Abstract
Background/Aim:
Women’s knowledge of cervical cancer (CC) and awareness of screening procedures are important to improve adherence and reduce mortality. This study was conducted to determine the knowledge, attitudes, and practices toward cervical cancer and screening among sexually active Saudi females visiting a primary care center in Riyadh, Saudi Arabia.
Methods:
We conducted a cross-sectional study among sexually active Saudi females who visited the primary care center of our institution using a self-administered survey questionnaire between July and December 2020.
Results:
Six hundred and one Saudi women participated in the survey with a mean age of 34.0 ± 10.8 years. Three in four women (75.7%) were aware of cervical cancer and 325 (54.1%) believed that doing a Paps smear helped them diagnose and prevent CC. However, 479 participants (79.7%) do not see the need to go for CC screening (n = 199, 41.5%) and 113 (23.6%) had not heard of Paps smear screening. There were 109 women (18.1%) who has good knowledge of cervical cancer and screening and 492 women (81.9%) had poor knowledge.
Conclusion:
There was a high proportion of women with poor knowledge and awareness about cervical cancer and screening. Most women do not feel the need to undergo screening. Primary care physicians and healthcare providers should revisit the implementation of policies or information dissemination of programs and materials to increase awareness and knowledge for cervical cancer screening and vaccination throughout primary healthcare centers.
Keywords: Attitudes, cervical cancer, knowledge, practices, screening
Introduction
The 2020 GLOBOCAN reported a worldwide increase in the prevalence of cervical cancer (CC) with 604,000 new cases and 342,000 deaths. It remained the fourth most commonly diagnosed cancer and the fourth leading cause of cancer death among women.[1] The World Health Organization (WHO) projected the increase of CC to 700,000 between 2018 and 2030, with the annual number of deaths projected to increase from 311,000 to 400,000.[2] In 2019, various gynecologic societies and WHO considered a global strategy to accelerate the elimination of CC with measurable goals and targets.[3] These included continued vaccination, screening, and treatment programs.[2,3,4]
Screening for CC has been regarded as one of the strategic approaches to early detection of cervical cancer. Studies have shown that screening obviates the development of CC into its later stages and the institution of early management can delay the progression into the more advanced stages.[5] Screening for CC was recommended for women with average risk at ages 25 – 65 years toward primary human papilloma virus (HPV) screening every 5 years since it was regarded as a more sensitive test for cancer precursor detection and risk stratification.[6,7] A US study showed that CC screening showed college-educated women, women with a regular source of care, women who frequently consulted a physician, women who had health insurance, and women had a higher level of monthly income had more cervical cancer screening compared to their counterparts.[8] A high rate of Pap screening coverage drop was observed in many countries (30% in Brazil, 18.17% in Ethiopia, 10% in the USA, and between 5 and 59.7% in many Asian countries) and many women were out of date for regular screening.[9,10,11,12] Many women still do not participate in cervical cancer screening in many countries.
The most common barrier to CC screening is knowledge of CC and on the benefits of screening.[13,14,15] Women generally do not undergo CC screening because of poor knowledge about CC as well as stigma, embarrassment, or anxiety related to the screening procedure.[13]
Women who were highly educated were found to be 122 times more likely to be interested in CC screening.[15] Knowledge of screening and management guidelines are important to improve adherence and avoid both over- and under-use of screening and colposcopy.
Although the prevalence of CC is relatively lower (<3% prevalence of all female cancers) compared to the worldwide prevalence, the overall 3-, 5-, and 10-year reported survival rates were 64, 55, and 40%, respectively.[16] Another study showed that less than 10% of the surveyed Saudi women had good knowledge and awareness, and 70% had poor knowledge and awareness of CC risk factors and screening.[17] On the contrary, another recent study showed a high awareness (84%) of CC but only 8% gave a history of CC screening.[18] A study conducted among 2,200 women in Saudi Arabia by Alnafisah et al.[19] in 2019 showed 79% with moderate knowledge about CC symptoms, prevention, and screening, and 84.7% of them had not undergone a Pap smear test.
Several similar studies aimed to determine the knowledge, attitudes, and practices of Saudi women toward CC and screening. However, we wanted to document the updated knowledge, attitude, and practices of Saudi women toward CC and screening to see if those previous research and institutional promotion campaigns had made an impact on such knowledge, attitude, and practices. We conducted this study to determine the knowledge, attitudes, and practices toward CC and screening among sexually active Saudi females visiting the primary care center in a tertiary center in Riyadh, Saudi Arabia.
Material and Methods
We conducted a cross-sectional study among sexually active Saudi females who were visiting the primary care center in Riyadh, Saudi Arabia, using a self-administered survey questionnaire between July and December 2020. The included participants were 18 years old and above. We excluded patients who were healthcare professionals and those who had a history of CC. The sample size was calculated based on the formula n = Z2 P (1-P)/d2, where n is the sample size, Z is the statistic for the level of significance, P is the expected prevalence and d is the allowable error. The calculated sample size was 385.
The survey questionnaire was adapted from the validated questionnaire used by Alnafisah et al.[19] which included sociodemographic information of the participants, questions on knowledge of CC and its signs and symptoms, knowledge about the risk factors for CC, knowledge and attitudes toward CC prevention, and perceived barriers to CC prevention and screening. Ethical approval was obtained from the Institutional Review Board of our institution in Riyadh, Saudi Arabia. With 27 items used for the assessment of knowledge of CC, the lowest possible score was 0 (with all questions answered incorrectly) and the highest possible score was 27 (with all questions answered correctly). The mean knowledge score was taken (mean score of 16) and poor knowledge was set at least <10% of the mean score (that is 14). Statistical analysis was done using the Statistical Package for Social Sciences (SPSS) version 23.0 (SPSS Inc., IBM, Armonk, New York, USA). Responses to the survey questions were expressed as numbers and percentages. Chi-square and independent t-tests were done to determine significant differences between categorical and continuous variables. A P value of < 0.05 was considered statistically significant.
Results
Six hundred and one Saudi women participated in the survey with a mean age of 34.0 ± 10.8 years. Three hundred and ninety-one participants (65.1%) were married and 388 (64.6%) were college educated. There were 200 women (33.3%) who had a history of contraceptive use, 125 (62.5%) of which were contraceptive pills. Fifty-nine women (9.8%) were smokers. There were 38 (6.3%) women who had a family history of cervical cancer. Table 1 shows the detailed sociodemographic profile of the participants.
Table 1.
Sociodemographic profile of the 601 survey participants
| Variables | Mean±SD | n (%) |
|---|---|---|
| Age in years | 34.0±10.8 | |
| Age groups | ||
| ≤30 years old | 262 (43.6) | |
| 31-45 years old | 243 (40.4) | |
| >45 years old | 96 (16.0) | |
| Marital status | ||
| Married | 391 (65.1%) | |
| Single | 173 (28.8%) | |
| Divorced | 27 (4.5%) | |
| Widow | 10 (1.7%) | |
| Educational level | ||
| Non-educated | 4 (0.7) | |
| High school | 141 (23.5) | |
| College | 388 (64.6) | |
| Postgraduate | 51 (64.6) | |
| Others/not indicated | 17 (2.8) | |
| Use of contraception, yes | 200 (33.3) | |
| Pill | 125 (62.5) | |
| Copper IUD | 30 (15.0) | |
| Implants | 5 (2.5) | |
| Hormonal IUD | 17 (8.5) | |
| Patch | 6 (3.0) | |
| Tubal ligation | 2 (1.0) | |
| Others | 15 (7.5) | |
| Smoking, yes | 59 (9.8) | |
| Cigarette | 12 (20.3) | |
| Electronic cigarette/vape | 10 (17.0) | |
| Hubble bubble | 35 (59.3) | |
| Others | 2 (3.4) | |
| With family history of cervical cancer | 38 (6.3) |
Table 2 shows the responses to questions about knowledge about CC, knowledge of signs and symptoms of CC, and knowledge of the risk factors for CC of 601 Saudi women. Three in four women (75.7%) heard of CC. The majority of these women (n = 573, 95.3%) thought that CC can be treated and 540 (89.9%) thought that it is a preventable disease. Three hundred and twenty-five participants (54.1%) believed that doing a Paps smear helps them diagnose and prevent CC. However, less than half of the participants (n = 253, 42.1%) knew that a Paps smear should be done every 3 years. Less than half of the participants knew any of the symptoms of CC. One hundred and forty-three participants (53.1%) believed that a positive family history of CC predisposes one to CC. There were less than 50% of women surveyed who believed that the use of contraceptive pills for a long time, smoking, HIV, multiple sexual partners, smoking, and HPV are risk factors for CC.
Table 2.
Responses to questions on knowledge of cervical cancer, screening, symptoms, and risk factors among 601 Saudi women
| Questions | n (%) |
|---|---|
| Knowledge of cervical cancer | |
| Heard about cervical cancer, yes | 455 (75.7) |
| Knows anyone with cervical cancer, yes | 55 (9.2) |
| Thinks that cervical cancer can be treated, yes | 573 (95.3) |
| Thinks that cervical cancer can be prevented, yes | 540 (89.9) |
| Heard about human papilloma virus (HPV), yes | 125 (20.8) |
| Heard about Paps smear, yes | 439 (73.0) |
| Prevention of cervical cancer* | |
| Paps smear | 325 (54.1) |
| Early diagnosis | 351 (58.4) |
| HPV vaccination | 139 (23.1) |
| Use of condom during sexual intercourse | 49 (8.2) |
| Quit smoking | 174 (29.0) |
| Regular check-up | 494 (82.2) |
| Use of barrier contraceptives | 18 (3.0) |
| Frequency of doing Paps smear test | |
| Every year | 321 (53.4) |
| Every three years | 253 (42.1) |
| Once in a lifetime | 27 (4.5) |
| Thinks that HPV vaccine is effective for prevention of cervical cancer | 450 (74.9) |
| Knowledge of symptoms* | |
| Post-menopausal bleeding | 271 (45.1) |
| Bleeding and pain during sex | 232 (38.6) |
| Excessive vaginal discharge | 174 (29.0) |
| Bleeding between menstrual periods | 252 (41.9) |
| Others | 139 (23.1) |
| Knowledge of risk factors for cervical cancer* | |
| Use of contraceptive pills for a long time | 260 (43.3) |
| Smoking | 164 (27.3) |
| Sexually transmitted disease | 244 (40.6) |
| Family history of cervical cancer | 319 (53.1) |
| Human immunodeficiency virus | 143 (23.8) |
| Early onset of sexual activity | 46 (7.7) |
| Multiple sexual partners | 290 (48.3) |
| Human papilloma virus | 176 (29.3) |
| Living with a cervical cancer patient | 15(2.5) |
*Multiple response question
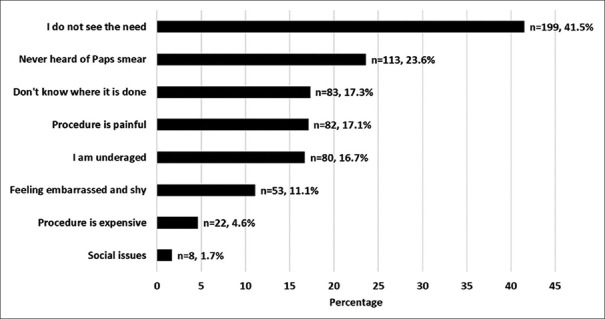
There were 479 participants (79.7%) who had not gone for CC screening. The most common reason was that they did not see the need to go for CC screening (n = 199, 41.5%) followed by “not heard of Paps smear screening” (n = 113, 23.6%) and screening is painful (n = 82, 17.1%). [Figure 1] The most common source of information among the participants was social media (n = 214, P = 35.6%) [Figure 2].
Figure 1.
Reasons why 479 of 601 women participants do not go for CC screening
Figure 2.
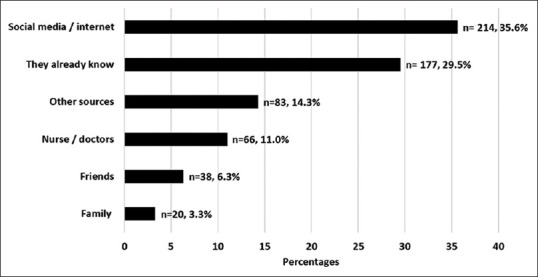
Sources of information and knowledge of CC among 601 participants 177
There were only 109 women (18.1%) who had good knowledge of CC and cervical screening and 492 women (81.9%) had poor knowledge of CC and screening. The level of knowledge of CC was significantly correlated with the level of education (r = 0.101, P = 0.014). There were significantly more women who had a college degree and above who had good knowledge than those who had high school and less education (n = 91/109, 83.5% versus n = 16/109, 14.7%, P = 0.016). There were no significant differences in the proportion of patients who had poor and good knowledge based on marital status and having a family history of CC (P = 0.162 and P = 0.667, respectively). There was also no significant differences in the mean age of participants as to their knowledge of CC (poor knowledge = 34.5 ± 11.1 years versus good = 34.0 ± 9.5 years, P = 0.696). The level of knowledge was also significantly correlated with the feeling of embarrassment toward CC screening (r = -0.119, P = 0.009), and Paps smear is a painful procedure (r = 0.093, P = 0.043).
Discussion
This study aimed to determine the knowledge, attitudes, and practices toward CC and screening among sexually active Saudi females. Although CC is relatively uncommon in Saudi Arabia, it is well-known that women of the reproductive age and those who are sexually active are most vulnerable and are the most exposed to the development of CC.
This study showed that the majority of our respondents (81.9%) had poor knowledge of CC and CC screening. Our study showed a higher rate of poor awareness and knowledge with rates from India (69.39%), China (48.9%), Iran (29.1%), Qatar (15-20%), and Kuwait (47.7%) to name a few.[20,21,22,23,24] The wide variations in the reported rates may be due to the differences in the study designs and the characteristics of the respondents, the questionnaire survey as well as other factors that may have affected the outcome of the statistical result. However, based on how much percentage of our women who have heard of CC, our results were far better at 75.7% compared to the countries that were mentioned earlier.[20,21,22,23,24] Furthermore, our study showed that 54.1% of our respondents believed that doing a Paps smear helps them diagnose and prevent CC, although 79.7% of these women have not gone for CC screening, which was far better than the approximately 95% of surveyed women in Jordan who had never undergone a Paps smear, but our rate had a higher percentage of non-screening compared to other Middle East countries like Kuwait (63%) and Jordan.[25,26,27] Many previous studies conducted in Saudi Arabia showed high rates of non-screening for CC.[17,28,29,30]
Another finding of this study was that of the 479 participants who did not undergo CC screening, 199 perceived that Paps smear was not necessary and some 113 participants had not even heard of Paps smear as a screening tool for CC. This is alarming because it reflects poor knowledge and poor attitude toward CC and CC screening. In contrast to the study done by Sait et al.[28] in 2019, 67.6% of participants were aware of the Paps smear test, but only 16.8% had been screened mainly due to lack of awareness. In another study conducted in Saudi Arabia, 42.8% refused to undergo a Paps smear because they did not know someone who had tried a Paps smear.[19] Several other major reasons for not undergoing Paps smear such as fear and painful procedure were not expressed much by our survey respondents. Instead, a majority of our participants said that “they do not see the need for CC screening.”
The importance of CC screening apart from knowledge about CC, its risk factors, and its clinical signs and symptoms has to be relayed to women who are of reproductive age. The importance and benefit of vaccination against HPV as a preventive measure have to be consistently allied to primary health care services to decrease the morbidity and mortality of CC. Having a high level of awareness or knowledge of CC has to be translated to prevention and action toward vaccination and increased uptake of screening procedures such as Paps smear. This has to be done in our population since our study results showed that despite 54.1% believing that doing a Paps smear helps them diagnose and prevent CC, many still do not undergo CC screening for reasons that can easily be addressed by proper information-dissemination and education of these women. Furthermore, this study highlighted which particular women sectors needed a heightening drive for such information-dissemination campaigns, i.e., lower educated women and women in past their 40s.
Comparing our results with similar previous studies conducted in Saudi Arabia showed that a high proportion of women still have poor knowledge, poor attitude, and poor awareness about cervical cancer and screening. This implies that the promotion campaigns toward awareness, knowledge, and actions set by our authorities have not been fully met. Primary care physicians who are on the frontlines of care and who are in contact with women in the rural areas have a greater advantage of promoting awareness, vaccination campaigns, and re-education toward CC awareness and CC screening. Primary care physicians should be encouraged to educate and promote awareness among Saudi women, and educational intervention programs should be part of their training and expertise. Despite so many papers that have been published on CC and screening, there seems to be a continuous rise in the prevalence of CC as a major cause of mortality among women, and Saudi Arabia is not spared from this. Despite so much research on the need to educate women on CC and screening procedures who are vulnerable and who are at high risk for CC, there is still a high proportion of women who do not go for screening. This will be a never-ending story; thus, we recommend that strategies are actively implemented to screen, vaccinate, and continuously educate women on CC and screening to the grassroots through schools, universities, healthcare providers, and social media. Primary care physicians and healthcare workers in the suburbs and rural areas should incorporate in their program a regular home visit to deliver the message to increase awareness, knowledge, and uptake of CC screening. All of these measures will improve CC awareness and increase the uptake of CC screening, and hopefully decrease the morbidity and mortality of CC in the future.
Since this study was conducted in a single primary care center of an institution, this may not reflect the entire picture of the general female population of Saudi Arabia when it comes to CC and CC screening which serves as a limitation to the study. However, despite this, we were able to deduce new information such as many women do not find the need to undergo screening, which is a major barrier to CC screening. It would certainly be a demanding task for doctors and healthcare providers to institute measures to offer women CC screening, education, vaccination, and follow-ups, however, if such steps will be taken seriously and consistently, step by step, the desired outcome will be achieved.
Conclusion
The current study demonstrated a high proportion of poor knowledge and awareness about cervical cancer and screening among the surveyed Saudi women. The most common reason for refusal to subject themselves to screening is that they do not feel the need to undergo screening. Primary care physicians and healthcare providers should revisit the implementation of policies or information dissemination of programs and materials to increase awareness and knowledge for cervical cancer screening and vaccination throughout the primary healthcare centers.
Key points and take-home messages
There is still a high prevalence of poor knowledge of cervical cancer, poor attitude, and poor practice toward cervical screening among Saudi women attending the primary care centers despite several types of research and institutional efforts that are recommended to increase awareness and promote screening for cervical cancer. Many women do not want to undergo CC screening because they do not feel the need to undergo screening.
A dedicated approach is required particularly among primary care physicians to include in their program the promotion and education of women regarding cervical cancer and the importance of CC screening. It must be part of primary care physicians discussion with their patients who are in the reproductive age, re-educate and heighten awareness about cervical cancer and discuss the benefits of CC screening and vaccination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Gultekin M, Ramirez PT, Broutet N, Hutubessy R. World Health Organization call for action to eliminate cervical cancer globally. Int J Gynecol Cancer. 2020;30:426–7. doi: 10.1136/ijgc-2020-001285. [DOI] [PubMed] [Google Scholar]
- 3.ESGO. Message from the ESGO president:ESGO at war with cervical cancer. [Last accessed on 2021 Sep 20]. Available: https://www.esgo.org/explore/council/esgo-cooperation-with-who/
- 4.IGCS. IGCS statement in support of the WHO initiative for the elimination of cervical cancer. [Last accessed on 2021 Sep 20]. Available: https://igcs.org/wp-content/uploads/2019/01/IGCS-Statement-in-Support-of-WHO-Initiative-to-Eliminate-Cervical-Cancer.pdf .
- 5.Shah V, Vyas S, Singh A, Shrivastava M. Awareness and knowledge of cervical cancer and its prevention among the nursing staff of a tertiary health institute in Ahmedabad, Gujarat, India. Ecancermedicalscience. 2012;6:1–6. doi: 10.3332/ecancer.2012.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fontham ET, Wolf AM, Church TR, Etzioni R, Flowers CR, Herzig A, et al. Cervical cancer screening for individuals at average risk:2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321–46. doi: 10.3322/caac.21628. [DOI] [PubMed] [Google Scholar]
- 7.Perkins RB, Guido RL, Saraiya M, Sawaya GF, Wentzensen N, Schiffman M, et al. Summary of current guidelines for cervical cancer screening and management of abnormal test results:2016–2020. J Womens Health. 2021;30:5–13. doi: 10.1089/jwh.2020.8918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donley T, Tshiswaka DI, Blanc J, Seixas A, Okafor A, Mbizo J. Differences in breast and cervical cancer screening among US women by nativity and family history. Am J Prev Med. 2020;59:578–87. doi: 10.1016/j.amepre.2020.05.018. [DOI] [PubMed] [Google Scholar]
- 9.Teixeira JC, Vale DB, Bragança JF, Campos CS, Discacciati MG, Zeferino LC. Cervical cancer screening program based on primary DNA-HPV testing in a Brazilian city:A cost-effectiveness study protocol. BMC Public Health. 2020;20:1–8. doi: 10.1186/s12889-020-08688-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dessalegn Mekonnen B. Cervical cancer screening uptake and associated factors among HIV-Positive women in Ethiopia:A systematic review and meta-analysis. Adv Prev Med. 2020;2020:7071925. doi: 10.1155/2020/7071925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Cancer screening-United States, 2010. MMWR. Morb Mortal Wkly Rep. 2012;61:41–5. [PubMed] [Google Scholar]
- 12.Aoki ES, Yin R, Li K, Bhatla N, Singhal S, Ocviyanti D, et al. National screening programs for cervical cancer in Asian countries. J Gynecol Oncol. 2020;31:e55. doi: 10.3802/jgo.2020.31.e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dsouza JP, Van den Broucke S, Pattanshetty S, Dhoore W. Exploring the barriers to cervical cancer screening through the lens of implementers and beneficiaries of the national screening program:A multi-contextual study. Asian Pac J Cancer Prev. 2020;21:2209–15. doi: 10.31557/APJCP.2020.21.8.2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liebermann EJ, VanDevanter N, Shirazian T, Frias Guzman N, Niles M, Healton C, et al. Barriers to cervical cancer screening and treatment in the Dominican Republic:Perspectives of focus group participants in the Santo Domingo area. J Transcult Nurs. 2020;31:121–7. doi: 10.1177/1043659619846247. [DOI] [PubMed] [Google Scholar]
- 15.Ampofo AG, Adumatta AD, Owusu E, Awuviry-Newton K. A cross-sectional study of barriers to cervical cancer screening uptake in Ghana:An application of the health belief model. PLoS One. 2020;15:e0231459. doi: 10.1371/journal.pone.0231459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manji M. Cervical cancer screening program in Saudi Arabia:Action is overdue. (Editorial) Ann Saud Med. 2000;20:355–7. doi: 10.5144/0256-4947.2000.355. [DOI] [PubMed] [Google Scholar]
- 17.Alshahrani M, Sultan SA. Awareness and attitude to the risk of cervical cancer and screening methods among women in the Najran Region of Southern Saudi Arabia. Res Square. 2020;1:1–3. [Google Scholar]
- 18.Akkour K, Arafah M, Alghosun L, Alhalal H, Bassi A, Alayed N, et al. Cervical cancer and human papillomavirus awareness, vaccine status and risk factors among women in Saudi Arabia. Int J Gynecol Cancer. 2020;30:A110–1. [Google Scholar]
- 19.Alnafisah RA, Alsuhaibani RA, Alharbi MA, Alsohaibani AA, Ismai AA. Saudi women's knowledge and attitude toward cervical cancer screening, treatment, and prevention:A cross-sectional study in Qassim Region (2018-2019) Asian Pac J Cancer Prev. 2019;20:2965–9. doi: 10.31557/APJCP.2019.20.10.2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alnafisah RA, Alsuhaibani R, Alharbi MA, Alsohaibani AA, Ismail AA. Saudi Women's Knowledge and Attitude toward-cervical cancer screening, treatment and prevention:A cross-sectional study in Qassim Region (2019-2019) Asian Pac J Cancer Prev. 2019;20:2965–9. doi: 10.31557/APJCP.2019.20.10.2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manikandan S, Behera S, Naidu NM, Angamuthu V, Mohammed OF, Debata A. Knowledge and awareness toward cervical cancer screening and prevention among the professional college female students. J Pharm Bioallied Sci. 2019;11(Suppl 2):S314–20. doi: 10.4103/JPBS.JPBS_21_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu T, Li S, Ratcliffe J, Chen G. Assessing knowledge and attitudes toward cervical cancer screening among rural women in Eastern China. Int J Environ Res Public Health. 2017;14:967. doi: 10.3390/ijerph14090967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asgarlou Z, Tehrani S, Asghari E, Arzanlou M, Naghavi-Behzad M, Piri R, et al. Cervical cancer prevention knowledge and attitudes among female university students and hospital staff in Iran. Asian Pac J Cancer Prev. 2016;17:4921–7. doi: 10.22034/APJCP.2016.17.11.4921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al Meer FM, Aseel MT, Al Khalaf J, Al Kuwari MG, Ismail MF. Knowledge, attitude and practices regarding cervical cancer and screening among women visiting primary health care in Qatar. East Mediterr Health J. 2011;17:855–61. doi: 10.26719/2011.17.11.856. [DOI] [PubMed] [Google Scholar]
- 25.Al Sairafi M, Mohamed FA. Knowledge, attitudes, and practice related to cervical cancer screening among Kuwaiti women. Med Princ Pract. 2009;18:35–42. doi: 10.1159/000163044. [DOI] [PubMed] [Google Scholar]
- 26.Amarin ZO, Badria LF, Obeidat BR. Attitudes and beliefs about cervical smear testing in ever-married Jordanian women. East Mediterr Health J. 2008;14:389–97. [PubMed] [Google Scholar]
- 27.El-Hammasi K, Samir O, Kettaneh S, Al-Fadli A, Thalib L. Use of and attitudes and knowledge about Pap smears among women in Kuwait. J Womens Health. 2009;18:1825–32. doi: 10.1089/jwh.2008.1227. [DOI] [PubMed] [Google Scholar]
- 28.Barghouti FF, Takruri AH, Froelicher ES. Awareness and behavior about Pap smear testing in family medicine practice. Saudi Med J. 2008;29:1036–40. [PubMed] [Google Scholar]
- 29.Sait KH. Attitudes, knowledge, and practices in relation to cervical cancer and its screening among women in Saudi Arabia. Saudi Med J. 2009;30:1208–12. [PubMed] [Google Scholar]
- 30.AlAyadhi D, Alyousif G, Alharbi A, Alnjeidi Z, El-Metwally A. Systematic review:Awareness, knowledge, attitude, and practice of cancer screening program in the kingdom of Saudi Arabia. Dr. Sulaiman Al Habib Medical J. 2020;2:151–61. [Google Scholar]
- 31.Al-Qasem MH, Badar O, Abokathiyah AM. Awareness, knowledge and practice of adult Saudi females about cervical cancer screening, in Aseer Region, Saudi Arabia. MEJFM. 2020;18:13–9. [Google Scholar]