Abstract
Streptococcus intermedius is a commensal bacterium reported in a few cases as the causative agent of brain and lung abscesses, pneumonia, and endocarditis. Lung abscesses due to Streptococcus intermedius are rare, especially in pregnancy. We describe the first case of lung abscess due to Streptococcus intermedius in a pregnant woman.
Keywords: infectious diseases; lung abscess; pneumonia, bacterial; respiratory system; SARS‐CoV‐2
Streptococcus intermedius is part of the commensal oral flora, but it has been described in a few cases as the causal agent of lung abscesses. We describe an unusual case of lung abscess caused by Streptococcus intermedius in pregnancy.
1. INTRODUCTION
Streptococcus intermedius is a catalase‐negative, gram‐positive cocci, whose most isolates are nonhemolytic with small colony‐forming species, which belongs to the Streptococcus anginosus group (SAG), which has also been referred to as the Streptococcus milleri group, which includes 3 organisms: S. anginous, S. intermedius, and S. constellatus. 1 This bacterial group has not been recognized as a causative pathogen. However, with the presence of certain factors, SAG could induce noninvasive infections and also invasive infections after getting into sterile body sites, such as the blood and serosal cavity, which is why it could affect the tissues and organs of several systems of the body. 2
The SAG species differ in the virulence factors that they produce. Because S. intermedius produces sialidase and hyaluronidase, which can destroy host tissues, converting them into nutrients for bacterial growth, whereas S. constellatus produces only hyaluronidase and S. anginous none of these. 3 Probably, for this reason, S. intermedius has the ability to form abscesses in several body locations. However, its virulence factors are unclear at present. 4 This feature gives it a unique distinction compared with other alpha‐hemolytic streptococcal species and makes its management require, in most cases, surgical intervention along with antibiotic therapy. 4
Streptococcus intermedius is part of the commensal oral flora in humans, and it is frequently associated with brain and liver abscesses, but less frequently with pleuropulmonary infections including pneumonia, pleural effusion, and empyema, and in a few cases, it can also be the causal agent of lung abscesses. 1 , 5 Among the risk factors for these infections, smoking, alcoholism, dental diseases, chronic obstructive pulmonary disease, malignant neoplasms, liver cirrhosis, and diabetes have been described. 1 Through this case report with a literature review, we discuss an acute presentation of S. intermedius lung abscess in a pregnant woman with radiological findings that make it difficult to distinguish it as a lung neoplasm, empyema, or abscess.
2. CASE REPORT
A 25‐year‐old woman with a 34‐week and 5‐day pregnancy, with a medical history of astigmatism, consulted the emergency department, stating that in the three previous weeks, she had presented with cough with hemoptysis, fatigue, headache, odynophagia, and 6 kg weight loss. On physical exam, vital signs were within the normal ranges, and a gravid uterus, fetal heart rate, and fetal movements were present. Initially, the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV2) antigen test was negative. However, chest radiography showed a lung mass in the upper segment of the right lower lobe. Also, serial sputum smear microscopy for tuberculosis was negative.
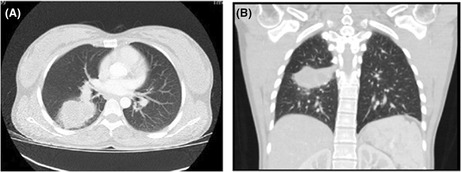
Given the persistence of symptoms, a polymerase chain reaction (PCR) to SARS‐CoV2 was performed with a positive result, confirming a mild acute respiratory infection due to SARS‐CoV2 that evolved satisfactorily with management at home. Nevertheless, a high‐resolution chest computed tomography (CT) was taken, reporting a lung mass in the upper segment of the right lower lobe adjacent to the horizontal pulmonary fissure of origin to be determined (Figure 1). Then, a sputum PCR was performed for Mycobacterium tuberculosis and tuberculin test, which were negative, so given the characteristics of the mass, tuberculosis, or pulmonary mycosis were discarded. The Pneumology service performed a fibrobronchoscopy and bronchoalveolar lavage, obtaining negative cytology for malignancy and also a Gram stain, KOH test, smear microscopy for tuberculosis, and PCR for mycobacteria with negative results, so the patient was discharged with ambulatory management.
FIGURE 1.
(A) Axial computed tomography view showing a lesion in the upper segment of the lower lobe on the right side. (B) Coronal computed tomography view.
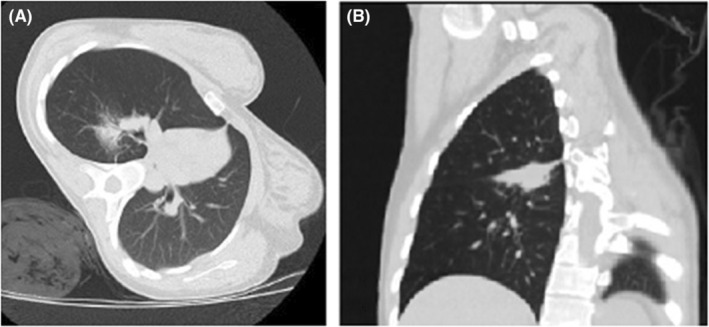
Ten days later, the patient was again consulted at the emergency department due to the persistence of respiratory symptoms. A high‐resolution chest CT reported an increase in the lung lesion size (Figure 2), so she was hospitalized. A lung biopsy was performed by interventional radiology after the pregnancy ended by cesarean section at 34 weeks and 5 days of the patient's pregnancy, draining purulent material. The newborn was female, with expected anthropometric measurements in relation to her prematurity and an Apgar score of 8 at 1 min and 10 at 10 min. The newborn did not present complications after birth; however, it required a kangaroo mother care intervention program.
FIGURE 2.
(A) Axial computed tomography view, shows an increase in the abscessed lesion in the upper segment of the lower lobe on the right side. (B) Coronal computed tomography view.
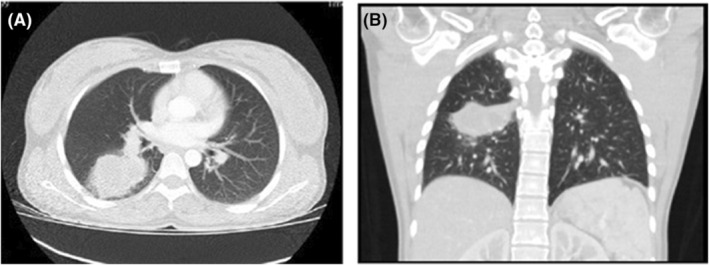
The microscopical examination of the purulent drained material from the lung lesion reported an acute bronchopneumonic process. The KOH test, Chinese ink, and smear microscopy for tuberculosis studies were also performed with negative results. However, the culture was positive, isolating a S. intermedius with the usual antibiotic susceptibility profile. The antibiotic management in the hospital was started with ceftriaxone and, 4 days later, given a good response to treatment, the patient was discharged with amoxicillin for 1 month. After discharge, symptoms resolved 1 week later, and tomographic findings reversed progressively after 4 months (Figure 3).
FIGURE 3.
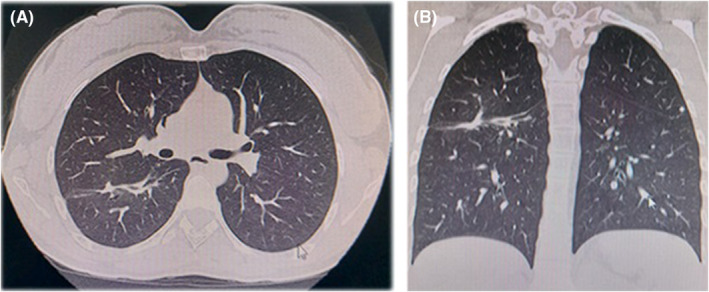
(A) Axial computed tomography view, showing thickening of the major fissure of the right lung associated with a small hyperdense image of irregular subpleural shape adjacent to the major fissure of the lower lobe, as residual changes in relation to pathological and surgical history. (B) Coronal computed tomography view.
3. DISCUSSION
Streptococcus intermedius infections have been described in a wide age range: For example, Nakagawa et al. 6 reported a lung abscess and empyema caused by S. intermedius in an immunocompetent 6‐month‐old boy, whereas Yanagihara et al. 7 reported a brain abscess as a complication of hepatopulmonary syndrome coexisting with interstitial pneumonia in a 76‐year‐old woman. However, the oldest patient reported was 80 years old and developed an empyema and a psoas abscess due to S. intermedius. 8 Our patient was also in this wide age range. Regarding sex predominance, respiratory infections due to SAG have been described more frequently in male patients with comorbid diseases who are typically complicated by pleural effusion. 9
Patients with infections due to S. intermedius usually present nonspecific symptoms such as fever, chills, and general discomfort among the cases described. However, additionally, patients would exhibit symptoms related to the body side affected by it, for example, seizures, headaches, nausea, vomiting in brain abscesses 10 , 11 or cough, sputum production, shortness of breath, hemoptysis in pneumonia, empyema, lung abscesses, 5 , 12 , 13 which are uncommon clinical complications from S. intermedius with few cases currently described (Table 1). Moreover, chest pain, chest distress, and even respiratory failure have been described in pleural effusion and mediastinal abscess due to SAG, besides, odynophagia, and cervicodynia in oropharynx infections. 2
TABLE 1.
Articles related to lung abscess due to Streptococcus intermedius.
| Age of publication—Article title | Type of article | Age | Gender | Medical history | Type of infection | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| 2006—A case of pulmonary abscess in which Haemophilus parainfluenzae and Streptococcus intermedius were isolated by percutaneous needle aspiration | Case report | 75 years old | Male | Esophago‐gastrectomy due to esophageal cancer | Lung abscess | Panipenem/Betamipron | Without data |
| 2013—Pyogenic Brain and Lung Abscesses due to Streptococcus intermedius | Case report | 36 years old | Male | Methamphetamine abuse | Lung and cerebral abscesses | Stereotaxic drainage of abscesses and unspecified intravenous antibiotic therapy | Without data |
| 2015—The clinical features of respiratory infections caused by the Streptococcus anginosus group | Cross‐sectional study (30 patients −16 patients with S. Intermedius) | 68.9 ± 14.2 years old (average) | 73.3% (22) Male |
Comorbidity diseases in 93.3% (28) Smoking history in 43.3% (13) Cerebrovascular disease in 40% (12) Neoplastic disease in 26.7% (8) Diabetes mellitus in 20% (6) |
Pneumonia in 63.3% (19) Lung abscess in 16.7% (5) Bacterial pleurisy in 20% (6) |
Antibiotic monotherapy in 83.3% (25) with Carbapenem 76% (19) Penicillin/beta‐lactamase inhibitors 12% (3) Macrolide 8% (2) Linezolid 4% (1) Drainage in 16.7% (5) Drainage + lung decortication in 46.7% (14) |
In‐hospital mortality in 6.7% (2) |
| 2016—Streptococcus intermedius Causing Necrotizing Pneumonia in an Immune Competent Female: A case report and literature Review | Case report | 52 years old | Female | Asthma, former smoker | Lung abscess | Ceftriaxone for 14 days plus decortication and resection of right upper lung lobe and chest tube insertion | Recovery from his symptoms and tomographic findings |
| 2017—Isolated Streptococcus intermedius pulmonary nodules | Case report | 29 years old | Male | Congenital nistagmus and umbilical hernia | Lung abscess | Ceftriaxone for 4 weeks | Recovery from his symptoms and tomographic findings |
| 2020—A case of an 80‐year‐old man with Empyema and Psoas Abscess | Case report | 80 years old | Male | Ischemic stroke, spinal stenosis, gastrectomy, coronary artery disease | Right empyema and psoas abscess | Thoracotomy for empyema and drainage of iliopsoas abscess plus ampicillin for 3 months | Recovery from his symptoms and tomographic findings |
| 2021—Streptococcus intermedius Pleuropulmonary Disease: A Not So Commonly Seen Radiological Picture | Case report | 54 years old | Male | Smoking | Right pneumonia with multiple intraparenchymal lung abscesses, empyema, and right pleural effusion | Azithromycin and ceftriaxone initially plus a right apical chest tube and vancomycin and piperacillin‐tazobactam subsequently due to clinical worsening | He died during hospitalization due to a septic shock |
| 2021—Streptococcus anginosus Lung Infection and Empyema: A Case Report and Review of the Literature | Case report | 37 years old | Male | Chronic bronchitis, colon polyps, smoking | Pneumonia with empyema | CT‐guided placement of pleural catheter with TPA irrigation with subsequently video‐assisted thoracoscopic surgery with lateral decortication and drainage of empyema with the placement of a chest tube plus ampicillin‐sulbactam for 10 days and oral amoxicillin for 2 days at the discharge | Full recovery from his symptoms and tomographic findings |
| 2021—Lateral thoracic artery aneurysm with a lung abscess and empyema caused by Streptococcus intermedius | Case report | 66 years old | Male | Arterial hypertension, Influenza infection in the previous month | Lung abscess with pyothorax and a pseudoaneurysm close to the lateral thoracic artery | Therapeutic thoracentesis plus ampicillin‐sulbactam, vancomycin, and transcatheter artery embolism | He died during hospitalization |
| 2021—Streptococcus intermedius: Unusual presentation and complication of lung abscess | Case report | 54 years old | Male | Without relevant medical history | Pneumonia, with lung abscess on the posterior medial aspect of the right lower lobe with discitis from T5 to T6 vertebral bodies | Thoracotomy with pulmonary decortication along with excision of the mediastinal mass plus metronidazole and ceftriaxone during hospitalization and amoxicillin‐clavulanate for 3 weeks after discharge | Recovery from his symptoms and tomographic findings |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging.
Also, it has been described with Haemophilus parainfluenzae as the causative pathogen in a pulmonary abscess in a 75‐year‐old man. 14 Besides, other rare infections in body sites due to S. intermedius have been described, such as a recently described case in which discitis was reported due to contiguous infection due to a lung abscess of the posterior right lower lobe due to S. intermedius. 15 It has also been described as a causative pathogen in Lemierre syndrome in a 21‐year‐old man with S. intermedius bacteremia 16 and in a 29‐year‐old woman who developed multiple lung abscesses secondary to a uterine empyema caused by an intrauterine device with the S. milleri group as the causative agent isolated. 17 Furthermore, isolated pulmonary nodules and infective endocarditis due to S. intermedius have also been described. 4 , 18 , 19 In our case, blood cultures were performed with a negative result, and no signs or symptoms related to probable or confirmed endocarditis were found. Moreover, a left thoracic artery pseudoaneurysm has been described as a secondary complication of a lung abscess in a 66‐year‐old man. 20
In regard to SARS‐CoV‐2 coinfection with Streptococcus intermedius, we reviewed the available medical literature in the major clinical databases (PubMed, Google Scholar, and SciELO). We found five articles, consisting of three case reports, 21 , 22 , 23 a case series, 24 and one cross‐sectional study. 25
The first case report describes a 14‐year‐old African American with SARS‐CoV‐2 infection who developed a severe rapidly progressive complicated sinusitis due to S. intermedius. 21 In this case, the infection progressed to orbital, subgaleal, and intracranial abscesses, requiring surgical intervention and a 4‐week course of intravenous antibiotic therapy, with a resolution of the infection and no neurologic sequelae. 21 The second case describes the case of an adult older than 65 years with a medical history of SARS CoV‐2 infection who developed a subdural empyema due to SAG, for which he underwent two craniectomies, achieving the eradication of the empyema and clinical improvement, for which he underwent two craniectomies, achieving the eradication of the empyema and clinical improvement. 22 Finally, the third case describes a 12‐year‐old adolescent with SARS‐CoV‐2 infection who developed appendicitis with perforated gangrenous tissue, from which the purulent material was positive for E. coli, SAG, and SARS‐CoV‐2. 23
Regarding the case series, this describes the course of six patients with complicated acute sinusitis and SARS CoV‐2 coinfection, of whom SAG was isolated in three patients. 24 Finally, one cross‐sectional study describes the incidence of beta‐hemolytic streptococci in patients with COVID‐19, finding an isolation rate of only 4.4% for SAG. 25 In sum, these observational studies show that coinfection between SARS CoV‐2 and SAG has been described, but they do not allow us to affirm that there is an association between SARS CoV‐2 coinfection and SAG.
In relation to SARS‐CoV‐2 infection in pregnancy, it could be higher than in the general population. 26 However, the risk factors for severe infection (asthma, hypertension, diabetes, overweight, obesity, and being a member of a black or ethnic minority ethnic group) are similar to those in the general population, 26 however, in our case, none of these risk factors were present. Although vertical transmission is possible, severe neonatal disease seems to be rare, which is consistent with the outcome obtained with the newborn in our case. 26 Furthermore, the use of corticosteroids anterograde in the case of preterm delivery as well as the treatment of severe COVID‐19 infection appears to be safe for the mother. 26 On the other hand, it is important to highlight that asymptomatic infections by COVID‐19 in pregnancy seem to be common, but their clinical significance seems to be uncertain. 26
With respect to the route of infection, the airway was the main route of dissemination for the infection in our case, and despite the fact that certain risk factors such as smoking, alcoholism, dental diseases, chronic obstructive pulmonary disease, malignant neoplasms, liver cirrhosis, and diabetes have been described, 1 in our case, none of these risk factors were present.
Regarding lung abscess, it is defined as a circumscribed area of pus or necrotic deposits in the lung tissue with the formation of cavities containing necrotic deposits or fluid caused by a microbial infection, and if suspected, chest computed tomography (CT) should be done because CT provides a more accurate anatomical definition than a chest X‐ray and can identify other abscesses and chest lesions that are not clearly delineated on a chest X‐ray. 27 On CT, an acute lung abscess is usually surrounded by a less well‐defined area of lung parenchyma filled with thick necrotic debris, often involving the apical segment of the inferior lobe of the right lung, which corresponds to the location in our case. 27 Furthermore, in some cases, CT can distinguish between lung carcinomas and abscesses because malignant lesions have a thicker wall and are more irregular than abscesses. 27 In our case, this differential diagnosis was considered due to the presence of irregular borders on CT, absence of fever, purulent sputum, and leukocytosis, as well as the persistence of the lesion. However, histological studies ruled out malignancy and confirmed a bacterial lung abscess due to S. intermedius.
Concerning the therapeutic approach, the first lines of treatment for susceptible S. intermedius strains to beta‐lactams could be penicilins, cephalosporins, and carbapenems. 28 Besides, a drainage procedure must be considered and performed in most abscess cases. 28
4. CONCLUSION
Pulmonary abscess due to S. intermedius is an uncommon clinical scenario, even more so in pregnancy. A few cases have been reported of S. intermedius associated with brain and lung abscesses, pleuropulmonary disease, and infective endocarditis. Thus, physicians should take this anaerobic gram‐positive organism into account in these clinical scenarios in order to allow a proper diagnosis and management.
AUTHOR CONTRIBUTIONS
Cristian Orlando Porras Bueno: Conceptualization; data curation; formal analysis; writing – original draft; writing – review and editing. Sharon Julieth González Trillos: Data curation; formal analysis; writing – review and editing. Diana Jimena Cano Rosales: Conceptualization; formal analysis; writing – review and editing. Edgar Augusto Bernal García: Conceptualization; formal analysis.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
None.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGEMENT
None.
Bueno COP, Trillos SJG, Rosales DJC, García EAB. Lung abscess due to Streptococcus intermedius associated with SARS CoV‐2 infection in pregnancy: Unusual presentation and complication of a commensal bacteria during pregnancy. Clin Case Rep. 2023;11:e06763. doi: 10.1002/ccr3.6763
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1. Tasleem A, Mahmood A, Sharma R. Streptococcus intermedius pleuropulmonary disease: a not so commonly seen radiological picture. Cureus. 2021;13(8):e17385. Published 2021 Aug 23. doi: 10.7759/cureus.17385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jiang S, Li M, Fu T, Shan F, Jiang L, Shao Z. Clinical characteristics of infections caused by Streptococcus anginosus group. Sci Rep. 2020;10(1):9032. Published 2020 Jun 3. doi: 10.1038/s41598-020-65977-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nagamune H, Whiley RA, Goto T, et al. Distribution of the intermedilysin gene among the anginosus group streptococci and correlation between intermedilysin production and deep‐seated infection with Streptococcus intermedius . J Clin Microbiol. 2000;38(1):220‐226. doi: 10.1128/JCM.38.1.220-226.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Catalya S, Komal B, Tulpule S, Raoof N, Sen S. Isolated Streptococcus intermedius pulmonary nodules. IDCases. 2017;8:48‐49. Published 2017 Mar 23. doi: 10.1016/j.idcr.2017.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Trabue C, Pearman R, Doering T. Pyogenic brain and lung abscesses due to Streptococcus intermedius . J Gen Intern Med. 2014;29(2):407. doi: 10.1007/s11606-013-2565-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nakagawa Y, Otake S, Oue T, Ryu H, Kasai M. Case of infant invasive Streptococcus intermedius infection suggesting the need for anaerobic cultures. J Infect Chemother. 2022;28(3):437‐439. doi: 10.1016/j.jiac.2021.11.002 [DOI] [PubMed] [Google Scholar]
- 7. Yanagihara T, Moriwaki A, Seki N, Akata K, Imanaga T. A brain abscess as a complication of hepatopulmonary syndrome coexisting with interstitial pneumonia. Nihon Kokyuki Gakkai Zasshi. 2011;49(7):534‐537. [PubMed] [Google Scholar]
- 8. Sakurai M, Nagasawa H, Takeuchi I, Yanagawa Y. A case of an 80‐year‐old man with empyema and psoas abscess. Case Rep Emerg Med. 2020;2020:8895785. Published 2020 Oct 24. doi: 10.1155/2020/8895785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Noguchi S, Yatera K, Kawanami T, et al. The clinical features of respiratory infections caused by the Streptococcus anginosus group. BMC Pulm Med. 2015;15:133. Published 2015 Oct 26. doi: 10.1186/s12890-015-0128-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erne BV, Exner C, Frauenfelder T, Schmid S, Weder W. A curious case of convulsion. Lancet. 2010;375(9730):2050. doi: 10.1016/S0140-6736(10)60592-2 [DOI] [PubMed] [Google Scholar]
- 11. Yamamoto M, Fukushima T, Ohshiro S, et al. Brain abscess caused by Streptococcus intermedius: two case reports. Surg Neurol. 1999;51(2):219‐222. doi: 10.1016/s0090-3019(97)00505-3 [DOI] [PubMed] [Google Scholar]
- 12. Hannoodi F, Ali I, Sabbagh H, Kumar S. Streptococcus intermedius causing necrotizing pneumonia in an immune competent female: a case report and literature review. Case Rep Pulmonol. 2016;2016:7452161. doi: 10.1155/2016/7452161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tripathi N, Ghosh K, Raghuram A. Streptococcus anginosus lung infection and empyema: a case report and review of the literature. Univ Louisville J Respir Infect. 2021;5(1):145‐154. [Google Scholar]
- 14. Miyamoto A, Tsuboi E, Takaya H, et al. A case of pulmonary abscess in which Haemophilus parainfluenzae and Streptococcus intermedius were isolated by percutaneous needle aspiration. Nihon Kokyuki Gakkai Zasshi. 2006;44(8):561‐566. [PubMed] [Google Scholar]
- 15. Manasrah N, Nanja Reddy S, Al Sbihi A, Hafeez W. Streptococcus intermedius: unusual presentation and complication of lung abscess. BMJ Case Rep. 2021;14(11):e245675. Published 2021 Nov 1. doi: 10.1136/bcr-2021-245675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chemlal K, Caby I, Memain N, Aubert D, Bruneel F. Syndrome de Lemierre dû à Streptococcus intermedius: une association inhabituelle [Streptococcus intermedius Lemierre syndrome: an unusual association]. Presse Med. 2000;29(29):1601‐1602. [PubMed] [Google Scholar]
- 17. van Laren M, van Walree NC, Kluytmans JA. Multiple lung abscesses secondary to a uterine empyema caused by an intrauterine device. Infection. 2011;39(4):385‐387. doi: 10.1007/s15010-011-0118-4 [DOI] [PubMed] [Google Scholar]
- 18. Tran MP, Caldwell‐McMillan M, Khalife W, Young VB. Streptococcus intermedius causing infective endocarditis and abscesses: a report of three cases and review of the literature. BMC Infect Dis. 2008;8:154. Published 2008 Nov 10. doi: 10.1186/1471-2334-8-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Salem A, Azeez S, Stirrup J, Lawrence D, Ruparelia N. Streptococcus intermedius masquerading as fungal infective endocarditis. Br J Hosp Med (Lond). 2019;80(11):674‐675. doi: 10.12968/hmed.2019.80.11.674 [DOI] [PubMed] [Google Scholar]
- 20. Fujihara T, Itoh N, Yamamoto S, Kurai H. Lateral thoracic artery aneurysm with lung abscess and empyema caused by Streptococcus intermedius . J Gen Fam Med. 2021;22(5):296‐297. Published 2021 May 5. doi: 10.1002/jgf2.448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Arteaga AA, Tran J, Frey H, Lewis AF. Rapidly progressive complicated acute bacterial sinusitis in the setting of severe pediatric SARS‐CoV‐2 infection. Ann Otol Rhinol Laryngol. 2022;131(10):1158‐1163. doi: 10.1177/00034894211055337 [DOI] [PubMed] [Google Scholar]
- 22. Charlton M, Nair R, Gupta N. Subdural empyema in adult with recent SARS‐CoV‐2 positivity case report. Radiol Case Rep. 2021;16(12):3659‐3661. Published 2021 Oct 2. doi: 10.1016/j.radcr.2021.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pani E, Collini L, Naselli A, et al. SARS‐Cov‐2 in peritoneal fluid of two children with COVID‐19: a rare finding. J Paediatr Child Health. 2022;58(4):702‐704. doi: 10.1111/jpc.15610 [DOI] [PubMed] [Google Scholar]
- 24. Guy K, Lelegren M, Shomaker K, Han J, Lam K. Management of complicated acute sinusitis in the setting of concurrent COVID‐19. Am J Otolaryngol. 2022;43(5):103603. doi: 10.1016/j.amjoto.2022.103603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Abdul‐hadi RA, Al‐charrakh AH. Prevalence of SARS‐CoV‐2 co‐ infection with β ‐ haemolytic streptococci in a sample of Iraqi patients. Teiko Med J. 2021;44(6):2917‐2928. [Google Scholar]
- 26. Wastnedge EAN, Reynolds RM, van Boeckel SR, et al. Pregnancy and COVID‐19. Physiol Rev. 2021;101(1):303‐318. doi: 10.1152/physrev.00024.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess‐etiology, diagnostic and treatment options. Ann Transl Med. 2015;3(13):183. doi: 10.3978/j.issn.2305-5839.2015.07.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Claridge JE 3rd, Attorri S, Musher DM, Hebert J, Dunbar S. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus ("Streptococcus milleri group") are of different clinical importance and are not equally associated with abscess. Clin Infect Dis. 2001;32(10):1511‐1515. doi: 10.1086/320163 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


