Abstract
Background.
Two major theories aid in explaining the association between anxiety and cannabis use: a symptom-driven pathway (heightened anxiety precedes greater cannabis use) and a substance-induced pathway (greater use precedes heightened anxiety). Although the co-occurrence of cannabis use and anxiety symptomology is well-established, less is known about the temporal sequence of cannabis use and anxiety symptomology over the course of young adult development.
Methods.
Data are from an ongoing, longitudinal, cohort study. All prospective analyses used data from wave 8, when participants were between the ages of 17 and 20, through wave 13, when participants are between ages 21 and 24 (N = 2,995). Data were set up in accelerated longitudinal design in which we estimated a series of latent difference score models between anxiety and cannabis use from 17 to 24 years old. Models were estimated for men and women, separately.
Results.
For the overall sample and men, greater cannabis use predicted greater subsequent increases in anxiety; however, greater anxiety symptoms were associated with decreasing cannabis use. For women, results were more complex. A positive association was noted between prior, trait-like levels of anxiety predicting greater change (increasing) in anxiety symptomology. However, when change is predicted by prior change we see that cannabis use decreases among women who have recently experienced an increase in anxiety.
Conclusion.
The nuanced set of results from this study support a dynamic interplay between anxiety symptoms and cannabis use, with important sex differences observed. Overall, our results pave the way for rethinking our guiding theories to include a more robust, flexible, and dynamic model for understanding associations between substance use and mental health symptomology during a key period of development.
1. Introduction
Besides alcohol, cannabis is the most used substance among young adults (ages 18 to 25), with 34.5% (11.6 million) reporting past year use, and men reporting greater cannabis use than women (Khan et al., 2013; SAMHSA, 2021). Many young adults also experience the onset or continuation of mental health problems, such as anxiety, which can vary by sex (women report greater anxiety symptoms than men; McLean et al., 2011). Epidemiological research reports general anxiety symptoms have increased over the past decade (5.1% to 6.8%), with young adults reporting the greatest increases in anxiety (7.9% to 14.6%) and similar increases noted for men and women (Goodwin, Weinberger, Kim, Wu, & Galea, 2020). Anxiety symptomology often co-occurs with substance use and substance use disorders, with a recent meta-analysis reporting high rates of cannabis use disorder among individuals with generalized anxiety disorder, and vice versa (Onaemo et al., 2021).
The co-occurrence of cannabis use and anxiety is well-established, however less is known about the developmental, temporal, sequence of cannabis use and anxiety symptomology. In general, there are two major theories that address the issue of directionality. The first is a symptom-driven pathway, in which anxiety symptomology precedes greater cannabis use. As one believes that cannabis use can be a method for coping with anxiety, heavy use can be established, which could potentially lead to negative consequences (Khantzian, 1985). The second is the substance-induced pathway, which posits that prolonged use of cannabis can prompt or exacerbate severity of anxiety symptomology (Ehlers et al., 2019; Schuckit, 2006). This can occur when heavier doses of THC (the psychoactive component of cannabis) are consumed in the immediate term but also among those who use cannabis more regularly (Sharpe et al., 2020).
Results from multiple cross-sectional studies across various populations reveal a robust and positive association between cannabis use and anxiety symptomology, with some research noting differences between men and women (Khan et al., 2013; McLean et al., 2011). However, a recent meta-analysis of longitudinal studies reported inconsistency in terms of temporal associations between cannabis use and anxiety, with some studies supporting a symptom-driven pathway, others supporting a substance-induced pathway, some noting no directional pathways, and others reporting reverse effects such that greater cannabis use is associated with less anxiety (Garey et al., 2020). For example, a large prospective study of Australian young adults showed support for a substance-induced pathway such that those who began using cannabis before 15 years old, and kept steadily using cannabis into their early 20’s, were more likely to report symptoms of an anxiety disorder later in young adulthood; however, early anxiety symptomology did not predict later cannabis use (Hayatbakhsh et al., 2007). Others have supported a symptom-driven model noting anxiety symptomology is associated with greater odds of cannabis use and transitioning from a non-use to cannabis use during the study (Stapinski et al., 2016). In contrast, a large cohort study of Swedish young adults reported no longitudinal associations between early cannabis use and later anxiety symptomology or vice versa (Danielsson et al., 2016). These mixed results are consistent with a recent review of longitudinal studies in which Garey and colleagues (2020) stated “there still remains no clear, consistent evidence for the temporal sequencing of anxiety and cannabis use” (p.348). The authors do note, however, plausible shared vulnerabilities that differ across sex as a potential explanation of mixed results among longitudinal studies.
Sex is known to affect both prevalence of anxiety (Copeland et al., 2014) as well as prevalence of cannabis use (Lev-Ran et al., 2014), with the former being higher in women and the latter higher in men (Goodwin et al., 2020; Khan et al., 2013; McLean et al., 2011). However, there is little research on whether temporal associations between anxiety and cannabis use differ for men and women. One cross-sectional study showed cannabis use to be a better indicator of poor mental health in women than men (Van Gastel et al., 2014). However, a three-year prospective study reported that the majority of results regarding effects of early cannabis on later anxiety symptomology and vice versa were similar for men and women (Danielsson et al., 2016). Thus, further work is needed to understand heterogeneity in temporal sequencing of cannabis use and anxiety symptoms between men and women.
1.1. The Present Study
Given the relatively nescient literature, the present study aims to better understand directionality between anxiety symptomology and cannabis use among young adults and how this may vary between men and women. To accomplish study aims, we tested two competing theoretical models. First, in line with symptom-driven pathway, we examined whether higher levels of anxiety were associated with subsequent increases in cannabis use (Aim 1). Second, in line with substance-induced pathway, we assessed whether higher levels of cannabis use were associated with subsequent increases in anxiety symptomology (Aim 2). Finally, to assess how associations between cannabis use and anxiety symptomology vary by sex, we estimated separate models for men and women. To provide readers with a visual representation of emergent results, we use coefficients from our final models and simulate increases in cannabis use to examine the long-term effects on anxiety symptomology and vice versa. Though the present study is testing multiple theories that provide context for directionality, we should note that all results are exploratory. We do not have any a-priori, directional, hypotheses given mixed results in the literature.
2. Methods
2.1. Participants and Procedures
Participants are from two cohorts of students in 6th and 7th grade in 2008 initially recruited from 16 middle schools in Southern California for an evaluation of a voluntary after-school substance use prevention program (D’Amico et al., 2012). Cohorts were followed annually across 13 waves through 2020. Participants who do not complete a particular survey wave remain eligible to complete all subsequent waves. Wave-to-wave retention rates average 85% across all 13 waves, and 90% from age 18 forward (waves 8-13). A multivariate logistic regression analysis was conducted to determine whether retention at wave 13 (in wave 13 vs. not) was predicted by substance use or demographics at wave 12. It was found that retention from wave 12 to wave 13 was not predicted by wave 12 past-month use of alcohol, cannabis, or cigarettes, similar to all previous waves; however, retention was slightly higher among females than males (89.5% vs. 85.6%, respectively; OR (95% CI) = 1.33 (0.85, 1.89), p = 0.02) and among those who were younger versus older (mean age = 22.5 vs. 22.9 at wave 12, respectively; OR (95% CI) = 0.59 (0.51, 0.68), p <.0001)A11 prospective analyses used data from wave 8, when participants were between the ages of 17 and 20, through wave 13, when participants were between ages 21 and 24 (N = 2,995). Characteristics of the sample can be found in Table 1 (and Supplement Table 1).
Table 1.
Participant demographic characteristics and behavioral health
| Variable | Total sample | Men | Women |
|---|---|---|---|
| Age M(SD) | 18.3 (0.73) | 18.3 (0.73) | 18.3 (0.72) |
| Female n(%) | 1,350 (54.3%) | ||
| Race/Ethnicity n(%) | |||
| Non-Hispanic White | 510 (20.5%) | 264 (22.3%) | 246 (18.2%) |
| Non-Hispanic Black | 60 (2.24%) | 25 (2.2%) | 35 (2.6%) |
| Hispanic | 1,127 (45.4%) | 480 (42.3%) | 647 (47.9%) |
| Asian | 503 (20.2%) | 240 (21.2%) | 263 (19.5%) |
| Multiracial/Other | 284 (11.4%) | 125 (11.0%) | 159 (11.8%) |
| Mother’s Education n(%) | |||
| High school or less | 733 (29.5%) | 307 (27%) | 426 (31.6%) |
| Days of Cannabis Use (Past Month) M(SD) | 2.34 (6.26) | 3.14 (7.27) | 1.67 (5.18) |
| Anxiety M(SD) | 4.12 (5.04) | 3.51 (4.71) | 4.62 (5.25) |
2.2. Measures
2.2.1. Background covariates.
Participants reported age, sex at birth (female vs. male), race/ethnicity [non-Hispanic white (reference), non-Hispanic black, Hispanic, Asian, and Other/Multiracial], and mother’s education (dichotomous indicator of family socioeconomic status; 1=“high school or less”, 0 = “greater than high school”). We also controlled for intervention status at wave 1 in 2008 (note that intervention effects on substance use were no longer significant after wave 3).
2.2.2. Cannabis use.
Participants reported the number of days they used cannabis in the past month (0 to 30 days) for waves 8 through 13.
2.2.3. Anxiety.
The GAD-7 (Spitzer, Kroenke, & Williams, 1999; α = .94 to .95 across waves) assessed symptoms of anxiety at waves 8 through 13. Items included symptoms such as feeling nervous, anxious, or on edge and not being able to stop or control worrying in the past two weeks. Items were rated on a scale from 0 = not at all to 3 = nearly every day and summed (total score range 0 – 21).
2.3. Analytic plan
Because data were set up in naturally occurring cohorts (e.g., age), an accelerated longitudinal cohort design was used. This creates a planned missing data pattern such that participants only contribute data at time points in which they were in the study. Because our metric of time is age (rather than follow-up wave), we are able to model developmental trajectories of anxiety symptoms and cannabis use from ages 17 to 24 years old.
2.3.1. Latent difference score model.
A series of latent difference score models (Grimm et al., 2016) were estimated to address study aims (see Figure 1 for conceptual model). The following procedures were carried out with the full sample and separate models for men and women. Latent difference score models provide various levels, and types, of prediction at the within- and between-person level of analysis. For the purposes of this study, we focus on the two within-person parameters estimated in the model. The first is the proportional coupling parameter, which models the lagged effect of changes in, for example, cannabis use at a given age resulting from an individual’s level of anxiety symptoms at the prior age (e.g., symptom-driven model). One would interpret a significant, positive, effect of this proportional coupling parameter as an individual’s level of anxiety at age t is associated with positive changes (e.g., greater use) in cannabis use from age t to t+1. Thus, this would imply that both lower initial levels of anxiety symptoms are associated with smaller but positive change in cannabis use, and that higher initial levels of anxiety symptoms are associated with larger, positive changes in cannabis use.
Figure 1.

Conceptual latent difference score model for anxiety and cannabis use. Note: conceptual model stops at age 20 for visual purposes only. The full model extends to 24 years old. Lagged effects labeled with the δ symbol represent proportional coupling parameters. Lagged effects labeled with the ξ symbol represent dynamic coupling parameters.
The second component is the dynamic coupling parameter. Here, we examine how lagged change (rather than level) in one variable is associated with subsequent change in another variable. Though these two parameters (proportional and dynamic coupling parameters) may seem similar, including both adds substantive information. For example, it may be that changes in cannabis use are affected by specific levels of anxiety, but these changes in cannabis use are further accelerated when anxiety symptoms have recently increased. A significant positive effect would imply that increases in anxiety symptoms between two years in age (e.g., 18 and 19 years old) is associated with positive changes in cannabis use (e.g., greater use) between two subsequent time points for a given individual (e.g., 20 and 21 years old). This would imply that smaller changes in anxiety between two ages are associated with smaller increases in cannabis use at the next age, whereas larger changes in anxiety are associated with greater increases in cannabis use at the next age. As recommended by Grimm et al., (2016) we have constrained each set of lagged effects to be equal over time for parsimony and to allow for replication
2.3.2. Missing data.
Prior to setting up data in an accelerated longitudinal design (N=2,507) in order to have enough people in the ‘tails’ of our developmental cohort we removed 23 individuals (which is .009% of the sample) who were age 16 (n = 11), age 21 (n = 4), and age 22 (n = 8) years old at wave 8 (N = 2,484). Due to missing data on some variables in our models, our final analytic sample size is 2,284. We used the robust maximum likelihood estimator, which can accommodate missing data and non-normality on all outcome variables, and provide unbiased and consistent estimates.
3. Results
For our final bivariate model, we only describe the two within-person lagged coupling parameters in the text below. However, in an effort to be thorough and provide readers with a full understanding of how cannabis use and anxiety symptoms use are associated we have developed a comprehensive supplemental materials document where we provide methods, results, and discussion for each of the univariate models as well as the final bivariate model.
3.1. Associations between Anxiety and Cannabis Use for the Whole Sample
Table 2 provides effects of coupling parameters (proportional and dynamic) as well as mean and variances of the intercept and constant change components for each construct in our final model. We have also included figures of significant lagged effects for each model (see supplemental Figures 2–4).
Table 2.
Coupling parameters for the final bivariate latent difference score model assessing longitudinal associations between anxiety symptoms and cannabis use
| Total sample | Men | Women | |
|---|---|---|---|
|
| |||
| Parameters for latent difference score model | B(SE) | B(SE) | B(SE) |
| Within construct proportional change | |||
| Level cannabis use➔ changes cannabis use | −0.06 (0.04) | −0.08 (0.06) | −0.03 (0.10) |
| Level anxiety ➔ changes anxiety | −0.18 (0.08)* | −0.10(0.12) | −0.28 (0.12)* |
| Proportional coupling parameters | |||
| Level cannabis use ➔ changes anxiety | 0.05 (0.02)* | 0.06 (0.02)* | 0.06 (0.02)* |
| Level anxiety ➔ changes cannabis use | −0.47 (0.15)* | −0.56 (0.15)* | 1.32 (0.52)* |
| Dynamic coupling parameters | |||
| Changes cannabis use➔ changes anxiety | 0.30 (0.14)* | 0.31 (0.23) | −0.11 (0.04)* |
| Changes anxiety ➔ changes cannabis use | 0.46 (0.25) | 0.51 (0.42) | −4.65 (1.64)* |
| Initial level and constant change parameters | |||
| Level cannabis use | 0.75 (0.28)* | 2.09 (0.43)* | 1.12 (0.28)* |
| Level anxiety | 4.89 (0.25)* | 3.61 (0.30)* | 5.37 (0.21)* |
| Change cannabis use | 3.04 (0.79)* | 3.03 (0.61)* | −6.52 (2.86)* |
| Change anxiety | 0.86 (0.46)* | 0.15 (0.53) | 1.50 (0.62)* |
| Correlation between initial levels and change parameters | |||
| Level cannabis use with Change cannabis use | −0.11 (0.05)* | −0.09 (0.11) | −0.19 (0.08)* |
| Level anxiety with Change anxiety | 0.39 (0.21)* | 0.09 (0.41) | 0.89 (0.09)* |
| Level anxiety with Change cannabis use | 0.79 (0.08)* | 0.78 (0.08)* | −0.89 (0.03)* |
| Level cannabis use with Level anxiety | −0.05 (0.05) | 0.03 (0.07) | 0.14 (0.06)* |
| Level cannabis use with Change anxiety | −0.12 (0.12) | −0.25 (0.29) | −0.11 (0.09) |
| Change cannabis use with Change anxiety | 0.25 (0.29) | −0.05 (0.58) | −0.84 (0.10)* |
| Variance of initial level and constant change parameters | |||
| Level cannabis use | 26.3 (2.11)* | 41.3 (3.70)* | 12.40 (1.72)* |
| Level anxiety | 15.7 (1.14)* | 12.9 (1.35)* | 15.8 (0.83)* |
| Change cannabis use | 5.46 (1.95)* | 6.45 (1.95)* | 28.7 (20.8)* |
| Change anxiety | 0.91 (0.40)* | 0.66 (0.32)* | 1.39 (1.06)* |
| Model Fit Criteria | |||
| χ 2 | 684.7 | 363.8 | 541.9 |
| df | 153 | 141 | 141 |
| CFI | 0.95 | 0.95 | 0.94 |
| TLI | 0.95 | 0.95 | 0.94 |
| RMSEA | 0.04 | 0.04 | 0.05 |
| SRMR | 0.06 | 0.07 | 0.06 |
In terms of proportional coupling parameters (see supplemental Figure 2), results supported a substance-induced pathway in that anxiety symptoms increased more rapidly for individuals reporting greater prior levels of past month cannabis use. Interestingly, effects for the symptom-driven pathway are opposite of what was expected with results showing changes in cannabis use decreasing among individuals reporting higher prior levels of anxiety. Table 2 (see supplemental Figure 2) also presents dynamic coupling parameters. Here, results support a substance-induced pathway such that greater, prior, increases in cannabis use (e.g., from 17 to 18 years old) are associated with greater change (increases) in anxiety (e.g., from 18 to 19 years old). No significant effect emerged for changes in anxiety predicting changes in cannabis use over time.
3.1.1. Visual representation of effects.
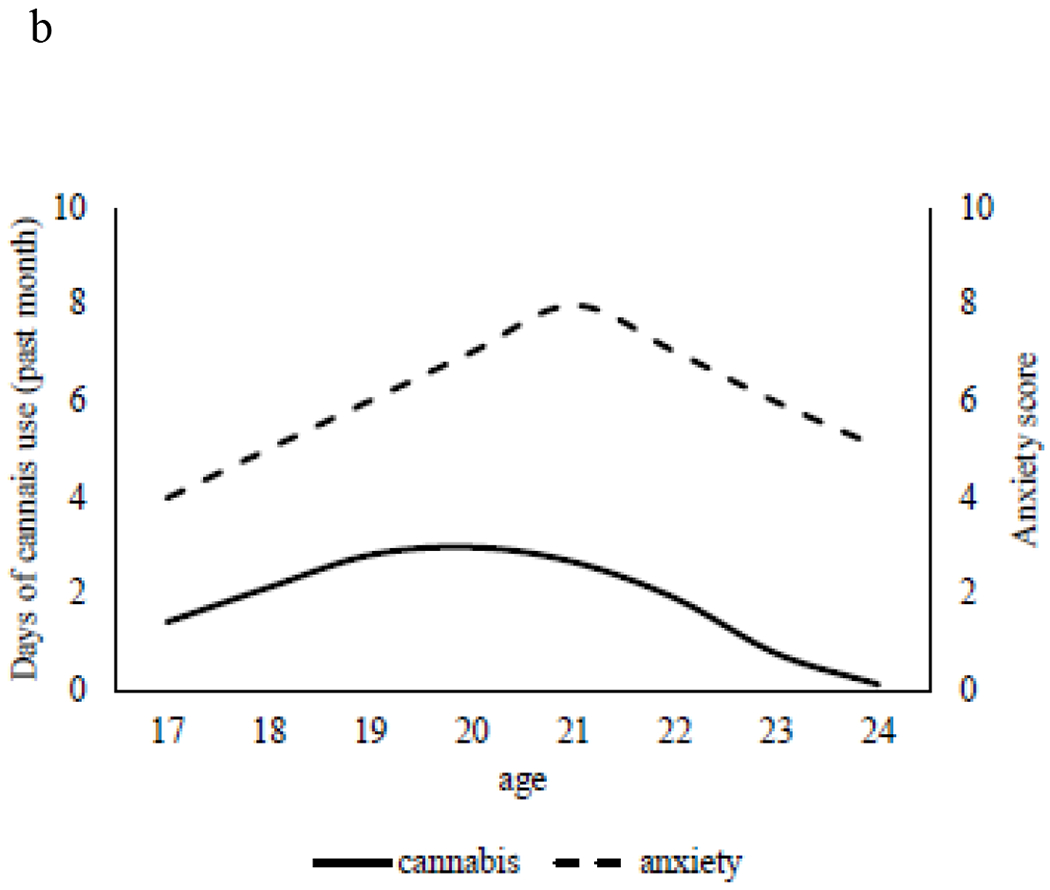
We provide visual representations of anxiety and cannabis use for a prototypical young adult to explore what happens to anxiety when we force increases in cannabis use and vice versa. As shown in Figure 2a, a hypothetical young adult starts with average levels (i.e., intercept values) of anxiety (score of 4) and cannabis use (average of 1.5 days per month) at age 17. We then forced increases in cannabis use by 2 additional days per month for each year from ages 18 to 21. As cannabis use increases to nearly 10 days per month by age 21, we see rapid increases in anxiety symptomology, which peaks at age 21. Of note, even when we force cannabis use to subside back to its initial value, anxiety symptoms still remain stably high through age 24. In Figure 2b, we do the opposite by forcing changes in anxiety symptoms (1 symptom increase per year through age 21) to understand effects on cannabis use. As anxiety symptoms increase from 17 to 21 years old, cannabis use remains consistently low (peaking at 3 days per month at age 20) before reducing to zero days of cannabis use by age 24.
Figure 2.

a. Effect of forced changes in cannabis use on anxiety from 17 to 24 years old for the full sample. Predicted trajectories for a hypothetical young adult who begins with average levels of anxiety and cannabis use (i.e., intercept values) at age 17. We then provide “system shocks” to cannabis use to understand the effect on anxiety symptoms over time.
b. Effect of forced changes in anxiety on cannabis use from 17 to 24 years old for the full sample. Predicted trajectories for a hypothetical young adult who begins with average levels of anxiety and cannabis use (i.e., intercept values) at age 17. We then provide “system shocks” to anxiety symptoms to understand the effect on cannabis use over time.
3.2. Associations between Anxiety and Cannabis Use for Men and Women
3.2.1. Men.
Table 2 provides final estimates of our latent difference score for men. Results for the proportional coupling parameters followed that of the full sample with support for the substance-induced pathway and an opposite effect (negative) for the symptom-driven pathway. In support of a substance-induced pathway, results revealed prior levels of cannabis use (i.e., higher use) are associated with greater subsequent increases in anxiety. Interestingly, an opposite effect (negative) for the symptom-driven pathway indicates prior levels of anxiety (i.e., greater anxiety symptoms) are associated with less change in cannabis use (e.g., decreasing cannabis use; see Supplemental Figure 3). No dynamic coupling parameters emerged.
3.2.2. Women.
In contrast, the model for women showed a different pattern than both the full sample and among men (see Table 2 for parameter estimates). For the proportional coupling parameters, we show support for both symptom-driven and substance-induced models such that prior levels of cannabis use are associated with greater subsequent increases in anxiety. However, for women, greater prior anxiety symptoms are associated with greater increases in cannabis use (see Supplemental Figure 4). Thus, women tend to show greater increases in cannabis use from, for example, age 18 to 19, for those reporting higher prior levels of anxiety at age 18.
Women also showed a very different pattern for the dynamic coupling parameters, with results noting significant, but negative associations, for both symptom-driven and substance-induced pathways. Results indicated greater previous increases in cannabis use (e.g., greater change) are associated with less change in anxiety symptoms (see Supplemental Figure 4). For example, changes in anxiety symptoms from 18 to 19 years old decreased more rapidly among individuals who experienced greater previous changes in cannabis use from 17 to 18 years old. We see the same effect for the other dynamic coupling parameter. Prior increases in anxiety symptoms are associated with decreases in cannabis use (negative effect). Thus, keeping with the same example, cannabis use from 18 to 19 years old decreased when women experienced greater previous changes (e.g., increasing) in anxiety from 17 to 18 years old.
3.3.3. Visual representation of effects.
We plotted a hypothetical male (Figure 3a) and female (Figure 3b), forcing changes in cannabis use as noted above. For men, forced changes in cannabis use (peak 10 days/month at age 20 and 21) show similar patterns with the full sample, noting rapid increases in anxiety (a three-symptom increase by age 21), which stabilize through age 24, even after cannabis use decreased. For women, however, these same forced increases in cannabis use have very little effect on anxiety, with women showing only a 1-symptom increase in anxiety from 17 to 24 years old.
Figure 3.


Effect of forced changes in cannabis use on anxiety from 17 to 24 years old for men and women. Predicted trajectories for a hypothetical young adult who begins with average levels of anxiety and cannabis use (i.e., intercept values) at age 17. We then provide “system shocks” to cannabis use to understand the effect on anxiety symptoms over time.
a. Hypothetical Man
b. Hypothetical Woman
On the other side of this dynamic process, we also showed that across both men and women prior levels of anxiety are associated with subsequent changes in cannabis use (i.e., proportional coupling). For men, this heightened anxiety was associated with less change in cannabis use (i.e., less use over time), but for women, heightened anxiety was associated with more change in cannabis use (i.e., more use over time). For men (Figure 4a), forced increases in anxiety (as noted above, 1 symptom per year) through age 21 had little effect on cannabis use, with men showing only a 1 day increase of use through age 20, which dropped to less than 1 day of use by age 24. For women (Figure 4b; note: this model only allowed us to increase anxiety by 0.5 points per year as it was very sensitive to change), as anxiety increased from 17 to 21 years old, cannabis use dropped to zero days per month at age 21, but as anxiety use slowly decreased through age 24, cannabis use rose exponentially from zero to 7.6 days per month by age 24.
Figure 4.


Effect of forced changes in anxiety symptoms on cannabis use from 17 to 24 years old for men and women. Predicted trajectories for a hypothetical young adult who begins with average levels of anxiety and cannabis use (i.e., intercept values) at age 17. We then provide “system shocks” to anxiety symptoms to understand the effect on cannabis use over time
a. Hypothetical man
b. Hypothetical Woman
4. Discussion
The transition from late adolescence into young adulthood is a time of numerous developmental changes and a time when cannabis use peaks. With all the challenges and choices that young adulthood brings, it is not surprising that during this period of life mental health symptoms, such as anxiety fueled by worry about the future, may begin to emerge (Copeland et al., 2014; Gustavson et al., 2017). We attempted to provide more clarity on longitudinal associations between cannabis use and anxiety symptomology during this developmental period by testing two theories: symptom-driven and substance-induced pathways. Our results both support and refute prior literature. That is, support for specific pathways emerged; however, we also note several instances where a negative association between cannabis and anxiety emerged. Overall, results point to a complex and dynamic interplay between anxiety symptoms and cannabis use, which varies across men and women.
In the full sample model, after accounting for constant change over the course of the study, we show support for substance-induced pathways at both levels of analysis (proportional and dynamic coupling parameters). Young adults reporting greater previous, trait-like, levels of cannabis use had greater increases in anxiety symptoms, with this pattern also emerging when examining dynamic effect processes (i.e., change-to-change). However, unexpectedly, we also noted that individuals reporting greater previous, trait-like, levels of anxiety reported decreases in cannabis use throughout young adulthood. This is in opposition to symptom-driven models which posit that greater anxiety is associated with greater cannabis use. Thus, the effect of anxiety on cannabis appears to depend on how anxiety is measured. It seems that when anxiety is assessed as more trait-like (e.g., point in time), greater levels are associated with less use – indicating cannabis may not be a useful mechanism for coping with anxiety. Interestingly, though, we show that when anxiety is assessed as a changing system, cannabis use increases. Thus, it may be that if anxiety increases year after year, individuals believe that cannabis may reduce their symptomology – thus cannabis use increases.
In an attempt to shed light onto this dynamic interplay, we created plots for hypothetical young adults to understand how forced changes in cannabis use may affect long-term anxiety and vice versa. First, results supported prior work showing that forced increases in cannabis use not only produce rapid escalations in subsequent anxiety, but these effects are lasting, even when cannabis use subsides. In contrast, when we forced increases in anxiety, we observed little change in cannabis use over time. Thus, although results support a dynamic interplay between anxiety and cannabis use (and a negative association between prior anxiety and subsequent cannabis use), it appears that increasing cannabis use has a much larger and lasting effect on anxiety symptoms. These results are supported in some prior research where some have noted that increased anxiety remains even after cessation of cannabis use, and the association between early cannabis use and later anxiety is greater among those with a history of daily adolescent cannabis use (Degenhardt et al., 2012).
We also sought to clarify associations between cannabis use and anxiety for men and women and note important similarities and differences across sex. Both models for men and women supported a dynamic interplay between anxiety and cannabis use. In particular, for men, our results mirrored that of the overall sample, supporting the substance-induced pathway and a significant, negative, association between prior levels of anxiety and subsequent changes in cannabis use, among proportional coupling parameters. This was also seen in our simulations when we forced increases in cannabis use, where men showed a rapid increase in anxiety, which was maintained through young adulthood even after cannabis use subsided. When we assessed forced changes in anxiety on cannabis use, men’s cannabis use changed very little. Thus, for men we show continued support for the substance- induced pathway and note opposite support for a symptom-driven pathway. However, given we show no effects for dynamic coupling parameters, this may indicate that for men, associations between cannabis use and anxiety are less about how change influences change and more about how prior trait-like aspects of cannabis and anxiety influence change.
For women, a much more complex story emerged. First, for women, the proportional coupling parameters supported both a substance-induced and a symptom-driven pathways. In our model for women, both dynamic coupling parameters were significant, giving us an opportunity to assess the dynamic interplay between cannabis use and anxiety symptoms. For example, it seems that when higher prior levels of cannabis use generate increases in anxiety symptoms, this recent change in anxiety is realized and is associated with a large decrease in cannabis use. Thus, it may be that some women who experience anxiety due to cannabis use are more likely to stop using cannabis to alleviate symptoms of anxiety. Support for this has been well documented such that those who use cannabis frequently tend to have higher levels of anxiety than those who do not use (Crippa et al., 2009). However, following the dynamic system from the other end, if increases in cannabis use are produced by greater prior levels of anxiety, this rapid increase in cannabis use is associated with a steady decrease in anxiety symptoms. Therefore, for some women, cannabis use may be a way to alleviate anxiety. This result is less consistent in the literature, but has recently seen some support in both animal and human studies. For example, some studies have found that specific aspects of cannabis, such as Cannabidiol (CBD), reduce anxiety behavior in mice (Zieba et al., 2019) and are a potential treatment for anxiety disorders (Blessing et al., 2015).
Overall, results add to the literature on directionality between cannabis use and anxiety and provide support for variation across men and women. Although the present study does shed light onto dynamic associations between cannabis use and anxiety, it raises important questions for future research. These questions mainly reside in how we, as researchers, contextualize cannabis use and anxiety: as stable, trait-like constructs or as constructs that change. Depending on how cannabis use and anxiety symptoms are conceptualized, support for our tested theories is either supported, not supported, or associations are in the opposite direction of what is theorized. For example, for the whole sample, we note full support of a substance-induced pathway across both estimated parameters; however, we found that greater anxiety is associated with less cannabis use, opposite of what a symptom-driven model posits. Thus, results partially support the well-established literature noting acute psychiatric symptoms following cannabis use. For example, results from a community survey in the 90’s on adverse effects of cannabis use found that acute anxiety or panic attacks were the most common problem noted (Thomas, 1996). More recently, a review of the literature addressing effects of cannabis potency on adolescent health showed that high-potency cannabis is associated with greater risk of anxiety and other mental health symptomology (Wilson et al., 2019).
Thus, the question remains, how can we reconcile these divergent results? Although contradictory results are typically viewed as problematic, results from the current study represent an opportunity to harness the strengths of distinct approaches to begin to form a consensus about how we assess change, and, further, what that may mean for future advancements in theory and practice. Theories such as the substance-induced pathway and symptom-driven pathway have certainly paved the way for uncovering important associations; however, the present study provides multiple ways of assessing change that may warrant expansion of these theories. Our model for women provides a good example of divergent results. A positive association was noted between prior, trait-like levels of anxiety predicting greater change (increasing) in anxiety symptomology. However, when change is predicted by prior change we see that cannabis use decreases among women who have recently experienced an increase in anxiety. This indicates that unlike existing theories, which assume unidirectional linear pathways, our results show a more integrated model in which bidirectional pathways between anxiety symptoms and cannabis use exist over the course of young adulthood.
4.1. Limitations and Conclusions
Our results should be interpreted in light of several limitations. First, data are self-reported and thus results are potentially biased due to shared variance. The measurement of anxiety (GAD-7) is a self-reported brief survey of anxiety symptoms and a well-established screener for possible anxiety disorder, but it is not a diagnostic measure, nor does it distinguish between anxiety disorders (e.g., panic disorder versus social phobia versus generalized anxiety). Second, although we do have temporally ordered data, we cannot determine causality, only association. Third, although we did address heterogeneity across participant sex, more research should be undertaken to address subgroup differences by race/ethnicity and sexual/gender identities.
This study takes an important first step in understanding pathways between cannabis use and anxiety symptoms during young adulthood for men and women, and the next step will be to continue to examine these pathways among young people who develop distinct (and co-occurring) diagnosed disorders. Findings fully supported a substance-induced pathway for men; however, results for women remain mixed. For those women who experienced increased anxiety due to prior cannabis use, cannabis may not be a useful mechanism for symptom relief. However, our results also note that when anxiety is a catalyst to greater changes in cannabis use, for some women, this greater cannabis use alleviates (reduces) anxiety symptoms. Future research should replicate and extend our results. Overall, our results pave the way for rethinking our guiding theories to include a more robust, flexible, and dynamic model for understanding associations between substance use and mental health symptomology during a key period of development.
Supplementary Material
HIGHLIGHTS.
Results indicated a complex and dynamic interplay between cannabis use and anxiety symptomology
For the overall sample and men, greater cannabis use predicted greater subsequent increases in anxiety; however, greater anxiety symptoms were associated with decreasing cannabis use.
Results for women were more complex, cannabis use decreases among women who have recently experienced an increase in anxiety
Funding:
Work on this article was supported by three grants from the National Institute of Alcohol Abuse and Alcoholism (R01AA016577; R01AA020883; R01AA025848) to Elizabeth D’Amico.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author disclosures
none
Conflict of Interest
No conflict declared
References
- Blessing EM, Steenkamp MM, Manzanares J, Marmar CR, 2015. Cannabidiol as a Potential Treatment for Anxiety Disorders. Neurother. 2015 124 12, 825–836. 10.1007/S13311-015-0387-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, Costello EJ, 2014. Longitudinal Patterns of Anxiety From Childhood to Adulthood: The Great Smoky Mountains Study. J. Am. Acad. Child Adolesc. Psychiatry 53, 21–33. 10.1016/J.JAAC.2013.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crippa JA, Zuardi AW, Martín-Santos R, Bhattacharyya S, Atakan Z, McGuire P, Fusar-Poli P, 2009. Cannabis and anxiety: a critical review of the evidence. Hum. Psychopharmacol. Clin. Exp 24, 515–523. 10.1002/HUP.1048 [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, Green HD, 2012. Preventing Alcohol Use with a Voluntary After-School Program for Middle School Students: Results from a Cluster Randomized Controlled Trial of CHOICE. Prev. Sci 13, 415–425. 10.1007/s11121-011-0269-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielsson AK, Lundin A, Agardh E, Allebeck P, Forsell Y, 2016. Cannabis use, depression and anxiety: A 3-year prospective population-based study. J. Affect. Disord 193, 103–108. 10.1016/J.JAD.2015.12.045 [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Coffey C, Romaniuk H, Swift W, Carlin JB, Hall WD, Patton GC, 2012. The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. 10.1111/j.1360-0443.2012.04015.x [DOI] [PubMed] [Google Scholar]
- Ehlers C, Gilder D, Gizer I, Addiction KW-, 2019, undefined, 2019. Indexing the “dark side of addiction”: substance-induced affective symptoms and alcohol use disorders. Addiction 114, 139–149. 10.1111/add.14431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garey L, Olofsson H, Garza T, Rogers AH, Kauffman BY, Zvolensky MJ, 2020. Directional Effects of Anxiety and Depressive Disorders with Substance Use: a Review of Recent Prospective Research. Curr. Addict. Reports 7, 344–355. 10.1007/S40429-020-00321-Z [DOI] [Google Scholar]
- Goodwin RD, Weinberger AH, Kim JH, Wu M, Galea S, 2020. Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. J. Psychiatr. Res 130, 441–446. 10.1016/J.JPSYCHIRES.2020.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm KKJ, Ram N, Estabrook R, 2016. Growth modeling: Structural equation and multilevel modeling approaches. Guilford Press, New York, New York, NY. [Google Scholar]
- Gustavson DE, Stallings MC, Corley RP, Miyake A, Hewitt JK, Friedman NP, 2017. Executive functions and substance use: Relations in late adolescence and early adulthood. J. Abnorm. Psychol 126, 257–270. 10.1037/abn0000250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayatbakhsh M, Najman J, Jamrozik K, Mamun A., Alati R, Bor W, 2007. Cannabis and anxiety and depression in young adults: a large prospective study. J. Am. Acad. Child Adolesc. Psychiatry 46, 408–417. [DOI] [PubMed] [Google Scholar]
- Khan S, Secades-Villa R, Okuda M, Wang S, Peres-Fuentes G, Kerridge B, Blanco C, 2013. Gender differences in cannabis use disorders: results from the National Epidemiologic Survey of Alcohol and Related Conditions. Drug Alcohol Depend. 130, 101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ, 1985. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am. J. Psychiatry 142, 1259–1264. 10.1176/ajp.142.11.1259 [DOI] [PubMed] [Google Scholar]
- Lev-Ran S, Roerecke M, Le Foll B, George TP, Mckenzie K, Rehm J, 2014. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol. Med 44. 10.1017/S0033291713001438 [DOI] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG, 2011. Gender Differences in Anxiety Disorders: Prevalence, Course of Illness, Comorbidity and Burden of Illness. J. Psychiatr. Res 45, 1027. 10.1016/J.JPSYCHIRES.2011.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onaemo VN, Fawehinmi TO, D’Arcy C, 2021. Comorbid Cannabis Use Disorder with Major Depression and Generalized Anxiety Disorder: A Systematic Review with Meta-analysis of Nationally Representative Epidemiological Surveys. J. Affect. Disord 281, 467–475. 10.1016/J.JAD.2020.12.043 [DOI] [PubMed] [Google Scholar]
- SAMHSA, 2021. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56; ). Rockville, MD. [Google Scholar]
- Schuckit MA, 2006. Comorbidity between substance use disorders and psychiatric conditions. Addiction 101, 76–88. 10.1111/J.1360-0443.2006.01592.X [DOI] [PubMed] [Google Scholar]
- Sharpe L, Sinclair J, Kramer A, De Manincor M, Sarris J, 2020. Cannabis, a cause for anxiety? A critical appraisal of the anxiogenic and anxiolytic properties. J. Transl. Med 18, 1–21. 10.1186/S12967-020-02518-2/TABLES/5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, 1999. Validation and utility of a self-report version of PREME-MD: The PHQ Primary Care Study. J. Am. Med. Assoc 282, 1737–1744. 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- Stapinski LA, Montgomery AA, Araya R, 2016. Anxiety, depression and risk of cannabis use: Examining the internalising pathway to use among Chilean adolescents. Drug Alcohol Depend. 166, 109–115. 10.1016/J.DRUGALCDEP.2016.06.032 [DOI] [PubMed] [Google Scholar]
- Van Gastel WA, Maccabe JH, Schubart CD, Van Otterdijk E, Kahn RS, Boks MPM, 2014. Cannabis Use is a Better Indicator of Poor Mental Health in Women Than in Men: A Cross-Sectional Study in Young Adults from the General Population. Community Ment. Health J 50, 823–830. 10.1007/s10597-014-9699-6 [DOI] [PubMed] [Google Scholar]
- Wilson J, Freeman TP, Mackie CJ, 2019. Effects of increasing cannabis potency on adolescent health. Lancet Child Adolesc. Heal 3, 121–128. 10.1016/S2352-4642(18)30342-0 [DOI] [PubMed] [Google Scholar]
- Zieba J, Sinclair D, Sebree T, Bonn-Miller M, Gutterman D, Siegel S, Karl T, 2019. Cannabidiol (CBD) reduces anxiety-related behavior in mice via an FMRP-independent mechanism. Pharmacol. Biochem. Behav 181, 93–100. 10.1016/J.PBB.2019.05.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


