Many with schizophrenia struggle with significant loss of role and social functioning even after engaging in pharmacological and psychosocial treatment.1 As a result of this functional disability, many apply for and receive federal assistance from one of the Social Security Administration’s (SSA) two disability programs. The oldest program, Social Security Disability Insurance (SSDI),2 was expanded to individuals with psychiatric disorders in 1956. SSDI provides income support to those with a disability who have a qualifying work history and have paid a portion of their income to Social Security. Established in 1972, Supplemental Security Income (SSI)3 provides financial assistance to persons with a disability, regardless of age and work history. Program recipients receive monthly cash benefits, and SSA receipt can be used to determine eligibility for Medicaid/Medicare insurance, food assistance, and temporary state assistance. Among those receiving SSA, mental disorders represent the largest group of SSI recipients, with 60.8% of recipients having a mental disorder and 11.6% of these having schizophrenia or another psychotic disorder.3 For SSDI, 13.1% of recipients report having a mental disorder, with 1.9% having schizophrenia or other psychotic disorders.2 However, SSA programs constitute significant economic costs, as yearly expenditure for SSA’s disability programs for individuals with schizophrenia was roughly $6.7 million for 2020.2,3 Despite these costs, SSA benefits are a lifeline for accessing basic needs for those unable to attain or maintain gainful employment by providing financial support to cover necessities and access to insurance that enables usage of mental health treatment.
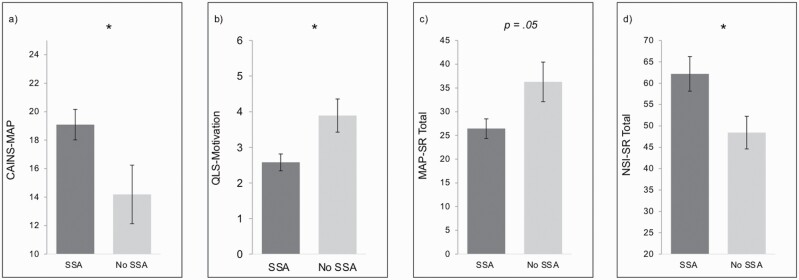
Recently, there has been renewed interest in improving SSA programs in order to make them maximally beneficial for those with serious mental illness (SMI). This is partially due to research showing that SSA benefits may unintentionally lead to poorer outcomes, such as increases in negative symptoms (anhedonia, avolition, asociality, alogia, and blunted affect).4 An analysis5 showed that initial receipt of SSA disability benefits was followed by a decrease in motivation and increase in anhedonia among persons with first-episode psychosis (FEP). Another study6 demonstrated that homeless veterans receiving SSA benefits showed less motivation for work 3 months after benefits receipt than non-recipients. In a randomized controlled trial,7 participants in the control condition receiving SSA benefits had greater impairments in motivation and pleasure after eight weeks when compared to participants not receiving SSA benefits (see figure 1). Although these longitudinal studies suggest that SSA receipt may lead to increases in negative symptoms among those with SMI, cross-sectional studies examining the association between SSI receipt and negative symptoms are more mixed. One of the above referenced studies5 found that FEP SSA recipients had greater concurrent negative symptoms than non-recipients, while another study8 did not find differences in motivation between those with FEP receiving or not receiving SSA benefits. In our cross-sectional data,9 those with schizophrenia receiving SSA benefits had significantly greater self-reported negative symptoms than those not receiving benefits (see figure 1). These discrepant cross-sectional findings may be due to the fact that initiation of SSA benefit receipt, which is difficult to assess in cross-sectional studies, appears to be most closely linked to greater severity of negative symptoms. While additional longitudinal work is needed to confirm whether there is a causal link between SSA benefit receipt and negative symptom increases, these extant results provide evidence for a potentially critical link between benefit receipt and increases in negative symptoms.
Fig. 1.
Differences in negative symptom severity among those receiving and not receiving social security administration (SSA) benefits. (A–C) Longitudinal analyses of the control group from Luther et al.7 showing that after controlling for baseline levels, schizophrenia participants receiving SSA benefits at baseline (n = 6) had greater motivation and pleasure (MAP) dimension negative symptoms on the Clinical Assessment Interview for Negative Symptoms (CAINS)27 8 weeks later (F(1, 25) = 4.45, p = .04, d = .55) (A), higher 8-week motivation reductions on the motivation item on the Heinrich’s Quality of Life Scale (QLS)28 (F(1, 25) = 6.14, p = .02, d = ‐.65) (B), and trending lower self-reported 8-week motivation and pleasure on the Motivation and Pleasure Scale: Self-Report (MAP-SR)29 (higher = less negative symptoms) (F(1, 25) = 4.23, p = .05, d = ‐.54) (C) than those not receiving SSA benefits at baseline (n = 22). (D) Cross-sectional comparison of schizophrenia participants from Strauss et al.9 showing that SSA recipients (n = 12) have greater negative symptoms (measured using the Negative Symptom Inventory-Self-Report (NSI-SR)30) than non-SSA recipients (n = 14); t(24)= ‐2.47, p = .02, d = .97). * p < .05.
While several factors (e.g., social cognition, prior work experience) may impact employment in those with schizophrenia, several studies suggest that SSA receipt may disincentivize joining or rejoining the workforce.10,11 Overtime, this prolonged lack of purposeful activity and community engagement may lead to increased negative symptoms. Although many with SMI experience waxing and waning symptoms, many eventually achieve symptomatic and/or functional improvement.12–14 Engagement in purposeful work is often a catalyst of recovery, leading to improved negative symptoms, self-esteem, quality of life, and health service utilization.15–17 Although many SSA beneficiaries with schizophrenia report a desire to work,18 they also describe significant barriers to engaging in work, including fear of losing stable income or health insurance and difficulty understanding the complex policies around earning additional income while receiving SSA benefits.19 SSA stipulates that for every dollar over a certain threshold (e.g., $65) earned through employment, some amount is deducted (e.g., 50 cents per dollar)20 and if recipients exceed a certain income threshold, their benefits will be terminated. Thus, receipt of SSA is suggested to “play conflicting roles”,12 as it provides essential compensation for individuals, but often prevents engagement in substantial employment that could provide additional resources needed to engage in goal-directed, recreational, and social activities.
Strauss21 proposed that failure to identify and target environmental factors, such as SSA benefits and associated policies/politics, has contributed to limited progress in understanding and treating negative symptoms. A new environmental systems theory, which was grounded in Bronfenbrenner’s22 ecological systems model, proposed that person-level biological and psychological processes interact with four environmental systems that contribute to negative symptoms: the microsystem (immediate environment), mesosystem (connections among mircosystems), exosystem (indirect environment), and macrosystem (sociocultural factors). Among these, the exosystem is particularly relevant to understanding the role of SSA benefits in negative symptoms as it reflects indirect environmental factors that an individual does not participate in but is affected by. Indirect factors influence both what happens to people within their direct environments (microsystems) and which resources are available to them. Examples of environmental factors impacting resource availability include transportation, street walkability, access to recreational facilities and shops/restaurants, crime, and the local economy. Factors influencing what happens to the individual depend upon external “power systems,” that exert an influence on the individual, typically outside of their awareness (e.g., mass media, politics, and laws). Disability benefits may impact negative symptoms via a tiered influence of these two exosystem pathways. Specifically, politics influence how decision-makers and those holding legislative power determine local disability policies, and these policies subsequently dictate whether individuals with schizophrenia have access to resources needed to perform recreational, social, and goal-directed activities. For example, SSA approval rates, monthly cash benefits ($510–720), and SSI supplements ($10–100+) differ considerably across states; local politics drive this variability. Given that the average monthly income for people with schizophrenia on SSI3 is $609.76 and $936.16 for SSDI,2 these policies put recipients well below the poverty line, even in the best of circumstances. Although they may provide just enough money to survive and meet bare minimum necessities, funds received are insufficient for engaging in typical activities that most others have resources to complete.23 Resource limitations resulting from disability policies may therefore impose barriers that cause and maintain negative symptoms; these barriers are not addressed by currently available treatments, potentially rendering any improvements in psychological or biological processes moot until relevant environmental factors are addressed.
Although SSA programs are an essential means of support for many with schizophrenia, we believe there are changes that could be made to improve SSA. Individuals with power to influence mental health and disability-related policies/laws could advocate to eliminate perceived barriers to employment and disability receipt to provide additional resources to combat negative symptoms. Increasing monthly SSA payments to a sustainable amount may improve the well-being of individuals. Further funding and advertisements for free or affordable recreational activities and access to transportation may encourage socialization and community engagement.24,25 Psychoeducation, including explaining conditions for SSA receipt and limitations around work/use of employment programs, as well as other resources that could help overcome the complexities of SSA benefits and working (e.g., greater access to disability attorney services)26 are important to incorporate into mental health services. Future studies should also examine whether negative symptoms influence the disability determination process and whether an applicant qualifies for benefits as well as the role that fear of losing SSA benefits may play in negative symptoms themselves (e.g., reduced work motivation). Although the SSA has tested some changes to their policies to increase work outcomes for SSA recipients,20 it is unclear whether these changes will be implemented at the national level and the role that these changes will have on disability receipt, working while on SSA, and negative symptoms in schizophrenia. Future longitudinal research, advanced modeling analyses, and intervention trials may better determine the direction of effect of receipt on the onset and development of negative symptoms within early psychosis, if some programs are more strongly associated with negative symptoms, and whether continued receipt of services maintains or influences negative symptoms once the illness becomes chronic. Such findings can contribute to more efficient use of resources and services to improve negative symptoms and enhance quality of life for those with schizophrenia.
Contributor Information
Delaney E Collins, Department of Psychology, University of Georgia, Athens, GA, USA.
Lauren Luther, Department of Psychology, University of Georgia, Athens, GA, USA.
Ian M Raugh, Department of Psychology, University of Georgia, Athens, GA, USA.
Ruth Condray, Biometrics Research Program, VA Pittsburgh Healthcare System, Pittsburgh, PA, USA.
Daniel N Allen, Department of Psychology, University of Nevada, Las Vegas, Las Vegas, NV, USA.
Gregory P Strauss, Department of Psychology, University of Georgia, Athens, GA, USA.
Conflict of interest statement
Dr. Gregory Strauss is one of the original developers of the Brief Negative Symptom Scale (BNSS) and receives royalties and consultation fees from Medavante-ProPhase LLC in connection with commercial use of the BNSS and other professional activities; these fees are donated to the Brain and Behavior Research Foundation. Dr. Strauss has received honoraria and travel support from Medavante-ProPhase LLC for training pharmaceutical company raters on the BNSS. In the past 2 years, Dr. Strauss has consulted for and/or been on the speaker bureau for Minerva Neurosciences, Acadia, Lundbeck, Sunovion, Boehringer Ingelheim, and Otsuka pharmaceutical companies. All other authors have no relevant disclosures to report.
Funding
This work was supported in part by the William and Dorothy Bevan Scholarship from the American Psychological Foundation (to Dr. Luther) and a predoctoral award (to Dr. Luther) from the Indiana Clinical and Translational Sciences Institute (ICTSI) (UL1TR001108). Additionally, research was supported by National Institute of Mental Health (NIMH) Grants R21-MH112925, R21-MH122863, R21-MH122863, and R01MH116039 to Dr. Strauss.
References
- 1. Harvey PD, Strassnig MT, Silberstein J.. Prediction of disability in schizophrenia: Symptoms, cognition, and self-assessment. J Exp Psychopathol. 2019;10(3):204380871986569. [Google Scholar]
- 2. U.S. Social Security Administration. Annual Statistical Report on the Social Security Disability Insurance Program, 2020. 2021. No. 13-11826. https://www.ssa.gov/policy/docs/statcomps/di_asr/2020/di_asr20.pdf. Accessed August 30, 2021. [Google Scholar]
- 3. U.S. Social Security Administration. SSI Annual Statistical Report, 2019. 2020. No. 13-11827. https://www.ssa.gov/policy/docs/statcomps/ssi_asr/2019/ssi_asr19.pdf. Accessed August 30, 2021. [Google Scholar]
- 4. Kirkpatrick B, Fenton WS, Carpenter WT, Marder SR.. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32(2):214–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rosenheck RA, Estroff SE, Sint K, et al. Incomes and outcomes: social security disability benefits in first-episode psychosis. Am J Psychiatry. 2017;174(9):886–894. [DOI] [PubMed] [Google Scholar]
- 6. Rosenheck RA, Dausey DJ, Frisman L, Kasprow W.. Outcomes after initial receipt of social security benefits among homeless veterans with mental illness. Psychiatr Serv. 2000;51(12):1549–1554. [DOI] [PubMed] [Google Scholar]
- 7. Luther L, Fischer MW, Johnson-Kwochka AV, et al. Mobile enhancement of motivation in schizophrenia: a pilot randomized controlled trial of a personalized text message intervention for motivation deficits. J Consult Clin Psychol. 2020;88(10):923–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fervaha G, Takeuchi H, Foussias G, Hahn MK, Agid O, Remington G.. Achievement motivation in early schizophrenia: relationship with symptoms, cognition and functional outcome. Early Interv Psychiatry. 2018;12(6):1038–1044. [DOI] [PubMed] [Google Scholar]
- 9. Strauss GP, Macdonald KI, Ruiz I, Raugh IM, Bartolomeo LA, James SH.. The impact of the COVID-19 pandemic on negative symptoms in individuals at clinical high-risk for psychosis and outpatients with chronic schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2022;272(1):17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rosenheck R, Leslie D, Keefe R, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163(3):411–417. [DOI] [PubMed] [Google Scholar]
- 11. Estroff SE, Patrick DL, Zimmer CR, Lachicotte WS.. Pathways to disability income among persons with severe, persistent psychiatric disorders. Milbank Q. 1997;75(4):495–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM.. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 2004;161(3):473–479. [DOI] [PubMed] [Google Scholar]
- 13. Grossman LS, Harrow M, Rosen C, Faull R, Strauss GP.. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49(6):523–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harrow M, Grossman LS, Jobe TH, Herbener ES.. Do patients with schizophrenia ever show periods of recovery? A 15-year multi-follow-up study. Schizophr Bull. 2005;31(3):723–734. [DOI] [PubMed] [Google Scholar]
- 15. Drake RE, Wallach MA.. Employment is a critical mental health intervention. Epidemiol Psychiatr Sci. 2020;29:e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nuechterlein KH, Subotnik KL, Ventura J, et al. Enhancing return to work or school after a first episode of schizophrenia: the UCLA RCT of individual placement and support and workplace fundamentals module training. Psychol Med. 20;50(1):20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bio DS, Gattaz WF.. Vocational rehabilitation improves cognition and negative symptoms in schizophrenia. Schizophr Res. 2011;126(1-3):265–269. [DOI] [PubMed] [Google Scholar]
- 18. Bond GR, Xie H, Drake RE.. Can SSDI and SSI beneficiaries with mental illness benefit from evidence-based supported employment? Psychiatr Serv. 2007;58(11):1412–1420. [DOI] [PubMed] [Google Scholar]
- 19. Drake RE, Frey W, Karakus M, Salkever D, Bond GR, Goldman HH.. Policy implications of the mental health treatment study. Psychiatr Serv. 2016;67(10):1139–1141. [DOI] [PubMed] [Google Scholar]
- 20. Nichols A, Hemmeter J.. An Introduction to Disability Policy and SSA’s Demonstrations. In: Nichols A, Hemmeter J, Goetz Engler D, eds. Lessons from SSA Demonstrations for Disability Policy and Future Research. Rockville, MD: Abt Associates; 2021:1–30. [Google Scholar]
- 21. Strauss G. A bioecosystem theory of negative symptoms in schizophrenia. Front Psychiatry. 2021;12:655471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bronfenbrenner U. Ecological systems theory. In: Vasta R, ed. Six Theories of Child Development: Revised Formulations and Current Issues. London, England: Jessica Kingsley Publishers; 1992:187–249. [Google Scholar]
- 23. Cooper JA, Barch DM, Reddy LF, Horan WP, Green MF, Treadway MT.. Effortful goal-directed behavior in schizophrenia: computational subtypes and associations with cognition. J Abnorm Psychol. 2019;128(7):710–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mote J, Gill K, Fulford D.. “Skip the small talk” virtual event intended to promote social connection during a global pandemic: online survey study. JMIR Formativ Res. 2021;5(9):e28002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Snethen G, McCormick BP, Van Puymbroeck M.. Community involvement, planning and coping skills: pilot outcomes of a recreational-therapy intervention for adults with schizophrenia. Disabil Rehabil. 2012;34(18):1575–1584. [DOI] [PubMed] [Google Scholar]
- 26. Lang K. Apply, deny, appeal: the difficult process of claiming disability benefits. Gener J. 2019;43(4):18–24. [Google Scholar]
- 27. Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP.. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170(2):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Heinrichs DW, Hanlon TE, Carpenter WT.. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10(3):388–398. [DOI] [PubMed] [Google Scholar]
- 29. Llerena K, Park SG, McCarthy JM, Couture SM, Bennett ME, Blanchard JJ.. The Motivation and Pleasure Scale-Self-Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr Psychiatry. 2013;54(5):568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Raugh IM, Luther L, Bartolomeo LA, et al. Negative symptom inventory—self—report (NSI-SR): initial development and validation. [DOI] [PMC free article] [PubMed] [Google Scholar]