Abstract
Background
India, the seventh-largest country in the world and the second-most populated faces enormous challenges when it comes to healthcare. The country’s healthcare system was close to collapse due to the detrimental effects of the COVID-19 pandemic. Telehealth, which enables treating patients remotely, played a critical role during these challenging times. This systematic review investigates in detail the role of telehealth during COVID-19 and its application beyond the pandemic.
Methods
Database searches on PubMed, Scopus, Science Direct and Web of Science were carried out for studies published on telehealth, and articles were included if they focused on any audio or video telehealth consultation during the pandemic in India. Findings were synthesised into three main themes: applications, benefits and challenges of telehealth services. Methodological quality was assessed using JBI critical appraisal tools.
Results
The initial search on databases yielded 1143 articles. Of those, 19 met the eligibility criteria. Findings highlight the effective utilisation of telehealth across multiple medical specialities. Although insufficient technological infrastructure and other barriers due to the virtual consultation challenge the successful implementation of telehealth in India, it has the potential to bridge the rural-urban healthcare divide with cost-effective and easily accessible services.
Conclusion
High patient/provider satisfaction underscores the need to integrate telehealth into routine healthcare practices in the country. However, the review urges the government and healthcare practitioners to address the telehealth challenges with prime importance to ensure quality healthcare throughout the nation even after the pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-022-08970-8.
Keywords: Telehealth, Mobile health, Remote consultation, COVID-19, India, Systematic review
Background
Respiratory viral pandemics are a massive challenge for nations and their healthcare systems. Research on earlier pandemics revealed that various approaches, such as non-pharmaceutical interventions, healthcare policies, mental health interventions, communication strategies, epidemiological surveillance strategies, and workplace and university measures employed by different countries could limit the spread of viral infections [1]. Similarly, the recent COVID-19 pandemic has also posed unanticipated hurdles to public healthcare systems across the world [2]. Based on previous experience, many countries enacted a variety of pharmaceutical (e.g., vaccination) and non-pharmaceutical (e.g., curfew) interventions as COVID-19 containment measures [3]. Yet, most of their available healthcare resources had to head off to deal with virus-related emergencies [4]. Additionally, the smooth functioning of the healthcare system was hampered due to patients’ and healthcare workers’ fear of infection and mobility restrictions [5]. Apparently, social isolation and lockdown made medical assistance difficult and people’s lives miserable [6]. Unfortunately, individuals with various illnesses, such as hypertension, diabetes, joint and musculoskeletal ailments, and neurological diseases, had limited access to healthcare services during the lockdown [7]. However, lockdowns got extended as most COVID-19 infections are caused by asymptomatic carriers [8]. As a result, reducing in-person interactions with patients became indispensable. Thus, there has been an urgent need to discover new ways to provide healthcare. This necessity has resulted in the rapid implementation and expansion of telehealth services worldwide [9, 10], and healthcare providers have begun to switch from traditional in-person consultations to telehealth [11, 12].
Telehealth refers to the use of digital communication technologies and telecommunications to provide and facilitate healthcare services such as provider and patient education, medical care, health-related information services, and self-care [13]. Some distinguish telehealth from telemedicine, with the former referring to all services provided by health professionals, such as nurses and pharmacists, and the latter restricted to physician-provided health services [14]. However, for this study, telemedicine is used as a subset of telehealth, and the review mainly focuses on delivering healthcare services via information and communication technologies (ICT) during the COVID-19 pandemic. Literature on earlier respiratory viruses suggested the use of telephone-based facilities and media to cope with the pressures of healthcare during pandemics [1]. According to a recent review, telehealth is a useful and popular technology for COVID-19 patients because it is portable, simple, and small [15]. Further, another review demonstrated teleconsultations as an application of internet of things (IoT) and could be used for behavioural and therapeutic adjustments, improving the quality of life of patients, training them about COVID-19, and follow-up [16]. Telehealth is especially beneficial in non-emergency/routine medical care and when direct patient-provider contact is not required, such as delivering psychological services [17]. Telehealth technology is found to be patient-centred, safeguards patients, doctors, and others [18, 19], and provides complete access to caregivers [20]. As a result, telehealth is appealing, affordable, and effective healthcare technology [21–23].
With the substantial urban-rural gap, India went through an unimaginable healthcare crisis during the COVID-19 pandemic. While cities employ 75% of qualified consulting doctors, only 23% work in semi-urban areas and 2% in rural areas [24]. Furthermore, the most disadvantaged and marginalised were publicly supported in primary and secondary healthcare [25]. However, the beneficiaries had limited access to these health facilities due to the COVID-19 restrictions. Thus, the pandemic has underscored the paradigm shift in the country’s healthcare system by switching to telehealth. However, providing the proper directives for telehealth services is crucial as its effective utilisation can substantially change how the country’s healthcare system works. Therefore, it is a dire need to understand the application of telehealth even after the pandemic. Hence, exploring telehealth’s role among medical professionals and patients is of utmost importance [26].
Although there are systematic reviews published on the diverse utilisations of telehealth during the COVID-19 pandemic [27, 28], no such studies specifically focused on the Indian context. On the other hand, India was among the first nations to quickly adopt telehealth to provide healthcare in response to the widespread disruptions due to the COVID-19 pandemic. Nevertheless, a recent study from the country used a scoping review methodology to identify the challenges in providing primary care via telemedicine technology [29]. However, a detailed investigation of telehealth utilisation in multidisciplinary primary and secondary healthcare has received minimal attention. Furthermore, a systematic literature review presents extensive evidence on the contribution of telehealth to the detection, management, and control of illnesses during and after the COVID-19 pandemic remains lacking. Therefore, the present study aimed to understand the role of telehealth-assisted healthcare delivery in the context of the COVID-19 pandemic in India and its applicability even after the pandemic. This review could systematically synthesise and integrate information related to the operation of telehealth services in the country from all available sources. Further, the findings could underscore the need to formulate policies to bolster telehealth services, initiate government-level telehealth services, train healthcare professionals and patients, coordinate awareness programmes, and expand smartphone use or network access among the Indian rural population.
The review question was: what are the applications, benefits and challenges of telehealth in India during the COVID-19 pandemic and beyond?
Methods
This systematic review was structured adhering to the updated guidelines for reporting systematic reviews (S1 Checklist) [30]. A systematic review methodology was chosen to provide a rigorous and replicable approach to critically analysing the available literature.
Eligibility criteria
The following inclusion criteria were used. Studies were included if they (a) focused on telehealth users or providers in India, (b) investigated the role of telehealth in any medical speciality during the COVID-19 pandemic, and (c) were published in English. Notably, taking telehealth as a broad concept, studies were selected if they used any form of information and communication technology (ICT) based healthcare services to diagnose, control or manage any diseases/illnesses. However, conference abstracts, secondary data, commentaries, editorials, brief reports, short communication and articles with insufficient data were excluded from the final analysis. Since the present review focused on the COVID-19 pandemic, the year of publication was limited between 2019 and 2021.
Search strategy
A systematic search was carried out on electronic databases PubMed, Science Direct, Scopus, and Web of Science in February 2022. This comprehensive search was complimented by a manual search on Google Scholar. Several synonyms were used to capture as many studies published on telehealth. Boolean operators “AND” and “OR” were applied to combine the keywords. For instance, the search strategy used in PubMed was (“telehealth” [Title/Abstract] OR “telemedicine” [Title/Abstract] OR “teleconsultation” [Title/Abstract] OR “telecare” [Title/Abstract] AND “covid” [Title/Abstract] OR “covid-19” [Title/Abstract] OR “novel coronavirus” [Title/Abstract]); in Scopus TITLE-ABS-KEY (“telehealth”) OR TITLE-ABS-KEY (“telemedicine”) OR TITLE-ABS-KEY (“teleconsultation”) OR TITLE-ABS-KEY (“telecare”) AND TITLE-ABS-KEY (“covid”) OR TITLE-ABS-KEY (“covid-19”) OR TITLE-ABS-KEY (“novel coronavirus”); and in Web of Science ((TI = “telehealth*”) OR TI = “telemedicine*”) OR (TI = “teleconsultation*”) OR (TI = “telecare*”)) AND ((TI = “covid*”) OR (TI = “covid-19*”) OR (TI = “novel coronavirus*”)).
Selection process and data extraction
The first author (RE) has done the study conceptualisation and identified the keywords. The first and second authors (RE & AG) simultaneously did an independent search for relevant articles in databases. Next, three authors (ANM, GSR & PK) screened the articles based on study titles and abstracts. After the initial screening, the first four authors independently assessed the remaining studies for full-text analysis and did the data extraction. The last four authors assisted in drafting the manuscript. Significant information was extracted from each finalised article: authors' details, where the study was conducted, study objectives, study design, sample information, and the major findings regarding telehealth applications, benefits, and challenges. Any disagreements during the study selection and review were settled by discussion.
Quality assessment and evidence synthesis
The methodological quality of included reports was assessed with the JBI appraisal tools [31]. Several study domains were scored on a rating scale of ‘yes’, ‘no’, ‘unclear’ and ‘not applicable’. The first two authors (RE and AG) appraised the studies, and a third reviewer (AJG) decided on discrepancies. A narrative synthesis of extracted information compared and contrasted the ample evidence and qualitatively presented as themes. The reviewers frequently met to discuss the study findings and reached a consensus.
Results
Study selection
A total of 1143 articles were yielded in the primary databases search. Of these, 387 were from PubMed, 316 from Scopus, 286 from Science Direct, 151 from Web of Science and three from Google Scholar. The entire search process for the systematic review is illustrated in the PRISMA flow diagram (Fig. 1). After removing 63 duplicates, the remaining 1080 records were screened based on eligibility criteria. Subsequently, 1006 studies were eliminated after the title and abstract screening. Out of 74 reports sought for retrieval, two were not retrieved because full text was unavailable. The remaining 72 reports were assessed for eligibility, and 53 studies were removed because they did not meet the inclusion criteria. Thus, the final synthesis included 19 studies emphasising the role of telehealth services across various medical specialities in Indian contexts during the COVID-19 pandemic.
Fig. 1.
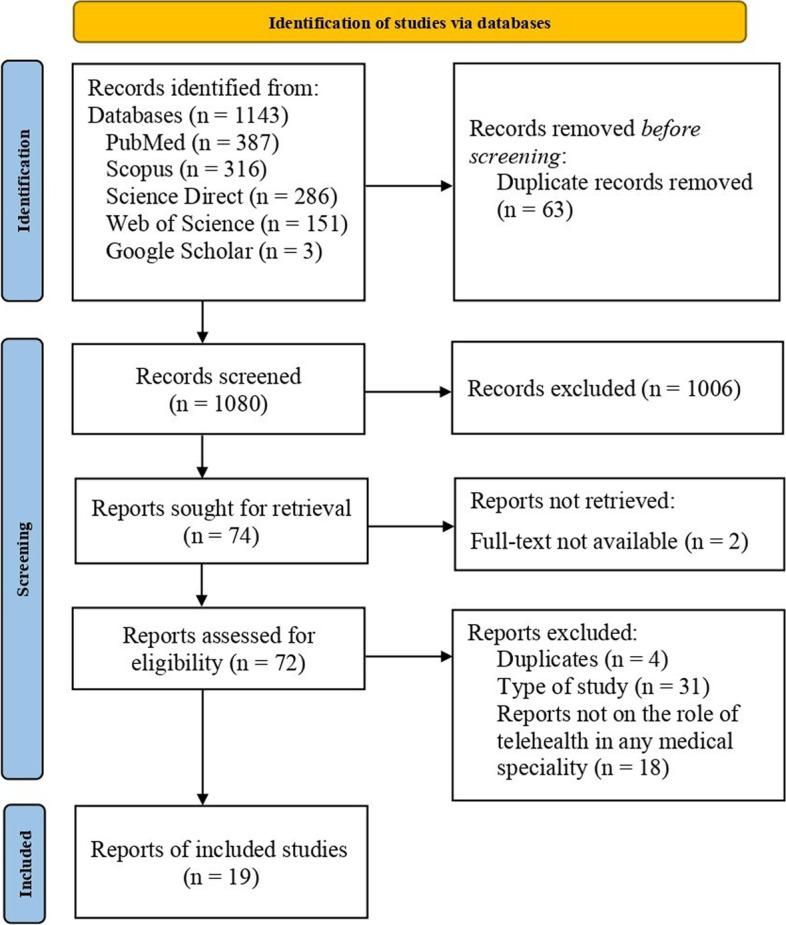
The PRISMA flow diagram
Study characteristics
The final sample for the present review included 19 studies (Table 1). Among these finalised articles, ten were published in 2020 [32–41], and nine were published in 2021 [42–50]. Included studies consisted of eleven cross-sectional studies [32, 33, 35–37, 39, 40, 45, 46, 49, 50] and eight cohort studies [34, 38, 41–44, 47, 48]. Studies covered the application of telehealth services for different medical issues, including ophthalmology (n = 4) [32, 39, 41, 46], neurology (n = 4) [38, 42, 45, 50], dermatology (n = 2) [35, 43], non-communicable diseases (n = 4) [33, 44, 48, 49], haematological illness (n = 1) [37], orthopaedic issues (n = 2) [36, 47], respiratory illness (n = 1) [34], and substance use disorders (SUDs) (n = 1) [40]. The current study findings offer a comprehensive understanding of telehealth services during the COVID-19 pandemic in India. Results were further synthesised into three main themes: applications, benefits and challenges of telehealth services.
Table 1.
Summary of study characteristics
| Sl. No. | Author(s) & Year | Location of study | Objectives | Type of study | Study population | Sample size | Applications | Benefits | Challenges |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Das et al., 2020 [32] | India | Examine the teleconsultation experience of patients. | Cross-sectional study | Ophthalmology patients | n = 2805 | Timely response to eye problems through the use of electronic medical records (EMR). | Positive feedback from the majority of patients. | Lack of EMR system. |
| 2 | Anjana et al., 2020 [33] | India | Evaluate the lockdown effects on the adoption of newer technologies. | Cross-sectional study | Type 2 diabetes patients | n = 2510 |
Provided diabetes education. Easy accessibility to diabetes care. |
Patient satisfaction. Access to specialists. Remote care. Reduce travel time and cost. |
Lack of physical touch. Lack of clarity in the legal framework. |
| 3 | Kumari et al., 2020 [34] | North India | Assess the use of telemedicine in follow-up care. | Cohort study | Children with respiratory illnesses | n = 188 | Successful follow-up care for children who have respiratory problems. |
Recommend to others. Time and cost-saving. |
Difficulty in phone communication. Connectivity issues. |
| 4 | Bhargava & Sarkar, 2020 [35] | India | Evaluate the usage, opinions and attitudes of dermatologists on virtual consultations. | Cross-sectional study | Dermatologists | n = 260 |
New and follow-up patients. Useful for the vulnerable and older population |
High physician satisfaction. Easy accessibility. Cost-effectiveness |
Difficult to understand patient needs. Internet speed. Technological illiteracy. |
| 5 | S. Kumar et al., 2020 [36] | India | Evaluate the telemedicine effectiveness in follow-up care and patient satisfaction. | Cross-sectional study | Orthopaedic patients | n = 450 | Successful follow-up of orthopaedic patients. |
High patient satisfaction Reduces long-distance travel and related costs and discomfort |
Lack of physical examination. Failed patient-provider communication. Network issues Unfamiliarity with video calls. Suitability of devices |
| 6 | P. Kumar et al., 2020 [37] | North India | Evaluate telemedicine feasibility and different factors that contribute to effective teleconsultation. | Cross-sectional study | Patients with different haematological illnesses | n = 944 |
Follow-up care. Provided advice on drug dose modification or continuation of therapy. |
Avoid long travel and tiring journey. Save man-hours. Decrease school/office holidays. Reduce overcrowding. |
Challenges in drug availability. Lack of physical examination. Lack of smartphones and internet facility. Limited patient education. Proper surroundings for communication. |
| 7 | Panda et al., 2020 [38] | Uttarakhand (North India) | Investigates the efficacy and feasibility of advanced techniques of telecommunication. | Cohort study | Children with various neurological disorders | n = 153 | Clarified queries of caregivers including drug availability and dosage and commercial brands. | A feasible and effective option for providing medical advice. |
Lack of smartphones. Slow-speed internet. Inadequate technical knowledge. Fake practitioners. |
| 8 | Pandey et al., 2020 [39] | North India | Examine the feasibility, patient’s clinical profile and addressability using teleconsultations. | Cross-sectional study | Ophthalmologists | n = 32 | About 60% of consultations were successfully managed without physical examination. | Virtual advice is sufficient for many eye care problems. |
Legal concerns. Unavailability of technology. Lack of trust in modality. Data confidentiality. Poor means of communication. Unawareness among rural people. |
| 9 | Sahu et al., 2020 [40] | India | Evaluate the acceptability of e-consult for substance use disorder management. | Cross-sectional study | Health care providers (HCPs) | n = 68 | Receive guidance from specialists. |
Increased accessibility. Time-saving. High HCP satisfaction. |
Patient privacy. Not as suitable as in-person consultations. |
| 10 | Agrawal and Agarwal, 2020 [41] | Indore, Madhya Pradesh | Analyse the impact of teleophthalmology in the management of eye diseases. | Cohort study | Patients with eye problems | n = 119 | Diagnosis and management of most of the cases of tele ocular surface disorders. |
Advancement of digital media. Easy availability of smartphones. |
Not effective in treating eye diseases that need intervention. |
| 11 | Garg et al., 2021 [42] | Delhi | Assess the feasibility of tele neurorehabilitation (TNR) in low-resource contexts. | Cohort study | Patients with Parkinson’s disease | n = 22 | The TNR intervention was shown to be safe, with no serious consequences. | TNR is a feasible option among patients with Parkinson’s disease |
Shared smartphones. Wi-Fi bandwidth issues. Lack of rapport. Inadequate technical skills. Poor hand-motor skills. |
| 12 | Handa et al., 2021 [43] | North India | Analyse patient-physician experience and acceptance of teledermatology | Cohort study |
Dermatology patients Dermatologists |
n = 6125 n = 34 |
The diagnosis was ascertained online in 93.45% of cases. 62% of acne patients reported being satisfied or very satisfied. |
High satisfaction among new and follow-up patients |
Duplicate entries. Privacy concerns Connectivity issues. Patient technological inability. Lack of rapport. |
| 13 | Mishra et al., 2021 [44] | Haryana | Examine the feasibility of telemedicine-based diabetes education | Cohort study | Hospitalised diabetes patients with COVID-19 | n = 100 | Telemedicine was accepted and appreciated by 96.0% of patients. | Effective means to provide diabetes education |
Lack of internet services. Difficulty following medical advice via telephone. Difficulty operating smartphones. |
| 14 | Nair et al., 2021 [45] | South India | Assess the satisfaction, feasibility and effectiveness of teleconsultation | Cross-sectional study | Persons with epilepsy | n = 141 |
Successful video consultations with no additional cost. Prescribed new drugs. |
An acceptable and effective method to follow up on persons with epilepsy. Effectively conveyed medical advice. |
Poor connectivity in rural areas. Lack of smartphones. Security and privacy concerns. |
| 15 | Ravindran et al., 2021 [46] | South India | Describe the teleconsultation experiences of patients during COVID-19 lockdown | Cross-sectional study | Ophthalmology patients | n = 621 | Treatment and management of eye care diseases for both new and follow-up patients. |
Ensure continuity of care during the lockdown. Save travel time. Avoid overcrowding. |
Poor network connectivity. Medicolegal implications. Data privacy and confidentiality. |
| 16 | Sandhu et al., 2021 [47] | North India | Discuss the telemedicine services available for patients during the COVID-19 pandemic. | Cohort study | Rheumatoid arthritis patients | n = 74 |
New and follow-up care. Medical advice regarding prescription changes and related issues. |
Use in future. Recommend to others. Saves waiting time at hospitals. Eliminates travel time. High patient satisfaction. |
Language of clinicians. Unfamiliar technology. No personal phone. Poor network connectivity. Lack of clarity of medical advice. Lack of expertise. |
| 17 | Adhikari et al., 2021 [48] | India | Evaluate the feasibility of telemedicine-based palliative interventions. | Cohort study | Advanced stage Cancer Patients | n = 547 |
Follow-up care. Evaluation of treatment response. Prognostication. |
High patient satisfaction. Chronic pain assessment and symptomatic supportive care. |
Voice/video quality. Advice clarity. Language. |
| 18 | Ullas et al., 2021 [49] | South India | Investigate the adoption rates and perception of telemedicine. | Cross-sectional study | Patients with non-communicable diseases. | n = 220 | New and routine follow-up care for non-communicable diseases |
Comfortable to use. An adequate surrogate for in-person consultations. |
Difficult to get an appointment with a regular doctor or obtain medicine on time. Data privacy risk. Technological unfamiliarity. Limited connectivity. |
| 19 | Raheja et al., 2021 [50] | India | Evaluate the current telemedicine practice gaps and address them for future consultations. | Cross-sectional study | Neurosurgical patients who used telemedicine facility | n = 231 | 97% of patients reported telemedicine in neurosurgery as beneficial. |
Less travel expenditure. Reduced time and resources. |
Poor network. Lack of physical examination. Reduced communication/discussion. Misinterpretation of prescription. |
Quality assessment
The quality appraisal of 19 included studies was done using JBI critical checklists. The risk of bias for assessed reports was generally moderate to high, mainly due to the lack of valid outcome measures. Also, no studies were removed based on the level of methodological quality. The results of the quality assessment can be found in the S2 File.
Applications of telehealth across medical specialities
The findings from the included studies highlight the application of telehealth services in diagnosing and managing different medical complaints related to ophthalmology, neurology, dermatology, non-communicable diseases, haematological illness, orthopaedic issues, respiratory illness and substance use disorders (SUDs).
Ophthalmology
The telehealth application in assisting patients with eye problems was presented in four studies [32, 39, 41, 46]. Notably, electronic medical records allowed for a quick response to patients with ophthalmology issues during the COVID-19 pandemic lockdown [32]. More than 80% of the consultations were from patients who had previously visited the clinic, and about 60% of ophthalmology patients were not prescribed for physical evaluation in person [39]. Teleophthalmology was used for both diagnosis and management of eye problems, especially any damage to the surface layers of the eye, namely the cornea and conjunctiva [41]. Further, it ensured continuity of care during the pandemic as a means of managing new as well as follow-up patients with most eye conditions [46].
Neurology
Synchronous video consultations using mobile phones were reported as an effective mode of telehealth delivery for follow-up patients with epilepsy [45]. Raheja et al. found that 82% of neurosurgery patients reported that teleconsultation call was made on time as per the allotted appointment schedule, and the majority of patients (97%) felt that it has at least one advantage [50]. While considering virtual interventions, teleneurorehabilitation was a viable choice for people with parkinson’s disease during the current pandemic as it was shown to be safe, with no serious consequences [42].
Dermatology
The application of telehealth in dermatology was more practical and easier to adopt as it is largely a visual area, and most disorders can be detected with a simple inspection and a few leading questions [35]. They also reported that teledermatology could be utilised for new and follow-up patients as well as vulnerable and older populations. Handa et al. revealed that diagnosis was made in 93.45% of cases through teleconsultations, and only 2.2% of cases were recommended for in-person visits, especially none of the patients with ectoparasitic, dermatophyte or acne infections required face-to-face consultation [43].
Non-communicable diseases
Patients with non-communicable diseases were more amenable to teleconsultations during the COVID-19 pandemic because of the shortened time for consultations, the difficulty in scheduling in-person visits, and the lessened physical evaluation during consultations [49]. Another study suggested that telemedicine-based diabetes education is an effective, viable and acceptable technology in the COVID-19 management of most patients with type 2 diabetes [44]. However, Anjana et al. concluded that the acceptance of telemedicine facilities is still suboptimal despite their importance in delivering diabetes education and the high levels of satisfaction among the users [33]. In their study, Adhikari et al. reported that teleconsultation could resolve most complaints of advanced cancer patients with a single-time call [48].
Haematological illness
One study considered the application of telehealth services to manage patients with haematological diseases [37]. They reported that three-fourths of patients used telemedicine for regular follow-up advice regarding the continuation of therapy or drug dose modifications. Successful consultations included patients with chronic myeloid leukaemia acquired or inherited marrow failures, myeloma or lymphoma and anaemia.
Orthopaedic conditions
Findings from a study reveal that telecall-based consultations in orthopaedics can be successfully applied to maintain follow-up care, particularly for patients with back pain and cervical complaints, which account for more than one-third of follow-up patients [36]. In another study, Sandhu et al. found telemedicine a feasible method to manage rheumatic diseases and highlighted a greater acceptance of telemedicine even though many patients had never seen or communicated over the internet [47].
Respiratory illness
One study assessed the role of teleconsultation in the follow-up care of children with respiratory problems [34]. The study suggested that telemedicine can successfully manage most children with respiratory complaints who receive follow-up care. They did not encounter any issues during teleconsultations, and 80% of the caretakers reported high satisfaction with telemedicine services.
Substance use disorders (SUDs)
In their study, Sahu et al. employed an asynchronous e-consult-based teleconsultation for substance use disorders, which connects healthcare providers (HCPs) with addiction specialists, found easy access of the majority of HCPs to the specialist, increased clinical care, and high clinician satisfaction as they are not required to meet real-time [40].
Benefits of telehealth in India
The majority of included studies highlighted the benefits of telehealth and stated that it would stay in the country’s healthcare system even after the pandemic [37, 47]. The main reasons for continuing teleconsultation were grouped into five subthemes: patient-provider satisfaction, cost-effectiveness and easy accessibility, new and follow-up care, instant medical advice, and bridging the urban-rural healthcare divide.
Patient-provider satisfaction
Included studies reported high satisfaction of patients [33, 36, 43, 47, 48], as well as the providers [35, 40] with telehealth services. Das el. in their study found that 82% of patients who used teleconsultations were happy with their experience, and 58.1% were willing to continue the use in the future [32]. More than half of the respondents in a study reported a future for teleconsultations in their routine practice of dermatology care as palpation and detailed physical examination are less required to diagnose and treat dermatological problems [35]. Further, findings revealed that patients/providers would recommend telehealth to others [34, 47].
Cost-effectiveness and easy accessibility
Teleconsultations provide access to quality healthcare at the patient’s doorstep [33]. Findings revealed that those who have preferred to continue telehealth services stopped in-person consultations during the pandemic to avoid exposure risk and thus saved time and money on hospital visits [33, 34, 47, 50]. It reduced the inconvenience caused due to long travel distances, expenses, and further discomfort to the patients [36, 42]. In another study, healthcare providers reported easy access to specialist care through e-consult and viewed it as an excellent addition to regular consultation [40].
New and follow-up care
Teleconsultations in the country were found to have benefits like more convenient follow-up [34, 37, 43, 45–47], thereby reducing overcrowding in hospitals [34, 37]. One study on teledermatology reported that earlier teleconsultations focused mainly on follow-up care, while virtual care was provided for new and follow-up patients during the pandemic [35]. Telehealth-based healthcare services were delivered successfully for new and follow-up patients [46, 49]. During follow-up calls, most patients asked for advice regarding prescription change and related complications, while teleconsultations of new patients included screening for disease signs, documentation and video conference if required [47].
Instant medical advice
Caretakers of children with epilepsy largely used teleconsultations to obtain medical advice, and their queries were mainly related to anti-epileptic drug usage and modification, commercial brands, routine visits, and concerns about the adverse effects of COVID-19 on epileptic children [38]. In a study, 74.3% of regular follow-up patients needed advice about drug dosage modification or continuation of treatment [37]. The most common advice given to the patients in another study was related to medications, followed by appointment-related queries and fixing surgical appointments [40]. Relatedly, in their study, Nair et al. successfully contacted post-epilepsy surgery cases and could provide advice about the tapering of drugs [45]. Whereas Adhikari et al. reported that changes in drug dosage or formulation or the prescription of a new medication were included in the most common medical advice offered to patients [48].
Bridging urban-rural healthcare divide
Lockdown has impaired the already difficult transportation of patients in geographically challenging regions [38]. Results from a survey of dermatologists revealed that almost 82% of respondents practised in an urban setting, and 50% had a private clinic of their own [35]. At the same time, teleconsultations have the potential to be accessed by patients in remote areas [32, 34–36, 41, 50]. Virtual consultations save money and effort, particularly for patients from the rural areas as they do not have to travel long distances to get consultation and treatment [35]. Most rural and semi-urban parts of the country have access to the internet and telecommunications facilities. As a result, teleconsultation is becoming more important in reaching out to people with restricted access to healthcare [45].
Challenges of telehealth services
The included studies identified potential challenges to the successful implementation of telehealth services in the country, which were synthesised into nine subthemes: insufficient medical and technological infrastructure, urban-rural digital divide, technological illiteracy, lack of physical examinations, limited patient-provider relationship, difficulty with appointment and consultation time, lack of experts, data security and privacy, and legal concerns.
Insufficient medical and technological infrastructure
Many institutions’ lack of electronic medical records leads to depending on patient-provided reports to the clinician via electronic media such as email or WhatsApp, which impedes the real-time resolution of patient queries [32, 46]. In addition, the unavailability of basic technical infrastructures such as smartphones and the internet is a major barrier to the integration of telehealth into practice [37]. The insufficient technological infrastructure reported in the included studies was lack of smartphones [36, 38, 42, 45] and network connectivity issues [35, 38, 42–45, 50]. One study found that caregivers without well-equipped smartphones could not share clinical reports via picture message or video recording and the medication was prescribed based on the best possible clinical judgment of the consulting doctor [38]. In another study, patients faced problems attending teleconsultations as many shared smartphones with their family members [42].
Urban-rural digital divide
Lack of proper internet connectivity in the country’s rural (especially remote hilly) areas may limit healthcare access to socially, economically, or geographically disadvantaged populations of patients in these regions [49]. One study reported that they had infrequent video consultations as most of their patients were from rural areas where internet connectivity was poor [46]. Similarly, another study revealed that some rural areas might experience weak network connectivity [45].
Technological illiteracy
Technology illiteracy among the citizens is a potential challenge to implementing a telehealth system in the country [35]. Many of the included studies reported on the technological inability from the patient’s end [43, 47] and unfamiliarity with video calls [36]. In their study, Mishra et al. found that several patients depended on their children to operate video-consultation devices [44]. In another study, patients with poor hand-motor skills faced difficulty using a smartphone, while none felt technologically skilled enough to handle a computer to manage this concern [42].
Lack of physical examinations
One of the challenging factors for telehealth is the lack of physical examination [37, 47, 50]. One study revealed that while a lack of physical examination could be justifiable for new patients, it may not always be suitable for patients who need follow-up care as a superficial knowledge of the general condition and the symptom progression can guide further treatment [36].
Limited patient-provider relationship
Telehealth lacks the human touch, one of the main prerequisites of an effective doctor-patient relationship [33]. Additionally, teleconsultations face reduced opportunities to show empathy to patients, understand their needs, and adequately counsel them [35]. In their study, Garg et al. reported that patients expressed inadequate rapport or sense of belonging that they otherwise feel after visiting the doctor in person [42]. Similarly, another study found suboptimal verbal communication and discussion as a limitation of telehealth services [50].
Difficulty with appointment and consultation time
Phone calls at inappropriate timings may contribute to a lack of interest in teleconsultations and a contributing reason some patients decline such services in the first place [36]. Whereas another study reported that treatment got affected as patients could not get an appointment with their routine doctor, possibly leading to patient dissatisfaction [49]. Moreover, about one-fourth of the patients in a study felt that pre-set time limit for teleconsultations restricted documenting their medical history in detail [36].
Lack of experts
In their study, Panda et al. reported that there are now only a few trained radiologists and radiologists in India who are well-versed in magnetic resonance imaging (MRI) and electroencephalogram (EEG) brain reporting, respectively, primarily locate in urban areas [38]. Further, they extend that while MRI images can be telemetrically transferred over a long distance, tele-EEG transportation is still out of reach for most places. Whereas in another study, 61.76% of healthcare providers reported low acceptability of e-consultations with medical specialists as they were concerned with the specialist’s expertise level [40]. The study further stated that addiction specialists in developing countries like India are very few, predominantly located in public sector teaching hospitals and busy with clinical services.
Data security and privacy
Although technological infrastructure is available, data security and privacy are major challenges to telehealth [36, 45]. Patient-provider apprehension about data confidentiality needs to be worked through with prime importance [39, 49]. There is no option to know if the mobile health application developer has taken the necessary precautions to ensure the privacy and security of the application against malicious attacks [45]. Adhikari et al. reported that the major limitation of using these mobile-based applications is the data safety of the patients [48].
Legal concerns
Pandey et al. revealed that 15.7% of doctors were reluctant to use teleophthalmology due to their concerns regarding the associated legal liabilities [39]. There is a potential risk of diagnostic errors and subsequent medicolegal implications [39, 46].
Discussion
This systematic review aimed to synthesise current evidence on the role of telehealth services in India during the COVID-19 pandemic. Results reveal that the virus outbreak and the resulting lockdown have significantly impacted the country’s healthcare system [39]. Surprisingly, the shift to telehealth was well accepted by healthcare professionals and patients. The results demonstrate a broad application of telehealth services to various medical specialities. These findings are in line with a review that revealed the utilisation of telehealth during the current pandemic to control and assess multiple diseases such as diabetes, epilepsy and cancer [27].
Telehealth is depicted in the literature as a feasible tool for delivering health services with high patient-provider satisfaction. The benefits include cost-effectiveness and easy accessibility, new and follow-up care, and instant medical advice. These findings support existing literature on teleconsultation satisfaction for convenience, shorter waiting times, avoidance of unnecessary travelling times and costs, and time off work [51]. Furthermore, studies within this review revealed cost savings that were particularly magnified if patients had to travel long distances. Only 37% of India’s rural population within 5 km can access inpatient services, while 8% of patients can access outpatient healthcare facilities [52]. Findings highlight the role of telehealth in bridging the rural-urban healthcare divide by delivering healthcare services in resource-constrained settings of the country. Consistent with these findings, existing literature claims that the aim to reduce healthcare costs, particularly for patients who reside distant from their healthcare facility, was a driving force for the implementation of telehealth [53–55].
However, evidence suggests that insufficient medical and technological infrastructure and technical illiteracy are potential challenges to telehealth. Similar results were found in other studies that reported technical and technological issues were major barriers to the implementation and adoption of telehealth [27, 56–58]. Furthermore, many patients had to share smartphones with their family members, which supports related research that some patients lack appropriate gadgets in their homes to access telehealth [58]. Additionally, findings reveal that virtual consultation leads to challenges such as lack of physical examination, limited patient-provider relationship and difficulty with appointment and consultation time. Corroborating these findings, other studies also reveal that physical examination can be accomplished only through face-to-face consultation and not by telehealth [59–62]. Evidence also suggests that a lack of experts and necessary equipment may hinder successful telehealth implementation. In contrast, the installation of expensive equipment can be justified as it holds the potential to minimise healthcare costs for patients in rural areas [63]. Also, patient/provider apprehension regarding data security, privacy, and other legal concerns challenge telehealth services. The safety risks of telehealth applications and the usage of telecommunication directly impact patient data privacy [58]. Inadequate medicolegal considerations to assist telehealth was reported as a critical barrier to the adoption of telehealth across different countries [64].
This systematic review presents comprehensive evidence on the role of telehealth technology in India within the COVID-19 pandemic and in the future. Although available reviews report the challenges in delivering primary care using telemedicine in the country during the pandemic [29], the current study demonstrates the applications, benefits and challenges of telehealth, including telemedicine across various medical specialities in primary and follow-up care. Further, the study proposes some crucial recommendations for effectively implementing telehealth practices in the country. Given the potential applications and benefits of telehealth services, the government and policymakers should try to improve technological infrastructure across the country as well as the technological literacy of the population in this era of digitalisation. Data privacy and security should be strictly maintained as these could influence the decision of patients, caregivers and healthcare providers to adopt telehealth services. Further, improved documentation and adherence to information management principles could help healthcare providers avoid medicolegal issues. All reasonable efforts should be made to deliver high-quality patient-centred care to benefit the nation from telehealth services irrespective of social, economic and geographical differences.
The present review included cross-sectional and cohort studies. Nevertheless, results were supported equally by both forms of evidence, and the inclusion of these reports enabled a comprehensive presentation of findings. However, the studies varied in their methodological quality. Notably, several studies omitted participants due to their lack of access to telehealth technology and poor language skills, leaving out a group of patients who perhaps were less satisfied with telehealth. Similarly, the included studies can have a selection bias because patients who consented to join telehealth studies were more likely to be aware of technical operations. Additionally, many studies examining patient/provider satisfaction used non-validated measures, which compromised the validity of the findings. Other studies deemed low quality by JBI appraisal checklists neglected to account for confounding factors that can influence the patients’ condition during the study period. Given the relevance of telehealth in the country, future studies can focus on developing a validated measure to assess provider and patient satisfaction for reliable and comparable study findings. Moreover, confounding factors such as extended time periods between teleconsultations can be explored further.
Furthermore, there are some limitations to this systematic review. Even though several technologies are being deployed for telehealth, the current review attempted to include all studies focused on the role of telehealth across various medical specialities during the COVID-19 pandemic in India. Nevertheless, these studies could cover all components and activities of healthcare and the healthcare system conducted through telecommunication technologies. In addition, the heterogeneity of patient/provider populations in the review sample makes the direct comparison of findings difficult. Therefore, it is difficult to determine the actual scope of telehealth. However, focusing on various medical specialities offers current insight into the wide-ranging application of telehealth within the Indian healthcare system. Although the present review employed a comprehensive search strategy and attempted to cover a wide range of evidence on telehealth services in the country, some articles on these themes in the literature could miss the analysis.
Conclusion
The current systematic review provides comprehensive evidence on the role of telehealth in ensuring continuity of care during the COVID-19 pandemic in India. The findings support the practical application of telehealth services for diagnosing and managing various medical complaints, including ophthalmology, neurology, dermatology, non-communicable diseases, haematological illness, orthopaedic issues, respiratory illness and substance use disorders (SUDs). The overall positive attitude and satisfaction of patients, caregivers and healthcare professionals with telehealth services due to its easy accessibility, time and money-saving expand the scope that lies ahead even after the pandemic. However, the technological challenges and other potential barriers that can impede the growth of telehealth should be addressed within the medical community to make it a viable option for the present and future healthcare practice in the country. Moreover, future research can explore telehealth’s advantages, validity and effectiveness in each medical speciality, mainly during an era of limited physical patient contact and even after that. Further, studies can also evaluate the facilitators and barriers to patient-provider satisfaction with telehealth services.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
The first author (RE) has done the study conceptualisation and identified the keywords. The first and second authors (RE & AG) simultaneously did an independent search for relevant articles in databases. Three authors (ANM, GSR & PK) screened the articles based on study titles and abstracts. After the initial screening, the first four authors independently assessed the remaining articles for full-text analysis and did the data extraction. Articles were appraised by the first two authors (RE and AG), and a third reviewer decided on any discrepancies (AJG). The last four authors assisted in drafting the manuscript. The authors read and approved the final manuscript.
Funding
The author(s) received no financial support for this study.
Availability of data and materials
All data relevant to the study are included in the article or uploaded as supplementary information.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Eslavath Rajkumar, Email: rajkumare@cuk.ac.in, Email: rajku123@uw.edu.
Aswathy Gopi, Email: 20dppsy02@cuk.ac.in, Email: aswathyavanika@gmail.com.
Aditi Joshi, Email: joshiaditi025@gmail.com.
Aleena Elizabeth Thomas, Email: aleenaelizabeth1161@gmail.com.
N. M. Arunima, Email: arunima0811nm@gmail.com
Gosetty Sri Ramya, Email: ursreelu@gmail.com.
Prachi Kulkarni, Email: prachik999@gmail.com.
P. Rahul, Email: rahulpch7@gmail.com
Allen Joshua George, Email: allenjoshua.george@iimranchi.ac.in.
John Romate, Email: romatejohn@cuk.ac.in.
John Abraham, Email: drjohnabraham1988@gmail.com.
References
- 1.Cascini F, Hoxhaj I, Zaçe D, Ferranti M, Di Pietro ML, Boccia S, et al. How health systems approached respiratory viral pandemics over time: a systematic review. BMJ Glob Health. 2020;5:e003677. doi: 10.1136/bmjgh-2020-003677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Madaan P, Sahu JK, Wanigasinghe J, Fatema K, Linn K, Lhamu Mynak M, et al. Teleneurology based management of infantile spasms during COVID-19 pandemic: a consensus report by the South Asia allied west syndrome research group. Epilepsy Behav Rep. 2020;31(15):100423. doi: 10.1016/j.ebr.2020.100423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cascini F, Failla G, Gobbi C, Pallini E, Hui J, Luxi W, et al. A cross-country comparison of Covid-19 containment measures and their effects on the epidemic curves. BMC Public Health. 2022;22(1):1-13. [DOI] [PMC free article] [PubMed]
- 4.Puliyath N, Huda F, Rai A, Munnamgi S, David L, Kumar P, et al. The Utility of Telemedicine in General Surgery during the Covid-19 pandemic and beyond: our experience. Nature. 2020;1(6):5455–5458. [Google Scholar]
- 5.Romanick-Schmiedl S, Raghu G. Telemedicine - maintaining quality during times of transition. Nat Rev Dis Primers. 2020;6(1):45. doi: 10.1038/s41572-020-0185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhagat R, Rs R, Sahoo H, Roy A, Govil D. The COVID-19, migration and livelihood in India: challenges and policy issues: challenges and policy issues. Migration Letters. 2020;28(17):705–718. doi: 10.33182/ml.v17i5.1048. [DOI] [Google Scholar]
- 7.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: results of a survey. Indian J Ophthalmol. 2020;68(5):725–730. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Satgunam P, Thakur M, Sachdeva V, Reddy S, Rani PK. Validation of visual acuity applications for teleophthalmology during COVID-19. Indian J Ophthalmol. 2021;69(2):385–390. doi: 10.4103/ijo.IJO_2333_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020;26(5):571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 10.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 11.Satin AM, Lieberman IH. The virtual spine examination: telemedicine in the era of COVID-19 and beyond. Global Spine J. 2021;11(6):966–974. doi: 10.1177/2192568220947744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sherwin J, Lawrence K, Gragnano V, Testa PA. Scaling virtual health at the epicentre of coronavirus disease 2019: a case study from NYU Langone health. J Telemed Telecare. 2022;28(3):224–229. doi: 10.1177/1357633X20941395. [DOI] [PubMed] [Google Scholar]
- 13.Ministry of Health and Family Welfare India. Telemedicine Practice Guidelines 2020 [cited 2021 Nov 30). Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf
- 14.WHO Global Observatory for eHealth. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. 2010; Available from: https://apps.who.int/iris/handle/10665/44497
- 15.Mehraeen E, Mehrtak M, SeyedAlinaghi S, Nazeri Z, Afsahi AM, Behnezhad F, et al. Technology in the era of COVID-19: a systematic review of current evidence. Infectious disorders - drug. Infect Disord Drug Targets. 2022;22(4):51-60. [DOI] [PubMed]
- 16.Shamsabadi A, Pashaei Z, Karimi A, Mirzapour P, Qaderi K, Marhamati M, et al. Internet of things in the management of chronic diseases during the COVID-19 pandemic: a systematic review. Health. Sci Rep. 2022;5(2):e557. [DOI] [PMC free article] [PubMed] [Retracted]
- 17.Fortney JC, Pyne JM, Edlund MJ, Williams DK, Robinson DE, Mittal D, et al. A randomised trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086–1093. doi: 10.1007/s11606-007-0201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med. 2016;375(2):154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 20.Chauhan V, Galwankar S, Arquilla B, Garg M, Somma SD, El-Menyar A, et al. Novel coronavirus (COVID-19): leveraging telemedicine to optimise care while Minimising exposures and viral transmission. J Emerg Trauma Shock. 2020;13(1):20–24. doi: 10.4103/JETS.JETS_32_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 22.Mehrotra A, Jena AB, Busch AB, Souza J, Uscher-Pines L, Landon BE. Utilisation of telemedicine among rural Medicare beneficiaries. JAMA. 2016;315(18):2015–2016. doi: 10.1001/jama.2016.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sauers-Ford HS, Hamline MY, Gosdin MM, Kair LR, Weinberg GM, Marcin JP, et al. Acceptability, usability, and effectiveness: a qualitative study evaluating a pediatric telemedicine program. Acad Emerg Med. 2019;26(9):1022–1033. doi: 10.1111/acem.13763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mishra SK, Kapoor L, Singh IP. Telemedicine in India: current scenario and the future. Telemed J E Health. 2009;15(6):568–575. doi: 10.1089/tmj.2009.0059. [DOI] [PubMed] [Google Scholar]
- 25.Kant S. The Covid-19 pandemic: impact on primary and secondary healthcare in India. Natl Med J India. 2020;33(4):193–194. doi: 10.4103/0970-258X.316251. [DOI] [PubMed] [Google Scholar]
- 26.Shenoy P, Ahmed S, Paul A, Skaria TG, Joby J, Alias B. Switching to teleconsultation for rheumatology in the wake of the COVID-19 pandemic: feasibility and patient response in India. Clin Rheumatol. 2020;39(9):2757–2762. doi: 10.1007/s10067-020-05200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, et al. Telehealth utilisation during the Covid-19 pandemic: a systematic review. Comput Biol Med. 2021;138:104878. doi: 10.1016/j.compbiomed.2021.104878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20(1):1–9. doi: 10.1186/s12889-020-09301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh V, Sarbadhikari S, Jacob A, John O. Challenges in delivering primary care via telemedicine during COVID-19 pandemic in India: a review synthesis using systems approach. J Family Med Prim Care. 2022;11(6):2581. doi: 10.4103/jfmpc.jfmpc_1559_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372):n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, et al. Conducting systematic reviews of association (etiology): the Joanna Briggs Institute’s approach. Int J Evid Based Healthc. 2015;13(3):163–169. doi: 10.1097/XEB.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 32.Das AV, Rani PK, Vaddavalli PK. Tele-consultations and electronic medical records driven remote patient care: responding to the COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68(6):1007–1012. doi: 10.4103/ijo.IJO_1089_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anjana RM, Pradeepa R, Deepa M, Jebarani S, Venkatesan U, Parvathi SJ, et al. Acceptability and utilization of newer technologies and effects on glycemic control in type 2 diabetes: lessons learned from lockdown. Diabetes Technol Ther. 2020;22(7):527–534. doi: 10.1089/dia.2020.0240. [DOI] [PubMed] [Google Scholar]
- 34.Kumari J, Jat KR, Kabra SK. Role of telemedicine in follow-up Care of Children with respiratory illnesses at a tertiary care hospital - an Ambispective observational study. Indian J Pediatr. 2021;88:974–978. doi: 10.1007/s12098-020-03590-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bhargava S, Sarkar R. Impact of COVID-19 pandemic on dermatology practice in India. Indian Dermatol Online J. 2020;11(5):712–719. doi: 10.4103/idoj.IDOJ_240_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar S, Kumar A, Kumar M, Kumar A, Arora R, Sehrawat R. Feasibility of telemedicine in maintaining follow-up of orthopaedic patients and their satisfaction: a preliminary study. J Clin Orthop Trauma. 2020;11:S704. doi: 10.1016/j.jcot.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar P, Aggarwal M, Dhawan R, Dass J, Kumar G, Sharma V, et al. Tele-medicine Services in Hematological Practice during Covid Pandemic: its feasibility and difficulties. Indian J Hematol Blood Transfus. 2021;37(4):528–533. doi: 10.1007/s12288-020-01385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Panda PK, Dawman L, Panda P, Sharawat IK. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pandey N, Srivastava RM, Kumar G, Katiyar V, Agrawal S. Teleconsultation at a tertiary care government medical university during COVID-19 lockdown in India - a pilot study. Indian J Ophthalmol. 2020;68(7):1381–1384. doi: 10.4103/ijo.IJO_1658_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sahu P, Mathur A, Ganesh A, Nair S, Chand P, Murthy P. Acceptance of e-consult for substance use disorders during the COVID 19 pandemic: a study from India. Asian J Psychiatr. 2020;54:102451. doi: 10.1016/j.ajp.2020.102451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Agrawal T, Agarwal M. Teleophthalmology and its impact- an eye disease pattern analysis in Central India’s hot spot during COVID-19 pandemic. Indian J Clin Exp Ophthalmol. 2020;6(4):522–526. doi: 10.18231/j.ijceo.2020.111. [DOI] [Google Scholar]
- 42.Garg D, Majumdar R, Chauhan S, Preenja R, Parihar J, Saluja A, et al. Teleneurorehabilitation among person with Parkinson’s disease in India: the initial experience and barriers to implementation. Ann Indian Acad Neurol. 2021;24(4):536–541. doi: 10.4103/aian.AIAN_127_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Handa S, Mehta H, Bishnoi A, Vinay K, Mahajan R, Narang T, et al. Teledermatology during the COVID-19 pandemic: experience at a tertiary care Centre in North India. Dermatol Ther. 2021;34(4):e15022. doi: 10.1111/dth.15022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mishra M, Bano T, Mishra SK, Wasir JS, Kohli C, Kalra S, et al. Effectiveness of diabetes education including insulin injection technique and dose adjustment through telemedicine in hospitalised patients with COVID-19. Diabetes Metab Syndr. 2021;15(4):102174. doi: 10.1016/j.dsx.2021.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nair PP, Aghoram R, Thomas B, Bharadwaj B, Chinnakali P. Video teleconsultation services for persons with epilepsy during COVID-19 pandemic: an exploratory study from public tertiary care hospital in southern India on feasibility, satisfaction, and effectiveness. Epilepsy Behav. 2021;117:107863. doi: 10.1016/j.yebeh.2021.107863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ravindran M, Segi A, Mohideen S, Allapitchai F, Rengappa R. Impact of teleophthalmology during COVID-19 lockdown in a tertiary care center in South India. Indian J Ophthalmol. 2021;69(3):714–718. doi: 10.4103/ijo.IJO_2935_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sandhu A, Agarwal A, Kaur P, Sharma M, Sra H, Singh M, et al. Evaluation of tele-rheumatology during the COVID-19 pandemic in Asian population: a pilot study. Int J Telemed Appl. 2021;2021:5558826. doi: 10.1155/2021/5558826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adhikari SD, Biswas S, Mishra S, Kumar V, Bharti SJ, Gupta N, et al. Telemedicine as an acceptable model of Care in Advanced stage Cancer patients in the era of coronavirus disease 2019 - an observational study in a tertiary care Centre. Indian J Palliat Care. 2021;27(2):306–312. doi: 10.25259/IJPC_45_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ullas S, Pradeep M, Surendran S, Ravikumar A, Bastine AM, Prasad A, et al. Telemedicine during the COVID-19 pandemic: a paradigm shift in non-communicable disease management? - a cross-sectional survey from a quaternary-Care Center in South India. Patient Prefer Adherence. 2021;15:2715–2723. doi: 10.2147/PPA.S332636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raheja A, Manjunath N, Garg K, Tandon V, Gupta V, Mishra S, et al. Turning a new chapter in neurosurgery outpatient services: telemedicine a “savior” in this pandemic. Neurol India. 2021;69(2):344. doi: 10.4103/0028-3886.314523. [DOI] [PubMed] [Google Scholar]
- 51.Haider Z, Aweid B, Subramanian P, Iranpour F. Telemedicine in orthopaedics during COVID-19 and beyond: a systematic review. J Telemed Telecare. 2022;28(6):391–403. doi: 10.1177/1357633X20938241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kasthuri A. Challenges to healthcare in India - the five A’s. Indian J Community Med. 2018;43(3):141–143. doi: 10.4103/ijcm.IJCM_194_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mouchtouris N, Lavergne P, Montenegro TS, Gonzalez G, Baldassari M, Sharan A, et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Layfield E, Triantafillou V, Prasad A, Deng J, Shanti RM, Newman JG, et al. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction. Head Neck. 2020;42(7):1681–1689. doi: 10.1002/hed.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Giudice A, Barone S, Muraca D, Averta F, Diodati F, Antonelli A, et al. Can Teledentistry improve the monitoring of patients during the Covid-19 dissemination? A descriptive pilot study. Int J Environ Res Public Health. 2020;17(10):E3399. doi: 10.3390/ijerph17103399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gurwitch RH, Salem H, Nelson MM, Comer JS. Leveraging parent-child interaction therapy and telehealth capacities to address the unique needs of young children during the COVID-19 public health crisis. Psychol Trauma. 2020;12(S1):S82–S84. doi: 10.1037/tra0000863. [DOI] [PubMed] [Google Scholar]
- 57.Strohl MP, Dwyer CD, Ma Y, Rosen CA, Schneider SL, Young VN. Implementation of telemedicine in a laryngology practice during the COVID-19 pandemic: lessons learned. Experiences Shared J Voice. 2022;36(3):396–402. doi: 10.1016/j.jvoice.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Negrini S, Kiekens C, Bernetti A, Capecci M, Ceravolo MG, Lavezzi S, et al. Telemedicine from research to practice during the pandemic. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020;56(3):327–330. doi: 10.23736/S1973-9087.20.06331-5. [DOI] [PubMed] [Google Scholar]
- 59.Atreya S, Kumar G, Samal J, Bhattacharya M, Banerjee S, Mallick P, et al. Patients’/caregivers’ perspectives on telemedicine Service for Advanced Cancer Patients during the COVID-19 pandemic: an exploratory survey. Indian J Palliat Care. 2020;26(Suppl 1):S40–S44. doi: 10.4103/IJPC.IJPC_145_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ashry AH, Alsawy MF. Doctor-patient distancing: an early experience of telemedicine for postoperative neurosurgical care in the time of COVID-19. Egypt J Neurol Psychiatr Neurosurg. 2020;56(1):80. doi: 10.1186/s41983-020-00212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ghai B, Malhotra N, Bajwa SJS. Telemedicine for chronic pain management during COVID-19 pandemic. Indian J Anaesth. 2020;64(6):456–462. doi: 10.4103/ija.IJA_652_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li HL, Chan YC, Huang JX, Cheng SW. Pilot study using telemedicine video consultation for vascular patients’ care during the COVID-19 period. Ann Vasc Surg. 2020;68:76–82. doi: 10.1016/j.avsg.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kappal R, Mehndiratta A, Anandaraj P, Tsanas A. Current impact, future prospects and implications of Mobile healthcare in India. Cent Asian J Glob Health. 2014;3(1):116. doi: 10.5195/cajgh.2014.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Daggubati LC, Eichberg DG, Ivan ME, Hanft S, Mansouri A, Komotar RJ, et al. Telemedicine for outpatient neurosurgical oncology care: lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859–e863. doi: 10.1016/j.wneu.2020.05.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


