PURPOSE:
Pain is a common complaint in patients with cancer presenting to the emergency department (ED). This prospective study evaluated whether biopsychosocial factors could help predict cancer patients with risk of higher pain severity, pain interference, and opioid consumption.
METHODS:
Patients with cancer presenting to the ED with a complaint of moderate-severe pain (≥ 4/10-numeric rating scale) completed validated self-report measures assessing sociodemographics, cancer-related treatments, pain severity and interference, medication use, and psychological symptoms (depression, anxiety, pain catastrophizing, and sleep disturbance). Opioids administered and subsequent hospitalization were abstracted. Univariable and multivariable regression analyses assessed factors associated with pain-related outcomes.
RESULTS:
Participants (n = 175) presented with a variety of cancer types, with 76% having metastatic disease and 42% reporting current outpatient opioid use. Higher pain catastrophizing, lower depressive symptoms, lower income, outpatient opioid use, and historical chronic pain were independently associated with worse pain (P ≤ .05). Higher pain catastrophizing, anxiety, sleep disturbance, outpatient opioid use, and education were independently associated with worse pain interference (P ≤ .05). The sole independent predictor of ED opioid administration was outpatient opioid use. Patients taking outpatient opioids were younger, had lower health literacy, worse pain catastrophizing, sleep disturbance, depression/anxiety, and greater rates of metastatic cancer and cancer-related surgery (P ≤ .05).
CONCLUSION:
Biopsychosocial factors, particularly pain catastrophizing, remained significantly associated with worse pain outcomes for patients with cancer in the ED even after controlling for demographic and clinical variables. Patient outpatient opioid use was independently associated with worse pain, interference, and greater opioid administration, identifying this as a marker for who may benefit most from adjuvant pharmacologic and behavioral interventions.
INTRODUCTION
Treating pain in patients with cancer is challenging, whether the pain is caused by local or metastatic cancer, chemotherapeutic agents, or from worsening of other noncancer etiologies.1,2 Despite a variety of pharmacologic (eg, opioids, nonsteroidal anti-inflammatories, and nerve medications) and behavioral interventions,3,4 managing pain remains a challenge for patients with cancer.5 More recently, patients with cancer face increased barriers to opioid access and may fear, and even intentionally avoid, opioid analgesics because of the stigma attached to opioids resulting from the opioid epidemic.6-8 These limitations, combined with the inherent limitations of opioid-based analgesia (eg, tolerance, hyperalgesia, and side effects), poor education about proper medication use, and limited access to alternative analgesics, can result in undertreated pain.6,7,9,10 Although opioids are effective at managing acute pain, the development of tolerance and hyperalgesic states associated with opioids makes the management of pain episodes among patients on chronic opioids particularly challenging.4,11,12 Pain during cancer also carries increased valence because of the potential negative implications of the pain (eg, fears of pain signifying disease progression), especially during acute pain episodes.13 The inability to effectively manage pain worsens patients' quality of life and leads to greater health care utilization, especially emergency department (ED) visits.5,14,15
Almost half of patients with cancer visit the ED at least once within the first year after diagnosis,16 and patients with cancer account for nearly four million annual ED visits in the United States.17 Patients often present to the ED with symptoms (eg, pain, nausea/vomiting, and respiratory distress) or complications from cancer treatment (eg, neutropenia) or progression.18 One of the most prominent primary complaints is pain,17,19,20 which accounts for 30%-65% of all ED visits among patients with cancer.14,18,21 Uncontrolled pain may represent a new and serious complication (eg, new fracture), worsening of a previous pain source, or an exhaustion of the resources available to a patient to self-manage ongoing pain.5,18 Although urgent evaluation is in fact often needed, episodic increases of pain resulting from difficulty with pain self-management, in the absence of urgent cancer-related complications, place a significant burden on patients' quality of life, their caregivers, hospital staff, and health care systems.14,20,22,23 As EDs experience capacity issues during the COVID-19 pandemic, reducing avoidable and/or unnecessary ED visits would likely benefit patients and payers alike.23 Of note, a two-fold increase in the incidence of opioid overdose-related ED visits for patients with cancer was observed between 2006 and 2015 in the United States.24 More comprehensive identification of relevant pain modulatory predictors may inform personalized outpatient cancer pain management, potentially identifying patients who would benefit most from proactive intervention.
The biopsychosocial model of chronic pain (pain lasting ≥ 3 months) highlights the importance of not only biological factors on pain but also physiological, cognitive (eg, pain appraisals), behavioral (eg, activity levels), affective, and social/environmental factors.28 Identifying biopsychosocial predictors of worse pain and higher analgesic requirements at the point of ED admission among patients with cancer can, therefore, inform patient-centered, targeted interventions to improve pain outcomes. Several studies to date have solely evaluated cancer patients' demographics and disease factors, without assessing psychological processes that are highly relevant to pain modulation, in studies of pain during ED admissions.19,20,22,29 Thus, these previous studies have not comprehensively evaluated all classes of potential predictors of pain together simultaneously to assess whether these biopsychosocial factors have an independent influence on pain outcomes and opioid administration among patients with cancer. Including biopsychosocial factors may help explain individual variability above and beyond demographic or disease variables. As such, this prospective cohort study used simultaneously-administered, validated measures of psychological functioning and pain outcomes to assess the unique relationships between a variety of potential biopsychosocial predictors (sociodemographics, disease status, surgical history, opioid use, and psychological health) and pain outcomes (pain severity and interference and hourly opioid analgesics administered in the ED). We hypothesized that patients with greater psychological burden (catastrophizing, anxiety, and depression) would report worse pain and require more opioids during their ED stay, even while controlling for other potential drivers of these outcomes (fewer socioeconomic resources, lower health literacy, and greater disease burden).
METHODS
This prospective observational cohort study recruited patients presenting to the ED at Brigham and Women's Hospital (BWH), an urban, academic, tertiary care center in Boston, MA, between January 2020 and June 2021 (recruitment paused between March 2020 and August 2020 because of COVID-19). The ED evaluates approximately 60,000 individuals annually and serves as the primary ED for the Dana-Farber Cancer Institute. Approximately 30% of ED visits at BWH involve patients with cancer. Study procedures were approved by the Mass General Brigham Institutional Review Board. Research assistants identified eligible patients and approached them to gauge willingness to participate after confirming medical stability with the medical team. Inclusion criteria included age 18 years and older, self-reported cancer treatment (eg, chemotherapy, surgery, immunotherapy, and radiation) within the past 2 years, and a complaint of moderate-severe cancer-related pain (≥ 4/10). Exclusion criteria were inability/unwillingness to complete or understand questionnaires, acute medical instability, primary psychiatric complaint, or only a non–life-threatening and/or completely resolved cancer diagnosis (nonmetastatic melanoma, squamous cell, or thyroid carcinoma).
Measures
Patients completed self-report measures assessing sociodemographics (race, education level, and household income), medication use, and validated psychosocial assessment tools. Patients self-reported recent cancer-related surgical procedures in the past 3 months, history of chronic pain (pain present for ≥ 3 months) before their cancer diagnosis, and current outpatient opioid use for pain management. Depression, anxiety, and sleep disturbance were assessed using the NIH Patient Reported Outcome Measurement Information System (PROMIS) short-forms.30 PROMIS measures use a 5-point Likert scale, with higher scores indicating higher symptom severity. Pain catastrophizing was measured using the 13-item Pain Catastrophizing Scale.31 Pain Catastrophizing Scale items are rated on a 5-point Likert scale, where higher scores reflect greater pain catastrophizing (range, 0-52). Age, sex, subsequent hospitalization status (patients admitted directly from the ED), length of stay, historical and recent cancer treatment (chemotherapy, radiation, and immunotherapy), and metastatic disease status were abstracted from the medical record. Outpatient opioid prescriptions were also abstracted from the medical record; however, to have a more accurate measure of medication usage, the patients self-report of opioid consumption was used for analysis.
Pain severity and interference.
Patients self-reported pain severity and pain interference using the Brief Pain Inventory (BPI).32 The BPI queries about worst, least, and average pain within the past 7 days, as well as current pain, with the four ratings averaged to calculate pain severity (range, 0-10). The BPI also contains 10 questions asking patients to rate the degree to which pain interferes with their daily activities. Items are then summed to give the pain interference (range, 0-100).
ED opioid administration.
All opioids administered while in the ED were normalized by converting each opioid administration to morphine milligram equivalents (MMEs). MMEs per hour were calculated by dividing total MMEs by total time (in hours) in the ED.
Statistical Analysis
To evaluate the relationships between independent (sociodemographics, cancer disease status, recent surgical history, mood, catastrophizing, sleep, current opioid use, and previous history of chronic pain) and dependent variables (pain severity, pain interference, MME per hour, and hospital admission), we conducted univariable and multivariable linear and logistic regression. Selection of independent variables for inclusion in the multivariable models was informed by variables identified as significant on the univariable analysis. Multicollinearity diagnostics indicated no violations (variance inflation factor < 4.0).33,34 For exploratory group comparisons, Mann-Whitney U, Wilcoxon signed-ranks tests, and χ2 tests were used to compare patients taking outpatient opioids to those who were not. All statistical analyses were performed using SPSS-v27.
RESULTS
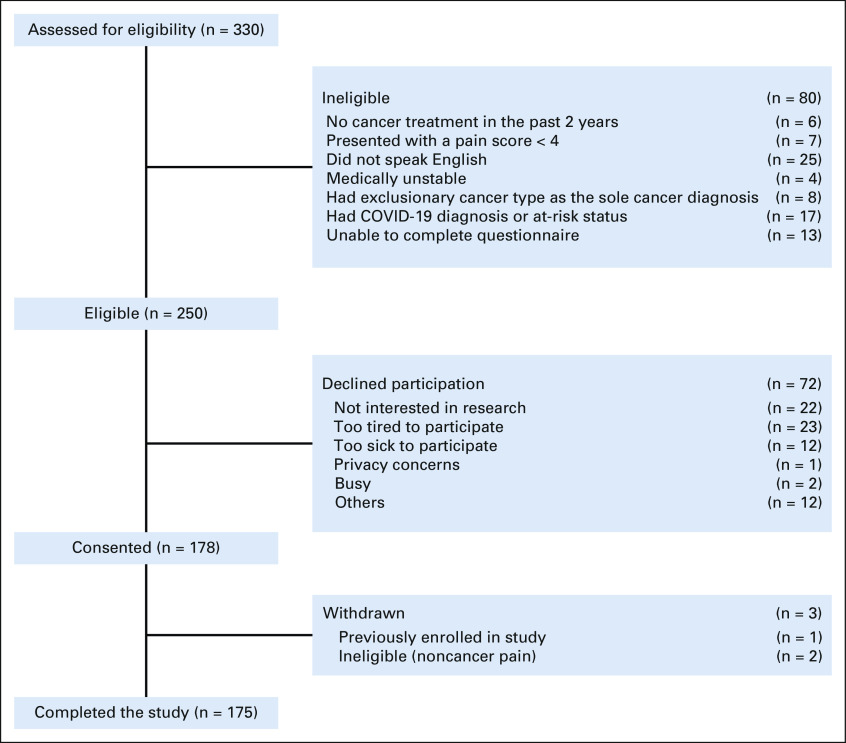
In total, 330 patients were screened, 250 were found to be eligible, and 178 signed consent (Appendix Fig A1, online only). Participants with complete data (n = 175) were 55% female and 81% White, with a variety of cancer types, frequently with metastatic disease (76%), and most had undergone some treatment for cancer within the past 6 weeks (71%; Table 1). The majority reported pain as the primary reason for the ED visit (69%). Taking outpatient opioids to manage pain was relatively common but not ubiquitous (42%); reported frequency of nonopioid OTC pain medications among the participants was 25%, and cannabis use was 8.5%. Roughly 30% of patients reported chronic pain before cancer diagnosis. Mean scores of depression, anxiety, and sleep disturbance in the 7 days before admission were close to 50th percentile using PROMIS t-scoring, and participants reported a relatively wide range of pain catastrophizing scores (18.1 ± 12.5). Patients remained in the ED for an average of 11 ± 10 hours (range, 2-83, median = 7); 59% received opioids during their ED stay, and 65% were admitted as hospital inpatients from the ED. Patients reported variable levels of worst pain (mean 7.6 ± 2.7), BPI mean pain severity (mean 5.9 ± 3.0), and BPI pain interference (mean 50.7 ± 27.0) in the week preceding their ED visit.
TABLE 1.
Participant Demographics, Clinical Characteristics, Psychosocial Measures, and Pain

Univariable Linear Regression Analyses
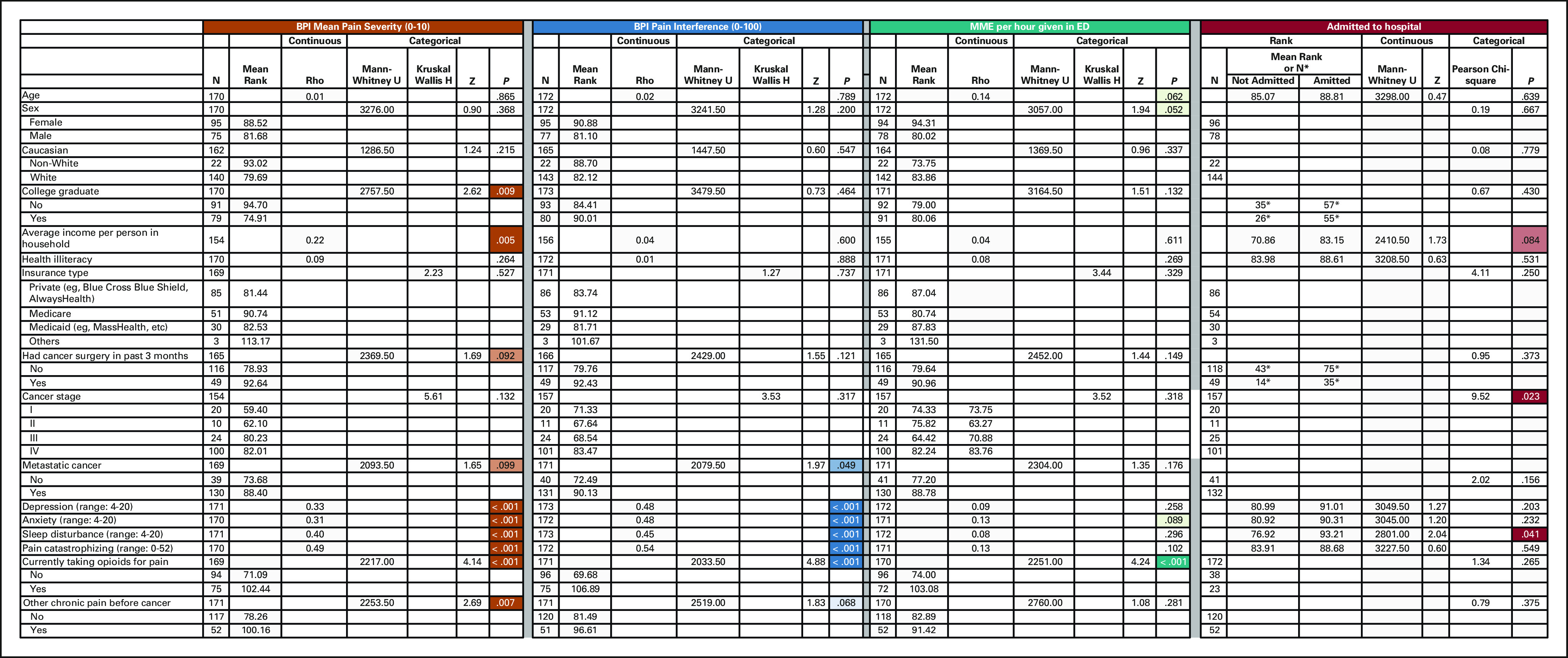
Univariable associations of sociodemographic, disease, opioid use, and psychosocial predictors with pain-related outcomes was assessed using simple linear (pain and opioid consumption) or logistic (hospital admission) regression (Appendix Fig A2, online only). Lower education, higher income, and recent cancer surgery were associated with greater pain severity, but not other outcomes. Older age and female sex were associated with higher hourly MME administration, but not other outcomes. More advanced cancer stage was only associated with subsequent hospital admission, but not other outcomes. Depression, pain catastrophizing, chronic pain before cancer diagnosis, and metastatic cancer were all associated with both greater pain severity and pain interference, but not hourly MME administration in the ED. Greater sleep disturbance was associated with greater pain interference and hospital admission. Higher anxiety and current outpatient opioid use were significantly related to pain severity, pain interference, and hourly MME administration, but not hospital admission.
Multivariable Linear Regression Models
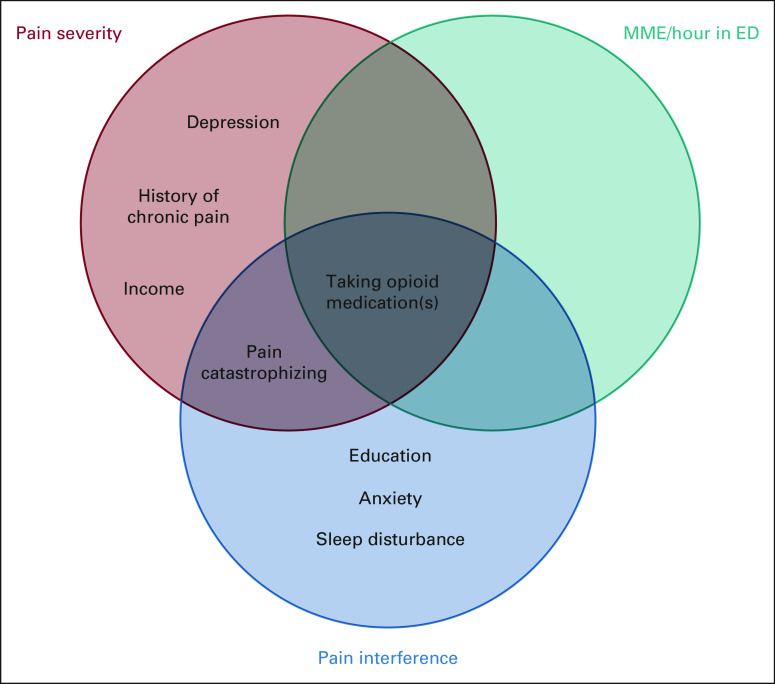
Recognizing that many sociodemographic, disease, treatment, and psychological variables are themselves interrelated (ie, metastasis related to greater opioid use), we performed multivariable linear regression analyses to identify independent predictors of pain outcomes, including all variables that were significantly associated (P ≤ .1) with at least one of the predetermined outcomes (pain severity, pain interference, and opioid use) on univariable analysis. Figure 1 summarizes variables that were independently associated with these different outcomes on multivariable analysis.
FIG 1.
Overlap of factors that were independently associated with pain-related outcomes in multivariable regression analyses. ED, emergency department; MME, morphine milligram equivalent.
Independent Predictors of Pain Severity
Lower income (β = −.17, P = .015), greater pain catastrophizing (β = .43, P ≤ .001), lower depressive symptoms (β = −.27, P = .035), current outpatient opioid use (β = .33, P ≤ .001), and previous history of chronic pain before cancer (β = .17, P = .019) were all independently associated with greater pain severity (Table 2, Fig 1).
TABLE 2.
Multivariable Linear Regression Assessing Independent Associations With Pain Severity

Independent Predictors of Pain Interference
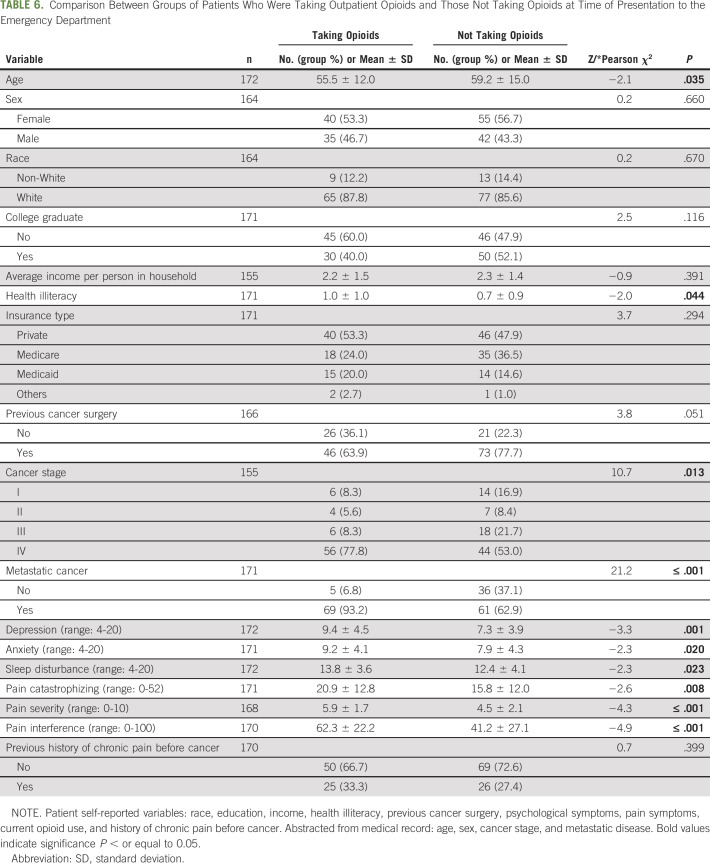
Having a college degree or higher (β = .17 P = .021), greater pain catastrophizing (β = .26, P = .004), anxiety symptoms (β = .23, P = .047), and sleep disturbance (β = .28, P = .001), and current outpatient opioid use (β = .32, P ≤ .001) were independently associated with greater pain interference (Table 3, Fig 1).
TABLE 3.
Multivariable Linear Regression Assessing Independent Associations With Pain Interference
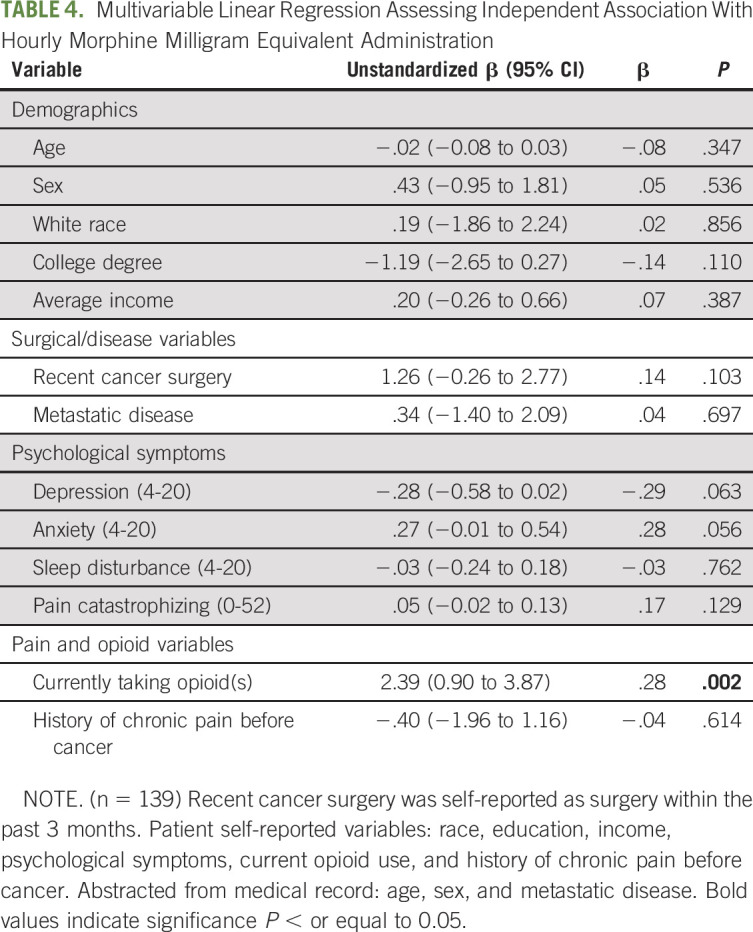
Independent Predictors of Hourly Opioid Administration
Only current outpatient opioid use (β = .28, P = .002) was independently associated with greater MME/h while in the ED. Anxiety and depressive symptoms were marginally associated with hourly MME administration (P = .063 and .056, respectively; Table 4, Fig 1).
TABLE 4.
Multivariable Linear Regression Assessing Independent Association With Hourly Morphine Milligram Equivalent Administration
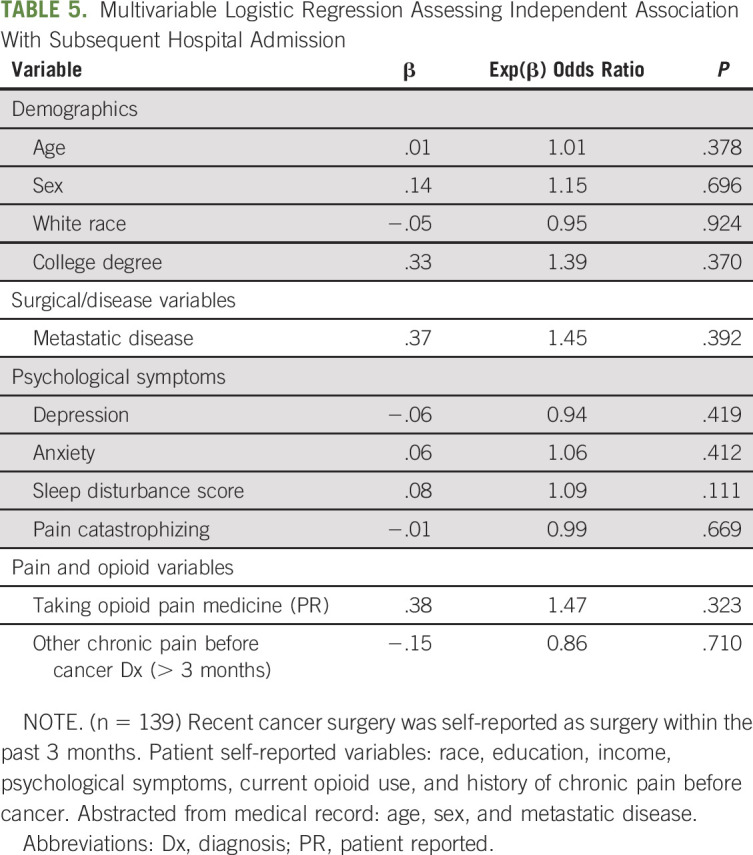
Hospitalization After ED Evaluation
In this multiple logistic regression model, none of the sociodemographic, disease, surgical, psychological, or opioid variables were independently associated with subsequent hospital admission from the ED (Table 5).
TABLE 5.
Multivariable Logistic Regression Assessing Independent Association With Subsequent Hospital Admission
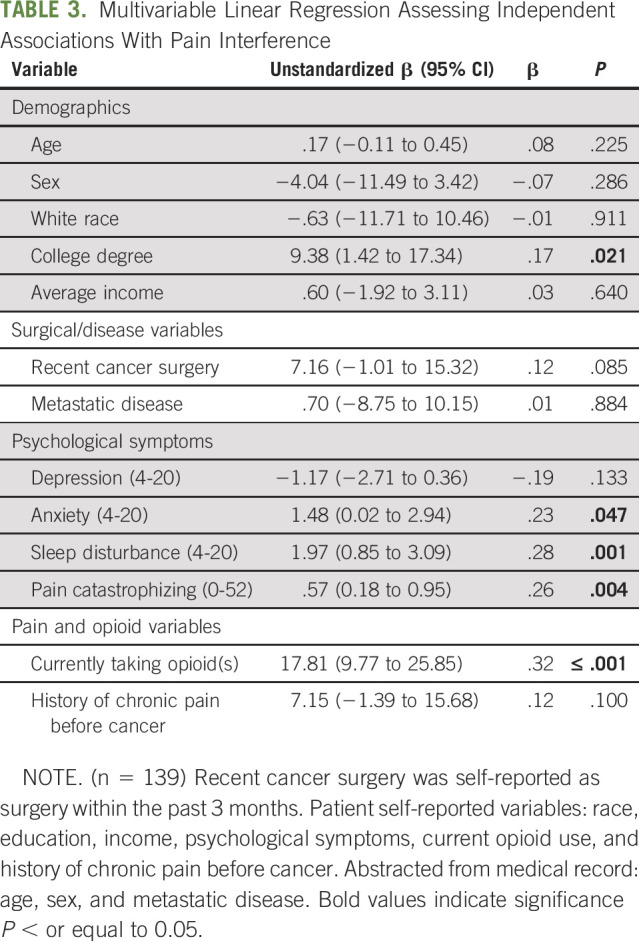
Comparison of Patients Taking Outpatient Opioids Versus Those Not Taking Opioids
Because current outpatient opioid use was the only significant independent predictor of pain severity, pain interference, and ED opioid administration, we further investigated patient characteristics of this group. Patients who reported current outpatient opioid use were significantly younger, had lower health literacy, and had higher rates of advanced cancer, as well as significantly higher depression, anxiety, sleep disturbance, and pain catastrophizing (Table 6).
TABLE 6.
Comparison Between Groups of Patients Who Were Taking Outpatient Opioids and Those Not Taking Opioids at Time of Presentation to the Emergency Department
DISCUSSION
In this prospective cohort study of patients with cancer presenting to the ED with pain, we sought to identify patient-level, biopsychosocial predictors associated with worse pain, greater opioid administration, and subsequent hospitalization. Our hypothesis that greater psychological burden would be independently associated with worse pain outcomes was generally supported. Several psychological factors, most prominently greater pain catastrophizing, but also anxiety and sleep disturbance, were independently associated with worse pain, even after controlling for the impact of demographic and disease variables. However, psychological factors were not independently associated with greater opioid administration or subsequent hospitalization. Interestingly, but perhaps not surprisingly, current outpatient opioid use was an independent predictor of greater opioid administration in the ED. Outpatient opioid use was also an independent predictor of greater pain severity and interference, indicating a greater difficulty in managing pain, despite higher overall opioid use. Individuals reporting current outpatient opioid use were significantly younger, had higher rates of metastatic disease, and had higher psychological symptoms including greater levels of depression, anxiety, pain catastrophizing, and more disturbed sleep.
Patients in this cohort reported relatively high levels of pain, consistent with previous studies finding pain to be an important driving complaint in ED visits for patients with cancer.14,18,21 Hospitalization rates in this sample (65%) were similar to other cancer pain ED studies.18,21 The current report corroborated previous findings that up to 60% of patients taking opioids for cancer pain continue to report significant pain.35 Our subsample of participants (41%) who reported taking outpatient opioids also endorsed mean pain scores in the moderate-severe range (5.9 ± 1.7 of 10). One striking finding of the multiple regression analyses was the consistency of this factor (taking outpatient opioids) as an independent predictor of both pain outcomes and hourly opioid administration while taking into account many biopsychosocial characteristics. It was in fact the lone independent predictor of opioid administration in the ED. A unique aspect of this study was the simulataneous entry of a wide range of potential biopsychosocial predictors into a multivariable model, after which several factors, including metastatic disease status and race, were not independently predictive of opioid administration.
Although psychological factors were not directly related to hourly ED opioid administration or subsequent hospitalization in the multivariable models, psychological symptoms, including anxiety and pain catastrophizing, were independently associated with worse pain severity and interference. Patients with cancer who presented to the ED with pain and reported taking outpatient opioids also had higher rates of psychological symptoms. Contextually, psychological distress generally increases during cancer treatment, and pain during cancer has been associated with significant suffering and worry about the underlying cause of pain (eg, fears that pain signifies worsening disease or progression).36,37 Psychological distress and pain also seem to reciprocally augment each other.38 Pain catastrophizing, which includes rumination about pain, magnification of pain symptoms, and feelings of helplessness in the face of pain, has been consistently associated with worse pain, greater opioid use, and more frequent ED visits in other cohorts with pain.25,26 As stressors increase (ie, previous chronic pain, pain catastrophizing, worsening disease), any small increase can may push a patient past their pain threshold, where previous opioid doses become insufficient—this process may explain why those taking outpatient opioids experienced significantly greater acute pain leading to an ED admission and the need for further evalaution or increased opioids. We found that pain catastrophizing independently predicted worse pain severity and interference, yet these variables were not related to hourly opioid consumption in the ED, in contrast to previous studies associating psychological variables with higher rates of opioid misuse/overuse and resulting ED visits among patients with noncancer pain.40 Although recognition of the opioid epidemic may be curbing opioid overprescription, treatment for concurrent psychological symptoms among patients with cancer is certainly an attractive alternative to lessen the overreliance on opioids in patients with cancer.
Future studies should longitudinally evaluate the relationship between biopsychosocial factors and pain among patients with cancer. Although opioids are essential for cancer pain treatment, supplementing pharmacologic treatment with accessible behavioral interventions aimed at pain-related psychological processes (eg, catastrophizing) may improve analgesia and more holistically alleviate cancer pain suffering—as well as potentially reduce ED use for worsening pain.1,2,36,41 Several investigations have demonstrated that deploying alternative treatments for cancer pain are feasible and may reduce both anxiety and pain.42-45 Targeted behavioral therapies may be even more effective in improving pain and psychological outcomes for patients with elevated psychological distress, concurrent chronic pain, higher education, lower income, and metastatic disease, although careful attention to patient characterization within future trials is needed to discern differential efficacy. Future studies using remote symptom monitoring systems which track both pain/psychological symptomatology are needed to gauge the efficacy of such a system to help personalize pain management and prevent ED admissions. Although biopsychosocial factors were not found to be related to the likelihood of hospital admission, future studies may explore whether a variety of preventive pain interventions (patient-centered education on analgesic use and cognitive behavioral therapy directed at patients' pain-related catastrophic thoughts) may help to avoid ED admissions for uncontrolled pain.27,36,41
Several limitations are important to consider. The sampling method was relatively inclusive from a diagnostic standpoint, encompassing a variety of cancer types and stages of progression. Participants had complaints beyond pain and potentially other overlapping sources of pain, ultimately increasing variability in the sample. At the same time, the sample was less racially diverse and more educated than the general population, which may preclude findings from being widely generalizable, although demographics were consistent with patients seen at this tertiary referral level-1 trauma center adjacent to a highly ranked cancer center. Future studies are needed to evaluate these relationships in more diverse, lower income, and community settings. Race and socioeconomic status are known to influence pain management in patients with cancer,8,46-51 underscoring the importance of understanding whether race moderates the relationship of psychosocial factors to worse pain outcomes.6,39 Finally, some patients were recruited during the time of the COVID-19 pandemic, although recruitment was paused during the months of heaviest COVID-related hospitalizations, which may have influenced whether some patients delayed presenting to the ED.
In conclusion, we found that greater psychosocial distress independently predicted worse pain outcomes in this sample of patients with cancer presenting to the ED with acute pain complaints. Taking outpatient opioids served as a consistent risk factor for both worse pain and hourly opioid administration in the ED. Future research which evaluates whether cancer patients with these characteristics may benefit from being identified earlier and targeted for augmentation of pharmacologic analgesia with behavioral interventions is necessary and important for achieving individualized, optimal pain management.
APPENDIX
FIG A1.
Consort diagram of the study.
FIG A2.
Univariable linear regressions assessing independent associations with pain severity, pain interference, and hourly MME administration. Univariable logisitic regression assessing independent associations with hospital admission. BPI, Brief Pain Inventory; ED, emergency department; MME, morphine milligram equivalent.
Desiree Azizoddin
Research Funding: National Palliative Care Research Center
Peter Chai
Stock and Other Ownership Interests: Biobot Analytics
Research Funding: E Ink Corporation, NIDA, Hans and Mavis Lopater Foundation, Bill and Melinda Gates Foundation
Lily Johnsky
Employment: Iterative Scopes
Travel, Accommodations, Expenses: Iterative Scopes
Edward Boyer
Research Funding: NIDA
Expert Testimony: Various law firms
Kristin L. Schreiber
Employment: Pfizer (I)
Stock and Other Ownership Interests: Pfizer (I)
Research Funding: NIGMS
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented at the ASCO Quality Care Symposium 2021, September 24-25, 2021; Society of Behavioral Medicine Annual Conference 2022 (Abstract Award Winner), April 6-9, 2021.
SUPPORT
NIH/NIGMS: R35 GM128691 (K.L.S.), The National Palliative Care Research Center Kornfeld Scholars Award (D.R.A.), PRC: K23DA044874, R44DA051106, Hans and Mavis Loapter Psychosocial Foundation, Bill and Melinda Gates Foundation INV-002177, Defense Advanced Research Projects Agency HR001120S0041.
AUTHOR CONTRIBUTIONS
Conception and design: Desiree R. Azizoddin, K. Mikayla Flowers, Peter Chai, Gabrielle Cremone, Robert Edwards, Edward Boyer, Kristin L. Schreiber
Financial support: Desiree R. Azizoddin, Peter Chai, Kristin Schreiber
Administrative support: Desiree R. Azizoddin, Kristin Schreiber
Provision of study materials or patients: Desiree R. Azizoddin, Edward Boyer, Kristin Schreiber
Collection and assembly of data: Desiree R. Azizoddin, Meghan Beck, K. Mikayla Flowers, Lily Johnsky, Gabrielle Cremone, Adriana Hasdianda,
Data analysis and interpretation: Desiree R. Azizoddin, K. Mikayla Flowers Jenna M. Wilson, Kristin Schreiber
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Psychological Evaluation of Patients With Cancer Presenting to the Emergency Department With Pain: Independent Predictors of Worse Pain Severity, Interference, and Higher Hourly Opioid Administration
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Desiree Azizoddin
Research Funding: National Palliative Care Research Center
Peter Chai
Stock and Other Ownership Interests: Biobot Analytics
Research Funding: E Ink Corporation, NIDA, Hans and Mavis Lopater Foundation, Bill and Melinda Gates Foundation
Lily Johnsky
Employment: Iterative Scopes
Travel, Accommodations, Expenses: Iterative Scopes
Edward Boyer
Research Funding: NIDA
Expert Testimony: Various law firms
Kristin L. Schreiber
Employment: Pfizer (I)
Stock and Other Ownership Interests: Pfizer (I)
Research Funding: NIGMS
No other potential conflicts of interest were reported.
REFERENCES
- 1.Swarm R, Abernethy AP, Anghelescu DL, et al. : Adult cancer pain. J Natl Compr Cancer Netw 8:1046-1086, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui D, Bruera E: A personalized approach to assessing and managing pain in patients with cancer. J Clin Oncol 32:1640-1646, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johannsen M, Farver I, Beck N, et al. : The efficacy of psychosocial intervention for pain in breast cancer patients and survivors: A systematic review and meta-analysis. Breast Cancer Res Treat 138:675-690, 2013 [DOI] [PubMed] [Google Scholar]
- 4.Dy SM, Asch SM, Naeim A, et al. : Evidence-based standards for cancer pain management. J Clin Oncol 26:3879-3885, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Kwon JH: Overcoming barriers in cancer pain management. J Clin Oncol 32:1727-1733, 2014 [DOI] [PubMed] [Google Scholar]
- 6.Bulls HW, Chu E, Goodin BR, et al. : Framework for opioid stigma in cancer pain. Pain 163:e182-e189, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azizoddin DR, Knoerl R, Adam R, et al. : Cancer pain self-management in the context of a national opioid epidemic: Experiences of patients with advanced cancer using opioids. Cancer 127:3239-3245, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bulls HW, Hoogland AI, Craig D, et al. : Cancer and opioids: Patient experiences with stigma (COPES)-A pilot study. J Pain Symptom Manage 57:816-819, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meghani SH, Rosa WE, Chittams J, et al. : Both race and insurance type independently predict the selection of oral opioids prescribed to cancer outpatients. Pain Manag Nurs 21:65-71, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meghani SH, Thompson AM, Chittams J, et al. : Adherence to analgesics for cancer pain: A comparative study of African Americans and Whites using an electronic monitoring device. J Pain 16:825-835, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volkow ND, McLellan AT: Opioid abuse in chronic pain—Misconceptions and mitigation strategies. N Engl J Med 374:1253-1263, 2016 [DOI] [PubMed] [Google Scholar]
- 12.Yoong J, Traeger LN, Gallagher ER, et al. : A pilot study to investigate adherence to long-acting opioids among patients with advanced lung cancer. J Palliat Med 16:391-396, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Thuné-Boyle IC, Myers LB, Newman SP: The role of illness beliefs, treatment beliefs, and perceived severity of symptoms in explaining distress in cancer patients during chemotherapy treatment. Behav Med 32:19-29, 2006 [DOI] [PubMed] [Google Scholar]
- 14.Elsayem AF, Merriman KW, Gonzalez CE, et al. : Presenting symptoms in the emergency department as predictors of intensive care unit admissions and hospital mortality in a comprehensive cancer center. JCO Oncol Pract 12:e554-e563, 2016 [DOI] [PubMed] [Google Scholar]
- 15.Chaftari P, Lipe DN, Wattana MK, et al. : Outcomes of patients placed in an emergency department observation unit of a comprehensive cancer center. JCO Oncol Pract 18:e574-e585, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Panattoni L, Fedorenko C, Greenwood-Hickman MA, et al. : Characterizing potentially preventable cancer-and chronic disease–related emergency department use in the year after treatment initiation: A regional study. JCO Oncol Pract 14:e176-e185, 2018 [DOI] [PubMed] [Google Scholar]
- 17.Hsu J, Donnelly JP, Moore JX, et al. : National characteristics of Emergency Department visits by patients with cancer in the United States. Am J Emerg Med 36:2038-2043, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caterino JM, Adler D, Durham DD, et al. : Analysis of diagnoses, symptoms, medications, and admissions among patients with cancer presenting to emergency departments. JAMA Netw Open 2:e190979, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbera L, Atzema C, Sutradhar R, et al. : Do patient-reported symptoms predict emergency department visits in cancer patients? A population-based analysis. Ann Emerg Med 61:427-437.e5, 2013 [DOI] [PubMed] [Google Scholar]
- 20.Gallaway MS, Idaikkadar N, Tai E, et al. : Emergency department visits among people with cancer: Frequency, symptoms, and characteristics. J Am Coll Emerg Physicians Open 2:e12438, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayer DK, Travers D, Wyss A, et al. : Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 29:2683-2688, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coyne CJ, Reyes-Gibby CC, Durham DD, et al. : Cancer pain management in the emergency department: A multicenter prospective observational trial of the Comprehensive Oncologic Emergencies Research Network (CONCERN). Support Care Cancer 29:4543-4553, 2021 [DOI] [PubMed] [Google Scholar]
- 23.Vandyk AD, Harrison MB, Macartney G, et al. : Emergency department visits for symptoms experienced by oncology patients: A systematic review. Support Care Cancer 20:1589-1599, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Jairam V, Yang DX, Yu JB, et al. : Emergency department visits for opioid overdoses among patients with cancer. J Natl Cancer Inst 112:938-943, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharifzadeh Y, Kao MC, Sturgeon JA, et al. : Pain catastrophizing moderates relationships between pain intensity and opioid prescription: Nonlinear sex differences revealed using a learning health system. Anesthesiology 127:136-146, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hackett J, Godfrey M, Bennett MI: Patient and caregiver perspectives on managing pain in advanced cancer: A qualitative longitudinal study. Palliat Med 30:711-719, 2016 [DOI] [PubMed] [Google Scholar]
- 27.Azizoddin DR, Schreiber K, Beck MR, et al. : Chronic pain severity, impact, and opioid use among patients with cancer: An analysis of biopsychosocial factors using the CHOIR learning health care system. Cancer 127:3254-3263, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gatchel RJ, Peng YB, Peters ML, et al. : The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol Bull 133:581-624, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Hong AS, Sadeghi N, Harvey V, et al. : Characteristics of emergency department visits and select predictors of hospitalization for adults with newly diagnosed cancer in a safety-net health system. JCO Oncol Pract 15:e490-e500, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cella D, Riley W, Stone A, et al. : The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 63:1179-1194, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan MJ, Bishop SR, Pivik J: The pain catastrophizing scale: Development and validation. Psychol Assess 7:524-532, 1995 [Google Scholar]
- 32.Tan G, Jensen MP, Thornby JI, et al. : Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 5:133-137, 2004 [DOI] [PubMed] [Google Scholar]
- 33.Mayers R: Classical and Modern Regression with Applications. Boston, MA, PWS-Kent, 1990 [Google Scholar]
- 34.Menard S: Applied Logistic Regression Analysis. London, UK, Sage, 2002 [Google Scholar]
- 35.van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, et al. : Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. J Pain Symptom Manage 51:1070-1090.e9, 2016 [DOI] [PubMed] [Google Scholar]
- 36.Syrjala KL, Jensen MP, Mendoza ME, et al. : Psychological and behavioral approaches to cancer pain management. J Clin Oncol 32:1703-1711, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carlson LE, Waller A, Mitchell AJ: Screening for distress and unmet needs in patients with cancer: Review and recommendations. J Clin Oncol 30:1160-1177, 2012 [DOI] [PubMed] [Google Scholar]
- 38.Vadivelu N, Kai AM, Kodumudi G, et al. : Pain and psychology—A reciprocal relationship. Ochsner J 17:173-180, 2017 [PMC free article] [PubMed] [Google Scholar]
- 39.Yennurajalingam S, Arthur J, Reddy S, et al. : Frequency of and factors associated with nonmedical opioid use behavior among patients with cancer receiving opioids for cancer pain. JAMA Oncol 7:404-411, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jairam V, Yang DX, Yu JB, et al. : Emergency department visits for opioid overdoses among patients with cancer. J Natl Cancer Inst 112:938-943, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gorin SS, Krebs P, Badr H, et al. : Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol 30:539, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keefe FJ: Managing acute pain with opioids in the emergency department: A teachable moment? Am J Public Health 112:S9-S11, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chai PR, Gale JY, Patton ME, et al. : The impact of music on nociceptive processing. Pain Med 21:3047-3054, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chai PR, Schwartz E, Hasdianda MA, et al. : A brief music app to address pain in the emergency department: Prospective study. J Med Internet Res 22:e18537, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bohnert AS, Bonar EE, Cunningham R, et al. : A pilot randomized clinical trial of an intervention to reduce overdose risk behaviors among emergency department patients at risk for prescription opioid overdose. Drug Alcohol Depend 163:40-47, 2016 [DOI] [PubMed] [Google Scholar]
- 46.Mack DS, Hunnicutt JN, Jesdale BM, et al. : Non-Hispanic Black-White disparities in pain and pain management among newly admitted nursing home residents with cancer. J Pain Res 11:753-761, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Enzinger AC, Ghosh K, Keating NL, et al. : US trends in opioid access among patients with poor prognosis cancer near the end-of-life. J Clin Oncol 39:2948-2958, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meghani SH, Byun E, Gallagher RM: Time to take stock: A meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med 13:150-174, 2012 [DOI] [PubMed] [Google Scholar]
- 49.Pletcher MJ, Kertesz SG, Kohn MA, et al. : Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA 299:70-78, 2008 [DOI] [PubMed] [Google Scholar]
- 50.Tamayo-Sarver JH, Hinze SW, Cydulka RK, et al. : Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health 93:2067-2073, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ludwick A, Corey K, Meghani S: Racial and socioeconomic factors associated with the use of complementary and alternative modalities for pain in cancer outpatients: An integrative review. Pain Manag Nurs 21:142-150, 2020 [DOI] [PubMed] [Google Scholar]