Abstract
The COVID-19 pandemic has forced many governments to halt public transport operations. A consequence of such disruption is the reduction in access to critical facilities by individuals who rely on public transport for their daily mobility. We investigate the impact disparities caused by the restriction of public transportation on the access of healthcare workers and patients to healthcare facilities during the COVID-19 pandemic. Metro Manila is an appropriate case study site because the duration of suspension of public transport in the mega-city is one of the longest in the world. The prolonged duration of the lockdown could have devastating impacts on the well-being of individuals who are reliant on public transport to access essential services. Guided by the Yin-Eisenhardt approach to qualitative research, we examined the data from 55 individuals using within-case and cross-case analyses iteratively for the purpose of building a model on the impact of change in access due to public transport disruption on well-being. We mobilized constructs and concepts known in the literature, such as well-being, access, disruption, resistance, resilience, and vulnerability, in developing our two-step conceptual model. Given the profound impact of the prolonged and system-wide suspension of public transport on the well-being of individuals, it is necessary to provide sufficient public transport and active transport infrastructure and services that can cover their mobility needs. The two-step conceptual model from this study can provide guidance on specific policy interventions.
Keywords: COVID-19, Public transport disruption, Accessibility, Equity, Well-being
1. Introduction
In the middle of March 2020, in response to the unfolding COVID-19 pandemic, the capital of the Philippines, Metro Manila, was placed on a total lockdown (Sunio et al., 2022a, Sunio and Mateo-Babiano, 2022). This was to restrict movements in order to curb the spread of the virus. Public transport operations were forcibly put to a halt. On 1 June 2020, the lockdown was eased to pave the way for a phased economic recovery.
One consequence of such disruption in public transport services is the reduction in access to healthcare facilities by individuals who are not only seeking critical medical attention, but also essential workers involved in the delivery of healthcare services (Tirachini and Cats, 2020, Núñez et al., 2021, Chen et al., 2021, Oluyede et al., 2022). Many of them rely on public transportation for their daily mobility, and the suspension and restriction of public transport services represent a severe transportation barrier to accessing critical facilities.
In this study, we examine the impact of a pandemic-induced public transport disruption on the accessibility to healthcare from the viewpoint of healthcare personnel who need to report for duty and of medical patients who need critical care. Accessibility is a multi-dimensional concept, consisting of several measures and components, such as transport (access by what modal option), land use (access to what valued destination), temporal (access when), and individual (access for whom) (Geurs and Van Wee, 2004, Vecchio et al., 2020). Here we consider accessibility primarily as “access for whom”. This means that we primarily examine the impact of (reduced or improved) access due to public transport disruption from the viewpoint of these individuals while de-emphasizing the other components such as land use and temporal dimensions.
This represents a novel area for research because many other public transport disruptions in the past are only short-term and isolated. In Metro Manila, these disruptions are often caused by (train) breakdowns, (trip) cancellations, or transport strikes. However, these are only short-term since operations resume after a few hours, or are isolated to only a few public transit lines or modes. As such, these disruptions can be withstood by affected individuals by adopting various strategies such as “remoding (using a different form of transport for at least a main leg of the trip), retiming (modifying the time at which the trip starts) and rescheduling/cancelling (cancelling the activity on that day and potentially undertaking it on a different day)” (Marsden et al, 2020). On the other hand, the disruption of public transport during the pandemic is prolonged and system-wide and thus requires costlier adaptive strategies. By prolonged, we mean it is protracted over a long period (2.5 months in the case of lockdown in Metro Manila), which contrasts with ‘short-term’. By system-wide, the disruption affects all public transport modes (in contrast to ‘isolated’). Moreover, such disruption during the pandemic is seen to have a far-reaching impact even on the more profound aspects of personal well-being (Dargin and Mostafavi, 2020). For instance, delaying or forgoing health care by patients who need critical care and essential service because of a lack of transport solutions may lead to disastrous health outcomes (Verma et al, 2020). This is true, for instance, for dialysis patients who face serious health risks if regular treatment is missed even once (Chen et al., 2021, Oluyede et al., 2022, Jain and Dupas, 2022). Workers who cannot travel because of transport-related barriers may face the risk of losing their jobs (Lemieux et al, 2020). It has been reported that 0.5 million job losses in the industry sector during the pandemic are attributed to transportation restrictions (The Straights Times, 2020). Transport resilience planning must thus ensure equitable access to healthcare facilities by reducing the disproportionate risks of such service outages to the most vulnerable members of a community (Dargin and Mostafavi, 2020, Chen et al., 2021).
In this paper, we ask: How do the resistance, resilience, or vulnerability of healthcare workers and patients impact their ability to continue accessing healthcare facilities during the period of prolonged suspension of public transportation due to the pandemic? And how does (dis)continued access impact their well-being? In asking “how” (and not “how much”, “how many” or “how often”), we employ qualitative research, specifically the Yin-Eisenhardt approach (Chandra and Shang, 2017), to develop a conceptual model. This task can only be done when there is a prolonged and system-wide public transport disruption that induces this reduction (or improvement) in access, and the context of the pandemic offers a good opportunity to investigate this. Although the context of the study is the COVID pandemic, the findings are applicable beyond the pandemic, especially in contexts where transportation barriers (or enablers) inhibit (or enhance) access, impacting health and well-being.
2. Case study Context: Metro Manila, Philippines
The geographical context of this study is the Philippines, with a special focus on its capital, Metro Manila. Metro Manila is the center of the economy, education, and government of the Philippines. It consists of sixteen highly urbanized cities and one independent municipality, with a total land area of about 620 km2. In 2020, the total population is about 13 million, which is approximately 12.75 % of the national population (Philippine Statistics Authority, 2020).
Based on the person-trip survey conducted by the Japan International Cooperation Agency (JICA) in 2017, the total transport demand in Metro Manila is 13.4 million trips/day, 60 % of which is served by public transport (Japan International Cooperation Agency, 2017). Only 40 % of the demand is made by private vehicles, to which only 11.5 % of the households in Metro Manila have access. When the pandemic hit and caused a suspension of public transport services, a huge segment of the commuting public was severely affected, among whom are healthcare and social workers which comprised 1.33 % of the total labor force in the Philippines (Philippine Statistics Authority, 2020).
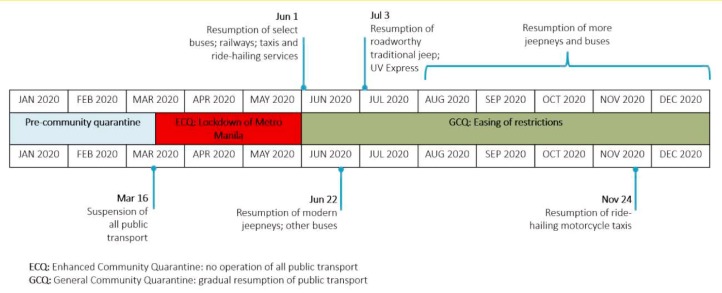
In March 2020, amidst the growing concern surrounding the spread of the COVID virus, the Philippine government enforced varying levels of lockdowns, officially called “community quarantine”. The “enhanced community quarantine” (ECQ), from 16 March until 31 May 2020, is the strictest of such measures.1 Under ECQ, all public transport services were suspended. On 1 June, the government eased the restrictions and placed Metro Manila on a more lenient lockdown, called the “general community quarantine” (GCQ). Under GCQ, the government allowed the resumption of public transport operations in Metro Manila, using a “partial, gradual, calculated, and phased” approach, following strict health protocols (Sunio and Mateo-Babiano, 2022). This means that public transport services are to operate, but at reduced capacities to ensure physical distancing. Operations resumed starting with 10 % of their normal capacity, then gradually increased over time to 50 %. The resumption began with selected buses, railways, taxis, and ride-sharing services, which were allowed to operate beginning 1 June. On 22 June, other buses and modern jeepneys resumed services. Next, in early July, some UV Express (mini-vans) and roadworthy traditional jeepneys were allowed to operate. Over the next months, jeepneys and buses operating plying on other routes resumed their services (Fig. 1 ).
Fig. 1.
Timeline of public transport suspension and phased resumption in Metro Manila in 2020.
To understand how such public transport suspension impacted the lives of Filipinos in Metro Manila, we rely on the survey data of the Social Weather Stations (SWS), a social research institution in the Philippines. Although the survey was conducted nationwide, we only present here the results from Metro Manila, which is the geographical scope of our study.
According to the May 2020 COVID-19 Mobile Phone Survey of the Social Weather Station (SWS), public transport suspension has been difficult and burdensome for many households and families (Social Weather Stations, 2020) Based on the responses via phone interviews from 4,010 households in the Philippines (294 of whom were from Metro Manila), the survey found that the suspension of public transport is burdensome for 81 % of the families surveyed in Metro Manila. The percentage of households experiencing the burden due to public transport suspension is higher for those who have no vehicle (82 %) than those who own one (73 %) (Social Weather Stations, 2020).
In November 2020, SWS conducted another survey nationwide using face-to-face interviews with 1,500 adults with jobs (300 of whom were from Metro Manila) (Social Weather Stations, 2021). Out of these 300, 55 % are able to work from home, and 45 % have to go to the office. Among those who must leave their homes to travel to their workplaces in Metro Manila (non-home-based jobs), only 31 % said that the difficulty of going to work now compared to pre-pandemic is the same as before. The rest said it is slightly harder (10 %), much harder (21 %), or very much harder (36 %) than pre-pandemic. The most common means of going to work are: walking (21 %), motorcycle (20 %), tricycle (14 %), jeepney (25 %), bicycle (11 %), bus (14 %), private car (5 %) and others (6 %).2
Two things can be highlighted from the preceding description regarding the suspension and resumption of public transport. First, a prolonged lockdown (2.5 months in Metro Manila) could have (negative) impacts on individuals who are completely reliant on public transport to access critical and essential services. The negative impact could be, at worst, job loss for healthcare workers or declining health due to delayed treatment for patients. It can be noted that the Philippine experience is different from other countries, which have already relaxed their public transport restrictions and have even resumed providing the pre-COVID level of public transport supply. Second, although public transport resumed on 1 June, it has not returned to full operation: the supply of public transport is still very much limited and below normal capacity due to requirements of physical distancing and the non-resumption of public transport services in many other routes. In fact, the government data indicates that although 58.2 % of workers in Metro Manila were allowed to resume work in September 2020, public transportation could only accommodate 35.5 %, which has left 22.7 % of workers unable to work (National Economic and Development Authority, 2020).
3. Literature Review: Transportation Barriers, Access, Health, and Well-Being
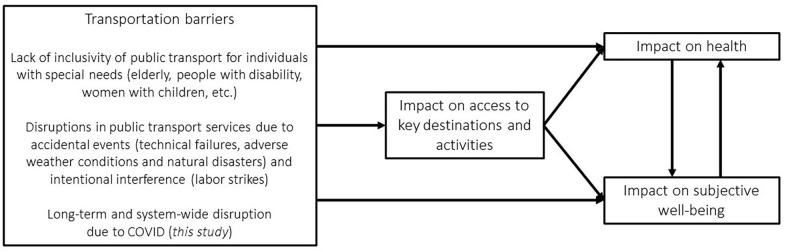
We situate this current study in the literature on the nexus of transportation, access, health, and/or well-being (e.g., Syed et al., 2013, Widener and Hatzopoulou, 2016, Varela et al., 2019, Tiikkaja et al., 2021). The literature has acknowledged the enabling role of transportation to the extent that it allows people to access key places, opportunities, and resources, which are important for their health and well-being (Vecchio et al, 2020). At the same time, many scholars have also examined the constraining role of transport disadvantage and the downstream impact of transport exclusion and lack of access on well-being (e.g., Delbosc and Currie, 2011, Delbosc, 2012, De Vos et al., 2013, Reardon and Abdallah, 2013, Nordbakke and Schwanen, 2014). Broadly speaking, the research field investigates how access to key destinations and activities, which are essential for health and well-being, is affected by transportation-related barriers (Fig. 2 ). In summary, we observe two streams of research in the extant literature.
Fig. 2.
Positioning of the current study within the literature.
The first stream focuses on the mobility, access, and quality of life of individuals with special needs, such as older adults (Hjorthol, 2013, Shergold, 2019), people with physical disability (Smith et al., 2021, Park and Chowdhury, 2022) and women accompanying their children for health checkups (Hernandez and Rossel, 2022). In Norway, as people get older, it becomes more difficult for them to leave their homes, move around, and engage in transport-dependent out-of-home activities, consequently reducing their quality of life (Hjorthol, 2013). In the UK, with continued reductions in public transport services in rural areas, older people living in rural communities face the prospect of mobility constraints and limited access to essential services if they do not drive or own a private vehicle (Shergold, 2019). In Australia, older women living alone experience several barriers, including transport, in accessing key services (Dickins et al, 2022). In their review, Park and Chowdhury (2022) present a systematic examination of various barriers encountered by independent public transport (PT) users with disabilities for the whole chain of their journey, which inhibit them from freely moving and participating in society. Smith et al (2021) consider the impediments to mobility experienced by disabled children and young people which negatively impact their well-being. Finally, in Uruguay, Hernandez and Rossel, 2015, Hernandez and Rossel, 2022 have examined the impact of transport-related factors on the mobility and well-being of women whenever they need to take their children to healthcare facilities for checkups.
The second stream, on the other hand, considers the disruptions in public transport services as constraints to mobility and access. According to Mattsson and Jenelius (2015), disruptions to the operations of transport systems include (a) accidental events, such as technical failures (e.g., Li et al, 2022), adverse weather conditions (Pregnolato et al, 2017) and natural disasters (Kocatepe et al, 2019), and (b) intentional interference such as labor strikes (Saberi et al, 2018). These disruptions may cause a reduction or even loss of access to critical facilities and services, adversely affecting general well-being (Dong et al., 2020, Andreasen et al., 2022).
Within the second stream, the recent years saw a dramatic rise in the number of papers related to the impact of pandemic-induced public transport restrictions. During the pandemic, travel to critical facilities (hospitals, grocery, pharmacies, etc.) has been severely restricted. Several studies have examined the impact of such mobility restrictions to access, health, and well-being. Palm et al (2021) measured the uneven impacts on the ability of former transit users to access healthcare and pharmacy services during the lockdowns. Oluyede et al (2022) identified the transportation barriers to healthcare access that patients encountered during the pandemic, and the solutions utilized to overcome these barriers. Liu et al (2022) analyzed the influence of containment policies in China on people’s mental health via losses in accessibility. Beaudet et al (2022) sought to understand the concerns and challenges of hemodialysis patients during the pandemic related to their travel to and from treatment. Similarly, Jain and Dupas (2022) studied the indirect effects of the lockdown in India on critical healthcare access and outcomes among low-income dialysis patients. Verma et al (2020) measured the effect of lockdowns on the glycemic control of patients with type 1 Diabetes Mellitus by comparing the glycemic levels before and during the lockdown phase. Cochran et al (2022) investigated the transportation barriers to care experienced by patients that resulted in having delayed, missed, or arrived more than 20 min late to appointments. Kar et al (2022) analyzed the equity impacts of reduced accessibility due to transit service cuts during the pandemic and the impacts of such transit service reductions on food and healthcare services across 22 cities in the United States. While these studies, in general, aimed to assess the impact of mobility restrictions on healthcare access and eventually health outcomes, some consider the direct impact of COVID disruptions on (mental) well-being. For example, Mars et al (2022) did a study examining the effect of the lockdowns and mobility restrictions on the psychological well-being of individuals in Spain. In their scoping review, Franklin and Gkiouleka (2021) provided an overview of various psychosocial risks affecting medical and non-medical healthcare workers and the negative impacts of these risks on the health outcomes among the workers. Xiong et al (2020) conducted a systematic review synthesizing important studies on the impact of the pandemic on the mental health of the general population (and not only of the patients and medical workers). Yan et al (2022) examined the effect of the pandemic on the perceptions of risk, severity, and vulnerability by residents in China, which drove automobile purchase intentions.
From the above-cited studies, we observe that there has indeed been a proliferation of studies investigating the impact of the suspension of public transport operations due to the pandemic on access and well-being. Most of these studies consider either only access impact (e.g., Oluyede et al., 2022, Palm et al., 2021, Beaudet et al., 2022, Verma et al., 2020, Cochran et al., 2022, Kar et al., 2022, Jain and Dupas, 2022), or health/well-being impact (e.g., Xiong et al., 2020, Franklin and Gkiouleka, 2021; Mars et al, 2022; Yan et al, 2022). Only one study considers the impacts on both access and health/well-being (Liu et al, 2022). However, this study considers perceived accessibility, understood as a mixture of physical and virtual accessibility. Moreover, mental health, and not well-being, is considered.
The current study aims to contribute to the burgeoning literature on the impact of the suspension of public transport services on the access and well-being of individuals. Although several studies have already shown the adverse impact of the pandemic-induced public transport suspension on the ability of individuals to access critical facilities/services which are essential for their well-being, what these studies have neglected so far are the sources of resistance, resilience, and vulnerability of individuals, which may account for the disparities in the impact on access and well-being. Furthermore, there are few studies that attempt to examine the impacts of (dis)continued access on (subjective) well-being. Our paper aims to address these research gaps by identifying these sources of resistance, resilience, and vulnerability, and explicitly establishing the link between (dis)continued access and well-being.
4. Development of a conceptual framework
4.1. Resistance, resilience, and vulnerability to disruption
Considering that the impact of public transport disruption on access and mobility is moderated by the extent to which the individual can re-mode, retime his/her trip, or reschedule his/her activity (Marsden et al, 2020), we mobilize ideas related to resilience and its related concepts of vulnerability and resistance. Resilience is used in a wide variety of fields (Bhamra et al, 2011), spanning physical and socio-ecological systems (Walker et al, 2004), disaster management (Kuhlicke, 2013), and individual and organizational psychology (Luthans et al, 2006). In defining resilience and its related terms, we draw primarily from the literature on transportation network performance under perturbation (Gu et al., 2020, Mattsson and Jenelius, 2015). In the transportation network performance literature, the concepts of resistance, resilience, and vulnerability are used to describe the capacity (or the lack of it) of transport systems to withstand, absorb and recover their functions after a perturbation.
Resilience refers to the ability of the transportation network to adapt or recover following the disruption (Mattsson and Jenelius, 2015, Bhamra et al., 2011). Resistance, a form of resilience, is the ability of the transportation system to absorb the effects of the perturbation, and therefore, it can be thought of as invulnerability (e.g., Gu et al, 2020). Finally, vulnerability implies the susceptibility of the transport systems to extreme disturbances.
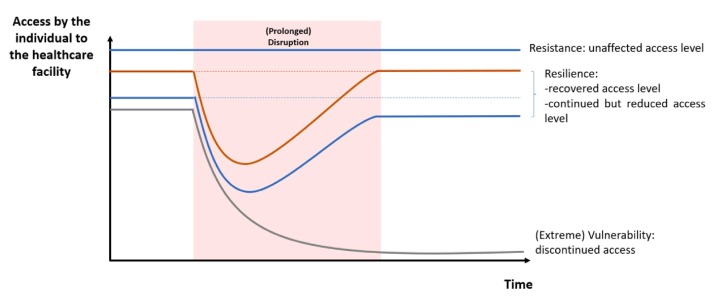
We use these definitions as the basis for our conceptualizations of the same terms in this paper. Instead of network performance as the measurement metric, we look at the change in access level due to the disruption. We define resilience as the ability of the individual to bounce back to the original access level after the disruption. Resilience also includes cases of continued but reduced access. Resistance, on the other hand, means the ability of the individual to withstand the effect of the disruption. In its extreme form, vulnerability is a lack of resistance or resilience (Gu et al, 2020), and it may even take the form of discontinued access. Fig. 3 presents the conceptual distinctions among these three terms in the form of an illustration.
Fig. 3.
Conceptual distinctions between resistance, resilience, and vulnerability.
4.2. Well-being
The well-being approach has become central in transport and urban planning, especially that improving the quality of life has increasingly become a critical policy goal for many cities (Mouratidis, 2021). In the literature, there have been a variety of conceptualizations of well-being. The psychology tradition considers subjective well-being as consisting of life satisfaction (or the cognitive evaluation of satisfaction with life) and of the prevalence of positive affect and the absence of negative affect (Erdogan et al, 2012). Kahneman and Deaton (2010) have somewhat similar conceptualization of well-being as having two distinct aspects: emotional well-being and evaluative well-being. Emotional well-being captures the emotional quality of an individual's everyday experience – the feeling of joy, anxiety, sadness, and affection. Evaluative well-being refers to the global evaluation that people make about their life (Kahneman and Deaton, 2010). In the transportation literature, Thaithatkul et al (2022) distinguish subjective well-being into two general categories: cognitive-judgmental aspects, including life satisfaction and happiness, and affective and emotional aspects. In another transport-related study on well-being, Stanley et al (2021) consider subjective well-being, affect, and eudaimonic well-being. Subjective well-being is like “life satisfaction”; while affect is similar to “emotional well-being”. Eudaimonic well-being measures autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance. In this paper, we do not consider eudaimonic well-being. From the foregoing, there seems to be a consensus concerning the two dimensions of subjective well-being: emotional well-being (affect) and life satisfaction (or evaluative well-being).
To these two dimensions, we add a third, namely satisfaction of needs (e.g., Nordbakke and Schwanen, 2014). Here we agree with Nordbakke and Schwanen (2015) on the importance of “considering wellbeing also in terms of the fulfillment of needs”. This dimension of well-being as needs fulfillment is quite prominent in studies focusing on the mobility of individuals in their later life (Kim, 2011, Nordbakke and Schwanen, 2014, Nordbakke and Schwanen, 2015). Needs satisfaction considers well-being in terms of the “entitlement to a minimally decent life and in terms of minimum thresholds for a decent life”, which can be obtained when there is access to food, water, shelter, and some medical services, education, money, and work (Nordbakke and Schwanen, 2014, Nordbakke and Schwanen, 2015). We believe that such a three-dimensional conceptualization of well-being is consistent with the notion of well-being found in other transportation studies – for example, by Reardon and Abdallah (2013) whose notion of well-being consists of “good feelings day-to-day and overall”, “good psychological functioning” and “need-satisfaction and engagement”.
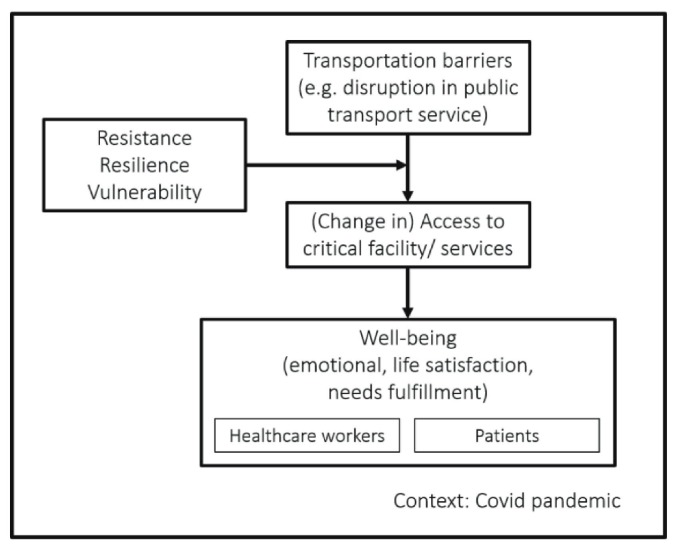
From the preceding, we summarize the links between transportation barriers (e.g., disruption in public transport), access, resilience, resistance, vulnerability, and well-being in the following conceptual framework (Fig. 4 ). These main variables of interest are brought together in the context of the COVID-19 pandemic, which has caused unprecedented (i.e., prolonged and system-wide) disruption in public transport operations. In this framework, we hypothesize that the disruption in public transport services due to the pandemic caused differential impacts on access to critical facilities and essential services depending on the resistance, resilience, and vulnerability of individuals. Accessibility loss or gains are hypothesized to influence various aspects of well-being. Since the literature also suggests differential well-being impacts experienced by different groups of individuals (for example, medical versus non-medical workers) (e.g., Kar et al., 2022, Franklin and Gkiouleka, 2021), we also explicitly distinguish different groups in our conceptual framework.
Fig. 4.
A conceptual framework linking different variables of interest.
5. Methodology
5.1. Methods
To test the conceptual framework and the hypothesis, we conducted a study examining the impact of the complete suspension of public transport operations during the lockdown in Metro Manila on the accessibility of healthcare facilities from the perspective of both healthcare workers and medical patients. We focused on both types of individuals because during the lockdown when the government ordered the suspension of public transport and required every-one to stay at home, healthcare workers and medical patients still had to travel to healthcare facilities for work or continuing care.
Institutional ethics approval from the University of Asia and the Pacific was obtained. Since the objective of this study is to explore a previously unexplored phenomenon (i.e., the impact of a prolonged public transport suspension to access and well-being), we employ a qualitative research approach. The insight from qualitative research is called “analytical generalization” (in contrast to statistical generalizations of quantitative research) (Chandra and Shang, 2017).
There are various methods to conduct qualitative research such as Gioia, Yin-Eisenhardt and Langley; the current study uses the method of Yin-Eisenhardt (Chandra and Shang, 2017, Eisenhardt, 1989). It is known as “variable-oriented theorizing”, whereby the researcher begins with some knowledge of prior theory, constructs or variables, but without explicating them further, then ends with establishing the relationships among these variables, regardless of context, to produce a mechanism, process, or theory that explains the phenomenon of interest (Eisenhardt, 1989, Eisenhardt and Graebner, 2007). In qualitative research, the modest objective is theory-building from multiple cases – a theory that is novel, testable, empirically valid, and a suitable complement to mainstream deductive research, e.g., quantitative research (Eisenhardt and Graebner, 2007). In short, the qualitative method is for hypothesis generation that can then be tested more empirically and robustly using quantitative methods. Through deductive research, the links, and the strengths of the relationships among the variables, can be tested via statistical sampling.
5.2. Sample and data
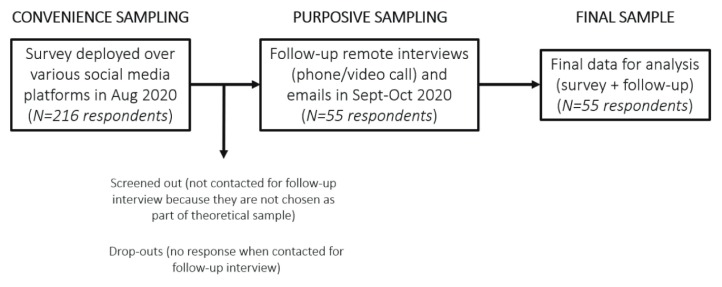
Data collection took place for three months (August-October) in 2020. Fig. 5 shows our data collection process. It shows a combination of convenience and purposive sampling.
Fig. 5.
Data collection process. In responding to our survey/interview, our respondents were asked to think of their situation from mid-March (when the lockdown was implemented) until August 2020 (during the time of the survey). The final sample consists of 38 healthcare workers and 17 patients.
Given that this study was executed during the time of the pandemic when only remote data collection is possible, the recruitment of participants was done over various social media platforms that are readily accessible to the researchers (convenience sampling). Two types of social media platforms were considered: the first type is for specialized groups (e.g., healthcare workers’ groups), and the second is for the general population (e.g., those maintained by the Philippines’ Department of Health, and mobility advocacy groups). Without any access to social media groups exclusive to medical patients, we relied on this second type of social media platform to recruit medical patients as participants. Initially 216 individuals showed interest and answered our survey that was deployed using Google forms. Since the initial survey (in August 2020) collected only “thin” data, we found it necessary to conduct follow-up video/phone call interviews and email exchanges to collect thicker and more comprehensive data. The researchers then contacted all 216 respondents for follow-up interviews.
Among those who agreed to the follow-up, we selected those who will be part of the final sample (purposive sampling). In doing the selection, we adopted theoretical (or purposive) sampling that seeks maximum variation of the data (Chandra and Shang, 2017). The theoretical samples can be defined in such a way that they cover the so-called “possibility space”, which represents the full envelope of key dimensions of variation. This is necessary to build variation into the theory in order to achieve theoretical saturation. Here we consider the pre-lockdown main transport mode and impact on access to constitute the key dimensions of variation.
Follow-up data collection includes a combination of video/phone calls (lasting about 60 min) and email exchanges (done in September-October 2020). During the video interviews, the survey form that was accomplished by the respondents was once again shown to them for validation and further data collection. The researcher who conducted the interview took down notes that were shown simultaneously to the respondents on the shared screen during the interview. After these video interviews, follow-up email exchanges were also done in case there are issues or questions for clarification. In case the respondent prefers a phone call interview, the researcher would simply read out the questions and answers for validation and further data collection. The type of data gathered is primarily qualitative data. The questions (included in the survey, the follow-up video/phone call interview and email exchanges) covered items about the socio-demographic profile, profession/job, modes of transport used (before and during the pandemic), location of the destination healthcare facility, medical condition (in the case of patients), and the impact of the public transportation suspension on access and well-being. The survey questionnaire and the interview protocols are shown in the Appendix.
Our final sample size N is 55 (38 healthcare workers and 17 patients). Although our aim is maximum theoretical variation within the sample, examining the distribution of the respondents by pre-lockdown main transport mode and impact on access (as shown in Table 2 below), we note that the respondents do not cover all the possible combinations of the variations of the variables. For example, there are no respondents for discontinued access by train, bus, or trike; or discontinued access by car. Two possible explanations can be given for this. First, our sampling reach is only limited to those we have ready access (convenience sampling). Second, it is highly likely that there are really no respondents who can be found belonging to these categories.
Table 2.
Pre-lockdown mode as moderator of accessibility impact. Note: MC stands for motorcycle and UV for Utility Vehicle Express (N = 55).
| Impact on Accessibility | Pre-lockdown mode | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Motorized personal transport - owned | Non-motorized personal transport | Motorized personal transport – shared/rented | Public transport | |||||||||
| Car | MC | Bike | Walk | Ride-hailing | MC-rented | Jeep | Train | Bus | Trike | UV | ||
| Discontinued access | 3 | 3 | ||||||||||
| Negative | 4 | 1 | 7 | 3 | 4 | 19 | ||||||
| None or positive | 23 | 2 | 1 | 1 | [1] | [2] | [2] | [1] | 33 | |||
| Total | 25 | 2 | 5 | 23 | ||||||||
5.3. Data processing and analysis
Responses from the survey questionnaire are first tallied and presented in tables and figures to examine the impact of the public transport disruption on access, and the moderating effects of resistance, resilience, and vulnerability. Of particular interest in this study are the resources for resilience. The latter can be obtained from the responses during the follow-up interview. The researchers asked the respondents considered resilient to enumerate all the factors that they think contribute to their resilience. A codebook based on Abramson et al (2015) was developed to categorize these resources into human (health, coping, emotional reactivity), economic (savings, job stability, credit), social (social networks, family, neighbor), institutional (government, company, and other organizations) and geographical (proximity) (Abramson et al, 2015).
To analyze the relationship between (dis)continued access and well-being, we tally the responses obtained from the survey, generated by asking the respondents how their well-being is impacted by (continued or discontinued) access to the health care facility (severe negative impact, moderate negative impact, no impact, moderate positive impact, high positive impact). Furthermore, guided by the conceptualization of well-being as consisting of emotional, life satisfaction, and basic-needs fulfillment dimensions, we coded the responses of the health workers and patients to our question concerning well-being impact along these three dimensions as well as categorized them as negative or positive. Categorizing the experience and evaluation concerning well-being as either negative or positive can be done straightforwardly by using the well-known methods of sentiment and corpus analysis (see, for example, Sunio et al., 2022b).
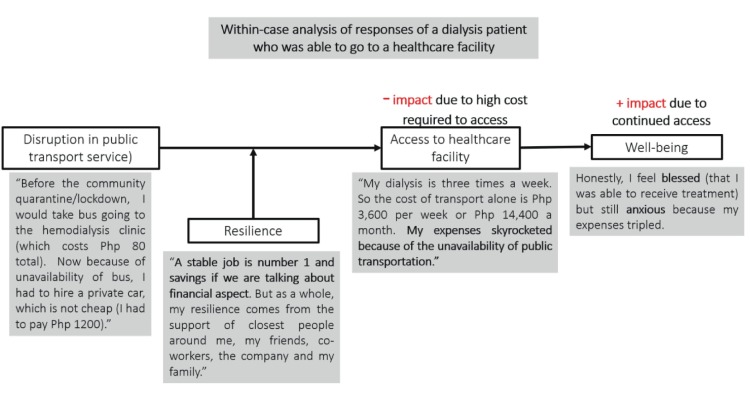
Finally, to formulate a process model describing the pathways of the impact of public transport service disruption on well-being, we conducted an analysis, consisting of the following steps, based on the Yin-Eisenhardt method of theory-building from multiple case studies (Eisenhardt, 1989). First, we examined the survey data to find any general patterns among the variables of interest (refer again to Fig. 4). We seek to develop an initial working model that captures the relationships among these variables. Second, we conducted a within-case analysis, which involves a separate analysis of each of the 55 cases. In this step, we enriched and improved the preliminary model developed in the previous step and modified it so a close fit with the individual case under consideration is achieved (see Fig. 6 for an example of a within-case analysis of one respondent). Third, we conducted a cross-case analysis to identify patterns. This step involves forcing researchers to go beyond initial impressions, and to generalize the model so it is applicable to more cases. Fourth, we used all themes, concepts, and relationships that emerged in the previous steps to confirm, extend, and sharpen our emerging theory. In all these, the processes are iterative: iterative among the four steps, iterative between data and emergent model, and iterative between data and relevant literature. Finally, we presented our results to some of our respondents in order to elicit remarks from them to verify our findings. Our final output is a model showing the pathways of the impact of public transport disruption on access to a healthcare facility and general well-being during the COVID-19 pandemic (see section 7 below).
Fig. 6.
Example of a within-case analysis (1 USD = Php 50 in 2020).
6. Results and discussion
In this section, we provide a summary of results obtained from the within-case and cross-case analyses in the following sections below. We divide this section into three main sub-sections following the conceptual framework shown in Fig. 4: Change in access to a healthcare facility (6.1), Resistance, Resilience, Vulnerability (6.2), and Well-being (6.3).
6.1. Change in access to a healthcare facility due to public transport disruption
6.1.1. Impact disparities on access
The public transport service outage caused impact disparities in the access levels of healthcare workers and patients to healthcare facilities (Table 1 ). Among the 38 healthcare workers and 17 patients interviewed, three of them were unable to access the healthcare facility during both ECQ (when transport was completely suspended) and GCQ (when some public transport resumed). This is transport-related discontinued access. These three individuals would take jeepneys as their mode of transportation before the community quarantine (or lockdown). When the lockdown was imposed, they had no other alternative modes of transport. One of the three said in the interview: “I haven’t been able to resume work at the hospital where I was working prior to the pandemic.… I don’t have my own car so I was dependent on public transport. Grab (a ride-hailing service) transportation is too expensive for me. As a result, my income is severely decreased.” Another – a patient – said: “Had there been public transportation I would have taken it but none were available at the onset of the pandemic.” On the other hand, 19 individuals experienced a negative impact on their access, while 26 did not experience any impact. Seven individuals reported having experienced a positive impact on their access.
Table 1.
Impact disparities on accessibility due to public transport suspension.
| Impact on Accessibility | Healthcare workers (N = 38) |
Patients (N = 17) |
Total (N = 55) |
|---|---|---|---|
| Discontinued access | 2 | 1 | 3 |
| Negative impact | 15 | 4 | 19 |
| No impact | 15 | 11 | 26 |
| Positive impact | 6 | 1 | 7 |
6.1.2. Pre-lockdown mode as moderating variable of the impact of public transport suspension on accessibility
We performed analyses to identify the relationship between accessibility impact and other variables. We found that only the pre-lockdown mode qualifies as a moderator variable that affects the strength of the impact of the disruption on accessibility. This is readily seen by simply tabulating the accessibility impact against the pre-lockdown mode as shown in Table 2. Generally, healthcare workers traveling mainly by motorized or non-motorized private transport prior to the lockdown (car, motorcycle, bicycle or walk) experience no negative accessibility impact during the lockdown, while those who use shared motorized (ride-hailing) and public transport before the lockdown (jeep, train, bus) experience reduced access (negative impact) and even discontinued access. There were six PT users who did not report negative impact or discontinued access (in brackets in Table 2).
6.2. Resistance, resilience, and vulnerability
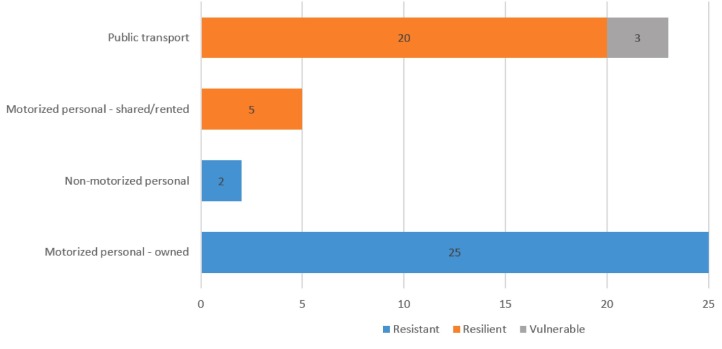
6.2.1. Impact of pre-lockdown mode
We further analyze the data shown in Table 2 to investigate the resistance, resilience, and vulnerability of the respondents. Fig. 7 is generated by tabulating the number of individuals by pre-lockdown and lockdown modes, and the impact on access. Resistance is present when the individual can use the same mode during the pre-lockdown and during the lockdown; consequently, there is no negative impact on his/her access. Resilience is present when the individual continues to have access to the healthcare facility, as a result of being able to find an alternative mode of transport. Vulnerability is present when the individual experiences discontinued access.
Fig. 7.
Resistance, resilience, and vulnerability of individuals by pre-lockdown transport mode (N = 55).
As Fig. 7 suggests, those who were using “motorized personal transport-owned” and “non-motorized personal transport” are highly resistant, i.e., public transport disruption has no (negative) effect at all on their mobility and access. They did not need to change their behavior or exert any extra effort to adapt. On the other hand, healthcare workers and patients alike, who depended on public transport and shared/rented motorized modes for their daily mobility, had to shift to other modes of transport. In other words, those who used “public transport” and “motorized personal transport-rented/shared” had to re-mode to be resilient. Those who could not re-mode experienced discontinued access to the healthcare facility, and were thus considered vulnerable.
6.2.2. Resources of resilience for re-moding
We pay particular focus on the sources of resilience since this is of major policy interest. Here we present in Table 3 the resources accessed by individuals to counter the effects of the disruption. Twenty-five individuals were able to re-mode and thus became resilient (orange bars in Fig. 7). We assume that the capacity of the individual to be resilient depends upon access to and activation of the following capital: human, economic, social, institutional and geographical (Abramson et al, 2015). Ten of them were able to re-mode because of access to economic resources (such as a car or financing), which enabled them to own, buy or rent personal transport. Seven relied on transport services provided by institutions as well as work-from-home arrangements (for health administrators) during the first few days of the lockdown. Seven individuals benefited from the help of their social circles (family, friends, and neighbors). One was living within the proximity of a healthcare facility.
Table 3.
Resources used by resilient individuals for re-moding (N = 55).
| Resource Type | Count | Excerpt |
|---|---|---|
| Economic (10) | ||
| Owned car | 1 | “The travel to and from work became stressful and tiring, before this pandemic my means of transportation is public transportation but due to this happening, I was forced to use a personal car.” |
| Bought bicycle | 3 | “I decided to buy a bike in April 2020. I used my 13th-month bonus for the purchase of the bike.” “The suspension of public transport gravely affected my capacity to work, and helped me decide to shift to biking to work.” |
| Bought e-scooter | 1 | “I bought an e-scooter which I used for 2–3 weeks of the lockdown. Then I got into an accident. A friend drove me to work. After that, I decided to buy my own car.” |
| Rented motorcycle/car | 5 | “It was challenging to find a means of transportation during the ECQ. Because the location of my residence is not along the routes of the free shuttles provided by various agencies, I had to find my own means to go to work. I had some difficulty finding tricycles that can take me to the hospital… In the end, I was able to make a deal with a certain tricycle driver who regularly fetched me from home and dropped me off at work.” “During the pandemic, I need to hire a private car which is not cheap… During this time, transferring to a closer [hemodialysis] center is not possible because every center does not accept a new patient.” |
| Institutional (7) | ||
| Special rides from the government, company, and hospital | 5 | “During the lockdown, I relied heavily on walking and the free shuttle service by the hospitals… I was limited to working only on clinics where I can go by foot, or hospitals that provide transportation service.” “During ECQ the company provided us shuttle while CDC [a government-owned corporation] provided us accommodation. Some local restaurants provided us with food which fueled us to continue our work.” |
| Work from home | 2 | “There was no need to go to the office because we were allowed to work from home during the ECQ.” |
| Social (7) | ||
| Family | 5 | “I do not drive going to the hospital. I had to ask my brother-in-law to bring me to the hospital and had to ask my sister to fetch me after my clinic hours. I feel that by doing so I burdened them.” “My father was the one who drives me to work so whenever he picks me up from work he is very much exposed to the virus since I also handled the COVID samples during my duty.” |
| Friends and neighbors | 2 | “Our neighbor took me to the hospital by car and then subsequently I was able to use tricycles from outside the hospital directly to my home, both at time of discharge and subsequent checkups, so again transportation was not really an issue in spite of lockdown restrictions.” |
| Geographical (1) | ||
| Walk | 1 | “I was lucky enough to be living near a medical facility at a walking distance. Had I been living farther away, I would have opted to cancel my medical appointment.” |
| Total | N = 25 |
6.2.3. Relaxation of traffic as a potential source of resilience
One of the consequences of the lockdown is that it has freed up the roads from vehicles: our cities saw a drastic reduction of traffic by private and public transport vehicles. This resulted to more pleasant travel to work by some health care workers who use private cars, as one respondent attests: “In my case, considering that I have a private vehicle, it is not really a problem for me in getting to work. In fact, it was an advantage for me because there is no traffic and the fuel got cheaper”. Moreover, the reduction in traffic also made streets safer for cycling for one respondent: “I decided to buy a bike in April 2020. I used my 13th-month bonus for the purchase of the bike… I am currently using a bicycle so I am happy with it because it serves as my cardio/ exercise and I am meeting friends down the road. It taught me to become more focused and disciplined”. In a sense, public transport suspension, and the lockdown in general, also loosened the barriers to the movement of pedestrians and cyclists.
6.3. Well-being impacts
We also investigated the impact of (continued or discontinued) access to work or medical care during the lockdown on well-being.
6.3.1. Association between access and well-being
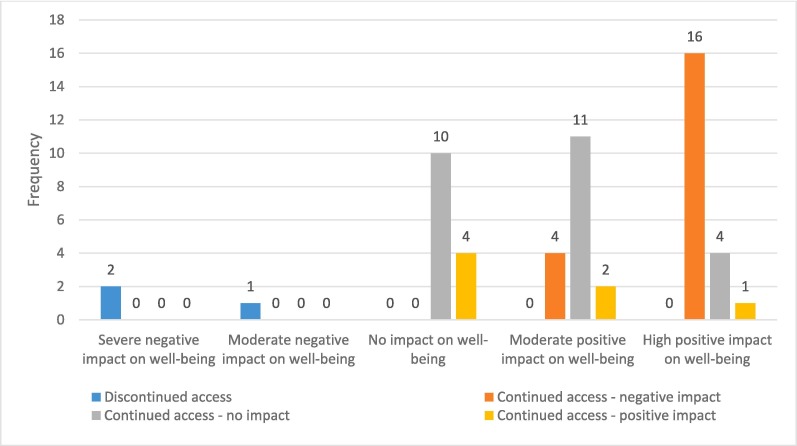
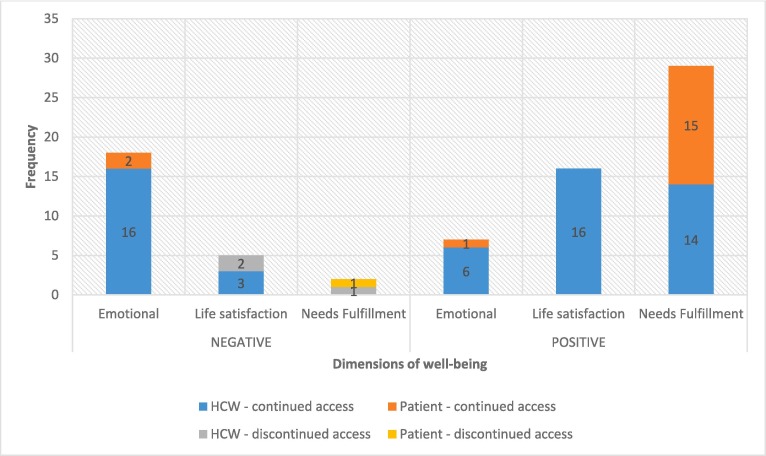
In Fig. 8 we show the relationship, obtained from the survey, between access and well-being impact.
Fig. 8.
Well-being impact of healthcare access (N = 55).
From the survey data, it seems there is no direct relationship between access and well-being. This only means that we cannot, for example, establish that reduced access is associated with lower well-being; in other words, access level and well-being level do not move in the same direction. While it is certain that those who were not able to access the healthcare facility experienced a negative impact on their personal well-being, those who were able to access it at varying degrees of ease/difficulty experienced differential impacts on their well-being. Considering the multi-dimensionality of well-being (emotional well-being, life satisfaction and needs fulfillment) (recall Section 4.2), we presume that respondents refer to different aspects of well-being when they thought of “well-being”. This is illustrated in the following quote from one respondent, where the three dimensions of well-being are present and can be distinguished:
“I feel tired (emotional well-being). I can't help but question my decisions, thinking if this is the life I ought to live, if this is the duty I am willing to take, etc. But at the end of the day, I still feel a bit of pride, knowing that somehow I am able to contribute to our fight against the pandemic (life satisfaction). Aside from the fact that it is my duty to serve, I also had to consider the workforce that would be affected. Some of my co-workers were stranded, and since I was able to find transportation, I needed to step up so I could cover for them. To be honest, on some days, I was mostly driven by my paycheck since staying at home is a luxury I can't fully afford (needs fulfillment).”.
6.3.2. Impact of (continued and discontinued) access on the dimensions of well-being
Fig. 9 presents the results of our analysis of the impact of (dis)continued access on subjective well-being. From the figure, we can highlight three things:
-
•
Discontinued access negatively impacts life satisfaction (e.g., loss of sense of fulfillment) and needs fulfillment (e.g., job loss) dimensions of the well-being of healthcare workers, and the needs satisfaction dimension of the well-being of patients (e.g., forgone medical check-ups).
-
•
Continued access by healthcare workers negatively impacts the emotional dimension the most (e.g., anxiety due to risk of infection, tiredness, and exhaustion), but positively impacts life satisfaction (e.g., opportunity to continue to help; feeling of pride and importance) and the needs fulfillment dimensions (e.g., able to continue to earn for a living).
-
•
Continued access by patients positively impacts the needs fulfillment dimension (e.g., timely medical care and medication access).
Fig. 9.
Impact of access on dimensions of well-being by patients and health care workers (HCW) (N = 77 does not equal the number of respondents since each response can be coded with more than one dimension).
Examining these results, we can make the following preliminary observations concerning the impact of public transport disruption-induced change in access on the three dimensions of well-being. Disruptions resulting in discontinued access to critical facilities impact negatively-one’s well-being on the evaluative and needs satisfaction dimensions. However, continued access, amidst the disruption, has mixed results. For example, continued access by healthcare workers negatively impacts the emotional dimension the most (anxiety and exhaustion), but positively impacts the life satisfaction (feeling of sense of self-fulfillment) and the needs fulfillment dimensions (able to work). In many empirical studies, only the emotional and life sastisfaction dimensions are measured or even aggregated into a personal well-being index (e.g. Cuignet et al., 2020, Delbosc and Currie, 2011, Stanley et al., 2011), but the context of the pandemic highlights the importance of the dimension of fulfillment of basic needs (e.g. Nordbakke and Schwanen, 2014), considering the reality of unmet needs during the pandemic as a result of discontinued access to critical facilities for some individuals.
7. Summary, Conclusions, and recommendations
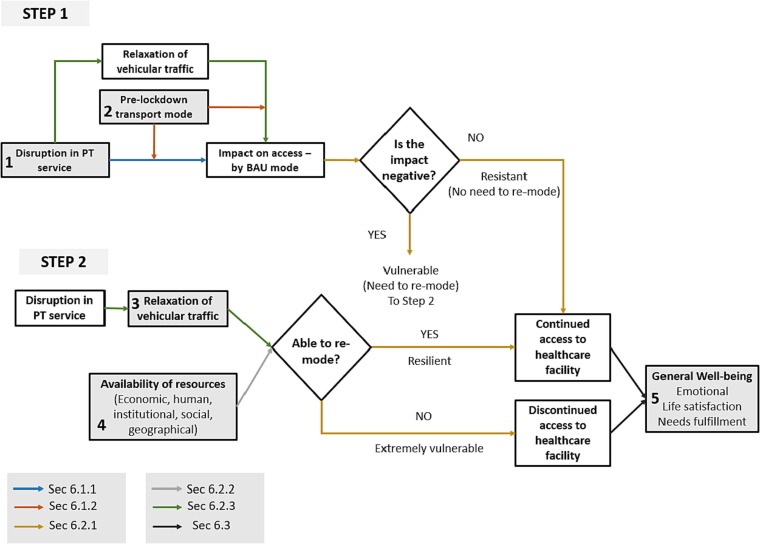
We summarize now the points from the foregoing sections, which are depicted in Fig. 10 . In this framework, the pandemic is an exogenous shock that caused a disruption in public transport service. The model consists of two steps. The first step considers the impact disparities by the disruption on access by business-as-usual (BAU) mode, the pre-lockdown mode (Section 6.1.1). The disparity is driven primarily by the pre-lockdown mode of transport (Section 6.1.2). In general, those using personal transport (motorized or non-motorized) are resistant to any disruption in public transport, while those using shared and public transport are the most vulnerable (Section 6.2.1). Resistance to disruption is shown as a path in the model when the “impact on access – by BAU mode” is not negative, i.e., access is unaffected by the public transport disruption. In some cases, access may also improve, considering the relaxation of vehicular traffic due to the suspension of public transport that makes streets attractive for cyclists and car drivers. Vulnerability is depicted as a path when the “impact on access – by BAU mode” is negative.
Fig. 10.
Two-step model describing the pathways of the impact of public transport service disruption on well-being. The links in the figure are color-coded for easier reference to the pertinent section of the paper. Numbered and shaded constructs are touchpoints for policies.
The second step of the model considers the case where vulnerable individuals identified in the previous step adopt a resilience strategy. Re-moding (mode switch) is the most common form of resilience, which only those who have access to critical resources (economic, human, institutional, social or geographical) are capable of (Section 6.2.2). Another factor that can influence re-moding (especially towards bicycle) is the relaxation of vehicular traffic due to public transport disruption, which loosened transportation-related barriers, positively impacting access to healthcare facility by personal transport, including bicycles (Section 6.2.3). When vulnerable individuals successfully re-mode, they are considered “resilient” since they are able to continue accessing the healthcare facilities despite the disruption, albeit in some cases with a degree of access worse than before. Others are not able to re-mode, making them extremely vulnerable to discontinued access. Finally, continued or discontinued access to healthcare facilities impacts well-being in its various dimensions (Section 6.3).
This work makes theoretical and practical contributions. Firstly, the study contributes novel theorizations on the conceptual links among disruption, access, and well-being in the context COVID-19 pandemic. The unique experience of Metro Manila – a public transport suspension that is very much prolonged and a resumption that did not restore pre-COVID transport capacity – makes our case study site theoretically revelatory and interesting. Although the impact of disruption on access, and ultimately well-being, has been explored in the extant literature (e.g. Delbosc, 2012, De Vos et al., 2013), there is a scarcity of studies applying these concepts in the context of a prolonged and system-wide disruption due to the pandemic. This research thus constitutes an in-depth empirical study.
Secondly, from the model, we can deduce practical implications of the study, i.e., identify possible touchpoints for policy interventions. We especially pay attention to those who are extremely vulnerable to disruptions in public transport service. They are those who, because of the disruption and their lack of resources to re-mode, experience discontinued access to critical healthcare facilities. In Fig. 8, the numbered constructs in shaded boxes are the touchpoints for policy interventions or recommendations in the event of a pandemic like COVID-19. Below are our five recommendations, which are drawn from the two-step model.
First, considering that public transport disruption renders many individuals vulnerable, we ensure that the suspension of public transport services is kept short, while maintaining proper health protocols. This can be done by first restoring the pre-COVID public transport supply (especially, traditional jeepney, which served a significant percentage of the trips pre-pandemic but were then prohibited from resuming full operations on all routes during the pandemic), and augmenting more supply if needed. Second, since individuals using personal transport during pre-lockdown are the most resistant to the disruption, our results imply the need to encourage a shift to personal (but environment-friendly) modes of transport, such as walking and cycling, and discourage the use of private vehicles. Third, when public transport was suspended, roads became safer, allowing the emergence of cycling as a viable transport mode. To ensure that people continue cycling even when road traffic returns, exclusive protected lanes must be set up so that cyclists are safely segregated from vehicular traffic. Fourth, since our transport systems can never be fully resistant to disruption, we must provide resources to vulnerable individuals to enable re-moding. This includes provision of bicycle-sharing or bike loans/subsidies to make bike-ownership more accessible, as well as public transport and shuttle services which are responsive to the new origin–destination patterns and trip schedules of health care workers, and finally special services to patients at the neighborhood level. Finally, given that the well-being impact of accessibility is in the emotional dimension, caused by exhaustion/tiredness and anxiety due to risk of infection, we can reduce unnecessary apprehension by adhering to health and social distancing requirements. We ensure that public transport services are safe and strictly compliant to health protocols.
Although the present study contributes valuable insights at both theoretical and practical levels, we acknowledge several limitations. First, the results are only preliminary, based on limited respondent size drawn from convenience and purposive sampling. Although a qualitative approach fits the current objectives of the study, we recommend that this be complemented by quantitative methods, especially if a more representative sampling can be done. Second, we also recommend more objective measures of access and well-being. In the present study, the change in access is self-reported and not quantified in terms of frequency, duration, and cost. The well-being construct is likewise only operationalized in its multi-faceted subjective dimensions (emotional, life satisfaction, and needs fulfillment). By resorting to objective measures, new data sources, beyond traditional surveys, can be explored (e.g., Voukelatou et al, 2021). Finally, we also propose the use of panel data in measuring change of access and well-being. Such longitudinal data should correspond to at least two time points: before the lockdown and during the lockdown.
Institutional ethics review. Ethics approval for this study was obtained from the University of Asia and the Pacific (#MAN116L/2020).
Funding
The Authors did not receive any specific funding for this work.
CRediT authorship contribution statement
Varsolo Sunio: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Visualization, Supervision, Project administration. Jedd Carlo Ugay: Conceptualization, Investigation, Writing – original draft. Chen-Wei Li: Conceptualization, Investigation, Writing – original draft. Harvy Joy Liwanag: Conceptualization, Investigation, Writing – original draft. Jerico Santos: Conceptualization, Investigation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We thank AltMobility PH for their assistance in the dissemination of the survey.
Footnotes
In the Philippines, there are four types of community quarantines implemented: enhanced community quarantine (ECQ), modified enhanced community quarantine (MECQ), general community quarantine (GCQ) and modified general community quarantine (MGCQ). The strictest form is ECQ, and the most lenient is MGCQ. Since public transport services are suspended during ECQ and MECQ, we therefore lump together both into just one category “ECQ” for brevity. Public transport operation is allowed in areas under GCQ and MGCQ.
Multiple answers are allowed so the sum of the responses exceeds 100%.
Appendix A: SURVEY QUESTIONNAIRE AND INTERVIEW PROTOCOLS
PHASE I. SURVEY QUESTIONNAIRE.
The survey form, prepared via Google form, first asks the respondent to choose one of the following 5 self-descriptions. Depending on the selected option, the follow-up questions are different.
|
Choose one: □ I am a health worker (e.g. doctor, nurse, other health personnel) who was able to work during either ECQ or GCQ (or both). □ I am a health worker (e.g. doctor, nurse, other health personnel) who was NOT at all able to work during BOTH ECQ and GCQ due to transport-related reasons. □ I am a patient who sought medical attention during community quarantine and was able to go to a healthcare facility. □ I am a patient who sought medical attention during community quarantine but was NOT able to go to a healthcare facility. □ None of the above *Note: ECQ and GCQ mean enhanced and general community quarantines, respectively. They refer to varying levels of lockdown or mobility restrictions, with ECQ being the strictest. |
If the respondent is a health worker (e.g. doctor, nurse, other health personnel), he/she answers the following questions:
| Choose your age group | □22 years old and below □23-35 years old □36 − 50 years old □51-60 years old □Above 60 years old |
|---|---|
| Choose your gender | □Male □Female □Other |
| Choose your income group (by monthly income) | □More than P200,000 □P100,000 - P200,000 □P40,000 - P99,999 □P10,000 - P39,999 □Less than P10,000 |
| Current Residence (Region) | [Input geographical region] |
| Current Residence (Barangay, Municipality/City) | [Input residence address] |
| Name of (main) healthcare facility where you work (facility can be hospital, community health center, drugstore, clinic, etc) | [Input name] |
| Location of workplace identified in previous number (Town/city and region) | [Input location] |
| Type of health worker | □Doctor – Resident/Fellows □Doctor – Specialist □Medical clerk/intern □Nurse □Associate (e.g. aides, helpers, social workers, therapists) □Lab personnel (medical technologist and technician) □Radiology personnel (radiologic technologist) □Health management & support worker (e.g. accountant in hospital, admin personnel, clerical worker) □Pharmacist □Other |
| Pre-Lockdown Mode of Transport (Primary Mode Used) | [Enter mode] |
| ECQ Mode of Transport (Primary Mode Used) | [Enter mode] |
| GCQ Mode of Transport (Primary Mode Used) | [Enter mode] |
| How was your access (or travel) to healthcare facility impacted during the quarantine since March 2020? | □Not able to access or go to the healthcare facility □Not impacted □Negatively impacted □Positively impacted |
| How was your access (or travel) to healthcare facility impacted by the reduction in mobility, particularly public transport? | □Not able to access or go to the healthcare facility □Not impacted □Negatively impacted □Positively impacted |
If the healthcare worker was able to work during either ECQ or GCQ (or both), the following are the next questions:
| During the ECQ or GCQ, you were still able to continue going to work. What is the impact of this on your well-being? | □Severe negative impact □Moderate negative impact □No impact □Moderate positive impact □High positive impact |
|---|---|
| Any individual/group who made possible your continued access to healthcare facility during ECQ/GCQ (e.g. someone who lent you transport mode)? Please specify in general terms. | [Free input] |
On the other hand, if the healthcare worker was not able to work during BOTH ECQ and GCQ due to transport-related reasons, the following are the next questions:
| What is the impact of discontinued access (or not being able to travel) to a healthcare facility on your general well-being? | □Severe negative impact □Moderate negative impact □No impact □Moderate positive impact □High positive impact |
If the respondent is a medical patient who sought medical attention during community quarantine, the following questions are asked:
| Choose your age group | □22 years old and below □23-35 years old □36 − 50 years old □51-60 years old □Above 60 years old |
|---|---|
| Choose your gender | □Male □Female □Other |
| Choose your income group (by monthly income) | □More than P200,000 □P100,000 - P200,000 □P40,000 - P99,999 □P10,000 - P39,999 □Less than P10,000 |
| Your employment sector | □Agriculture □Industry □Services □Others □Not employed |
| Your occupation | □Manager □Professional □Technician/associate professional □Clerical support worker □Skilled agricultural, forestry and fishery worker □Plant machine operator / assembler □Others □Not employed |
| Current Residence (Region) | [Input geographical region] |
| Current Residence (Barangay, Municipality/City) | [Input residence address] |
| Name of Healthcare facility you went to / would have gone to | [Input name] |
| Location of the healthcare facility identified in previous number (Town/city and region) | [Input location] |
| Was your medical appointment during ECQ/GCQ considered necessary? / Was the (missed/canceled) medical appointment supposed to be necessary? | □Yes, it was an essential medical appointment. □No, it could be deferred to a later date. |
| What health condition did you have that required a visit to the medical facility? | □Communicable disease (e.g. TB, dengue, etc.) □Non-communicable (e.g. Diabetes, Hypertension, etc.) □Covid-related □I do not wish to disclose □Others |
| Kindly further specify your health condition (e.g. diabetes, dengue, etc.) You may leave it blank if you prefer not to disclose it. | [Free input] |
| When did you seek medical attention for this case? Choose all that apply. / When was the appointment supposed to have been made? Choose all that apply. Choose all that apply | □Within 2 months before lockdown □ECQ □GCQ |
| Pre-Lockdown Mode of Transport (Primary Mode Used in going to/from the healthcare facility) | [Enter mode] |
| ECQ Mode of Transport (Primary Mode Used in going to/from the healthcare facility) | [Enter mode] |
| GCQ Mode of Transport (Primary Mode Used in going to/from the healthcare facility) | [Enter mode] |
If the medical patient was able to go to a healthcare facility for medical care, the next set of questions is:
| How was your access (or visit) to the healthcare facility impacted during the quarantine since March 2020? | □Not able to access or visit the healthcare facility □Not impacted □Negatively impacted (i.e. able to visit the healthcare facility, but with so much difficulty) □Positively impacted |
|---|---|
| How was your access (or visit) to the healthcare facility impacted by the reduction in mobility, particularly public transport? | □Not able to access or visit the healthcare facility □Not impacted □Negatively impacted (i.e. able to visit the healthcare facility, but with so much difficulty) □Positively impacted |
| What is the impact of (continued) access to medical care during ECQ/GCQ to your health and well-being? | □Severe negative impact □Moderate negative impact □No impact □Moderate positive impact □High positive impact |
| If applicable, what is the impact of (reduced) access to medical care during ECQ/GCQ to your health and well-being? | □No impact □Moderate impact □Severe impact □Not applicable (I received proper medical care during ECQ/GCQ) |
| Any individual/group who made possible your continued access to healthcare facility during ECQ/GCQ (e.g. someone who lent you transport mode)? Please specify in general terms. |
On the other hand, if the medical patient was not able to go to a healthcare facility for medical care, the questions are:
| How was your access (or visit) to the healthcare facility impacted during the quarantine since March 2020? | □Not able to access or visit the healthcare facility □Not impacted □Negatively impacted □Positively impacted |
|---|---|
| How was your access (or visit) to healthcare facility impacted by the reduction in mobility, particularly public transport? | □Not able to access or visit the healthcare facility □Not impacted □Negatively impacted □Positively impacted |
| What is the impact of having discontinued access (or not being able to travel) to healthcare facility to your general well-being? | □Severe negative impact □Moderate negative impact □No impact □Moderate positive impact □High positive impact □Not applicable (I received proper medical care during ECQ/GCQ) |
PHASE II. INTERVIEW.
After answering the survey form, all the respondents were contacted for follow-up interviews by video/phone call.
For healthcare workers.
1. SUBJECTIVE WELL-BEING IN GENERAL.
Considering that you were able (were not able) to continue working and providing essential health-related services during the quarantine, how do you generally feel about yourself and your life?
2. IMPACT OF SUSPENSION/REDUCTION OF PUBLIC TRANSPORT SERVICE ON YOUR ACCESS TO HEALTHCARE FACILITY Considering that during ECQ public transport was suspended and during GCQ public transport was reduced, kindly describe its impact on your travel to the health facility where you work.
(Additional question if applicable) You did mention that you were not able to travel during the ECQ. Is this due to the unavailability of transport? Can you elaborate on the impact then of public transport suspension?
3. MODES USED BEFORE QUARANTINE, DURING ECQ AND GCQ.
Considering that you were able (were not able) to continue going to the health facility where you work, can you enumerate all transport modes you used pre-lockdown, during ECQ, and then GCQ? Among the modes enumerated, please identify the primary/typical modes used.
4. FACTORS INFLUENCING RESILIENCE AGAINST PUBLIC TRANSPORT SUSPENSION/REDUCTION.
(Question if applicable) Considering that you were able to continue going to the health facility where you work despite the suspension or reduction in public transport, you can be considered resilient. Can you enumerate all the factors that you think contribute to your resilience?
For medical patients.
1. SUBJECTIVE WELL-BEING IN GENERAL.
Considering that you were able to (not able to) avail of an essential health-related service during the quarantine, how do you generally feel about yourself and your life?
2. IMPACT OF SUSPENSION/REDUCTION OF PUBLIC TRANSPORT SERVICE ON YOUR ACCESS TO HEALTHCARE FACILITY.
Considering that during ECQ public transport was suspended and during GCQ public transport was reduced, kindly describe its impact on your travel to the health facility where you availed the medical service.
(Additional question if applicable) You did mention that you were not able to go to the healthcare facility for medical care during the ECQ. Is this due to the unavailability of transport? Can you elaborate on the impact then of public transport suspension?
3. MODES USED BEFORE QUARANTINE, DURING ECQ AND GCQ.
Considering that you managed (did not manage) to go to the health facility where you availed (or would have availed) of a healthcare service, can you enumerate all transport modes you used pre-lockdown, during ECQ, and then GCQ? Among the modes enumerated, please identify the primary/typical modes used.
4. FACTORS INFLUENCING RESILIENCE AGAINST PUBLIC TRANSPORT SUSPENSION/REDUCTION.
(Question if applicable) Considering that you were able to go to the health facility where you availed of medical service despite the suspension or reduction in public transport, you can be considered resilient. Can you enumerate all the factors that you think contribute to your resilience? I understand that in your case, you have been resilient amidst the limitation/suspension of public transport. Can you describe the efforts required from you in order to be resilient?
PHASE III. FOLLOW-UP INTERVIEW ON WELL-BEING.
The researchers processed and examined the data collected so far from the preceding phases, and then requested the respondents for follow-up interviews by video/phone call or email.
To the respondent: We have done an initial comparison of the responses of all respondents and we are hoping you will take time once again to answer a few questions. You may have already touched on some in your previous answers, but we would like to be more explicit.
We asked you about your well-being in general in #1 (“….how do you generally feel about yourself and your life?”). Well-being has multiple dimensions and based on the answers from our respondents, different respondents focus on different aspects of well-being. We would like therefore to ask your views on each dimension of your well-being to make responses across respondents comparable. Also if you think it is significant to divide the period from the start of the lockdown (mid-March) to the present day (mid-September) in terms for example of ECQ and GCQ, please feel free to do so when responding to each question below.
-
1.
Wellbeing- Daily Experience. How stressed, exhausted, anxious, rested, calm, etc. do you feel these past months (from start of lockdown until today)? Also, please rate your answer on a scale from −10 (very stressed) to + 10 (well rested) with 0 as neutral.
-
2.
Wellbeing- Life fulfillment. Over-all, how fulfilled or satisfied do you feel about your life nowadays (from start of lockdown until today)? To what extent do you feel the things you do these days in your life are worthwhile? Also, please rate your answer on a scale from −10 (extremely dissatisfied) to + 10 (extremely satisfied) with 0 as neutral.
-
3.
Wellbeing-Essential Needs. To what extent are your basic needs (e.g. employment, medical, family needs) satisfied these days (from start of lockdown until today)? Also, please rate your answer on a scale from −10 (extremely not satisfied) to + 10 (extremely satisfied) with 0 as neutral.
-
4.
How much does each of the three dimensions above affect your over-all well-being? Please assign percentage weights (totaling 100 %) to each dimension:
References
- Abramson D.M., Grattan L.M., Mayer B., Colten C.E., Arosemena F.A., Bedimo-Rung A., Lichtveld M. The resilience activation framework: a conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. J. Behav. Heal. Serv. Res. 2015;42(1):42–57. doi: 10.1007/s11414-014-9410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen M.H., Agergaard J., Møller-Jensen L., Oteng-Ababio M., Yiran G.A.B. Mobility disruptions in Accra: Recurrent flooding, fragile infrastructure and climate change. Sustainability. 2022;14(21):13790. [Google Scholar]
- Beaudet M., Ravensbergen L., DeWeese J., Beaubien-Souligny W., Nadeau-Fredette A.C., Rios N., El-Geneidy A. Accessing hemodialysis clinics during the COVID-19 pandemic. Transport. Res. Interdiscipl. Perspect. 2022;13 doi: 10.1016/j.trip.2021.100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhamra R., Dani S., Burnard K. Resilience: the concept, a literature review and future directions. Int. J. Prod. Res. 2011;49(18):5375–5393. [Google Scholar]
- Chandra Y., Shang L. An RQDA-based constructivist methodology for qualitative research. Qual. Mark. Res. Int. J. 2017;20(1):90–112. [Google Scholar]
- Chen K.L., Brozen M., Rollman J.E., Ward T., Norris K.C., Gregory K.D., Zimmerman F.J. How is the COVID-19 pandemic shaping transportation access to health care? Transport. Res. Interdiscipl. Perspect. 2021;10 doi: 10.1016/j.trip.2021.100338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran A.L., McDonald N.C., Prunkl L., Vinella-Brusher E., Wang J., Oluyede L., Wolfe M. Transportation barriers to care among frequent health care users during the COVID pandemic. BMC Public Health. 2022;22(1):1–10. doi: 10.1186/s12889-022-14149-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuignet T., Perchoux C., Caruso G., Klein O., Klein S., Chaix B., Gerber P. Mobility among older adults: Deconstructing the effects of motility and movement on wellbeing. Urban Stud. 2020;57(2):383–401. [Google Scholar]
- Dargin J.S., Mostafavi A. Human-centric infrastructure resilience: Uncovering well-being risk disparity due to infrastructure disruptions in disasters. PLoS One. 2020;15(6):e0234381. doi: 10.1371/journal.pone.0234381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vos J., Schwanen T., Van Acker V., Witlox F. Travel and subjective well-being: A focus on findings, methods and future research needs. Transp. Rev. 2013;33(4):421–442. [Google Scholar]
- Delbosc A. The role of well-being in transport policy. Transp. Policy. 2012;23:25–33. [Google Scholar]
- Delbosc A., Currie G. Exploring the relative influences of transport disadvantage and social exclusion on well-being. Transp. Policy. 2011;18(4):555–562. [Google Scholar]
- Dickins M., Johnstone G., Renehan E., Lowthian J., Ogrin R. The barriers and enablers to service access for older women living alone in Australia. Ageing Soc. 2022;42(4):849–867. [Google Scholar]
- Dong S., Esmalian A., Farahmand H., Mostafavi A. An integrated physical-social analysis of disrupted access to critical facilities and community service-loss tolerance in urban flooding. Comput. Environ. Urban Syst. 2020;80 [Google Scholar]
- Eisenhardt K.M. Building theories from case study research. Acad. Manag. Rev. 1989;14(4):532–550. [Google Scholar]
- Eisenhardt K.M., Graebner M.E. Theory building from cases: Opportunities and challenges. Acad. Manag. J. 2007;50(1):25–32. [Google Scholar]
- Franklin P., Gkiouleka A. A scoping review of psychosocial risks to health workers during the Covid-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18(5):2453. doi: 10.3390/ijerph18052453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geurs K.T., Van Wee B. Accessibility evaluation of land-use and transport strategies: review and research directions. Journal of Transport Geography. 2004;12(2):127–140. [Google Scholar]
- Gu Y., Fu X., Liu Z., Xu X., Chen A. Performance of transportation network under perturbations: Reliability, vulnerability, and resilience. Transport. Res. Part E: Logist. Transport. Rev. 2020;133 [Google Scholar]
- Hernandez D., Rossel C. Inequality and access to social services in Latin America: space–time constraints of child health checkups and prenatal care in Montevideo. J. Transp. Geogr. 2015;44:24–32. [Google Scholar]
- Hernandez D., Rossel C. Gender inequality, transport, and wellbeing: the case of child healthcare in Uruguay. J. Transp. Health. 2022;26 [Google Scholar]
- Hjorthol R. Transport resources, mobility and unmet transport needs in old age. Ageing Soc. 2013;33(7):1190–1211. [Google Scholar]
- Jain R., Dupas P. The effects of India's COVID-19 lockdown on critical non-COVID health care and outcomes: Evidence from dialysis patients. Soc Sci Med. 2022;296 doi: 10.1016/j.socscimed.2022.114762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Japan International Cooperation Agency (2017). Follow-up Survey on Roadmap for Transport Infrastructure Development for Greater Capital Region (GCR). FINAL REPORT. Retrieved October 2, 2022, from https://openjicareport.jica.go.jp/pdf/1000041638_02.pdf.
- Kahneman, D., & Deaton, A. (2010). High income improves evaluation of life but not emotional well-being. Proceed. Natl. Acad. Sci., 107(38), 16489-16493. [DOI] [PMC free article] [PubMed]
- Kar A., Carrel A.L., Miller H.J., Le H.T. Public transit cuts during COVID-19 compound social vulnerability in 22 US cities. Transp. Res. Part D: Transp. Environ. 2022;110 doi: 10.1016/j.trd.2022.103435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. Assessing mobility in an aging society: Personal and built environment factors associated with older people’s subjective transportation deficiency in the US. Transport. Res. F: Traffic Psychol. Behav. 2011;14(5):422–429. [Google Scholar]
- Kocatepe A., Ulak M.B., Kakareko G., Ozguven E.E., Jung S., Arghandeh R. Measuring the accessibility of critical facilities in the presence of hurricane-related roadway closures and an approach for predicting future roadway disruptions. Nat. Hazards. 2019;95(3):615–635. [Google Scholar]
- Kuhlicke C. Resilience: a capacity and a myth: findings from an in-depth case study in disaster management research. Nat. Hazards. 2013;67(1):61–76. [Google Scholar]
- Lemieux T., Milligan K., Schirle T., Skuterud M. Initial impacts of the COVID-19 pandemic on the Canadian labour market. Can. Public Policy. 2020;46(S1):S55–S65. doi: 10.3138/cpp.2020-049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Zhang Y., Sze N.N., Wang P. Effects of tube service disruptions on the usage of the London Cycle Hire. Travel Behav. Soc. 2022;29:257–265. [Google Scholar]
- Liu Q., Liu Z., Lin S., Zhao P. Perceived accessibility and mental health consequences of COVID-19 containment policies. J. Transp. Health. 2022;101354 doi: 10.1016/j.jth.2022.101354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthans F., Vogelgesang G.R., Lester P.B. Developing the psychological capital of resiliency. Hum. Resour. Dev. Rev. 2006;5(1):25–44. [Google Scholar]
- Marsden G., et al. Studying disruptive events: innovations in behaviour, opportunities for lower carbon transport policy? Transp. Policy. 2020;94:89–101. [Google Scholar]
- Mattsson L.G., Jenelius E. Vulnerability and resilience of transport systems–A discussion of recent research. Transp. Res. A Policy Pract. 2015;81:16–34. [Google Scholar]
- Mouratidis K. Urban planning and quality of life: A review of pathways linking the built environment to subjective well-being. Cities. 2021;115 [Google Scholar]
- National Economic and Development Authority (2020).Managing Risks while letting economy recover key to PH solid growth and development. Retrieved February 14, 2020, from https://neda.gov.ph/managing-risks-while-letting-economy-recover-key-to-ph-solid-growth-and-development-neda/.
- Nordbakke S., Schwanen T. Well-being and mobility: A theoretical framework and literature review focusing on older people. Mobilities. 2014;9(1):104–129. [Google Scholar]
- Nordbakke S., Schwanen T. Transport, unmet activity needs and wellbeing in later life: exploring the links. Transportation. 2015;42(6):1129–1151. [Google Scholar]
- Núñez A., Sreeganga S.D., Ramaprasad A. Access to Healthcare during COVID-19. Int. J. Environ. Res. Public Health. 2021;18(6):2980. doi: 10.3390/ijerph18062980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oluyede L., Cochran A.L., Wolfe M., Prunkl L., McDonald N. Addressing transportation barriers to health care during the COVID-19 pandemic: perspectives of care coordinators. Transp. Res. A Policy Pract. 2022;159:157–168. doi: 10.1016/j.tra.2022.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palm M., Sturrock S.L., Howell N.A., Farber S., Widener M.J. The uneven impacts of avoiding public transit on riders’ access to healthcare during COVID-19. J. Transp. Health. 2021;22 doi: 10.1016/j.jth.2021.101112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J., Chowdhury S. Towards an enabled journey: barriers encountered by public transport riders with disabilities for the whole journey chain. Transp. Rev. 2022;42(2):181–203. [Google Scholar]
- Philippine Statistics Authority, 2020. Statistical Tables on Labor Force Survey (LFS): January 2020. Retrieved March 1, 2020. https://psa.gov.ph/content/statistical-tables-labor-force-survey-lfs-january-2020.
- Pregnolato M., Ford A., Wilkinson S.M., Dawson R.J. The impact of flooding on road transport: A depth-disruption function. Transp. Res. Part D: Transp. Environ. 2017;55:67–81. [Google Scholar]
- Reardon L., Abdallah S. Well-being and transport: Taking stock and looking forward. Transp. Rev. 2013;33(6):634–657. [Google Scholar]
- Saberi M., Ghamami M., Gu Y., Shojaei M.H.S., Fishman E. Understanding the impacts of a public transit disruption on bicycle sharing mobility patterns: A case of Tube strike in London. J. Transp. Geogr. 2018;66:154–166. [Google Scholar]
- Shergold I. Taking part in activities, an exploration of the role of discretionary travel in older people's wellbeing. J. Transp. Health. 2019;12:195–205. [Google Scholar]
- Smith M., Calder-Dawe O., Carroll P., Kayes N., Kearns R., Lin E.Y.J., Witten K. Mobility barriers and enablers and their implications for the wellbeing of disabled children and young people in Aotearoa New Zealand: A cross-sectional qualitative study. Wellbeing, Space Soc. 2021;2 [Google Scholar]
- Social Weather Stations Fourth Quarter 2020 Social Weather Survey: 42% of non-home-based working Filipinos say going to work is very much harder; 44% of them walk to work. 2021. http://www.sws.org.ph/swsmain/artcldisppage/?artcsyscode=ART-20210507063140 Retrieved October 2, 2022, from.
- Stanley J.K., Hensher D.A., Stanley J.R., Vella-Brodrick D. Mobility, social exclusion and well-being: Exploring the links. Transp. Res. A Policy Pract. 2011;45(8):789–801. [Google Scholar]
- Stanley J.K., Hensher D.A., Stanley J.R., Vella-Brodrick D. Valuing changes in wellbeing and its relevance for transport policy. Transp. Policy. 2021;110:16–27. [Google Scholar]
- Social Weather Stations (2020). SWS May 2020 Covid-19 Mobile Phone Survey – Report No. 8: The suspension of public transport is burdensome for 77% of families; the shutdown of private businesses and stores is burdensome for 80%. Retrieved October 2, 2022, from http://www.sws.org.ph/swsmain/artcldisppage/?artcsyscode=ART-20200605180641.
- Sunio V., Mateo-Babiano I. Pandemics as ‘windows of opportunity’: Transitioning towards more sustainable and resilient transport systems. Transp. Policy. 2022;116:175–187. [Google Scholar]
- Sunio V., Li W.J., Pontawe J., Dizon A., Valderrama J.B., Robang A. Service contracting as a policy response for public transport recovery during the Covid-19 Pandemic: A preliminary evaluation. Transport. Res. Interdiscipl. Perspect. 2022;13 doi: 10.1016/j.trip.2022.100559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunio V., Cortes R.Z., Lactao J. Rhetorical orientations for promoting sustainable travel behavior: A perspective. Res. Transp. Econ. 2022;91 [Google Scholar]
- Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J. Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaithatkul P., Chalermpong S., Laosinwattana W., Kato H. Case Studies on Transport Policy; 2022. Mobility, Activities, and Happiness in Old Age: Case of the Elderly in Bangkok. [Google Scholar]
- The Straights Times (2020). Philippines suffers worst job losses in 15 years due to Covid-19 and lockdown. Retrieved January 9, 2020, from https://www.straitstimes.com/asia/se-asia/philippines-suffers-worst-job-losses-in-15-years-due-to-covid-19-and-lockdown.
- Tiikkaja H., O'Hern S., Viri R. Perceptions of trip making and wellbeing. Transportat. Res. Interdiscipl. Perspect. 2021;12 doi: 10.1016/j.trip.2021.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirachini A., Cats O. COVID-19 and public transportation: Current assessment, prospects, and research needs. J. Public Transp. 2020;22(1):1. doi: 10.5038/2375-0901.22.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varela C., Young S., Mkandawire N., Groen R.S., Banza L., Viste A. Transportation barriers to access health care for surgical conditions in Malawi a cross sectional nationwide household survey. BMC Public Health. 2019;19(1):264. doi: 10.1186/s12889-019-6577-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vecchio G., Tiznado-Aitken I., Hurtubia R. Transport and equity in Latin America: a critical review of socially oriented accessibility assessments. Transp. Rev. 2020;40(3):354–381. [Google Scholar]
- Verma A., Rajput R., Verma S., Balania V.K., Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 Diabetes Mellitus. Diabetes Metab. Syndr. 2020;14(5):1213–1216. doi: 10.1016/j.dsx.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voukelatou V., Gabrielli L., Miliou I., Cresci S., Sharma R., Tesconi M., Pappalardo L. Measuring objective and subjective well-being: dimensions and data sources. Int. J. Data Sci. Analyt. 2021;11(4):279–309. [Google Scholar]
- Walker B., Holling C.S., Carpenter S.R., Kinzig A. Resilience, adaptability and transformability in social–ecological systems. Ecol. Soc. 2004;9(2) [Google Scholar]
- Widener M.J., Hatzopoulou M. Contextualizing research on transportation and health: a systems perspective. J. Transp. Health. 2016;3(3):232–239. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan Y., Zhong S., Tian J., Jia N. An empirical study on consumer automobile purchase intentions influenced by the COVID-19 outbreak. J. Transp. Geogr. 2022;104 doi: 10.1016/j.jtrangeo.2022.103458. [DOI] [PMC free article] [PubMed] [Google Scholar]