.e., the Gb3 species) (29) and the characteristics of the microenvironment in which the glycolipid is anchored (2, 3, 40). Toxin binding is also different in different endothelial cell types. For example, Jacewicz et al. have reported that transformed human intestinal microvascular endothelial cells are more sensitive to Shiga toxin than are macrovascular endothelial cells from human saphenous vein (14). In contrast, human brain microvascular endothelial cells are more resistant to Shiga toxin, but their sensitivity increases significantly in response to cytokines (31).
Human brain microvascular endothelial cells, which are essential constituents of the blood-brain barrier, form a network of complex tight junctions while permitting asymmetric transport and vesicular transcytosis (16, 28). Lacking fenestrations, these specialized cells, strategically located at the interface between blood and brain, are actively involved in maintaining homeostasis of the CNS.
In HUS, endothelial damage by Shiga toxin could result in CNS pathology as a consequence of loss of homeostasis, direct nerve cell damage by Shiga toxin crossing the blood-brain barrier, and/or production of toxic mediators by endothelial cells. Pathologic events could occur at toxin levels that cause endothelial cell dysfunction or individual cell death without triggering frank widespread endothelial necrosis and intravascular thrombosis. Although vascular occlusions due to thrombosis might sometimes cause cerebral ischemia, the critical common event in CNS involvement during HUS could be damage that occurs early and at low Shiga toxin levels.
To test this hypothesis on the neuropathology of HUS, the effects of TNF-α and Shiga toxin on human brain endothelial cells (HBEC) were studied and compared with results obtained in the more commonly used HUVEC model. Specifically, we investigated whether the increased sensitivity caused by TNF-α in microvascular HBEC is mediated by elevated Gb3 levels, as it is in macrovascular HUVEC. Using both cell types, we also determined whether normal fatty acyl (NFA) or hydroxylated fatty acyl (HFA) species of Gb3 are more strongly associated with increased sensitivity.
HUVEC were isolated from one to four human umbilical vein segments by collagenase digestion as described previously (7). HBEC were obtained from fresh autopsied brains and processed as described previously (5, 39). Once the cultures were established, their cerebral endothelial nature was confirmed morphologically and by the presence of factor VIII antigen. The cells in these experiments were between passages 2 and 3.
Shiga toxin was purified from a sonic extract of Shigella dysenteriae serotype 1 strain 60R (30). Purity was confirmed with silver staining, and the specific activity was confirmed in a HeLa cell assay system.
Confluent HUVEC were treated with Shiga toxin alone or in combination with either TNF-α or interleukin-4 (IL-4). Shiga toxin, TNF-α, and IL-4 were diluted in the appropriate growth media before their addition to cell cultures. Cell cultures were examined for morphological changes using an inverted phase-contrast microscope.
For tests of Shiga toxin binding to HUVEC, purified toxin was iodinated with 125I-labeled sodium iodide (New England Nuclear, Boston, Mass.) by the solid-phase lactoperoxidase and glucose oxidase technique (Enzymobead, Bio-Rad, Hercules, Calif.). The radioiodinated toxin was separated from the reaction products on a Bio-Gel (Bio-Rad) P-6 column. Binding to HUVEC was quantitated as previously described (15). Briefly, cells were treated for 72 h with recombinant human TNF-α (500 IU/ml) or vehicle alone and harvested nonenzymatically. Cells (2.5 × 104) were resuspended in 100 μl of medium 199 containing 1% bovine serum albumin with radioiodinated Shiga toxin (4 × 10−8 to 10−9 M) with or without 100-fold excess unlabeled toxin. After incubation for 2 h at 4°C, samples were layered over oil [0.2 ml of dibutylphthalate–bis(2-ethylhexyl)phthalate 1.5:1 (vol/vol); Kodak, Rochester, N.Y.] and centrifuged at 12,000 × g for 15 s. Cell pellets (bound fraction) were recovered by cutting off the tube bottom; pellets and supernatants (free fraction) were counted in a γ counter (Beckman 5500B). Each of two experiments was performed in triplicate. Data reduction was performed by linear regression analyses, and significance was tested by the Wilcoxon signed ranks test.
Concentrations of Gb3 species were determined by high-performance liquid chromatography (HPLC). Cultured cells (2 million to 20 million cells) were harvested, rinsed, resuspended in 0.6 ml of distilled water, sonicated, extracted overnight by the addition of 4 volumes of methanol and then 8 volumes of chloroform, and filtered. The filtrate was analyzed as described previously (24). The perbenzoylated glycolipids were separated by HPLC on a silica column with a hexane-dioxane gradient (1 to 23%) and detected at 229 nm; the peaks were integrated by Dynamax software (Rainin [now Varian Corporation], Walnut Creek, Calif.) and then identified and quantified by comparison with authentic standard glycolipids. This HPLC method resolved each glycolipid type into a peak containing short-chain and any HFA moieties and another peak containing NFA moieties.
For measurement of protein synthesis, HUVEC were incubated with and without cytokine for 48 h, whereupon all media were supplemented with [14C]leucine (0.5 Ci/ml, 1,000 Ci/mmol; New England Nuclear, Boston, Mass.); at 48 h, cells were also supplemented with Shiga toxin and/or additional cytokine. At 72 h, all cells were incubated for 3 h at 37°C with unlabeled medium, whereupon incorporation of label into protein was measured to determine inhibition of protein synthesis in HUVEC. HBEC were likewise treated with or without TNF-α (100 IU/ml) for 48 h and an additional 24 h with logarithmic dilutions of Shiga toxin. The cells were incubated in a methionine-cysteine-free medium with [35S]Met-Cys (specific activity, >1,000 Ci/mmol; ICN Pharmaceutical, Irvine, Calif.) for 3 h at 37°C. At the end of the incubation period, the cells were rinsed and solubilized in detergent, and labeled proteins were precipitated and counted in a scintillation counter (6).
The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay was used to assess cell viability (9, 23). Results were expressed as percent reduction of MTT relative to controls.
Effect of TNF-α on HUVEC Gb3.
TNF-α exerted differential effects on the upregulation of NFA glycolipids and HFA glycolipids. The HFA glycolipid levels were low and were not upregulated by treatment with cytokines. NFA glycolipid levels were initially higher than HFA glycolipid levels; they were significantly increased by treatment with proinflammatory cytokines such as IL-1β and IL-6 (not shown), and especially by TNF-α, but not by others, exemplified by IL-4 (Table 1). Treatment with TNF-α caused a general elevation of NFA glycolipids and a threefold elevation of NFA-Gb3. Furthermore, the ratio of NFA-Gb3 to lactosylceramide increased significantly with TNF-α treatment; the loss of lactosylceramide concurrent with increased Gb3 is consistent with increased activity of the galactose-α1,4-galactosyltransferase responsible for the synthesis of NFA-Gb3 from NFA-lactosylceramide, although other mechanisms are also possible.
TABLE 1.
Effects of cytokine treatment on HUVEC
| Cytokine treatment | Glycosphingolipid level after treatment (amol/cell)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| NFA glycolipid
|
HFA glycolipid
|
|||||||
| Glucosylceramide | Lactosylceramide | Gb3 | Gb4 | Glucosylceramide | Lactosylceramide | Gb3 | Gb4 | |
| Control | 100 | 50 | 60 | 170 | 8 | NDa | 24 | 18 |
| IL-4 | 110 | 50 | 60 | 190 | 9 | ND | 23 | 24 |
| TNF-α | 160 | 90 | 210 | 390 | 9 | ND | 27 | 21 |
ND, not detected; signal to noise was not greater than 5.
TNF-α-mediated sensitivity to Shiga toxin in HUVEC.
This increase in cellular NFA-Gb3 levels was accompanied by increased binding of 125I-labeled Shiga toxin to the TNF-α-treated HUVEC (Fig. 1), supporting our hypothesis that the NFA-Gb3 upregulated by TNF-α is a functional receptor for Shiga toxin in these cells. HUVEC treated for 72 h with TNF-α (500 IU/ml) demonstrated the ability to bind increasing quantities of toxin as the amount of radiolabeled toxin was raised; naive HUVEC showed essentially no binding of radiolabeled Shiga toxin (P = 0.01). The specificity of this binding was determined by the ability of excess unlabeled toxin to displace bound labeled toxin.
FIG. 1.
Shiga toxin binding to HUVEC treated with TNF-α. HUVEC, pretreated with recombinant human TNF-α (500 IU/ml) or vehicle alone, were incubated with 125I-labeled Shiga toxin (1 × 10−9 to 4 × 10−8 M) in the absence or presence of 10−6 M unlabeled toxin. Specific binding is the difference between total binding (in the absence of competing unlabeled toxin) and nonspecific binding (in the presence of excess competing unlabeled toxin). Each value represents the mean (± standard error) of triplicate determinations; these results are representative of two similar experiments. Cells treated with TNF-α show significant, specific, dose-dependent binding by Shiga toxin, while the untreated cells did not show specific binding (P = 0.01), indicating that TNF-α induces the expression of Shiga toxin receptors in these cells.
The functional relevance of this binding was tested directly by measuring protein synthesis in HUVEC (Table 2). Although TNF-α treatment per se depressed protein synthesis slightly, it also rendered HUVEC more susceptible to inhibition of protein synthesis by Shiga toxin. This increased sensitivity caused by TNF-α was both dose and time dependent. The inhibition was noted even when TNF-α exposure for 48 h was followed by 24 h in medium alone, indicating that increased susceptibility to inhibition of protein synthesis did not depend on the presence of TNF-α, but rather was related to the glycolipid accumulation shown in Table 1. Thus, in cells with elevated NFA-Gb3 levels, susceptibility to the effects of Shiga toxin increases significantly. These findings are consistent with previous reports that TNF-α exposure upregulates Gb3 expression and renders HUVEC sensitive to Shiga toxin (26), and they define NFA-Gb3 as the species relevant to toxin sensitivity.
TABLE 2.
Effects of TNF-α and Shiga toxin treatment on HUVEC
| Treatment | Protein synthesisa (% of control) at toxin concn of:
|
|||
|---|---|---|---|---|
| 0 M | 10−10 M | 10−9 M | 10−8 M | |
| Medium (72 h) | 725 ± 16 (100) | 619 ± 30 (85) | 701 ± 13 (97) | 678 ± 13 (94) |
| TNF-α (48 h) + medium (24 h) | 534 ± 16 (74) | 436 ± 14 (60) | 354 ± 7 (49) | 309 ± 16 (43) |
| TNF-α (72 h) | 484 ± 32 (67) | 317 ± 32 (44) | 266 ± 6 (37) | 182 ± 12 (25) |
Protein synthesis (mean ± standard error of three independent experiments) after treatment with TNF-α (100 IU/ml) or Shiga toxin, expressed as 103 cpm of [14C]leucine incorporated per mg of protein.
Effect of TNF-α on HBEC Gb3.
Confluent cultures of HBEC were exposed for 72 h to concentrations of human TNF-α varying from 5 to 1,000 IU/ml, and levels of Gb3 were measured. As in HUVEC, the predominant species of Gb3 were NFA-Gb3, and only the NFA species changed in response to TNF-α. Untreated HBEC contain NFA-Gb3 at 20 amols/cell; TNF-α increased the NFA-Gb3 content in a dose-dependent manner, up to a level of 120 amols/cell at 500-IU/ml TNF-α treatment (Table 3). In a replicate experiment with primary HBEC from a different source, the maximum increase in Gb3 again occurred at 500 IU of TNF-α per ml. Thus, the basal levels of NFA-Gb3 and their upregulation by TNF-α are very similar to those observed in HUVEC.
TABLE 3.
Gb3 expression in TNF-α-treated HBEC
| TNF-α (IU/ml) | Human Gb3 (amol/cell) |
|---|---|
| 0 | 20 |
| 5 | 50 |
| 50 | 70 |
| 500 | 120 |
| 1,000 | 120 |
TNF-α-mediated sensitivity to Shiga toxin in HBEC.
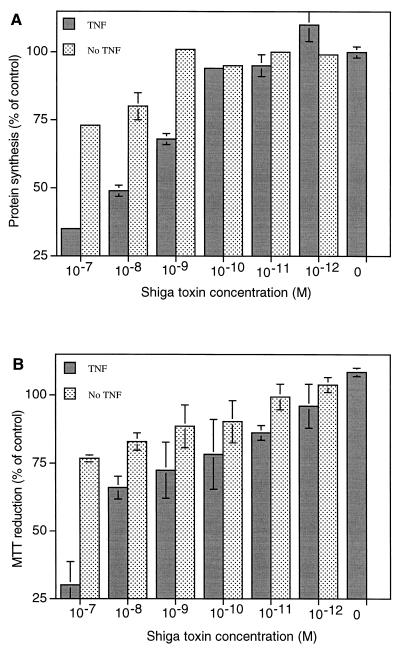
As with HUVEC, the sensitivity of HBEC cultures to toxin increased in parallel with the increases in NFA-Gb3 levels. Confluent HBEC, treated with TNF-α at 100 IU/ml and exposed to 10−7 to 10−12 M Shiga toxin for 24 h, displayed a dose-dependent decrease in protein synthesis (Fig. 2A) and a corresponding decrease in cell viability as measured by reduction of MTT (Fig. 2B). At 10−8 M Shiga toxin, the level of protein synthesis was reduced by 25% and cell viability was 84% of untreated controls.
FIG. 2.
TNF-α treatment increases the sensitivity of HBEC to multiple concentrations of Shiga toxin. HBEC were treated with TNF-α (0 or 100 IU/ml) for 48 h, after which cultures from each group were treated with serial logarithmic dilutions of Shiga toxin from 10−7 to 10−12 M for an additional 24 h. (A) Protein synthesis was determined by [35S]Met-Cys incorporation. (B) Cell viability was determined by MTT assay. Data are means ± standard deviations of triplicate samples at each concentration of Shiga toxin.
To test whether the concentrations of TNF-α (0 to 500 IU/ml) that cause incremental increases of Gb3 levels in HBEC also result in incremental increases in toxin sensitivity, HBEC were exposed for 3 days to TNF-α (5, 100, or 500 IU/ml), with 10−8 M Shiga toxin added for the last 24 h. Exposure to TNF-α resulted in a dose-dependent decrease in the level of protein synthesis (not shown). In a parallel experiment, HBEC were exposed for 4 days to 5, 100, or 500 IU of TNF-α per ml, and 10−8 M Shiga toxin was added for the last 48 h. These cells were examined through an inverted phase-contrast microscope. As the concentration of TNF-α increased, so did the number of round, birefringent, obviously dead or dying cells when also exposed to Shiga toxin (not shown).
HBEC cultures were exposed to various concentrations of Shiga toxin after exposure to TNF-α at 100 IU/ml, a level shown to increase Gb3 expression significantly while remaining within the linear range of doses shown to increase Gb3 expression. In these cells, Shiga toxin caused a dose-dependent decrease in protein synthesis (as assessed by incorporation of [35S]methionine), and the inhibition was stronger than in cells not treated with TNF-α (Fig. 2A). Upon exposure to 10−8 M Shiga toxin, total protein synthesis was reduced by 50%. TNF-α alone did not affect protein synthesis. These cells also displayed a linear dose-dependent increase in sensitivity to logarithmic increases in toxin exposure, and the cells treated with TNF-α were significantly more sensitive to Shiga toxin, as measured by cell viability (Fig. 2B).
Conclusion.
EHEC contains distinct phage genes that encode two major classes of Shiga toxin: Shiga toxin 1 and Shiga toxin 2. The Shiga toxins all contain an enzymatically active A subunit that inhibits protein synthesis at the ribosome, and five B subunits that each bind to glycosphingolipids whose carbohydrate structures contain a Galα1, 4Gal moiety. Gb3 contains Galα1, 4Gal as its nonreducing terminus, and it is thought to be the major functional receptor for both Shiga toxin 1 and the forms of Shiga toxin 2 associated with human disease. The specific mechanism whereby toxin binding and inhibition of protein synthesis results in the pathology associated with HUS is not clear and may vary among endothelia from different tissues. Proposed mechanisms include direct or indirect injury to vascular endothelial cells (4) and, possibly, apoptosis (13).
Lipopolysaccharide (endotoxin) sensitizes HUVEC to Shiga toxin but has no direct cytotoxic effect (20). Lipopolysaccharide is known to induce the production of cytokines, including TNF-α. Cytokines sensitize endothelial cells to Shiga toxin; TNF-α and Shiga toxin are synergistic in their cytotoxic effects on HUVEC (20). TNF-α was found to increase the concentration of total Gb3 in such cells (37).
Clinical evidence for involvement of TNF-α in HUS (i.e., elevated TNF-α in the blood of HUS patients) has been inconsistent because TNF-α has a short half-life and its release can be transient or pulsatile. Therefore, only large, broad studies capturing individuals during transient peaks of cytokine release and at particular stages of infection are likely to consistently find increases in cytokine levels that might be related to the onset of HUS. In an Argentine population of 139 children, the level of TNF-α in the circulation of those infected with EHEC was significantly elevated, over 2.5-fold (3.5 IU/ml of serum) that of controls (19), with values as high as 10 IU/ml. Furthermore, local production of cytokine can augment cytokine in the general circulation (35); we have observed induction of mRNA and protein for both TNF-α and IL-6 by brain endothelial cells in response to Shiga toxin (P. B. Eisenhauer, O. Koul, R. Ventura, J. M. Wells, R. E. Fine, and D. S. Newburg, Abstr. 100th Gen. Meet. Am. Soc. Microbiol. abstr. D-172, 2000). Thus, in our studies the dose-dependent increase of Gb3 levels in HBEC treated with 5 to 500 IU of TNF-α per ml includes physiologically relevant concentrations. Although 5 IU/ml resulted in 2.5-fold elevations of Gb3 (Table 3), we chose 100 IU/ml to investigate these phenomena in endothelial cells to compensate for any loss of activity over the course of the experiments and to optimize our ability to measure significant TNF-α-related changes with as few cells as possible.
Inflammatory cytokines are known to elevate total Gb3 levels in HUVEC (21, 37), but the specific species of Gb3 affected was unknown. Although toxin binds to most species of Gb3 in artificial systems, the avidity of binding differs for different species of Gb3 (29); moreover, different species bind most avidly in different environments (2, 3, 40). The species of Gb3 most likely to be involved in the pathogenesis of HUS is that found in the physiologically relevant environment of the endothelial cell membrane. We found that the majority of the glycolipids of both HBEC and HUVEC are NFA species. In both cell types, levels of the NFA-Gb3 species, unlike HFA-Gb3 species, responded to treatment with TNF-α. The absolute concentrations of NFA-Gb3 in HBEC and HUVEC are quite similar, as is Gb3 upregulation by TNF-α. Likewise, HBEC and HUVEC display similar sensitivity to Shiga toxin in their basal state, and TNF-α treatment of HUVEC and HBEC resulted in specific elevation of NFA-Gb3 that was directly proportional to elevated Shiga toxin binding, to inhibition of protein synthesis, and to Shiga toxin toxicity.
These data are consistent with the hypothesis that the underlying mechanisms of Shiga toxin damage are similar for many endothelial cell types, including HBEC. Infection by EHEC causes cytokines to be elicited into circulation which, along with any locally produced cytokines, results in increased NFA-Gb3 levels in endothelium. These elevated levels of the relevant Gb3 allow Shiga toxin in the bloodstream to bind to target endothelial cells, become internalized, and inhibit cellular function.
We had originally hypothesized that endothelial cells from brain microvasculature might have levels of the relevant Gb3 species high enough to render these cells highly sensitive to Shiga toxin, and thus account for CNS involvement in HUS. However, we found the sensitivity and Gb3 levels of microvascular HBEC to be more comparable to macrovascular HUVEC than to the microvascular endothelial cells from intestine, foreskin, and kidney, which reportedly contain appreciably more glycolipid than do HUVEC (14, 26). These microvascular endothelial cells, in contrast to those from the brain, are more susceptible to Shiga toxin injury than macrovascular endothelial cells by several orders of magnitude (14, 26). These data run counter to our hypothesis that CNS involvement in HUS is due to relatively high sensitivity of cerebral endothelial cells to Shiga toxin; however, it is consistent with clinical findings that coagulopathy is usually absent from the vasculature of brains of HUS patients with severe CNS complications.
This suggests a distinction in the pathophysiology of CNS from that of other tissues such as kidney in HUS based on the differential sensitivity of their endothelial cells to toxin. With even a limited amount of toxin arriving into the circulation from the lumen of the intestine by translocation across intestinal epithelial (1, 12) and endothelial cells (M. Jacewicz, personal communication), the endothelium of intestinal and renal microvascular tissue could be sufficiently damaged to cause the massive overt coagulopathy, the consequent extreme loss of kidney function, and the circulating macroelements of the blood that are pathognomonic for HUS. In the brain, where coagulopathy is not a consistent feature in HUS, Shiga toxin may subtly damage cerebral endothelium without causing overt coagulopathy. Healthy HBEC are essential components of the blood-brain barrier; subtle damage could compromise the tight junctions of the cerebral endothelium, thereby disrupting the blood-brain barrier, resulting in loss of homeostasis of the CNS. Furthermore, subtle damage to HBEC could cause the release of humoral factors that are toxic to the CNS. Finally, Shiga toxin could be transcytosed through the intact blood-brain barrier and subsequently damage any neurons or other cells that express Gb3 and are sensitive to Shiga toxin.
The upregulation by TNF-α of only one type of species, the NFA-Gb3s rather than the HFA-Gb3s, and the association of the NFA-Gb3 species with Shiga toxin binding and toxicity are consistent with our hypothesis (25) that genetic heterogeneity in the expression of Gb3 species may underlie differential susceptibility to HUS. This hypothesis may now be expanded to the involvement of the CNS in HUS, which may depend on heterogeneity in the expression of specific species of Gb3 by the cerebral endothelial cells of individuals. Cerebral endothelial cells isolated from different individuals displayed variation in the absolute amounts of total Gb3 levels (unpublished data); furthermore, the absolute levels of these cells' responses to stimulation varied. We are currently investigating the relationship of native species of Gb3 to sensitivity to Shiga toxin.
Neurologic damage is the most irreversible and untreatable consequence of HUS and occurs in as many as 30% of its victims. Understanding the pathogenesis of CNS involvement in HUS may provide the basis for preventing or ameliorating the devastating CNS damage that occurs in many cases of this syndrome.
Acknowledgments
This work was supported by a REAP grant and a Merit Review Grant from the Veteran's Administration and by NIH grants AG13846, DK52122, and HL36003.
REFERENCES
- 1.Acheson D W K, Moore R, DeBreucker S, Lincicome L, Jacewicz M, Skutelsky E, Keusch G T. Translocation of Shiga toxin across polarized intestinal cells in tissue culture. Infect Immun. 1996;64:3294–3300. doi: 10.1128/iai.64.8.3294-3300.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arab S, Lingwood C A. Influence of phospholipid chain length on verotoxin/globotriaosyl ceramide binding in model membranes: comparison of a supported bilayer film and liposomes. Glycoconj J. 1996;13:159–166. doi: 10.1007/BF00731490. [DOI] [PubMed] [Google Scholar]
- 3.Boyd B, Magnusson G, Zhiuyan Z, Lingwood C A. Lipid modulation of glycolipid receptor function. Availability of Gal(α1-4)Gal disaccharide for verotoxin binding in natural and synthetic glycolipids. Eur J Biochem. 1994;223:873–878. doi: 10.1111/j.1432-1033.1994.tb19064.x. [DOI] [PubMed] [Google Scholar]
- 4.de Chadarevian J P, Kaplan B S. The hemolytic uremic syndrome of childhood. Perspect Pediatr Pathol. 1978;4:465–502. [PubMed] [Google Scholar]
- 5.Eisenhauer P B, Wells J M, McKenna D C, Shanmugaratnam J, Fine R E, Billingslea A M, Long H J, Simons E R, Davies T A. β-APP processing and regulation by interleukin 1 in brain endothelial cells. Alzheimer's Rep. 1998;1:241–247. [Google Scholar]
- 6.Ewenstein B M, Warhol M J, Handin R I, Pober J S. Composition of the von Willebrand factor storage organelle (Weibel-Palade body) isolated from cultured human umbilical vein endothelial cells. J Cell Biol. 1987;104:1423–1433. doi: 10.1083/jcb.104.5.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gimbrone M A., Jr Culture of vascular endothelium. Prog Hemostasis Thromb. 1976;3:1–28. [PubMed] [Google Scholar]
- 8.Hahn J S, Havens P L, Higgins J J, O'Rourke P P, Estroff J A, Strand R. Neurological complications of hemolytic-uremic syndrome. J Child Neurol. 1989;4:108–113. doi: 10.1177/088307388900400206. [DOI] [PubMed] [Google Scholar]
- 9.Hansen M B, Nielson S E, Berg K. Re-examination and further development of a precise and rapid dye method for measuring cell growth/cell kill. J Immunol Methods. 1989;119:203–210. doi: 10.1016/0022-1759(89)90397-9. [DOI] [PubMed] [Google Scholar]
- 10.Hughes A K, Stricklett P K, Kohan D E. Cytotoxic effect of Shiga toxin-1 on human proximal tubule cells. Kidney Int. 1998;54:426–437. doi: 10.1046/j.1523-1755.1998.00015.x. [DOI] [PubMed] [Google Scholar]
- 11.Hughes A K, Stricklett P K, Kohan D E. Shiga toxin-1 regulation of cytokine production by human proximal tubule cells. Kidney Int. 1998;54:1093–1106. doi: 10.1046/j.1523-1755.1998.00118.x. [DOI] [PubMed] [Google Scholar]
- 12.Hurley B P, Jacewicz M, Thorpe C M, Lincicome L L, King A J, Keusch G T, Acheson D W. Shiga toxins 1 and 2 translocate differently across polarized intestinal epithelial cells. Infect Immun. 1999;67:6670–6677. doi: 10.1128/iai.67.12.6670-6677.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inward C D, Williams J, Chant I, Crocker J, Milford D V, Rose P E, Taylor C M. Verocytotoxin-1 induces apoptosis in Vero cells. J Infect. 1995;30:213–218. doi: 10.1016/s0163-4453(95)90693-2. [DOI] [PubMed] [Google Scholar]
- 14.Jacewicz M S, Acheson D W, Binion D G, West G A, Lincicome L L, Fiocchi C, Keusch G T. Responses of human intestinal microvascular endothelial cells to Shiga toxins 1 and 2 and pathogenesis of hemorrhagic colitis. Infect Immun. 1999;67:1439–1444. doi: 10.1128/iai.67.3.1439-1444.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson D R, Pober J S. Tumor necrosis factor and immune interferon synergistically increase transcription of HLA class I heavy- and light-chain genes in vascular endothelium. Proc Natl Acad Sci USA. 1990;87:5183–5187. doi: 10.1073/pnas.87.13.5183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joo F. The blood-brain barrier in vitro: the second decade. Neurochem Int. 1993;23:499–521. doi: 10.1016/0197-0186(93)90098-p. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan B S, Cleary T G, Obrig T G. Recent advances in understanding the pathogenesis of the hemolytic uremic syndromes. Pediatr Nephrol. 1990;4:276–283. doi: 10.1007/BF00857676. [DOI] [PubMed] [Google Scholar]
- 18.Kaye S A, Louise C B, Boyd B, Lingwood C A, Obrig T G. Shiga toxin-associated hemolytic uremic syndrome: interleukin-1β enhancement of Shiga toxin cytotoxicity toward human vascular endothelial cells in vitro. Infect Immun. 1993;61:3886–3891. doi: 10.1128/iai.61.9.3886-3891.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez E L, Contrini N N, Devoto S, de Rosa M F, Grana M G, Genero M H, Canepa C, Gomez H F, Cleary T G. Tumor necrosis factor concentrations in hemolytic uremic syndrome patients and children with bloody diarrhea in Argentina. Pediatr Infect Dis J. 1995;14:594–598. doi: 10.1097/00006454-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Louise C B, Obrig T G. Shiga toxin-associated hemolytic-uremic syndrome: combined cytotoxic effect of Shiga toxin and lipopolysaccharide (endotoxin) on human vascular endothelial cells in vitro. Infect Immun. 1992;60:1536–1543. doi: 10.1128/iai.60.4.1536-1543.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Louise C B, Obrig T G. Shiga toxin-associated hemolytic-uremic syndrome: combined cytotoxic effects of Shiga toxin, interleukin-1ß, and tumor necrosis factor alpha on human vascular endothelial cells in vitro. Infect Immun. 1991;59:4173–4179. doi: 10.1128/iai.59.11.4173-4179.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mariani-Kurkdjian P, Bingen E. Hemolytic-uremic syndrome after verotoxin-producing Escherichia coli infection. Presse Med. 1995;24:99–101. [PubMed] [Google Scholar]
- 23.Mossman T. Rapid colorimetric assay for cellular growth and survival; application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65:55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 24.Newburg D S, Chaturvedi P. Neutral glycolipids of human and bovine milk. Lipids. 1992;27:923–927. doi: 10.1007/BF02535874. [DOI] [PubMed] [Google Scholar]
- 25.Newburg D S, Chaturvedi P, Lopez E L, Devoto S, Gayad A, Cleary T G. Susceptibility to hemolytic-uremic syndrome relates to erythrocyte glycosphingolipid patterns. J Infect Dis. 1993;168:476–479. doi: 10.1093/infdis/168.2.476. [DOI] [PubMed] [Google Scholar]
- 26.Obrig T G, Louise C B, Lingwood C A, Boyd B, Barley-Maloney L, Daniel T O. Endothelial heterogeneity in Shiga toxin receptors and responses. J Biol Chem. 1993;268:15484–15488. [PubMed] [Google Scholar]
- 27.Ohlmann D, Hamann G F, Hassler M, Schimrigk K. Involvement of the central nervous system in hemolytic uremic syndrome/thrombotic thrombocytopenic purpura. Nervenarzt. 1996;67:880–882. doi: 10.1007/s001150050066. [DOI] [PubMed] [Google Scholar]
- 28.Pardridge W M. Recent advances in blood-brain barrier transport. Annu Rev Pharmacol Toxicol. 1988;28:25–39. doi: 10.1146/annurev.pa.28.040188.000325. [DOI] [PubMed] [Google Scholar]
- 29.Pellizzari A, Pang H, Lingwood C A. Binding of verocytotoxin 1 to its receptor is influenced by differences in receptor fatty acid content. Biochemistry. 1992;31:1363–1370. doi: 10.1021/bi00120a011. [DOI] [PubMed] [Google Scholar]
- 30.Prado D, Cleary T G, Pickering L K, Ericsson C D, Bartlett A V, DuPont H L, Johnson P C. The relation between production of cytotoxin and clinical features in shigellosis. J Infect Dis. 1986;154:149–155. doi: 10.1093/infdis/154.1.149. [DOI] [PubMed] [Google Scholar]
- 31.Ramegowda B, Samuel J E, Tesh V L. Interaction of Shiga toxins with human brain microvascular endothelial cells: cytokines as sensitizing agents. J Infect Dis. 1999;180:1205–1213. doi: 10.1086/314982. [DOI] [PubMed] [Google Scholar]
- 32.Sheth K J, Swick H M, Haworth N. Neurological involvement in hemolytic-uremic syndrome. Ann Neurol. 1986;19:90–93. doi: 10.1002/ana.410190120. [DOI] [PubMed] [Google Scholar]
- 33.Shibolet O, Shina A, Rosen S, Cleary T G, Brezis M, Ashkenazi S. Shiga toxin induces medullary tubular injury in isolated perfused rat kidneys. FEMS Immunol Med Microbiol. 1997;18:55–60. doi: 10.1111/j.1574-695X.1997.tb01027.x. [DOI] [PubMed] [Google Scholar]
- 34.Takagi C, Naruse T. Verotoxin induced hemolytic uremic syndrome: pathophysiology of neurological involvement. Nippon Rinsho. 1997;55:731–735. . (In Japanese.) [PubMed] [Google Scholar]
- 35.Tesh V L. Cytokine response to Shiga toxins. In: Kaper J B, O'Brien A D, editors. Escherichia coli O157:H7 and other Shiga toxin-producing E. coli strains. Washington, D.C.: ASM Press; 1998. pp. 226–235. [Google Scholar]
- 36.Tesh V L, Samuel J E, Perera L P, Sharefkin J B, O'Brien A D. Evaluation of the role of Shiga and Shiga-like toxins in mediating direct damage to human vascular endothelial cells. J Infect Dis. 1991;164:344–352. doi: 10.1093/infdis/164.2.344. [DOI] [PubMed] [Google Scholar]
- 37.van de Kar N C A J, Monnens L A H, Karmali M A, van Hinsbergh V W. Tumor necrosis factor and interleukin-1 induce expression of the verocytotoxin receptor globotriaosylceramide on human endothelial cells: implications for the pathogenesis of the hemolytic uremic syndrome. Blood. 1992;80:2755–2764. [PubMed] [Google Scholar]
- 38.van Setten P A, van Hinsbergh V W, van der Velden T J, van de Kar N C, Vermeer M, Mahan J D, Assmann K J, van den Heuvel L P, Monnens L A. Effects of TNF alpha on verocytotoxin cytotoxicity in purified human glomerular microvascular endothelial cells. Kidney Int. 1997;51:1245–1256. doi: 10.1038/ki.1997.170. [DOI] [PubMed] [Google Scholar]
- 39.Wells J, Amaratunga A, McKenna D, Abraham C, Fine R. Amyloid b-protein precursor and apolipoprotein E production in cultured cerebral endothelial cells. Amyloid. 1995;2:229–233. [Google Scholar]
- 40.Yiu S C K, Lingwood C A. Polyisobutylmethacrylate modifies glycolipid binding specificity of verotoxin 1 in thin-layer chromatogram overlay procedures. Anal Biochem. 1992;202:188–192. doi: 10.1016/0003-2697(92)90226-w. [DOI] [PubMed] [Google Scholar]
- 41.Zoja C, Corna D, Farina C, Sacchi G, Lingwood C, Doyle M P, Padhye V V, Abbate M, Remuzzi G. Verotoxin glycolipid receptors determine the localization of microangiopathic process in rabbits given verotoxin-1. J Lab Clin Med. 1992;120:229–238. [PubMed] [Google Scholar]